Содержание
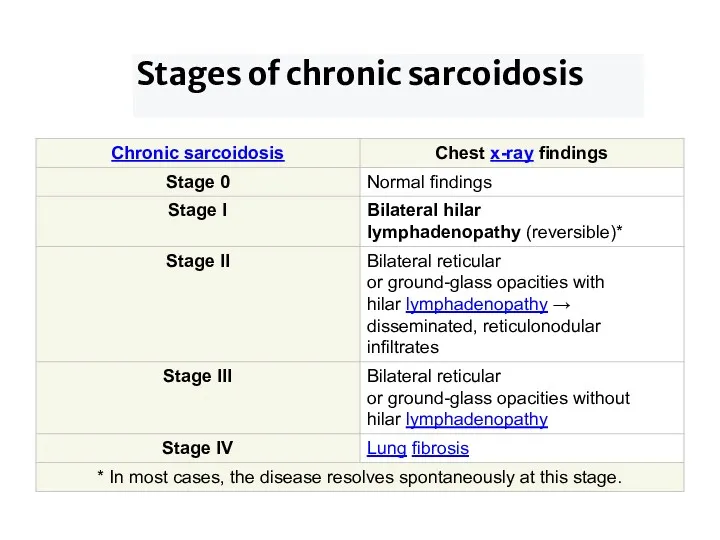
- 2. Stages of chronic sarcoidosis
- 3. Etiology of Sarcoidosis 1. Genetics Studies have shown that a mutation of the gene BTNL2, as
- 4. Risk factors While anyone can develop sarcoidosis, factors that may increase your risk include: Age. Sarcoidosis
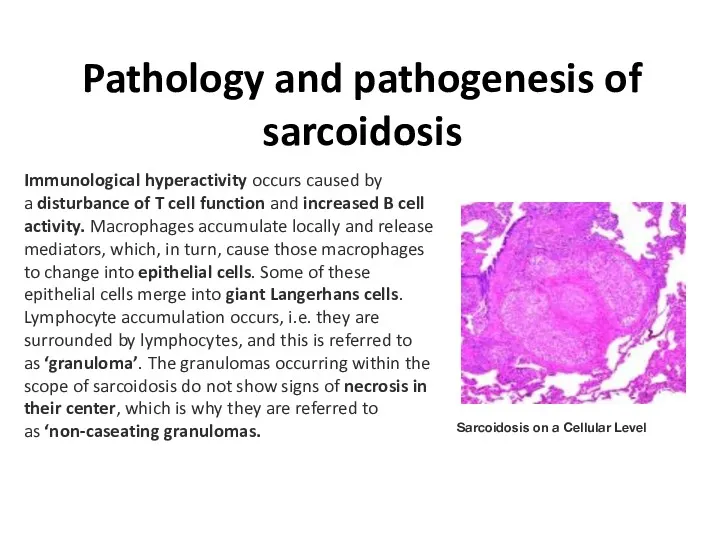
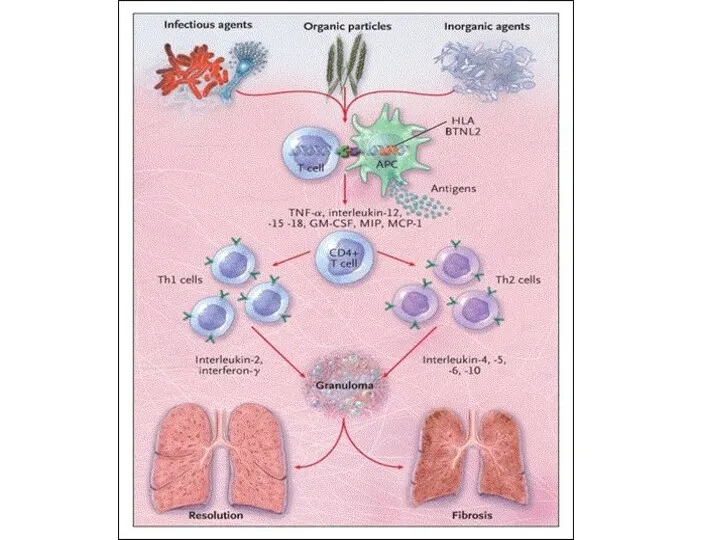
- 5. Pathology and pathogenesis of sarcoidosis Sarcoidosis on a Cellular Level Immunological hyperactivity occurs caused by a
- 6. . While this information may not be as relevant for the exam, one may come across
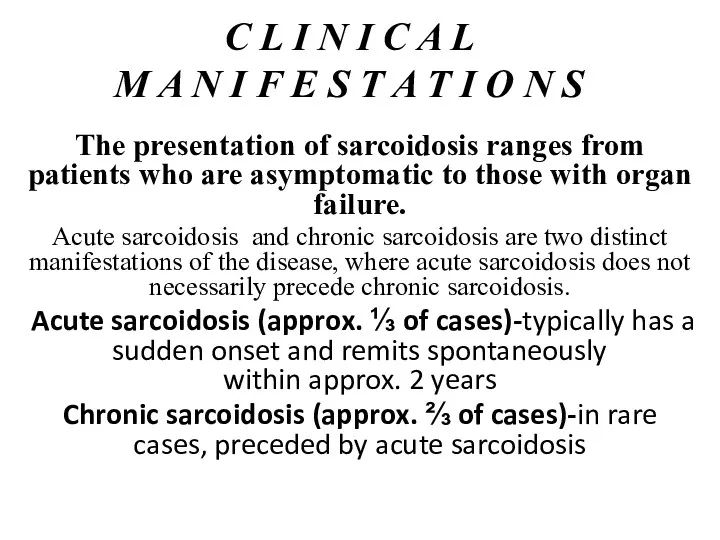
- 8. C L I N I C A L M A N I F E S T
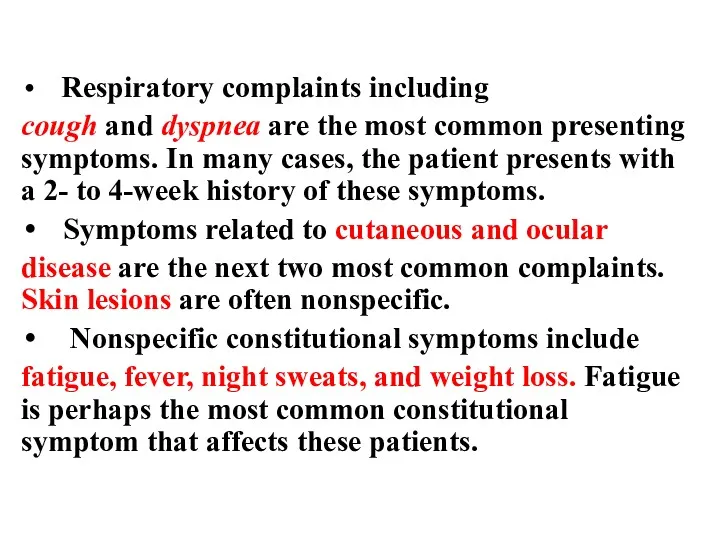
- 9. Respiratory complaints including cough and dyspnea are the most common presenting symptoms. In many cases, the
- 10. Lung symptoms Lung involvement occurs in >90 % of sarcoidosis patients and may cause lung problems,
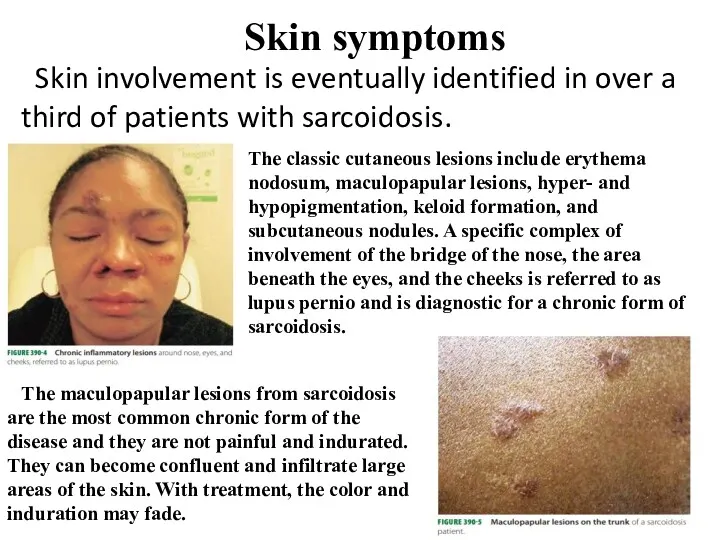
- 11. Skin symptoms Skin involvement is eventually identified in over a third of patients with sarcoidosis. The
- 12. Eye symptoms Blurred vision Eye pain Burning, itching or dry eyes Severe redness Sensitivity to light
- 13. Laboratory diagnostics In case of suspicion, the patient is prescribed a General and biochemical blood test,
- 14. General blood test: The changes observed in the General analysis of blood: *decrease in the concentration
- 15. Biochemical analysis Specific changes: *Angiotensin-converting enzyme. The level is significantly increased, the norm is from 17
- 16. Acute sarcoidosis: ↑ Inflammatory markers Findings typical for sarcoidosis are absent (e.g., ↑ ACE, ↑ IgG,
- 17. Instrumental investigations: Chest x-ray CT Biopsy Endoscopic examination: bronchoscopy and thoracoscopy Pulmonary function tests (to assess
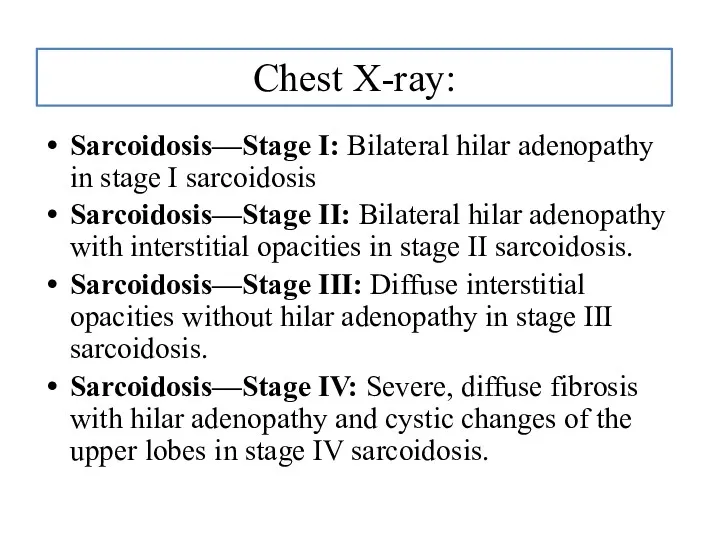
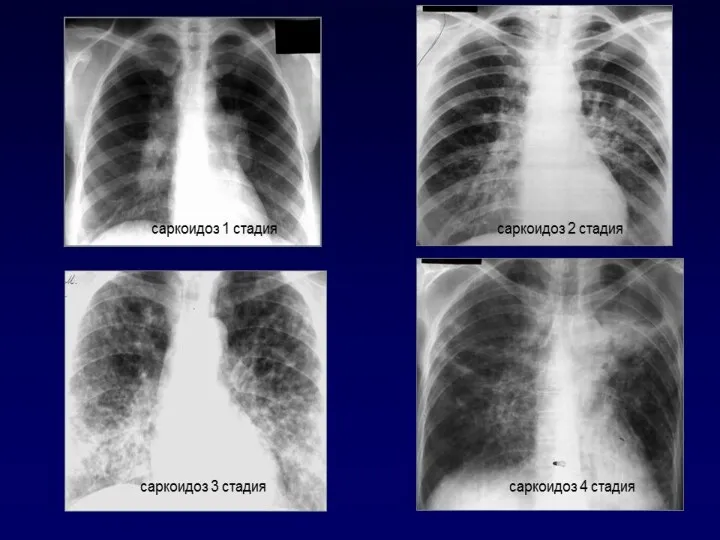
- 18. Chest X-ray: Sarcoidosis—Stage I: Bilateral hilar adenopathy in stage I sarcoidosis Sarcoidosis—Stage II: Bilateral hilar adenopathy
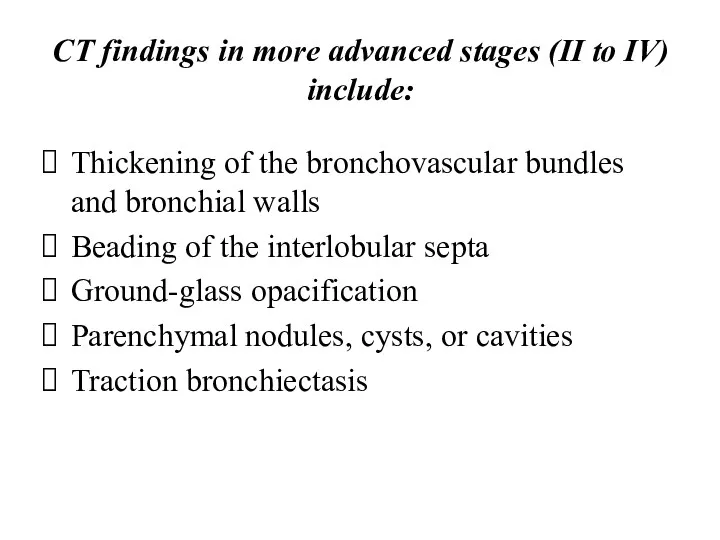
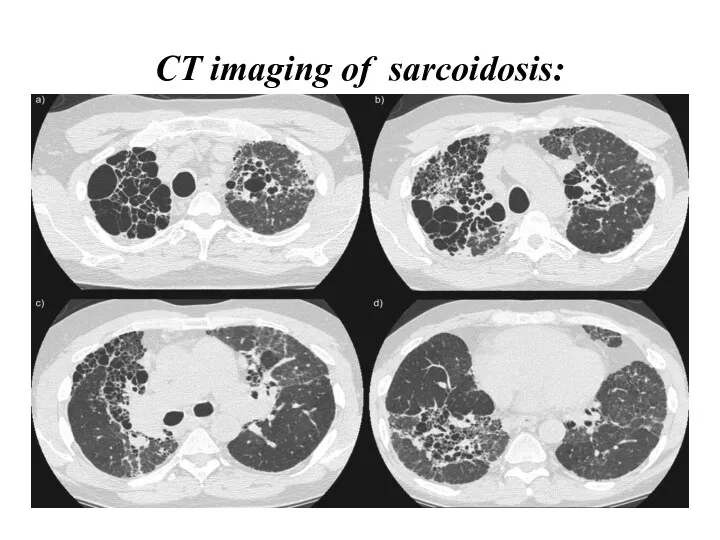
- 20. CT findings in more advanced stages (II to IV) include: Thickening of the bronchovascular bundles and
- 21. CT imaging of sarcoidosis:
- 22. When imaging suggests sarcoidosis, the diagnosis is confirmed by demonstration of noncaseating granulomas on biopsy and
- 23. Biopsy methods: Bronchoscopic: Transbronchial lung biopsy (PLL). Classical transbronchial needle biopsy of intrathoracic lymph nodes Endoscopic
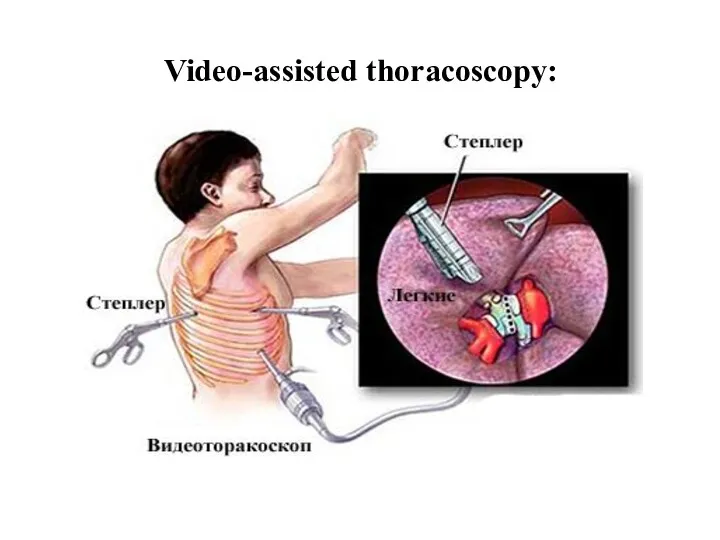
- 24. Video-assisted thoracoscopy:
- 25. Bronchoscopy: changes in the vessels of the bronchial mucosa (expansion) lumpy eruptions (sarcoid granulomas) in the
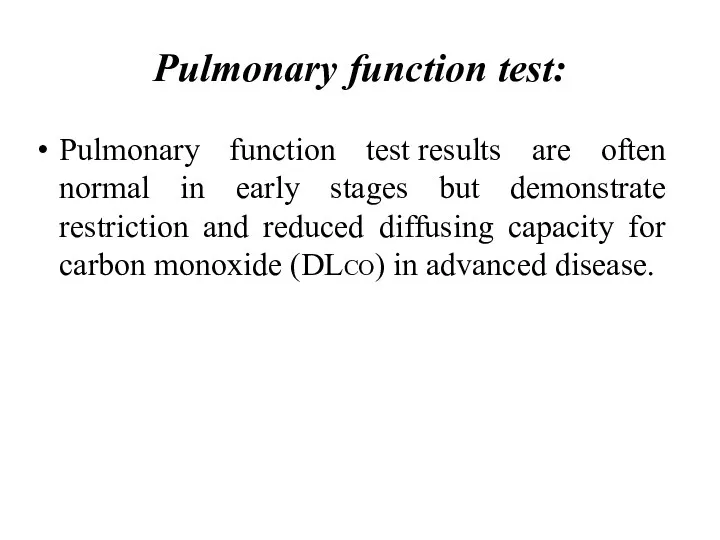
- 26. Pulmonary function test: Pulmonary function test results are often normal in early stages but demonstrate restriction
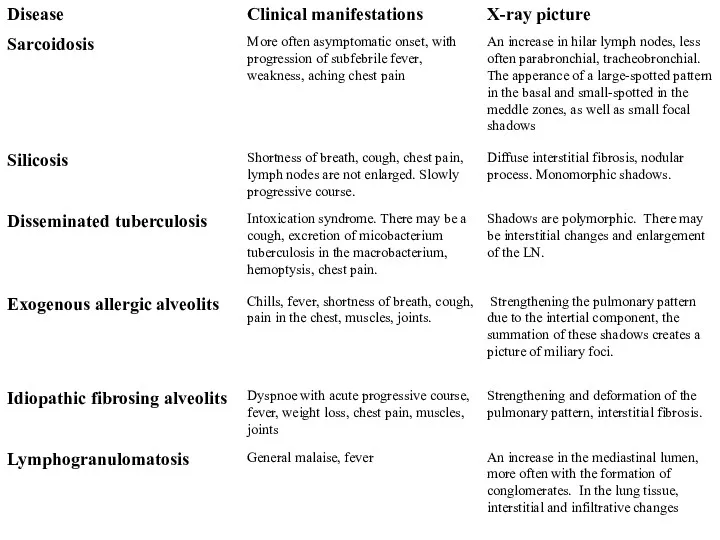
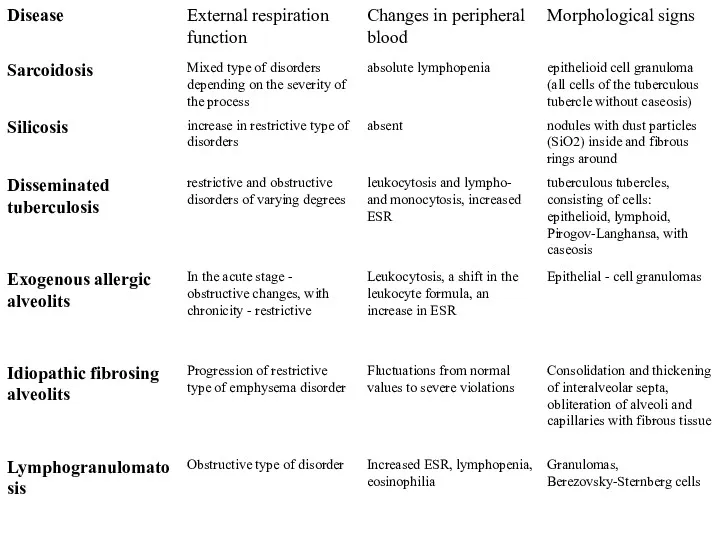
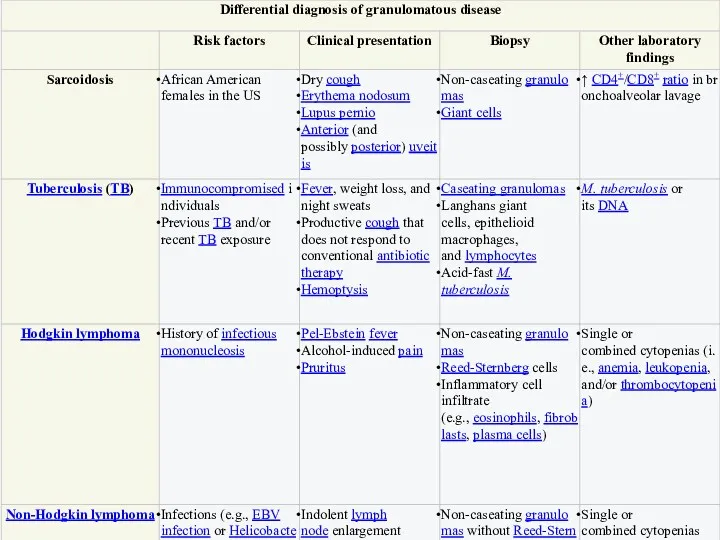
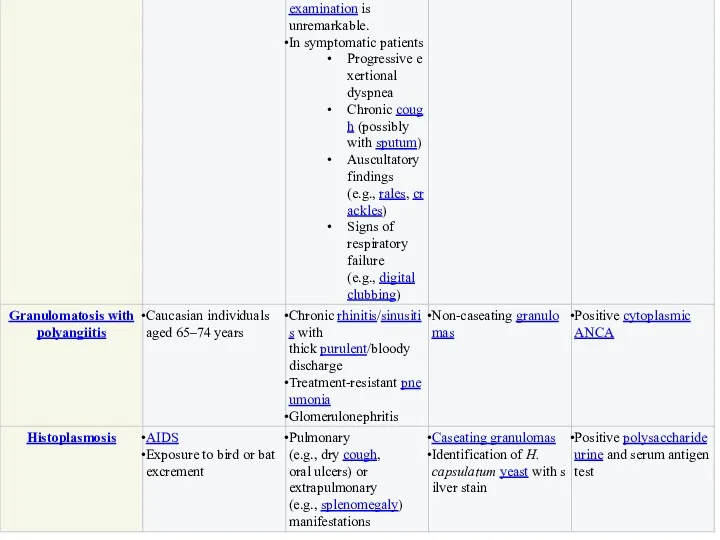
- 27. Differential diagnosis sarcoidosis
- 32. Treatment NSAIDs Corticosteroids Sometimes used immunosuppressants
- 33. Patients who need treatment regardless of stage include the following: Worsening symptoms Activity limitation Significant impairment
- 34. Corticosteroids Symptom management begins with corticosteroids. ! The presence of abnormalities on chest scans without significant
- 35. The optimal duration of treatment is unknown. A premature dose reduction may lead to relapse. In
- 36. Inhaled corticosteroids can relieve cough in patients with endobronchial involvement or airway hyperresponsiveness. Inhalation of large
- 37. Immunosuppressants ! Treatment with immunosuppressants is carried out in case of intolerance to moderate doses of
- 38. Other drugs that have been effective in a small number of patients who do not respond
- 39. Oxygen therapy The administration of oxygen to patients with LH on the background of sarcoidosis is
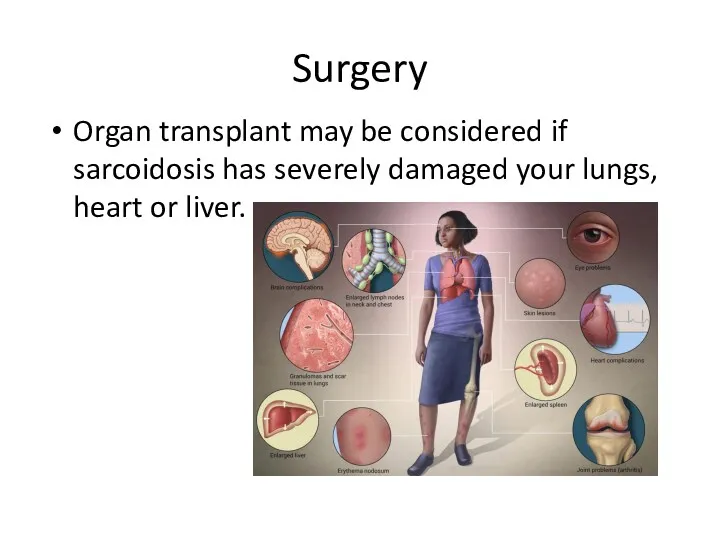
- 40. Surgery Organ transplant may be considered if sarcoidosis has severely damaged your lungs, heart or liver.
- 41. Complication of sarcoidosis: Complications list for Sarcoidosis: Lung damage - about 90% of cases Collapsed lung
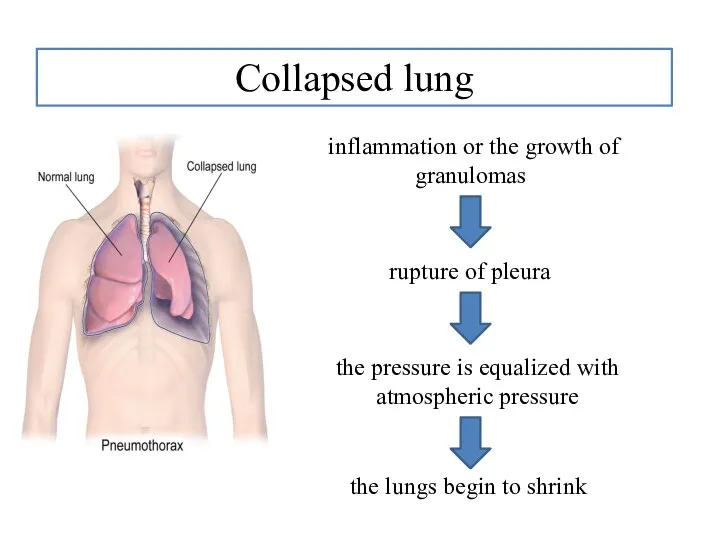
- 42. Collapsed lung inflammation or the growth of granulomas rupture of pleura the pressure is equalized with
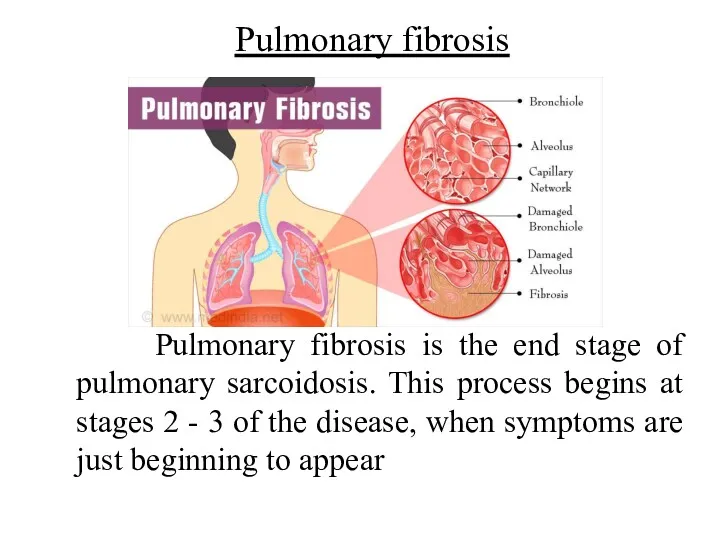
- 43. Pulmonary fibrosis Pulmonary fibrosis is the end stage of pulmonary sarcoidosis. This process begins at stages
- 45. Скачать презентацию
 Синдром Шарпа. Клинический разбор
Синдром Шарпа. Клинический разбор Ауыз қуыстың гигиенасы
Ауыз қуыстың гигиенасы Менструальный цикл и его регуляция. Дисфункциональные маточные кровотечения
Менструальный цикл и его регуляция. Дисфункциональные маточные кровотечения Массаж при сколиозе
Массаж при сколиозе Спортивный массаж
Спортивный массаж Көк іріңді таяқша. Экология. Резистенттілігі. Адам үшін патогенділігі және науқас ағзасында орналасуы
Көк іріңді таяқша. Экология. Резистенттілігі. Адам үшін патогенділігі және науқас ағзасында орналасуы Неотложная помощь при остром кровотечении. Неотложная помощь при остром кровотечении
Неотложная помощь при остром кровотечении. Неотложная помощь при остром кровотечении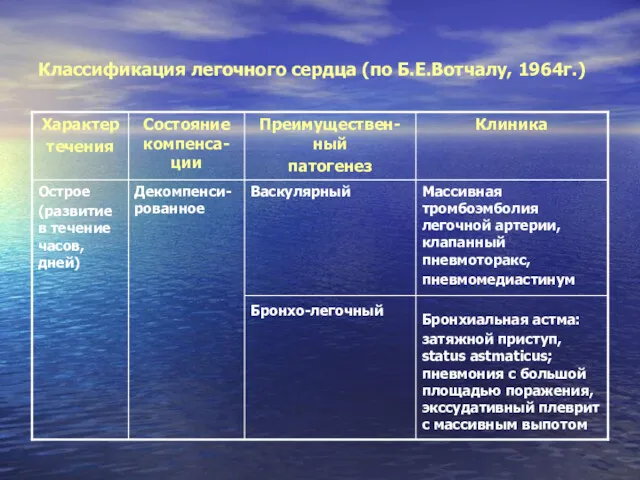 Классификация легочного сердца (по Б.Е.Вотчалу, 1964г.)
Классификация легочного сердца (по Б.Е.Вотчалу, 1964г.) Ответственность медицинских работников по уголовному кодексу
Ответственность медицинских работников по уголовному кодексу Здоровьесберегающие образовательные технологии в педиатрии. Роль центров здоровья в укреплении здоровья детей и подростков
Здоровьесберегающие образовательные технологии в педиатрии. Роль центров здоровья в укреплении здоровья детей и подростков Воспаление. Общие признаки воспаления
Воспаление. Общие признаки воспаления Жансыздандыру
Жансыздандыру Bases physiques de l’échographie EPG. Theme 15
Bases physiques de l’échographie EPG. Theme 15 Изменения слизистой оболочки полости рта при эндокринных расстройствах
Изменения слизистой оболочки полости рта при эндокринных расстройствах Подготовка к лабораторным исследованиям (2)
Подготовка к лабораторным исследованиям (2) 3d-моделирование челюстей и их фрагментов, полученных из результатов конусно-лучевой компьютерной томографии
3d-моделирование челюстей и их фрагментов, полученных из результатов конусно-лучевой компьютерной томографии Непрерывное медицинское образование
Непрерывное медицинское образование Пластикалық хирургияның негіздері
Пластикалық хирургияның негіздері Организация производства экстракта полыни гмелина (Artemisia gmelini)
Организация производства экстракта полыни гмелина (Artemisia gmelini) Бронхиальная астма
Бронхиальная астма Первая доврачебная помощь при утоплении, электротравме, поражении молнией. Практика по уходу за больным
Первая доврачебная помощь при утоплении, электротравме, поражении молнией. Практика по уходу за больным Особенности кровообращения плода и детей раннего возраста
Особенности кровообращения плода и детей раннего возраста Одонтогенные воспалительные заболевания челюстно лицевой области
Одонтогенные воспалительные заболевания челюстно лицевой области Наркотики и их влияние на организм человека
Наркотики и их влияние на организм человека Новая концепция лечения диффузного альвеолярного кровотечения (DAH)
Новая концепция лечения диффузного альвеолярного кровотечения (DAH) 2 типті қант диабеті дамуының факторлары
2 типті қант диабеті дамуының факторлары Мезенхимальные опухоли. Опухоли из меланинобразуюшей ткани. Опухоли нервной системы и оболочек мозга
Мезенхимальные опухоли. Опухоли из меланинобразуюшей ткани. Опухоли нервной системы и оболочек мозга Инъекциялар кезіндегі асқынулар және оның алдын алу
Инъекциялар кезіндегі асқынулар және оның алдын алу