Содержание
- 2. Causes of inflammation Exogenous Infectious factors Exogenous Non-infectious factors: physical chemical biological Endogenous products of tissue
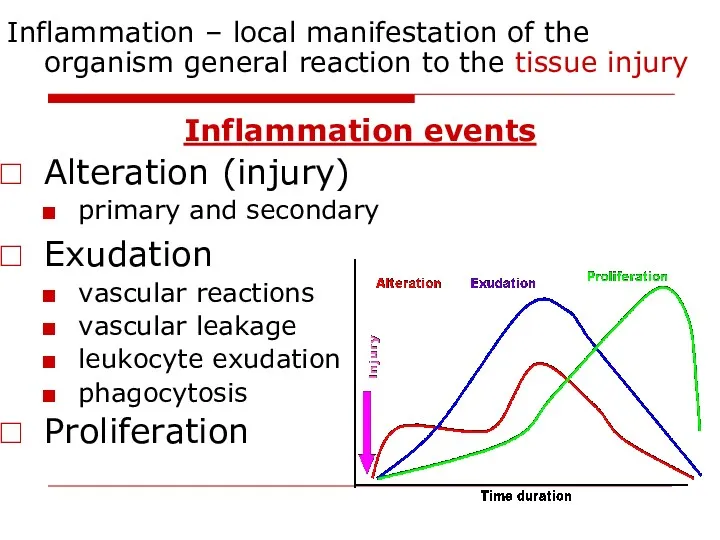
- 3. Inflammation – local manifestation of the organism general reaction to the tissue injury Inflammation events Alteration
- 4. Signs of inflammation Local: Calor - heat Rubor - redness Dolor - pain Tumor - swelling
- 5. Alteration Primary alteration - direct action of pathogenic factor (functional and structural injury of the cells)
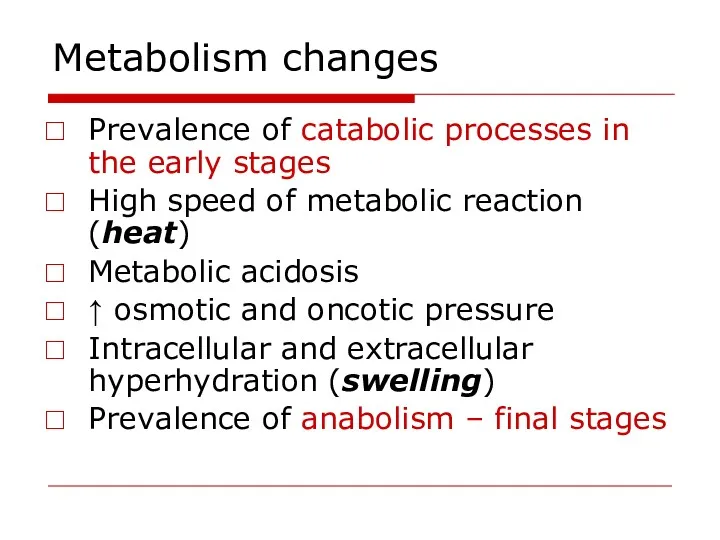
- 6. Metabolism changes Prevalence of catabolic processes in the early stages High speed of metabolic reaction (heat)
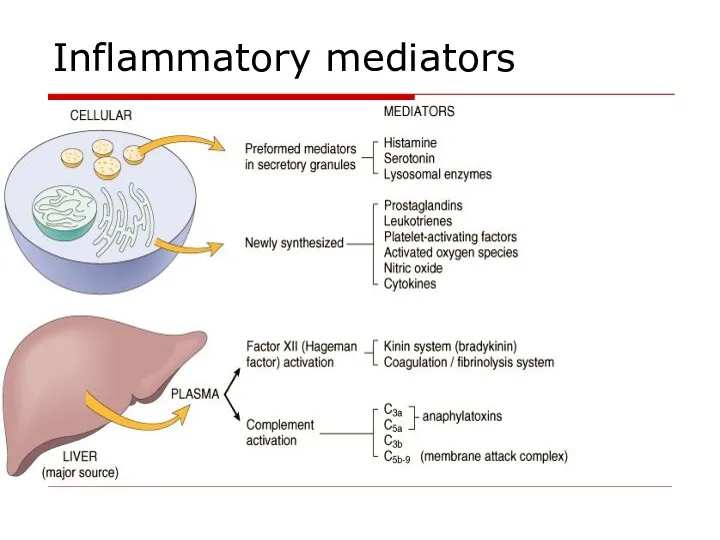
- 7. Inflammatory mediators
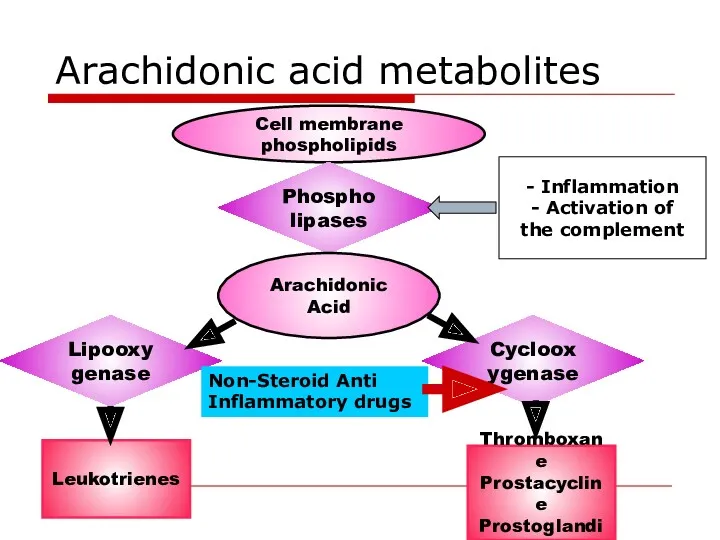
- 8. Arachidonic acid metabolites Cell membrane phospholipids Phospholipases Arachidonic Acid Lipooxygenase Cyclooxygenase Leukotrienes Thromboxane Prostacycline Prostoglandins -
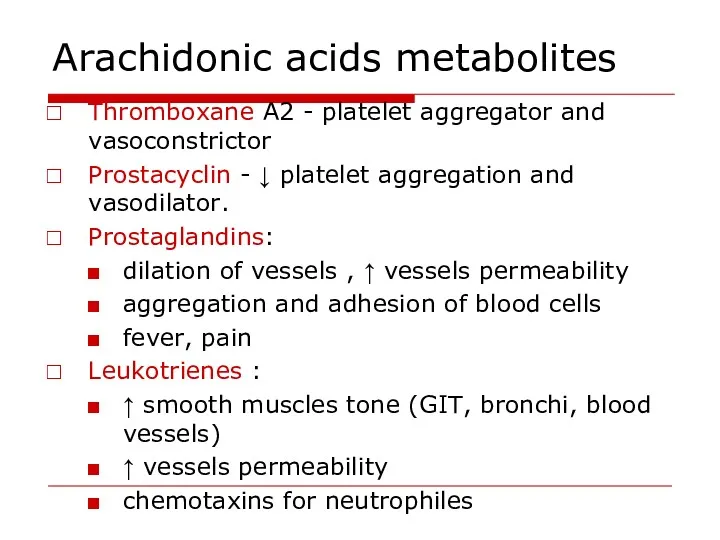
- 9. Arachidonic acids metabolites Thromboxane A2 - platelet aggregator and vasoconstrictor Prostacyclin - ↓ platelet aggregation and
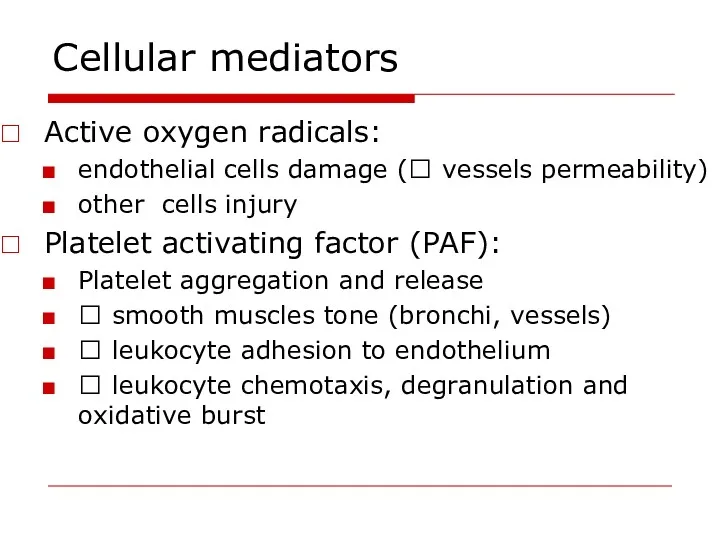
- 10. Cellular mediators Active oxygen radicals: endothelial cells damage (? vessels permeability) other cells injury Platelet activating
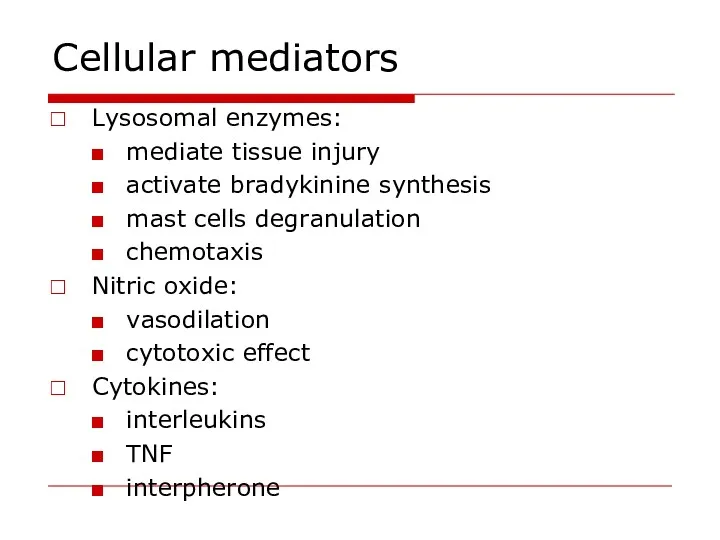
- 11. Cellular mediators Lysosomal enzymes: mediate tissue injury activate bradykinine synthesis mast cells degranulation chemotaxis Nitric oxide:
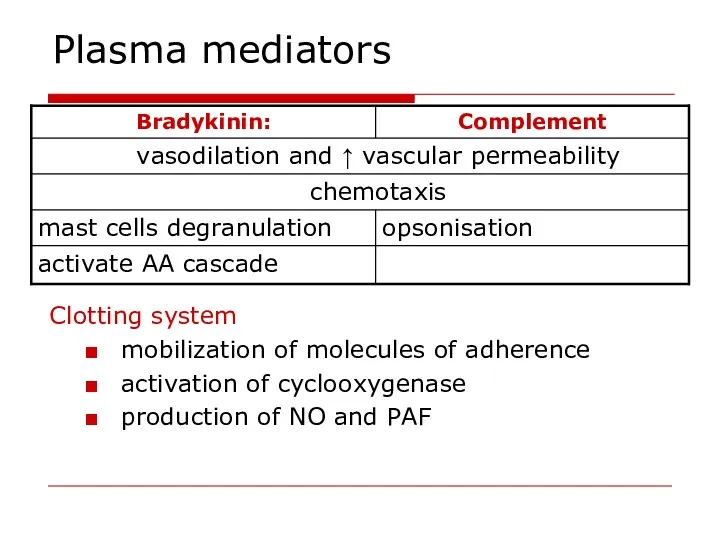
- 12. Plasma mediators Clotting system mobilization of molecules of adherence activation of cyclooxygenase production of NO and
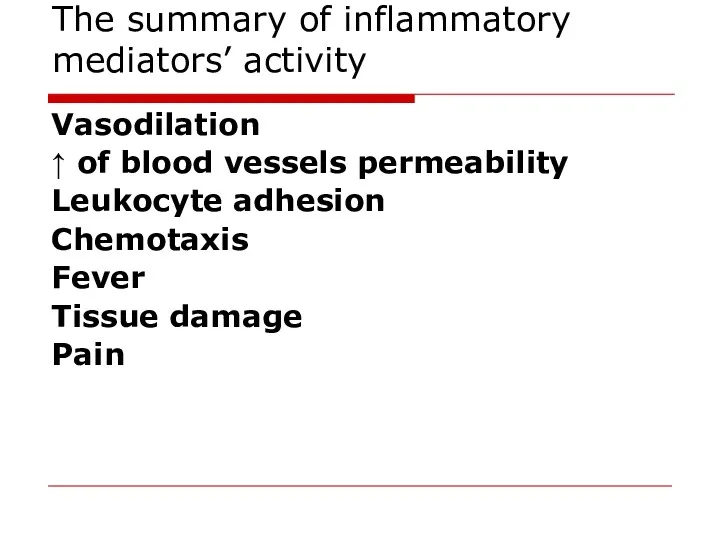
- 13. The summary of inflammatory mediators’ activity Vasodilation ↑ of blood vessels permeability Leukocyte adhesion Chemotaxis Fever
- 14. Changes in vascular flow Arterioles constriction (activation of sympathetic nerves, mediators influence) -localization of injuring agent
- 15. Changes in vascular flow Venous hyperemia and pre-stasis (dilation of venules and post-capillaries): increased blood viscosity
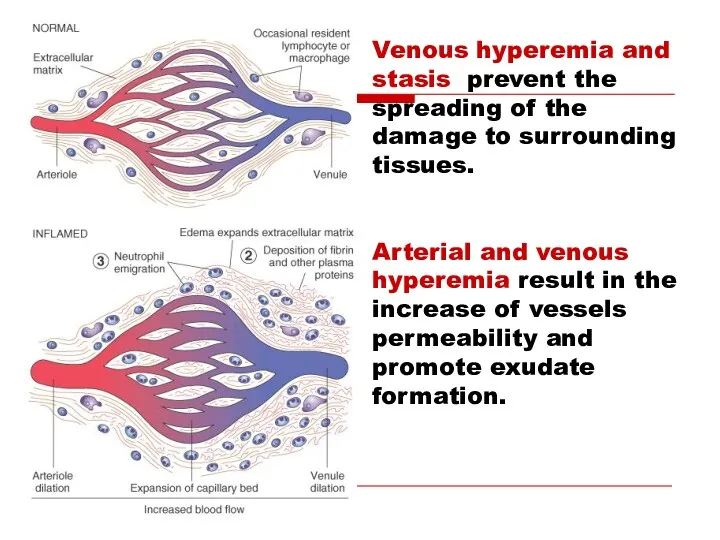
- 16. Venous hyperemia and stasis prevent the spreading of the damage to surrounding tissues. Arterial and venous
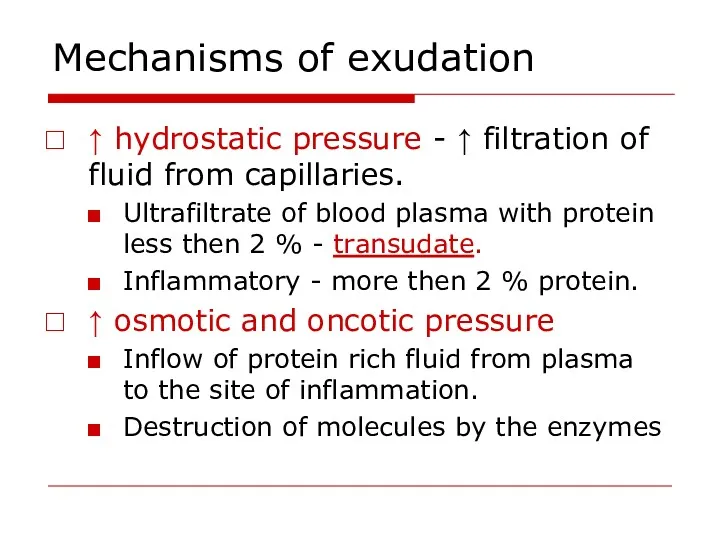
- 17. Mechanisms of exudation ↑ vascular permeability (vascular leakage). ↑ intravascular hydrostatic pressure ↑ osmotic and oncotic
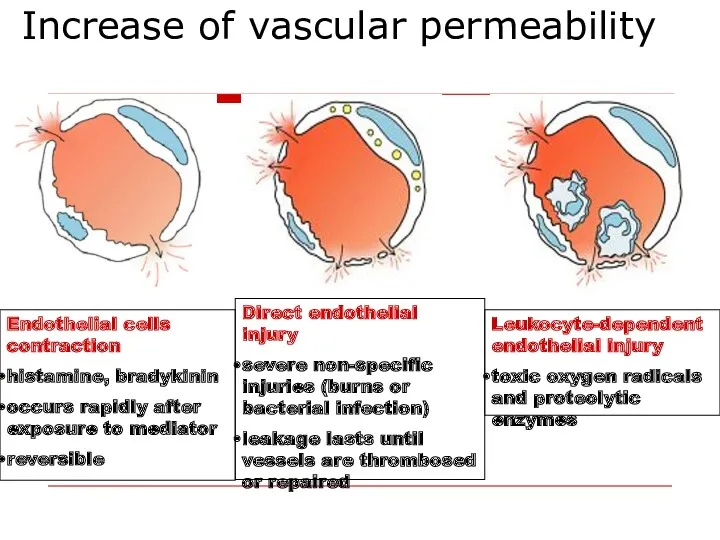
- 18. Increase of vascular permeability Endothelial cells contraction histamine, bradykinin occurs rapidly after exposure to mediator reversible
- 19. Mechanisms of exudation ↑ hydrostatic pressure - ↑ filtration of fluid from capillaries. Ultrafiltrate of blood
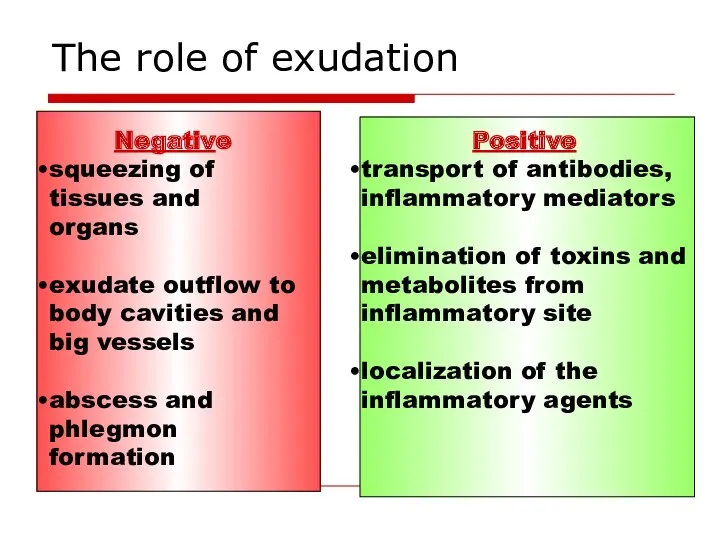
- 20. The role of exudation Negative squeezing of tissues and organs exudate outflow to body cavities and
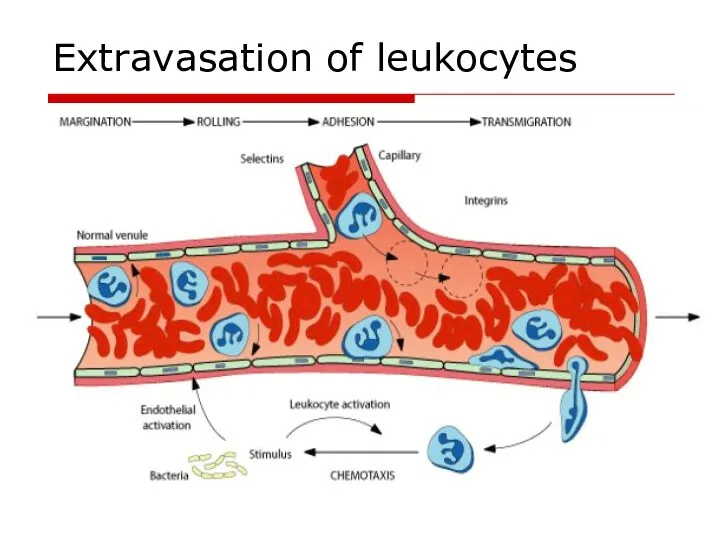
- 21. Extravasation of leukocytes
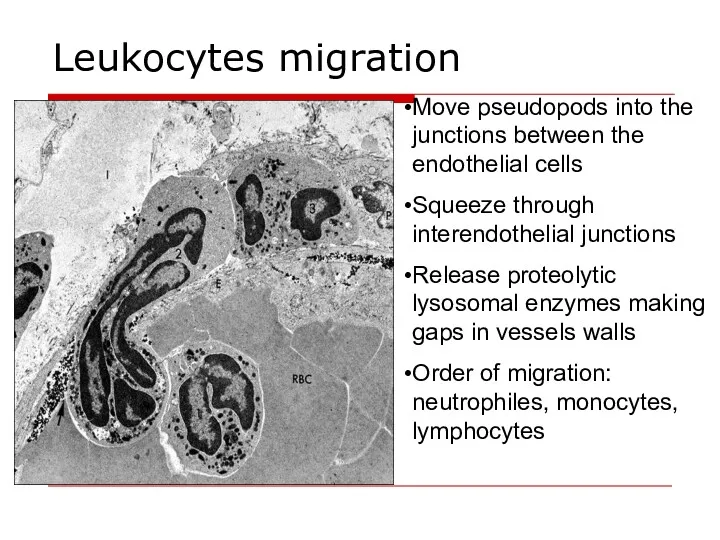
- 22. Leukocytes migration Move pseudopods into the junctions between the endothelial cells Squeeze through interendothelial junctions Release
- 23. Chemotaxis Chemotactic agents: bacterial membrane lipopolysaccharides components of the complement (3b, 5a,5b,6,7 leukotrienes products of tissue
- 24. Leukocytes role in inflammation Protective function – phagocytosis. Synthesis and secretion of inflammatory mediators. Processing and
- 25. Stages of phagocytosis Chemotaxis 2. Adherence (opsonins - IgM, IgG, C3b) 3. Phagosome formation 4. Killing
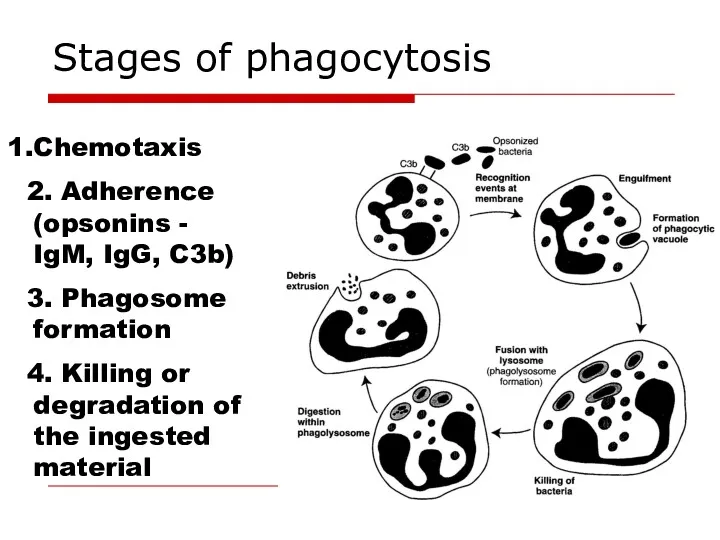
- 26. Two mechanisms of bacterial killing Oxygen-dependent mechanism reactive oxygen species – superoxide anion, hydroxyl ion, hydroperoxide
- 27. Proliferation in inflammation Regeneration - replacement of dead cells with new ones; the function is restored.
- 28. The steps of repair Phagocytosis Proliferation of endothelial cells and fibroblasts in the damaged area. The
- 29. Factors influencing proliferation Local: Persisting infection, foreign material Inadequate blood supply Excessive movement Irradiation Systemic: Age
- 30. Classification of inflammation Classification based on the cause of inflammation: Infectious: non-specific (cocci) and specific (tuberculosis,
- 31. Classification of inflammation Classification based on the prevailing mechanism: Alterative –prevailing alteration develops in parenchymal organs
- 32. Types of exudative inflammation Serous inflammation - 3-8% of protein, single neutrophiles in exudate. Catarrhal inflammation
- 33. Types of exudative inflammation Purulent (suppurative) inflammation production of pus - pyogenic bacteria (staphylococci). Abscesses are
- 34. Neural and hormonal control of inflammation Pro-inflammatory hormones - growth hormone, mineralocorticoids Glucocorticoids, catecholamines - anti-inflammatory
- 35. Inflammation outcomes Complete resolution - the injury is limited Healing by scarring – impossibility of regeneration
- 37. Скачать презентацию
 Пневмония. Пневмония жіктелуі
Пневмония. Пневмония жіктелуі Основные принципы современной химиотерапии злокачественных опухолей
Основные принципы современной химиотерапии злокачественных опухолей Эпидемиялық процестің әртүрлі халық топтары арасындағы көрінуінің қазіргі кездегі сипаттамасы
Эпидемиялық процестің әртүрлі халық топтары арасындағы көрінуінің қазіргі кездегі сипаттамасы Гиподинамия как фактор риска развития заболеваний
Гиподинамия как фактор риска развития заболеваний Лабораторная диагностика сахарного диабета
Лабораторная диагностика сахарного диабета Доброкачественные и злокачественные опухоли радужной оболочки и цилиарного тела
Доброкачественные и злокачественные опухоли радужной оболочки и цилиарного тела Комплексний порівняльний аналіз стану громадського здоров’я та діяльності системи охорони здоров’я України та Румунії
Комплексний порівняльний аналіз стану громадського здоров’я та діяльності системи охорони здоров’я України та Румунії Методы контрацепции
Методы контрацепции Лазеры в медицине
Лазеры в медицине Соединительно-тканный массаж
Соединительно-тканный массаж Түрлі мүшелер электрлік белсеңділігін зерттеу әдістері
Түрлі мүшелер электрлік белсеңділігін зерттеу әдістері Осторожно! Клещи
Осторожно! Клещи Грипп и ОРВИ: Обоснованные подходы к лечению и профилактике
Грипп и ОРВИ: Обоснованные подходы к лечению и профилактике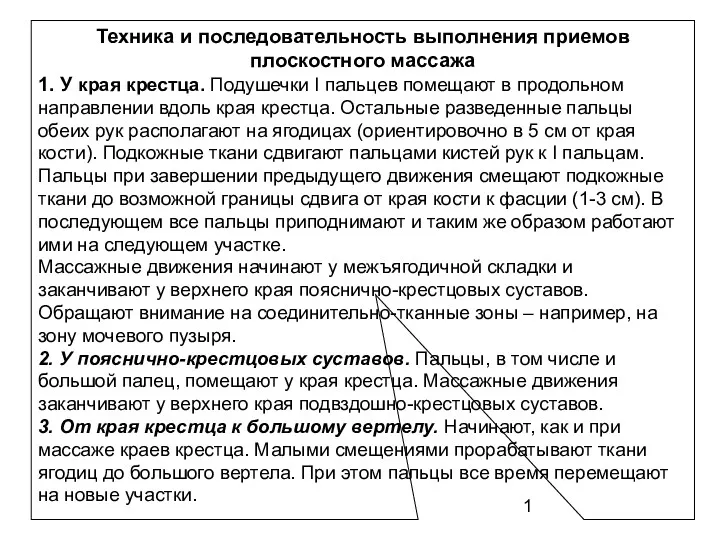 Техника и последовательность выполнения приемов плоскостного массажа
Техника и последовательность выполнения приемов плоскостного массажа Болезнь Виллебранда
Болезнь Виллебранда Вступ в курс інфектології. Поняття про інфекційні хвороби. Принципи діагностики, лікування, профілактики
Вступ в курс інфектології. Поняття про інфекційні хвороби. Принципи діагностики, лікування, профілактики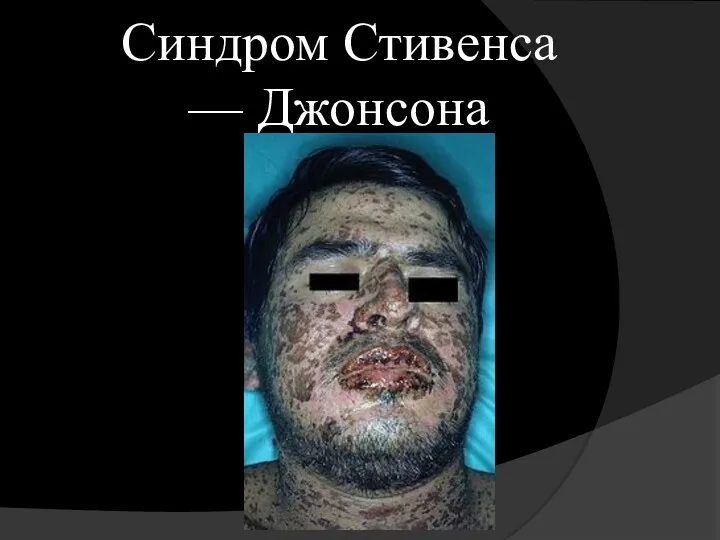 Синдром Стивенса — Джонсона
Синдром Стивенса — Джонсона Инфекционно-токсический шок. Критические состояния и факторы риска их развития у инфекционных больных
Инфекционно-токсический шок. Критические состояния и факторы риска их развития у инфекционных больных Долихосигма. Этиология
Долихосигма. Этиология Гормоны
Гормоны Интенсивная терапия и анестезия при кровопотере в акушерстве
Интенсивная терапия и анестезия при кровопотере в акушерстве Дезинфекционные технологии и оборудование для обеззараживания воздуха
Дезинфекционные технологии и оборудование для обеззараживания воздуха Обучение по оказанию первой помощи пострадавшим на производстве
Обучение по оказанию первой помощи пострадавшим на производстве Рентгеновская и позитронная томография
Рентгеновская и позитронная томография Анестезиологическое обеспечение экстренных хирургических вмешательств у детей. Оценка риска и безопасность
Анестезиологическое обеспечение экстренных хирургических вмешательств у детей. Оценка риска и безопасность Физкультура в семье. Здоровье родителей и детей
Физкультура в семье. Здоровье родителей и детей Обучение в сестринском деле
Обучение в сестринском деле Возрастные особенности формирования и развития эндокринной системы (гипо- и гиперфункция эндокринных желез)
Возрастные особенности формирования и развития эндокринной системы (гипо- и гиперфункция эндокринных желез)