Содержание
- 2. Definitions of shock Severe hemodynamic impairment which causes hypoperfusion of vital organs Clinical syndrome that results
- 3. Signs of hypoperfusion - clouded sensorium - cool extremities - oliguria - acidosis
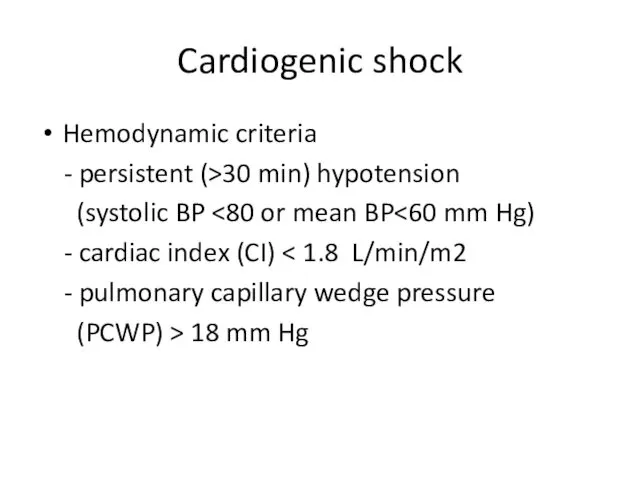
- 4. Cardiogenic shock Hemodynamic criteria - persistent (>30 min) hypotension (systolic BP - cardiac index (CI) -
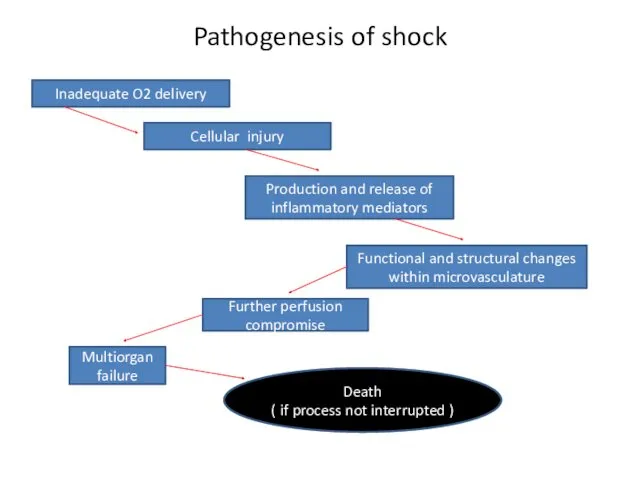
- 5. Pathogenesis of shock Inadequate O2 delivery Cellular injury Production and release of inflammatory mediators Functional and
- 6. Types of shock Hypovolemic Traumatic Cardiogenic Septic Neurogenic Hypoadrenal
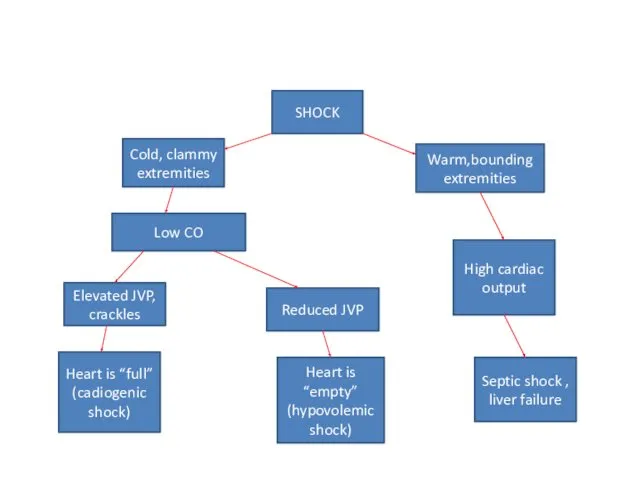
- 7. SHOCK Cold, clammy extremities Warm,bounding extremities High cardiac output Septic shock , liver failure Elevated JVP,
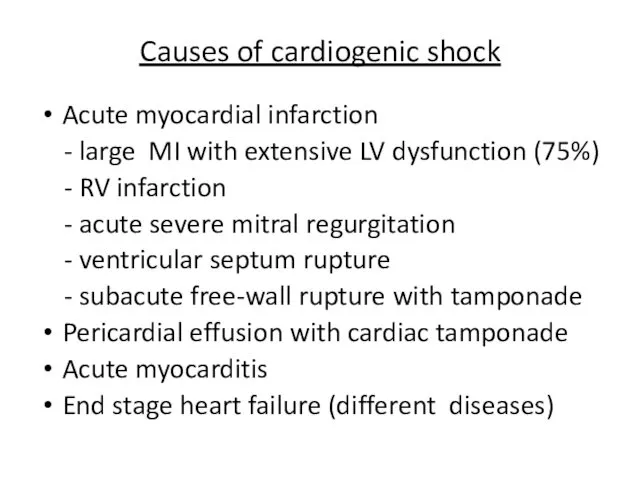
- 8. Causes of cardiogenic shock Acute myocardial infarction - large MI with extensive LV dysfunction (75%) -
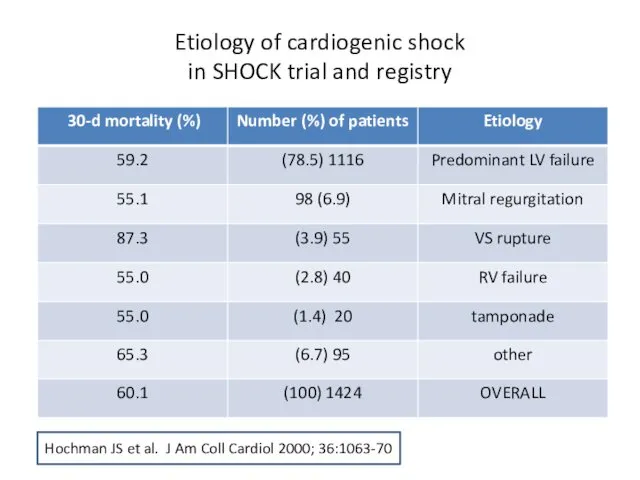
- 9. Etiology of cardiogenic shock in SHOCK trial and registry Hochman JS et al. J Am Coll
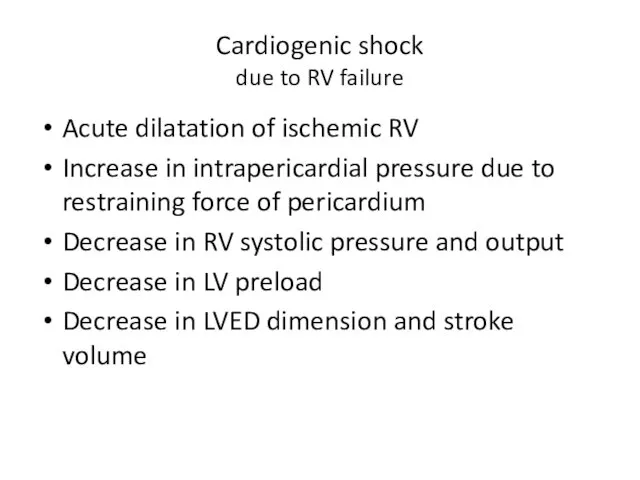
- 10. Cardiogenic shock due to RV failure Acute dilatation of ischemic RV Increase in intrapericardial pressure due
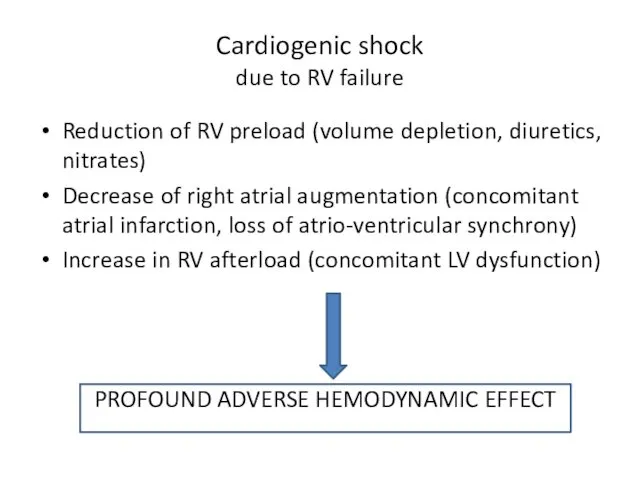
- 11. Cardiogenic shock due to RV failure Reduction of RV preload (volume depletion, diuretics, nitrates) Decrease of
- 12. Hemodynamic monitoring
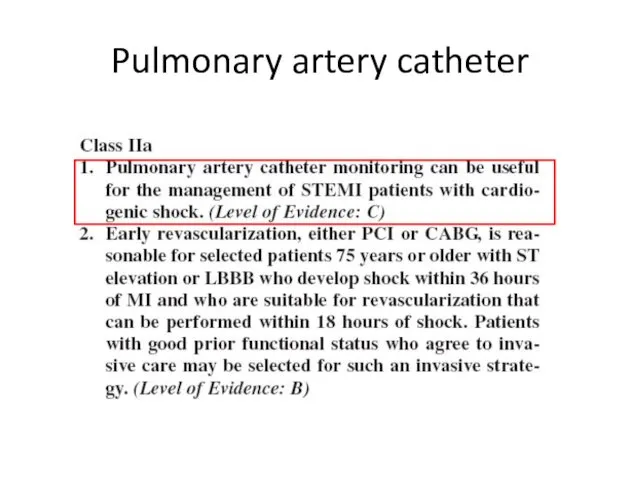
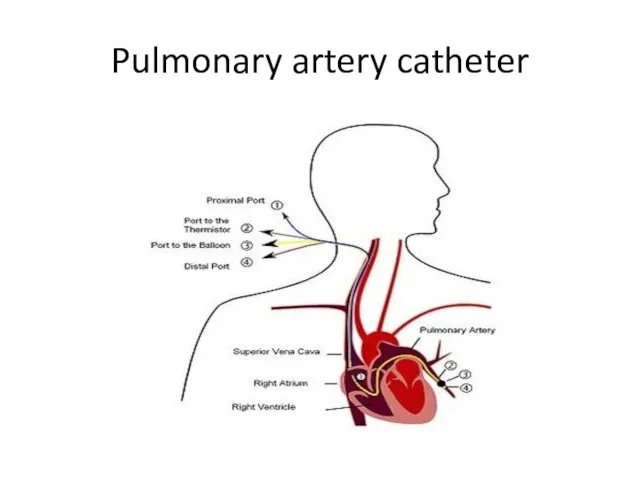
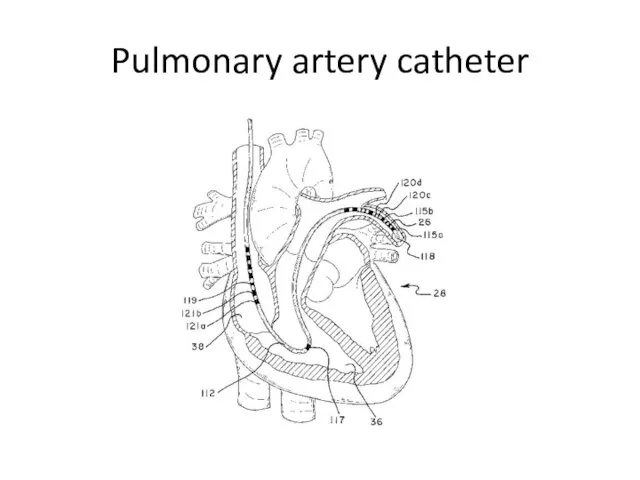
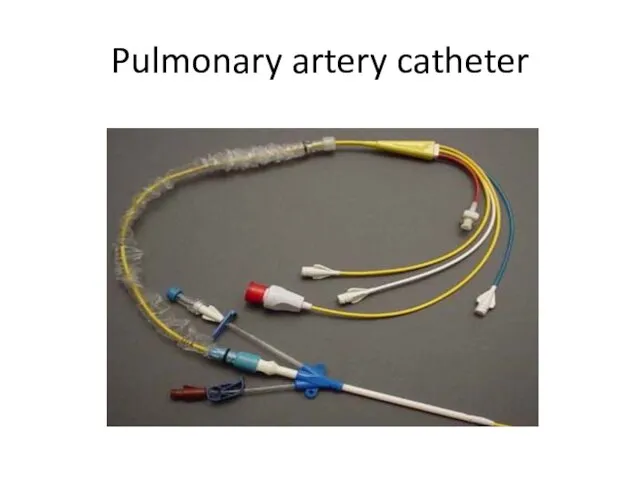
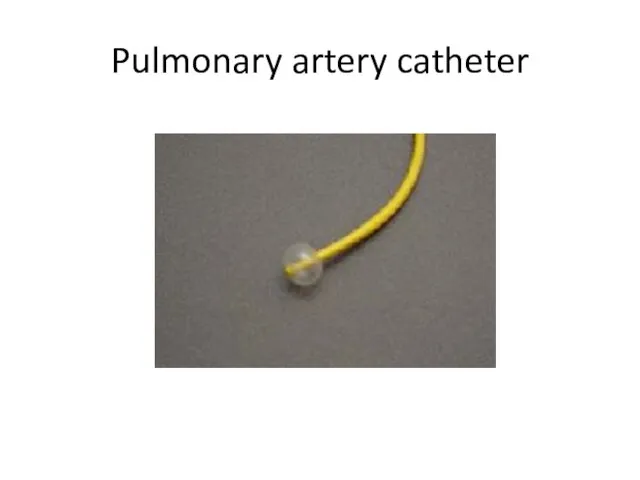
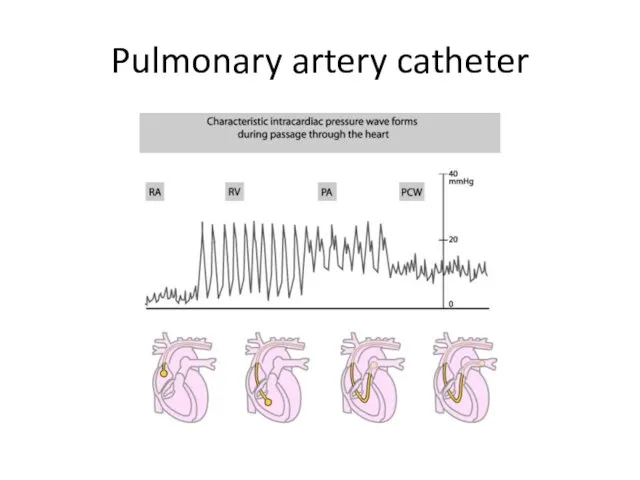
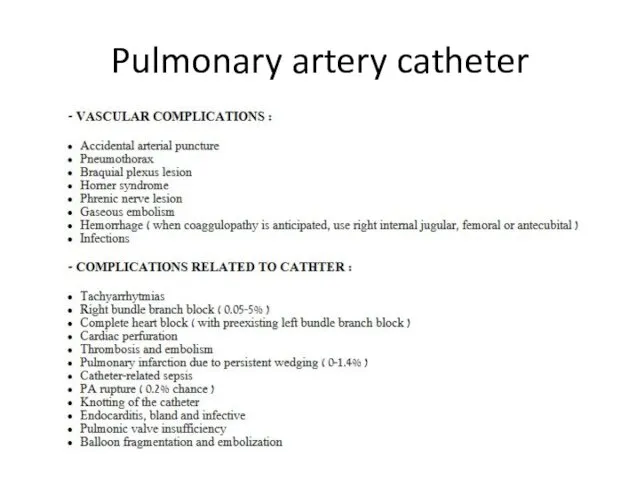
- 13. Pulmonary artery catheter
- 14. Pulmonary artery catheter
- 15. Pulmonary artery catheter
- 16. Pulmonary artery catheter
- 17. Pulmonary artery catheter
- 18. Pulmonary artery catheter
- 19. Pulmonary artery catheter
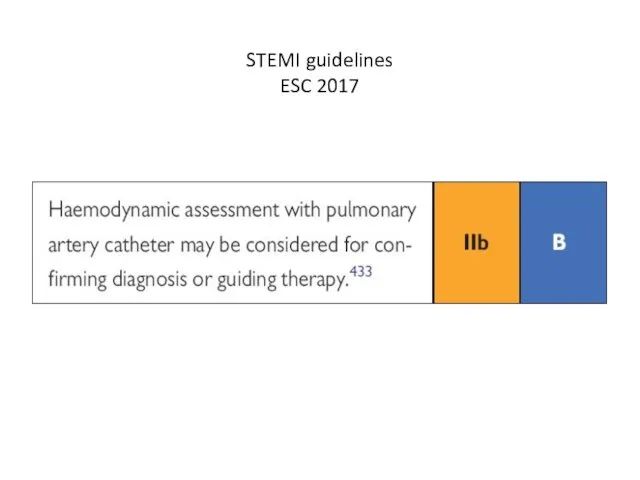
- 20. STEMI guidelines ESC 2017
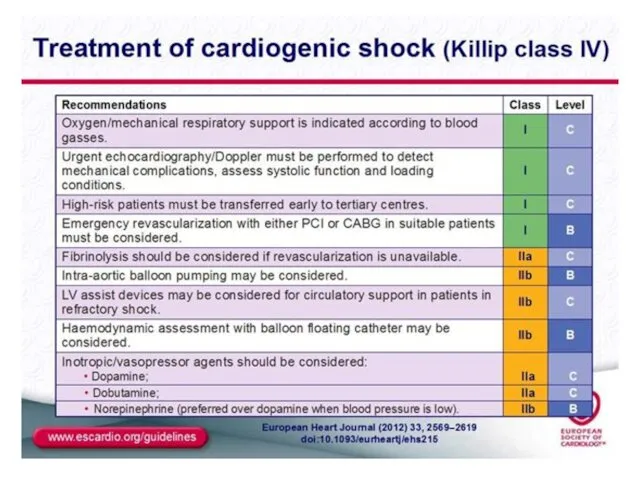
- 21. Treatment of cardiogenic shock
- 22. Inotropes IABP Early revascularization (PCI or CABG) Surgery for mechanical complications Pericardiocentesis (if tamponade is a
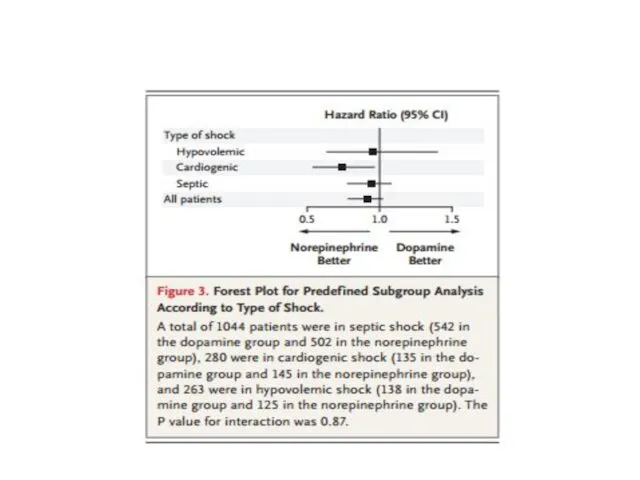
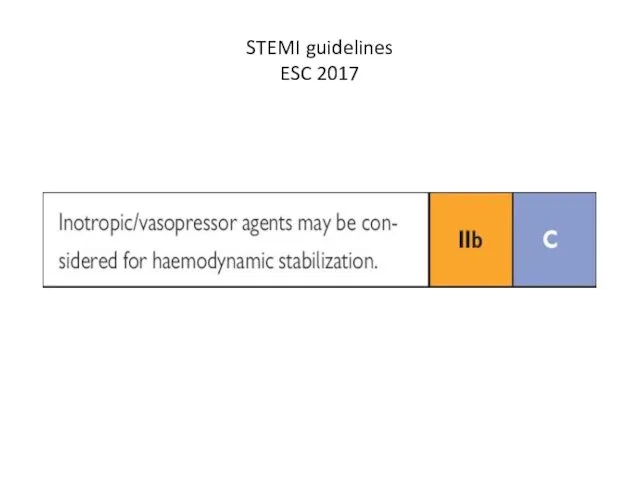
- 27. STEMI guidelines ESC 2017
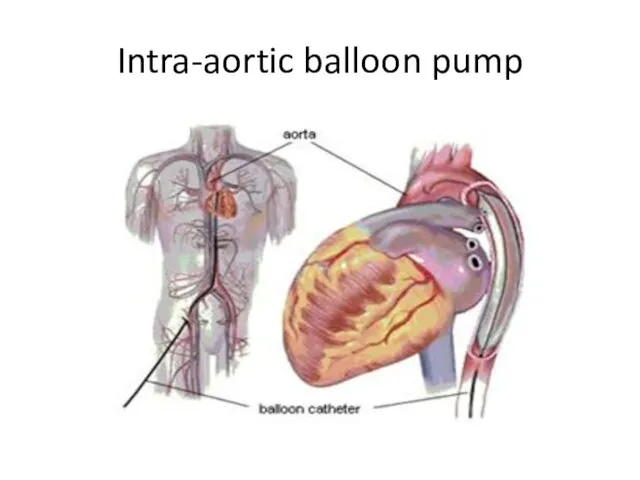
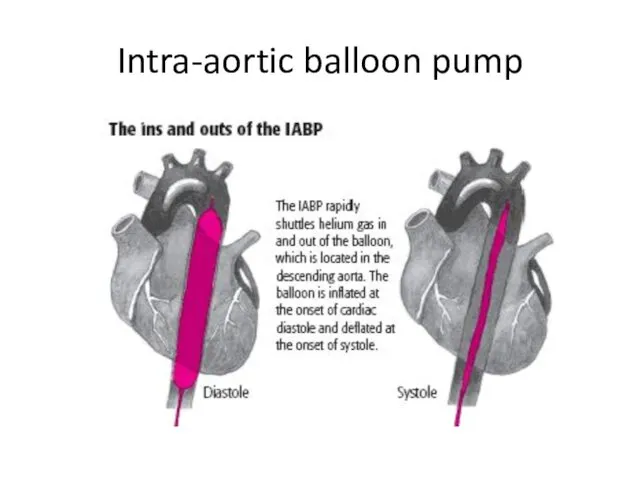
- 28. Intra-aortic balloon pump (IABP)
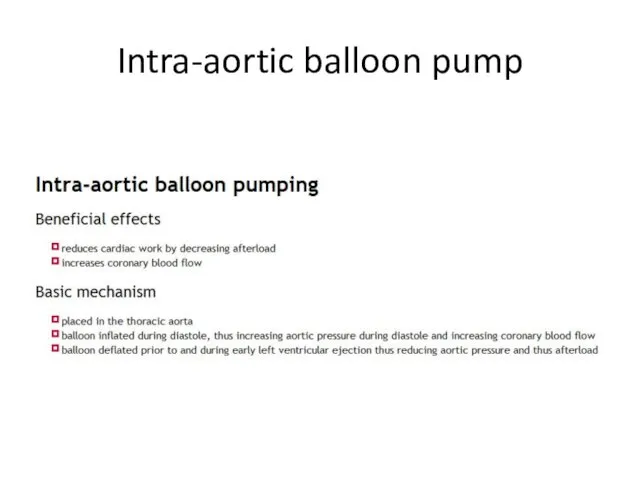
- 29. Intra-aortic balloon pump
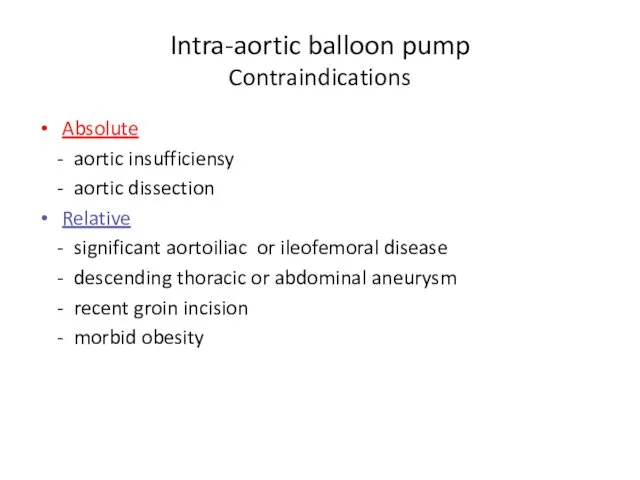
- 30. Intra-aortic balloon pump Contraindications Absolute - aortic insufficiensy - aortic dissection Relative - significant aortoiliac or
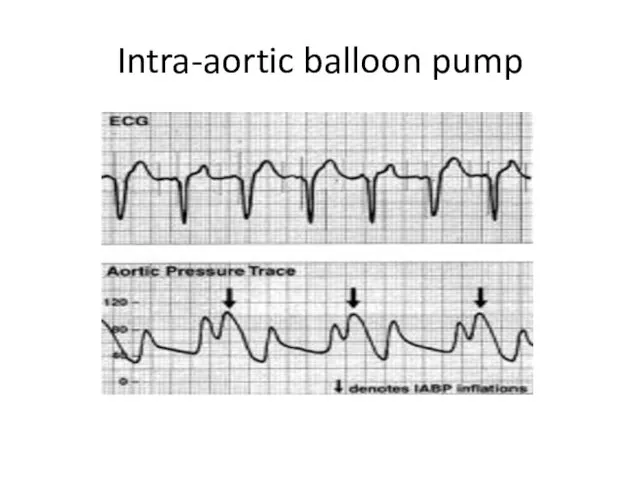
- 31. Intra-aortic balloon pump
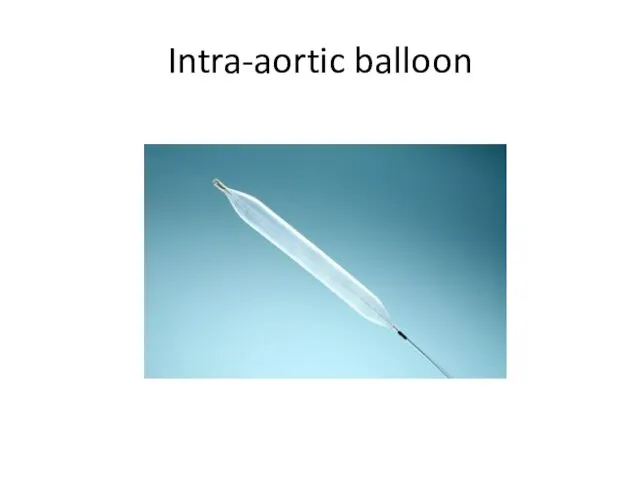
- 32. Intra-aortic balloon
- 33. Intra-aortic balloon pump
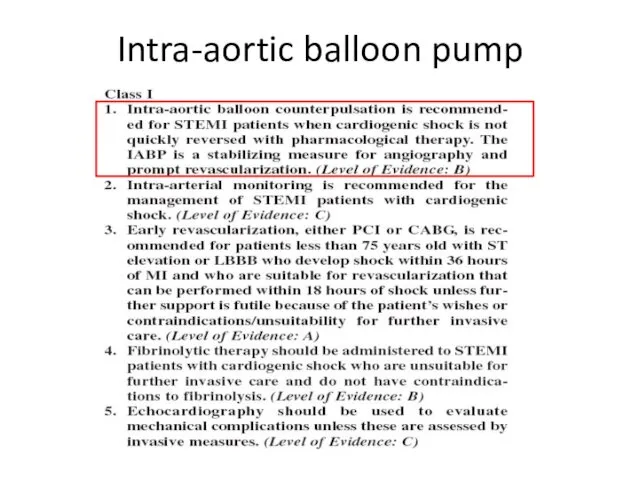
- 34. Intra-aortic balloon pump
- 35. Intra-aortic balloon pump
- 36. Intra-aortic balloon pump
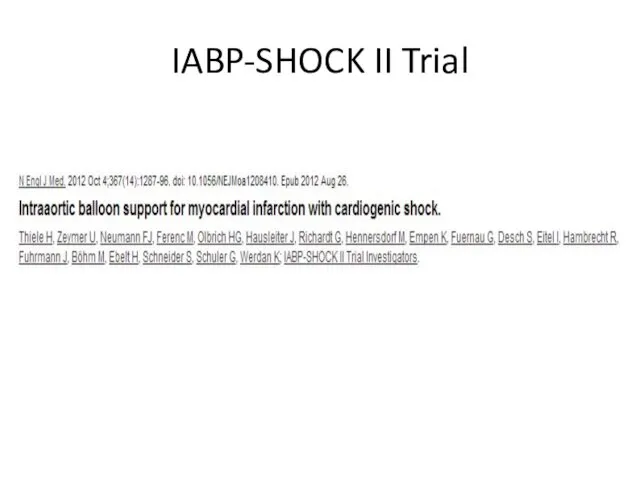
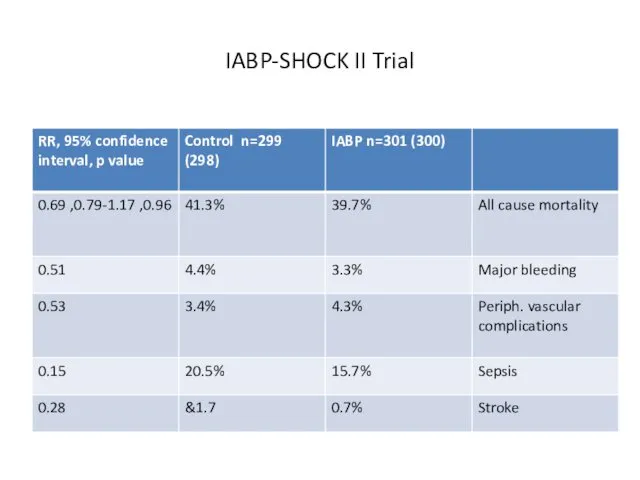
- 37. IABP-SHOCK II Trial
- 38. IABP-SHOCK II Trial
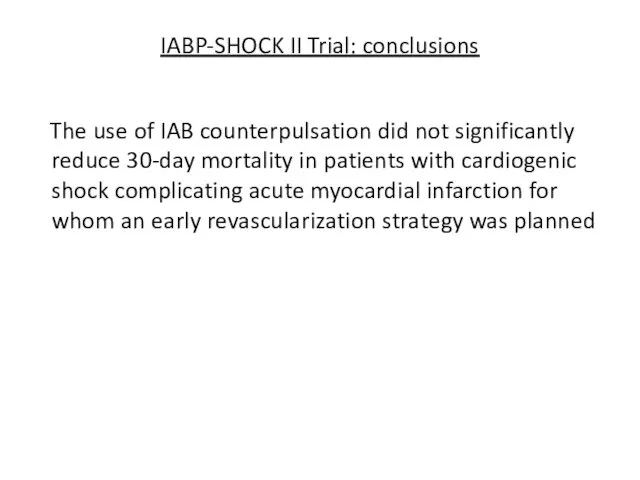
- 39. IABP-SHOCK II Trial: conclusions The use of IAB counterpulsation did not significantly reduce 30-day mortality in
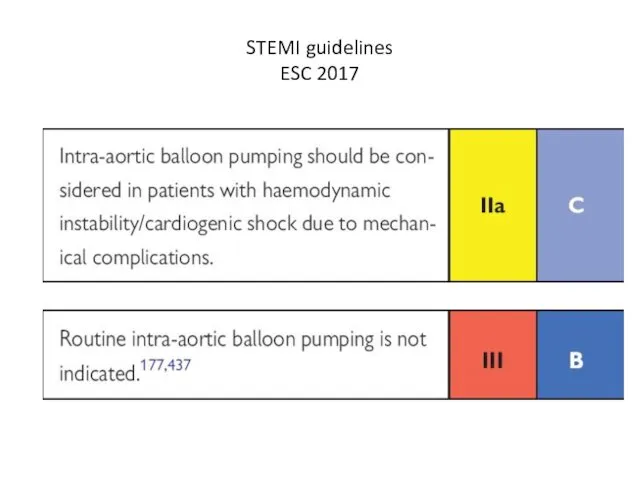
- 40. STEMI guidelines ESC 2017
- 41. Early revascularization
- 42. SHOCK trial Early revascularization in acute myocardial infarction complicated by cardiogenic shock J. Hochman et al
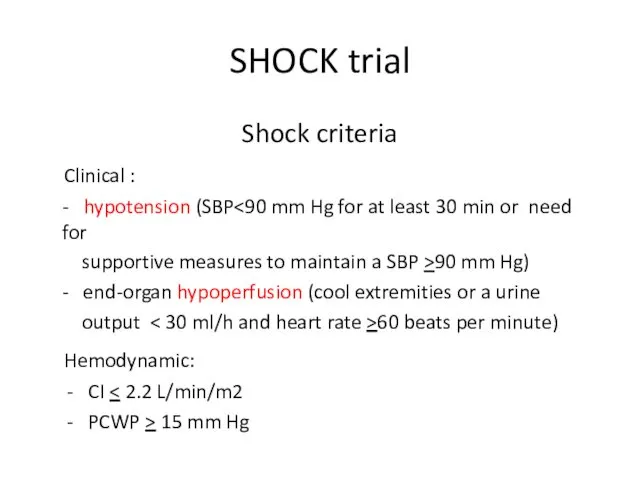
- 43. SHOCK trial Shock criteria Clinical : - hypotension (SBP supportive measures to maintain a SBP >90
- 44. SHOCK trial Timing - onset of shock within 36 h of infarction - randomization as soon
- 45. SHOCK trial Exclusion criteria - severe systemic illness - mechanical or other cause of shock -
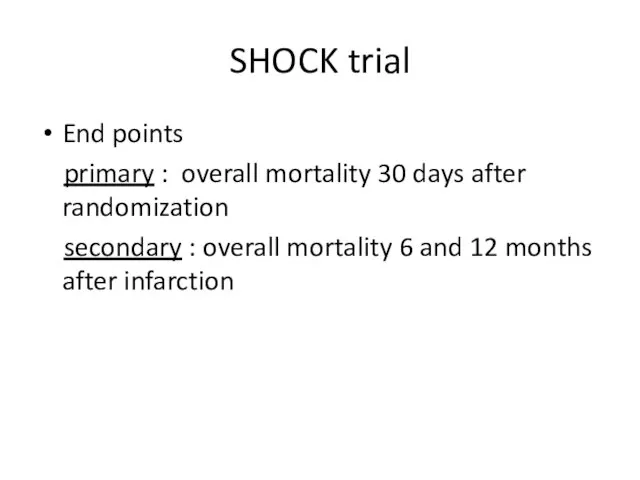
- 46. SHOCK trial End points primary : overall mortality 30 days after randomization secondary : overall mortality
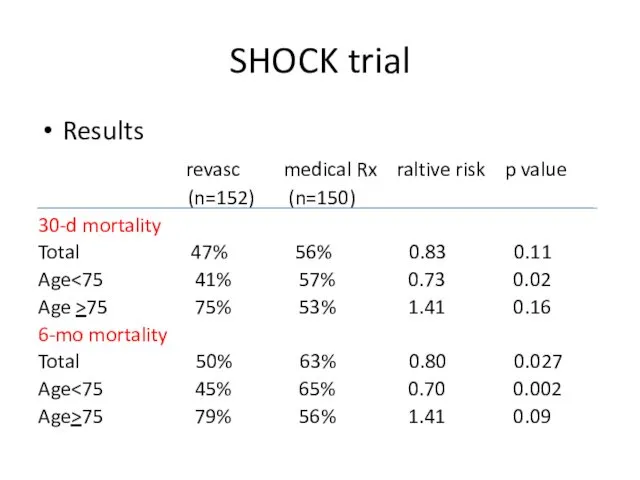
- 47. SHOCK trial Results revasc medical Rx raltive risk p value (n=152) (n=150) 30-d mortality Total 47%
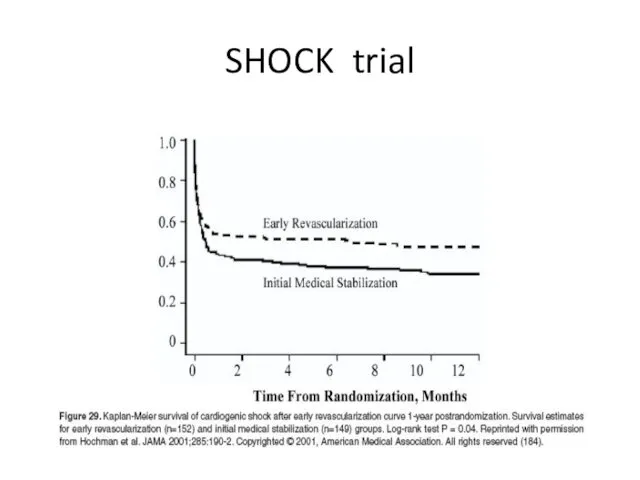
- 48. SHOCK trial
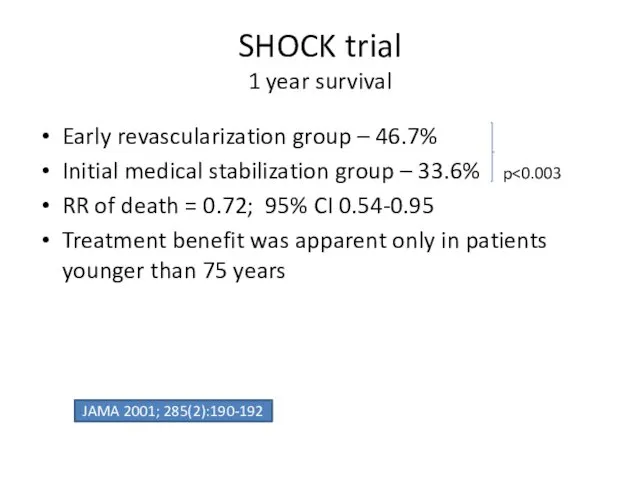
- 49. SHOCK trial 1 year survival Early revascularization group – 46.7% Initial medical stabilization group – 33.6%
- 50. SHOCK trial
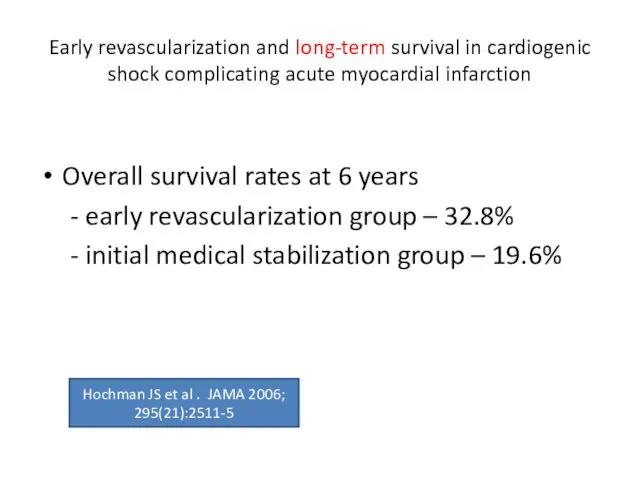
- 51. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction Overall survival rates at
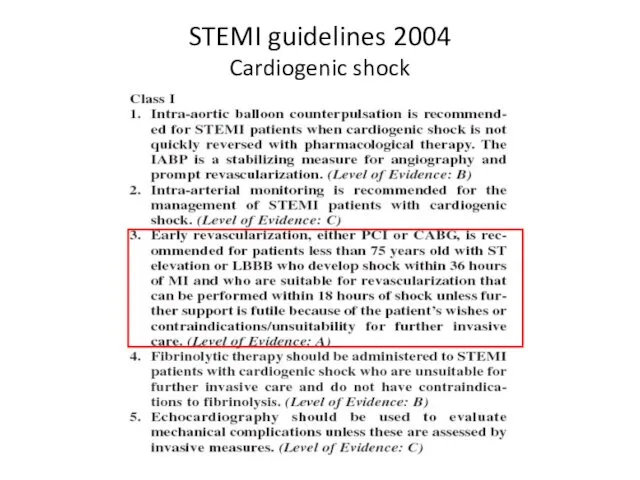
- 52. STEMI guidelines 2004 Cardiogenic shock
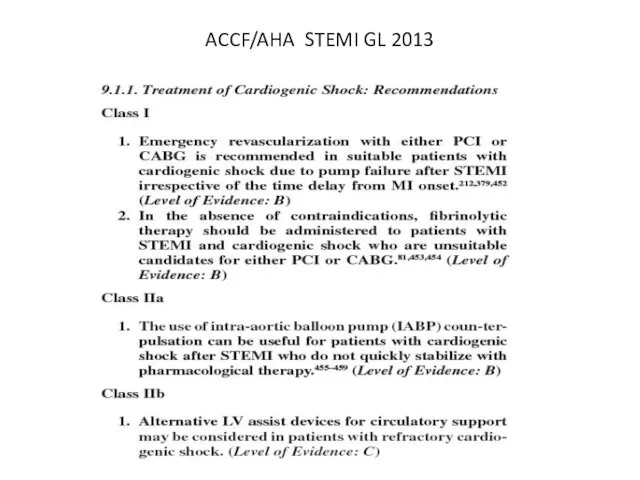
- 53. ACCF/AHA STEMI GL 2013
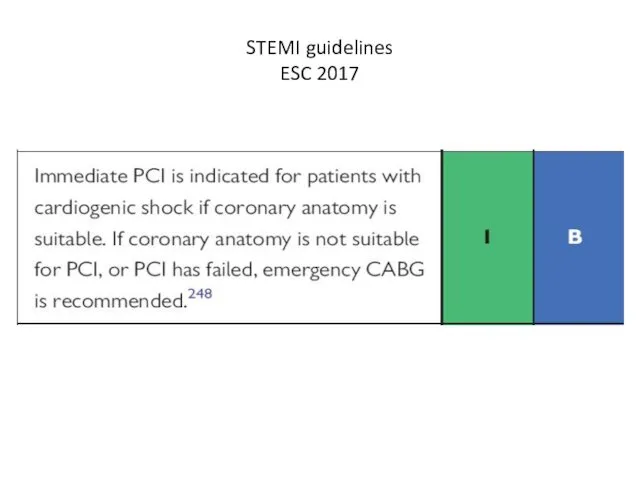
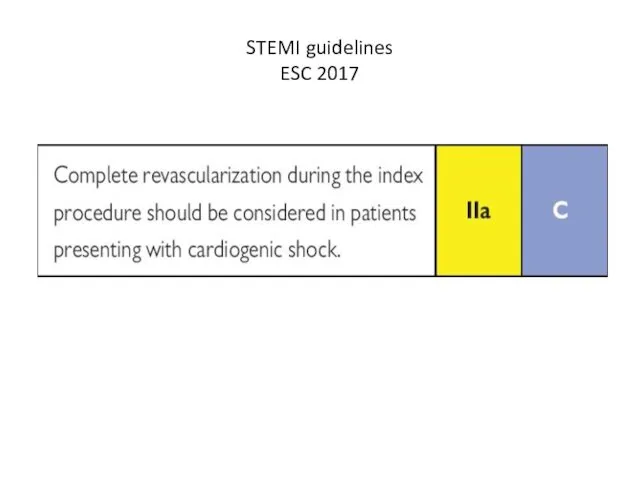
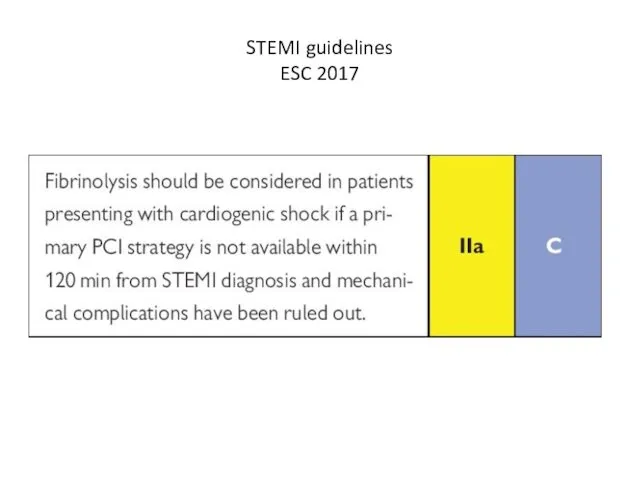
- 54. STEMI guidelines ESC 2017
- 55. STEMI guidelines ESC 2017
- 56. STEMI guidelines ESC 2017
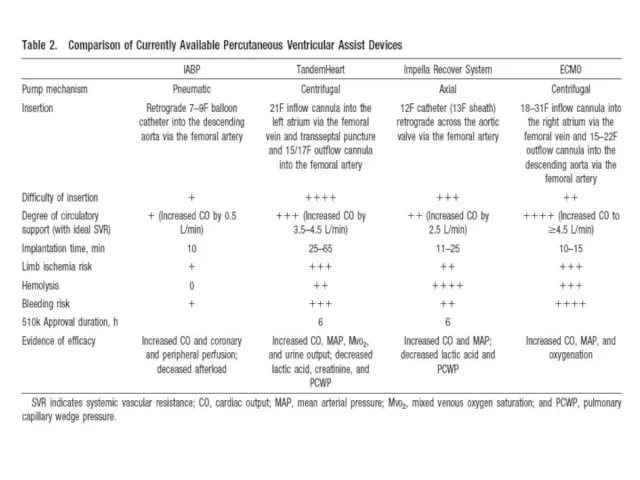
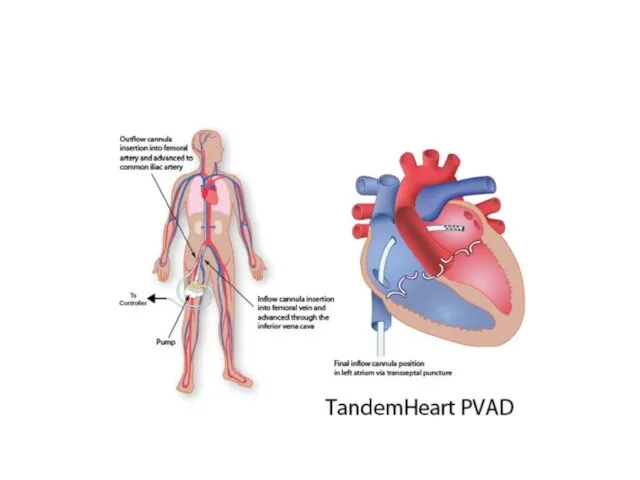
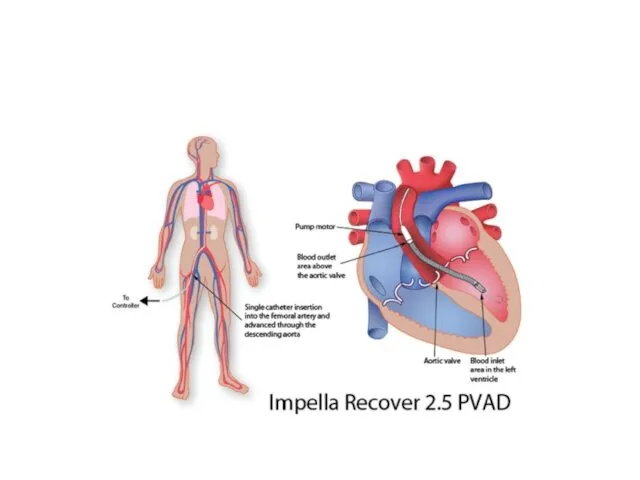
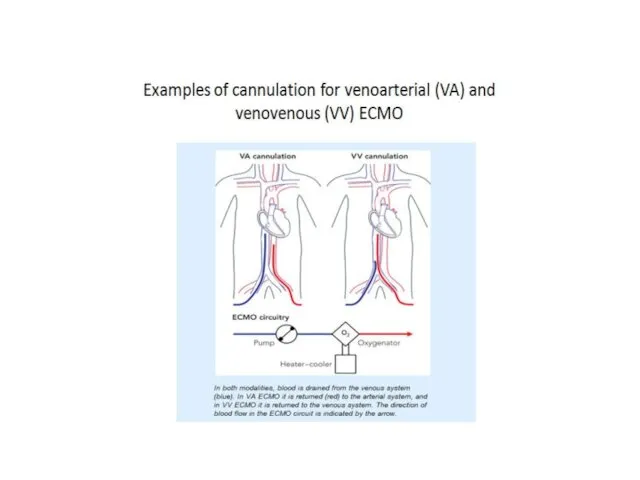
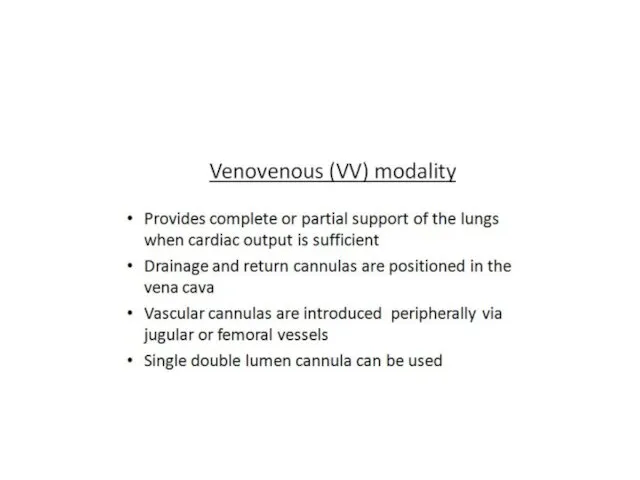
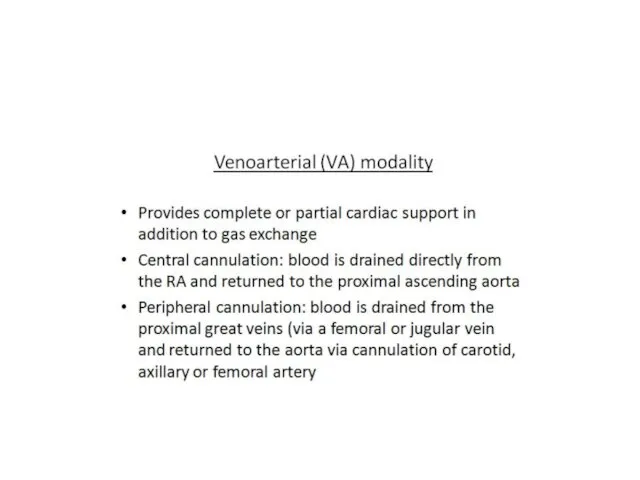
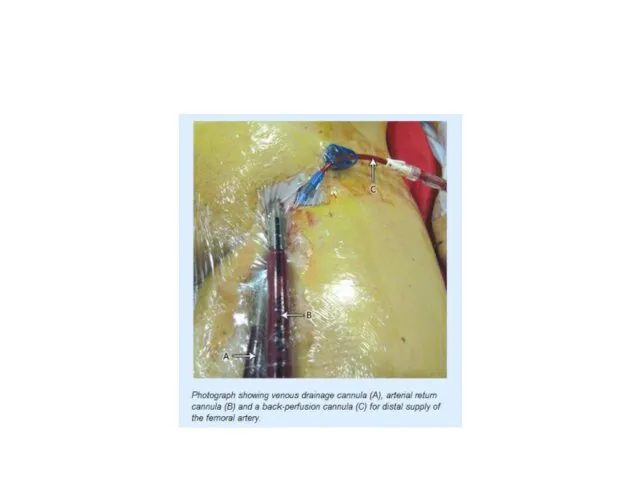
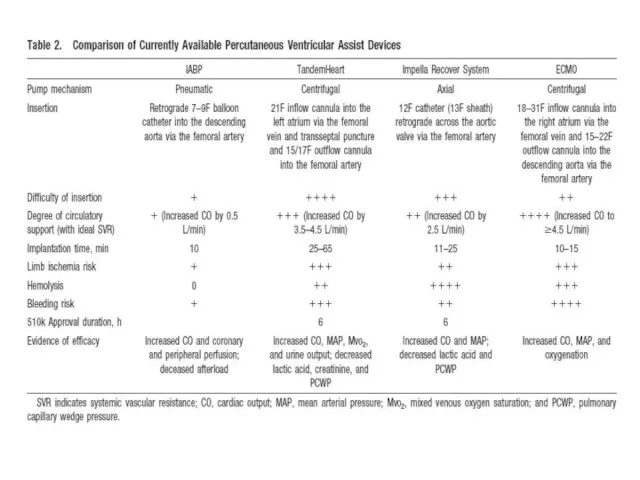
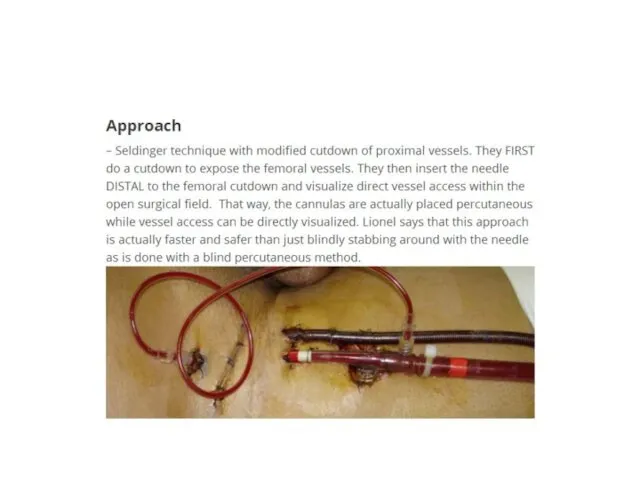
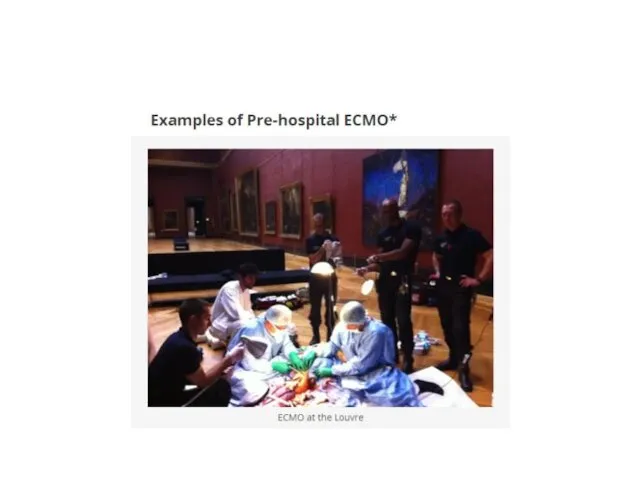
- 57. Percutaneous ventricular assist devices
- 69. STEMI guidelines ESC 2017
- 70. Thank you for attention
- 71. Back up slides
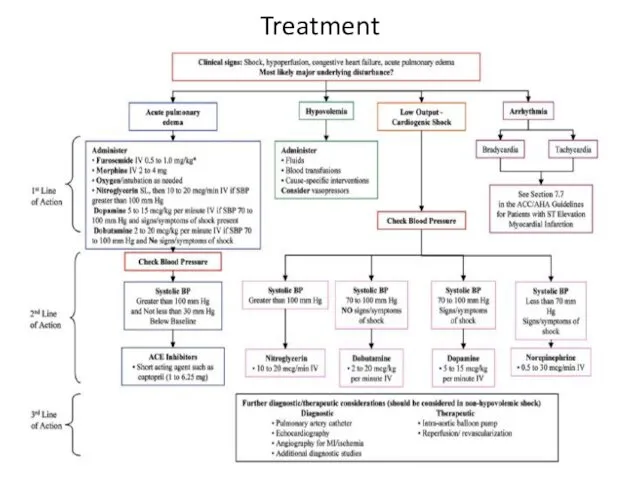
- 73. Treatment
- 76. Скачать презентацию


 Методичні особливості лікувального масажу при захворюваннях серцево-судинної системи
Методичні особливості лікувального масажу при захворюваннях серцево-судинної системи Гормональная деятельность эпифиза
Гормональная деятельность эпифиза Болезнь Паркинсона
Болезнь Паркинсона Микроскоп және оның шығу тарихы. Микроскоптың түрлері
Микроскоп және оның шығу тарихы. Микроскоптың түрлері Миопия. Группы риска. Этиология и диагностика миопии
Миопия. Группы риска. Этиология и диагностика миопии Сестринский процесс при заболеваниях органов дыхания. Лекция 7,8
Сестринский процесс при заболеваниях органов дыхания. Лекция 7,8 Тактика ВОП при подозрении на особо опасной инфекции(ООИ). Профилактические мероприятия в очаге
Тактика ВОП при подозрении на особо опасной инфекции(ООИ). Профилактические мероприятия в очаге Менингококковая инфекция
Менингококковая инфекция Хирургиялық құралдар. Микрохирургия ұғымы. Тіндерді қосу және ажырату ережелері мен әдістері
Хирургиялық құралдар. Микрохирургия ұғымы. Тіндерді қосу және ажырату ережелері мен әдістері Дезинфекция медицинских изделий
Дезинфекция медицинских изделий Возрастная анатомия, физиология и гигиенаПредмет и содержание курса возрастной анатомии, физиологии и гигиены
Возрастная анатомия, физиология и гигиенаПредмет и содержание курса возрастной анатомии, физиологии и гигиены Спинной мозг
Спинной мозг Острые респираторные заболевания. Грипп
Острые респираторные заболевания. Грипп Лекарственные препараты при беременности, возможный вред при их применении
Лекарственные препараты при беременности, возможный вред при их применении Aberration of normal development and involution (andi) of thebreast
Aberration of normal development and involution (andi) of thebreast ООО СМО Спасение. Добровольное медицинское страхование
ООО СМО Спасение. Добровольное медицинское страхование Безопасность и биоэтика в биотехнологии. Основы науки о стволовых клетках. (Лекция 8)
Безопасность и биоэтика в биотехнологии. Основы науки о стволовых клетках. (Лекция 8) Психологічні основи спілкування. Особливості взаємовідносин медичних працівників і хворих
Психологічні основи спілкування. Особливості взаємовідносин медичних працівників і хворих Лучевая терапия опухолей
Лучевая терапия опухолей Аномалии и деформации зубов и зубных рядов
Аномалии и деформации зубов и зубных рядов Национальный проект Здравоохранение. Финансирование, цели и задачи
Национальный проект Здравоохранение. Финансирование, цели и задачи Рак мочевого пузыря
Рак мочевого пузыря Правила формулировки диагноза
Правила формулировки диагноза Умирание, смерть и трупные изменения
Умирание, смерть и трупные изменения Иммунопрофилактика. Общие вопросы
Иммунопрофилактика. Общие вопросы Венерические заболевания
Венерические заболевания Алкоголизм
Алкоголизм Симптомы, проявления, диагностика и лечение васкулита
Симптомы, проявления, диагностика и лечение васкулита