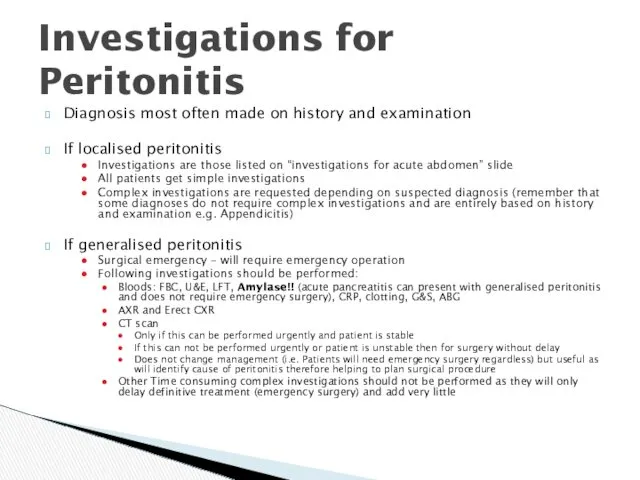
Diagnosis most often made on history and examination
If localised peritonitis
Investigations are
those listed on “investigations for acute abdomen” slide
All patients get simple investigations
Complex investigations are requested depending on suspected diagnosis (remember that some diagnoses do not require complex investigations and are entirely based on history and examination e.g. Appendicitis)
If generalised peritonitis
Surgical emergency – will require emergency operation
Following investigations should be performed:
Bloods: FBC, U&E, LFT, Amylase!! (acute pancreatitis can present with generalised peritonitis and does not require emergency surgery), CRP, clotting, G&S, ABG
AXR and Erect CXR
CT scan
Only if this can be performed urgently and patient is stable
If this can not be performed urgently or patient is unstable then for surgery without delay
Does not change management (i.e. Patients will need emergency surgery regardless) but useful as will identify cause of peritonitis therefore helping to plan surgical procedure
Other Time consuming complex investigations should not be performed as they will only delay definitive treatment (emergency surgery) and add very little
Investigations for Peritonitis
 Питание кормящей матери
Питание кормящей матери Эффект Допплера
Эффект Допплера Управление качеством медицинской помощи
Управление качеством медицинской помощи Медицинские приборно-компьютерные системы. (Лекция 4)
Медицинские приборно-компьютерные системы. (Лекция 4) Вакцинопрофилактика коклюша. Часть 2
Вакцинопрофилактика коклюша. Часть 2 Хронические миелопролиферативные заболевания
Хронические миелопролиферативные заболевания Дәрілік өсімдіктерді халық медицинасында қолдану тарихы
Дәрілік өсімдіктерді халық медицинасында қолдану тарихы Естественные факторы защиты организма. Механизмы иммунной защиты
Естественные факторы защиты организма. Механизмы иммунной защиты Энтеровирусная инфекция
Энтеровирусная инфекция Определение и оценка физического развития
Определение и оценка физического развития Токсоплазмоз. Распространённость токсоплазмоза
Токсоплазмоз. Распространённость токсоплазмоза Науқасқа, оның отбасына және туыстарына каралы хабарды жеткiзу
Науқасқа, оның отбасына және туыстарына каралы хабарды жеткiзу Философия сестринского дела
Философия сестринского дела Респираторлық дистресс синдромы
Респираторлық дистресс синдромы Шизофрения, шизотипические и бредовые расстройства
Шизофрения, шизотипические и бредовые расстройства Хирургическое лечение приобретенных пороков сердца. Митральный, аортальный порок, сочетанное поражение двух клапанов сердца
Хирургическое лечение приобретенных пороков сердца. Митральный, аортальный порок, сочетанное поражение двух клапанов сердца Клинический случай миелодиспластического синдрома
Клинический случай миелодиспластического синдрома Морфологические элементы сыпи
Морфологические элементы сыпи Деонтология.Дәрігер-стоматолог
Деонтология.Дәрігер-стоматолог Проблемы нормативного обеспечения в сфере информатизации здравоохранения
Проблемы нормативного обеспечения в сфере информатизации здравоохранения Портфели влияют на нашу осанку
Портфели влияют на нашу осанку Симптомы, проявления, диагностика и лечение васкулита
Симптомы, проявления, диагностика и лечение васкулита Жылқының шаншу түрінде өтетін аурулары
Жылқының шаншу түрінде өтетін аурулары Техника кесарева сечения
Техника кесарева сечения Массаж
Массаж Новое рентгеновское оборудование в медицине
Новое рентгеновское оборудование в медицине Заболевания конечностей и их лечение. Ортопедическая ковка
Заболевания конечностей и их лечение. Ортопедическая ковка ЛФК в хирургии после оперативных вмешательств
ЛФК в хирургии после оперативных вмешательств