Содержание
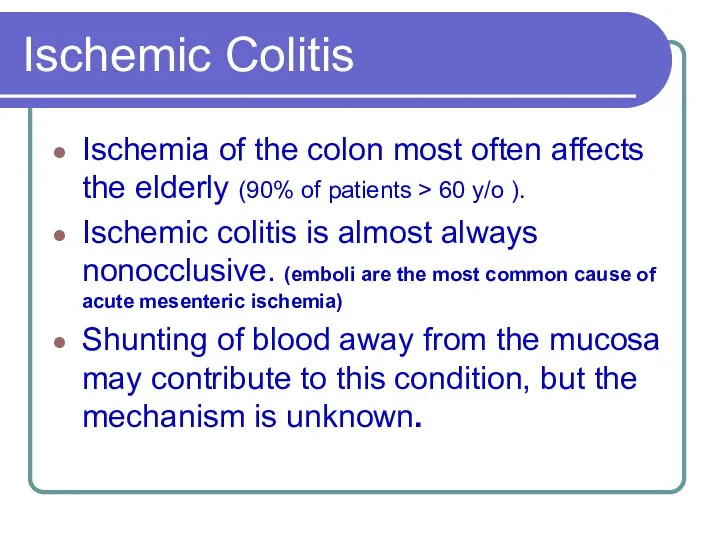
- 2. Ischemic Colitis Ischemia of the colon most often affects the elderly (90% of patients > 60
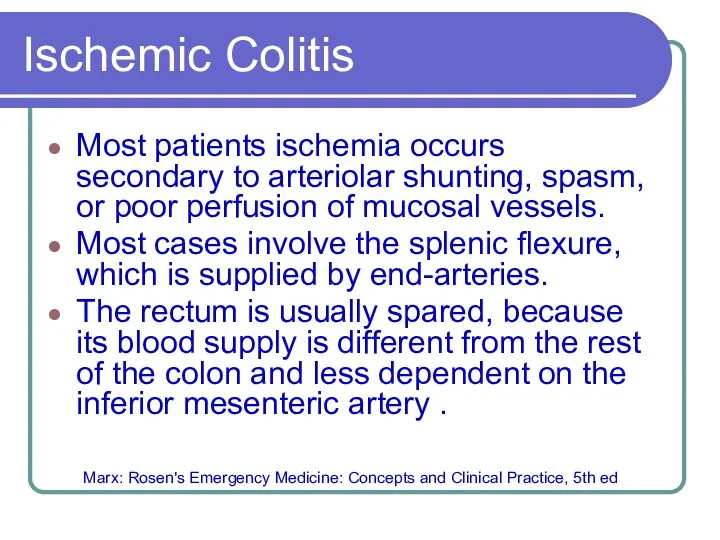
- 3. Ischemic Colitis Most patients ischemia occurs secondary to arteriolar shunting, spasm, or poor perfusion of mucosal
- 4. Types of Ischemic Colitis Acute fulminant ischemic colitis Subacute ischemic colitis HARRISON’S ONLINE 15TH
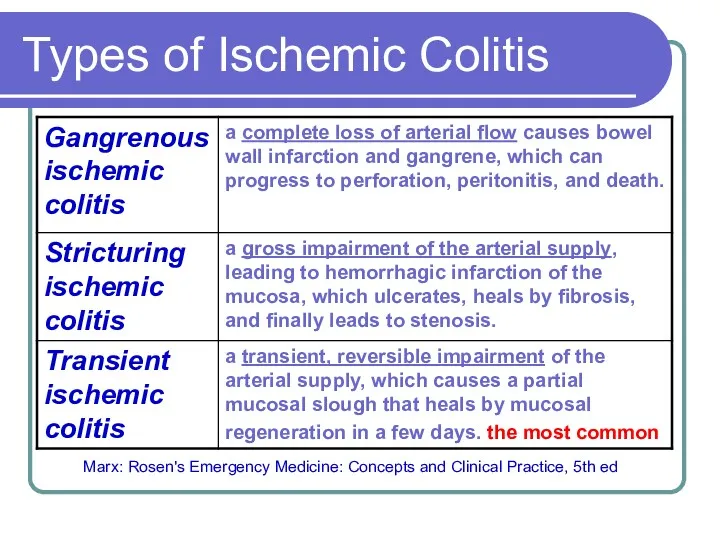
- 5. Types of Ischemic Colitis Marx: Rosen's Emergency Medicine: Concepts and Clinical Practice, 5th ed
- 6. Acute fulminant ischemic colitis manifestations The onset is characteristically acute, with generalized lower abdominal pain, usually
- 7. Acute fulminant ischemic colitis Diagnostic Strategy No specific serum markers proven in the diagnosis of intestinal
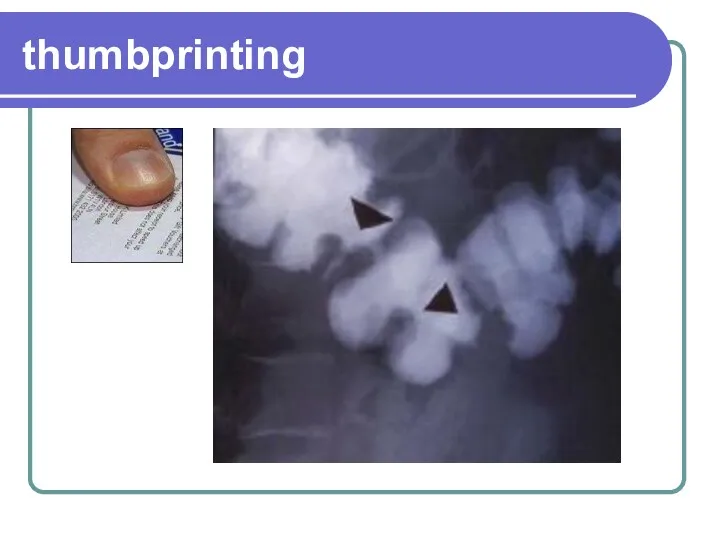
- 8. thumbprinting
- 9. Acute fulminant ischemic colitis Diagnostic Strategy Sigmoidoscopy or colonoscopy may detect ulcerations, friability, and bulging folds
- 10. Acute fulminant ischemic colitis Diagnostic Strategy Angiography is not helpful in the management of patients with
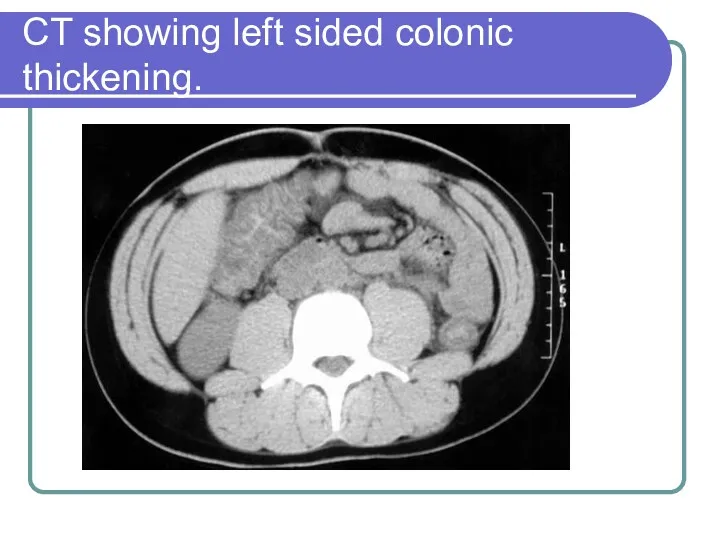
- 11. CT showing left sided colonic thickening.
- 12. Acute fulminant ischemic colitis management When ischemic colitis is suspected, a surgeon should be consulted. Gangrenous
- 13. management Vasopressors should be avoided, if possible. Low blood-flow states (hypotension) should be aggressively reversed.
- 14. Types of Ischemic Colitis Acute fulminant ischemic colitis Subacute ischemic colitis
- 15. Subacute ischemic colitis manifestations It produces lesser degrees of pain and bleeding, often occurring over several
- 16. Subacute ischemic colitis management Subacute Ischemic colitis without evidence of peritonitis or perforation is generally self-limited
- 17. Subacute ischemic colitis management Most cases of nonocclusive ischemic colitis resolve in 2 to 4 weeks
- 18. Differential Considerations Ischemic colitis often mimics infectious colitis, inflammatory bowel disease, or even colon carcinoma. Many
- 20. Скачать презентацию
 Наследственные болезни, их причина и профилактика. Методы изучения генетики человека
Наследственные болезни, их причина и профилактика. Методы изучения генетики человека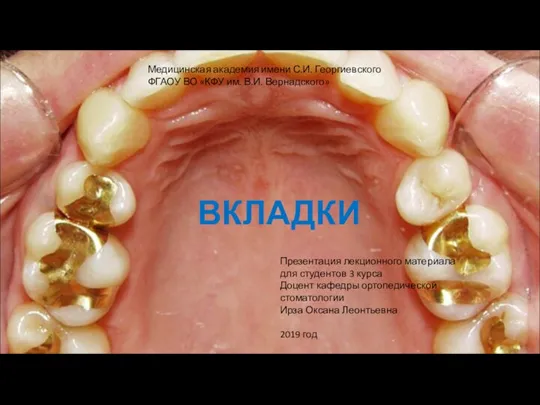 Вкладки - микропротезы, заполняющие дефект коронковой части зуба
Вкладки - микропротезы, заполняющие дефект коронковой части зуба Examination of the patient
Examination of the patient Ветеринарные лекарственные формы
Ветеринарные лекарственные формы Общая характеристика биологических препаратов для лечения и профилактики инфекций
Общая характеристика биологических препаратов для лечения и профилактики инфекций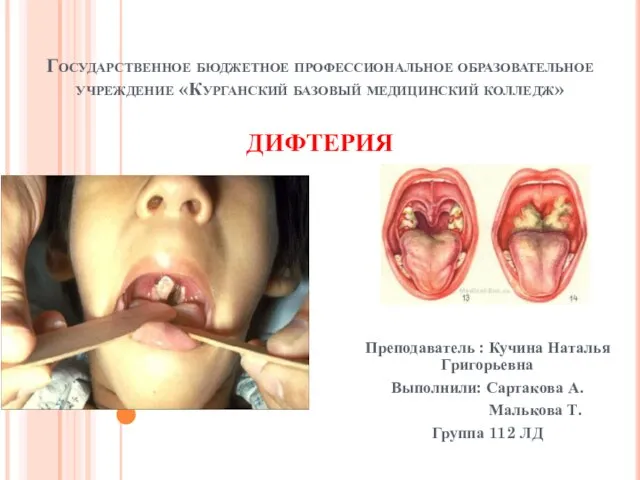 Дифтерия
Дифтерия Медициналық мекеменің бизнес жоспары
Медициналық мекеменің бизнес жоспары Сон - как основа жизнедеятельности организма
Сон - как основа жизнедеятельности организма Программа добровольного медицинского страхования Международный медицинский стандарт
Программа добровольного медицинского страхования Международный медицинский стандарт Гнойные заболевания серозных полостей
Гнойные заболевания серозных полостей Патофизиология пищеварения. Нарушения аппетита.. Язвенная болезнь желудка и ДП
Патофизиология пищеварения. Нарушения аппетита.. Язвенная болезнь желудка и ДП Осуществление ПСО ИМН
Осуществление ПСО ИМН Понятия здоровье, образ жизни, качество жизни
Понятия здоровье, образ жизни, качество жизни Психологические особенности личности инсультного больного
Психологические особенности личности инсультного больного Гемофилия А, В, С
Гемофилия А, В, С Гемостаз. Свертывающая система крови
Гемостаз. Свертывающая система крови Нейротропные средства
Нейротропные средства Характеристика государственной, муниципальной, частной систем здравоохранения
Характеристика государственной, муниципальной, частной систем здравоохранения Черепно-мозговая травма
Черепно-мозговая травма Глиниды. Прандиальные регуляторы
Глиниды. Прандиальные регуляторы Методики рентгенологического исследования тонкой и толстой кишки
Методики рентгенологического исследования тонкой и толстой кишки Гестозы (токсикозы беременных)
Гестозы (токсикозы беременных) Өндірістік шу, діріл. Адам ағзасына шу мен дірілдің әсер етуін гигиеналық бағалау және оларды анықтау әдістері
Өндірістік шу, діріл. Адам ағзасына шу мен дірілдің әсер етуін гигиеналық бағалау және оларды анықтау әдістері Өкпенің созылмалы обструктивті ауруы
Өкпенің созылмалы обструктивті ауруы Реабилитация несовершеннолетних с синдромом зависимости вследствие употребления психоактивных веществ
Реабилитация несовершеннолетних с синдромом зависимости вследствие употребления психоактивных веществ Белковый, жировой и углеводный обмены и методы исследования
Белковый, жировой и углеводный обмены и методы исследования Антисептика и асептика в хирургии
Антисептика и асептика в хирургии Аномалії розвитку плідного яйця
Аномалії розвитку плідного яйця