Содержание
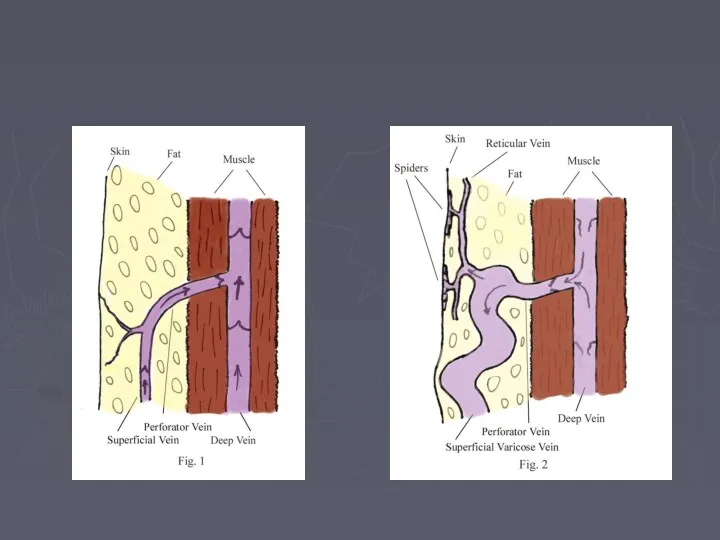
- 5. Venous return Muscle pump ( peripheral hearts) - ve intra thoracic pressure Arterial pulsation Vise at
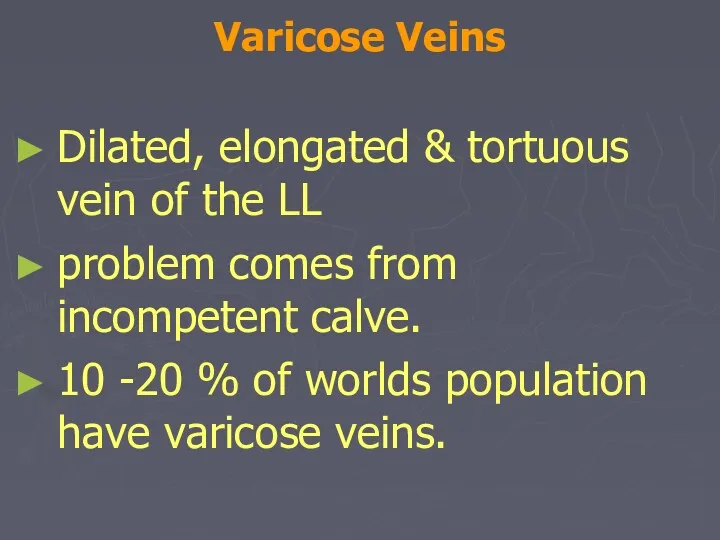
- 8. Varicose Veins Dilated, elongated & tortuous vein of the LL problem comes from incompetent calve. 10
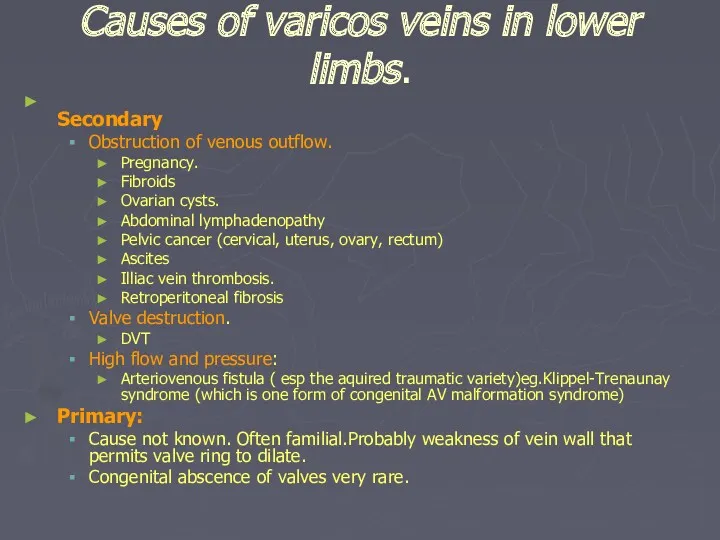
- 9. Causes of varicos veins in lower limbs. Secondary Obstruction of venous outflow. Pregnancy. Fibroids Ovarian cysts.
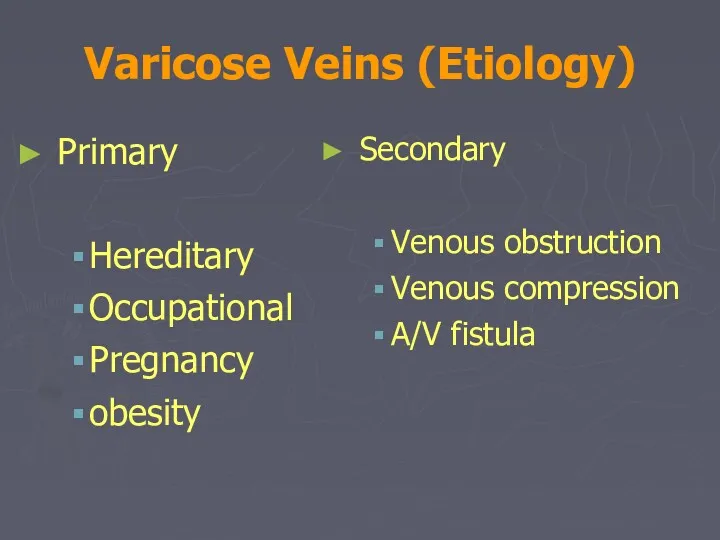
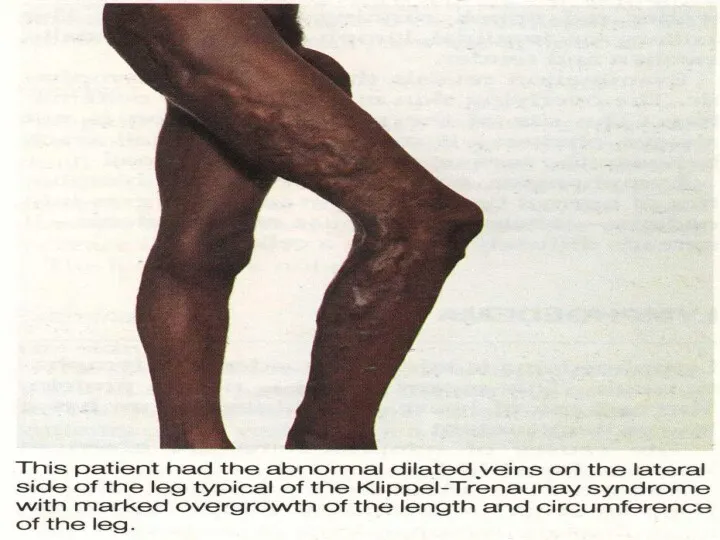
- 10. Varicose Veins (Etiology) Primary Hereditary Occupational Pregnancy obesity Secondary Venous obstruction Venous compression A/V fistula
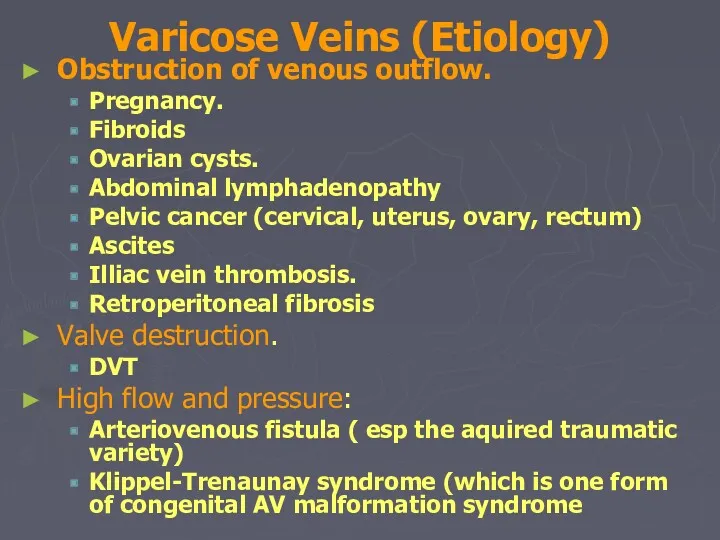
- 11. Varicose Veins (Etiology) Obstruction of venous outflow. Pregnancy. Fibroids Ovarian cysts. Abdominal lymphadenopathy Pelvic cancer (cervical,
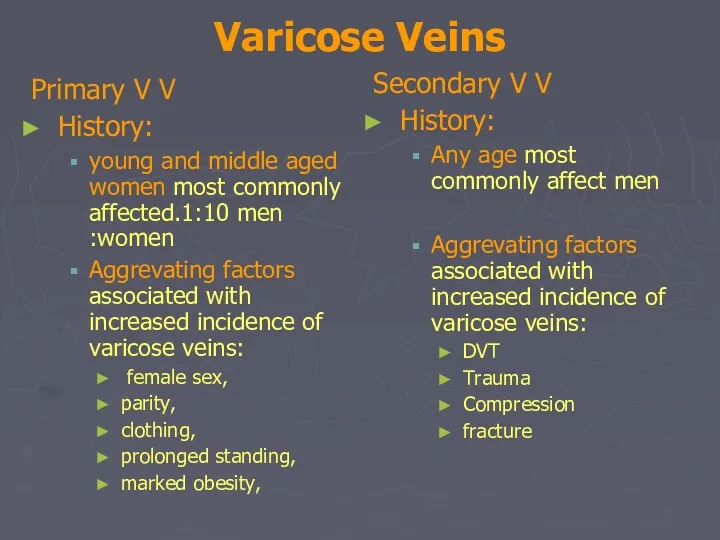
- 12. Varicose Veins Primary V V History: young and middle aged women most commonly affected.1:10 men :women
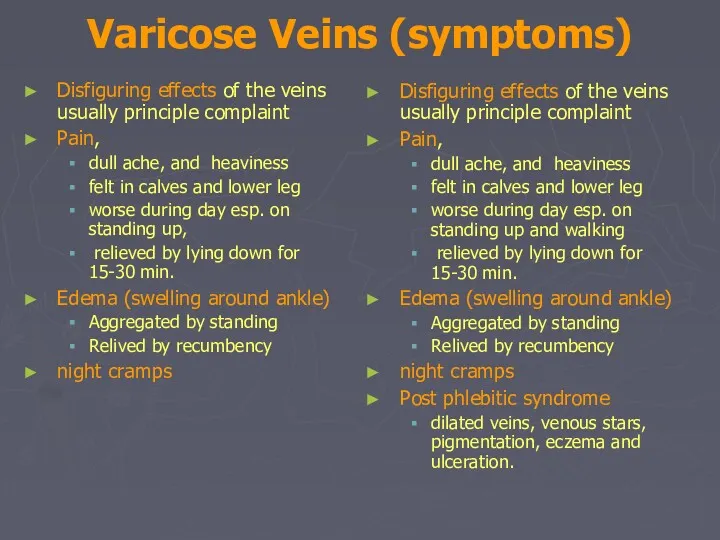
- 13. Varicose Veins (symptoms) Disfiguring effects of the veins usually principle complaint Pain, dull ache, and heaviness
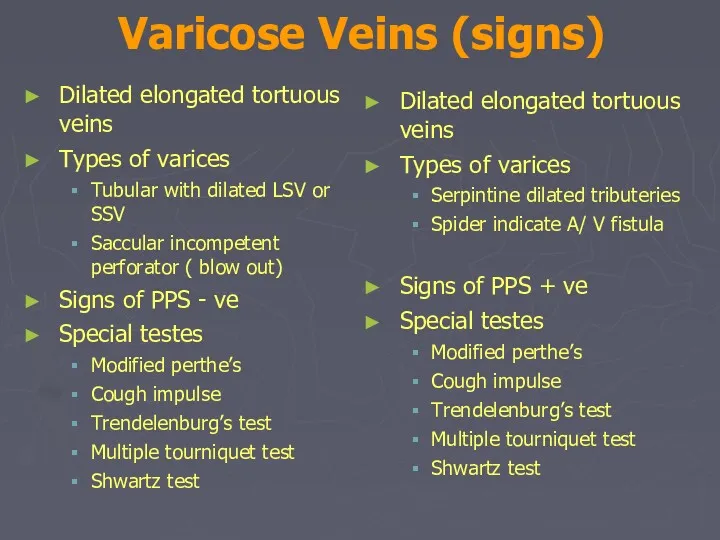
- 14. Varicose Veins (signs) Dilated elongated tortuous veins Types of varices Tubular with dilated LSV or SSV
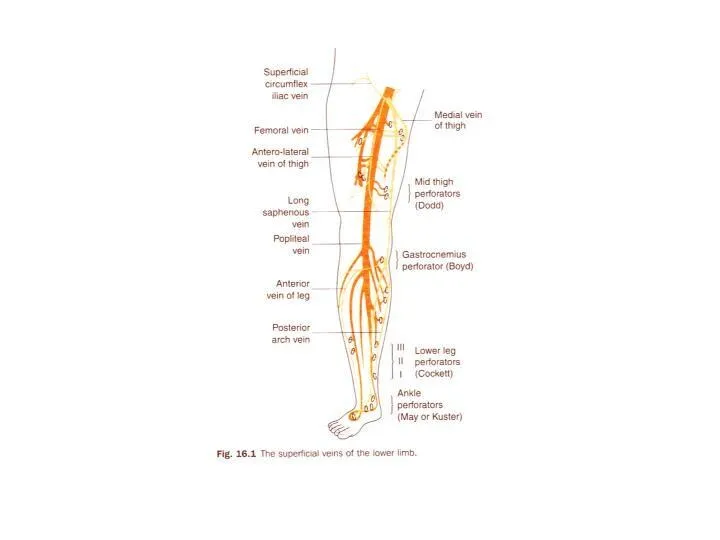
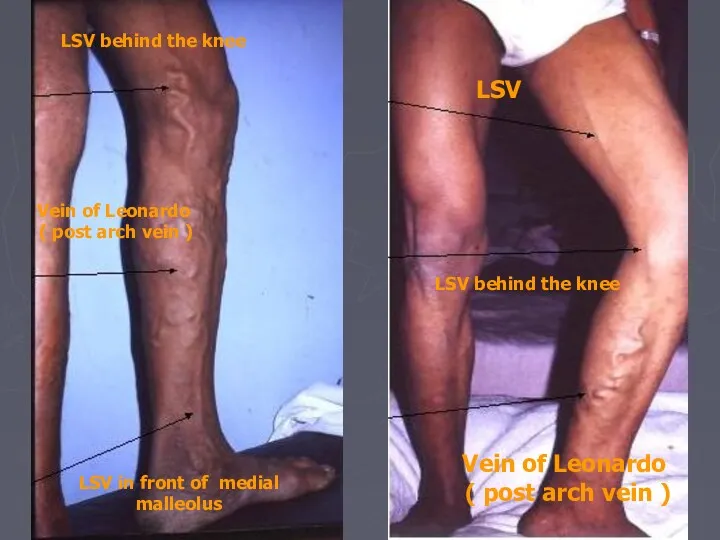
- 15. LSV LSV behind the knee Vein of Leonardo ( post arch vein ) LSV behind the
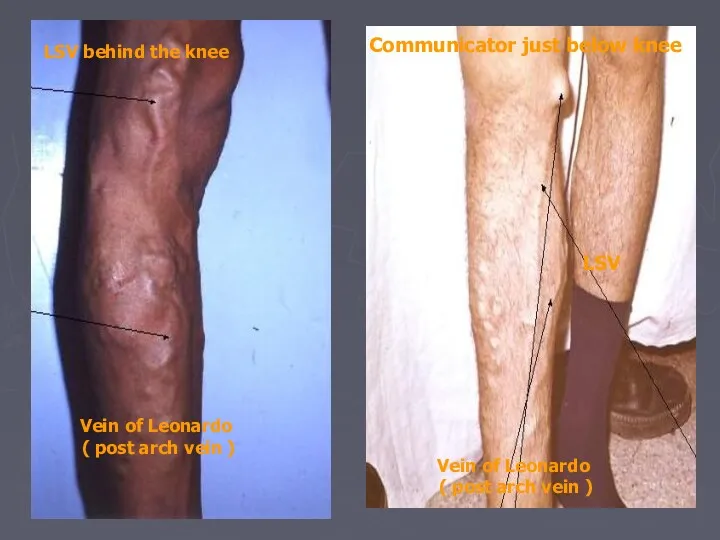
- 16. Communicator just below knee LSV Vein of Leonardo ( post arch vein ) LSV behind the
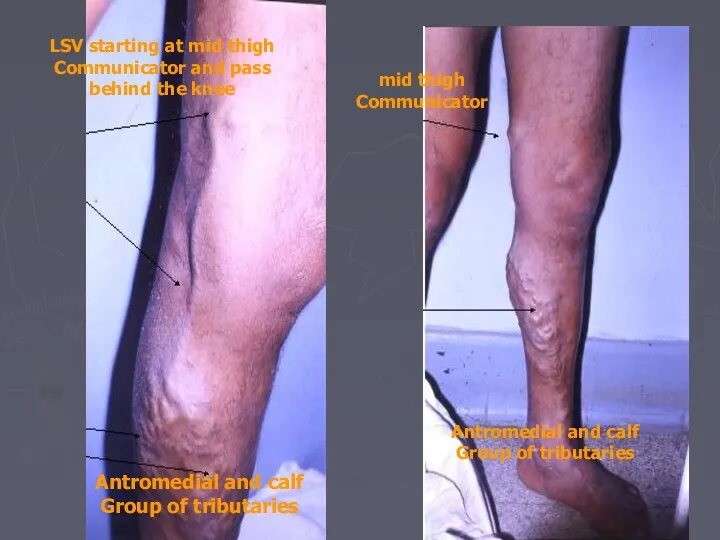
- 17. LSV starting at mid thigh Communicator and pass behind the knee Antromedial and calf Group of
- 18. Examination: Inspection: ask patient to stand up. look for abnormal visible subcutaneous veins. if dilated and
- 19. Examination: Palpation: feel along the course of the veins and feel the tension in the veins
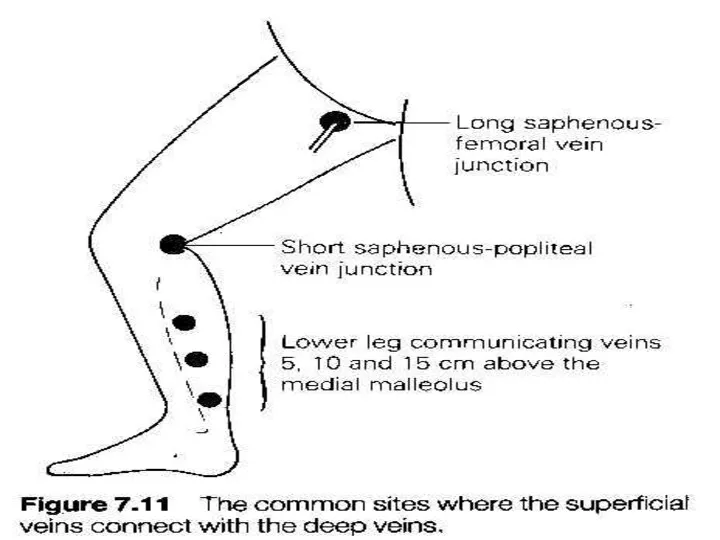
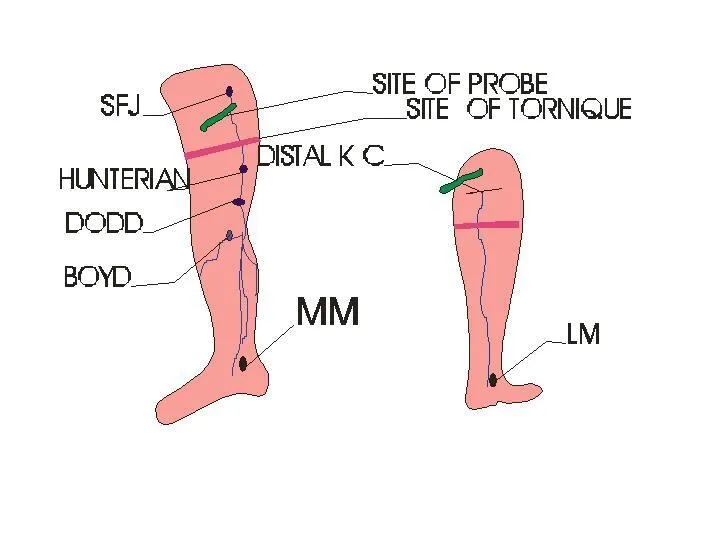
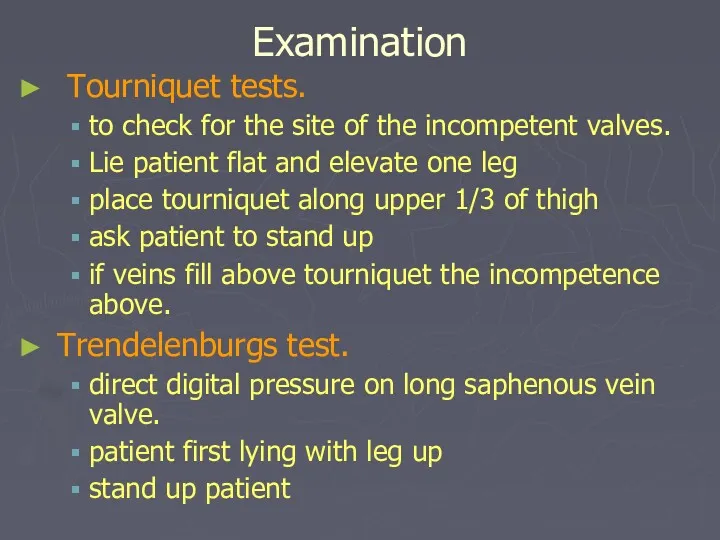
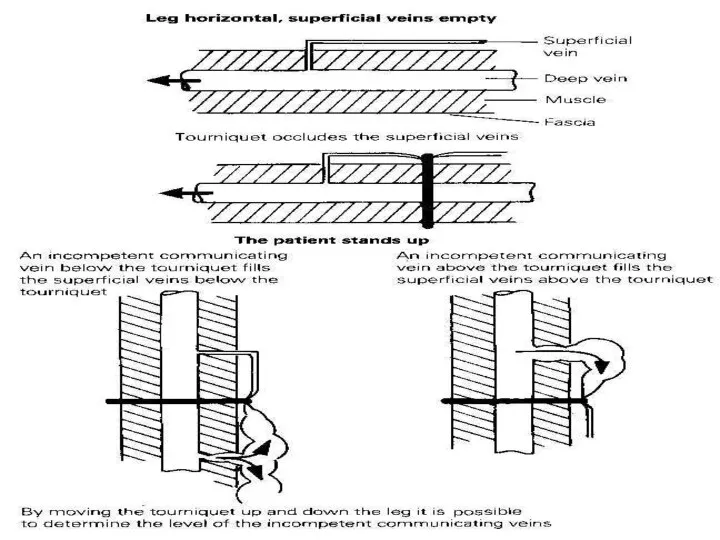
- 20. Examination Tourniquet tests. to check for the site of the incompetent valves. Lie patient flat and
- 22. Examination Percussion: transmission of percussion waves downward implies incompetent valves ( Shwartz test). Place fingers of
- 23. Examination General examination: examine abdomen, incl rectal and vaginal examination. men: palpate testes, testicular tumours can
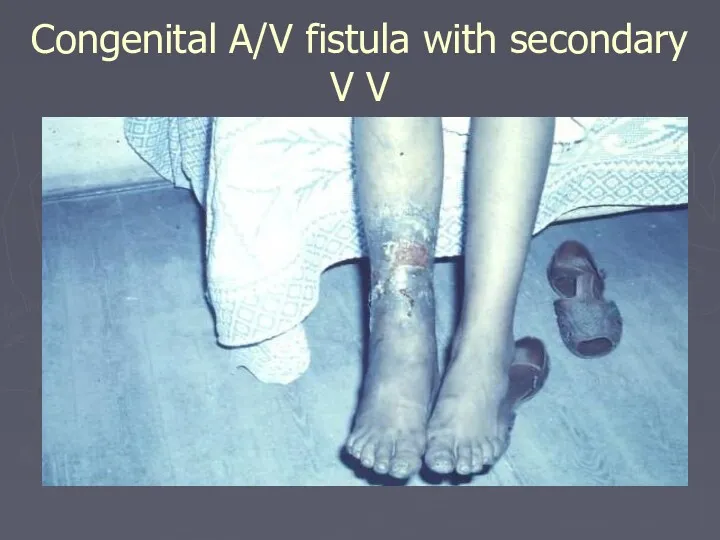
- 24. Congenital A/V fistula with secondary V V
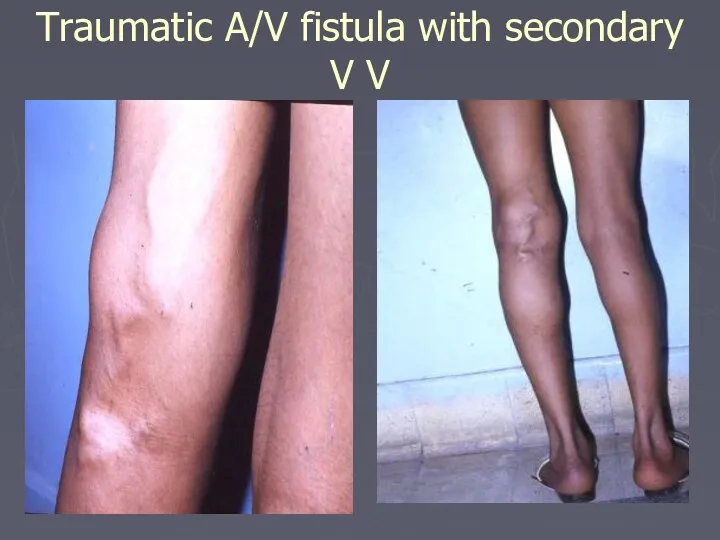
- 26. Traumatic A/V fistula with secondary V V
- 27. Investigation Routine Lab mainly BSL Hand held Doppler Continuous wave Doppler (CWD) (phono-angiography)
- 28. Investigation Doppler US
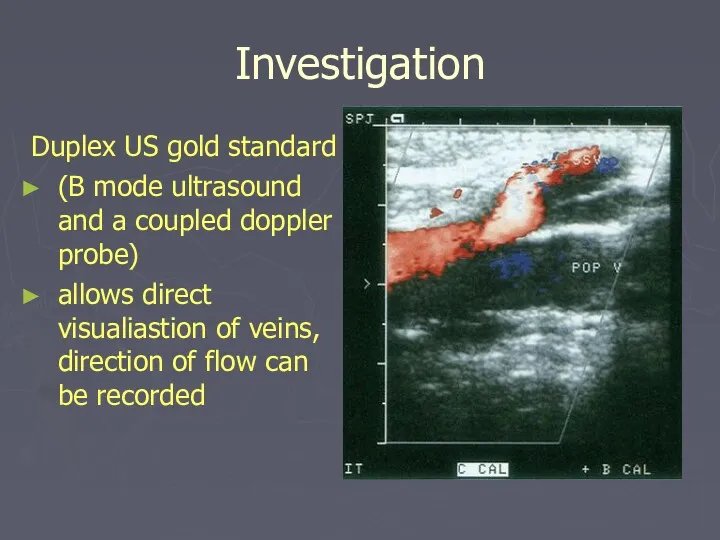
- 29. Investigation Duplex US gold standard (B mode ultrasound and a coupled doppler probe) allows direct visualiastion
- 30. Investigation Plethysmography and Venography are obsolete Venous pressure Radio-active isotope scanning Arteriograpgy if A/V fistula
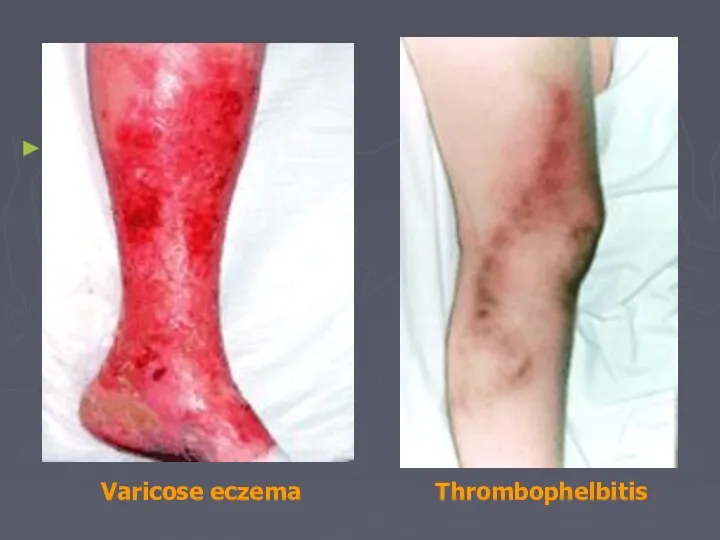
- 31. Complications: Haemorrhage Oedema Skin pigmentation Lipodermatosclerosis Varicose eczema Venous ulceration Thrombophlebitis Atrophie blanche Marjolin ulcer Equinous
- 32. Thrombophelbitis Varicose eczema
- 33. Treatment A. Non- operative management. walking should be encouraged and prolonged sitting and standing should be
- 34. Treatment Compression sclerotherapy. permanent fibrotic occlusion of collapsed veins. patient is recumbent and veins collapsed, a
- 35. Compression sclerotherapy. continuous pressure is maintained for 1-2 weeks with elastic stockings. much less expensive than
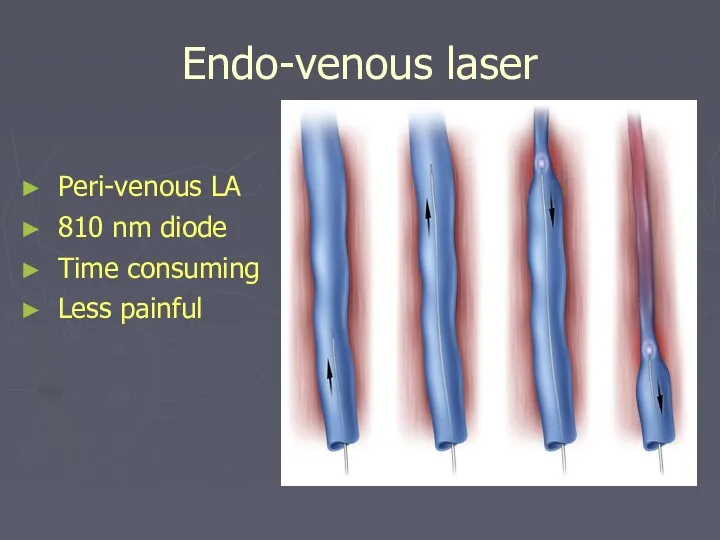
- 36. Endo-venous laser Peri-venous LA 810 nm diode Time consuming Less painful
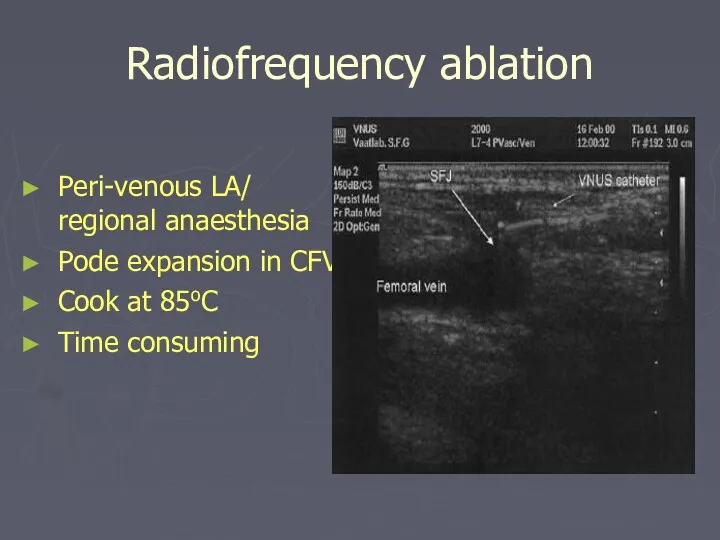
- 37. Radiofrequency ablation Peri-venous LA/ regional anaesthesia Pode expansion in CFV Cook at 85oC Time consuming
- 38. Treatment Surgical therapy. Indications: severe symptoms very large varices attacks of superficial phlebitis haemorrhage from rupturd
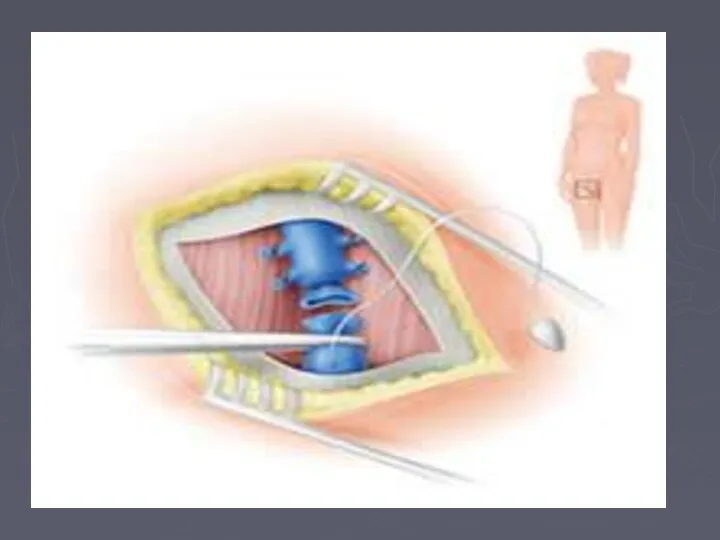
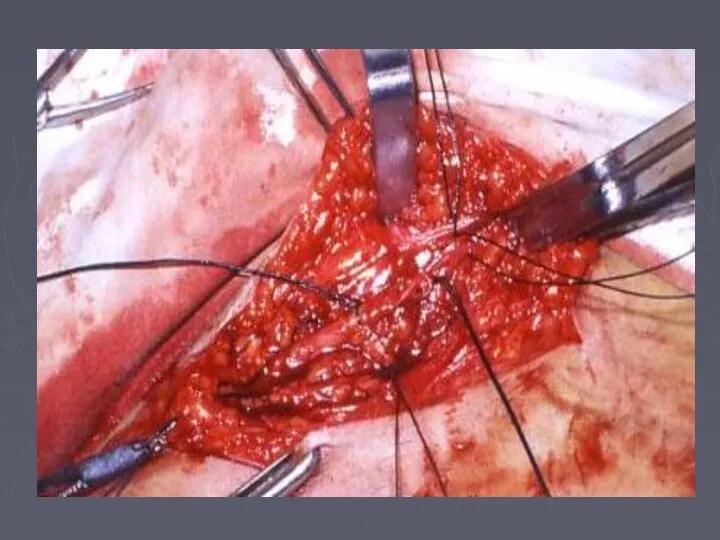
- 39. Treatment Surgical therapy. identify all perforating and superficial veins preoperatively and mark them. results depend on
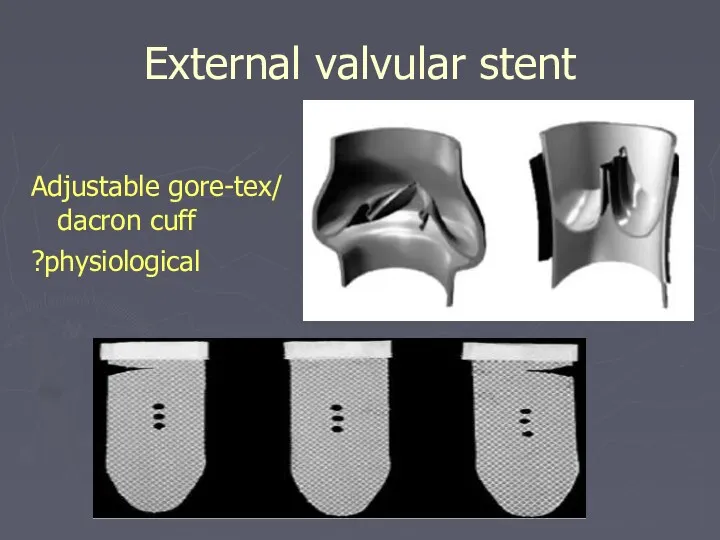
- 43. External valvular stent Adjustable gore-tex/ dacron cuff ?physiological
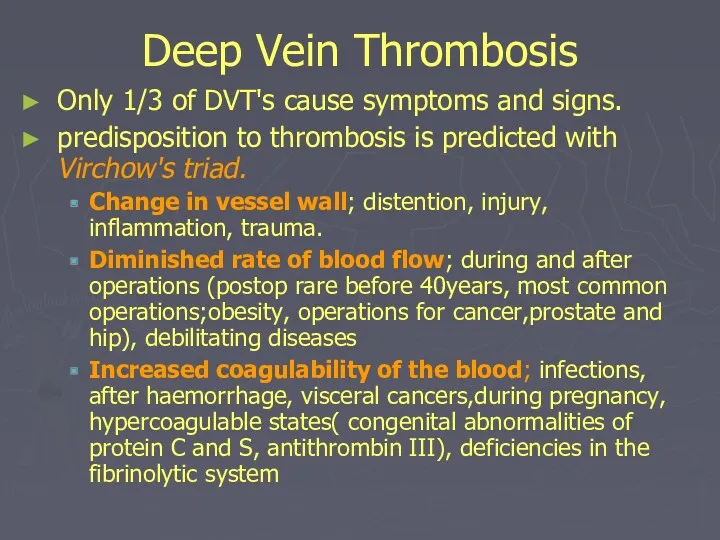
- 44. Deep Vein Thrombosis Only 1/3 of DVT's cause symptoms and signs. predisposition to thrombosis is predicted
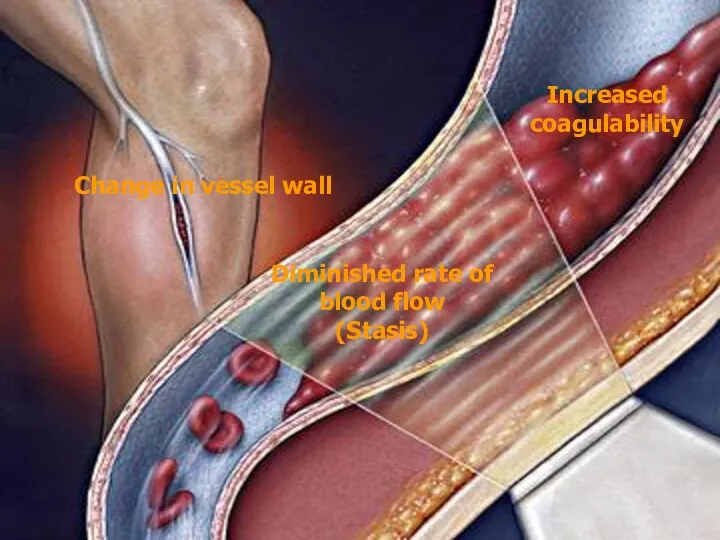
- 45. Increased coagulability Change in vessel wall Diminished rate of blood flow (Stasis)
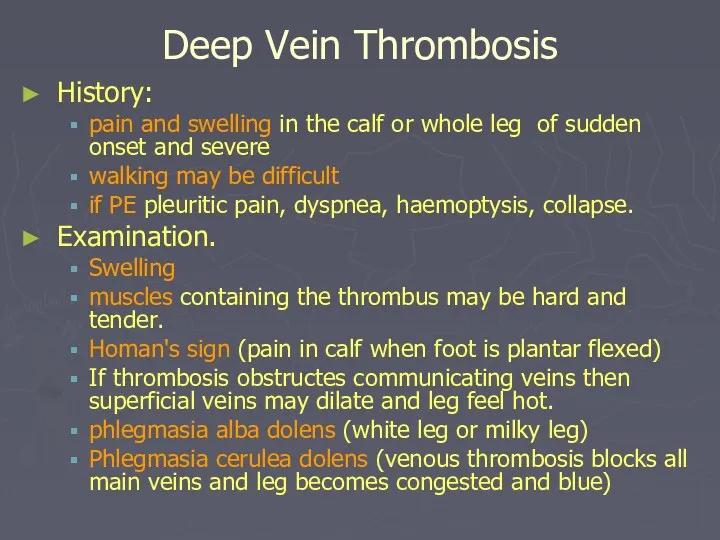
- 46. Deep Vein Thrombosis History: pain and swelling in the calf or whole leg of sudden onset
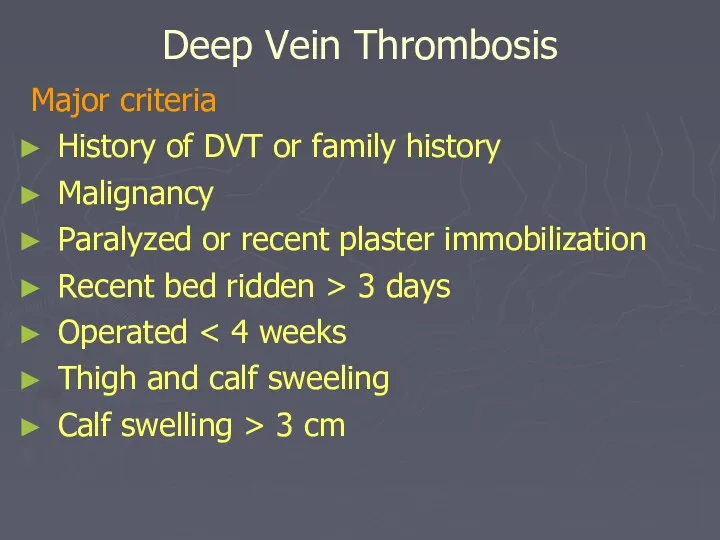
- 47. Deep Vein Thrombosis Major criteria History of DVT or family history Malignancy Paralyzed or recent plaster
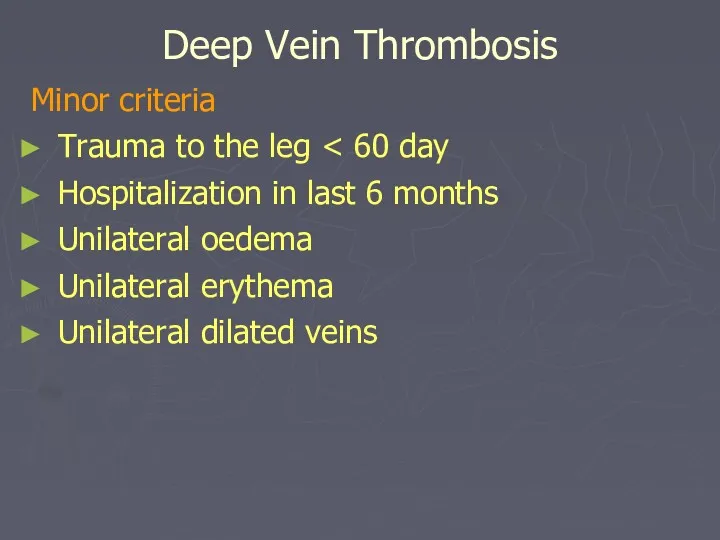
- 48. Deep Vein Thrombosis Minor criteria Trauma to the leg Hospitalization in last 6 months Unilateral oedema
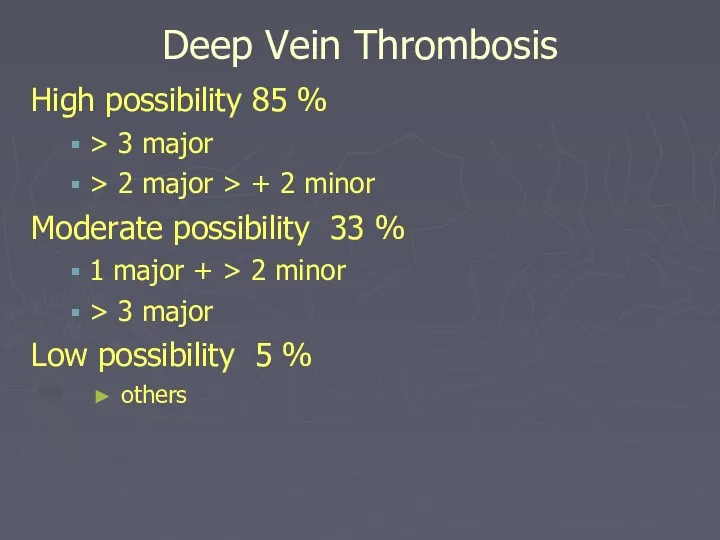
- 49. Deep Vein Thrombosis High possibility 85 % > 3 major > 2 major > + 2
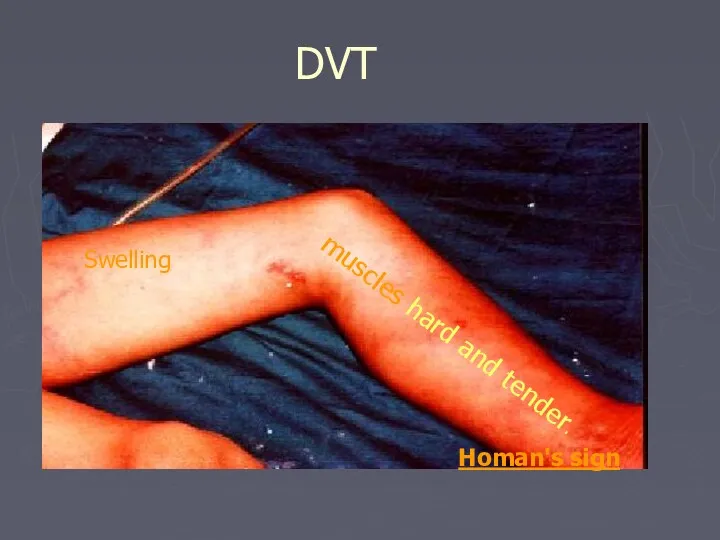
- 50. DVT Swelling muscles hard and tender. Homan's sign
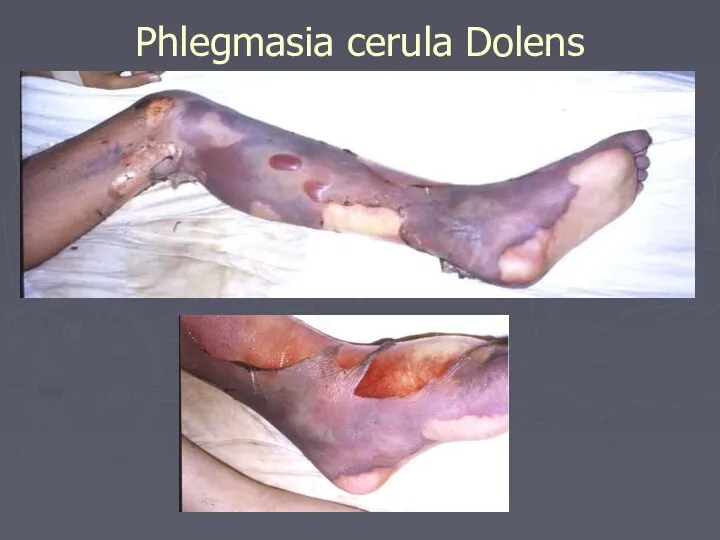
- 51. Phlegmasia cerula Dolens
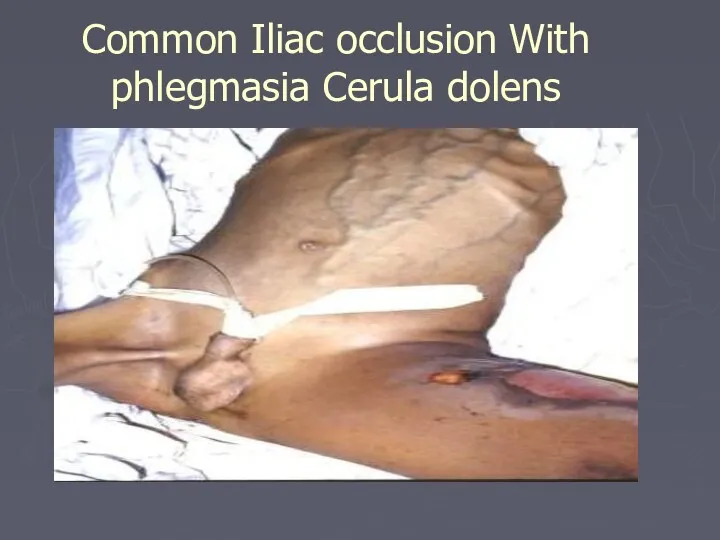
- 52. Common Iliac occlusion With phlegmasia Cerula dolens
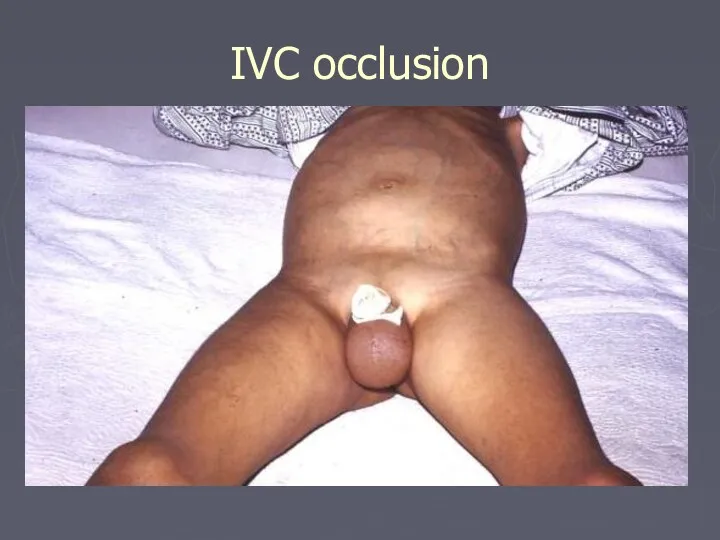
- 53. IVC occlusion
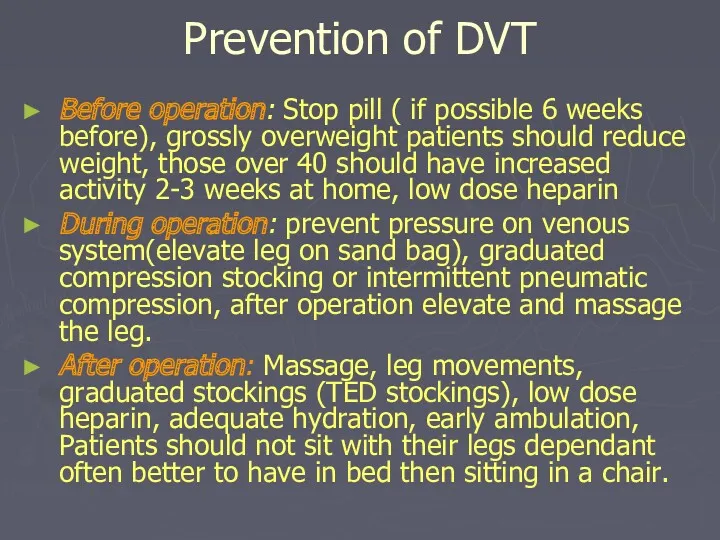
- 54. Prevention of DVT Before operation: Stop pill ( if possible 6 weeks before), grossly overweight patients
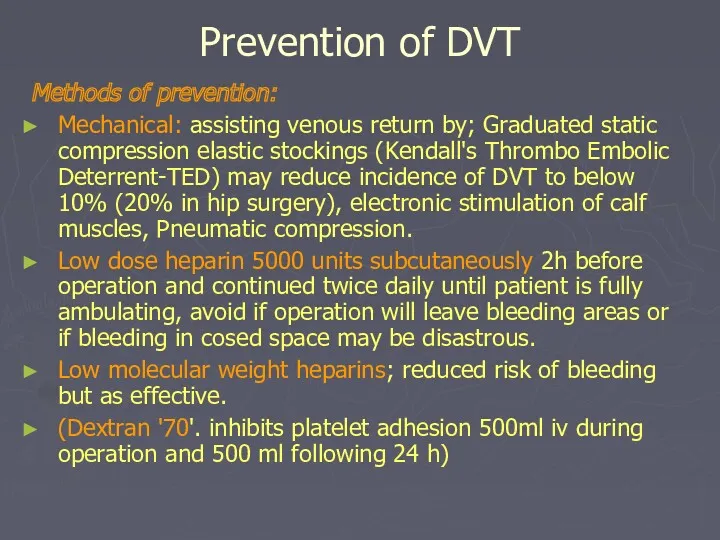
- 55. Prevention of DVT Methods of prevention: Mechanical: assisting venous return by; Graduated static compression elastic stockings
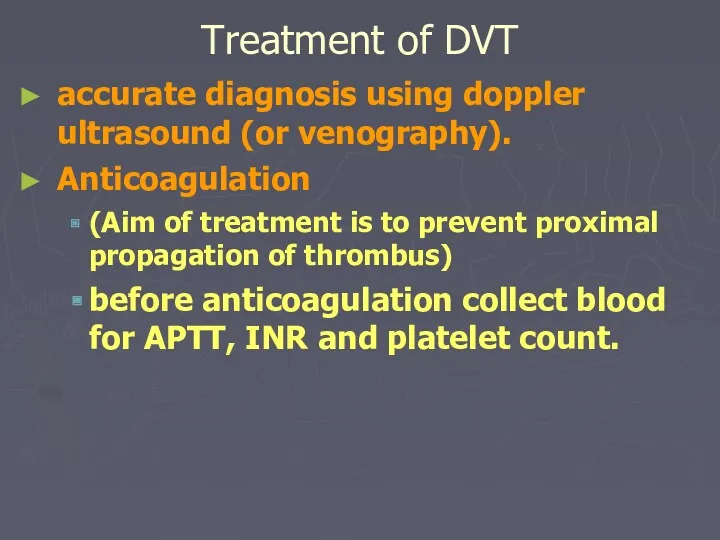
- 56. accurate diagnosis using doppler ultrasound (or venography). Anticoagulation (Aim of treatment is to prevent proximal propagation
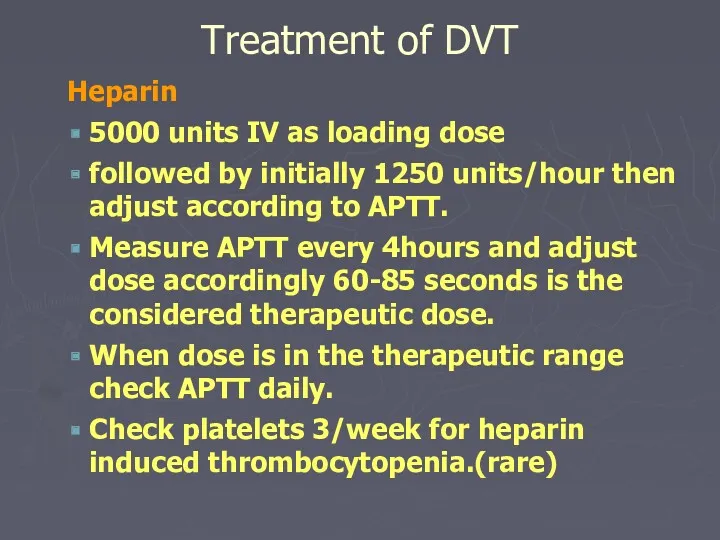
- 57. Heparin 5000 units IV as loading dose followed by initially 1250 units/hour then adjust according to
- 58. cease heparin when warfarin is established with a therapeutic INR 2 initial Warfarin 10mg orally, once
- 59. Treatment of DVT Thrombectomy; rarely indicated Fibrinolytic treatment: streptokinase, urokinase or combination of streptokinase with tissue
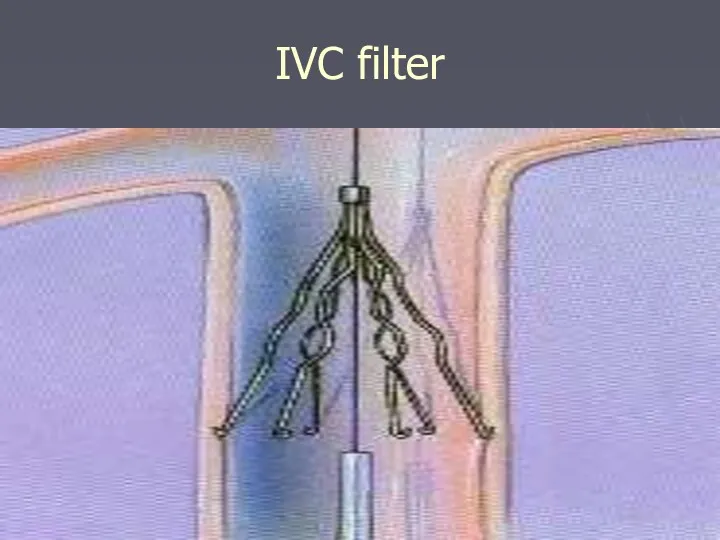
- 60. IVC filter
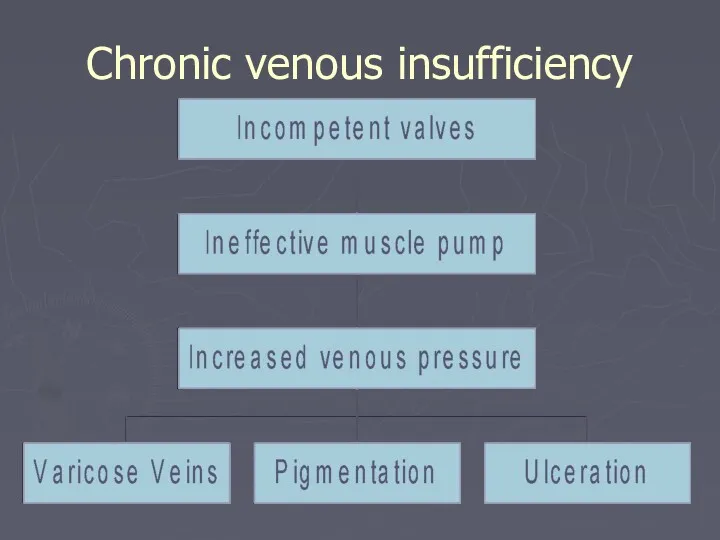
- 61. Chronic venous insufficiency
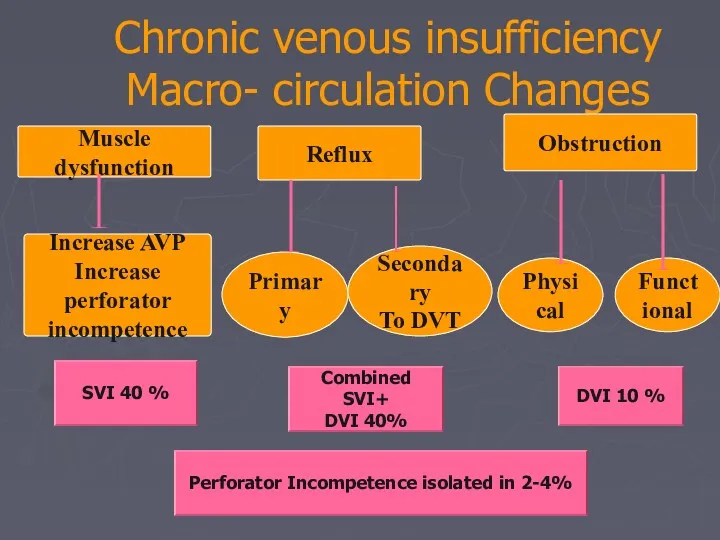
- 62. Chronic venous insufficiency Macro- circulation Changes Muscle dysfunction Obstruction Reflux Increase AVP Increase perforator incompetence Primary
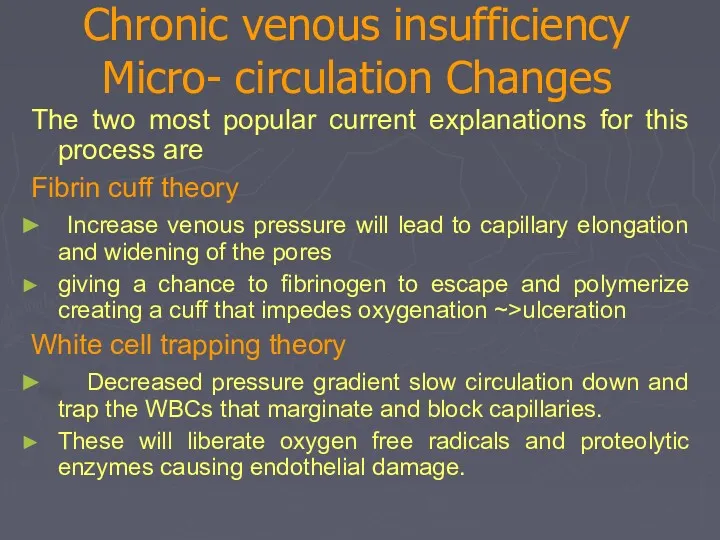
- 63. Chronic venous insufficiency Micro- circulation Changes The two most popular current explanations for this process are
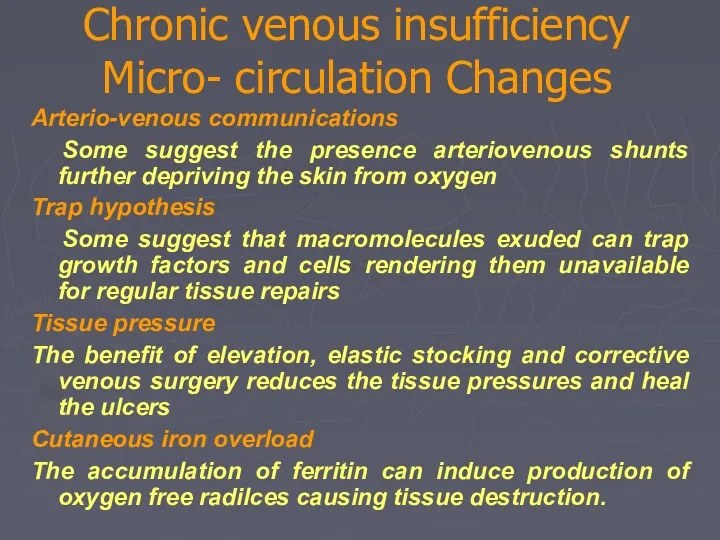
- 64. Chronic venous insufficiency Micro- circulation Changes Arterio-venous communications Some suggest the presence arteriovenous shunts further depriving
- 65. Chronic venous insufficiency Oedema Skin pigmentation Lipodermatosclerosis Varicose eczema Venous ulceration Thrombophlebitis Atrophie blanche Marjolin ulcer
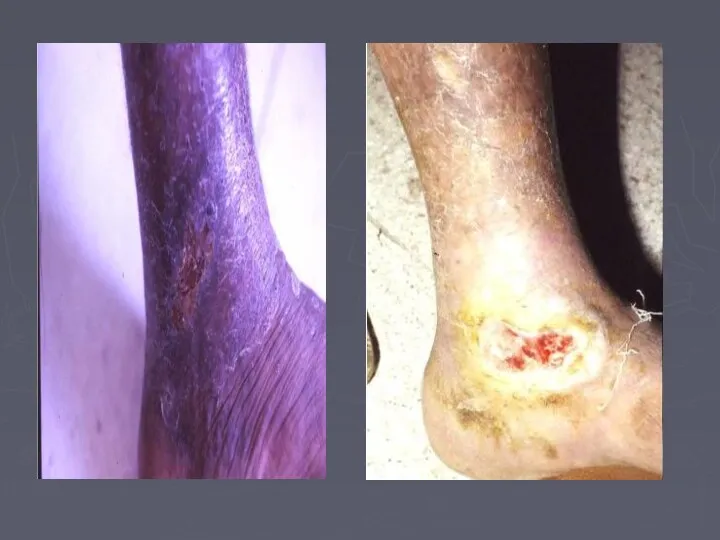
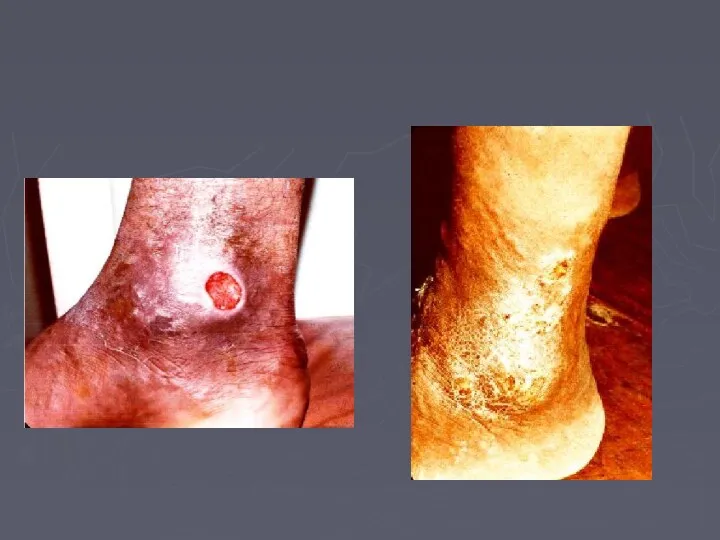
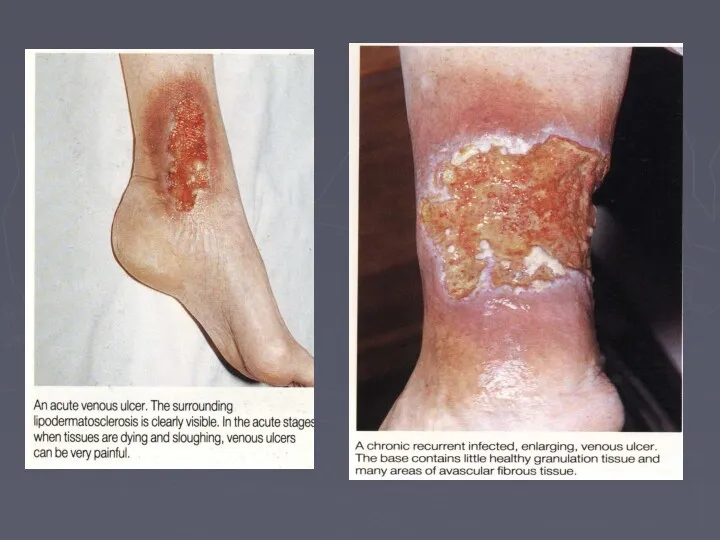
- 66. Venous Ulcer The ulcer Gaiter area lower leg (medial lower 1/3) edge sloping and pale purple-blue
- 68. LSV CVI Ankle flare LSV CVI Ankle flare
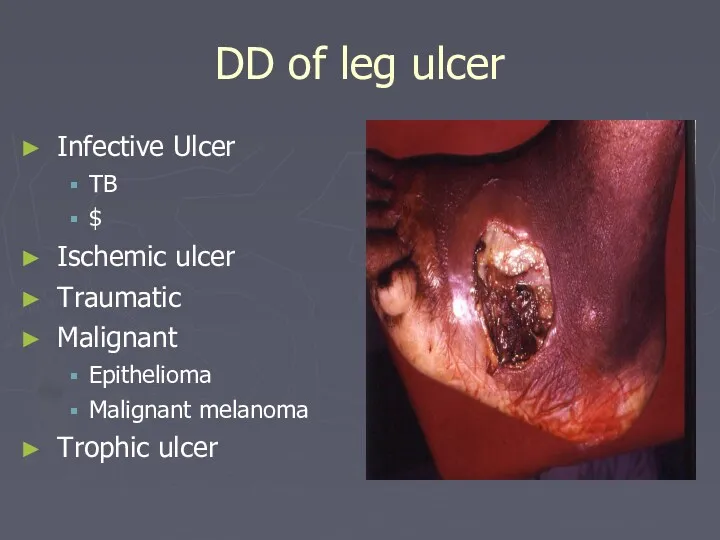
- 73. DD of leg ulcer Infective Ulcer TB $ Ischemic ulcer Traumatic Malignant Epithelioma Malignant melanoma Trophic
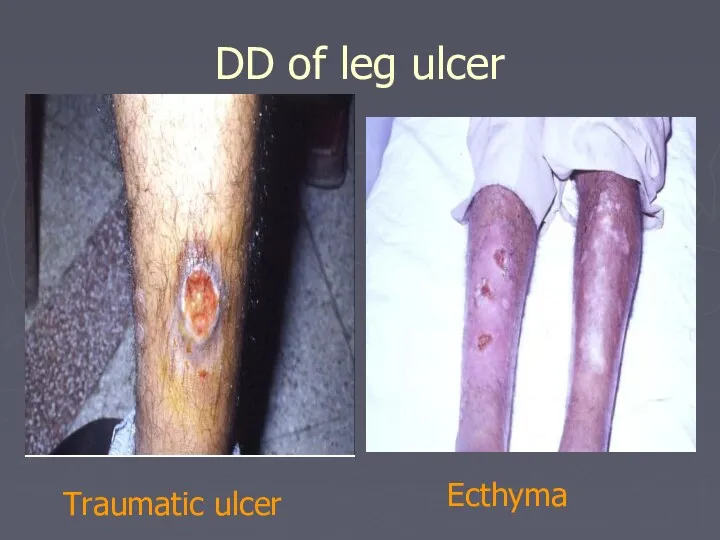
- 74. DD of leg ulcer Traumatic ulcer Ecthyma
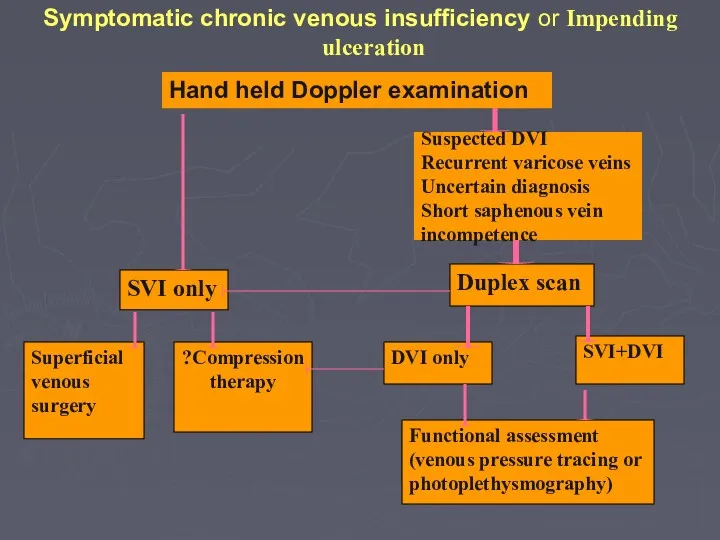
- 75. Symptomatic chronic venous insufficiency or Impending ulceration Hand held Doppler examination SVI only Superficial venous surgery
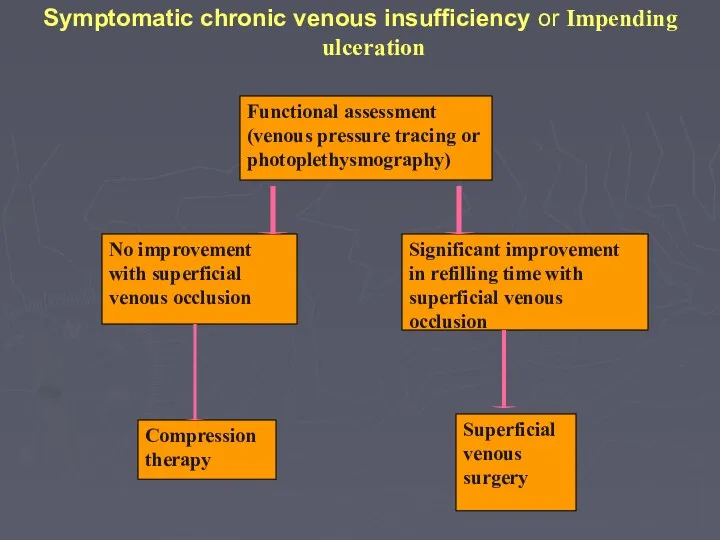
- 76. Symptomatic chronic venous insufficiency or Impending ulceration Compression therapy Functional assessment (venous pressure tracing or photoplethysmography)
- 77. Conservative Treatment Bisgaar method: Elevation, bandaging, exercises and massage. Compression bandaging: multilayer bandaging for several weeks
- 78. Surgical Treatment Ligation and division of incompetent perforating veins to prevent hydrodynamic forces generated in the
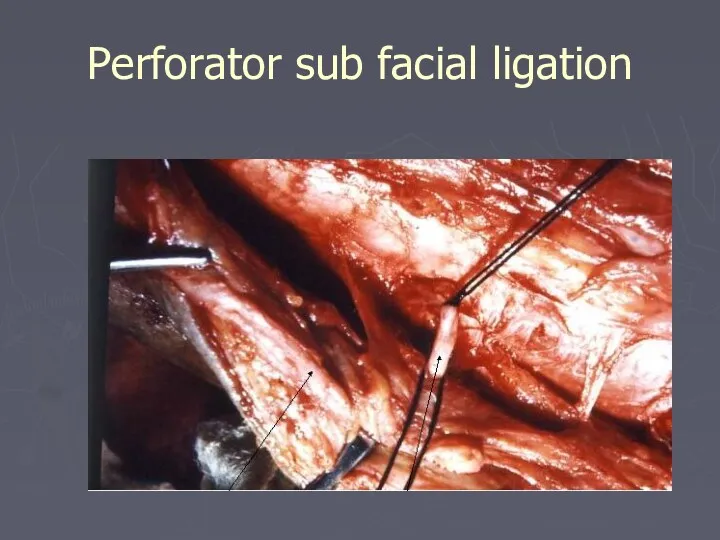
- 79. Perforator sub facial ligation
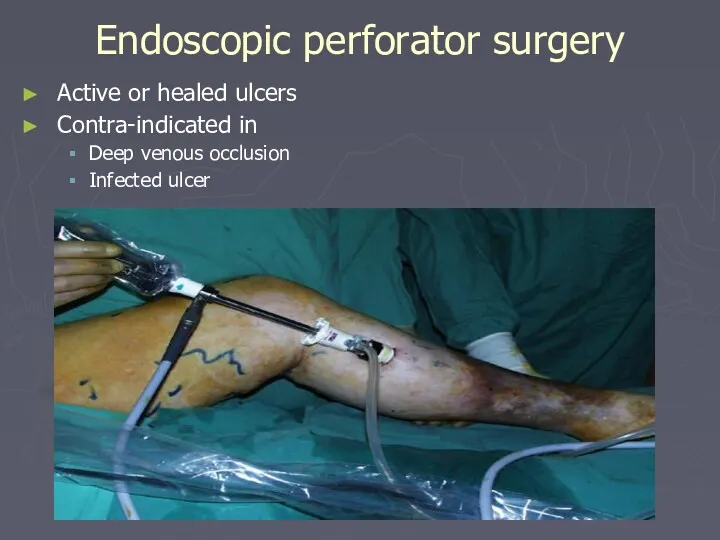
- 80. Endoscopic perforator surgery Active or healed ulcers Contra-indicated in Deep venous occlusion Infected ulcer
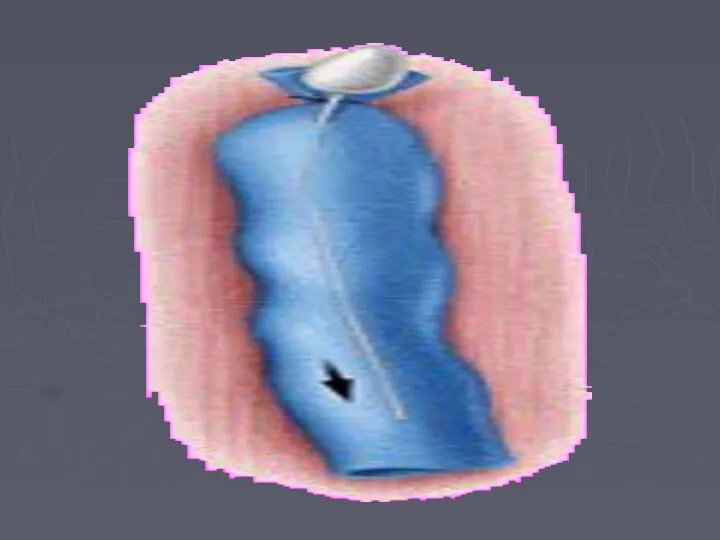
- 81. Treatment Deep venous reconstruction Not yet standard treatment Can correct primary deep veins reflux but not
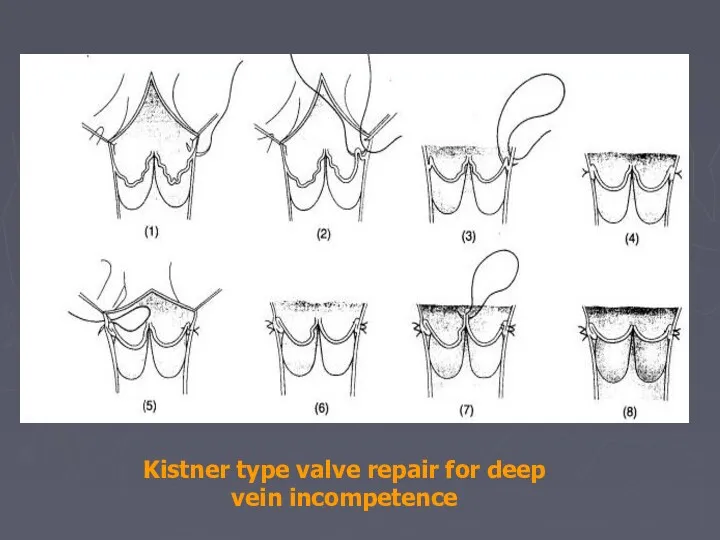
- 82. Kistner type valve repair for deep vein incompetence
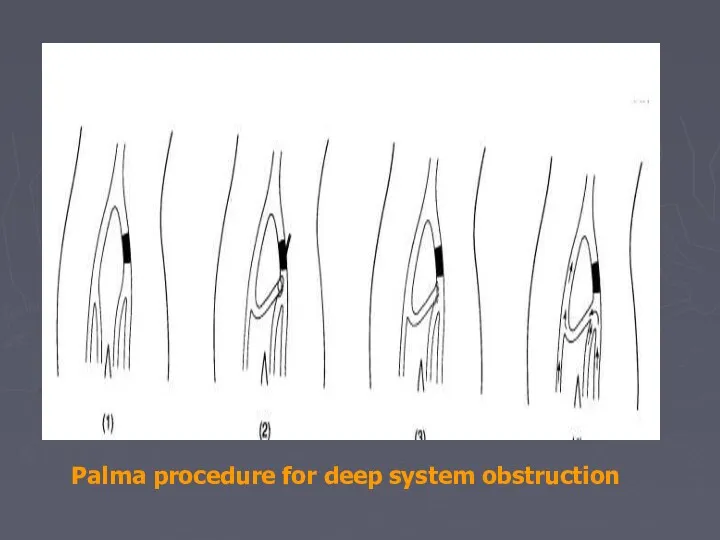
- 83. Palma procedure for deep system obstruction
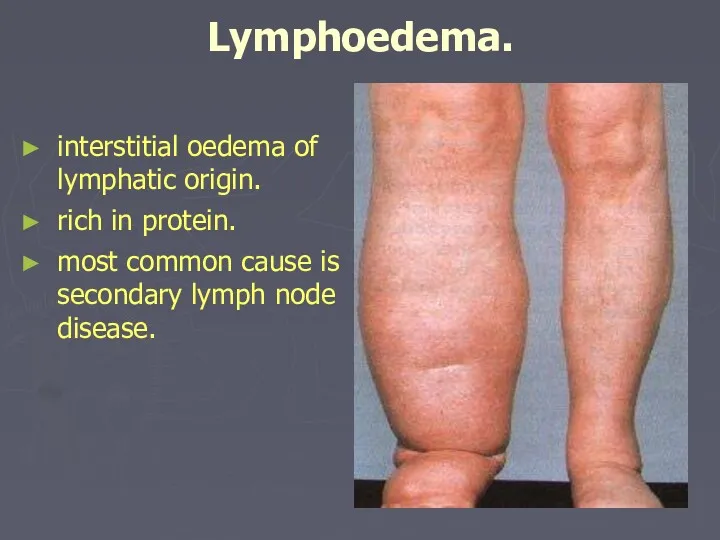
- 84. Lymphoedema. interstitial oedema of lymphatic origin. rich in protein. most common cause is secondary lymph node
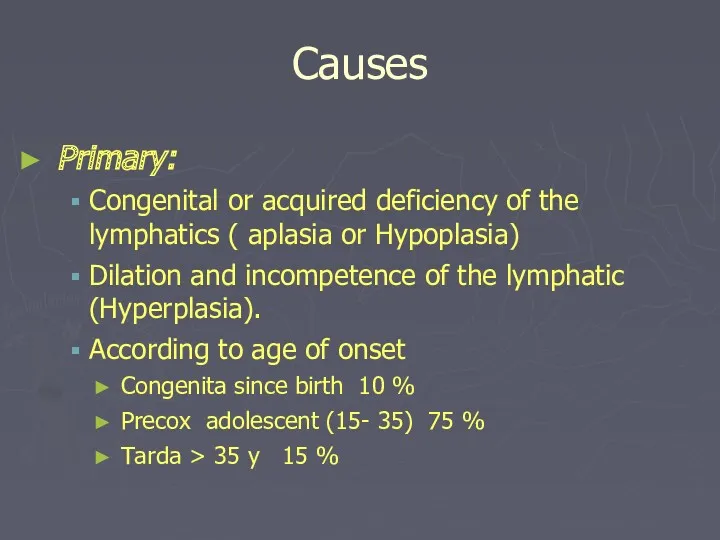
- 85. Causes Primary: Congenital or acquired deficiency of the lymphatics ( aplasia or Hypoplasia) Dilation and incompetence
- 86. Causes Secondary: Neoplastic infiltration of lymph nodes. secondary carcinoma Primary reticuloses. Infection Filariasis (parasite Wuchereria bancrofti)
- 87. Clinical Classification Sub clinical with histological abnormalities of LN and lymphatic Grade I Oedema pit on
- 88. Lymphoedema. History. females>males. slowly progressive swelling of the limb or genitelia. lower limb most often affected
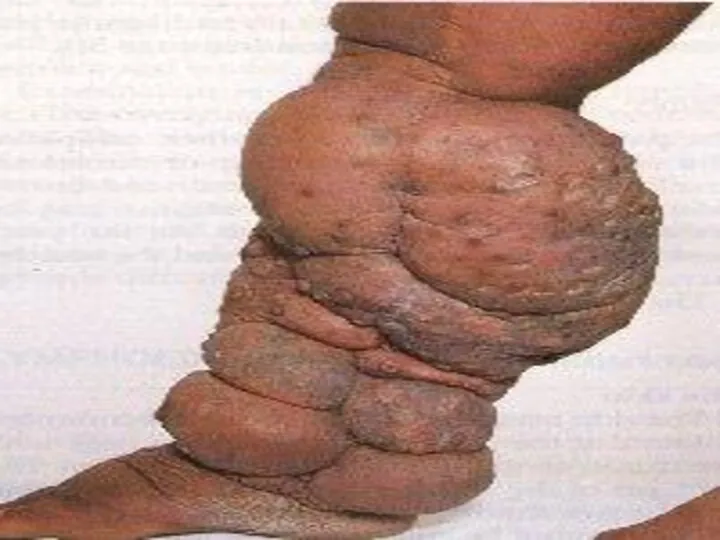
- 89. Examination. oedema all oedema pits (clasically sayed to be non-pitting). lymphoedema of the lower limb affect
- 90. Examination. In advanced cases Chronic eczema Fungal skin infection ( Dermatophtosis) Fungal nail infection ( Dermatomycosis)
- 92. Investigation Laboratory Pathology Radiology Contrast lymphangiography Isotope lymphangiography CT scan MRI
- 93. Management: goals of treatment is to control the oedema and to prevent recurrent infection. early treatment
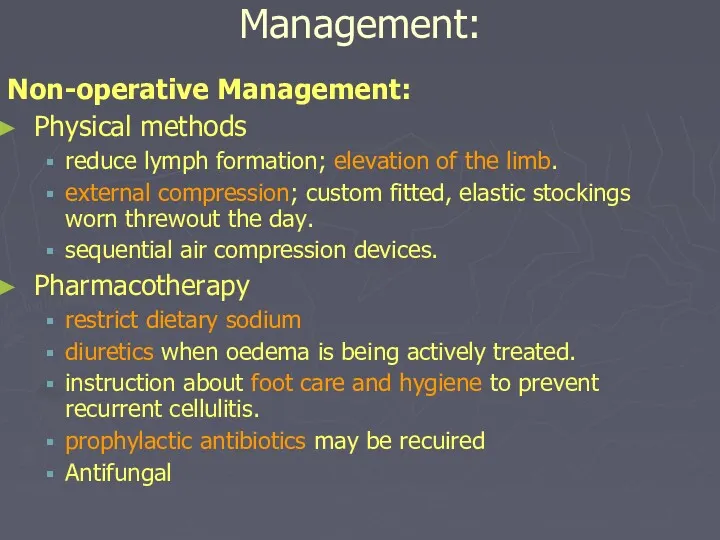
- 94. Management: Non-operative Management: Physical methods reduce lymph formation; elevation of the limb. external compression; custom fitted,
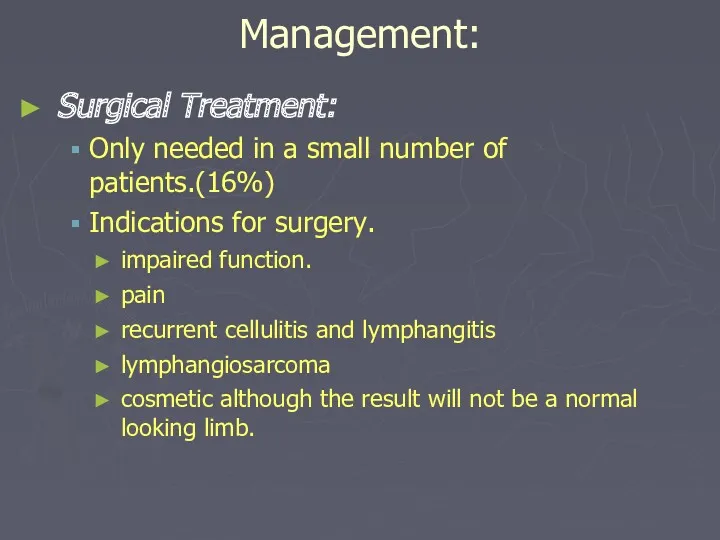
- 95. Management: Surgical Treatment: Only needed in a small number of patients.(16%) Indications for surgery. impaired function.
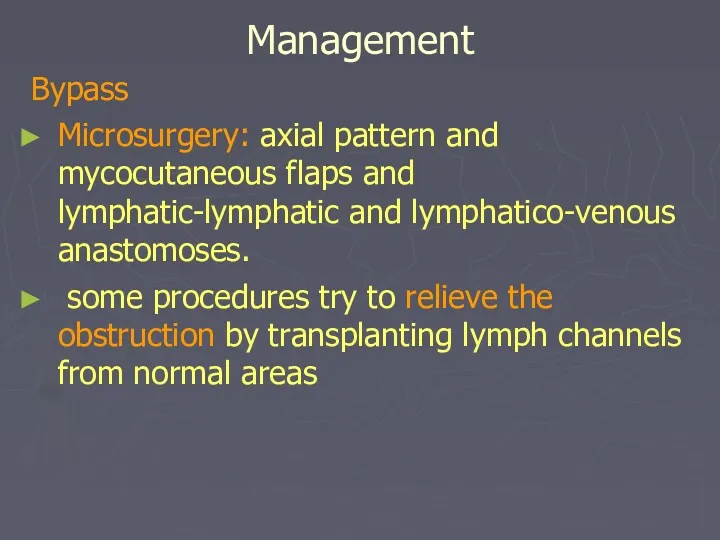
- 96. Management Bypass Microsurgery: axial pattern and mycocutaneous flaps and lymphatic-lymphatic and lymphatico-venous anastomoses. some procedures try
- 98. Скачать презентацию




 Тыныс алудың маңызы. Тыныс алу мүшелері көмей бронхылар кеңірдек
Тыныс алудың маңызы. Тыныс алу мүшелері көмей бронхылар кеңірдек Металды қалыпталған сауытты дайындауда қолданылатын болат маркасы
Металды қалыпталған сауытты дайындауда қолданылатын болат маркасы Средства, влияющие на Н-холинорецепторы. Н-холиномиметики. Ганглиоблокаторы. Миорелаксанты периферического действия (Лекция 5)
Средства, влияющие на Н-холинорецепторы. Н-холиномиметики. Ганглиоблокаторы. Миорелаксанты периферического действия (Лекция 5) Особенности фармакокинетики и фармакотерапии в неонатальном периоде
Особенности фармакокинетики и фармакотерапии в неонатальном периоде Острые промиелоцитарные лейкозы
Острые промиелоцитарные лейкозы Журектiн аускультациясы патологияда
Журектiн аускультациясы патологияда Промывание желудка
Промывание желудка Осложнения желудочно-кишечного тракта внутриутробного развития
Осложнения желудочно-кишечного тракта внутриутробного развития Продуктивное воспаление
Продуктивное воспаление 05. медичне страхування
05. медичне страхування Рестриктивные кардиомиопатии. Формы РКМП
Рестриктивные кардиомиопатии. Формы РКМП Опухоли слюнных желез
Опухоли слюнных желез Изосерологическая несовместимость крови матери и плода
Изосерологическая несовместимость крови матери и плода Болезнь Лайма
Болезнь Лайма Рак яичников
Рак яичников Введение в доказательную медицину
Введение в доказательную медицину Вплив алкоголю на дітей та підлітків
Вплив алкоголю на дітей та підлітків Дерматомиозит
Дерматомиозит Кавказские Минеральные Воды
Кавказские Минеральные Воды Профессиональная гигиена полости рта
Профессиональная гигиена полости рта Т-20С.31 янв
Т-20С.31 янв Дифференциально-диагностический поиск у пациентов с гипогликемическим синдромом
Дифференциально-диагностический поиск у пациентов с гипогликемическим синдромом Сердце, аорта, кровь, вены, капилляры
Сердце, аорта, кровь, вены, капилляры Ларингит
Ларингит Проблемы нормативного обеспечения в сфере информатизации здравоохранения
Проблемы нормативного обеспечения в сфере информатизации здравоохранения Қан айналымды зерттеу әдістері. Интегралдық және регионарлық реография. Реография
Қан айналымды зерттеу әдістері. Интегралдық және регионарлық реография. Реография Анемия у детей
Анемия у детей Клиническая характеристика больных и оказание неотложной помощи при почечной колике
Клиническая характеристика больных и оказание неотложной помощи при почечной колике