Содержание
- 2. 9/4/2019 Management of Patients With Chest and Lower Respiratory Tract Disorders
- 3. Learning outcomes 1. Identify patients at risk for atelectasis and nursing interventions related to its prevention
- 4. Atelectasis Atelectasis refers to closure or collapse of alveoli and often is described in relation to
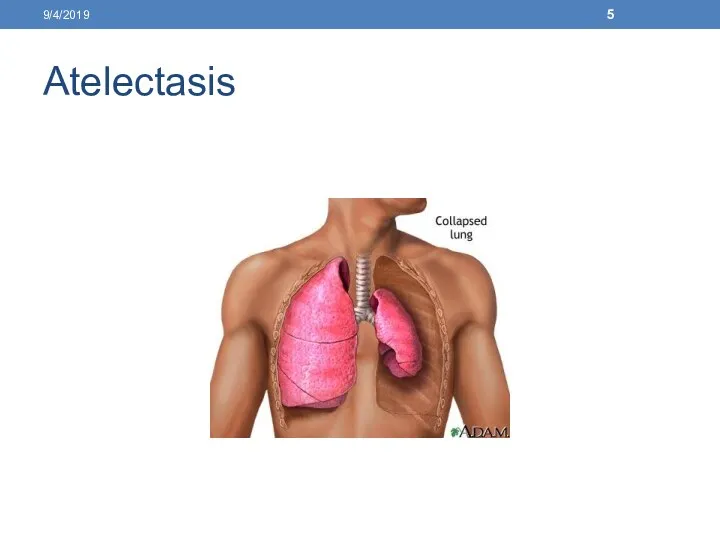
- 5. Atelectasis 9/4/2019
- 6. Causes Altered breathing patterns, retained secretions, alterations in small airway function Pain, prolonged supine positioning, Reduced
- 7. Clinical manifestations Increasing dyspnea cough, sputum production In acute atelectasis involving a large amount of lung
- 8. Assessment and diagnostic findings Chest x-ray Pulse oximetry demonstrate low saturation of hemoglobin with O2 (
- 9. Prevention Change patient’s position frequently, especially from supine to upright position, to promote ventilation and prevent
- 10. Prevention Administer prescribed opioids and sedatives to prevent respiratory depression. Perform postural drainage and chest percussion,
- 11. Medical management The strategies to prevent atelectasis, which include frequent turning, early ambulation, lung volume expansion
- 12. Medical management The secretions must be removed by coughing or suctioning to permit air to re-enter
- 13. Medical management A bronchoscopy is performed to remove secretions and increase ventilation. Endotracheal intubation or mechanical
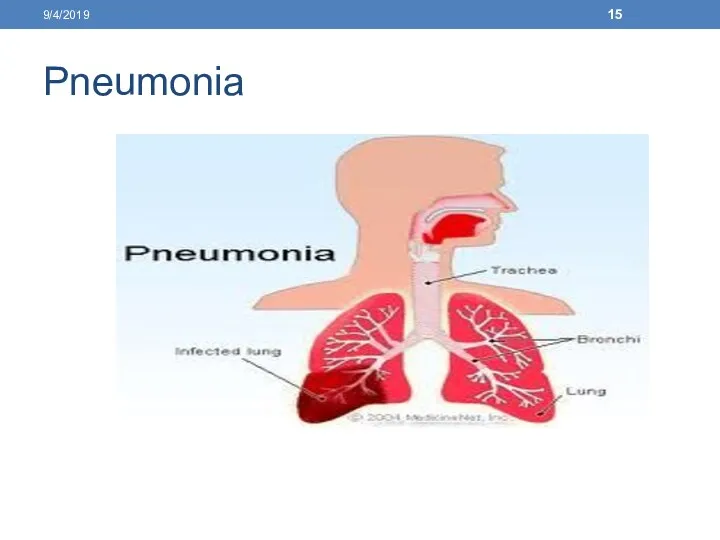
- 14. Pneumonia Pneumonia is an inflammation of the lung parenchyma that is caused by various microorganisms, including
- 15. Pneumonia 9/4/2019
- 16. Pneumonia Pneumonia is an inflammatory process, involving the terminal airways and alveoli of the lung, caused
- 17. Pathophysiology and Etiology The organism gains access to the lungs through aspiration of oropharyngeal contents, by
- 18. When bacterial pneumonia occurs in a healthy person, there is usually a history of preceding viral
- 19. Clinical Manifestations For most common forms of bacterial pneumonia: Sudden onset; shaking chill; rapidly rising fever
- 20. Management Antimicrobial therapy ”depends on laboratory identification of causative organism and sensitivity to specific antimicrobials, or
- 21. Nursing Diagnoses Impaired Gas Exchange related to decreased ventilation secondary to inflammation and infection involving distal
- 22. Nursing Interventions Improving Gas Exchange Observe for cyanosis, dyspnea, hypoxia, and confusion, indicating worsening condition. Follow
- 23. Nursing Interventions Enhancing Airway Clearance Obtain freshly expectorated sputum for gram stain and culture, preferably early
- 24. Nursing Interventions Relieving Pleuritic Pain Place in a comfortable position (semi-Fowler's) for resting and breathing; encourage
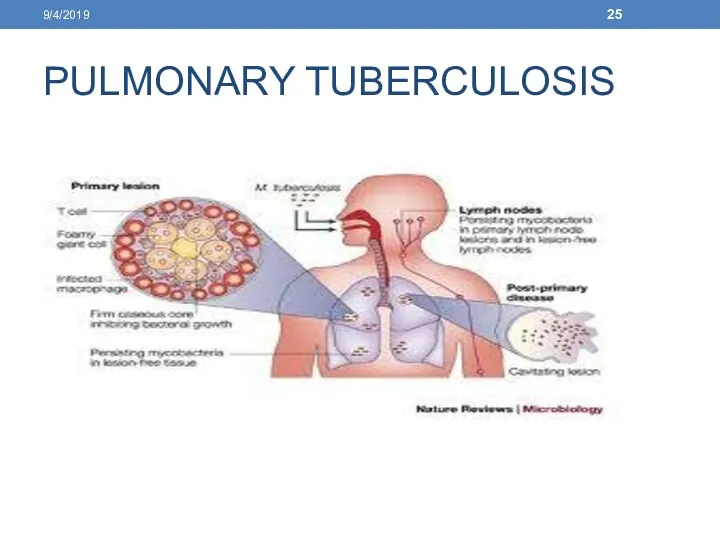
- 25. PULMONARY TUBERCULOSIS 9/4/2019
- 26. TUBERCULOSIS TB is an infectious disease caused by bacteria (Mycobacterium tuberculosis) that are usually spread from
- 27. Pathophysiology and Etiology Transmission The term Mycobacterium is descriptive of the organism, which is a bacterium
- 28. Clinical Manifestations Patient may be asymptomatic or may have insidious symptoms that may be ignored. Constitutional
- 29. Diagnostic Evaluation Sputum smear ”detection of acid-fast bacilli in stained smears is the first bacteriologic clue
- 30. Management Current recommended regimen of uncomplicated, previously untreated pulmonary TB is an initial phase of 2
- 31. Nursing Diagnoses 9/4/2019
- 32. Nursing Interventions Improving Breathing Pattern Administer and teach self-administration of medications as ordered. Encourage rest and
- 33. Nursing Interventions Improving Nutritional Status Explain the importance of eating a nutritious diet to promote healing
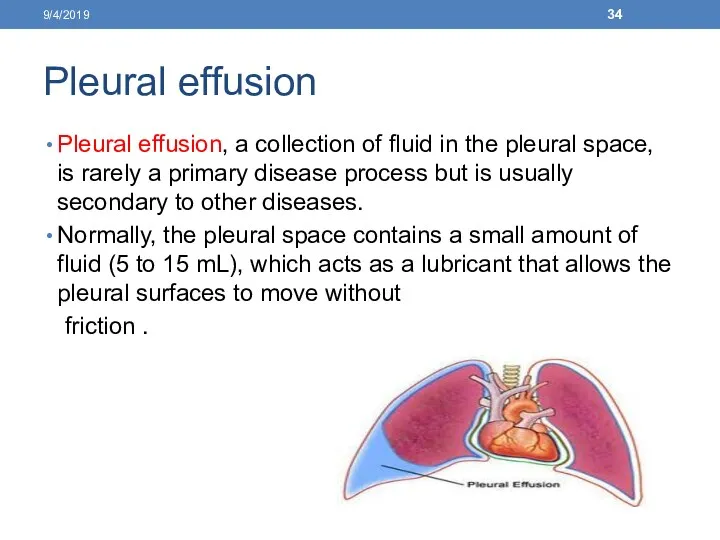
- 34. Pleural effusion Pleural effusion, a collection of fluid in the pleural space, is rarely a primary
- 35. PLEURAL EFFUSION Pleural effusion refers to a collection of fluid in the pleural space. It is
- 36. Pathophysiology and Etiology May be either transudative or exudative. Transudative effusions occur primarily in noninflammatory conditions;
- 37. Clinical Manifestations Dyspnea, pleuritic chest pain, cough. Dullness or flatness to percussion (over areas of fluid)
- 38. Nursing Diagnosis Ineffective Breathing Pattern related to collection of fluid in pleural space Nursing Interventions Maintaining
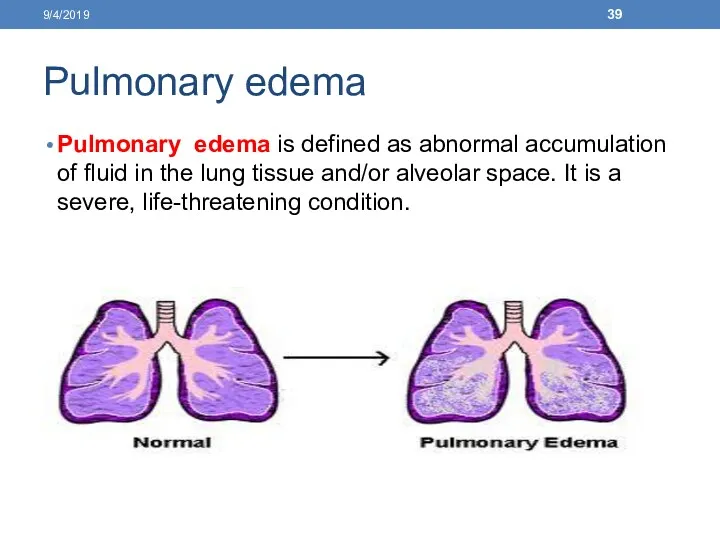
- 39. Pulmonary edema Pulmonary edema is defined as abnormal accumulation of fluid in the lung tissue and/or
- 40. Causes of pulmonary edema Inadequate left ventricular function Hypervolemia Sudden increase in the intravascular pressure in
- 41. Clinical manifestations Respiratory distress, characterized by dyspnea, and central cyanosis. The patient is very anxious and
- 42. Assessment and Diagnostic Findings Auscultation reveals crackles in the lung bases. Chest x-ray Pulse oximetry Arterial
- 43. Medical management Management focuses on correcting the underlying disorder. Oxygen is administrated to correct hypoxemia 9/4/2019
- 44. Nursing management Assisting with administration of oxygen and intubation and mechanical ventilation if respiratory failure occurs.
- 45. Acute Respiratory Failure Acute respiratory failure (ARF) is defined as a fall in arterial oxygen tension
- 46. RESPIRATORY FAILURE Respiratory failure is an alteration in the function of the respiratory system that causes
- 47. Classification Acute Respiratory Failure Characterized by hypoxemia (Pao2 less than 50 mm Hg) and/or hypercapnia (Paco2
- 48. Acute and Chronic Respiratory Failure Characterized by an abrupt increase in the degree of hypoxemia or
- 49. Pathophysiology and Etiology Oxygenation Failure Characterized by a decrease in Pao2 and normal or decreased Paco2.
- 50. Clinical Manifestations Hypoxemia €”restlessness, agitation, dyspnea, disorientation, confusion, delirium, loss of consciousness. Hypercapnia €”headache, somnolence, dizziness,
- 51. NURSING ALERT Obtain ABG levels whenever the history or signs and symptoms suggest the patient is
- 52. Diagnostic Evaluation ABG analysis €”show changes in Pao2, Paco2, and pH from patient's normal; or Pao2
- 53. NURSING ALERT Avoid administration of oxygen at Fio2 of 100% for COPD patients because you may
- 54. Nursing Diagnoses Impaired Gas Exchange related to inadequate respiratory center activity or chest wall movement, airway
- 55. Nursing Interventions Improving Gas Exchange Administer antibiotics, cardiac medications, and diuretics as ordered for underlying disorder.
- 56. Pulmonary arterial hypertension Pulmonary hypertension exists when the systolic pulmonary artery pressure exceeds 25 mm Hg.
- 57. Pulmonary arterial hypertension In the absence of these measurements, clinical recognition becomes the only indicator for
- 58. Causes of pulmonary arterial hypertension Collagen vascular diseases Portal hypertension Altered immune mechanisms Chronic thrombotic or
- 59. Causes of pulmonary arterial hypertension Pulmonary venous hypertension Pulmonary vasoconstriction due to hypoxemia Chronic obstructive pulmonary
- 60. Clinical manifestations Dyspnea is the main symptom of pulmonary hypertension, occurring at first with exertion and
- 61. Assessment and diagnosis History Physical examination Chest x-ray Pulmonary function studies Electrocardiogram (ECG), echocardiogram cardiac catheterization.
- 62. Medical management Management of the underlying cardiac or pulmonary condition: Anticoagulation Diuretics and oxygen Vasodilators as
- 63. Nursing management The nurse also must be alert for signs and symptoms of pulmonary hypertension Administer
- 64. Pulmonary embolism Pulmonary embolism (PE) refers to the obstruction of the pulmonary artery or one of
- 65. PULMONARY EMBOLISM Pulmonary embolism refers to the obstruction of one or more pulmonary arteries by a
- 66. Pathophysiology and Etiology Obstruction, either partial or full, of pulmonary arteries, which causes decrease or absent
- 67. Predisposing factors include: Stasis, prolonged immobilization. Concurrent phlebitis. Previous heart (heart failure, myocardial infarction [MI]) or
- 68. NURSING ALERT Be aware of high-risk patients for pulmonary embolism€”immobilization, trauma to pelvis (especially surgical) and
- 69. Clinical Manifestations Dyspnea, pleuritic pain, tachypnea, apprehension. Chest pain with apprehension and a sense of impending
- 70. Diagnostic Evaluation ABG levels €”decreased Pao2 is usually found, due to perfusion abnormality of the lung.
- 71. Emergency Management Oxygen is administered to relieve hypoxemia, respiratory distress, and cyanosis. An infusion is started
- 72. Subsequent Management €”Anticoagulation and Thrombolysis I.V. heparin €”stops further thrombus formation and extends the clotting time
- 73. Nursing Diagnoses 9/4/2019
- 74. Nursing Interventions Correcting Breathing Pattern Assess for hypoxia, headache, restlessness, apprehension, pallor, cyanosis, behavioral changes. Monitor
- 75. Improving Tissue Perfusion Closely monitor for shock €”decreasing blood pressure, tachycardia, cool, clammy skin. Monitor prescribed
- 76. Patient Education and Health Maintenance Advise patient of the possible need to continue taking anticoagulant therapy
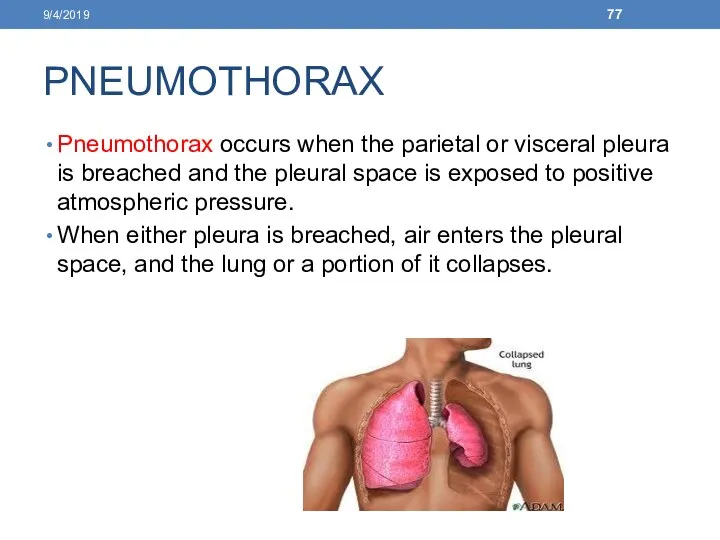
- 77. PNEUMOTHORAX Pneumothorax occurs when the parietal or visceral pleura is breached and the pleural space is
- 78. TRAUMATIC DISORDERS PNEUMOTHORAX Air in the pleural space occurring spontaneously or from trauma (see Figure 11-4).
- 79. Spontaneous pneumothorax €”sudden onset of air in the pleural space with deflation of the affected lung
- 80. Pathophysiology and Etiology When there is a large open hole in the chest wall. A portion
- 81. Clinical Manifestations Hyperresonance; diminished breath sounds. Reduced mobility of affected half of thorax. Tracheal deviation away
- 82. Diagnostic Evaluation Chest X-ray confirms presence of air in pleural space. Management Spontaneous Pneumothorax Treatment is
- 83. Tension Pneumothorax Immediate decompression to prevent cardiovascular collapse by thoracentesis or chest tube insertion to let
- 84. Nursing Diagnoses Ineffective Breathing Pattern related to air in the pleural space Impaired Gas Exchange related
- 85. Resolving Impaired Gas Exchange Encourage patient in the use of incentive spirometer. Monitor oximetry and ABG
- 86. Hemothorax Blood in pleural space as a result of penetrating or blunt chest trauma. Accompanies a
- 88. Скачать презентацию
 Коллапсотерапия. Виды
Коллапсотерапия. Виды Состав микробиоты разных локусов организма
Состав микробиоты разных локусов организма Аккредитация медицинского персонала в 2023 году
Аккредитация медицинского персонала в 2023 году Производные индола
Производные индола Диагностика заболеваний органов дыхания у детей
Диагностика заболеваний органов дыхания у детей Медицина катастроф
Медицина катастроф Особенности препарирования кариозных полостей по Блеку
Особенности препарирования кариозных полостей по Блеку Стероидты емес қабынуға қарсы дәрілер
Стероидты емес қабынуға қарсы дәрілер Острые кишечные заболевания
Острые кишечные заболевания Ревматическая болезнь сердца
Ревматическая болезнь сердца Симптомы заболеваний почек
Симптомы заболеваний почек Інфекційні захворювання нервової системи у дітей
Інфекційні захворювання нервової системи у дітей Лікування хворих на цукровий діабет
Лікування хворих на цукровий діабет Профилактика профессионального заражения ВИЧ
Профилактика профессионального заражения ВИЧ Воспалительные заболевания слуховой трубы
Воспалительные заболевания слуховой трубы Сердечно-легочная реанимация у детей
Сердечно-легочная реанимация у детей Плацентарная недостаточность
Плацентарная недостаточность Паллиативная помощь онкологическим больным
Паллиативная помощь онкологическим больным Роды при неправильных положениях и предлежаниях плода
Роды при неправильных положениях и предлежаниях плода Международный день медицинской сестры
Международный день медицинской сестры Организация питания пациентов в стационаре
Организация питания пациентов в стационаре Профилактика, диагностика и лечение туберкулеза
Профилактика, диагностика и лечение туберкулеза Гипоксически-ишемическая энцефалопатия новорожденных детей
Гипоксически-ишемическая энцефалопатия новорожденных детей Test job and introduction. Trial Task Lecturio
Test job and introduction. Trial Task Lecturio Физиотерапия в стоматологии
Физиотерапия в стоматологии Сестринский процесс
Сестринский процесс Гипертоническая болезнь
Гипертоническая болезнь Історія розвитку хірургії. Асептика, антисептика
Історія розвитку хірургії. Асептика, антисептика