Содержание
- 2. PULPITIS Pulpitis is the most common cause of pain and loss of teeth in younger persons.
- 3. CAUSES OF PULP DISEASE The causes of pulp disease are Physical, Chemical and Bacterial. Physical Mechanical
- 4. 2. Chemical -Phosphoric acid, acrylic monomer, etc. -Erosion (acids) 3. Bacterial -Toxin associated with caries -Direct
- 5. I. According to pathological condition: - Focal or acute reversible pulpitis (Pulp hyperaemia) Irreversible pulpitis II.
- 6. According to extension of inflammation in pulp tissue: - Partial pulpitis Complete / total pulpitis According
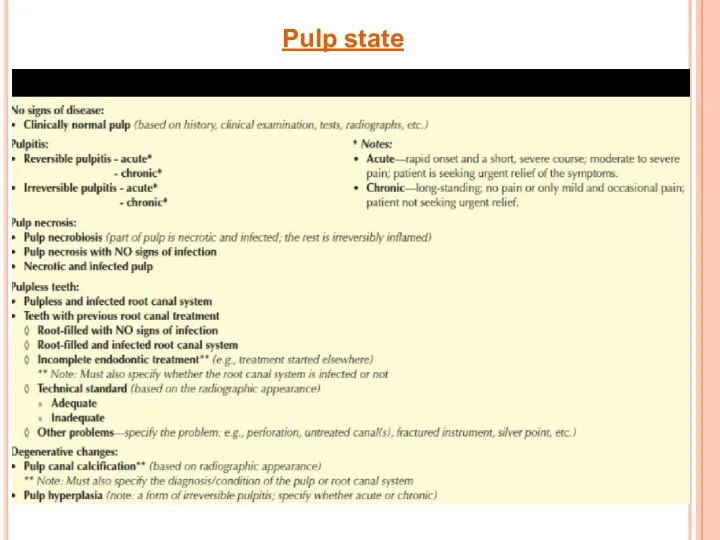
- 7. Pulp state
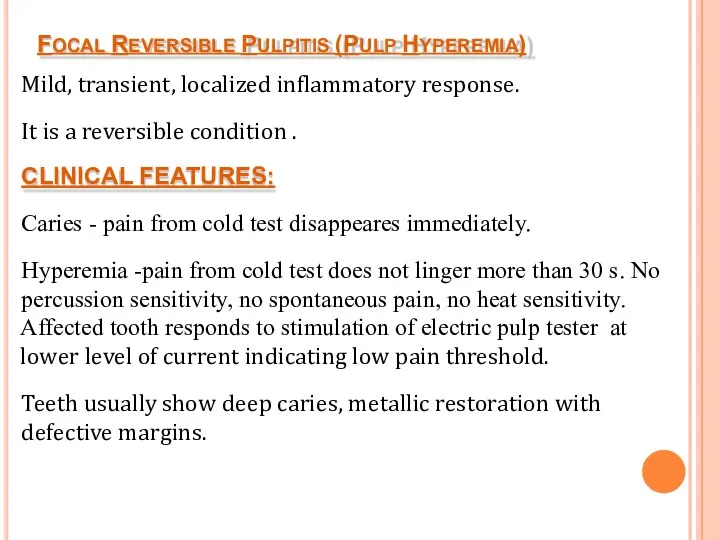
- 8. FOCAL REVERSIBLE PULPITIS (PULP HYPEREMIA) Mild, transient, localized inflammatory response. It is a reversible condition .
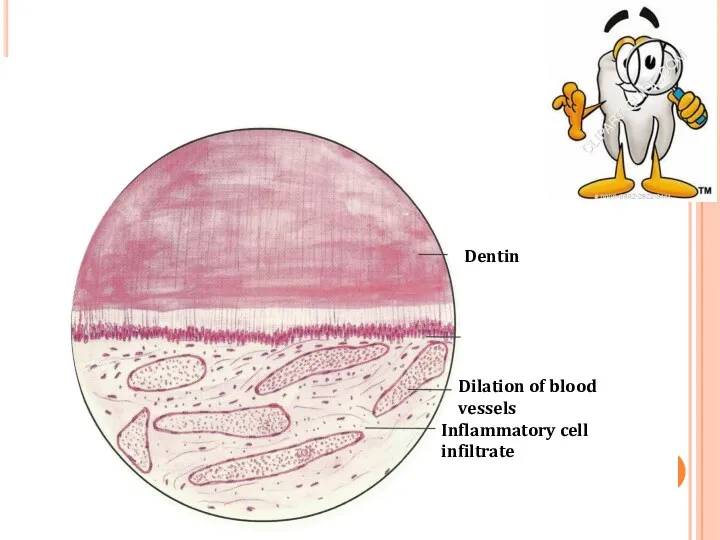
- 9. HISTOLOGICAL FEATURES: Dilation of pulp blood vessels. Edema fluid collection due to damage of vessel wall
- 10. Dilation of blood vessels Inflammatory cell infiltrate Dentin
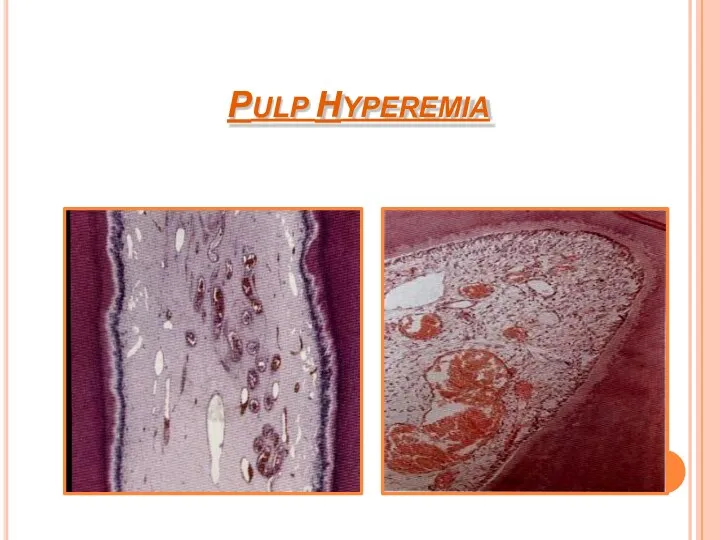
- 11. PULP HYPEREMIA
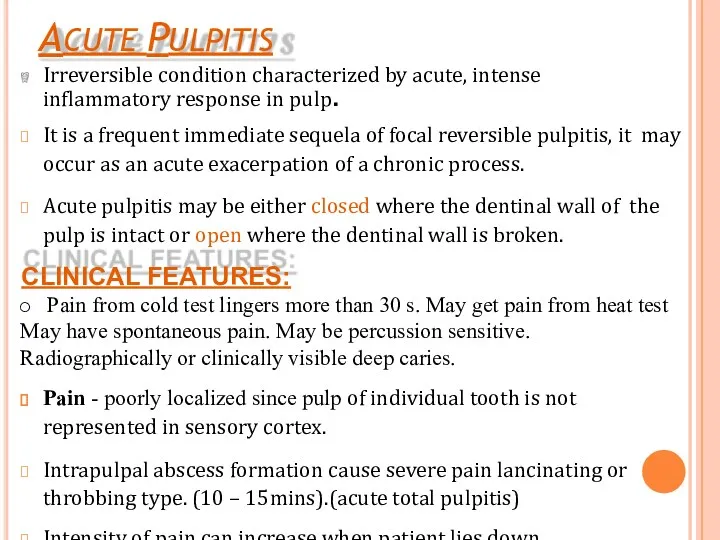
- 12. ACUTE PULPITIS Irreversible condition characterized by acute, intense inflammatory response in pulp. It is a frequent
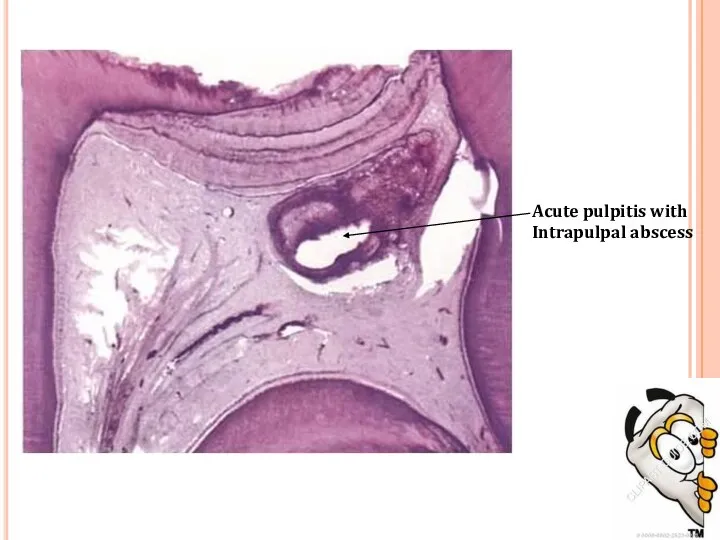
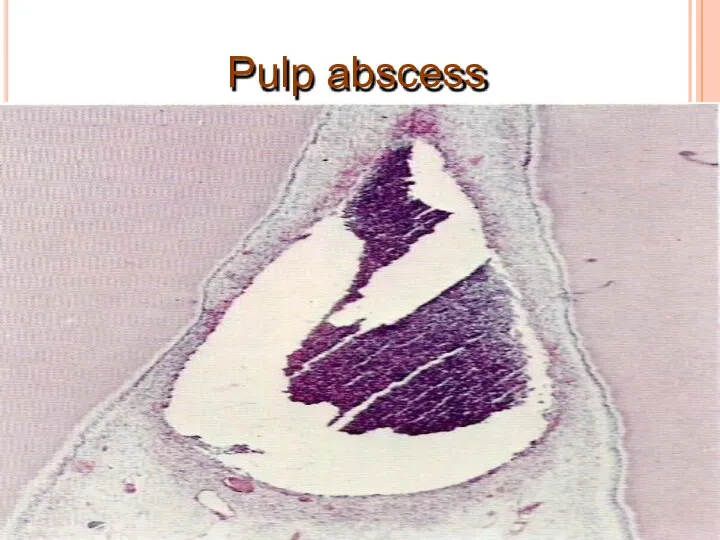
- 13. Acute pulpitis with Intrapulpal abscess
- 14. Pulp vitality test indicates increased sensitivity at low level of current. Pulpal pain is due to:
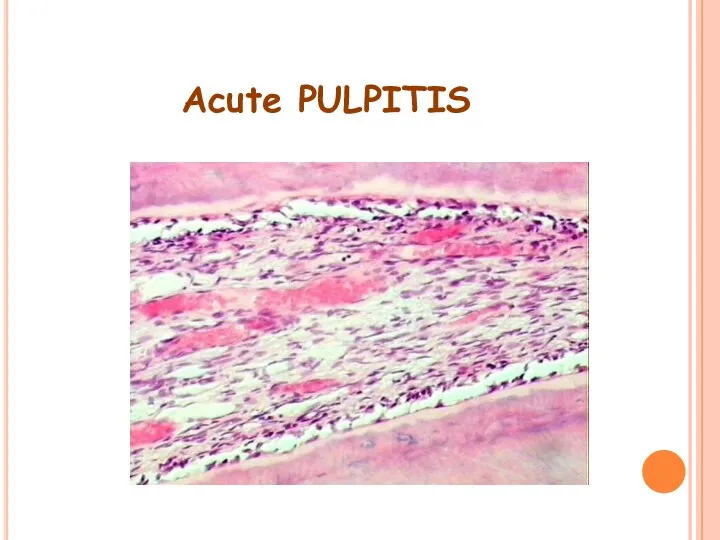
- 15. HISTOLOGIC FEATURES: Edema in pulp with vasodilation. Infiltration of polymorphonuclear leukocytes along vascular channels & migrate
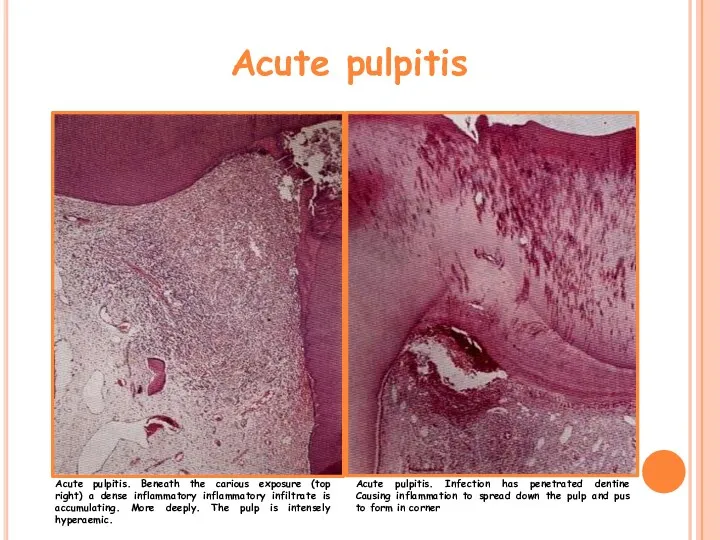
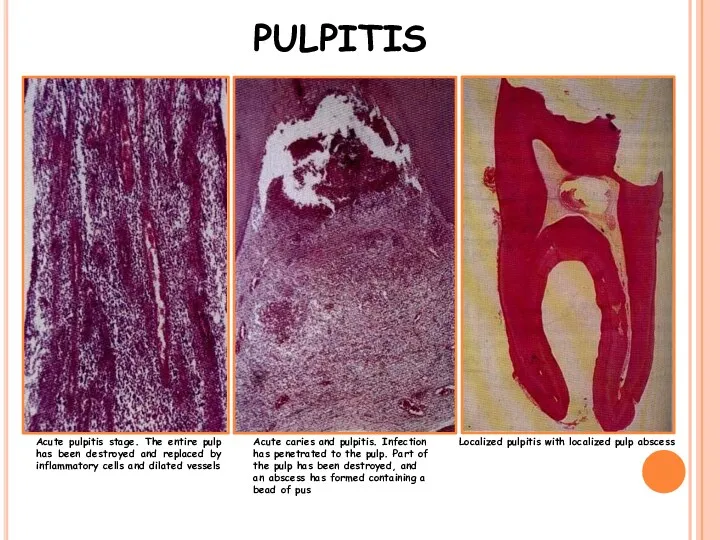
- 16. Acute pulpitis Acute pulpitis. Beneath the carious exposure (top right) a dense inflammatory inflammatory infiltrate is
- 17. Acute pulpitis stage. The entire pulp has been destroyed and replaced by inflammatory cells and dilated
- 18. Acute PULPITIS
- 19. Pulp abscess
- 20. Pulp abscess
- 21. TREATMENT & PROGNOSIS: Options for management: ◊ Extraction ◊ Pulpectomy and root canal treatment—with the following
- 22. Chronic Pulpitis Persistent inflammatory reaction in pulp with little or non symptoms. It can arise from
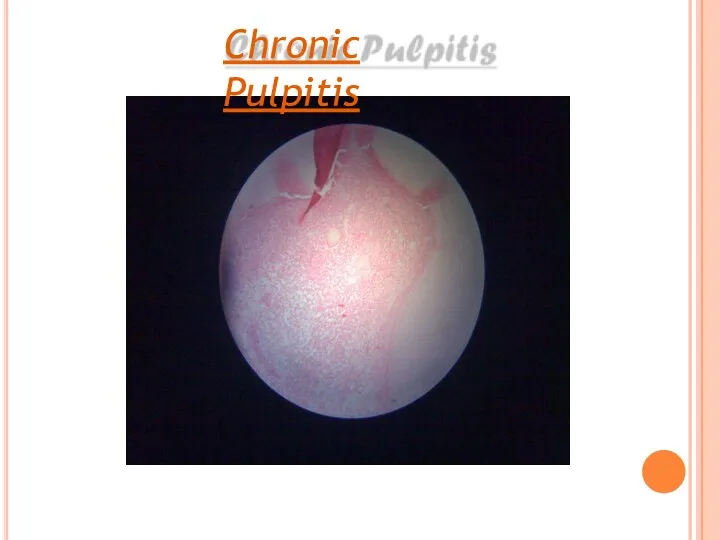
- 23. HISTOLOGIC FEATURES: Infiltration of mononuclear cells, lymphocytes & plasma cells, with vigorous connective tissue reaction. Capillaries
- 24. Chronic Pulpitis
- 25. TREATMENT & PROGNOSIS: Root canal therapy Extraction of tooth.
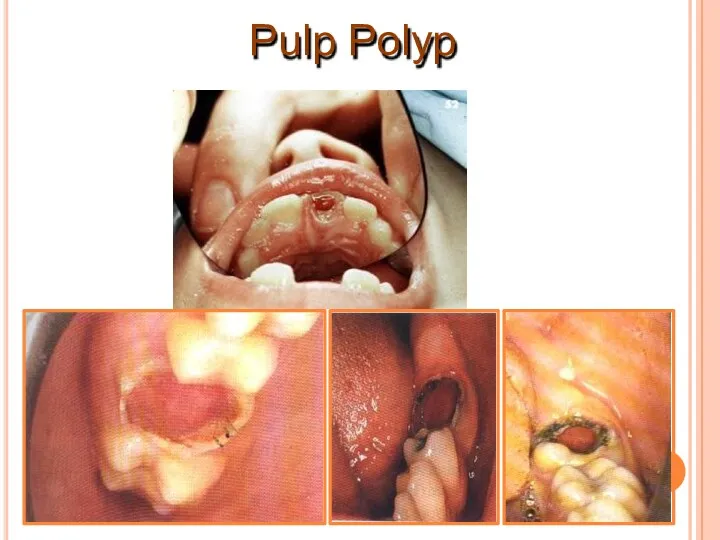
- 26. Chronic Hyperplastic Pulpitis (pulp polyp) It is a form of a chronic pulp disease. Overgrowth of
- 27. Lesion bleeds profusely upon provocation. Due to excellent blood supply high tissue resistance & reactivity in
- 28. Pulpal tissue Stratified sq. epithelium covering polyp Granulation tissue Carious tooth
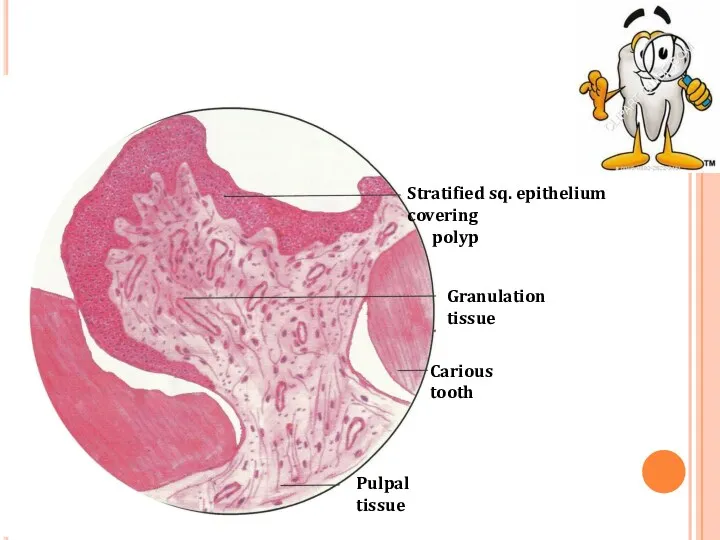
- 29. Stratified squamous type epithelial lining resembles oral mucosa with well formed rete pegs. Grafted epithelial cells
- 30. Pulp Polyp
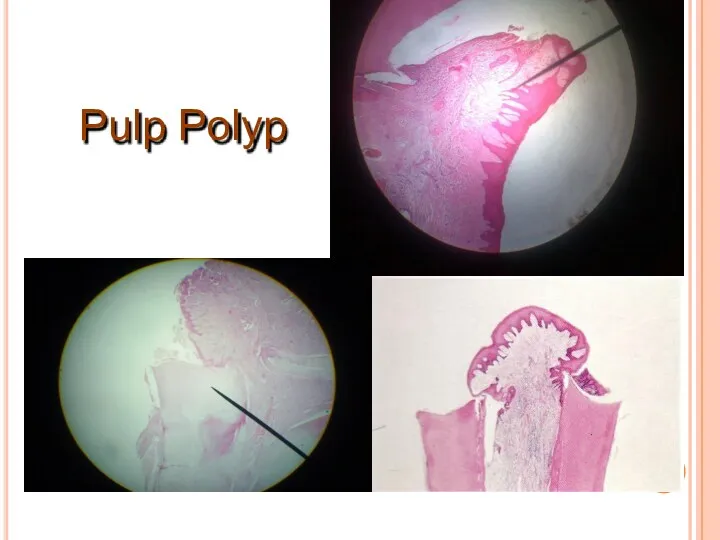
- 31. Pulp Polyp
- 32. Untreated pulpitis results complete necrosis of pulp. As this is associated with bacterial infection – pulp
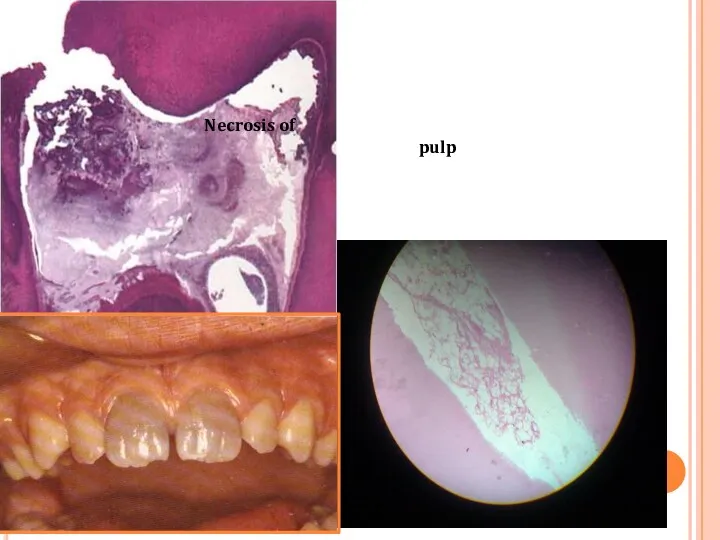
- 33. Necrosis of pulp
- 34. REVERSIBLE PULPITIS condition. Nature of pain is mild & diffuse. Brief duration & can be produce
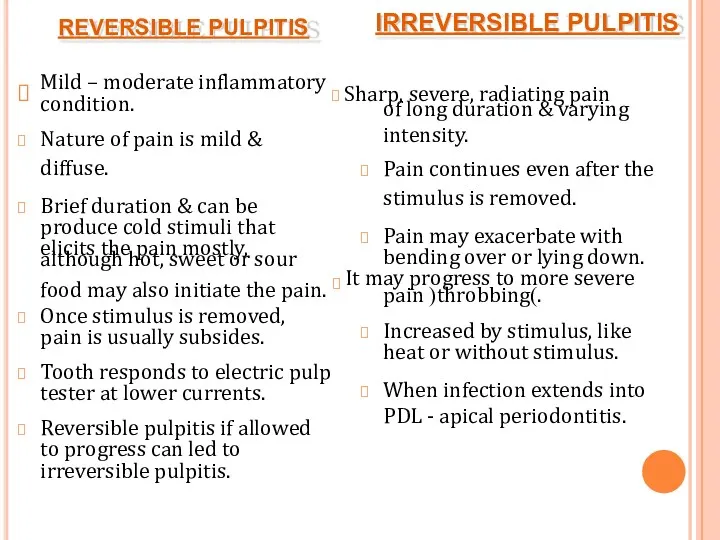
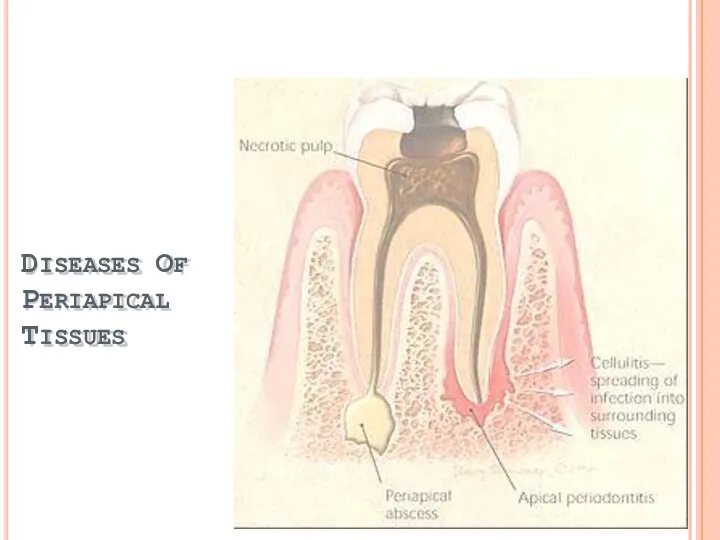
- 35. DISEASES OF PERIAPICAL TISSUES
- 36. Inflammation of PDL around apical portion of root. Cause:1. spread of infection following pulp necrosis,2. occlusal
- 37. Pulpitis Acute chronic Apical peiodontitis Acute chronic Periapical abscess Acute chronic Periapical granuloma Periodontal cyst Periosteitis
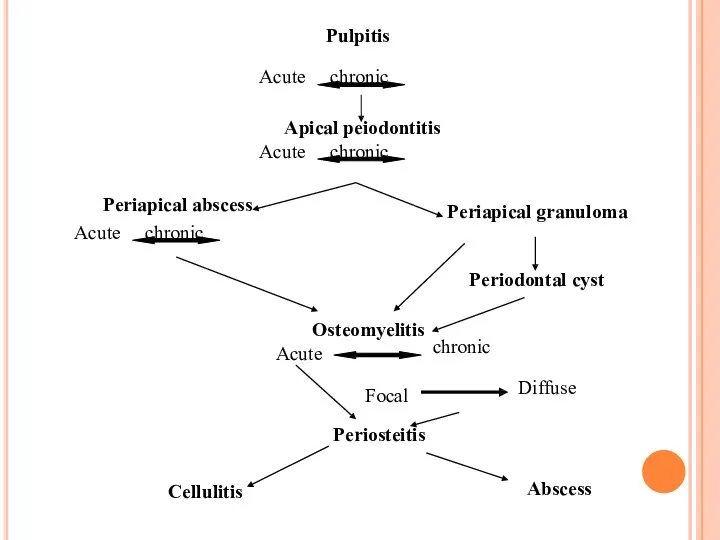
- 38. CLINICAL FEATURES: Thermal changes does not induce pain. Slight extrusion of tooth from socket. Cause tenderness
- 40. HISTOLOGIC FEATURES: PDL shows signs of inflammation -vascular dilation -infiltration of PMNs Inflammation is transient, if
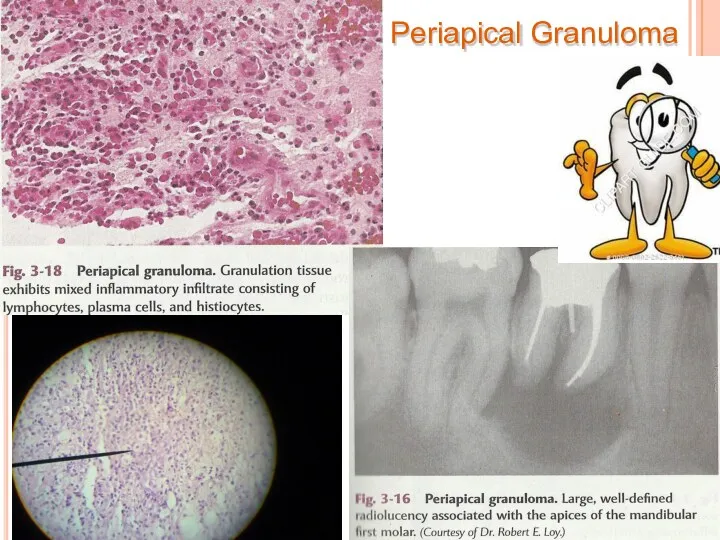
- 41. Chronic Apical Periodontitis (Periapical Granuloma) Most common sequelae of pulpitis or apical periodontitis. If acute (exudative)
- 42. Mild pain on chewing on solid food. Tooth may be slightly elongated in socket. Sensitivity is
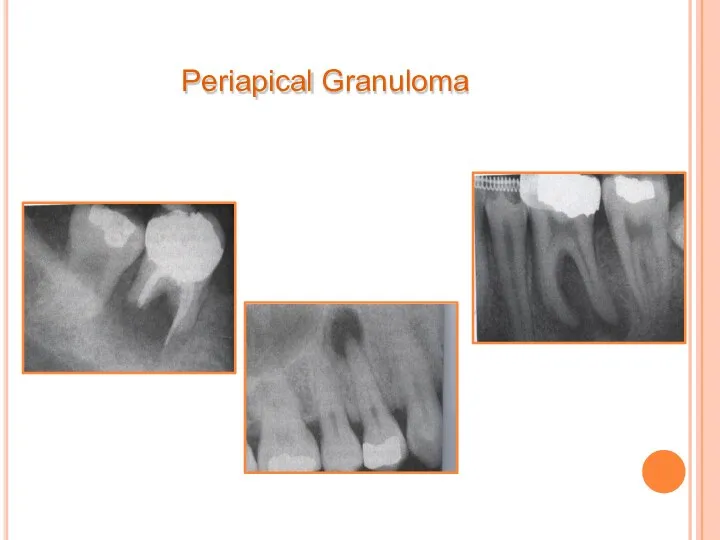
- 43. Periapical Granuloma
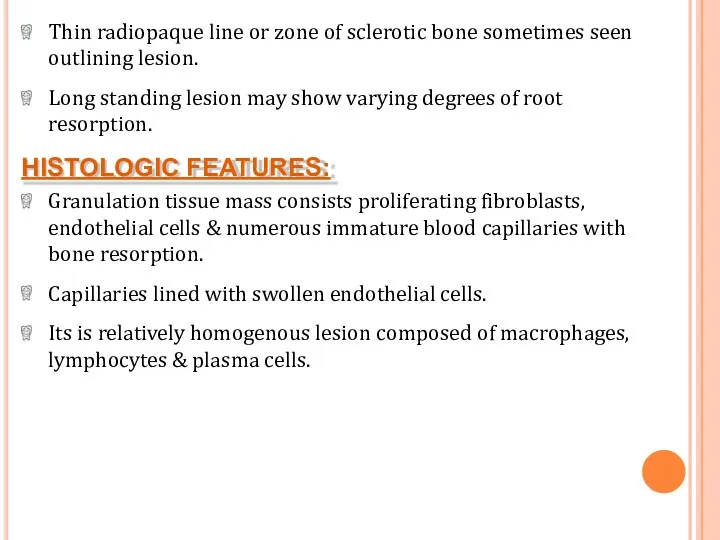
- 44. Thin radiopaque line or zone of sclerotic bone sometimes seen outlining lesion. Long standing lesion may
- 45. Periapical Granuloma
- 46. Cholesterol clefts
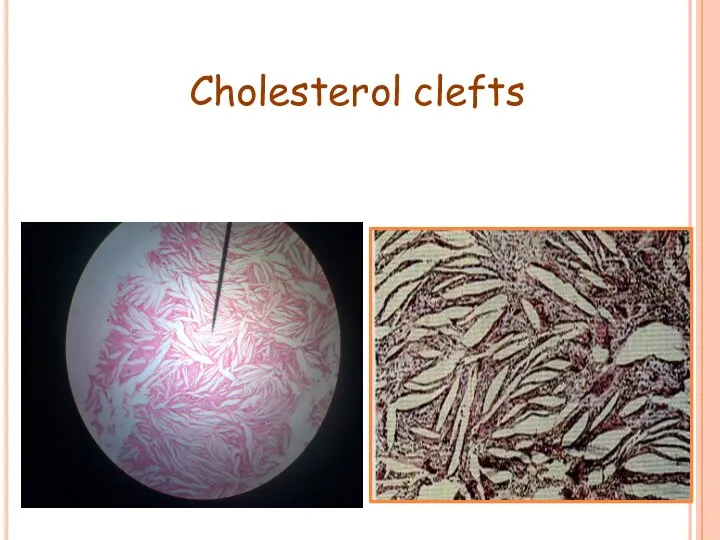
- 47. Collection of cholesterol clefts, with multinuclear gaint cells. Epithelial rests of Malassez may proliferate in response
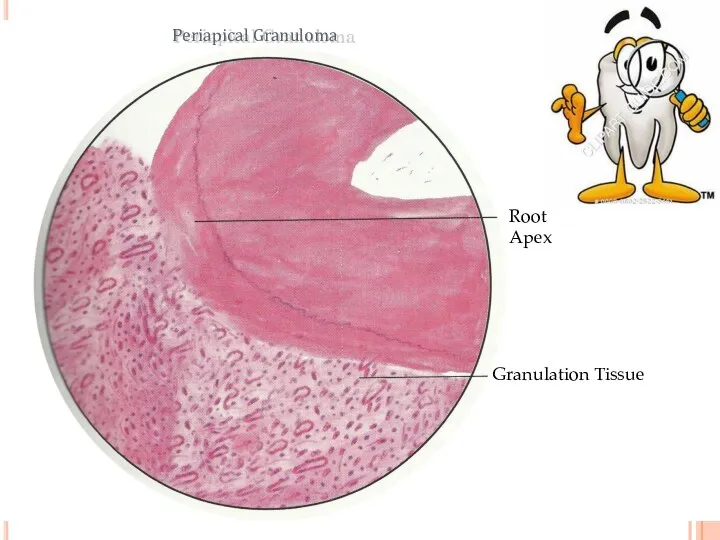
- 48. Root Apex Granulation Tissue Periapical Granuloma
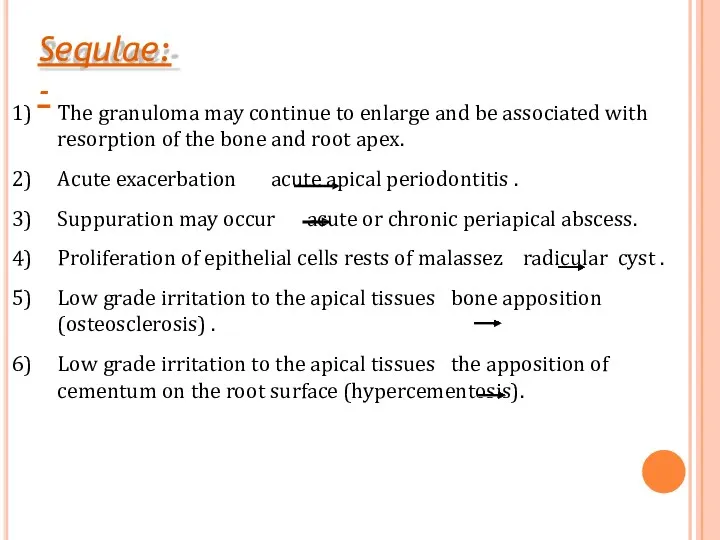
- 49. The granuloma may continue to enlarge and be associated with resorption of the bone and root
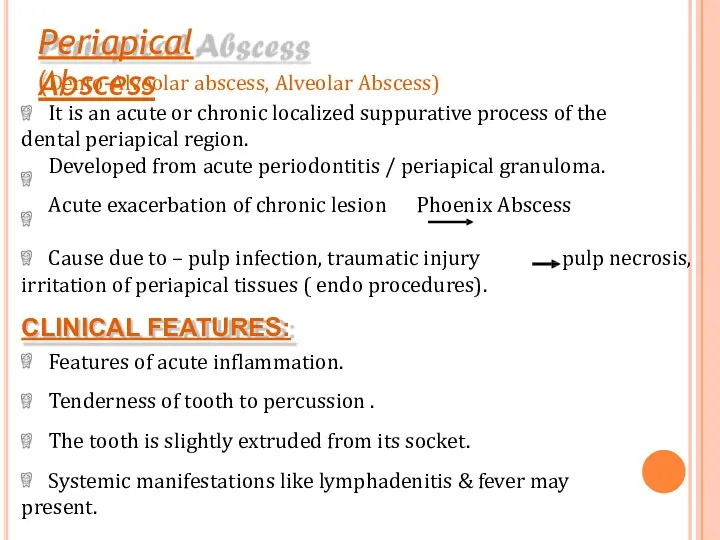
- 50. pulp necrosis, Cause due to – pulp infection, traumatic injury irritation of periapical tissues ( endo
- 51. Periapical abscess
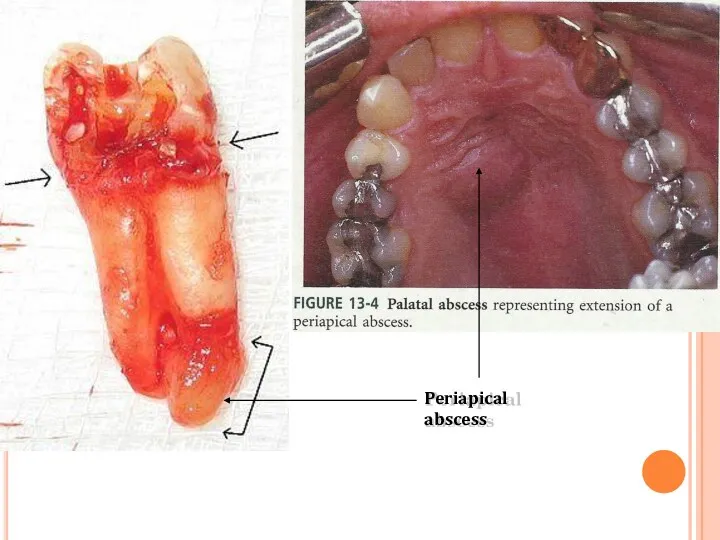
- 53. The pus tends to track through the cancellous bone and eventually perforates the cortex, it becomes
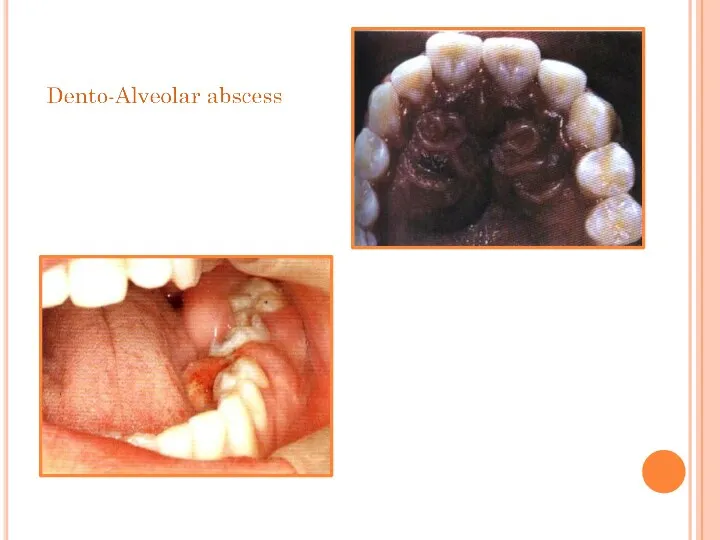
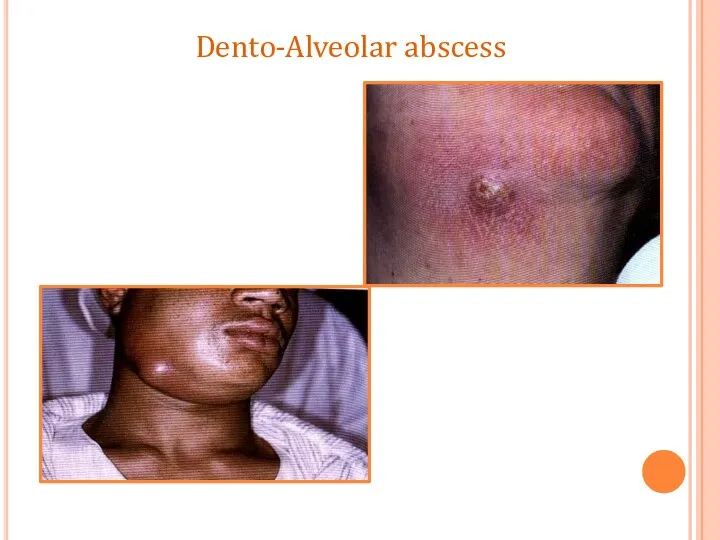
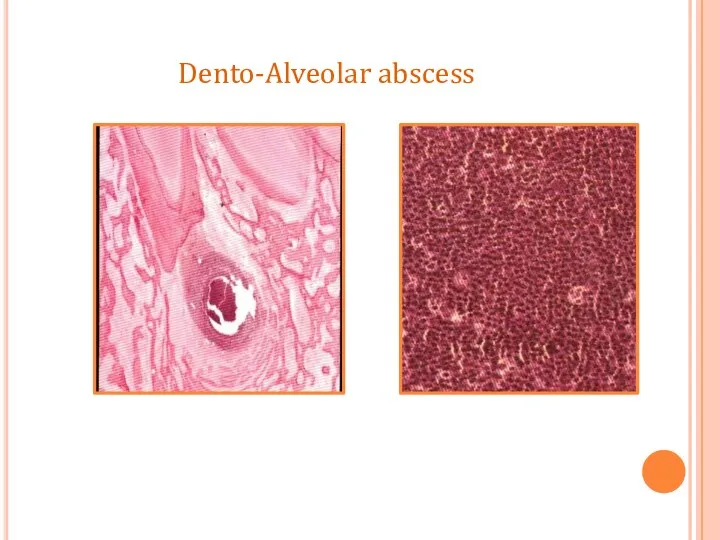
- 54. Dento-Alveolar abscess
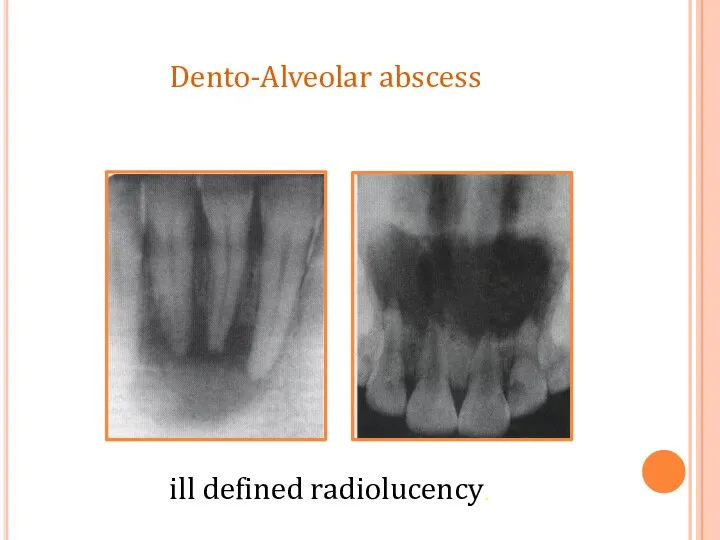
- 55. ill defined radiolucency. Dento-Alveolar abscess
- 56. Dento-Alveolar abscess
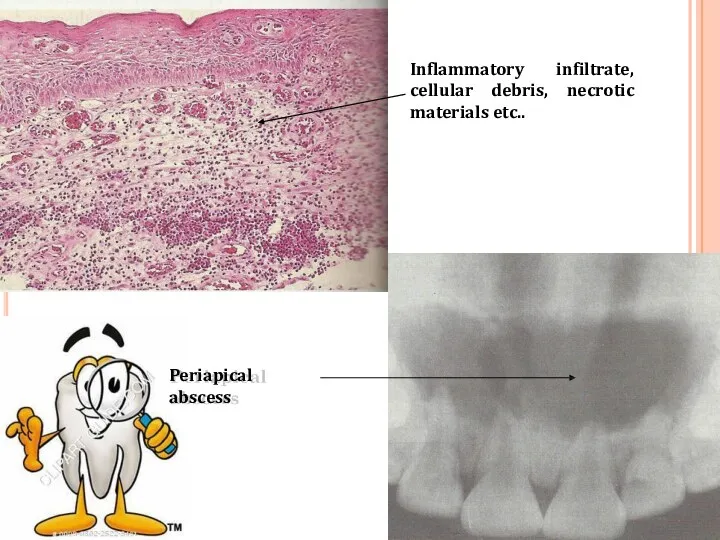
- 57. Periapical abscess Inflammatory infiltrate, cellular debris, necrotic materials etc..
- 58. The abscess cavity is surrounded by acute inflammatory cell and few chronic inflammatory cells. Dilation of
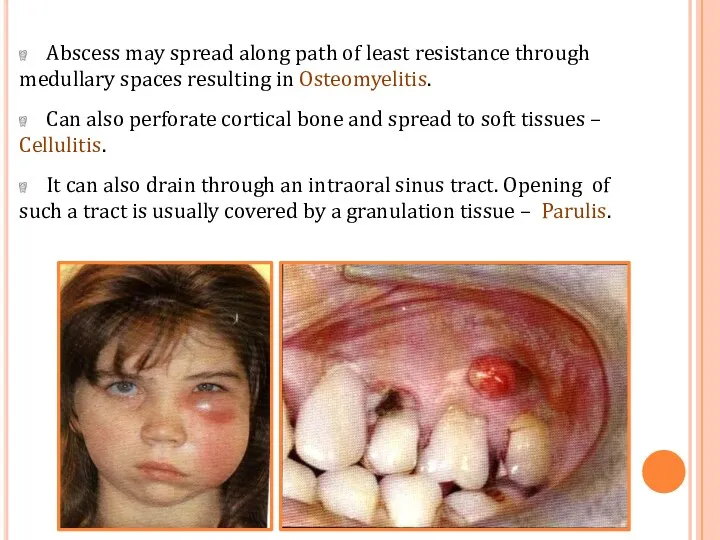
- 59. Abscess may spread along path of least resistance through medullary spaces resulting in Osteomyelitis. Can also
- 60. COMPLICATIONS Facial Cellulitis Ludwig's angina Osteomyelitis Septicaemia Menengitis, brain abscess, cavernous sinus thrombosis
- 61. It is a rapidly spreading inflammation of the soft tissues characterized by diffuse pus formation, usually
- 62. Two especially dangerous forms of cellulitis are:- cellulitis associated with mandibular teeth into submandibular and cervical
- 63. LUDWIG’S ANGINA Cellulitis of submandibular region involving sublingual, submandibular and submental spaces. In 70% cases develops
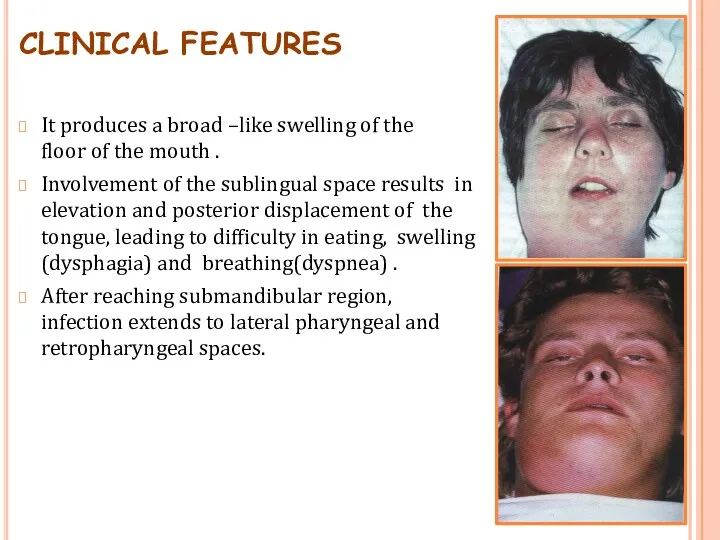
- 64. CLINICAL FEATURES It produces a broad –like swelling of the floor of the mouth . Involvement
- 65. Lateral pharyngeal space involvement may cause respiratory obstruction due to laryngeal edema(suffocation). In sever cases –
- 66. CAVERNOUS SINUS THROMBOSIS The infection from the posterior maxillary teeth reach the orbit via the maxillary
- 67. CLINICAL FEATURES Periorbital edema including lateral border of nose, protrusion and fixation of eyeball. Pupil dilatation,
- 68. Treatment High dose of penicillin. Extraction and drainage(if fluctuant). Corticosteroid and anticoagulant to prevent thrombosis and
- 70. Скачать презентацию



 Аппендициттің асқынулары
Аппендициттің асқынулары Здоровье и гигиена. Рекомендательный список литературы для родителей
Здоровье и гигиена. Рекомендательный список литературы для родителей Бронхо-обструктивный синдром у детей
Бронхо-обструктивный синдром у детей Мифы о питании
Мифы о питании Философия и принципы паллиативной помощи Palliative Care
Философия и принципы паллиативной помощи Palliative Care Гастроэзофагеальная рефлюксная болезнь
Гастроэзофагеальная рефлюксная болезнь Таңдама әдісі Кездеймоқ шамалардың негізгі статистикалық сипаттамалары
Таңдама әдісі Кездеймоқ шамалардың негізгі статистикалық сипаттамалары Болевой синдром. Медикаментозное лечение
Болевой синдром. Медикаментозное лечение Особо опасные инфекции. Холера. Чума. Геморрагические лихорадки
Особо опасные инфекции. Холера. Чума. Геморрагические лихорадки 1 грудня - Всесвітній день боротьби зі СНІДом
1 грудня - Всесвітній день боротьби зі СНІДом Фармакологическая регуляция гемостаза
Фармакологическая регуляция гемостаза Профессиональная бронхиальная астма
Профессиональная бронхиальная астма Перикардит
Перикардит Infectious diseases
Infectious diseases Поперечные методы исследования
Поперечные методы исследования Организация работы родильного дома, женской консультации
Организация работы родильного дома, женской консультации Физиологические основы формирования речевой функции
Физиологические основы формирования речевой функции Гемопоэз. Современные представления о кроветворении
Гемопоэз. Современные представления о кроветворении Всасывание лекарств
Всасывание лекарств Лекция Хир. пат. прямой кишки
Лекция Хир. пат. прямой кишки Операции при портальной гипертензии
Операции при портальной гипертензии Тромбоцитопенії, тромбоцитопатії у новонароджених. Діагностика, клініка, лікування
Тромбоцитопенії, тромбоцитопатії у новонароджених. Діагностика, клініка, лікування Определение групп крови
Определение групп крови Тірегі имплант болғанда тіс протездерін қалыптастыру ерекшеліктері
Тірегі имплант болғанда тіс протездерін қалыптастыру ерекшеліктері Листериялар. Морфология, физиология, листериялар антигені. Экологиясы. Әйелдер патологиясындағы маңызы
Листериялар. Морфология, физиология, листериялар антигені. Экологиясы. Әйелдер патологиясындағы маңызы Көмей обыры
Көмей обыры Высотная болезнь
Высотная болезнь Противоаритмические лекарственные средства
Противоаритмические лекарственные средства