Содержание
- 2. What are medical ethics? What are medical ethics? Why do we as future care professionals need
- 3. Ethics & Human Rights? Ethics, from ēthos, “practice, custom” Ethics is about doing the right thing.
- 4. Medical ethics: very complex... There are some easy guidelines and tools to tackle difficult ethical situations
- 5. Principlism Four principles Respect for autonomy (A, C) Beneficence (B) Non-maleficence (D) Justice (E,F) Specifying and
- 6. ABCDEF Principlism: as easy as ABCDEF?
- 7. A - Autonomy “Self rule” - Competent, informed patients have the right to choose among treatment
- 8. B - Beneficence Physicians must act in the best interests of their patients. Maximize health Prolong
- 9. C - Confidentiality Confidentiality respects patient autonomy. Encourages patients to be candid. Can confidentiality be overridden?
- 10. D - Do No Harm The principle of nonmaleficence directs physicians to “do no harm” to
- 11. E - Equality/Equity The principle of distributive justice deals with issues of treating patients equally. Economic
- 12. F - Fairness The principle of procedural justice requires that the process for making decisions for
- 13. ABCDE A - Autonomy B - Beneficence C - Confidentiality D - Do no harm E
- 14. ABCDEF Medical ethics: really as easy as ABCDEF?
- 15. Principlism Individualist approach Focus on autonomy, privacy and confidentiality Patients are seen as individuals Self-determination Privacy
- 16. Care ethics Relational approach Context and interpretation, sharing and negotiation of responsibilities Patients are seen as
- 17. Care ethics Origin: feminist critique in the 1980’s Basic ideas: All individuals are interdependent for achieving
- 18. Hermeneutic/Dialogical Ethics hermēneuein: to interpret Meaning is related to lived experience Understanding is always partial and
- 19. Tools Principles, values and virtues
- 20. To summarize ABCDEF: easy tool to medical ethics But in practice: way more complex and many
- 21. Ethics in medical research video!
- 22. Ethical medical research The Helsinki declaration (2013) ETHICAL PRINCIPLES FOR MEDICAL RESEARCH INVOLVING HUMAN SUBJECTS Article
- 23. Ethical medical research (1) value (2) scientific validity (3) fair subject selection (4) favorable risk-benefit ratio—
- 24. Ethical medical research → Exploitation Community exploitation vs. individual exploitation Exploitation: unfairness in distribution of benefits
- 25. Ethical medical research Are the risks/benefits fair for both sides? Individual benefits =/ community benefits Why
- 26. Cases Values Virtues Process Outcome Reflection
- 28. Скачать презентацию




 Узкий таз в современном акушерстве. (Лекция 18)
Узкий таз в современном акушерстве. (Лекция 18) Общие принципы интенсивной терапии острой дыхательной недостаточности
Общие принципы интенсивной терапии острой дыхательной недостаточности Вторичная профилактика инволюционной депрессии
Вторичная профилактика инволюционной депрессии Здоровье - наше богатство
Здоровье - наше богатство Эктопротездер
Эктопротездер Группы крови. Гемостаз
Группы крови. Гемостаз Профессиональная гигиена полости рта
Профессиональная гигиена полости рта Гломерулонефриты. Этиопатогенез, клиника, диагностика, лечение
Гломерулонефриты. Этиопатогенез, клиника, диагностика, лечение Семейные школы сахарного диабета и артериальной гипертонии: опыт работы
Семейные школы сахарного диабета и артериальной гипертонии: опыт работы Кинезитерапия при муковисцидозе
Кинезитерапия при муковисцидозе Боль в спине
Боль в спине Фармакотерапия гастро-эзофагеальной рефлюксной болезни
Фармакотерапия гастро-эзофагеальной рефлюксной болезни Сестринский процесс в ортопедической стоматологии
Сестринский процесс в ортопедической стоматологии Ахметбекова Жаухар 106
Ахметбекова Жаухар 106 Наследственные гемолитические анемии
Наследственные гемолитические анемии Синдром кашля в работе врача общей практики
Синдром кашля в работе врача общей практики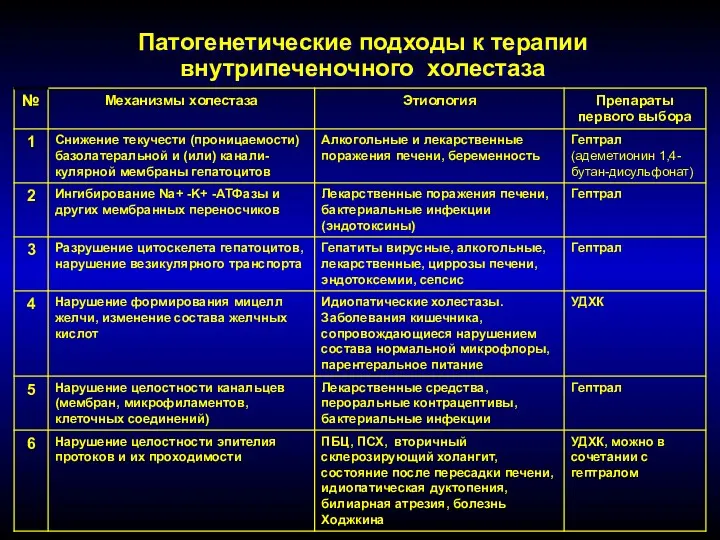 Патогенетические подходы к терапии внутрипеченочного холестаза
Патогенетические подходы к терапии внутрипеченочного холестаза Anomalii_refraktsii_dalnozorkost_blizorukost_astigmatizm
Anomalii_refraktsii_dalnozorkost_blizorukost_astigmatizm Обезболивание и его виды
Обезболивание и его виды Лечебное питание при инфекционных заболеваниях и аллергических реакциях
Лечебное питание при инфекционных заболеваниях и аллергических реакциях О порядке оказания медицинской помощи беременным, роженицам и родильницам на время пандемии COVID-19
О порядке оказания медицинской помощи беременным, роженицам и родильницам на время пандемии COVID-19 Слухопротезирование и его значение для обучения и воспитания. Рекомендации по привыканию к слуховому аппарату
Слухопротезирование и его значение для обучения и воспитания. Рекомендации по привыканию к слуховому аппарату Малые инфекции и корь у детей. Ангинозные инфекции. Менингококковая инфекция. Этиология, эпидемиология, клинические проявления
Малые инфекции и корь у детей. Ангинозные инфекции. Менингококковая инфекция. Этиология, эпидемиология, клинические проявления Материаловедение медицинских и фармацевтических товаров
Материаловедение медицинских и фармацевтических товаров Транспортировка больных и пострадавших
Транспортировка больных и пострадавших Тіс пульпасының анатомиясы, гистологиясы, физиологиясы, қызметтері
Тіс пульпасының анатомиясы, гистологиясы, физиологиясы, қызметтері Репродуктивне здоров’я молоді
Репродуктивне здоров’я молоді Отчет главного врача ГАУЗ СО ГБ г. Асбест Брагина Игоря Вячеславовича
Отчет главного врача ГАУЗ СО ГБ г. Асбест Брагина Игоря Вячеславовича