Содержание
- 2. Cartilages The human skeleton is initially made up of cartilages and fibrous membranes , then they
- 3. Growth of cartilage cartilage has a flexible matrix which can accommodate mitosis. So it’s ideal to
- 5. Function of bones Support : bones supports the body and cradles its soft organs ,ex, low
- 6. Bone structure Bones are organs because they contains different types of tissues , so bone structure
- 7. 3. Long bones : diaphysis is the part that form the long axis of the bone
- 8. Location of hematopoietic tissue in bones : hematopoietic tissue , red marrow , is found in
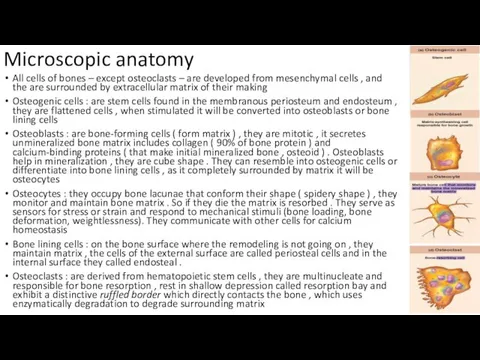
- 10. Microscopic anatomy All cells of bones – except osteoclasts – are developed from mesenchymal cells ,
- 11. Compact bone Osteon ( Haversian system ) : is the structural unit of the compact bone
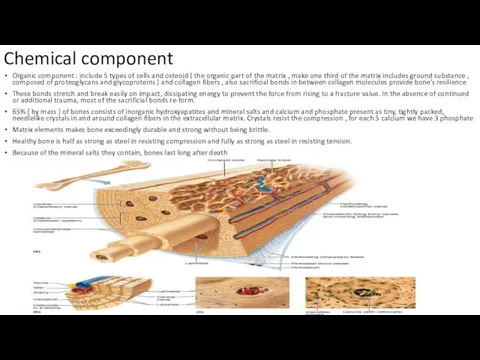
- 12. Chemical component Organic component : include 5 types of cells and osteoid ( the organic part
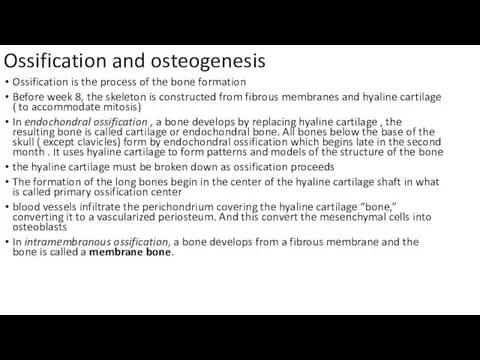
- 13. Ossification and osteogenesis Ossification is the process of the bone formation Before week 8, the skeleton
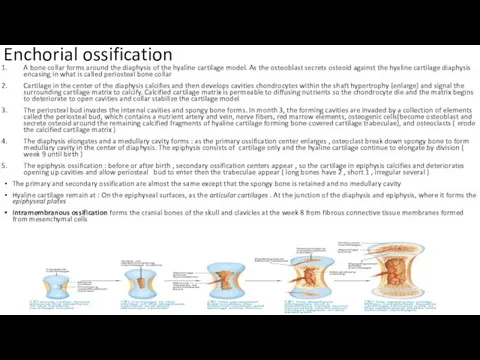
- 14. Enchorial ossification A bone collar forms around the diaphysis of the hyaline cartilage model. As the
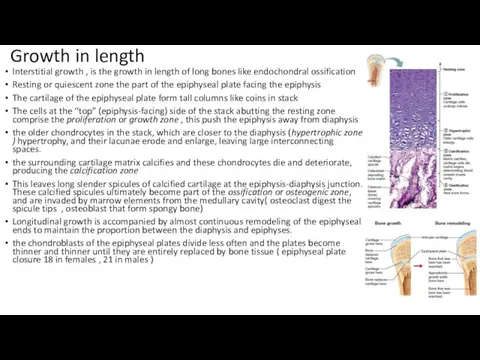
- 15. Growth in length Interstitial growth , is the growth in length of long bones like endochondral
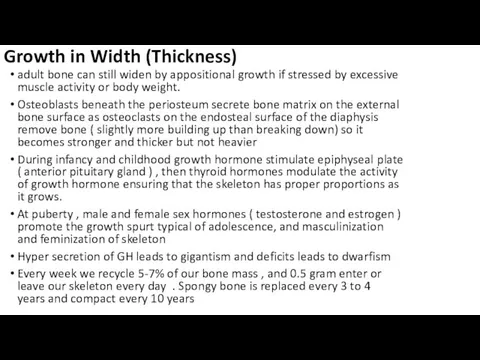
- 16. Growth in Width (Thickness) adult bone can still widen by appositional growth if stressed by excessive
- 17. Bone remodeling bone deposit and bone resorption occur at the surfaces of both the periosteum and
- 18. Calcium is absorbed from the intestine under the control of vitamin D metabolites The daily dietary
- 20. Bone Repair Fractures may be classified by : Position of the bone ends after fracture: In
- 22. Скачать презентацию
Cartilages
The human skeleton is initially made up of cartilages and
Cartilages
The human skeleton is initially made up of cartilages and
Skeletal cartilage is made of cartilage tissue molded to fit its body location and function
Cartilages consists mainly of water that give them resilience ( spring back to original shape )
Cartilage doesn’t have nerves or blood vessels , but it is surrounded by a layer of dense irregular connective tissue ( perichondrium ) that prevent outward expansion
The perichondrium contains blood vessels from which nutrients diffuse through the matrix to reach the cartilage cells internally , and this limit the cartilage thickness
There are three types of cartilages in the body : hyaline, elastic, and fibrocartilage. They have all the basic components cells called chondrocytes, encased in small cavities (lacunae) within an extracellular matrix containing a jellylike ground substance and fibers.
Hyaline cartilages, are the most abundant , which look like frosted glass , provide support with flexibility and resilience. They have spherical chondrocyte and fine collagen fibers ( not detected by microscope ) , they include :
Articular cartilages : cover bones at movable joints
Costal cartilages : connect ribs to sternum
Respiratory cartilages : in larynx (voicebox) and reinforce other respiratory passageways
Nasal cartilages : support external nose
Elastic cartilages resemble hyaline cartilages , they contain more stretchy elastic fibers ,they can found the external ear and the epiglottis (the flap that bends to cover the opening of the larynx each time we swallow).
Fibrocartilages Highly compressible with great tensile strength consist of roughly parallel rows of chondrocytes alternating with thick collagen fibers , are found in site that are subjected to both pressure and stretch (menisci) of the knee and the discs between vertebrae,
Growth of cartilage
cartilage has a flexible matrix which can accommodate mitosis.
Growth of cartilage
cartilage has a flexible matrix which can accommodate mitosis.
Growth can be appositional growth , cartilages form cells in the perichondrium that secrete matrix on the external face of the existing cartilages
Interstitial growth ,the lacunae divide and produce new matrix so expanding the cartilage within
Cartilage growth ends during adolescence when the skeleton stops growing.
calcified cartilage is not bone; cartilage and bone are always distinct tissues
There are 206 bones in our bodies classified into
axial skeleton ( form the long axis of the body ex, bone of skull , vertebral column , rib cage ,and serve to protect and support or carry other body parts )
Appendicular skeleton : ( upper and lower limbs and girdles- shoulder and hip bones that attach limbs to axial skeleton – bones of the limbs help in movement and manipulate our environment )
There are other classification based on shape and size , these differences help in serve and function in different areas , as femur long bone with hollow-cylinder that provide the strength with minimum weight , classes of bones :
Long bones : are considerably longer than they are wide , and has a shaft and two expanded ends all limbs bones except wrist patella and ankle ( fingers are long bones even they are small as classification based on elongation not overall size )
Short bones : are cube shaped bones like in ankle and wrist
Sesamoid bones : have a shape like sesame , are special type of short bones that form in tendon ( patella) , they act to alter the direction of pull of a tendon
Flat bones : are flattened ( sternum or breast bone , scapulae , ribs , skull bones )
Irregular bones : have a complicated shape include the vertebrae and hip bones
Function of bones
Support : bones supports the body and cradles
Function of bones
Support : bones supports the body and cradles
Protection : as they protect the brain , and vertebrae that protect spinal cord , and rib cage protects organs of the thoracic cavity
Movement : the muscles use bones as leavers to move the body parts
Mineral and growth factor storage. Bone is a reservoir for minerals, most importantly calcium and phosphate, these minerals are released into the bloodstream in the ionic form when needed , and bone matrix stores important growth factors.
Blood cell formation : most blood cell formation ( hematopoiesis ) occur in red marrow cavities of certain bones
Triglyceride ( fat ) : can be stored in the bone cavity
Hormone production : Bones produce osteocalcin, a hormone which not only helps regulate bone formation, but also protects against obesity, glucose intolerance, and diabetes mellitus.
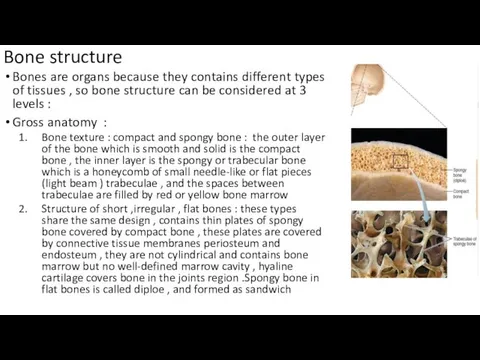
Bone structure
Bones are organs because they contains different types of tissues
Bone structure
Bones are organs because they contains different types of tissues
Gross anatomy :
Bone texture : compact and spongy bone : the outer layer of the bone which is smooth and solid is the compact bone , the inner layer is the spongy or trabecular bone which is a honeycomb of small needle-like or flat pieces (light beam ) trabeculae , and the spaces between trabeculae are filled by red or yellow bone marrow
Structure of short ,irregular , flat bones : these types share the same design , contains thin plates of spongy bone covered by compact bone , these plates are covered by connective tissue membranes periosteum and endosteum , they are not cylindrical and contains bone marrow but no well-defined marrow cavity , hyaline cartilage covers bone in the joints region .Spongy bone in flat bones is called diploe , and formed as sandwich
3. Long bones :
diaphysis is the part that form
3. Long bones :
diaphysis is the part that form
Epiphyses : are the two wide ends portions of the long bone , consists of outer shell of compact bone covers the inner spongy bone . There is epiphyseal line between diaphysis and epiphysis , a remnant of the epiphyseal plate , a disc of hyaline cartilage that grows during childhood to lengthen the bone . articular (hyaline) cartilage covers the joint surface of each epiphysis, cushioning the opposing bone ends during movement and absorbing stress.
The region where epiphysis meets diaphysis and contains epiphyseal plate or line is sometimes called metaphysis
membranes : periosteum is a glistening white double layered of connective tissue covers the outer surface of the bone The outer fibrous layer of the periosteum is dense irregular connective tissue. The inner osteogenic layer, consists mainly of primitive stem cells ( osteogenic cells) that give arise the all types of bone cells except osteoclast . The periosteum is supplied with nerves and blood vessels and these enter the bone marrow through nutrient foramina . Proliferating ( sharpey’s ) fibers tufts of collagen fibers that extend from its fibrous layer into the bone matrix to secure the periosteum to the underlying bone . The periosteum provide anchoring points for tendons and ligaments. Another delicate membrane cover the inner surface of the bone ( trabeculae and lines the canals of compact bones) and it also contains osteogenic cells
Location of hematopoietic tissue in bones : hematopoietic tissue , red
Location of hematopoietic tissue in bones : hematopoietic tissue , red
bone markings serve as sites of muscle, ligament, and tendon attachment, as joint surfaces, or as conduits for blood vessels and nerves. They can be projections ( heads , trochanters , spines ) projections indicate the stresses created by muscles attached to and pulling on them, or depression or opening (fossae , sinuses, foramina, grooves )
Microscopic anatomy
All cells of bones – except osteoclasts – are
Microscopic anatomy
All cells of bones – except osteoclasts – are
Osteogenic cells : are stem cells found in the membranous periosteum and endosteum , they are flattened cells , when stimulated it will be converted into osteoblasts or bone lining cells
Osteoblasts : are bone-forming cells ( form matrix ) , they are mitotic , it secretes unmineralized bone matrix includes collagen ( 90% of bone protein ) and calcium-binding proteins ( that make initial mineralized bone , osteoid ) . Osteoblasts help in mineralization , they are cube shape . They can resemble into osteogenic cells or differentiate into bone lining cells , as it completely surrounded by matrix it will be osteocytes
Osteocytes : they occupy bone lacunae that conform their shape ( spidery shape ) , they monitor and maintain bone matrix . So if they die the matrix is resorbed . They serve as sensors for stress or strain and respond to mechanical stimuli (bone loading, bone deformation, weightlessness). They communicate with other cells for calcium homeostasis
Bone lining cells : on the bone surface where the remodeling is not going on , they maintain matrix , the cells of the external surface are called periosteal cells and in the internal surface they called endosteal .
Osteoclasts : are derived from hematopoietic stem cells , they are multinucleate and responsible for bone resorption , rest in shallow depression called resorption bay and exhibit a distinctive ruffled border which directly contacts the bone , which uses enzymatically degradation to degrade surrounding matrix
Compact bone
Osteon ( Haversian system ) : is the structural unit
Compact bone
Osteon ( Haversian system ) : is the structural unit
tiny crystals of bone salts align between the collagen fibrils and thus also alternate their direction in adjacent lamellae.
Canals and Canaliculi Running through the core of each osteon is the central canal, or Haversian canal , contains blood vessels and nerve fibers
Perforating canals ( Volkmann canals ) lie at right angles to the long axis of the bone and connect the blood and nerve supply of the periosteum to those in the central canals and the medullary cavity , these canals aren’t surrounded by concentric lamellae , but they are lined with endosteum
Canaliculi are hair like canal connect the lacunae with each other
the osteoblasts secreting bone matrix surround blood vessels and maintain contact with one another and local osteocytes by tentacle-like projections containing gap junctions
interstitial lamellae Lying between Intact osteons are incomplete lamellae , they either fill the gaps between forming osteons or are remnants of osteons that have been cut through by bone remodeling
Circumferential lamellae, located just deep to the periosteum and just superficial to the endosteum
Spongy bone : is poorly organized , the trabecula in spongy bone align along lines of stress and help resist stress
Only a few cells thick, trabeculae contain irregularly arranged lamellae and osteocytes interconnected by canaliculi
There is no osteons are present in spongy bone , so they diffuse nutrients through canaliculi
Chemical component
Organic component : include 5 types of cells and
Chemical component
Organic component : include 5 types of cells and
These bonds stretch and break easily on impact, dissipating energy to prevent the force from rising to a fracture value. In the absence of continued or additional trauma, most of the sacrificial bonds re-form.
65% ( by mass ) of bones consists of inorganic hydroxyapatites and mineral salts and calcium and phosphate present as tiny, tightly packed, needlelike crystals in and around collagen fibers in the extracellular matrix. Crystals resist the compression , for each 5 calcium we have 3 phosphate
Matrix elements makes bone exceedingly durable and strong without being brittle.
Healthy bone is half as strong as steel in resisting compression and fully as strong as steel in resisting tension.
Because of the mineral salts they contain, bones last long after death
Ossification and osteogenesis
Ossification is the process of the bone formation
Before
Ossification and osteogenesis
Ossification is the process of the bone formation
Before
In endochondral ossification , a bone develops by replacing hyaline cartilage , the resulting bone is called cartilage or endochondral bone. All bones below the base of the skull ( except clavicles) form by endochondral ossification which begins late in the second month . It uses hyaline cartilage to form patterns and models of the structure of the bone
the hyaline cartilage must be broken down as ossification proceeds
The formation of the long bones begin in the center of the hyaline cartilage shaft in what is called primary ossification center
blood vessels infiltrate the perichondrium covering the hyaline cartilage “bone,” converting it to a vascularized periosteum. And this convert the mesenchymal cells into osteoblasts
In intramembranous ossification, a bone develops from a fibrous membrane and the bone is called a membrane bone.
Enchorial ossification
A bone collar forms around the diaphysis of the hyaline
Enchorial ossification
A bone collar forms around the diaphysis of the hyaline
Cartilage in the center of the diaphysis calcifies and then develops cavities chondrocytes within the shaft hypertrophy (enlarge) and signal the surrounding cartilage matrix to calcify. Calcified cartilage matrix is permeable to diffusing nutrients so the chondrocyte die and the matrix begins to deteriorate to open cavities and collar stabilize the cartilage model
The periosteal bud invades the internal cavities and spongy bone forms. In month 3, the forming cavities are invaded by a collection of elements called the periosteal bud, which contains a nutrient artery and vein, nerve fibers, red marrow elements, osteogenic cells(become osteoblast and secrete osteoid around the remaining calcified fragments of hyaline cartilage forming bone-covered cartilage trabeculae), and osteoclasts ( erode the calcified cartilage matrix )
The diaphysis elongates and a medullary cavity forms : as the primary ossification center enlarges , osteoclast break down spongy bone to form medullary cavity in the center of diaphysis. The epiphysis consists of cartilage only and the hyaline cartilage continue to elongate by division ( week 9 until birth )
The epiphysis ossification : before or after birth , secondary ossification centers appear , so the cartilage in epiphysis calcifies and deteriorates opening up cavities and allow periosteal bud to enter then the trabeculae appear ( long bones have 2 , short 1 , irregular several )
The primary and secondary ossification are almost the same except that the spongy bone is retained and no medullary cavity
Hyaline cartilage remain at : On the epiphyseal surfaces, as the articular cartilages . At the junction of the diaphysis and epiphysis, where it forms the epiphyseal plates
Intramembranous ossification forms the cranial bones of the skull and clavicles at the week 8 from fibrous connective tissue membranes formed from mesenchymal cells
Growth in length
Interstitial growth , is the growth in length
Growth in length
Interstitial growth , is the growth in length
Resting or quiescent zone the part of the epiphyseal plate facing the epiphysis
The cartilage of the epiphyseal plate form tall columns like coins in stack
The cells at the “top” (epiphysis-facing) side of the stack abutting the resting zone comprise the proliferation or growth zone , this push the epiphysis away from diaphysis
the older chondrocytes in the stack, which are closer to the diaphysis (hypertrophic zone ) hypertrophy, and their lacunae erode and enlarge, leaving large interconnecting spaces.
the surrounding cartilage matrix calcifies and these chondrocytes die and deteriorate, producing the calcification zone
This leaves long slender spicules of calcified cartilage at the epiphysis-diaphysis junction. These calcified spicules ultimately become part of the ossification or osteogenic zone, and are invaded by marrow elements from the medullary cavity( osteoclast digest the spicule tips , osteoblast that form spongy bone)
Longitudinal growth is accompanied by almost continuous remodeling of the epiphyseal ends to maintain the proportion between the diaphysis and epiphyses.
the chondroblasts of the epiphyseal plates divide less often and the plates become thinner and thinner until they are entirely replaced by bone tissue ( epiphyseal plate closure 18 in females , 21 in males )
Growth in Width (Thickness)
adult bone can still widen by appositional growth
Growth in Width (Thickness)
adult bone can still widen by appositional growth
Osteoblasts beneath the periosteum secrete bone matrix on the external bone surface as osteoclasts on the endosteal surface of the diaphysis remove bone ( slightly more building up than breaking down) so it becomes stronger and thicker but not heavier
During infancy and childhood growth hormone stimulate epiphyseal plate ( anterior pituitary gland ) , then thyroid hormones modulate the activity of growth hormone ensuring that the skeleton has proper proportions as it grows.
At puberty , male and female sex hormones ( testosterone and estrogen ) promote the growth spurt typical of adolescence, and masculinization and feminization of skeleton
Hyper secretion of GH leads to gigantism and deficits leads to dwarfism
Every week we recycle 5-7% of our bone mass , and 0.5 gram enter or leave our skeleton every day . Spongy bone is replaced every 3 to 4 years and compact every 10 years
Bone remodeling
bone deposit and bone resorption occur at the surfaces of
Bone remodeling
bone deposit and bone resorption occur at the surfaces of
adjacent osteoblasts and osteoclasts called remodeling units coordinate bone remodeling (with help from the stress sensing osteocytes).
In healthy young adults, total bone mass remains constant, an indication that the rates of bone deposit and resorption are essentially equal
Different parts of bone are replaced in different rate
Osteoid seam is an unmineralized band of gauzy looking bone matrix 10-12 micrometers , Between the osteoid seam and the older mineralized bone, there is an abrupt transition called the calcification front.
the osteoid must mature for about a week before it can calcify.
concentrations of calcium and phosphate (Pi) ions (the Ca2+・Pi product) in the endosteal cavity will help in control of remodeling .
tiny crystals of hydroxyapatite form spontaneously and catalyze further crystallization of calcium salts in the area.
Other factors involved are matrix proteins that bind and concentrate calcium, and the enzyme alkaline phosphatase (shed in matrix vesicles by the osteoblasts), which is essential for mineralization
the giant osteoclasts accomplish bone resorption.
Osteoclasts move along a bone surface, digging depressions or grooves as they break down the bone matrix , and Lysosomal enzymes that digest the organic matrix and protons (H+ ) , then they will be converted into soluble form
Osteoclasts may also phagocytize the demineralized matrix and dead osteocytes , and endocytoses GF and minerals and transport them through transcytosis
The human body contains 1200–1400 g of calcium, more than 99% present as bone minerals and less than 1.5 in blood
control loop normally maintains blood Ca21 within the narrow range of 9–11 mg per dl (100 ml) of blood
Calcium is absorbed from the intestine under the control of vitamin
Calcium is absorbed from the intestine under the control of vitamin
The daily dietary calcium requirement is 400–800 mg from birth until age 10, and 1200–1500 mg from ages 11 to 24.
parathyroid hormone (PTH), produced by the parathyroid glands. And calcitonin by parafollicular cells (C cells) of the thyroid gland , involve in control loop
The increased PTH level stimulates osteoclasts ( not specific , in old and new ) to resorb bone, releasing calcium into blood
Calcitonin lowers blood calcium levels temporarily
leptin, a hormone released by adipose tissue, plays a role in regulating bone density, leptin appears to inhibit osteoblasts through additional pathway mediated by hypothalamus
Serotonin reduces the bone turnover after eating and lock calcium of the bone , some antidepressant can inhibit serotonin so causes lower bone density and more fractures
bone’s response to mechanical stress (muscle pull) and gravity, keeps the bones strong where stressors are acting
Wolff’s law holds that a bone grows or remodels in response to the demands placed on it.
Bone is subjected to compression ( bending the bone ) and tension ( stretching the bone )
As a result of these mechanical stressors, long bones are thickest midway along the diaphysis, exactly where bending stresses are greatest (bend a stick and it will split near the middle). And both tension and compression cancel each other internally, much less bone material is needed internally than superficially.
Hormonal controls determine whether and when remodeling occurs in response to changing blood calcium levels.
Mechanical stress determines where remodeling occurs (determine which osteoclasts are most sensitive to PTH stimulation)
Bone Repair
Fractures may be classified by :
Position of the bone
Bone Repair
Fractures may be classified by :
Position of the bone
Completeness of the break: If the bone is broken through, the fracture is a complete fracture. If not, it is an incomplete fracture.
Whether the bone ends penetrate the skin: If so, the fracture is an open (compound) fracture. If not, it is a closed (simple) fracture.
There are two types of reduction (the realignment of the broken bone ends ) treatment : external coax the bone ends into position. In open (internal) reduction, the bone ends are secured together surgically with pins or wires
simple fracture of small or medium-sized bones in young adults heals in six to eight weeks , but it takes much longer for large, weight-bearing bones and for bones of elderly people (because of their poorer circulation)









 Витамины. Определение, классификация
Витамины. Определение, классификация Информационная биология. Семантическая и прагматическая информация. (Тема 5)
Информационная биология. Семантическая и прагматическая информация. (Тема 5) Круги кровообращения
Круги кровообращения Строение нервной системы. Спинной мозг
Строение нервной системы. Спинной мозг ЕГЭ по биологии
ЕГЭ по биологии Физиология центральной нервной системы
Физиология центральной нервной системы Осенние приметы. (Урок 15. 1 класс)
Осенние приметы. (Урок 15. 1 класс) Открытый урок биологии по теме Движение 6 класс (УМК Н.И.Сонин) , автор учитель биологии Сизова С.В.
Открытый урок биологии по теме Движение 6 класс (УМК Н.И.Сонин) , автор учитель биологии Сизова С.В. Класс Пресмыкающиеся или Рептилии (Reptilia)
Класс Пресмыкающиеся или Рептилии (Reptilia) Фотосинтез
Фотосинтез Организм человека. Анатомия человека
Организм человека. Анатомия человека Биология кошек
Биология кошек Технология выращивания томатов
Технология выращивания томатов Теории происхождения человека
Теории происхождения человека Породи свиней
Породи свиней Бактериологическая разведка и индикация бактериологического (биологического) оружия
Бактериологическая разведка и индикация бактериологического (биологического) оружия Методы оценки биоразнообразия
Методы оценки биоразнообразия Размножение и развитие земноводных. Сезонные явления в жизни земноводных
Размножение и развитие земноводных. Сезонные явления в жизни земноводных Мал азықтық жемдік дақылдар
Мал азықтық жемдік дақылдар Газообмен в легких и тканях. Дыхательные движения. Регуляция дыхания
Газообмен в легких и тканях. Дыхательные движения. Регуляция дыхания Бабочки
Бабочки Нуклеиновые кислоты
Нуклеиновые кислоты Молекулярные механизмы образования хромосомных перестроек с учетом структурной организации хромосомных районов
Молекулярные механизмы образования хромосомных перестроек с учетом структурной организации хромосомных районов Царство грибы. Общая характеристика
Царство грибы. Общая характеристика презентация к уроку биологии в 8 классе
презентация к уроку биологии в 8 классе Изготовление компоста из листьев
Изготовление компоста из листьев Гепард — хищное млекопитающее семейства кошачьих
Гепард — хищное млекопитающее семейства кошачьих Внутреннее строение корня
Внутреннее строение корня