Содержание
- 2. General information First reports – ancient times ‘diabetes’ – excessive urination ‘mellitus’ –honey. 1922 – insulin
- 3. DM statistics (IDF) 382 millions diabetic patients worldwide (8,3%) 46% undiagnosed (in Sub-Saharan Africa up to
- 4. Insulin effects Carbohydrate Metabolism Insulin dependent tissues– muscles, adipose tissue, liver - can uptake glucose ONLY
- 5. Insulin effects Carbohydrate Metabolism Increases glycogen synthesis in the liver. ↓ blood glucose concentration. In the
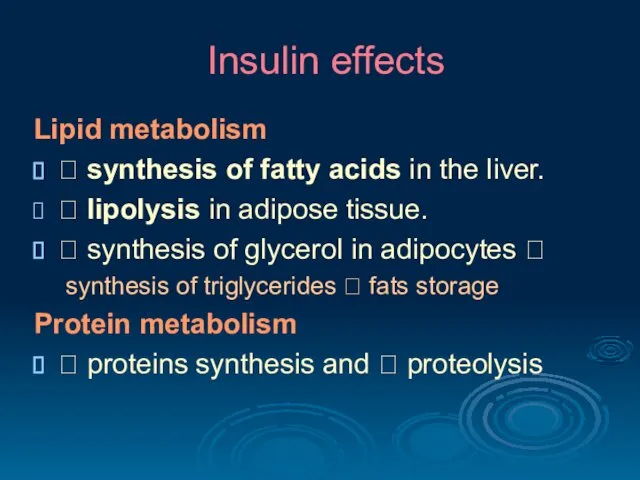
- 6. Insulin effects Lipid metabolism ? synthesis of fatty acids in the liver. ? lipolysis in adipose
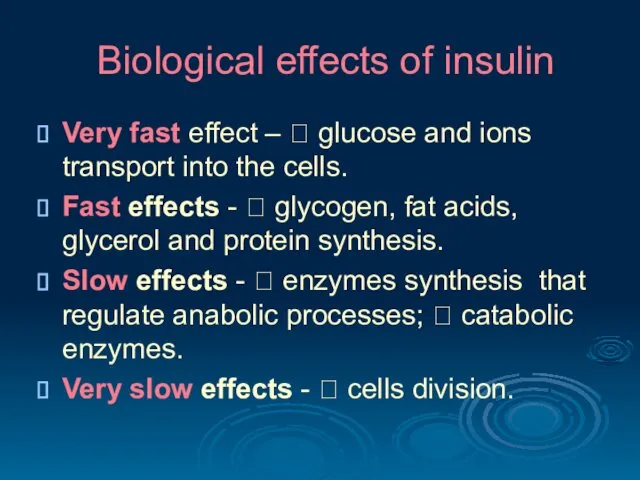
- 7. Biological effects of insulin Very fast effect – ? glucose and ions transport into the cells.
- 8. DIABETES - is a complex metabolic disorder resulting from absolute or relative insulin deficiency
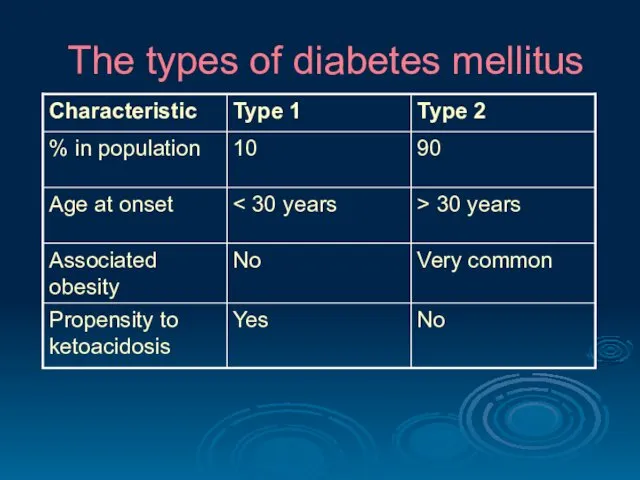
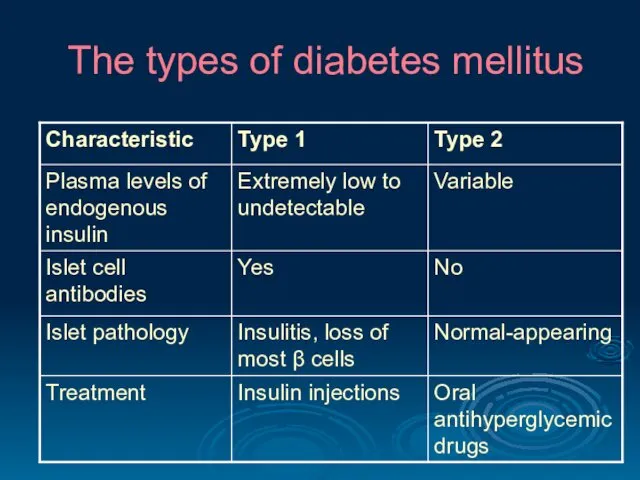
- 9. The types of diabetes mellitus
- 10. The types of diabetes mellitus
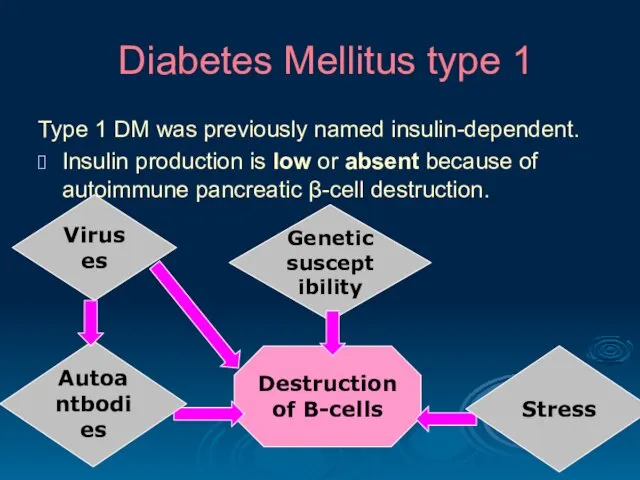
- 11. Diabetes Mellitus type 1 Type 1 DM was previously named insulin-dependent. Insulin production is low or
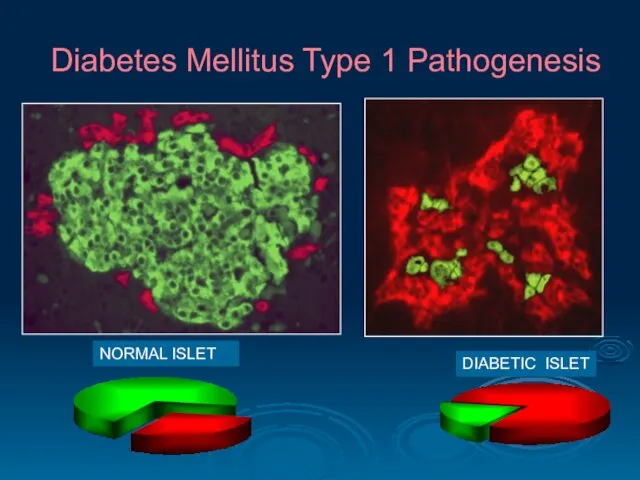
- 12. Diabetes Mellitus Type 1 Pathogenesis NORMAL ISLET DIABETIC ISLET
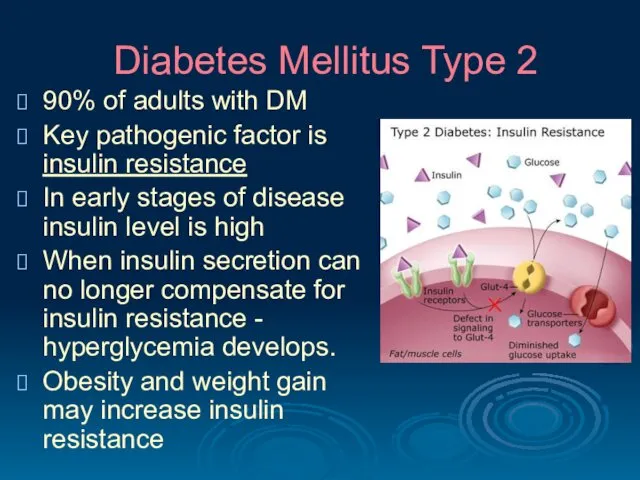
- 13. Diabetes Mellitus Type 2 90% of adults with DM Key pathogenic factor is insulin resistance In
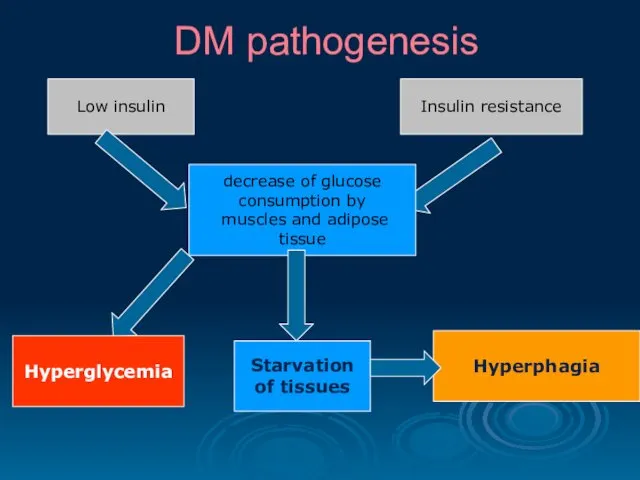
- 14. DM pathogenesis Hyperglycemia Low insulin Insulin resistance decrease of glucose consumption by muscles and adipose tissue
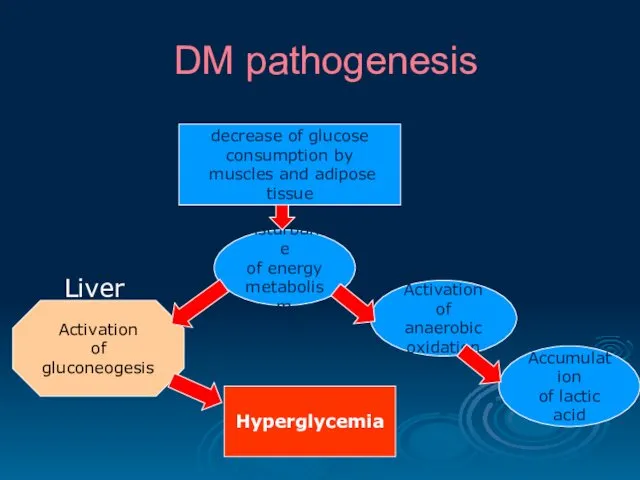
- 15. DM pathogenesis decrease of glucose consumption by muscles and adipose tissue Disturbance of energy metabolism Activation
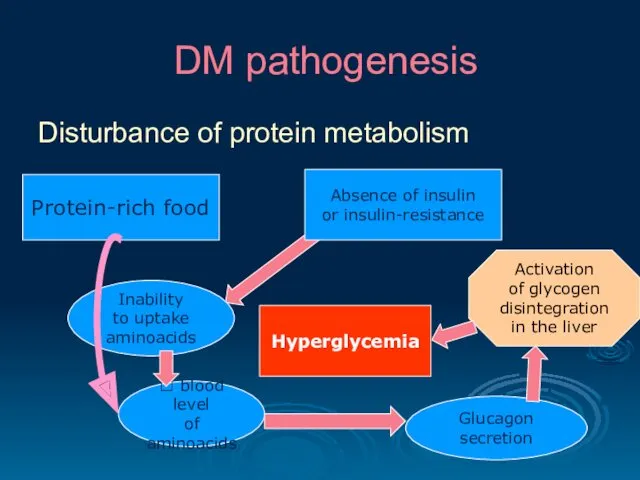
- 16. DM pathogenesis Disturbance of protein metabolism Protein-rich food Inability to uptake aminoacids Absence of insulin or
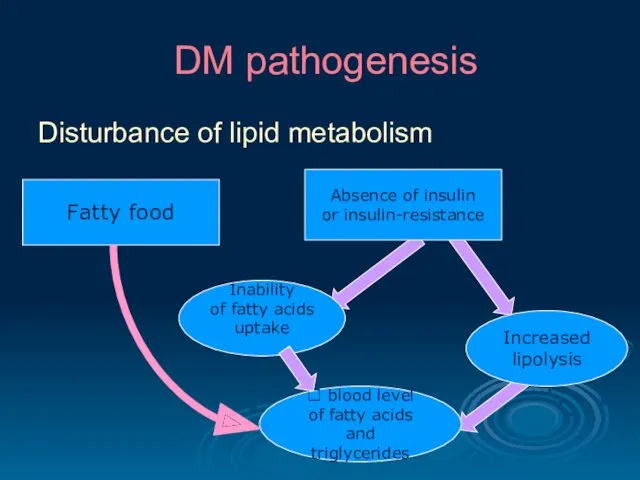
- 17. DM pathogenesis Disturbance of lipid metabolism Fatty food Inability of fatty acids uptake Absence of insulin
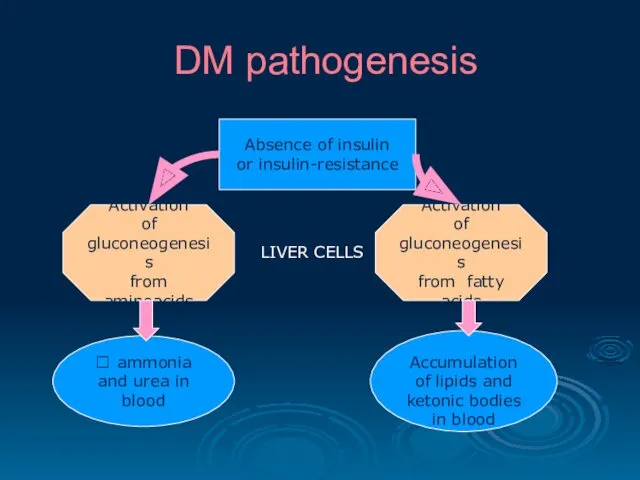
- 18. DM pathogenesis Absence of insulin or insulin-resistance Activation of gluconeogenesis from aminoacids Activation of gluconeogenesis from
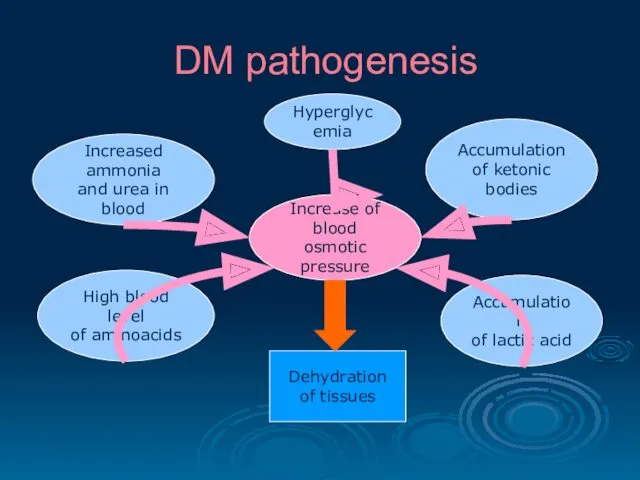
- 19. DM pathogenesis Accumulation of lactic acid High blood level of aminoacids Increased ammonia and urea in
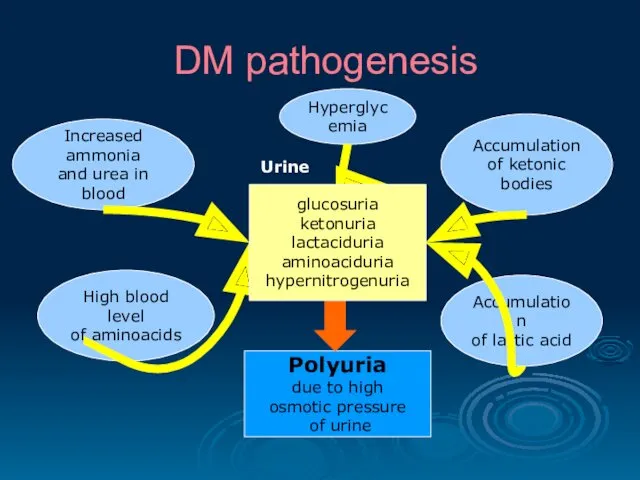
- 20. DM pathogenesis Accumulation of lactic acid High blood level of aminoacids Increased ammonia and urea in
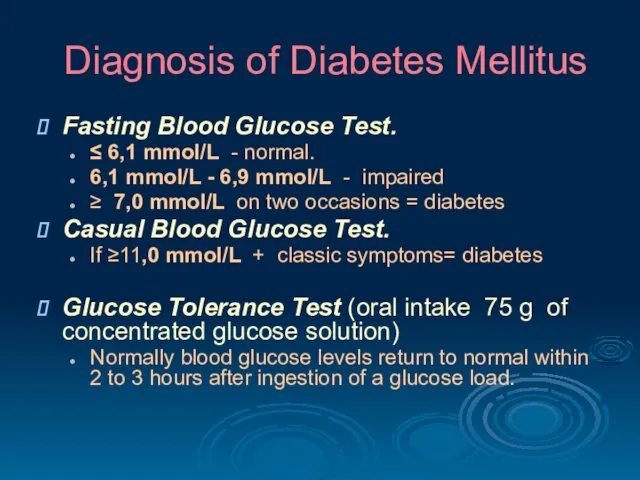
- 21. Diagnosis of Diabetes Mellitus Fasting Blood Glucose Test. ≤ 6,1 mmol/L - normal. 6,1 mmol/L -
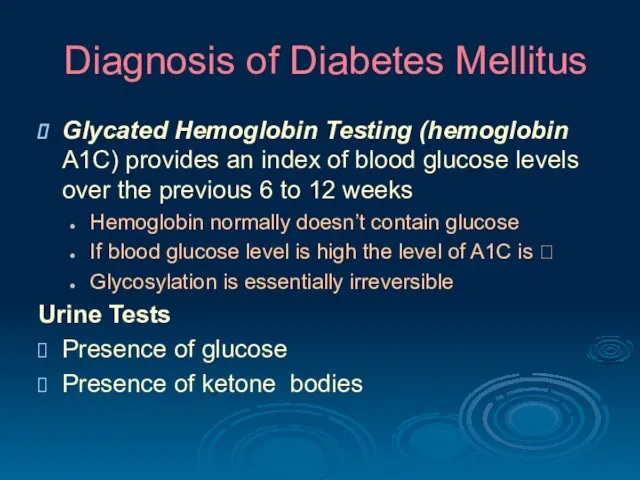
- 22. Diagnosis of Diabetes Mellitus Glycated Hemoglobin Testing (hemoglobin A1C) provides an index of blood glucose levels
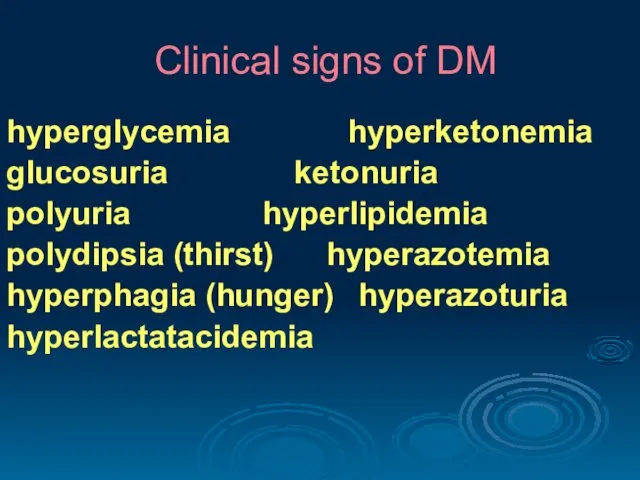
- 23. Clinical signs of DM hyperglycemia hyperketonemia glucosuria ketonuria polyuria hyperlipidemia polydipsia (thirst) hyperazotemia hyperphagia (hunger) hyperazoturia
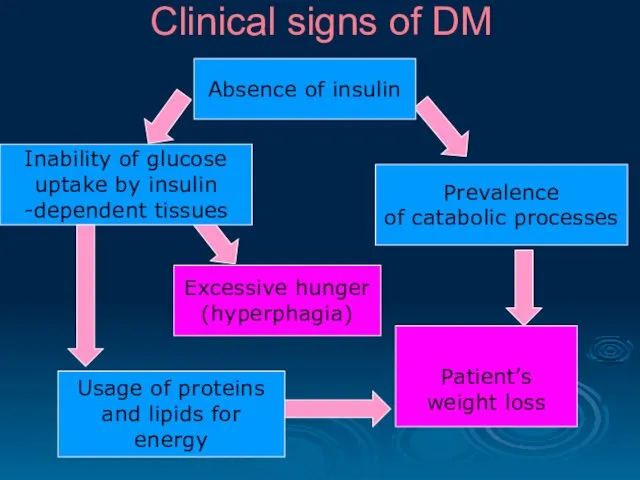
- 24. Clinical signs of DM Absence of insulin Prevalence of catabolic processes Excessive hunger (hyperphagia) Usage of
- 25. Choose the characteristic feature of type 1 diabetes mellitus Middle age at onset Associated obesity Low
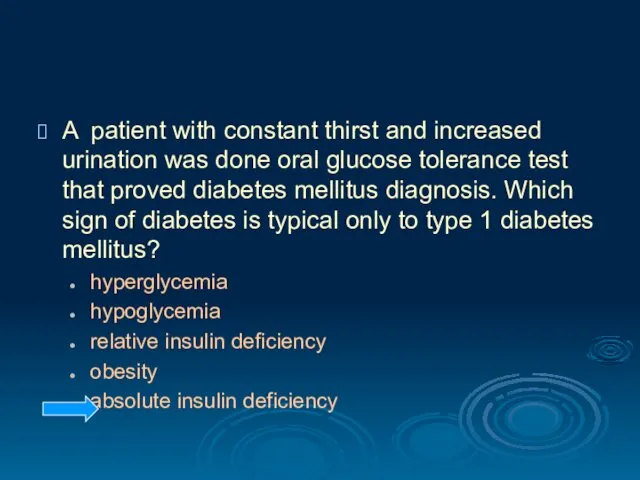
- 26. A patient with constant thirst and increased urination was done oral glucose tolerance test that proved
- 27. One of the diabetes mellitus clinical symptoms is hyperphagia. It is developed due to… lack of
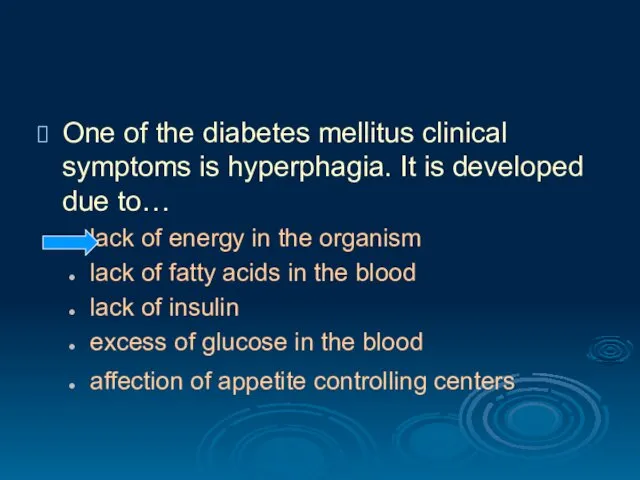
- 28. Patient with diabetes mellitus has hyperglycemia 19 mmol/ l, which is clinically developed as glucosuria, polyuria,
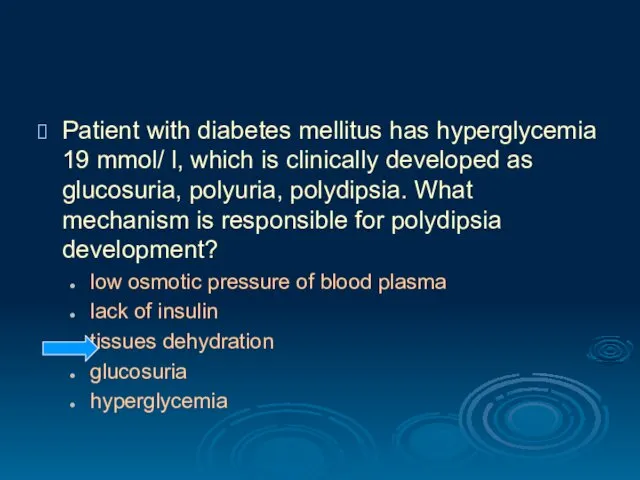
- 29. Acute complications of DM Diabetic comas hyperglycemic hypoglycemic hyperosmolar hyperlactatacidemic
- 30. Acute complications of DM Hyperglycemic coma expressed hyperglycemia (>20 mmol/l); progressive dehydration of the organism; ketoacidosis
- 31. Acute complications of DM Hypoglycemic coma may develop if the glucose intake does not match the
- 32. Acute complications of DM Hyperosmolar coma high concentration of glucose, Na, Cl, bicarbonates, urea, ammonia in
- 33. Chronic complications of DM Microvascular disturbances Diabetic retinopathy - severe vision loss or blindness. Diabetic neuropathy
- 34. Chronic complications of DM Macrovascular disease Coronary artery disease, leading to myocardial infarction ("heart attack") or
- 35. Chronic complications of DM Diabetic cardiomyopathy results from many factors (atherosclerosis, hypertension, microvascular disease, endothelial and
- 36. Principles of treatment Control of hyperglycemia. Type 1 diabetics require insulin. Type 2 diabetics should be
- 37. Prevention of DM Early type 1 DM in some patients may be prevented by suppression of
- 38. Which coma often occurs in the patients with diabetes mellitus type 1 when diet is not
- 39. Patient R., 46 years old, has diabetic neuropathy. What is the main mechanism in nervous fibers
- 41. Скачать презентацию
 Жалпы практика дәрігерінің жұмысын ұйымдастыру. Дәрігерлік амбулатория жұмысының менеджмент негіздері
Жалпы практика дәрігерінің жұмысын ұйымдастыру. Дәрігерлік амбулатория жұмысының менеджмент негіздері Жергілікті жансызданудың асқынулары
Жергілікті жансызданудың асқынулары Гигиена аптечных заведений
Гигиена аптечных заведений Женское бесплодие. Современные технологии в диагностике и лечении
Женское бесплодие. Современные технологии в диагностике и лечении :Пародонтоз аурулары. Патогенез. Алдын алу және емдеу
:Пародонтоз аурулары. Патогенез. Алдын алу және емдеу Рентгенологические признаки заболеваний легких: как читать рентгенограммы и КТ органов грудной клетки
Рентгенологические признаки заболеваний легких: как читать рентгенограммы и КТ органов грудной клетки Неспецифические заболевания тонкого и толстого кишечника
Неспецифические заболевания тонкого и толстого кишечника Балалардағы герпестік және цитомегаловирустық
Балалардағы герпестік және цитомегаловирустық Легочная гипертензия
Легочная гипертензия Медицина и первая помощь
Медицина и первая помощь Валидация очистки помещения и оборудования
Валидация очистки помещения и оборудования Дисплазия коленного сустава
Дисплазия коленного сустава Синдромы поражения плевры
Синдромы поражения плевры Лікарські помилки, моральна та правова відповідальність лікаря
Лікарські помилки, моральна та правова відповідальність лікаря Ожоги органа зрения
Ожоги органа зрения ЛП, влияющие на функции органов дыхания
ЛП, влияющие на функции органов дыхания Пневмония. Внебольничные и внутрибольничные пневмонии
Пневмония. Внебольничные и внутрибольничные пневмонии Обеспечение безопасности при неблагоприятной экологической обстановке
Обеспечение безопасности при неблагоприятной экологической обстановке Страховая система здравоохранения США
Страховая система здравоохранения США Нейродиетология тиков и гиперкинезов
Нейродиетология тиков и гиперкинезов Pathophysiology of loco-motor system
Pathophysiology of loco-motor system Гемопоэз. Теория кроветворения
Гемопоэз. Теория кроветворения Кровотечение. Методы остановки кровотечений
Кровотечение. Методы остановки кровотечений Пластические операции в маммологии
Пластические операции в маммологии Ультразвуковое исследование тазобедренного сустава
Ультразвуковое исследование тазобедренного сустава Микробиологическая диагностика спирохетозов
Микробиологическая диагностика спирохетозов Реабилитация пациентов при инфекционных и паразитарных заболеваниях
Реабилитация пациентов при инфекционных и паразитарных заболеваниях Эшерихии. Классификация эшерихий
Эшерихии. Классификация эшерихий