Содержание
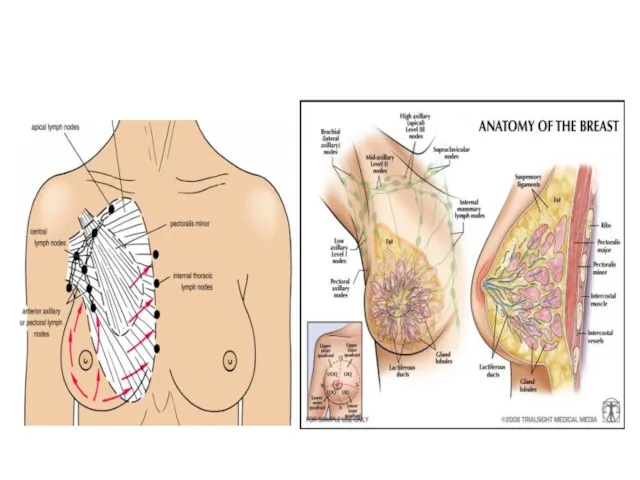
- 2. Anatomy of the Breast
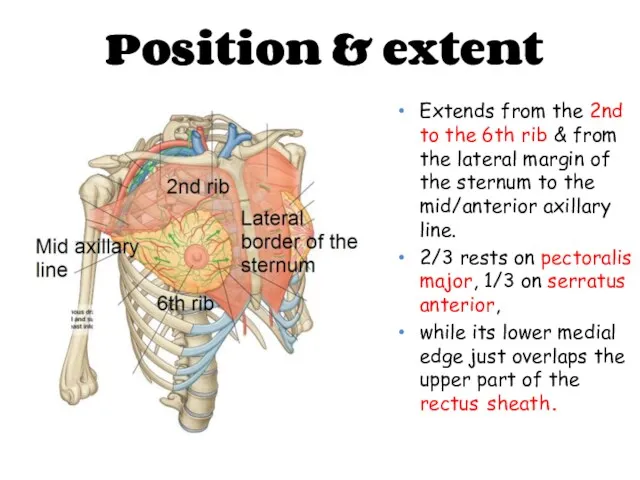
- 3. Position & extent Extends from the 2nd to the 6th rib & from the lateral margin
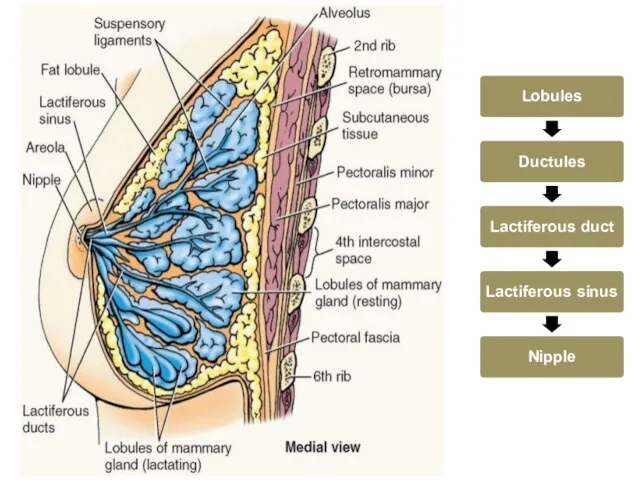
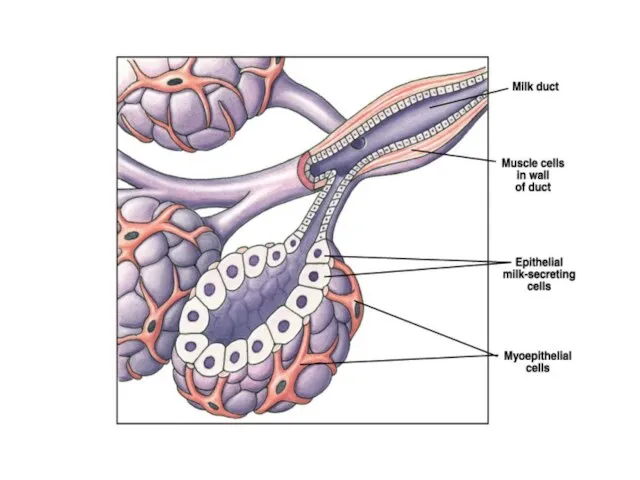
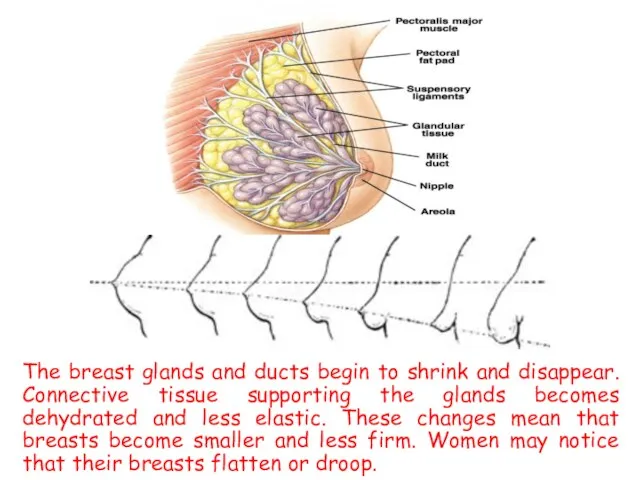
- 4. Structure of the Breast The lobule is the basic structural unit of the mammary gland.The number
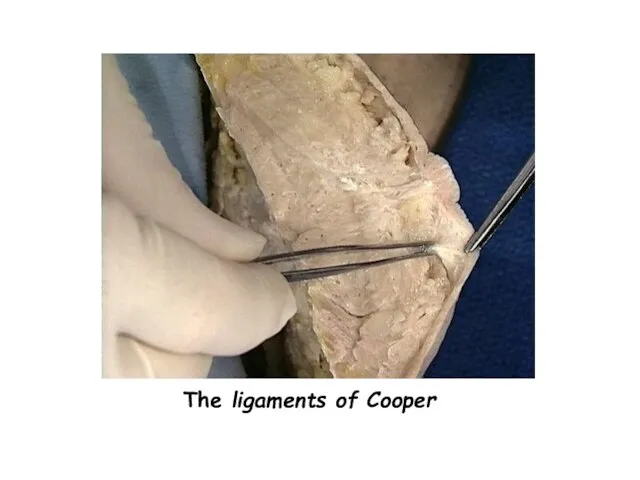
- 5. The ligaments of Cooper are hollow conical projections of fibrous tissue filled with breast tissue; the
- 7. The ligaments of Cooper
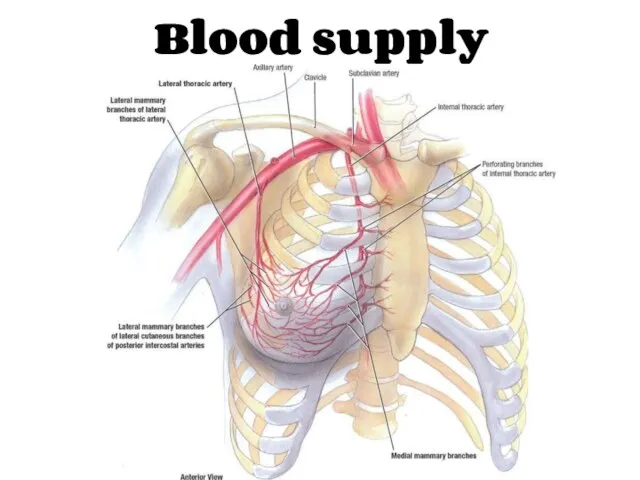
- 8. Blood supply
- 9. Internal thoracic”mammary” artery – perforating branches Axillary artery – Lateral thoracic artery ”mainly” Superior thoracic artery
- 10. Venous drainage Sub areolar venous plexus Posterior intercostal veins communicate with internal vertebral venous plexus veins
- 11. • Cutaneous innervation • Medial pectoral nerve • Lateral pectoral nerve • Long thoracic nerve Nerves
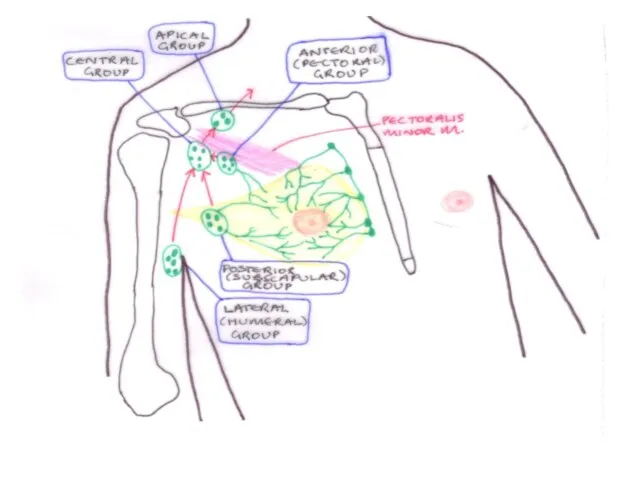
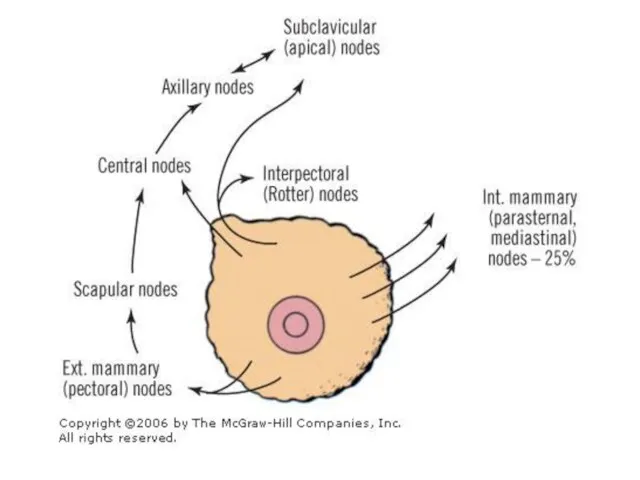
- 12. The lymphatics of the breast drain predominantly into the axillary and internal mammary lymph nodes. The
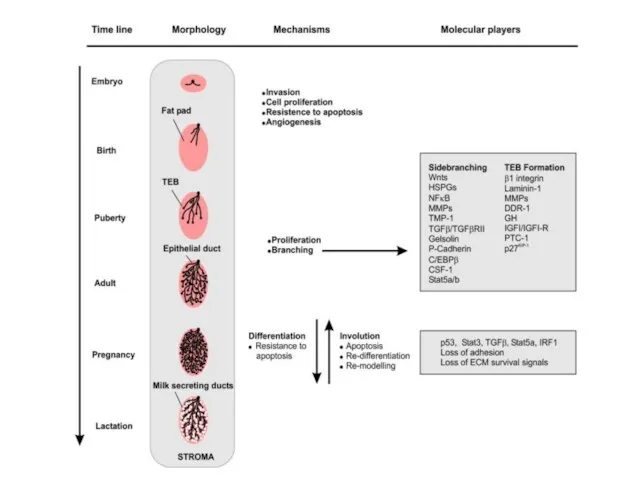
- 17. Physiology of the Breast
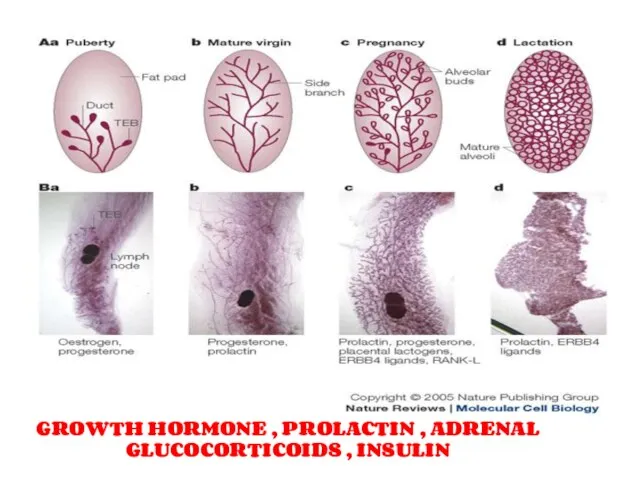
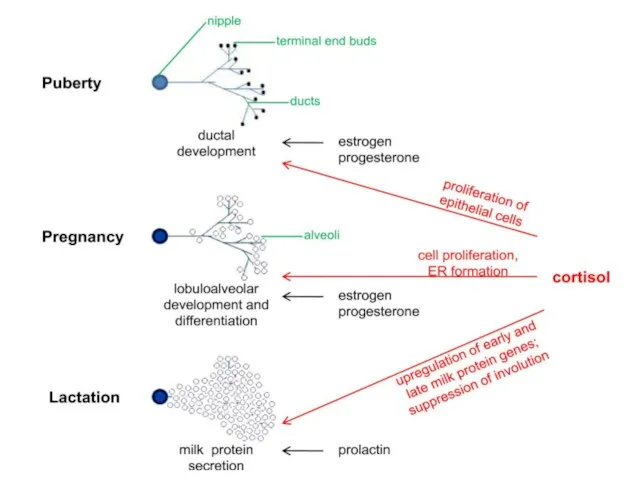
- 18. GROWTH HORMONE , PROLACTIN , ADRENAL GLUCOCORTICOIDS , INSULIN
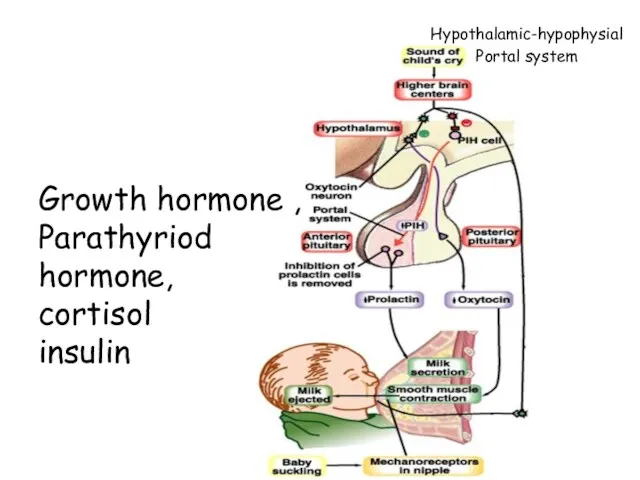
- 20. Hypothalamic-hypophysial Portal system Growth hormone , Parathyriod hormone, cortisol insulin
- 22. The breast glands and ducts begin to shrink and disappear. Connective tissue supporting the glands becomes
- 23. Benign Breast Disease
- 24. Benign Breast Disease The most common cause of breast problems. 30% of women will suffer from
- 25. Benign breast disease Benign conditions of the nipple. Aberrations of normal development & involution. Fibroadenomas &
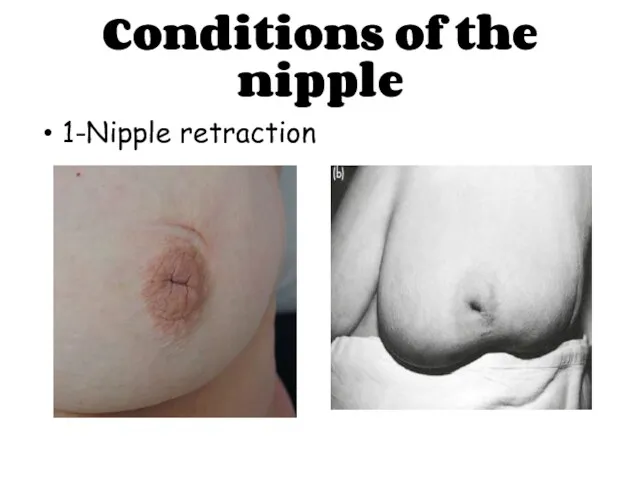
- 26. Conditions of the nipple 1-Nipple retraction
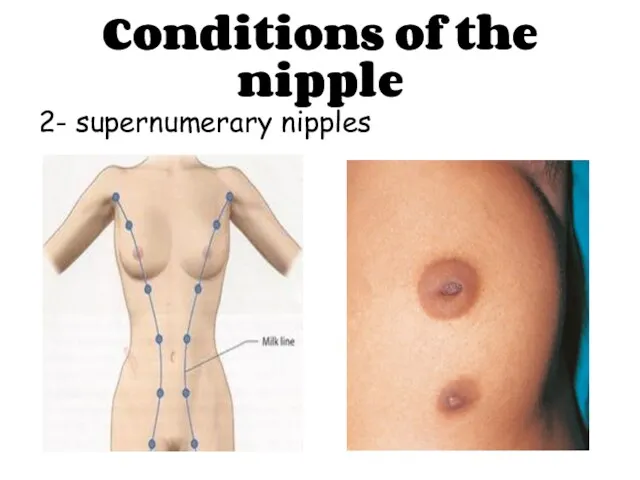
- 27. Conditions of the nipple 2- supernumerary nipples
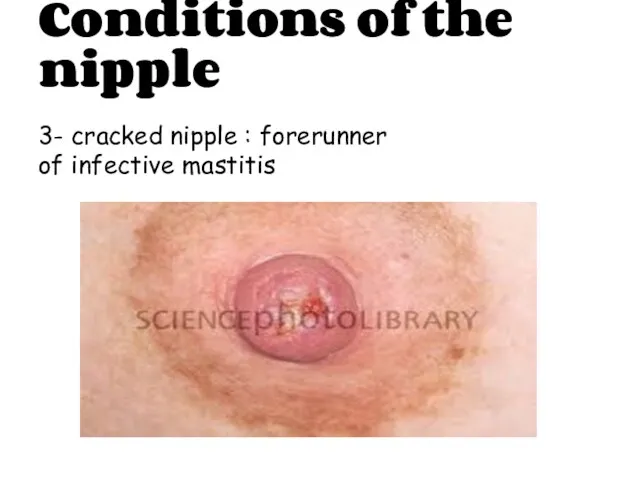
- 28. Conditions of the nipple 3- cracked nipple : forerunner of infective mastitis
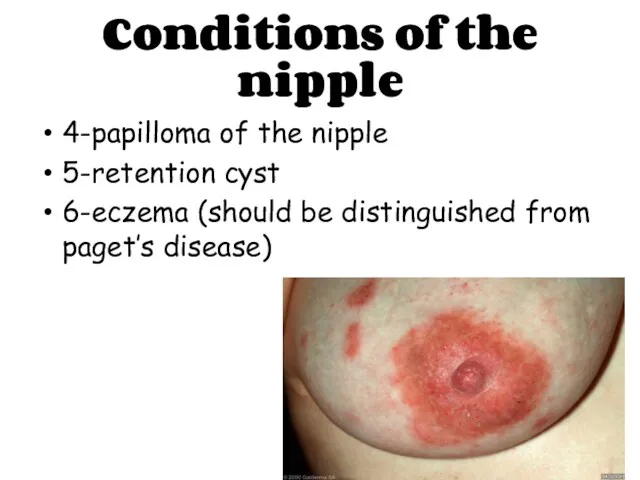
- 29. Conditions of the nipple 4-papilloma of the nipple 5-retention cyst 6-eczema (should be distinguished from paget’s
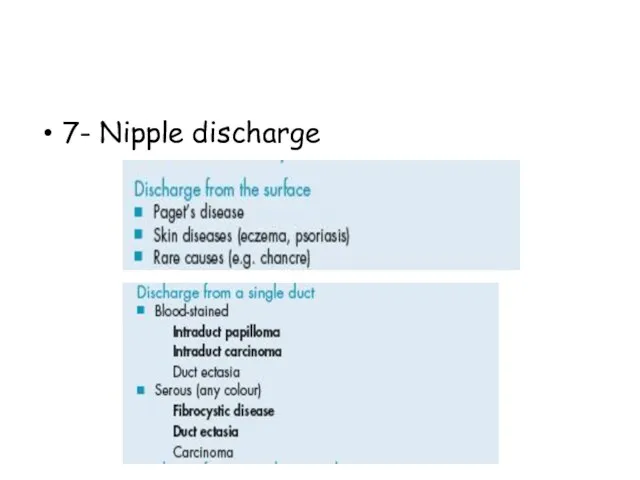
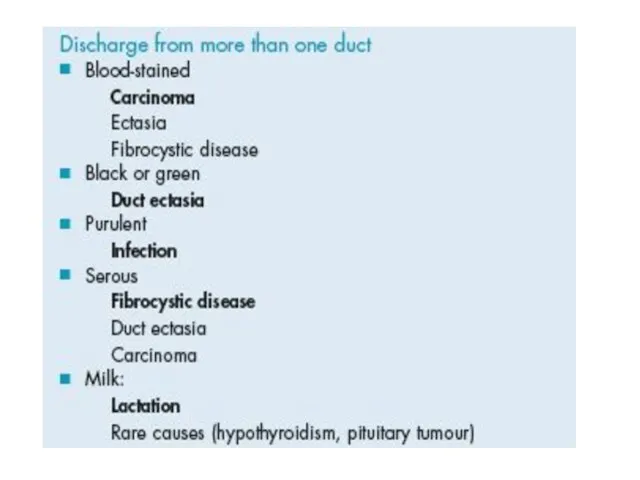
- 31. 7- Nipple discharge
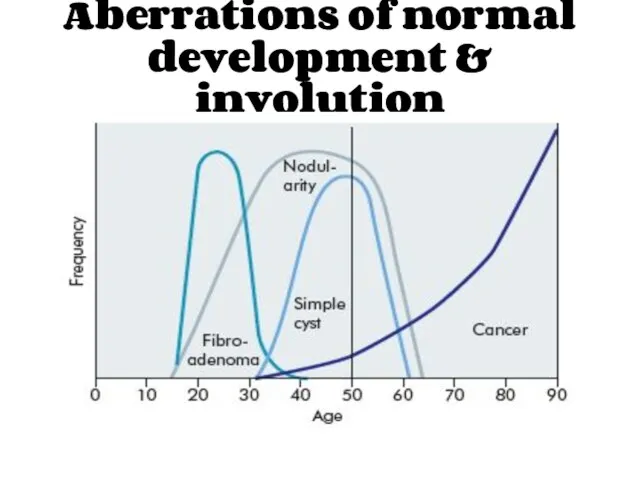
- 33. Aberrations of normal development & involution
- 34. Aberrations of normal development & involution Cyst formation Fibrosis Hyperplasia Papillomatosis
- 35. ANDI Breast cysts
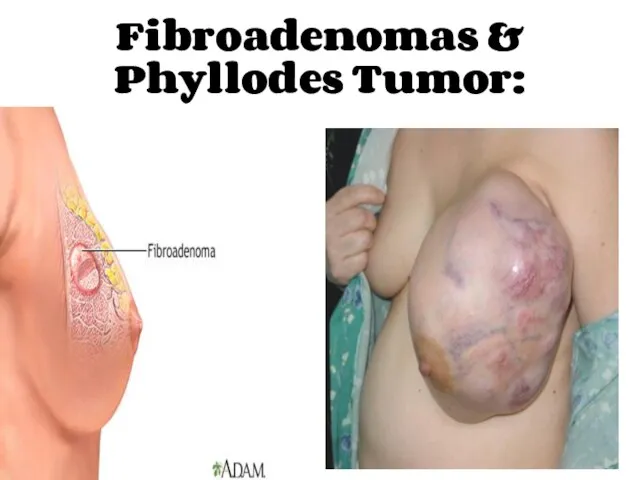
- 36. Fibroadenomas & Phyllodes Tumor:
- 37. Acute and Subacute Inflammations of the Breast:
- 38. 1- Bacterial mastitis & breast abscess:
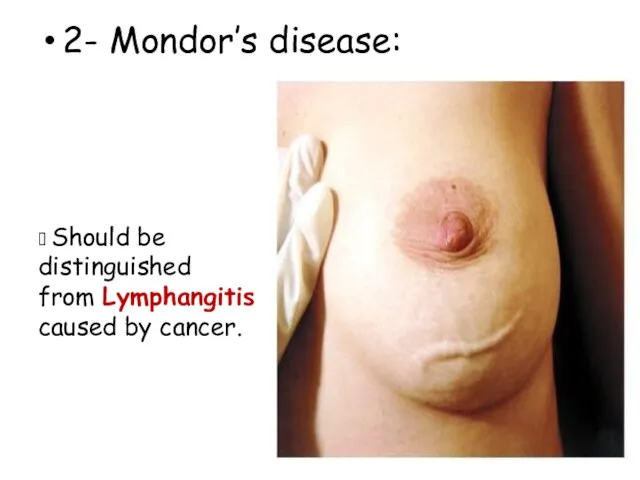
- 39. 2- Mondor’s disease: ? Should be distinguished from Lymphangitis caused by cancer.
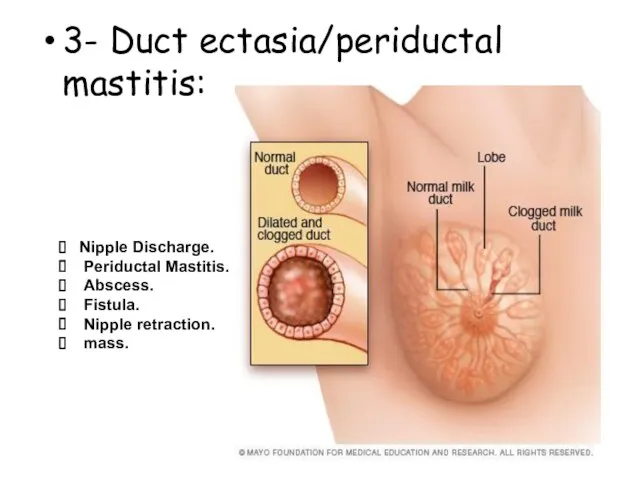
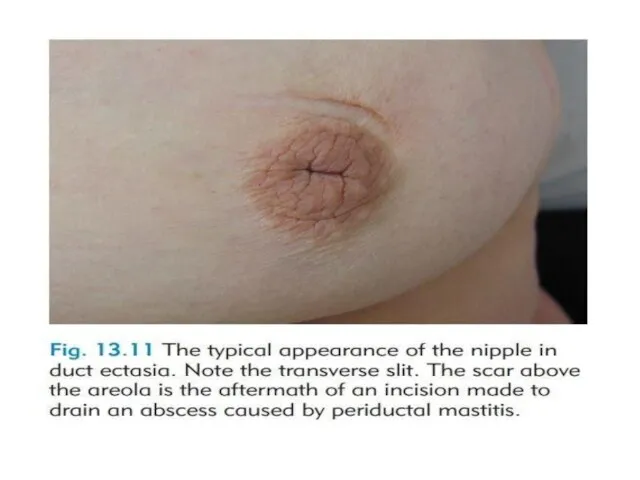
- 40. 3- Duct ectasia/periductal mastitis: Nipple Discharge. Periductal Mastitis. Abscess. Fistula. Nipple retraction. mass.
- 42. Injuries to the Breast: 1- Haematoma. 2-Traumatic fat necrosis.
- 43. Congenital Abnormalities:
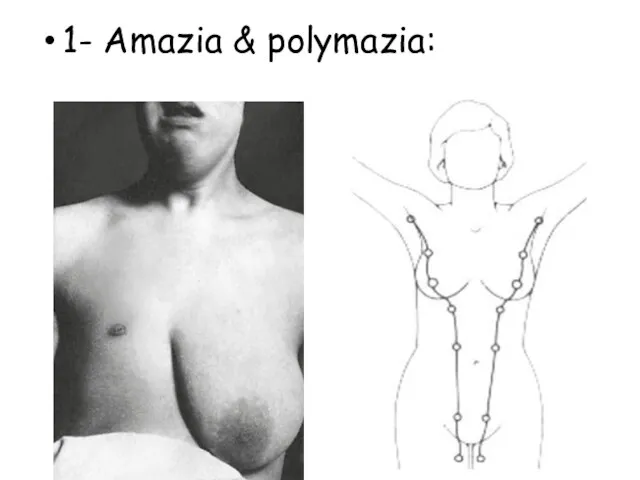
- 44. 1- Amazia & polymazia:
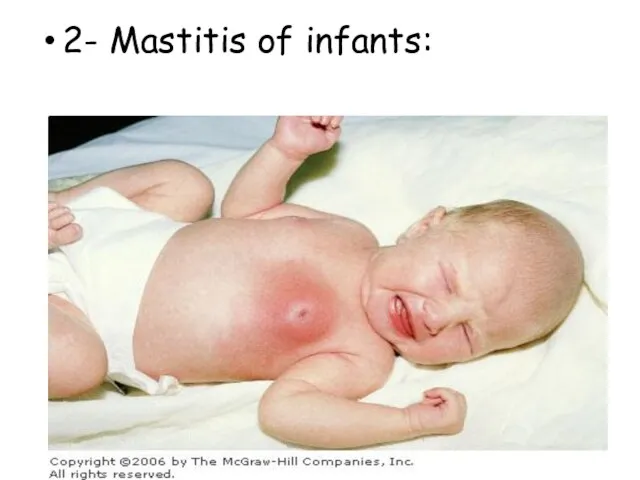
- 45. 2- Mastitis of infants:
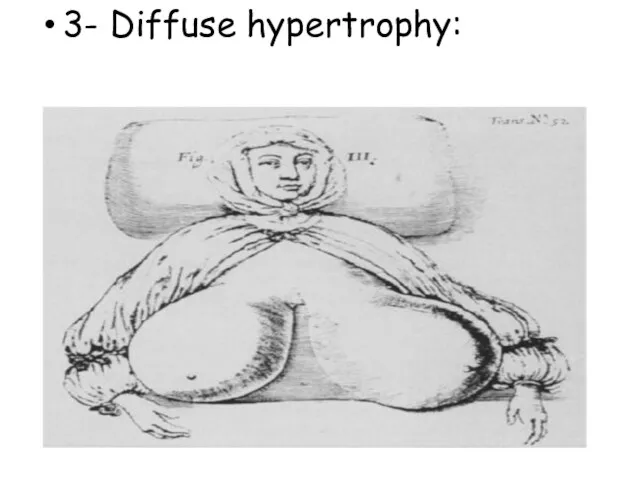
- 46. 3- Diffuse hypertrophy:
- 47. Malignant diseases CARCINOMA OF THE BREAST
- 48. Breast cancer is the second most common cancer with nearly 1.7 million new cases in 2012.
- 49. Aetiological factors Geographical… Age… Gender… Genetic… Diet… Endocrine… Previous radiation…
- 50. Pathogenesis Genetic factor… Hormonal factor… Enviromental factor…
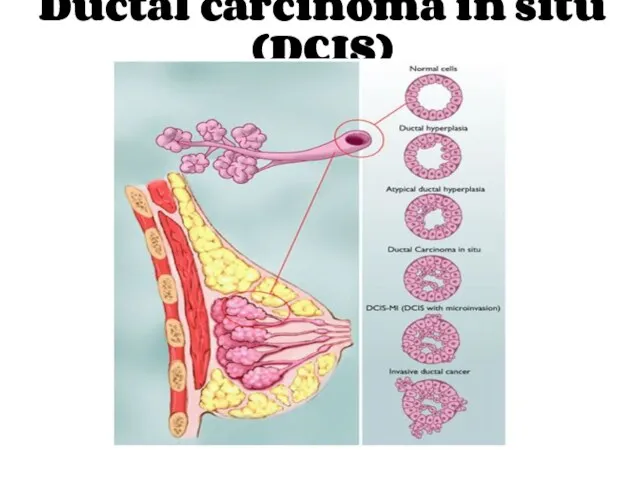
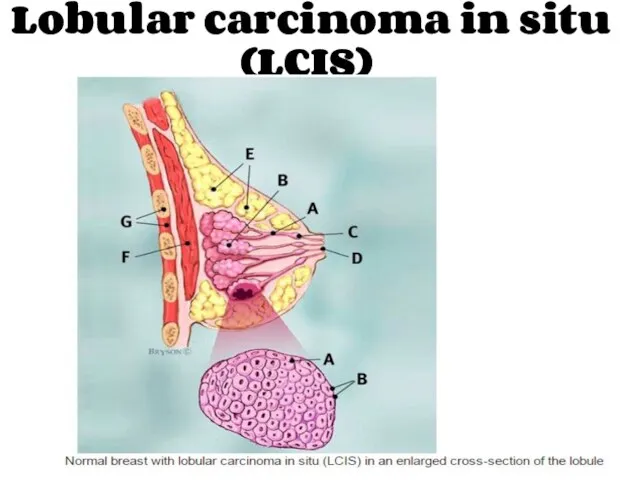
- 51. Histopathologic classification Ductal ------ Lobular Invasive ------ In situ
- 52. Breast carcinoma in situ
- 53. Ductal carcinoma in situ (DCIS)
- 54. Lobular carcinoma in situ (LCIS)
- 55. In situ carcinoma is pre-invasive cancer. Becoming increasingly common. At least 20% of patients will develop
- 56. Treatment Surgical excision Mastectomy? Partial mastectomy with safety margins > 1cm Radiotherapy?
- 57. Invasive breast carcinoma
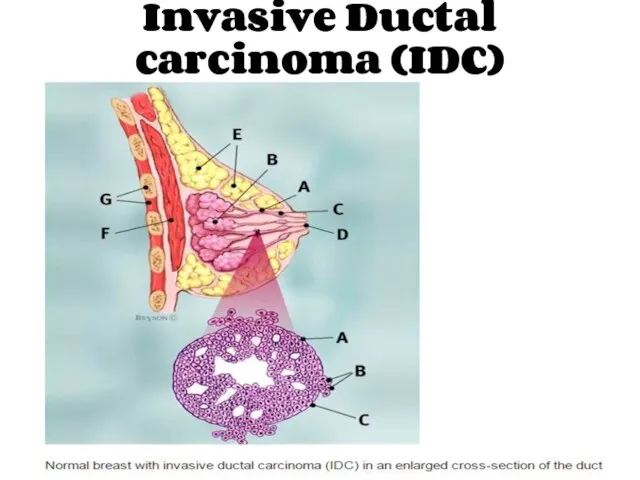
- 58. Invasive Ductal carcinoma (IDC)
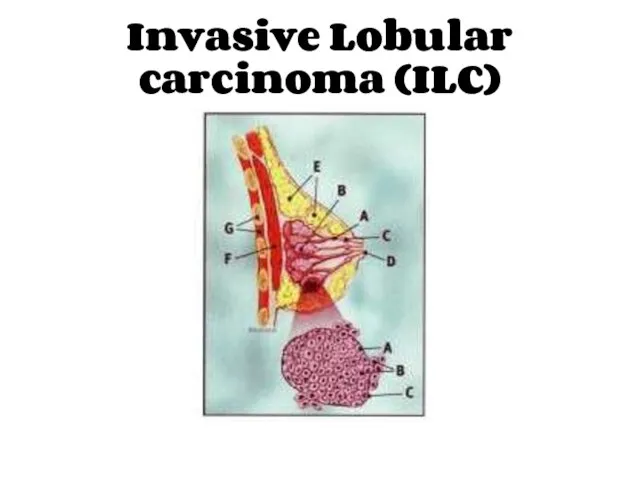
- 59. Invasive Lobular carcinoma (ILC)
- 60. Other rarer variants Colloid (mucinous) carcinoma: produce abundant mucin. Medullary carcinoma: solid sheets of large cells
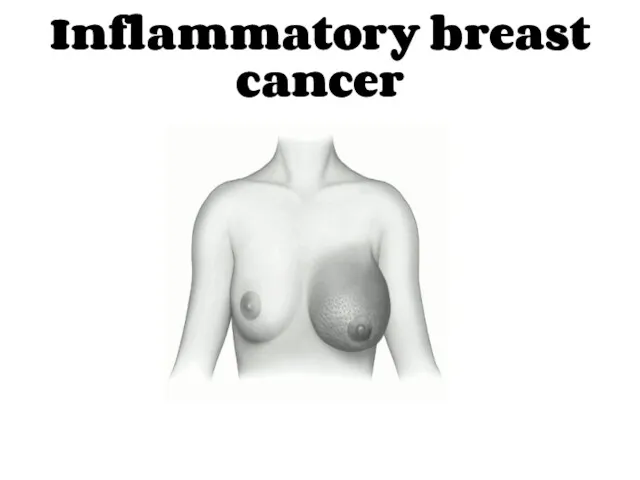
- 61. Inflammatory breast cancer
- 62. Rare, highly aggressive cancer that presents as a painful, swollen breast, which is warm with cutaneous
- 63. Paget Disease of the Nipple
- 64. It is a superficial manifestation of an underlying breast carcinoma (IDC or DCIS). Presents as an
- 65. The spread of breast cancer Local spread… Lymphatic metastasis… Hematogenous spread…
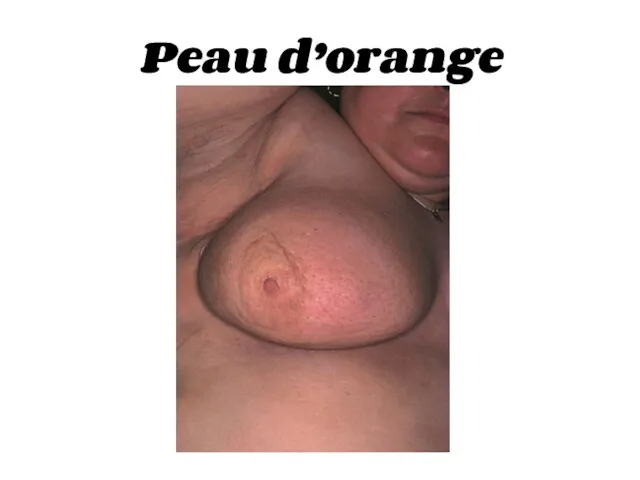
- 66. Phenomena resulting from lymphatic obstruction in advanced breast cancer:
- 67. Peau d’orange
- 68. Cancer-en-cuirasse
- 69. Lymphangiosarcoma
- 71. Breast Carcinoma Grading The degree of differentiation: Well differentiated. Moderately differentiated. Poorly differentiated.
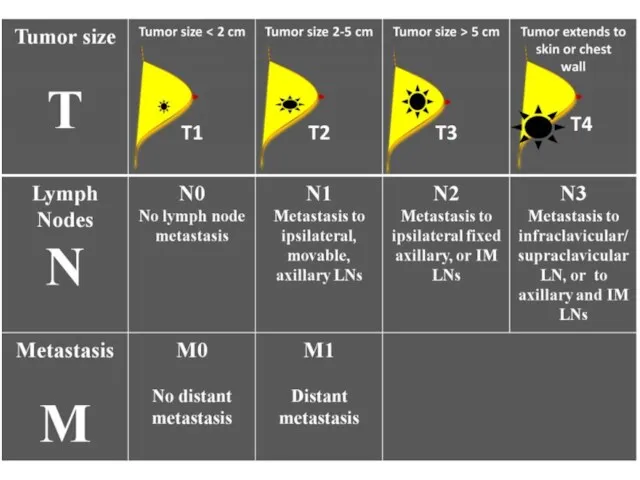
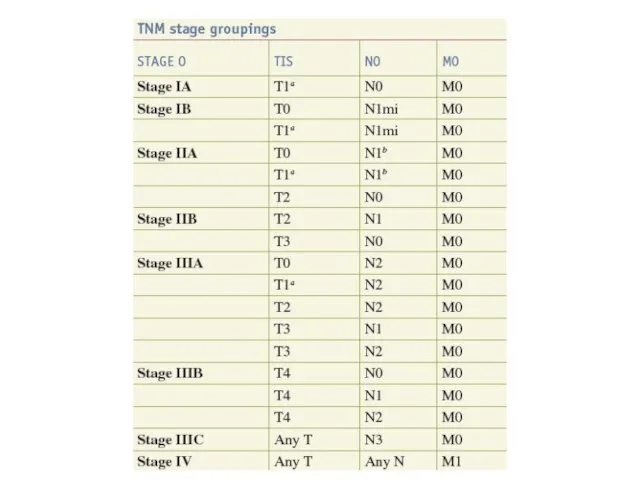
- 72. Breast cancer staging TNM staging takes into account: The size of the tumour (T). Whether the
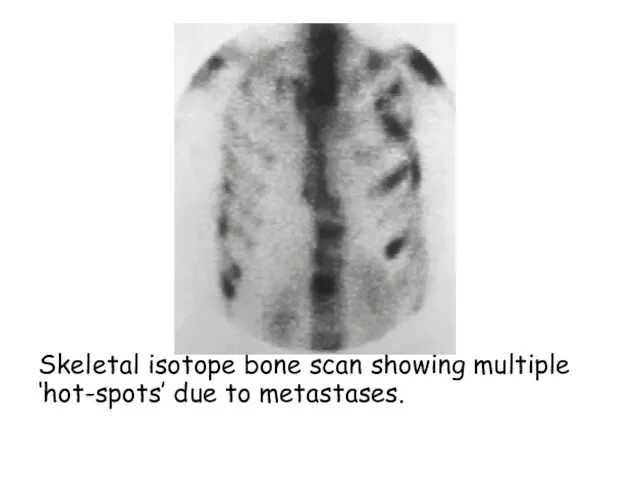
- 75. Skeletal isotope bone scan showing multiple ‘hot-spots’ due to metastases.
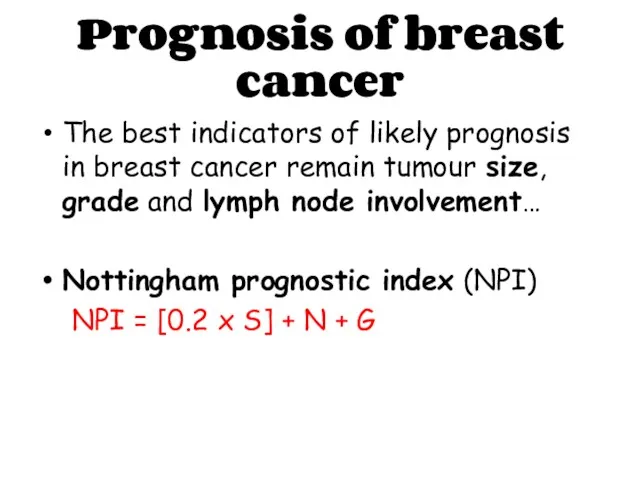
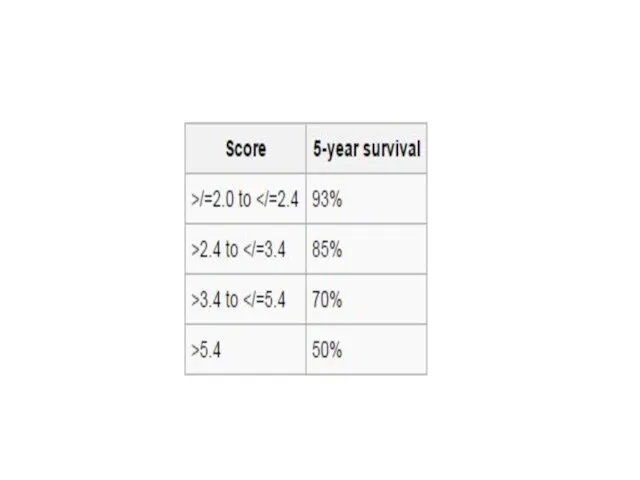
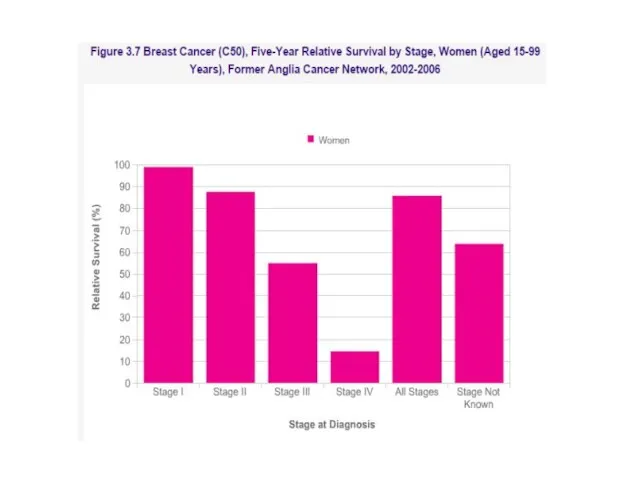
- 76. Prognosis of breast cancer The best indicators of likely prognosis in breast cancer remain tumour size,
- 79. Breast Cancer in Men Breast Cancer in Men accounts for less than 1% of male cancers
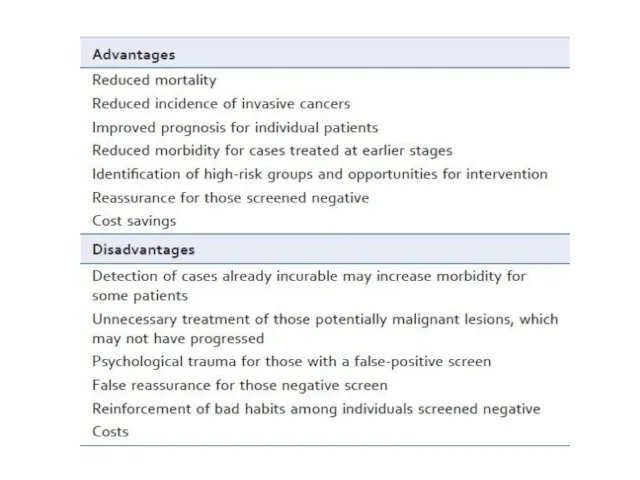
- 80. Screening & Imaging Breast screening aims to find breast cancers early. It uses an X-ray test
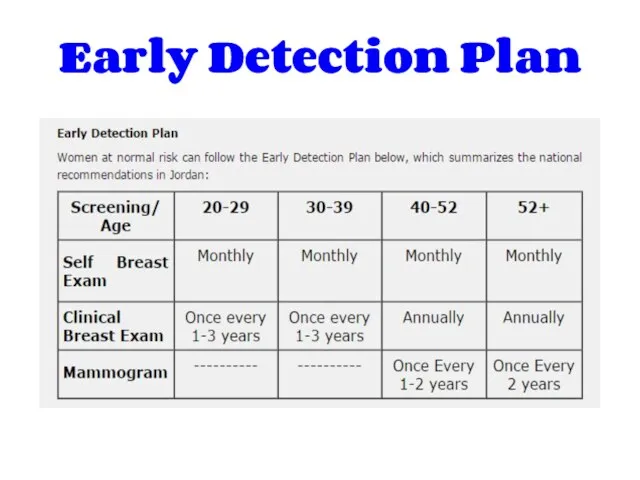
- 82. Early Detection Plan
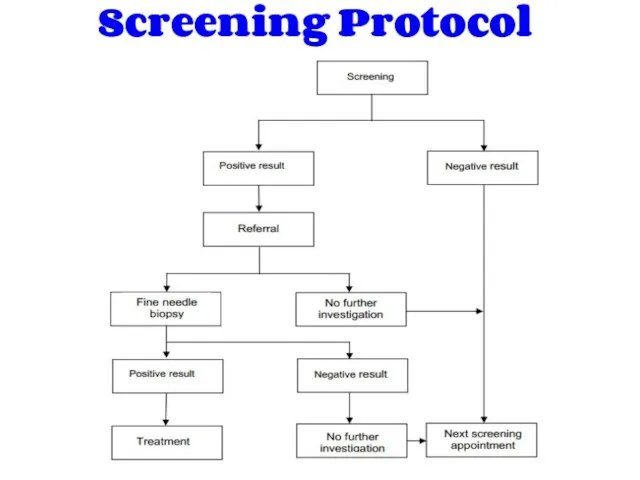
- 83. Screening Protocol
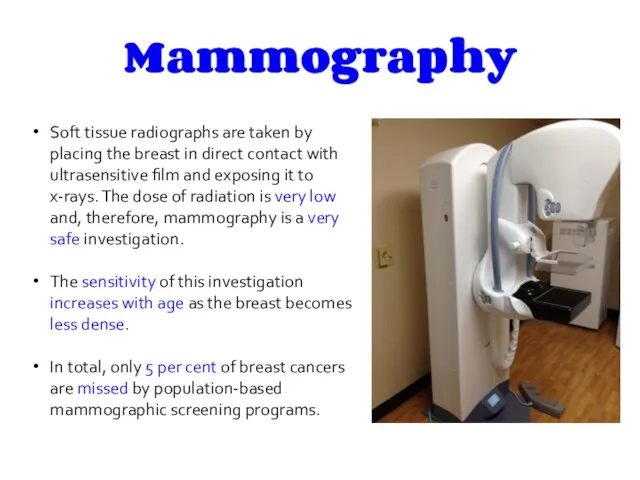
- 84. Mammography Soft tissue radiographs are taken by placing the breast in direct contact with ultrasensitive film
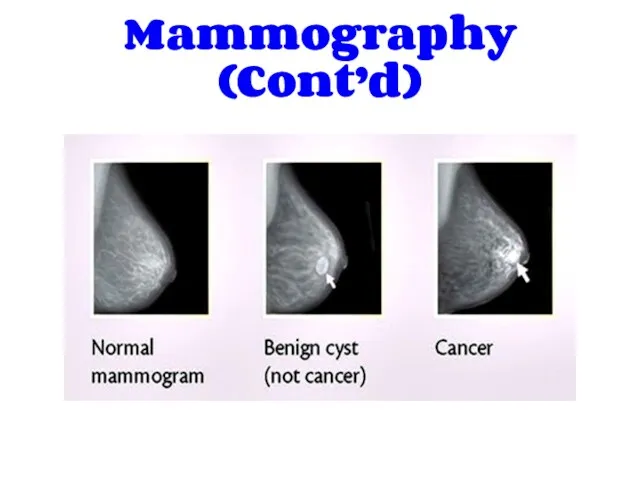
- 85. Mammography (Cont’d)
- 86. Ultrasonography Ultrasound is particularly useful in young women with dense breasts in whom mammograms are difficult
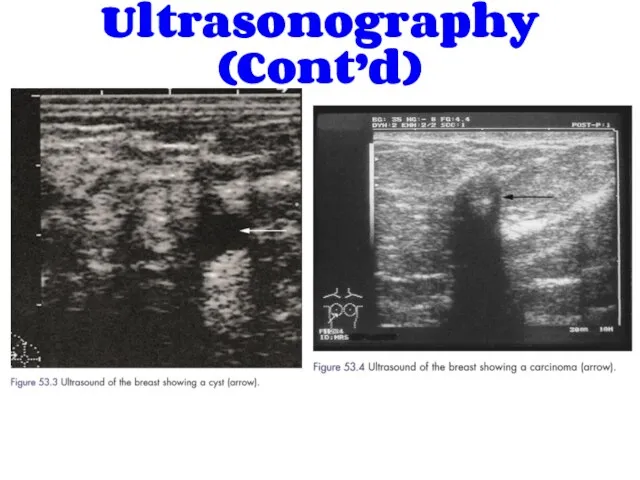
- 87. Ultrasonography (Cont’d)
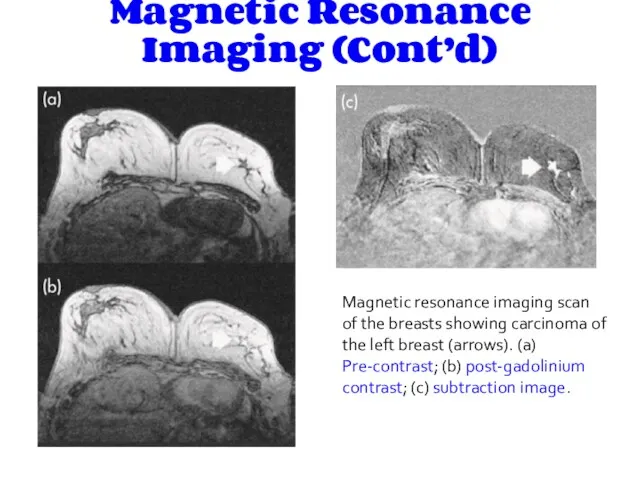
- 88. Magnetic Resonance Imaging Magnetic resonance imaging (MRI) is of increasing interest to breast surgeons in a
- 89. Magnetic Resonance Imaging (Cont’d) Magnetic resonance imaging scan of the breasts showing carcinoma of the left
- 90. History:
- 91. PRESENTATION OF BREAST DISEASE Breast disease presents in three main ways: lump, which may or may
- 92. Breast lump (Mass) When did the patient first notice it & how? Site Painful or not
- 93. Breast pain Duration SOCRATES Relation with periods Nipple discharge Discoloration and hotness of skin Fever, fatigue,
- 94. Nipple Discharge Site (nipple itself or adjacent area) Episodic or continuous Color Viscosity Passive or induced
- 95. Skin changes Skin dimple Eczema Indrawing of the skin Ulceration Discoloration Redness and hotness Overall swelling
- 96. Nipple changes Is it retracted or destroyed Uni/bilateral Can it be everted easily
- 97. Gynecological symptoms : Last menstrual cycle duration menarche menopause Any changes: Increased blood, clots or irregularity
- 98. Past History (e.g breast cyst) Drug History (e.g oral contraceptives, hormone replacement therapy) Family History (
- 99. Physical Examination:
- 100. Position Inspection Palpation
- 101. position The patient must be fully undressed to the waist. sitting 45 degrees Patients sometimes say
- 102. Inspection Stand or sit directly in front of the patient, inspect both breasts and look for
- 103. 4. Nipples & Areolae: Depression Destruction Discoloration Displacement Deviation Discharge
- 104. To check for accessory nipple: check the nipple line ( axilla-->groin), if the nipple is inverted
- 105. (Supraclavicular fossa) Ectopic breast tissue in the anterior axillary fold Visible LN in arm, axilla and
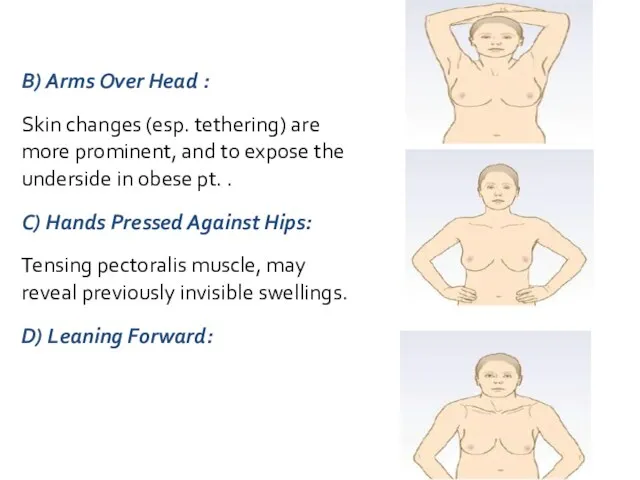
- 106. B) Arms Over Head : Skin changes (esp. tethering) are more prominent, and to expose the
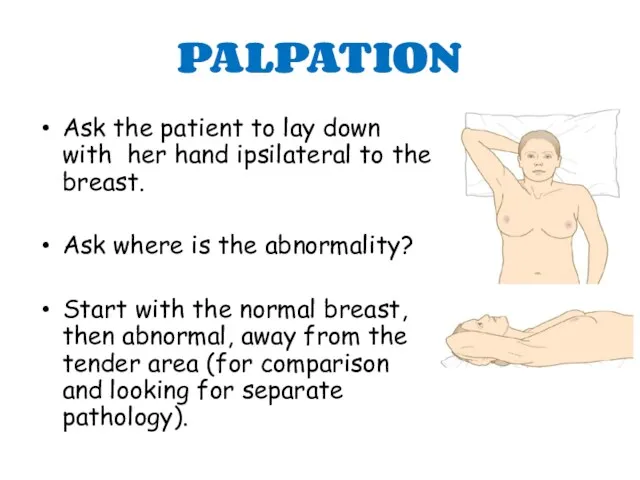
- 107. PALPATION Ask the patient to lay down with her hand ipsilateral to the breast. Ask where
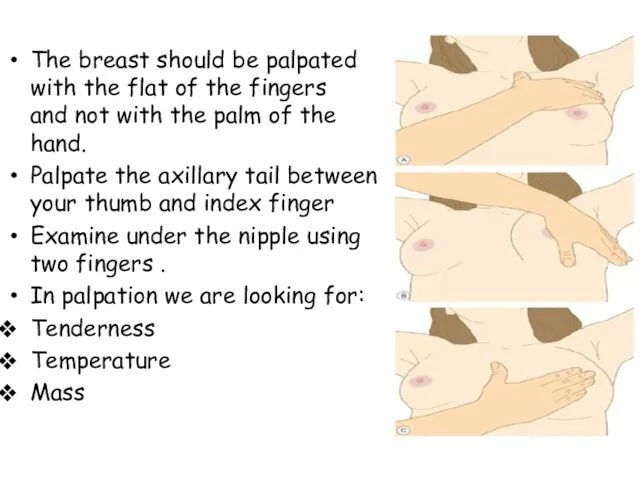
- 108. The breast should be palpated with the flat of the fingers and not with the palm
- 109. * If there is a lump we should analyze it : Lump Site Size Shape Edge
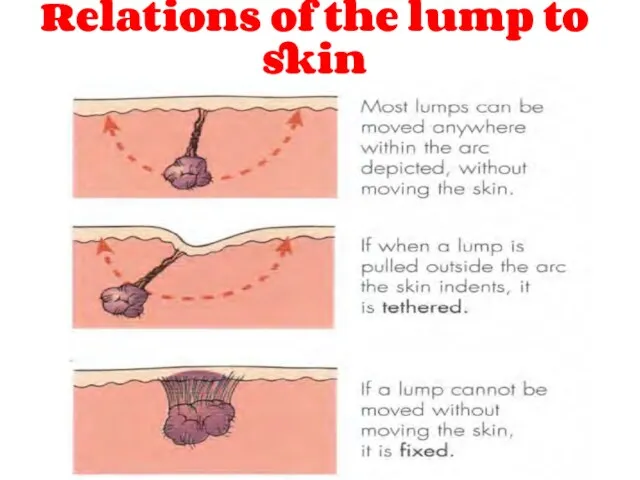
- 110. Relations of the lump to skin
- 112. Скачать презентацию







 Терминальное состояние: стадии, клиника, диагностика, критерии оценки тяжести состояния больного
Терминальное состояние: стадии, клиника, диагностика, критерии оценки тяжести состояния больного Абдомінальний ішемічний синдром. Тема 05
Абдомінальний ішемічний синдром. Тема 05 Нутритивная поддержка в хирургии. Обзор современных клинических рекомендаций
Нутритивная поддержка в хирургии. Обзор современных клинических рекомендаций История изучения сердечно-сосудистой системы
История изучения сердечно-сосудистой системы Учение о биосфере. Ноосфера. (Лекция 18)
Учение о биосфере. Ноосфера. (Лекция 18) Клинические рекомендации пациенту с заболеванием мочеполовой системы. Тактика ведения пациента на уровне ПМСП
Клинические рекомендации пациенту с заболеванием мочеполовой системы. Тактика ведения пациента на уровне ПМСП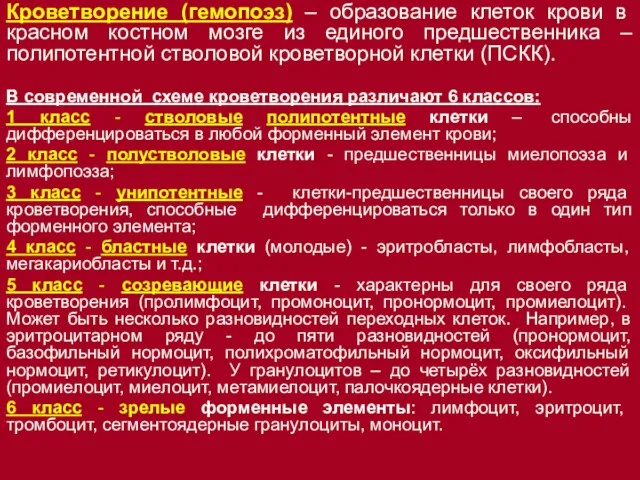 Кроветворение (гемопоэз) – образование клеток крови в красном костном мозге
Кроветворение (гемопоэз) – образование клеток крови в красном костном мозге Обмороження та його періоди. Класифікація обмороження. Домедична допомога при обмороженнях
Обмороження та його періоди. Класифікація обмороження. Домедична допомога при обмороженнях ХТА пестицидов ФОС
ХТА пестицидов ФОС Атомная медицина и медицинская физика
Атомная медицина и медицинская физика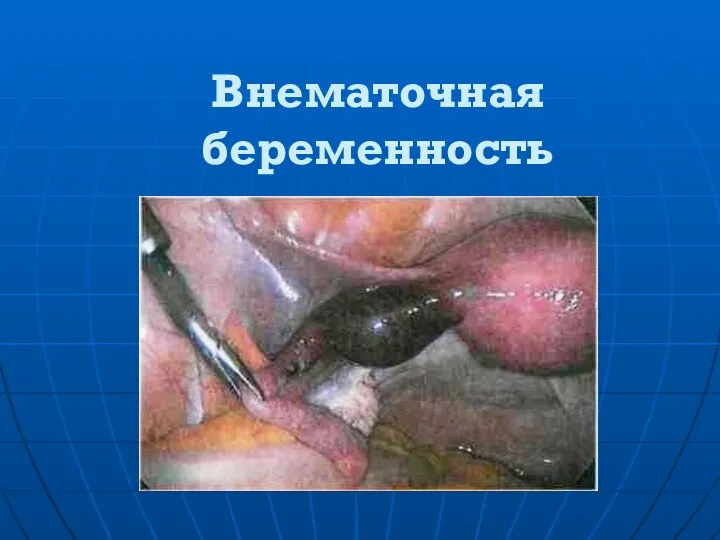 Внематочная беременность
Внематочная беременность История сестринского дела
История сестринского дела Гирсутизм. Вирилизация. Гипертрихоз
Гирсутизм. Вирилизация. Гипертрихоз Коронавирус 2019, профилактика, санитарно-просветительская работа
Коронавирус 2019, профилактика, санитарно-просветительская работа Қарыншалар гипертрофиясының ЭКГ белгілері
Қарыншалар гипертрофиясының ЭКГ белгілері Багатоплідна вагітність
Багатоплідна вагітність Фізіологічні основи оздоровчої фізичної культури
Фізіологічні основи оздоровчої фізичної культури Больные с заболеваниями крови и органов кроветворения
Больные с заболеваниями крови и органов кроветворения Возрастные особенности строения уха
Возрастные особенности строения уха Раны. Классификация ран. Лечение чистой раны
Раны. Классификация ран. Лечение чистой раны Обмен нуклеотидов. Матричные биосинтезы
Обмен нуклеотидов. Матричные биосинтезы Переломы скуловых костей и дуг
Переломы скуловых костей и дуг Бейспецификалық жаралы колит
Бейспецификалық жаралы колит Травма позвоночника
Травма позвоночника Фенотипические особенности наследственных синдромов рака молочной железы и яичников среди татарского этноса
Фенотипические особенности наследственных синдромов рака молочной железы и яичников среди татарского этноса Профессиональное здоровье педагогов по результатам социологического опроса
Профессиональное здоровье педагогов по результатам социологического опроса בן 45עם כאבי פרקים סימטרים עם נפיחויות ,קשיון בוקר מעל שעה חודשיים
בן 45עם כאבי פרקים סימטרים עם נפיחויות ,קשיון בוקר מעל שעה חודשיים Демография. Медицинская демография
Демография. Медицинская демография