Содержание
- 2. - Morbidity of intestinal infection is the highest: - in warm and/or rainy period of year
- 3. Typhoid fever Paratyphoid A, B, C
- 4. Definition Typhoid fever – is an acute intestinal anthroponotic infection with fecal - oral mechanism of
- 5. History The first data on typhoid fever obtained from the writings of the ancient historian Thucydides,
- 6. The most notorious carrier of typhoid fever was Mary Mallon, also known as Typhoid Mary. In
- 7. Gerard Manley Hopkins English poet, died of typhoid fever in 1889; Dr Tup Scott captain of
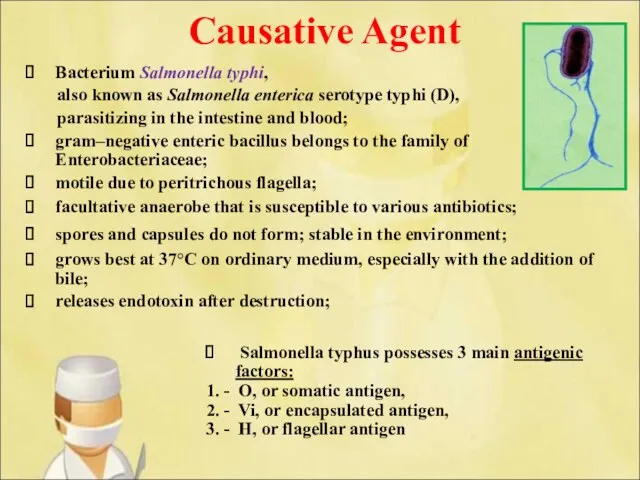
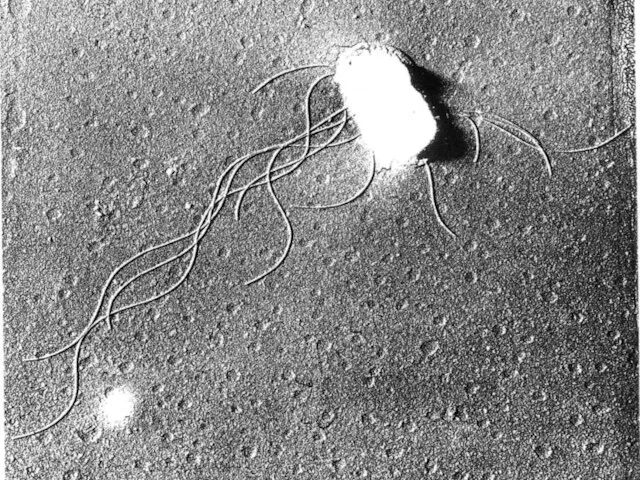
- 8. Causative Agent Bacterium Salmonella typhi, also known as Salmonella enterica serotype typhi (D), parasitizing in the
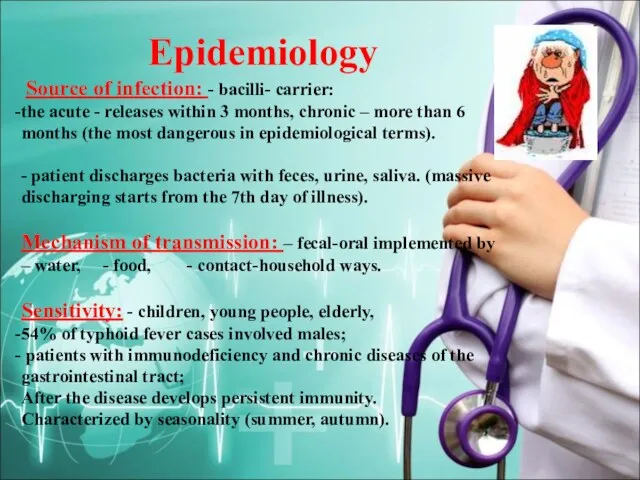
- 10. Epidemiology Source of infection: - bacilli- carrier: the acute - releases within 3 months, chronic –
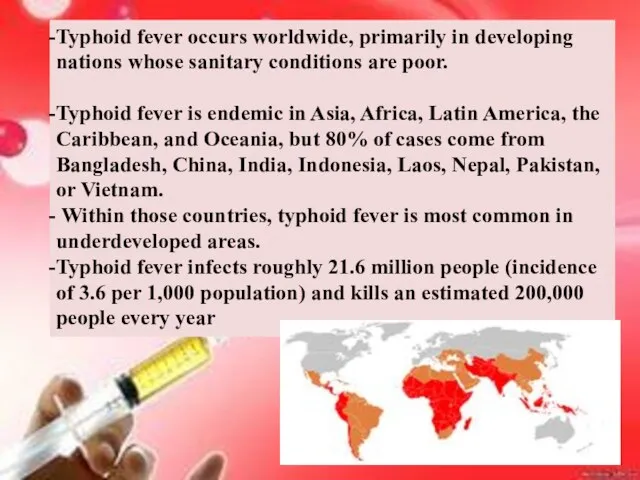
- 11. Typhoid fever occurs worldwide, primarily in developing nations whose sanitary conditions are poor. Typhoid fever is
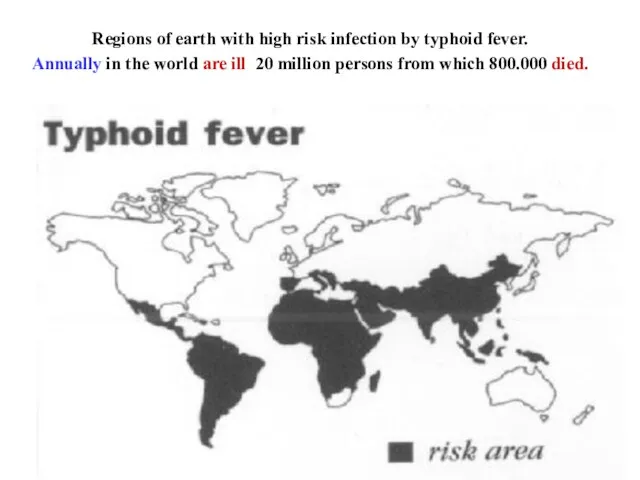
- 12. Regions of earth with high risk infection by typhoid fever. Annually in the world are ill
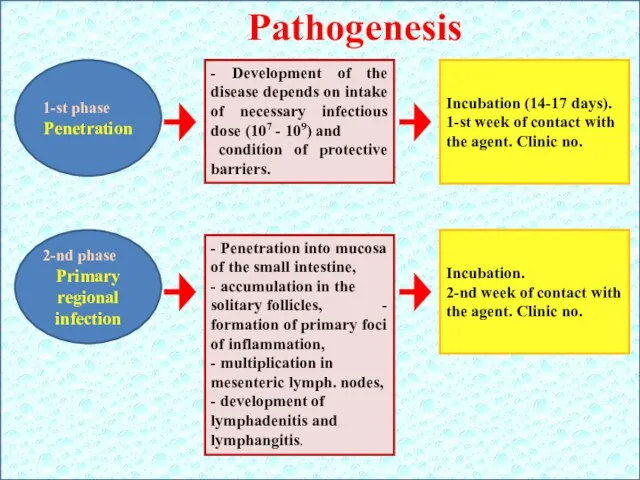
- 13. Pathogenesis 1-st phase Penetration - Development of the disease depends on intake of necessary infectious dose
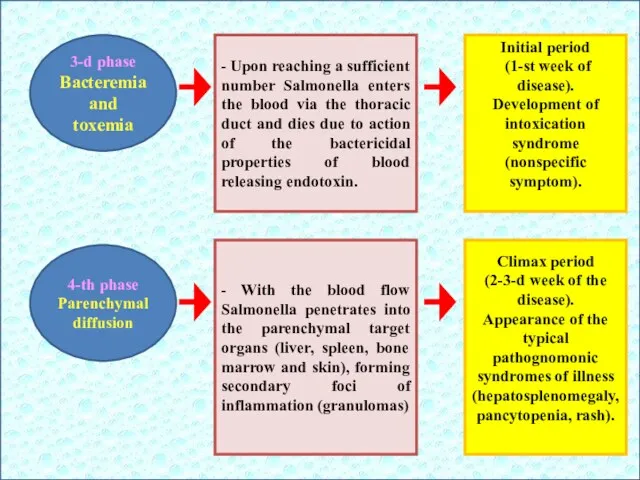
- 14. 3-d phase Bacteremia and toxemia 4-th phase Parenchymal diffusion - Upon reaching a sufficient number Salmonella
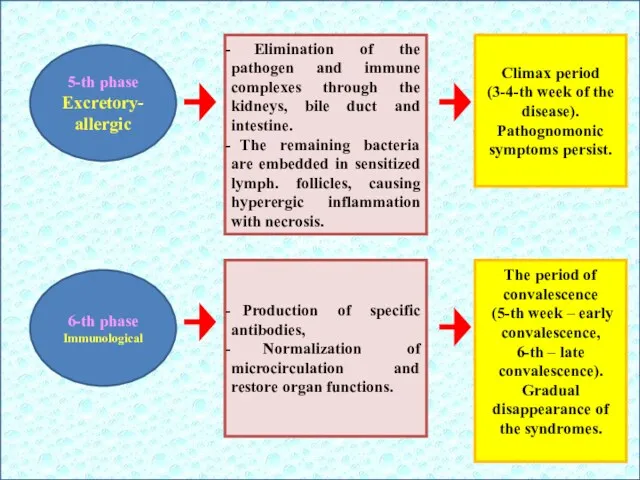
- 15. symptom 5-th phase Excretory- allergic 6-th phase Immunological Elimination of the pathogen and immune complexes through
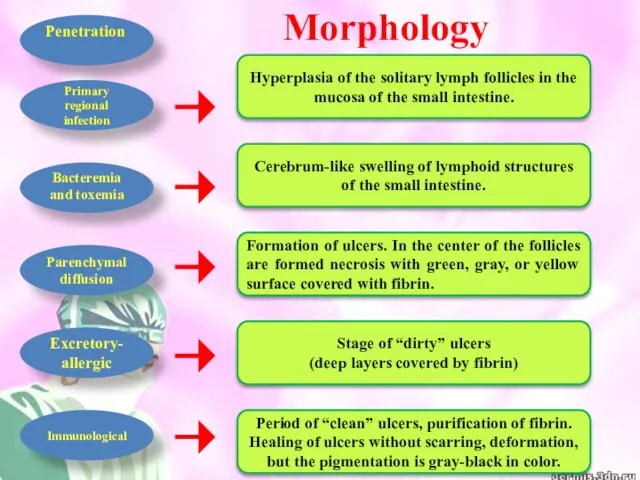
- 16. Morphology Penetration Bacteremia and toxemia Parenchymal diffusion Primary regional infection Excretory- allergic Immunological Hyperplasia of the
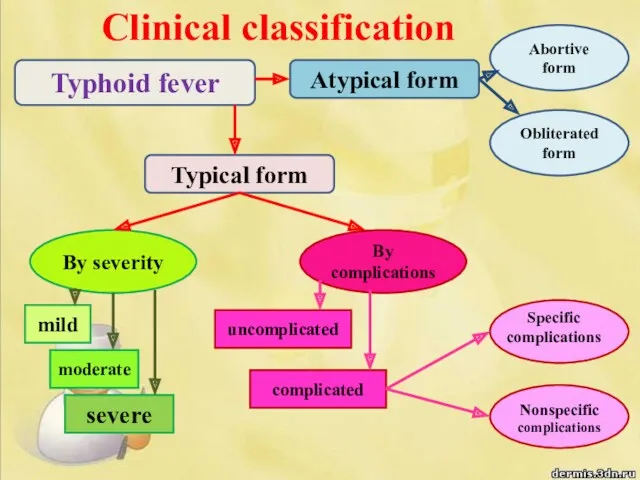
- 20. Clinical classification Typhoid fever Typical form Atypical form By severity By complications Obliterated form Abortive form
- 21. Clinical characteristics Incubation – (14-17 days) - asymptomatic; Initial period – (1 week) – nonspesific syndroms:
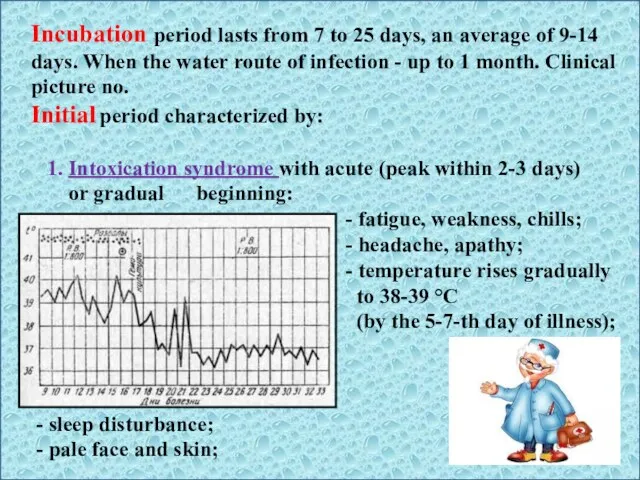
- 22. Incubation period lasts from 7 to 25 days, an average of 9-14 days. When the water
- 23. 2. Cardio-vascular syndrome: - relative bradycardia and puls dicrotia; - decrease of blood pressure; 3. Respiratory
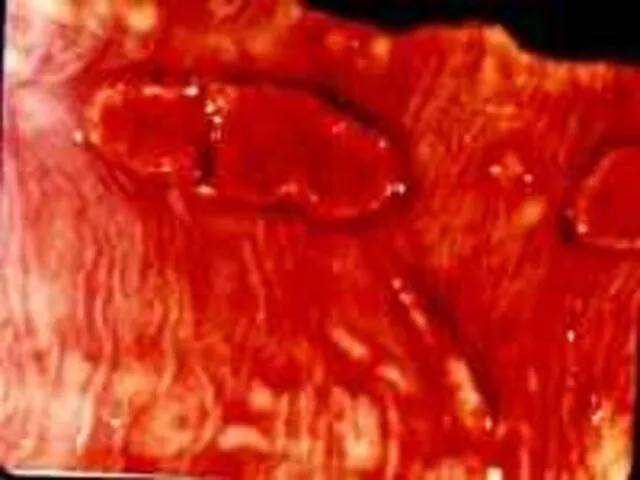
- 24. meteorism, abdomen distended, rumbling, painful along the small intestine at palpation ( ileitis); - at percussion
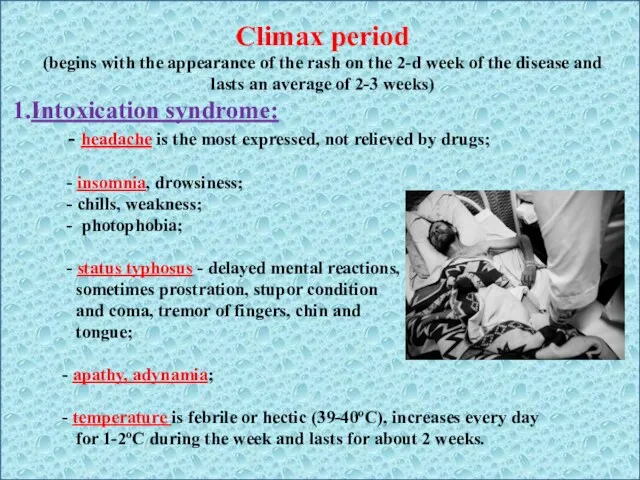
- 25. Climax period (begins with the appearance of the rash on the 2-d week of the disease
- 27. Wunderlich – trapezoidal – f. continua - daily fluctuations of temperature not more then 1ºC, The
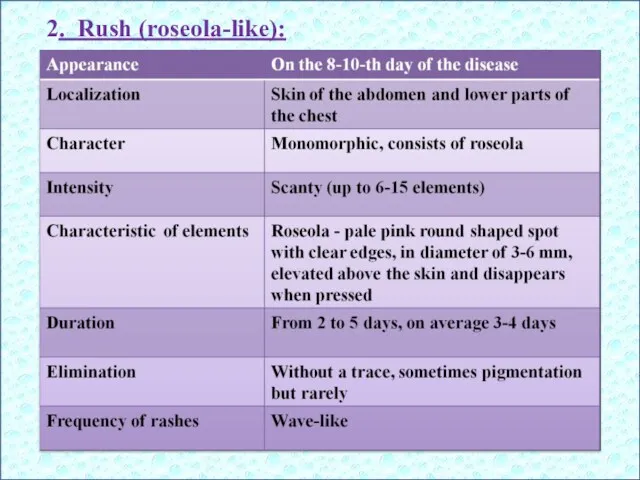
- 28. 2. Rush (roseola-like):
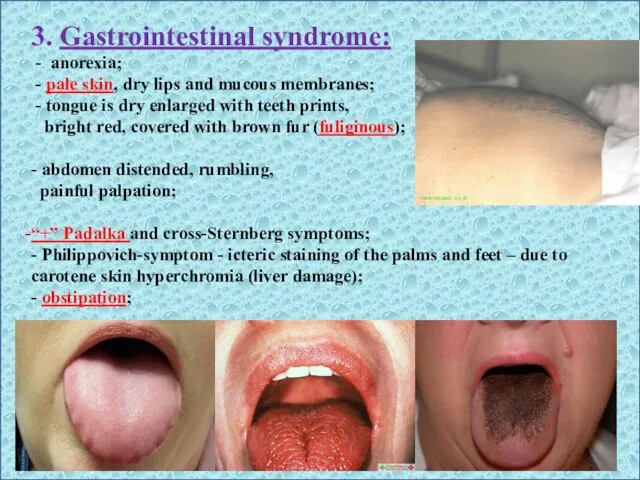
- 30. 3. Gastrointestinal syndrome: - anorexia; - pale skin, dry lips and mucous membranes; - tongue is
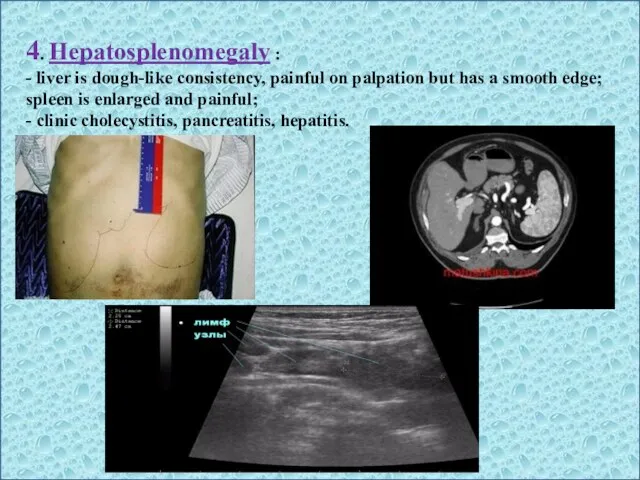
- 31. 4. Hepatosplenomegaly : - liver is dough-like consistency, painful on palpation but has a smooth edge;
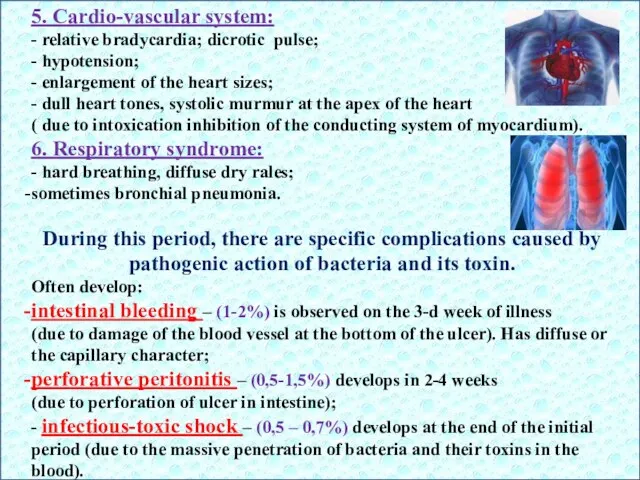
- 32. 5. Cardio-vascular system: - relative bradycardia; dicrotic pulse; - hypotension; - enlargement of the heart sizes;
- 33. Laboratory diagnostics Specific studies (allow to confirm the diagnosis): Bacteriologic analysis - the main method of
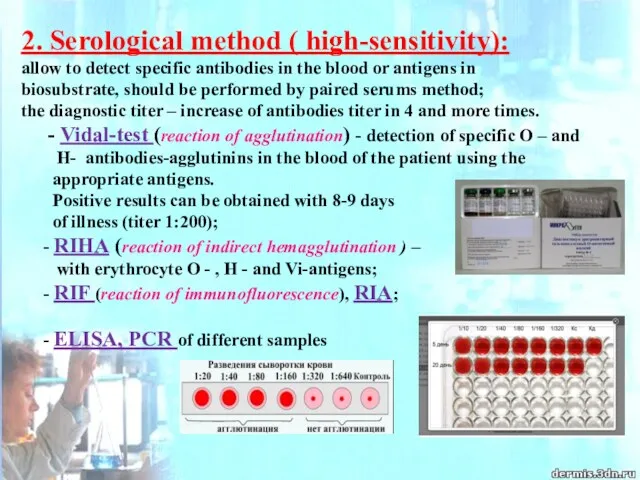
- 34. 2. Serological method ( high-sensitivity): allow to detect specific antibodies in the blood or antigens in
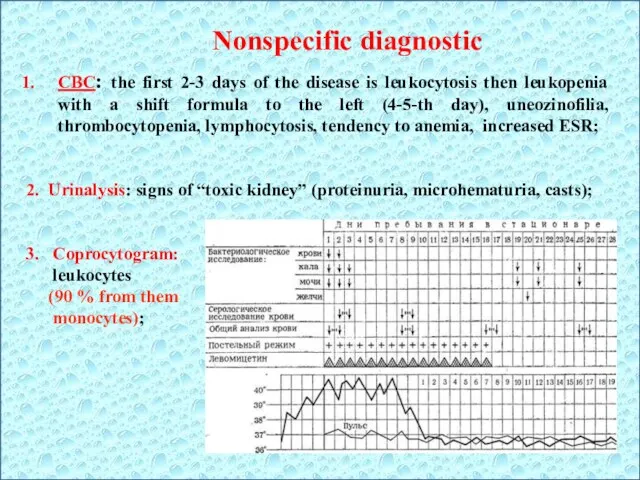
- 35. Nonspecific diagnostic CBC: the first 2-3 days of the disease is leukocytosis then leukopenia with a
- 36. Additional methods of diagnostics 1. Chest x-ray – to detect focal changes in lungs (pneumonia). 2.
- 37. Diagnostic criteria for typhoid fever epidemiological anamnesis (contact with the sick person or carrier, using of
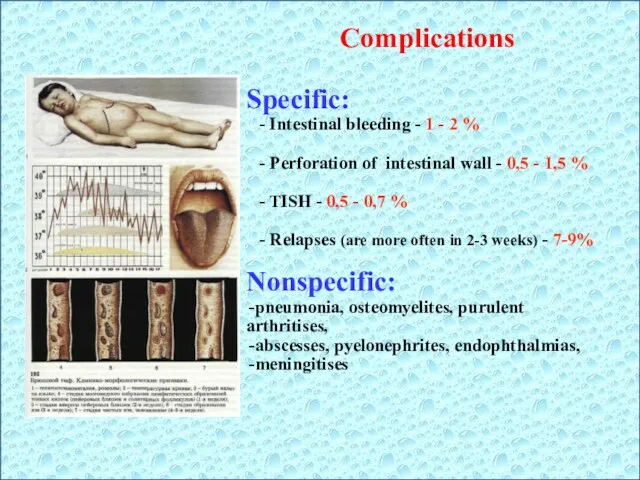
- 38. Complications Specific: - Intestinal bleeding - 1 - 2 % - Perforation of intestinal wall -
- 39. Treatment 1. Bed rest regime (prevention of complications): - strict bed regime - up to 6-7-th
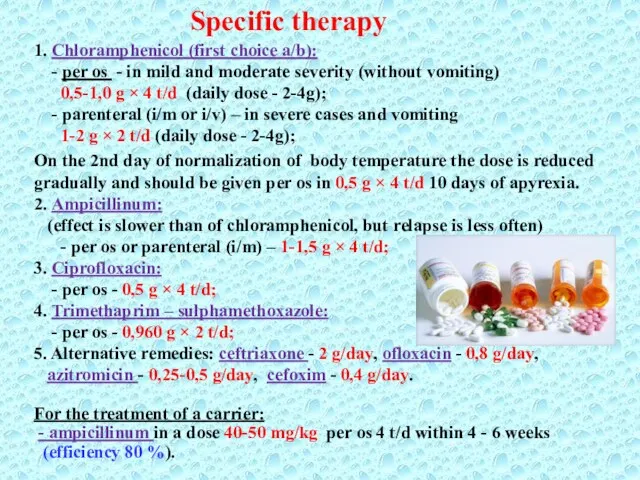
- 40. Specific therapy 1. Chloramphenicol (first choice a/b): - per os - in mild and moderate severity
- 41. Nonspesific (supporting) therapy: - desintoxication therapy (PO or IV); - sufficient hydration (PO or IV); -
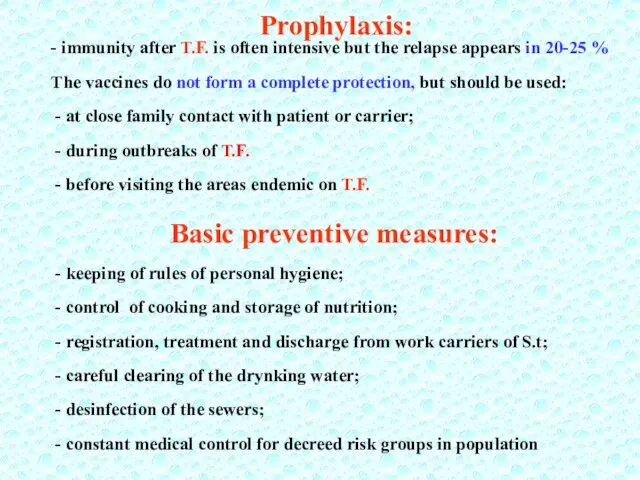
- 42. Prophylaxis: - immunity after T.F. is often intensive but the relapse appears in 20-25 % The
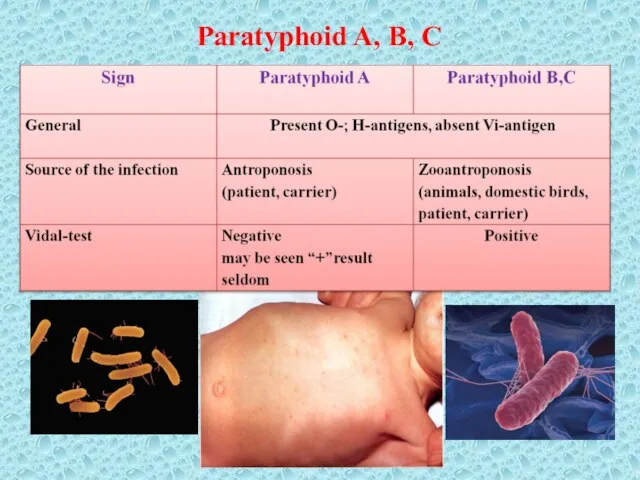
- 43. Paratyphoid A, B, C
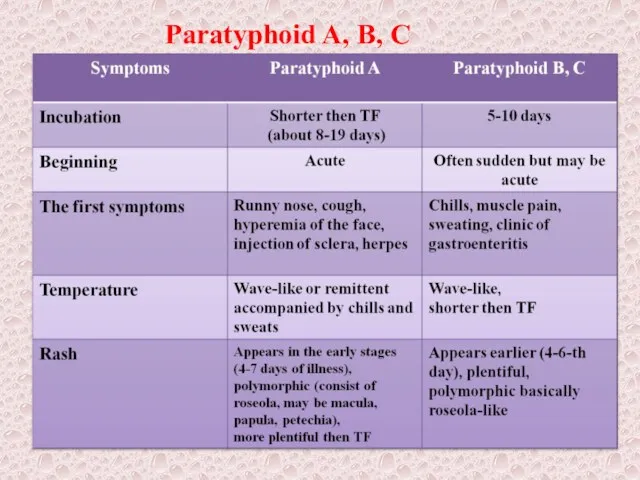
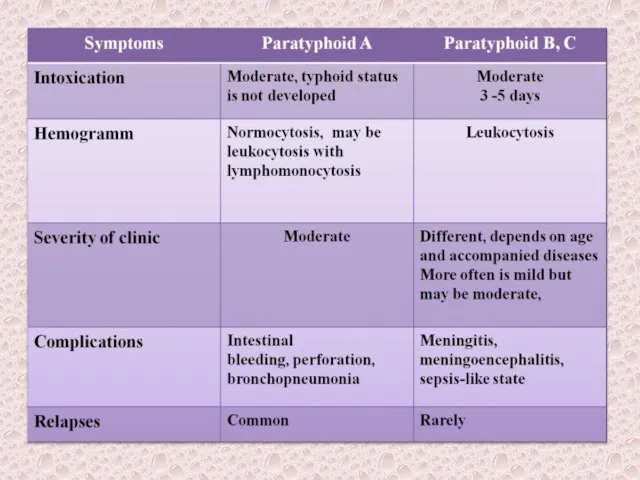
- 44. Paratyphoid A, B, C
- 48. Скачать презентацию









 US presidenticl
US presidenticl Print from the folder
Print from the folder Present Simple. Простое настоящее время
Present Simple. Простое настоящее время An englishman`s home is his castle
An englishman`s home is his castle Past Simple
Past Simple Kids box3
Kids box3 Английский алфавит
Английский алфавит Hospital Role Play
Hospital Role Play Epistemology - the doctrine of cognition
Epistemology - the doctrine of cognition Quiz. The United Kingdom of Great Britain and Northern Ireland
Quiz. The United Kingdom of Great Britain and Northern Ireland PPT - Present simple tense
PPT - Present simple tense Think level . Comparative adjectives
Think level . Comparative adjectives My room. A flat
My room. A flat Idioms with parts of the body
Idioms with parts of the body Customs,Traditions and people of wales
Customs,Traditions and people of wales What’s the weather like
What’s the weather like How about jogging
How about jogging Тренажёр ЕГЭ
Тренажёр ЕГЭ My perfect school!
My perfect school! The past form of become is
The past form of become is Иностранный язык в сфере юриспруденции
Иностранный язык в сфере юриспруденции Sport
Sport Domestic and wild animals
Domestic and wild animals Australia
Australia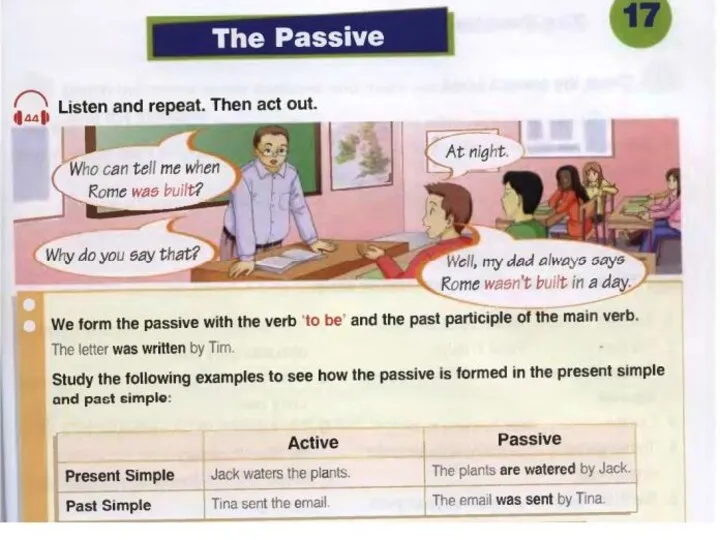 Passive voice
Passive voice Hobby in Britain
Hobby in Britain The United States of America
The United States of America My home
My home