Drug allergy: the mechanisms of development, symptoms, diagnostics, and treatment. Measures preventing the drug allergy презентация
Содержание
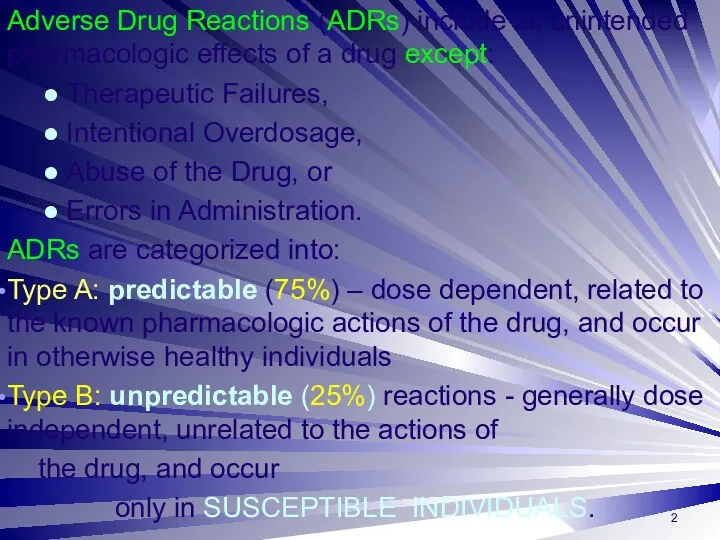
- 2. Adverse Drug Reactions (ADRs) include all unintended pharmacologic effects of a drug except: ● Therapeutic Failures,
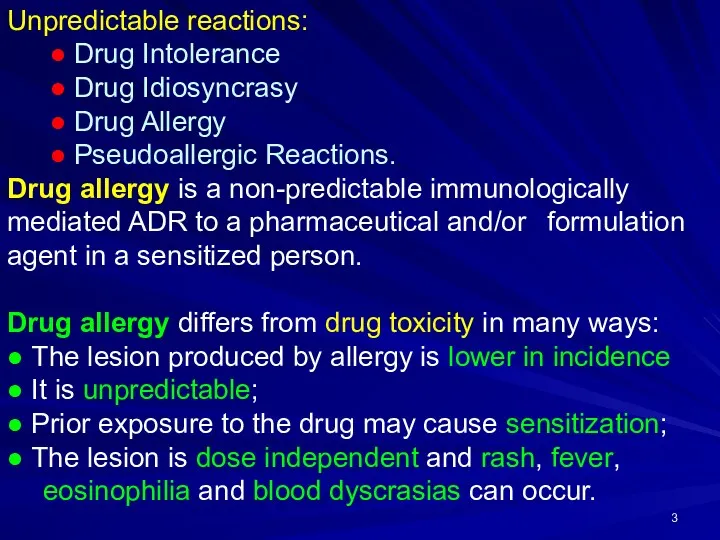
- 3. Unpredictable reactions: ● Drug Intolerance ● Drug Idiosyncrasy ● Drug Allergy ● Pseudoallergic Reactions. Drug allergy
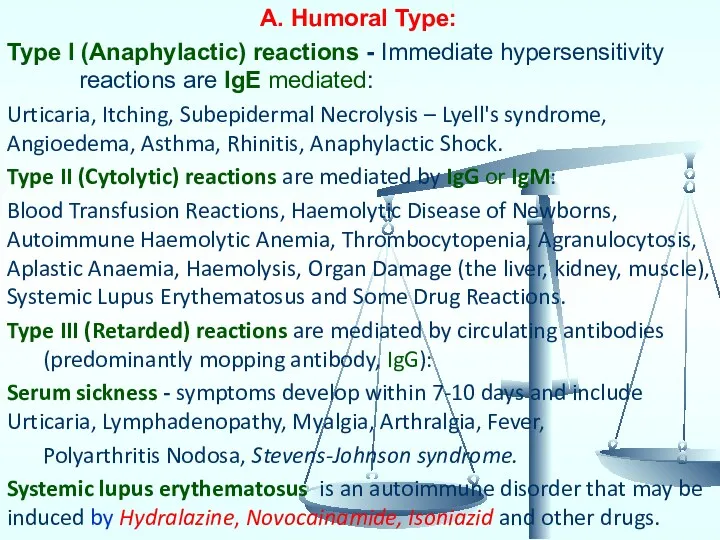
- 4. A. Humoral Type: Type I (Anaphylactic) reactions - Immediate hypersensitivity reactions are IgE mediated: Urticaria, Itching,
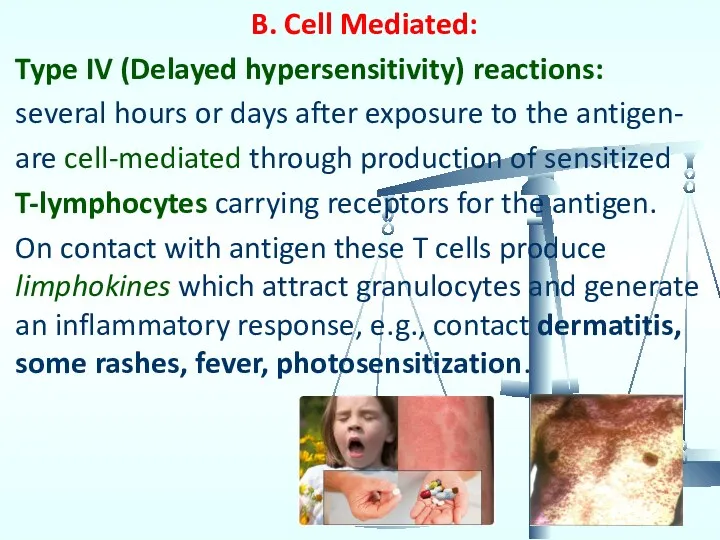
- 5. B. Cell Mediated: Type IV (Delayed hypersensitivity) reactions: several hours or days after exposure to the
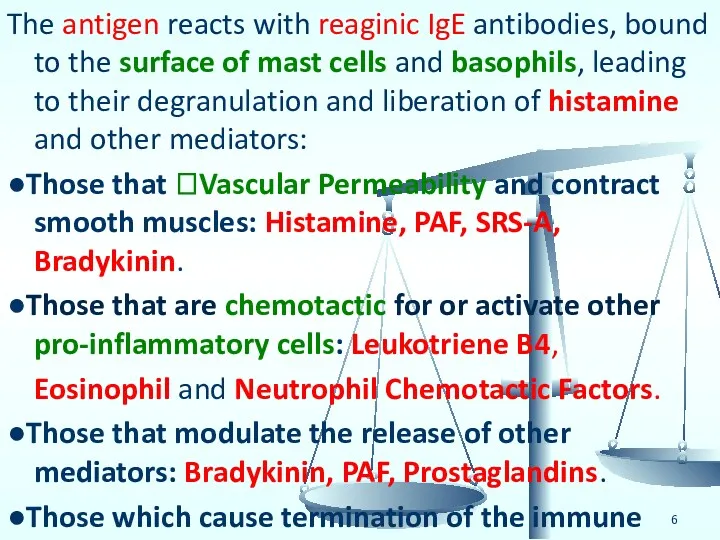
- 6. The antigen reacts with reaginic IgE antibodies, bound to the surface of mast cells and basophils,
- 7. DRUG ALLERGY The most dangerous type of ADRs. 45% reports of AR/SE of drugs in town
- 8. Allergic Anamnesis Ignoring Analgin, Aspirin, Ampicillin were administered in patients with allergic anamnesis (sometimes with other
- 9. The various subtypes of T lymphocytes (Cytotoxic, Helper and Suppressor) and their responses constitute Cell Mediated
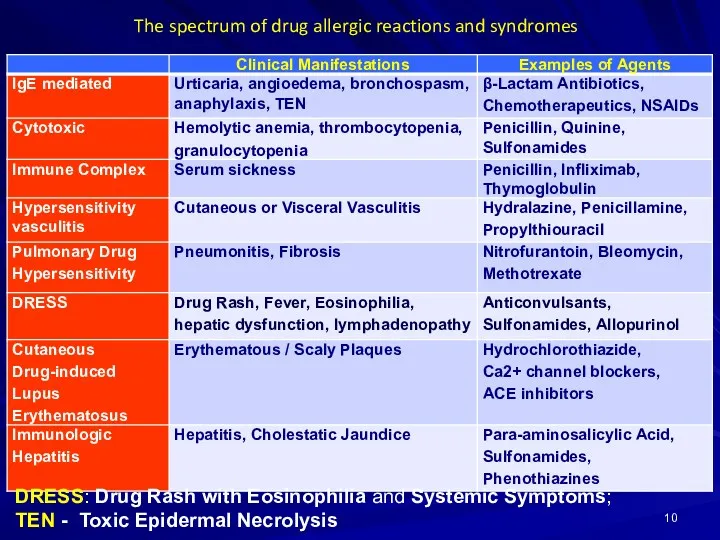
- 10. The spectrum of drug allergic reactions and syndromes DRESS: Drug Rash with Eosinophilia and Systemic Symptoms;
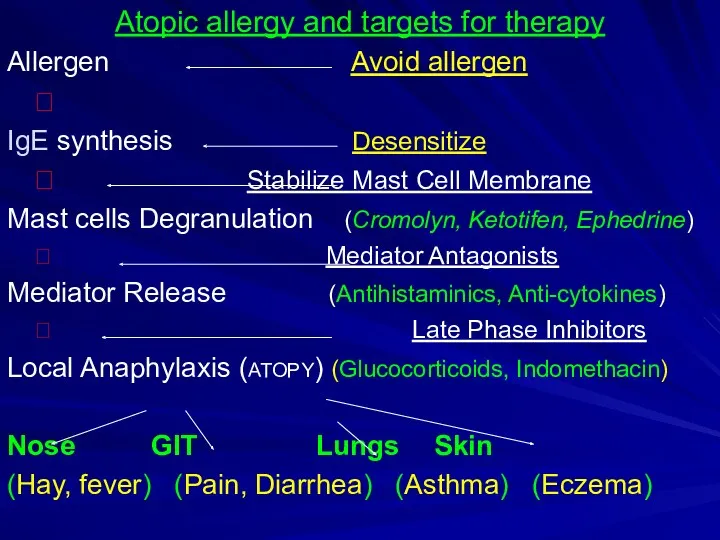
- 11. Atopic allergy and targets for therapy Allergen Avoid allergen ? IgE synthesis Desensitize ? Stabilize Mast
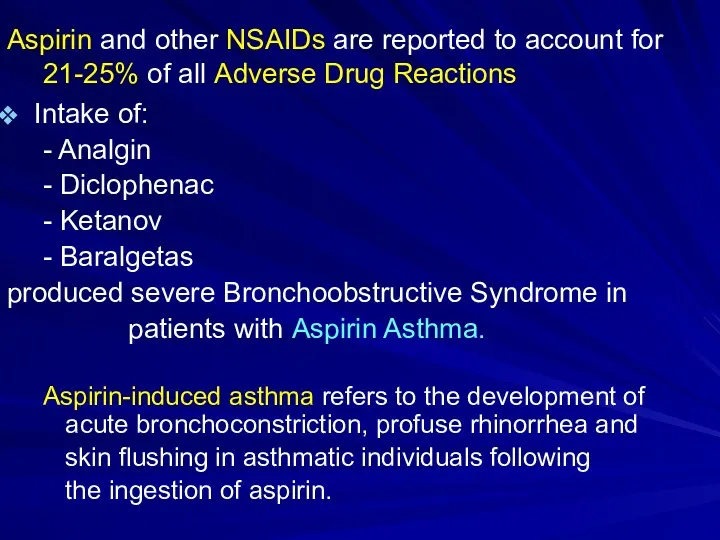
- 12. Aspirin and other NSAIDs are reported to account for 21-25% of all Adverse Drug Reactions Intake
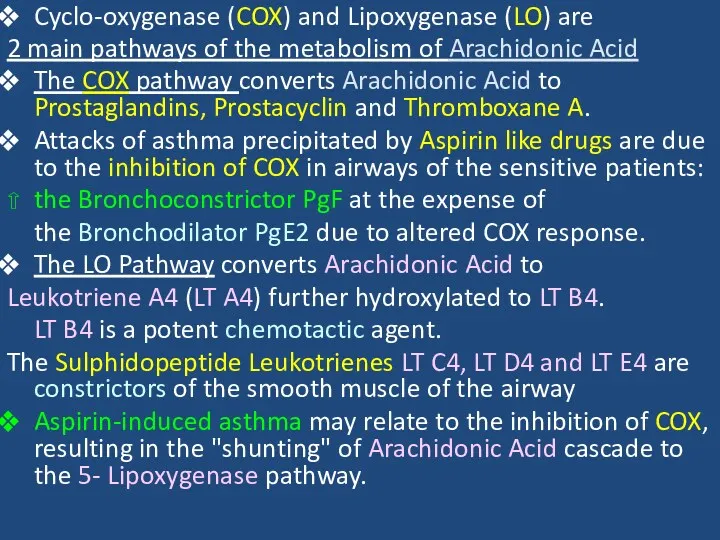
- 13. Cyclo-oxygenase (COX) and Lipoxygenase (LO) are 2 main pathways of the metabolism of Arachidonic Acid The
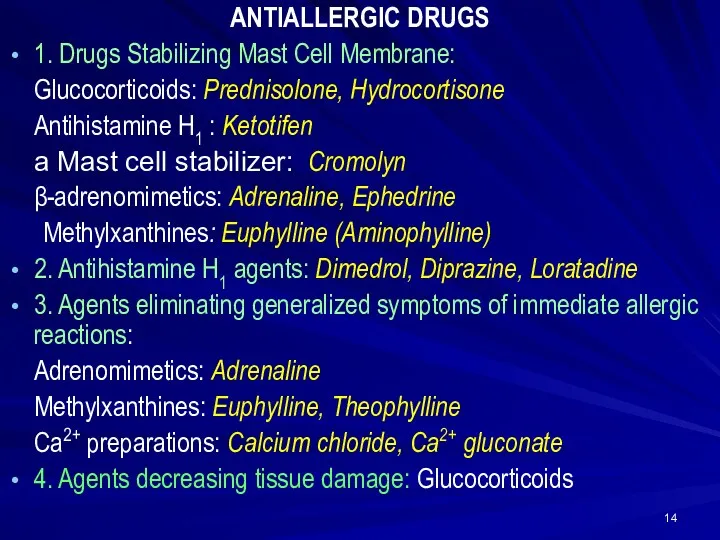
- 14. ANTIALLERGIC DRUGS 1. Drugs Stabilizing Mast Cell Membrane: Glucocorticoids: Prednisolone, Hydrocortisone Antihistamine H1 : Ketotifen a
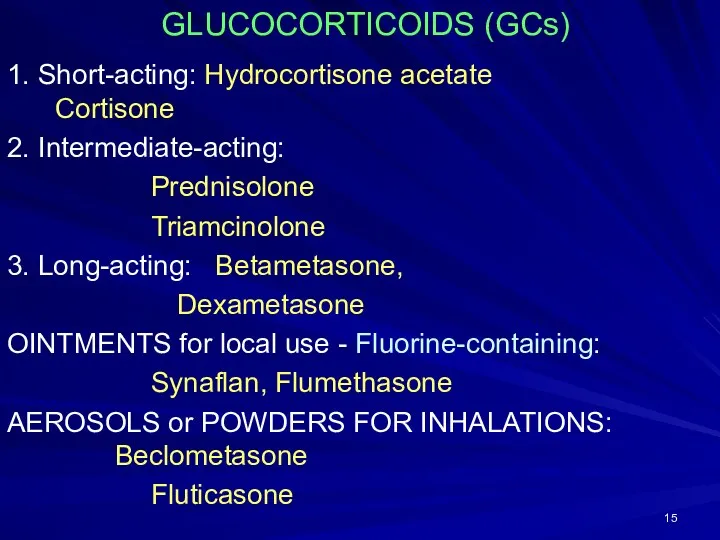
- 15. GLUCOCORTICOIDS (GCs) 1. Short-acting: Hydrocortisone acetate Cortisone 2. Intermediate-acting: Prednisolone Triamcinolone 3. Long-acting: Betametasone, Dexametasone OINTMENTS
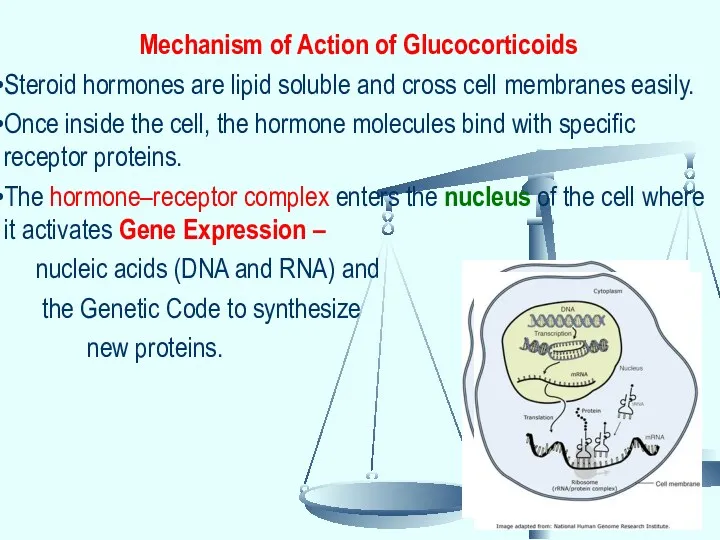
- 16. Mechanism of Action of Glucocorticoids Steroid hormones are lipid soluble and cross cell membranes easily. Once
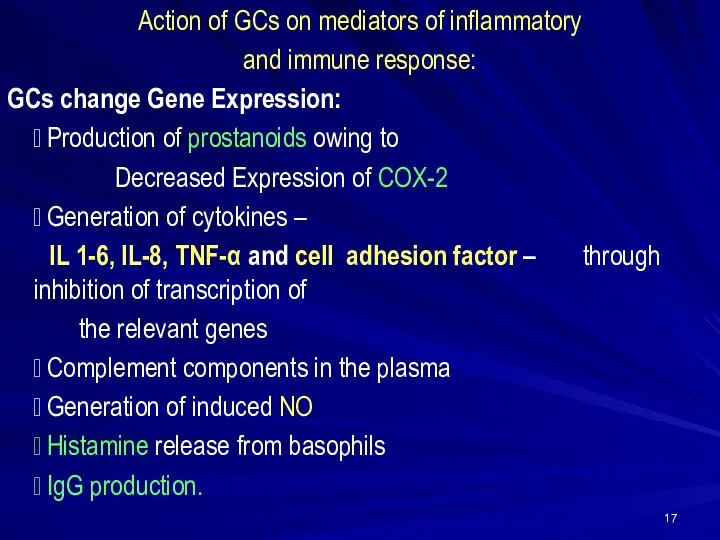
- 17. Action of GCs on mediators of inflammatory and immune response: GCs change Gene Expression: ? Production
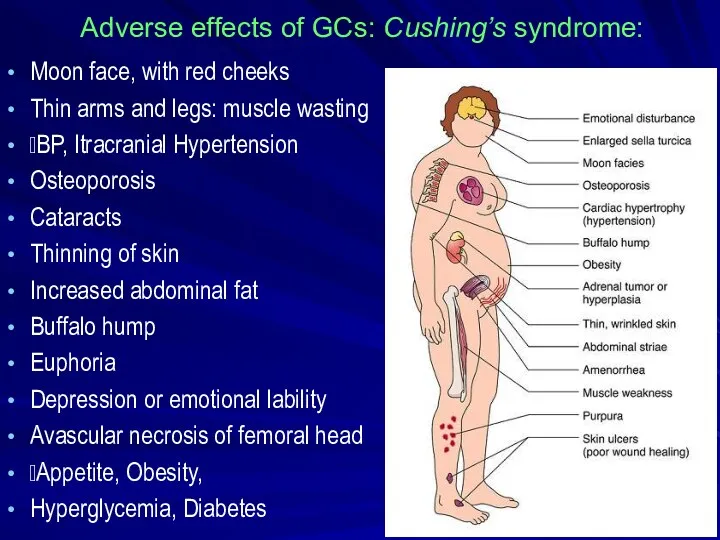
- 18. Adverse effects of GCs: Cushing’s syndrome: Moon face, with red cheeks Thin arms and legs: muscle
- 19. Cromolyn sodium (caps. 20 mg for inhalation) and Nedocromil (aerosol: 2 mg/dose) stabilize mast cells and
- 20. Ketotifen (tab. 1 mg), a cromolyn analog, is an antihistaminic (H1) and mast cell stabilizer. ●
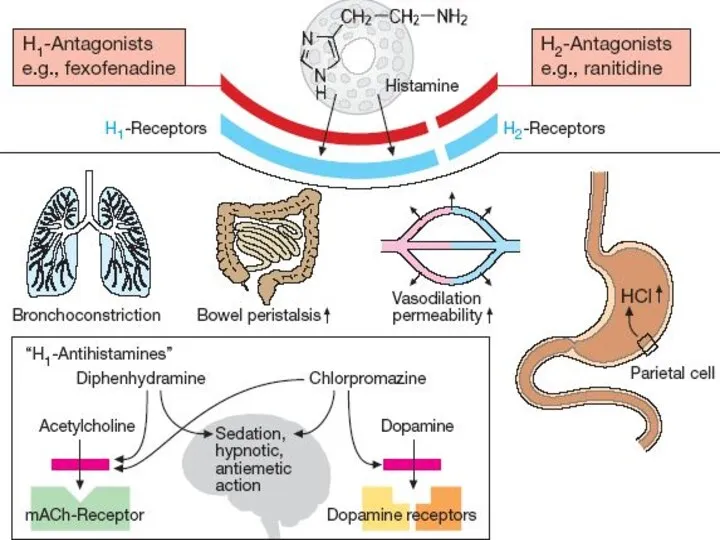
- 21. H1-Receptors: Exocrine excretion => ?Nasal and Bronchial mucus Bronchial smooth muscle constriction => bronchospasm Intestinal smooth
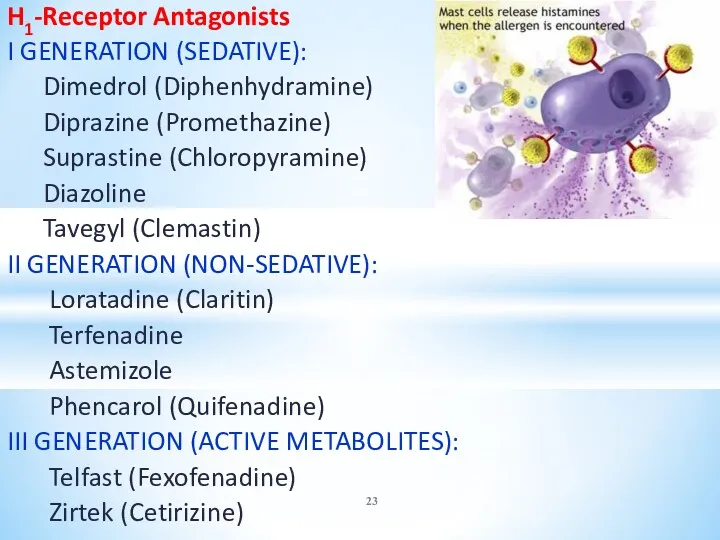
- 23. H1-Receptor Antagonists I GENERATION (SEDATIVE): Dimedrol (Diphenhydramine) Diprazine (Promethazine) Suprastine (Chloropyramine) Diazoline Tavegyl (Clemastin) II GENERATION
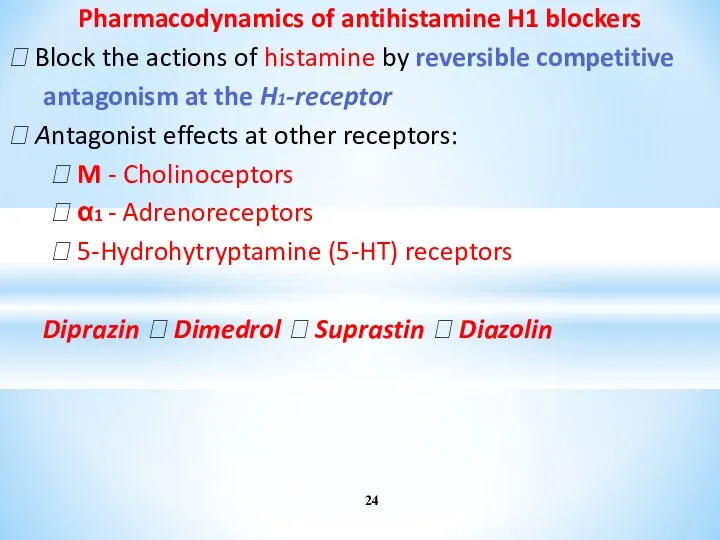
- 24. Pharmacodynamics of antihistamine H1 blockers ⮞ Block the actions of histamine by reversible competitive antagonism at
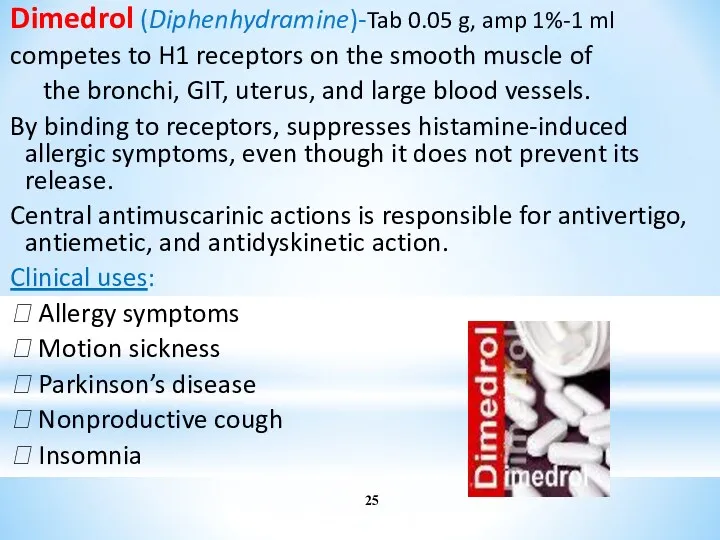
- 25. Dimedrol (Diphenhydramine)-Tab 0.05 g, amp 1%-1 ml competes to H1 receptors on the smooth muscle of
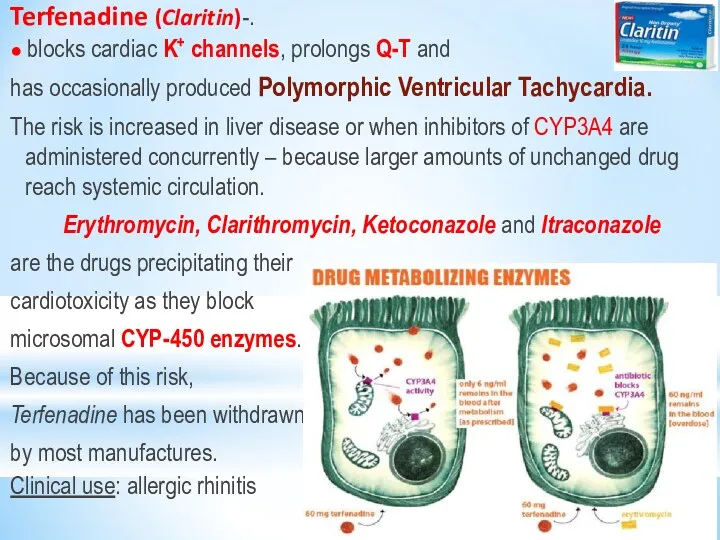
- 26. Terfenadine (Claritin)-. ● blocks cardiac K+ channels, prolongs Q-T and has occasionally produced Polymorphic Ventricular Tachycardia.
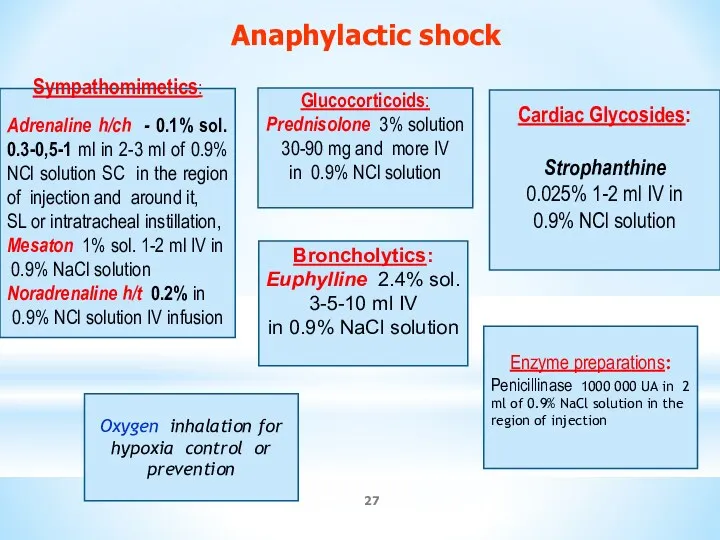
- 27. Sympathomimetics: Adrenaline h/ch - 0.1% sol. 0.3-0,5-1 ml in 2-3 ml of 0.9% NCl solution SC
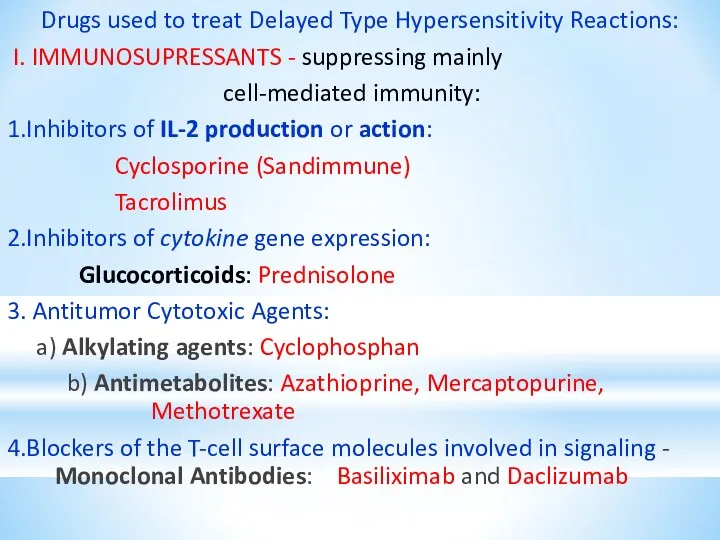
- 28. Drugs used to treat Delayed Type Hypersensitivity Reactions: I. IMMUNOSUPRESSANTS - suppressing mainly cell-mediated immunity: 1.Inhibitors
- 29. Drugs used to treat Delayed Type Hypersensitivity Reactions: II. Drugs decreasing tissue damage – 1. Glucocorticoids
- 31. Скачать презентацию
 Aims and Rationale
Aims and Rationale Рекуррентные ОРВИ в практике педиатра
Рекуррентные ОРВИ в практике педиатра Лечение шизофрении
Лечение шизофрении Международной классификации болезней (МКБ-10)
Международной классификации болезней (МКБ-10)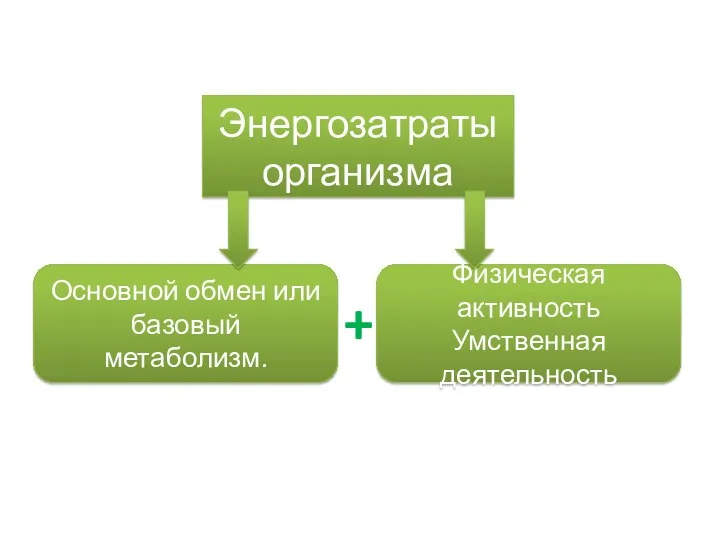 Энергозатраты организма
Энергозатраты организма Острые эндогенные психозы
Острые эндогенные психозы Эпидемиологическая ситуация по ТБ в мире и Украине
Эпидемиологическая ситуация по ТБ в мире и Украине Острый нелимфобластный лейкоз. Клинический случай
Острый нелимфобластный лейкоз. Клинический случай Неправильные положения плода. Разгибательные предлежания головки плода. Тема 6
Неправильные положения плода. Разгибательные предлежания головки плода. Тема 6 Применение левосимендана в практике кардиологической и кардиохирургической реанимации – голос За
Применение левосимендана в практике кардиологической и кардиохирургической реанимации – голос За Возбудители инфекций верхних дыхательных путей, характеризующихся специфичностью патогенеза и клинической картины
Возбудители инфекций верхних дыхательных путей, характеризующихся специфичностью патогенеза и клинической картины Электрокардиограмма при гипертрофии различных отделов миокарда
Электрокардиограмма при гипертрофии различных отделов миокарда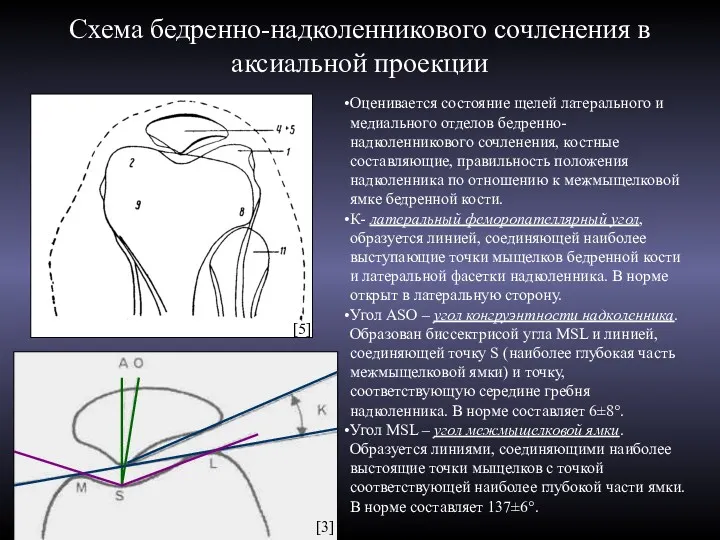 Схема бедренно-надколенникового сочленения в аксиальной проекции
Схема бедренно-надколенникового сочленения в аксиальной проекции Медицинская демография. (Лекция 4)
Медицинская демография. (Лекция 4) Профилактика врожденной патологии лица
Профилактика врожденной патологии лица Причины интеллектуальных нарушений и слабовыраженных отклонений. Классификация нарушения по степени тяжести
Причины интеллектуальных нарушений и слабовыраженных отклонений. Классификация нарушения по степени тяжести Гомеопатия
Гомеопатия Гематология анализаторлар тобы
Гематология анализаторлар тобы Медициналық аспаптарды стерилизациялау
Медициналық аспаптарды стерилизациялау Питание пациентов терапевтического профиля
Питание пациентов терапевтического профиля Медицинские приборнокомпьютерные системы (МПКС)
Медицинские приборнокомпьютерные системы (МПКС) Общая хирургическая техника. Хирургический инструментарий. Принципы местной анестезии
Общая хирургическая техника. Хирургический инструментарий. Принципы местной анестезии Жасушалық иммунитет жүйесінің негізгі қызметтері. Иммунологиялық төзімділік
Жасушалық иммунитет жүйесінің негізгі қызметтері. Иммунологиялық төзімділік Адаптаційні зміни в організмі жінки під час вагітності. Лабораторна діагностика при вагітності. Методи обстеження вагітних
Адаптаційні зміни в організмі жінки під час вагітності. Лабораторна діагностика при вагітності. Методи обстеження вагітних Адам эмбриогенезі. Дамудың қауіпті кезеңдері
Адам эмбриогенезі. Дамудың қауіпті кезеңдері Интенсивная терапия острых отравлений
Интенсивная терапия острых отравлений Заикание. Особенности течения заикания
Заикание. Особенности течения заикания Клещевой энцефалит, болезнь Лайма
Клещевой энцефалит, болезнь Лайма