Содержание
- 2. Primary tumor brain spinal Secondary tumor brain spinal Paraneoplastic syndrome
- 3. Imaging for Brain Tumors Skull X-rays: Rarely necessary. Useful in demonstrating calcification, erosion, or hyperostosis CT:
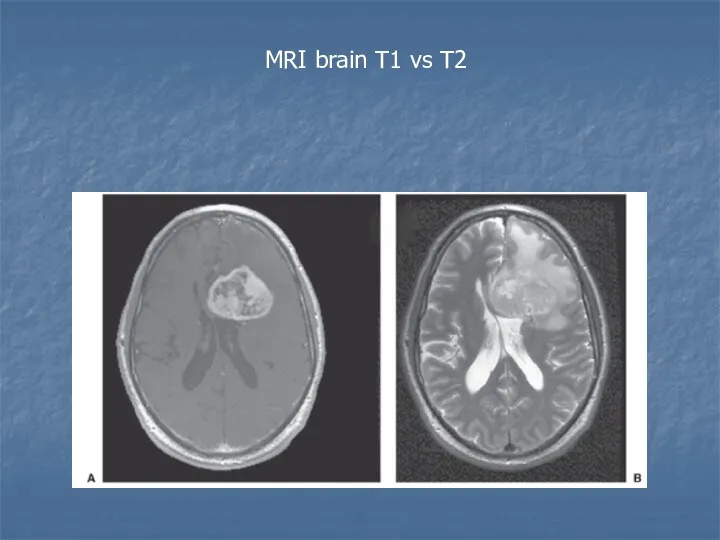
- 4. MRI brain T1 vs T2
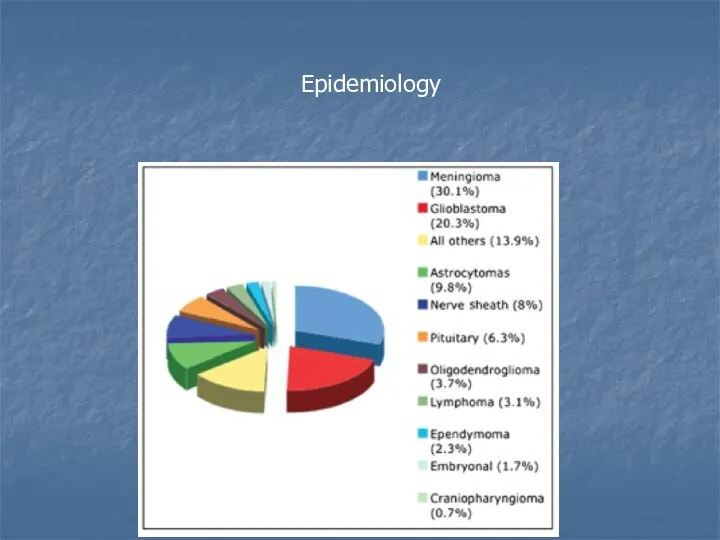
- 5. Epidemiology
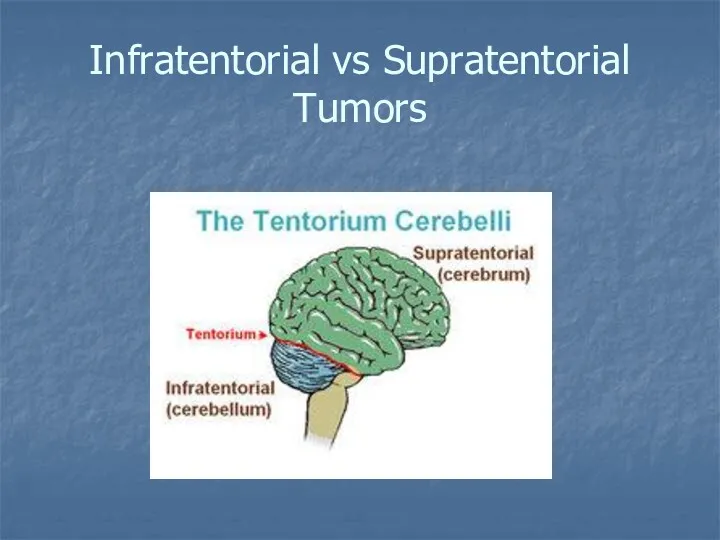
- 8. Infratentorial vs Supratentorial Tumors
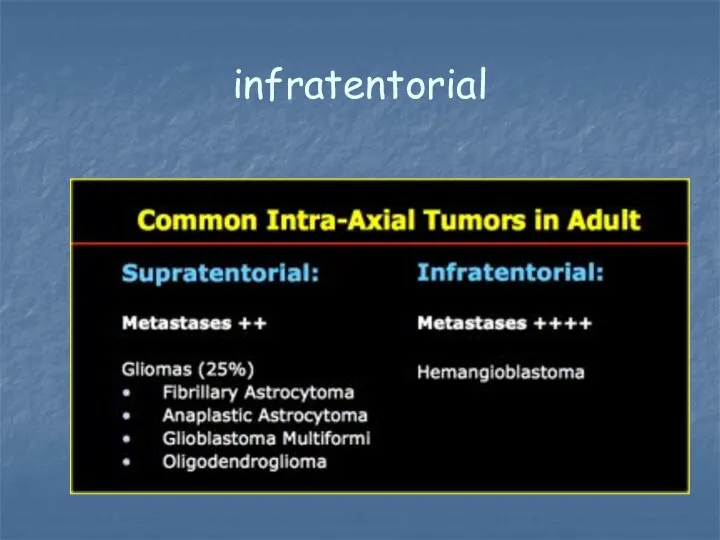
- 9. infratentorial
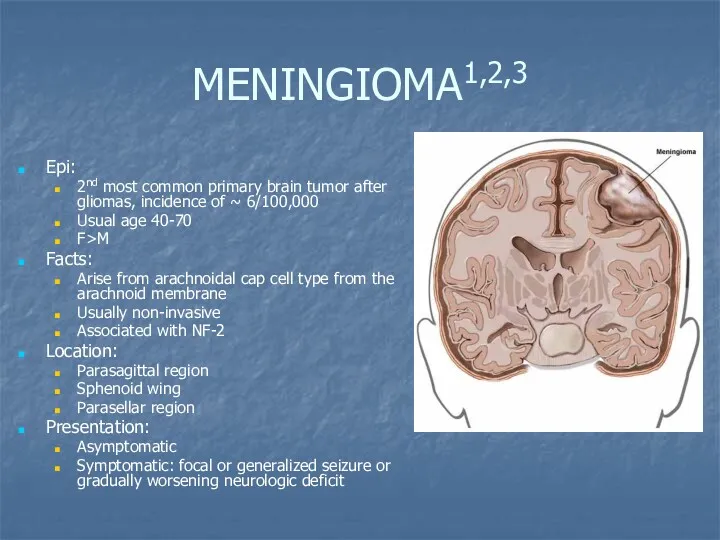
- 10. MENINGIOMA1,2,3 Epi: 2nd most common primary brain tumor after gliomas, incidence of ~ 6/100,000 Usual age
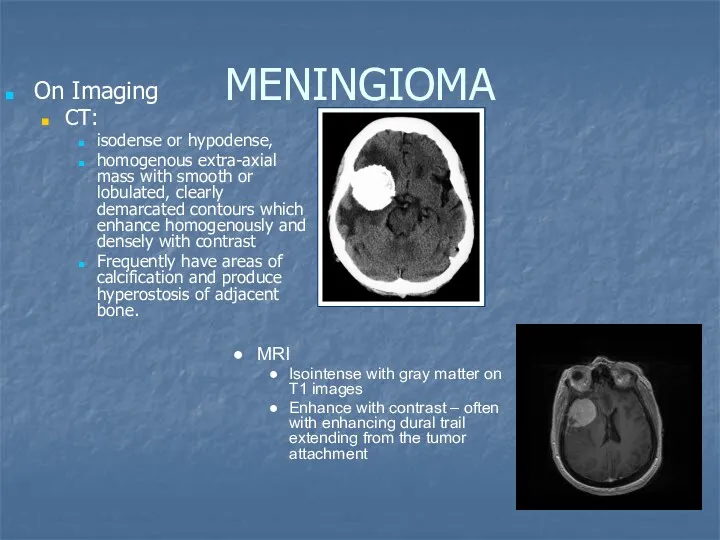
- 11. MENINGIOMA On Imaging CT: isodense or hypodense, homogenous extra-axial mass with smooth or lobulated, clearly demarcated
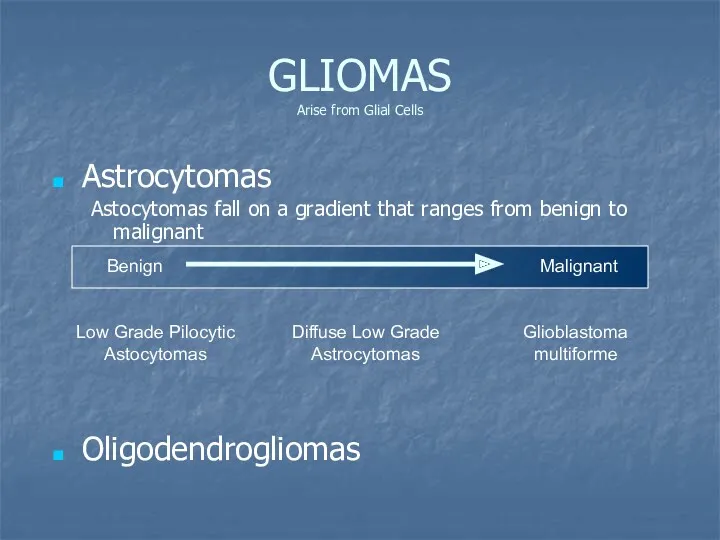
- 12. GLIOMAS Arise from Glial Cells Astrocytomas Astocytomas fall on a gradient that ranges from benign to
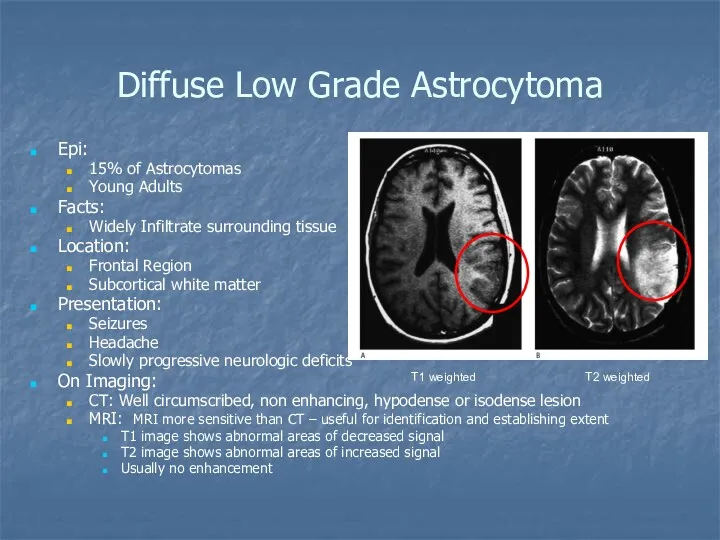
- 13. Diffuse Low Grade Astrocytoma Epi: 15% of Astrocytomas Young Adults Facts: Widely Infiltrate surrounding tissue Location:
- 14. High Grade glioma: Glioblastoma Epi: The 2-nd place of primary brain tumor in adults Age of
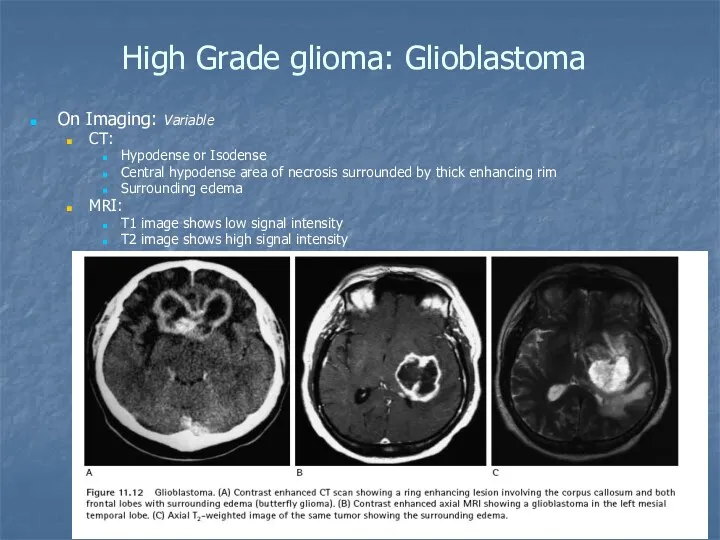
- 15. High Grade glioma: Glioblastoma On Imaging: Variable CT: Hypodense or Isodense Central hypodense area of necrosis
- 16. High Grade glioma: Glioblastoma Treatment: steroids surgical removal radiotherapy chemotherapy (temozolomide) anticonvulsive drugs
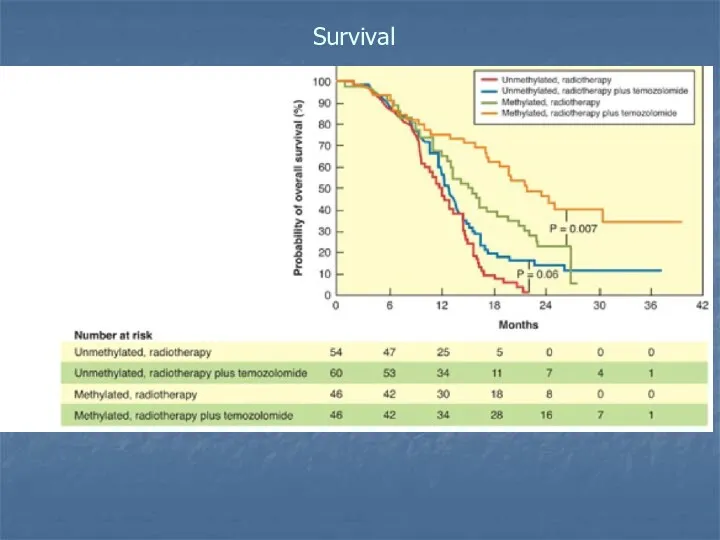
- 17. Survival
- 18. OLIGODENDROGLIOMA Epi: 5-10% of primary brain tumors Mean age of onset 40 years Facts: Distinguished pathologically
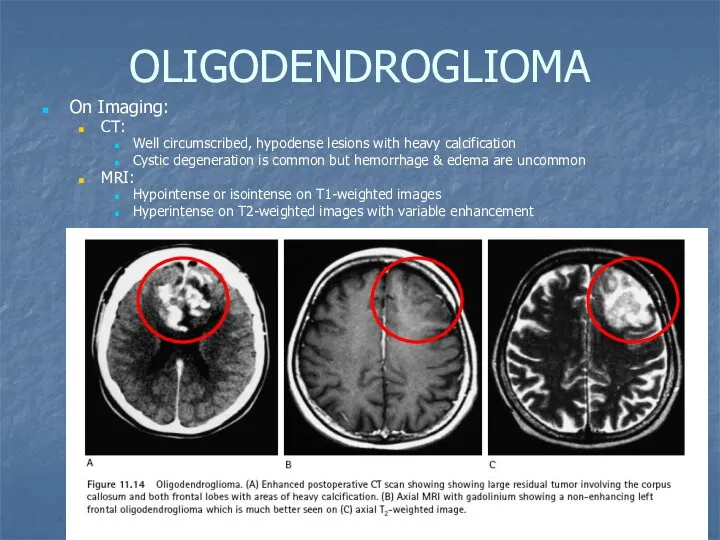
- 19. OLIGODENDROGLIOMA On Imaging: CT: Well circumscribed, hypodense lesions with heavy calcification Cystic degeneration is common but
- 20. OLIGODENDROGLIOMA Treatment: Surgical excision radiation therapy anticonvulsive drugs The median survival over 7 years.
- 21. INFRATENTORIAL TUMORS Choroid plexus papillomas Cerebellar astrocytomas Medulloblastomas Hemangioblastomas Ependymomas Brainstem gliomas Schwannomas Pituitary adenomas Craniopharyngiomas
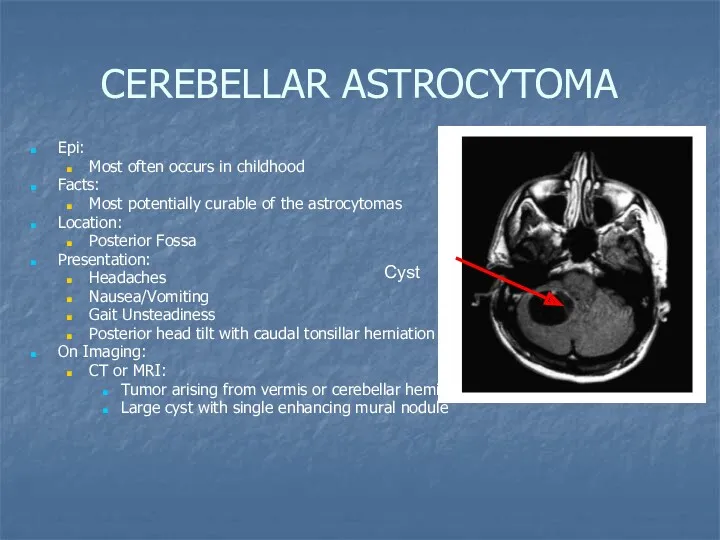
- 22. CEREBELLAR ASTROCYTOMA Epi: Most often occurs in childhood Facts: Most potentially curable of the astrocytomas Location:
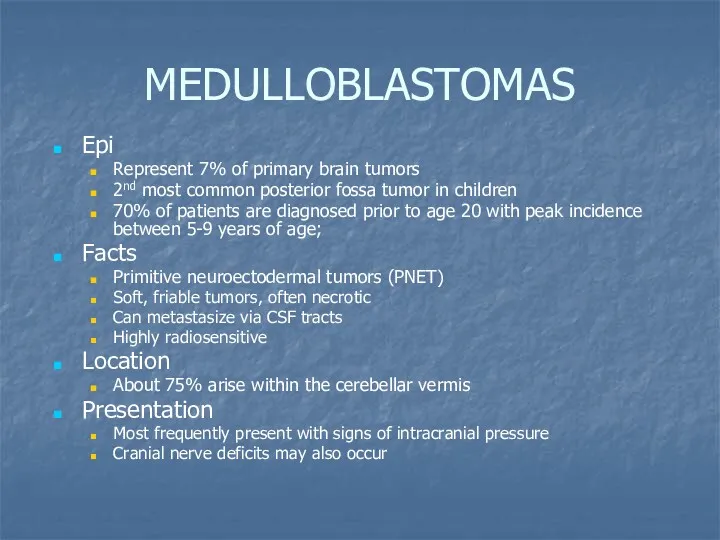
- 23. MEDULLOBLASTOMAS Epi Represent 7% of primary brain tumors 2nd most common posterior fossa tumor in children
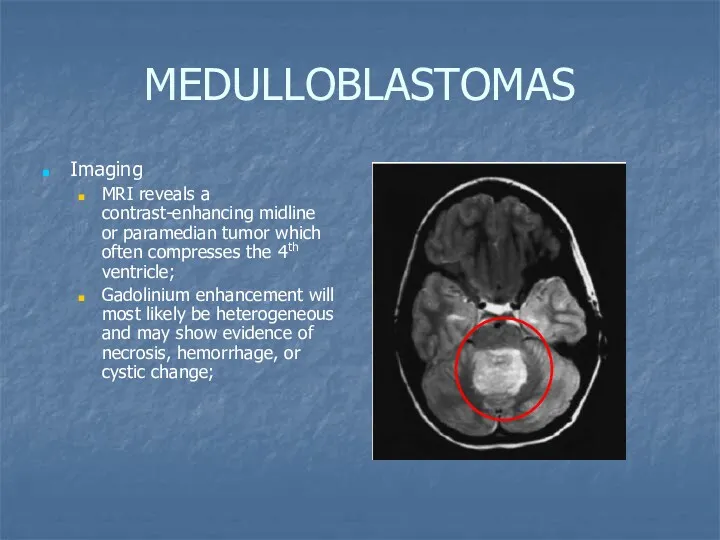
- 24. MEDULLOBLASTOMAS Imaging MRI reveals a contrast-enhancing midline or paramedian tumor which often compresses the 4th ventricle;
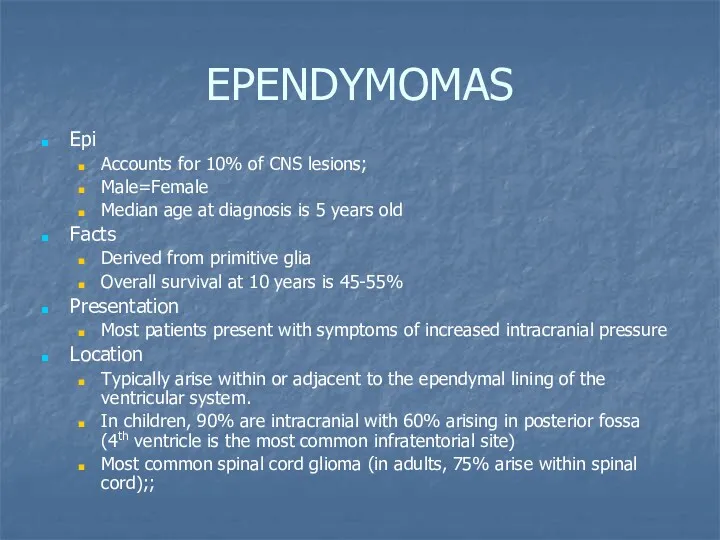
- 25. EPENDYMOMAS Epi Accounts for 10% of CNS lesions; Male=Female Median age at diagnosis is 5 years
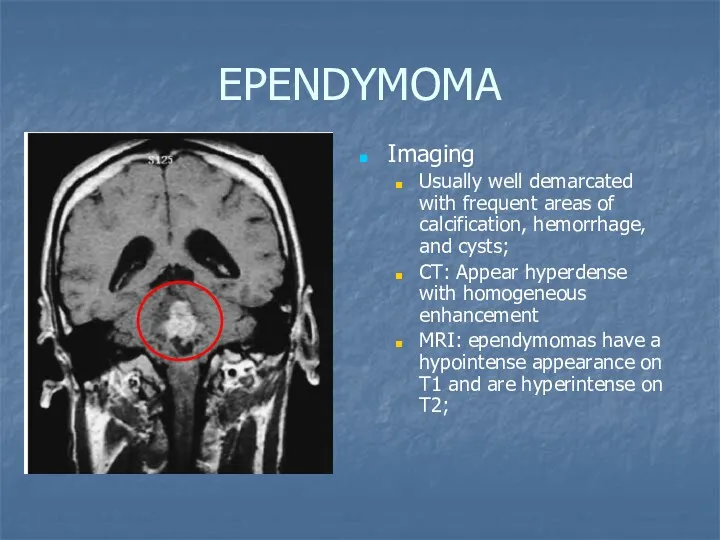
- 26. EPENDYMOMA Imaging Usually well demarcated with frequent areas of calcification, hemorrhage, and cysts; CT: Appear hyperdense
- 27. SCHWANNOMAS Epi Female>male Median age at diagnosis is 50 Account for 80-90% of cerebellopontine angle tumors
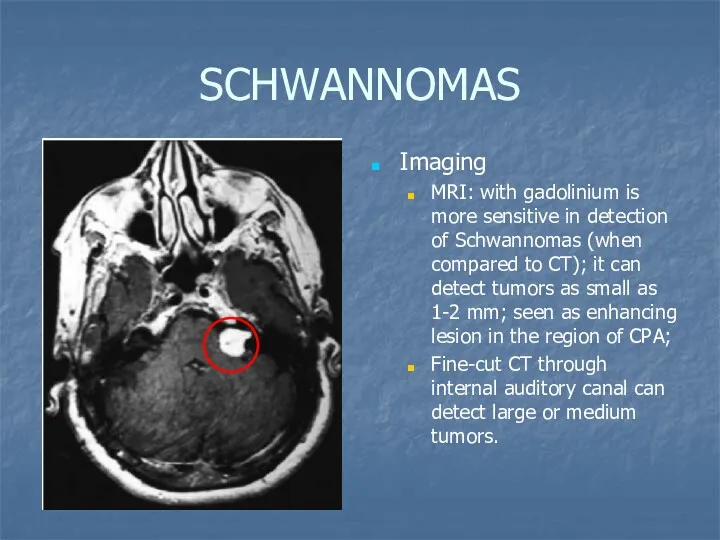
- 28. SCHWANNOMAS Imaging MRI: with gadolinium is more sensitive in detection of Schwannomas (when compared to CT);
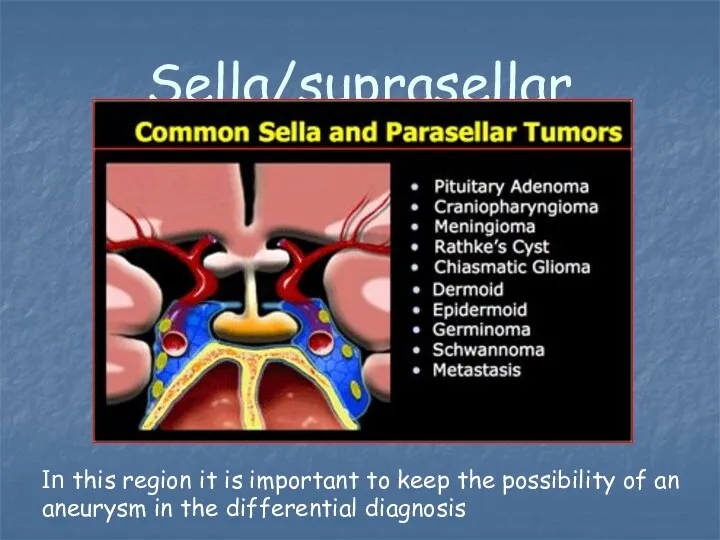
- 29. Sella/suprasellar In this region it is important to keep the possibility of an aneurysm in the
- 30. PITUITARY ADENOMAS Epi Most common tumors of pituitary gland Represent 8% of primary brain tumors Facts
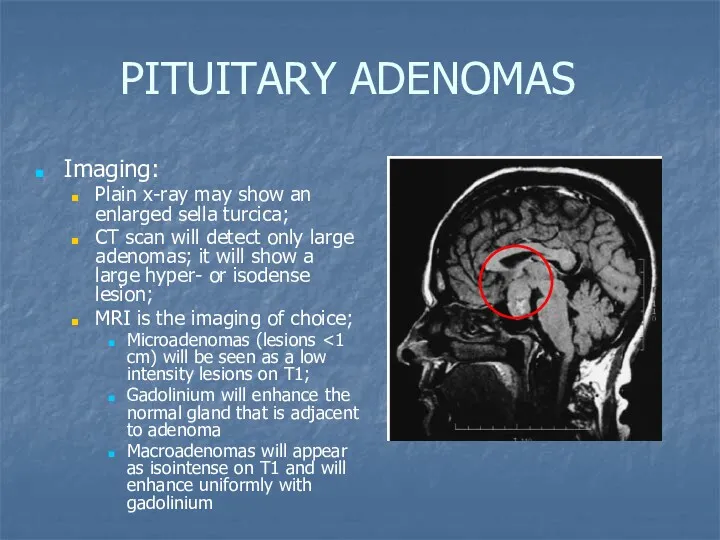
- 31. PITUITARY ADENOMAS Imaging: Plain x-ray may show an enlarged sella turcica; CT scan will detect only
- 32. BRAINSTEM GLIOMAS Epi Male=Female Account for 10-20% on all CNS tumors More common in children (account
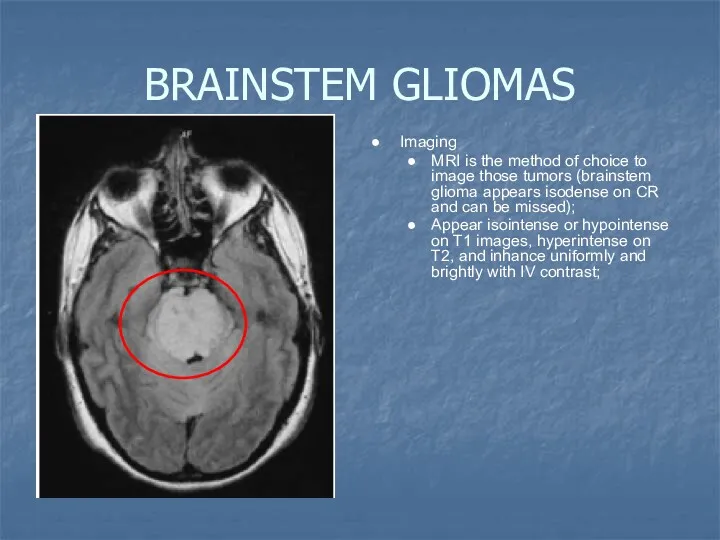
- 33. BRAINSTEM GLIOMAS Imaging MRI is the method of choice to image those tumors (brainstem glioma appears
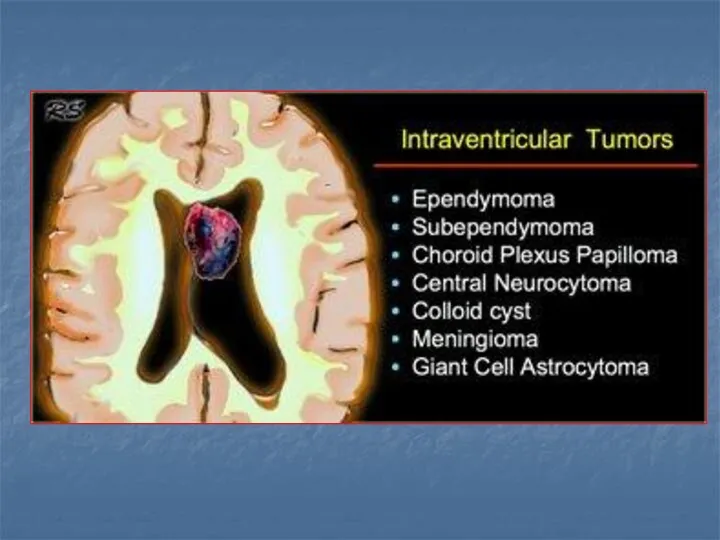
- 34. 4th ventricle In adults tumors in the 4th ventricle are uncommon. Metastases, followed by hemangioblastomas, choroid
- 35. Metastatic tumors Parenchymal meta – most common masses in the in supratentorial and infratentorial spaces (more
- 36. Hemorrhagic meta Breast Choriocarcinoma lung Melanoma RCC Thyroid retinoblastoma
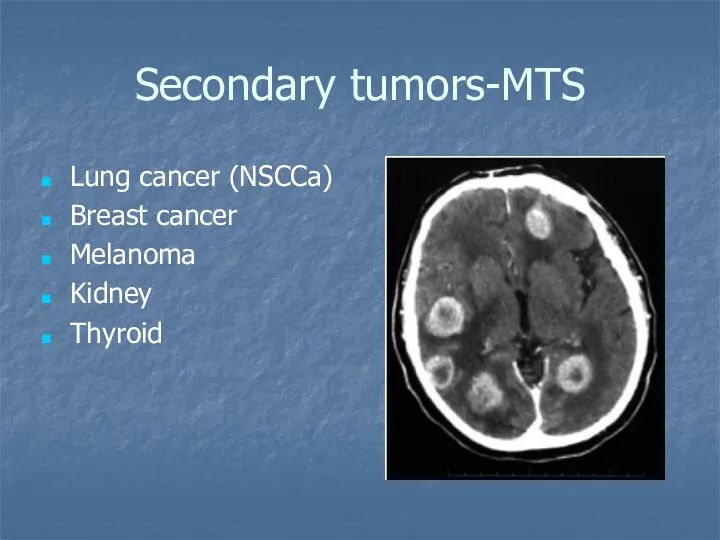
- 37. Secondary tumors-MTS Lung cancer (NSCCa) Breast cancer Melanoma Kidney Thyroid
- 38. Carcinomatous Meningitis (Meningeal Carcinomatosis) Dissemination of tumor cells throughout the meninges and ventricles. 5 percent of
- 40. Скачать презентацию


 Задача №6. Команда Морфий
Задача №6. Команда Морфий Corticosteroids. Steroids: the worst drugs for adverse effects
Corticosteroids. Steroids: the worst drugs for adverse effects Закупка лекарственных средств для нужд государственных и муниципальных организаций. Тема 1
Закупка лекарственных средств для нужд государственных и муниципальных организаций. Тема 1 Гигиена и антисептика рук в медицинском учреждении
Гигиена и антисептика рук в медицинском учреждении История развития отоларингологии
История развития отоларингологии Купероз и Anti-Aging
Купероз и Anti-Aging Акушерськиі операції. Класифікація. Принципи і методи знеболення
Акушерськиі операції. Класифікація. Принципи і методи знеболення Обсессивно-компульсивное расстройство (ОКР)
Обсессивно-компульсивное расстройство (ОКР) Туберкулез лимфатических узлов
Туберкулез лимфатических узлов Childhood Obesity
Childhood Obesity Содержимое аптечки, первичный комплекс сердечно-лёгочной реанимации (СЛР), первая помощь при неотложных состояниях
Содержимое аптечки, первичный комплекс сердечно-лёгочной реанимации (СЛР), первая помощь при неотложных состояниях Куріння та його вплив на організм людини
Куріння та його вплив на організм людини Буынның гипермобильдігі. Майтабан
Буынның гипермобильдігі. Майтабан Введение в доказательную медицину
Введение в доказательную медицину Домедична допомога в умовах бойових дій (тактична медицина). Тема №3.5
Домедична допомога в умовах бойових дій (тактична медицина). Тема №3.5 Wyposażenie torby R1-R2
Wyposażenie torby R1-R2 Жевательный аппарат. Анатомическое строение верхней и нижней челюстей. Височно-нижнечелюстной сустав. Пародонт
Жевательный аппарат. Анатомическое строение верхней и нижней челюстей. Височно-нижнечелюстной сустав. Пародонт Особенности паллиативной медицинской помощи
Особенности паллиативной медицинской помощи Обследование больных с патологией органов кровообращения
Обследование больных с патологией органов кровообращения Синдром Лайелла (токсический эпидермальный некролиз)
Синдром Лайелла (токсический эпидермальный некролиз) Понятие утомление и переутомление
Понятие утомление и переутомление Снотворные средства
Снотворные средства Рак тела матки
Рак тела матки Снотворные средства
Снотворные средства Тактика ведения ревматологических больных при беременности
Тактика ведения ревматологических больных при беременности Sistemul circulator limfatic organele hematopoietice
Sistemul circulator limfatic organele hematopoietice Коклюш
Коклюш Черный мор (чума)
Черный мор (чума)