Содержание
- 2. Parenteral Nutrition in Neonates Prepared By Neveen Hassan Abdel Aal Clinical Pharmacist at NICU Assuit University
- 3. Parenteral Nutrition: Definition & Goals. Types of PN Admixtures. Routes of Administration of PN. Nutritional Components
- 4. Parenteral Nutrition PN is the administration of intravenous nutrition in patients with a Non- functioning or
- 5. Parenteral Nutrition Goals (1) Weight maintenance or promoting growth. (2) Preservation of lean body mass& visceral
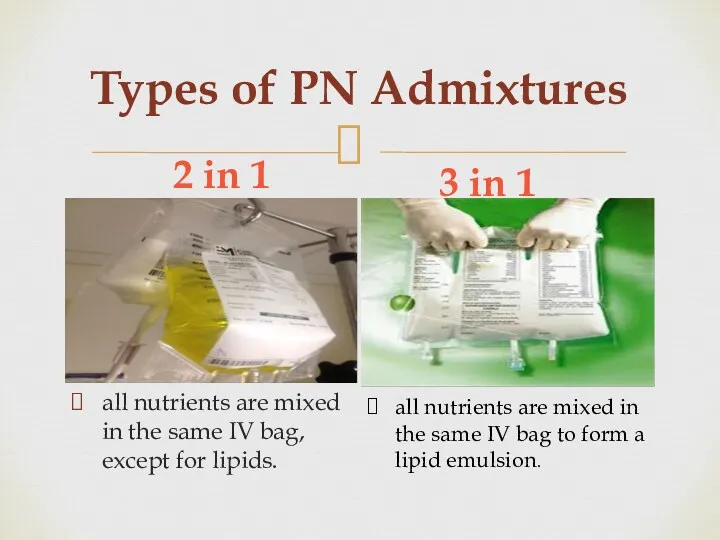
- 6. Types of PN Admixtures 2 in 1 3 in 1 all nutrients are mixed in the
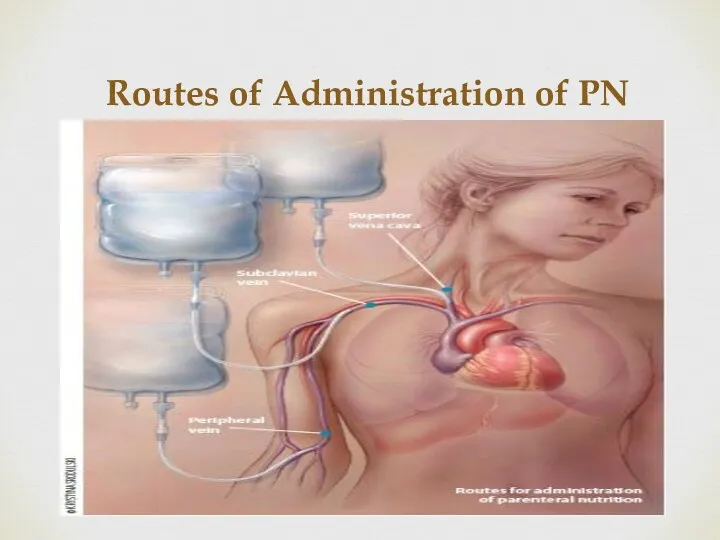
- 7. Routes of Administration of PN
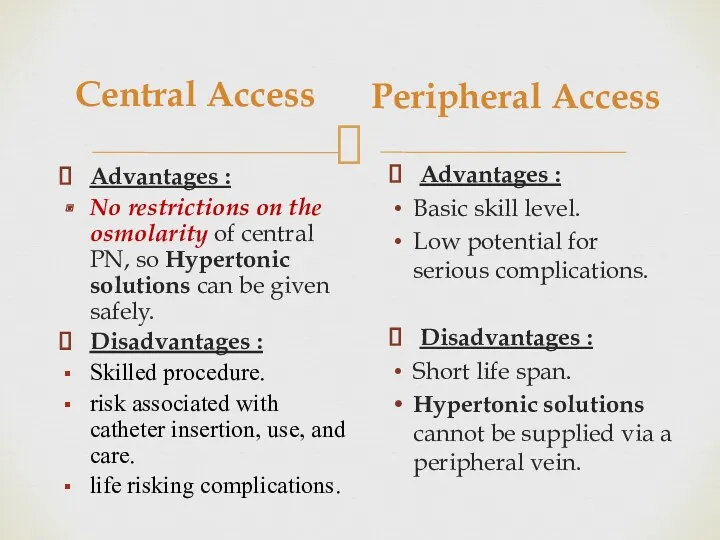
- 8. Central Access Advantages : No restrictions on the osmolarity of central PN, so Hypertonic solutions can
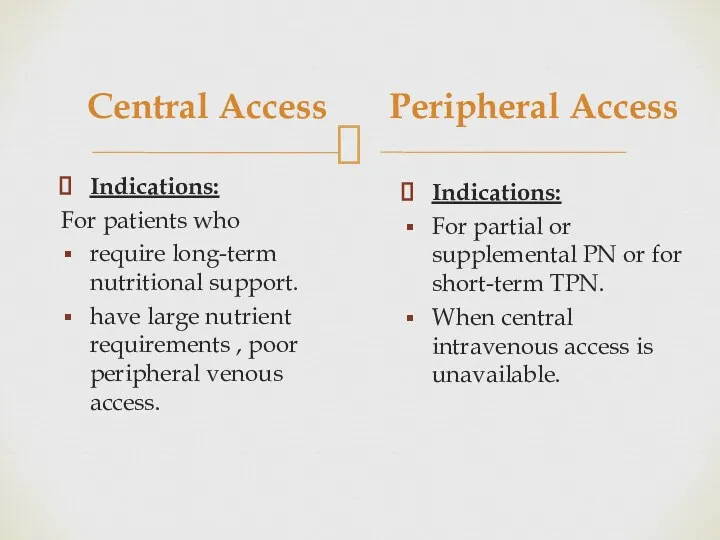
- 9. Central Access Indications: For patients who require long-term nutritional support. have large nutrient requirements , poor
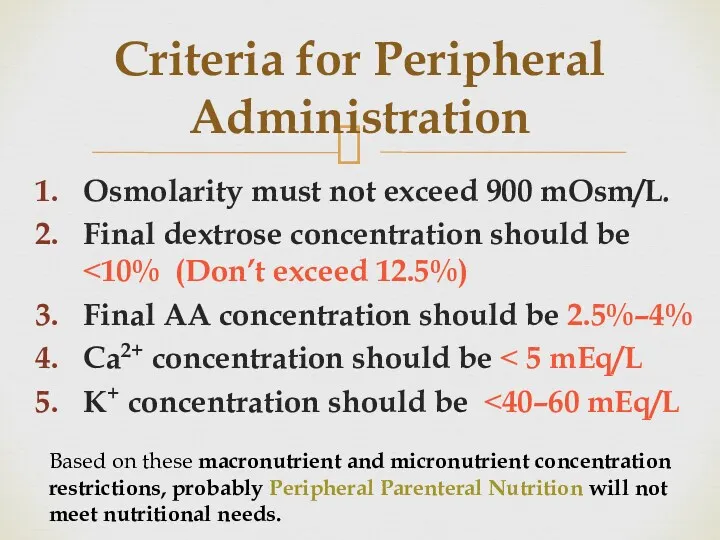
- 10. Criteria for Peripheral Administration Osmolarity must not exceed 900 mOsm/L. Final dextrose concentration should be ˂10%
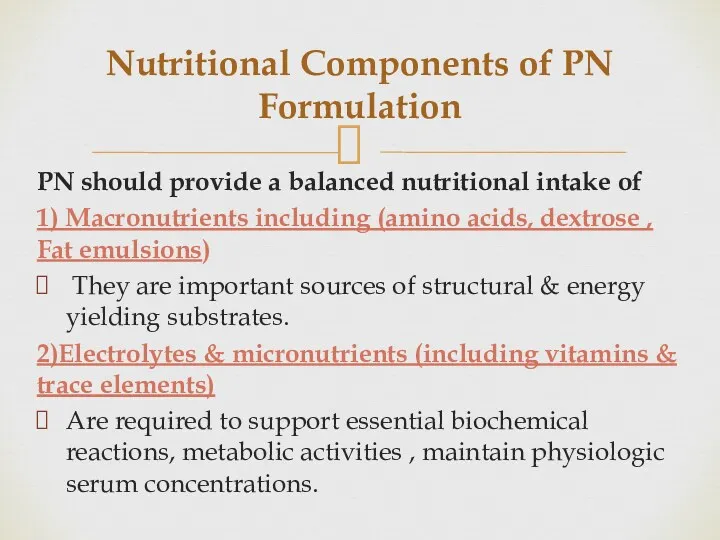
- 11. Nutritional Components of PN Formulation PN should provide a balanced nutritional intake of 1) Macronutrients including
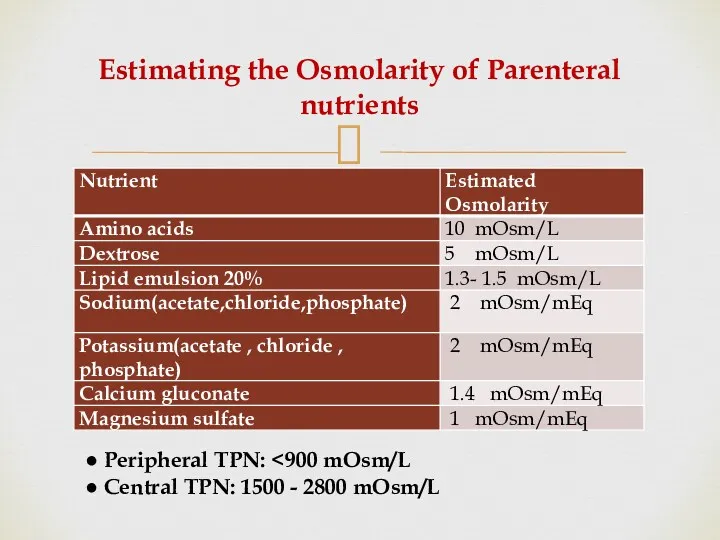
- 12. Estimating the Osmolarity of Parenteral nutrients ● Peripheral TPN: ● Central TPN: 1500 - 2800 mOsm/L
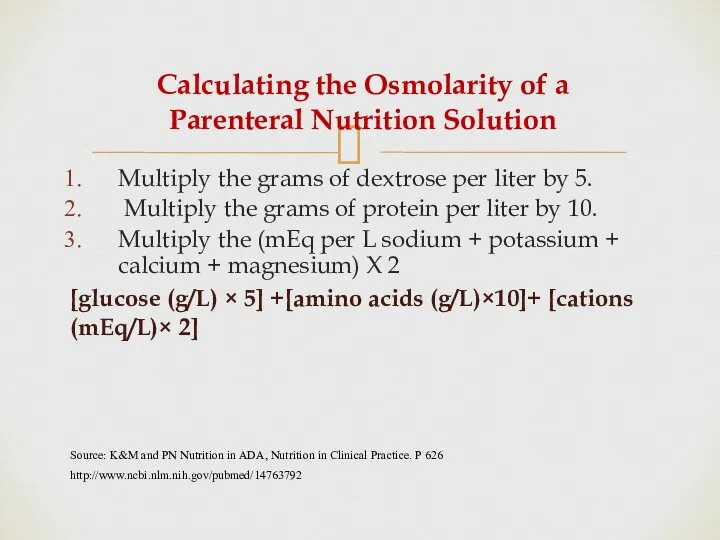
- 13. Calculating the Osmolarity of a Parenteral Nutrition Solution Multiply the grams of dextrose per liter by
- 14. Developing a Regimen for PN Administration Through Central Line
- 15. I. Evaluation of patient case PN components should be adjusted individually to each patient according to:
- 16. I. Evaluation of patient case First of all Review: Patient Age, weight ( Kg). Make sure
- 17. Evaluation of patient case continue 4. Assessment of degree of hydration. Signs of dehydration: Reduced urine
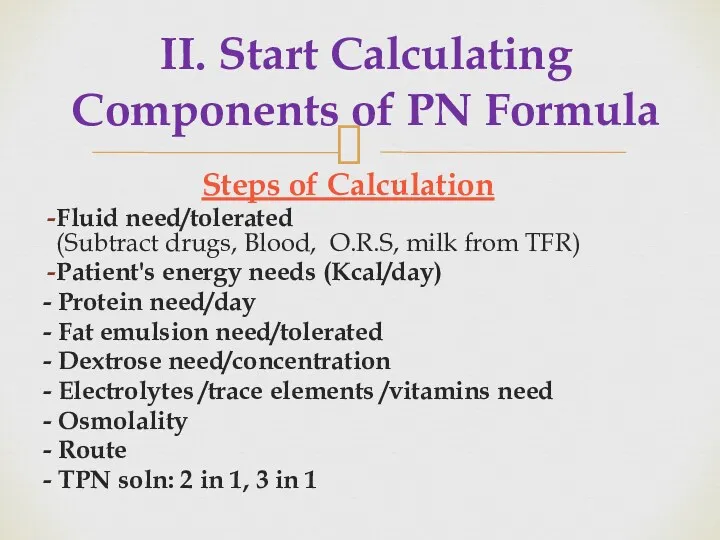
- 18. II. Start Calculating Components of PN Formula Steps of Calculation Fluid need/tolerated (Subtract drugs, Blood, O.R.S,
- 19. 1.Determine Fluid Requirements
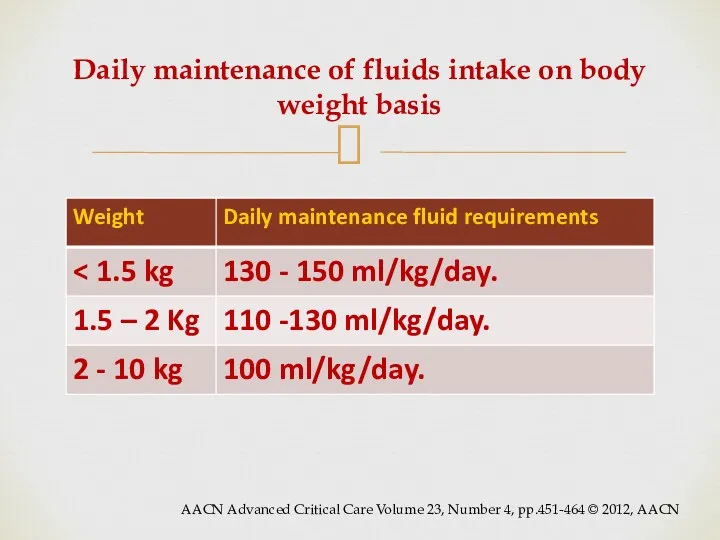
- 20. Daily maintenance of fluids intake on body weight basis AACN Advanced Critical Care Volume 23, Number
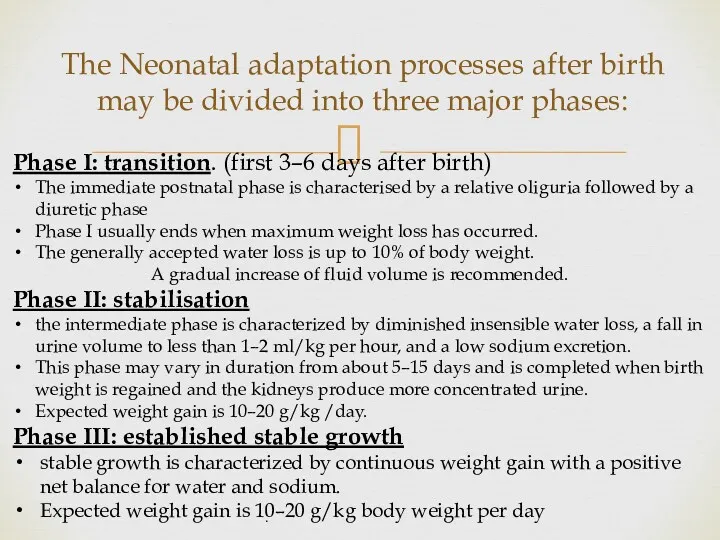
- 21. The Neonatal adaptation processes after birth may be divided into three major phases: Phase I: transition.
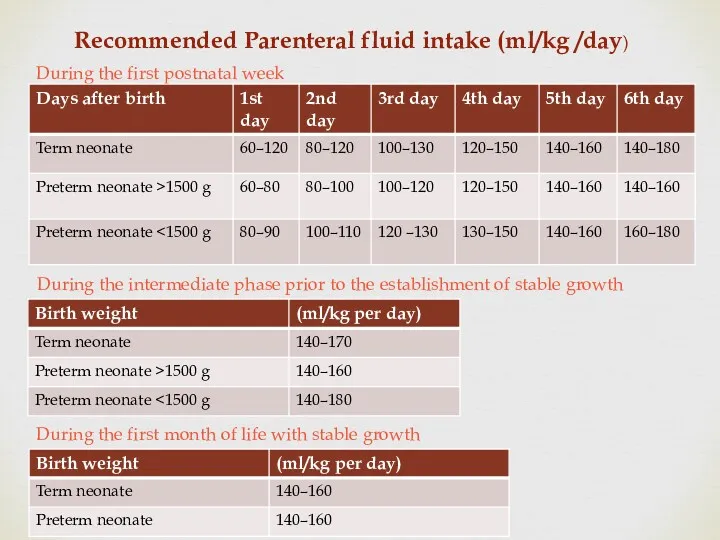
- 22. Recommended Parenteral fluid intake (ml/kg /day) During the first postnatal week During the intermediate phase prior
- 23. Variations in Fluid Requirements Do not use PN for fluid replacement but for maintenance fluid only.
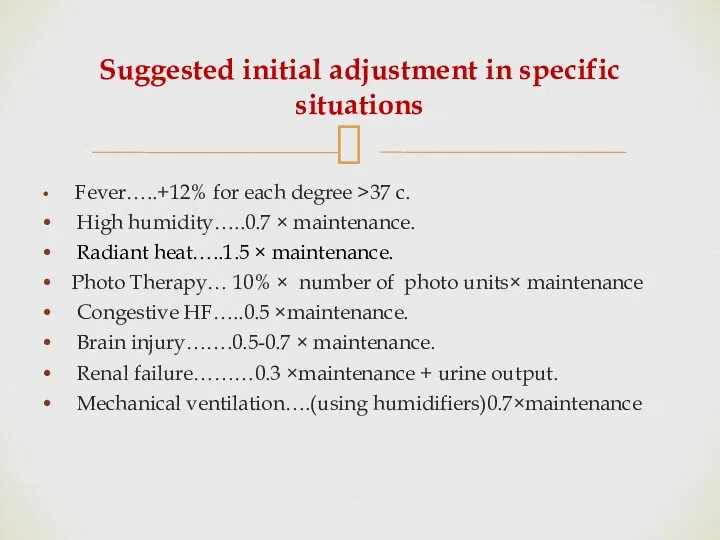
- 24. Suggested initial adjustment in specific situations Fever…..+12% for each degree >37 c. High humidity…..0.7 × maintenance.
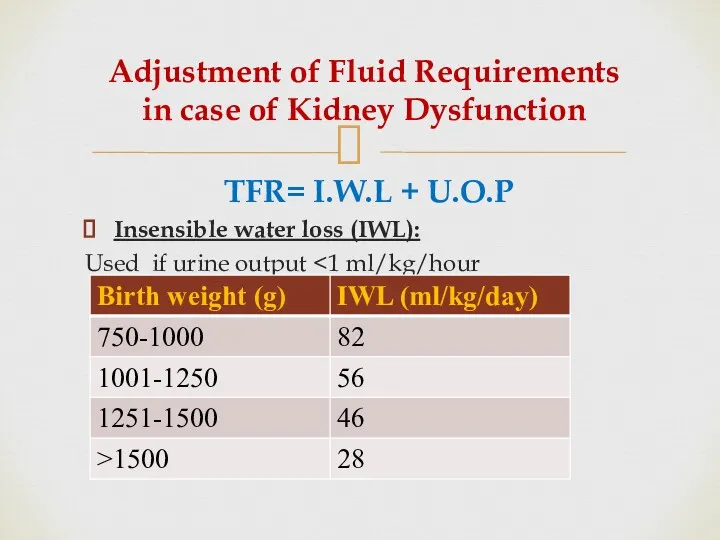
- 25. Adjustment of Fluid Requirements in case of Kidney Dysfunction TFR= I.W.L + U.O.P Insensible water loss
- 26. 2. Determine Caloric Requirements
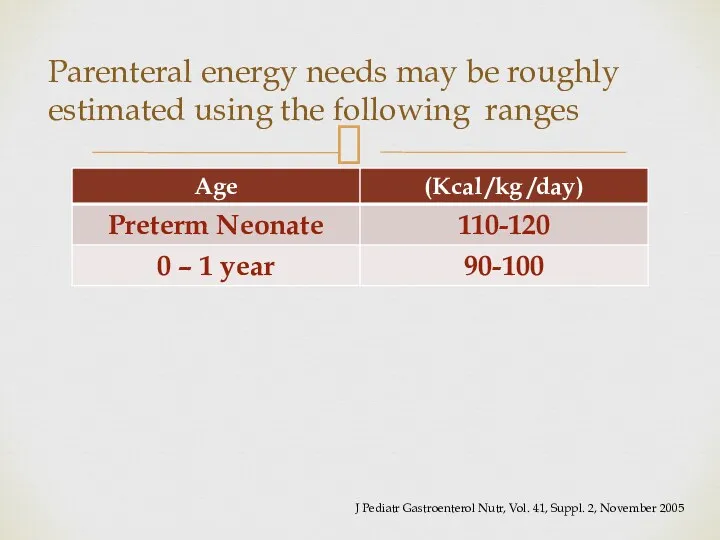
- 27. Parenteral energy needs may be roughly estimated using the following ranges J Pediatr Gastroenterol Nutr, Vol.
- 28. Further aspects need to be taken into account according to clinical parameters: Weight gain in regard
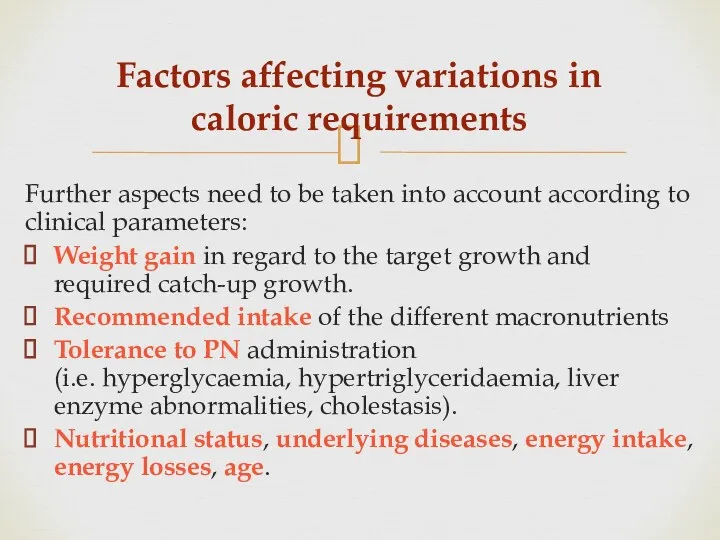
- 29. Variations in Caloric Requirements Patient require increased caloric needs in case of fever, inflammation, sepsis, burn,
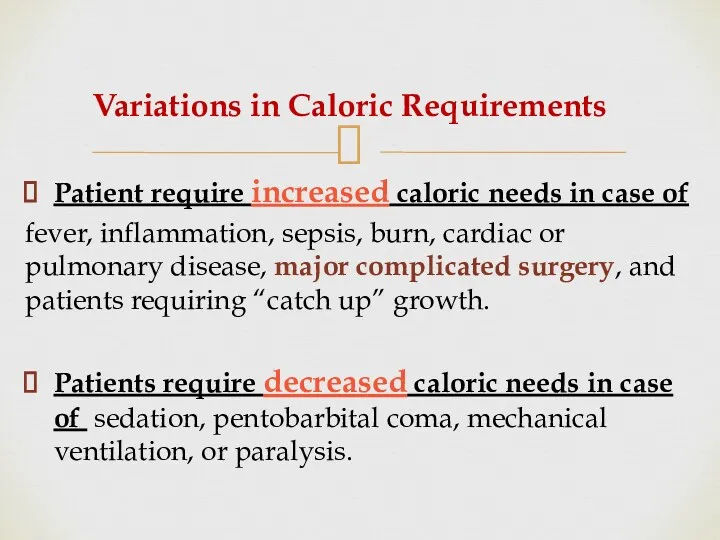
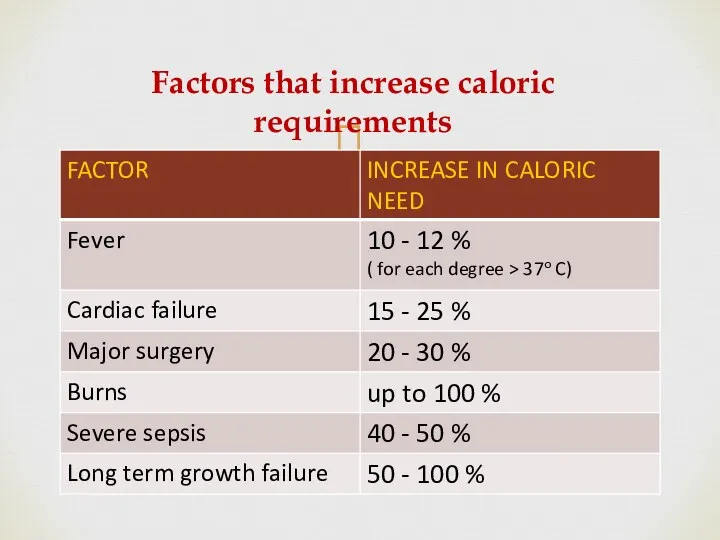
- 30. Factors that increase caloric requirements
- 31. The Caloric balance of PN Formula Caloric needs are met by a proper balance of carbohydrates,
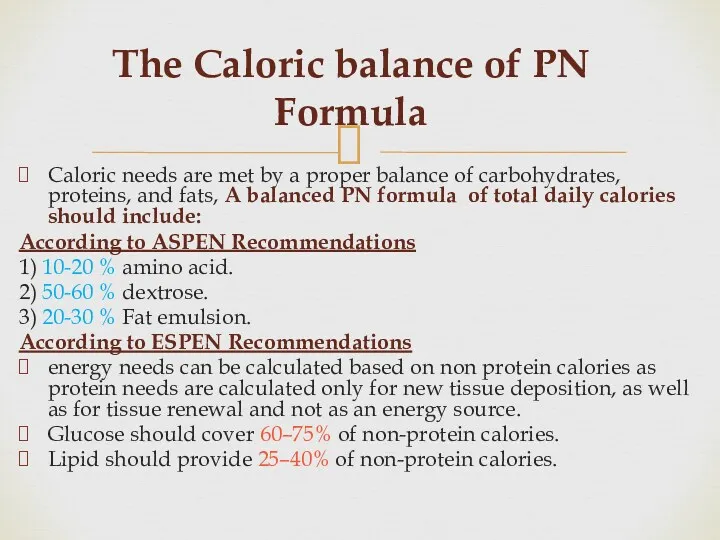
- 32. 3.Determine Protein Requirements Proteins are the major structural and functional components of all cells in the
- 33. Protein requirements of neonates and children depend on age and weight J Pediatr Gastroenterol Nutr, Vol.
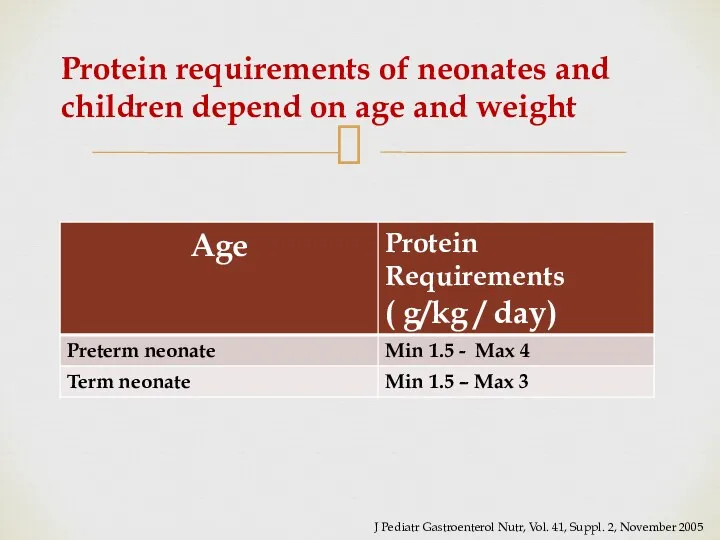
- 34. Regimen of Protein Administration Start with 1.5 gm/kg/d and then increase by 1 gm/kg/d to maximum
- 35. Protein requirements Variations Increased amount of amino acids are required in case of patients with short
- 36. Potential complications and risks of providing IV amino acids 1- Acidosis 2- Elevated BUN 3- Hyper-
- 37. Caloric Value of Proteins Calories from protein (4 kcal/g) Inadequate supplementation of energy from carbohydrates and
- 38. 4.Determine Lipid Requirements Providing fat is essential to Achieve adequate caloric intake in TPN Utilize amino
- 39. The lipid requirements of neonates and children depending on age J Pediatr Gastroenterol Nutr, Vol. 41,
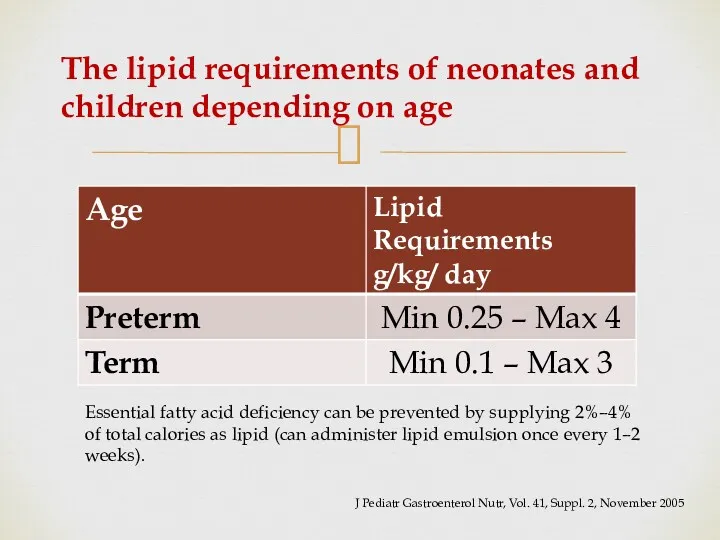
- 40. Regimen of Lipid Administration Starting dose of 1 g/kg/day Titrate toward the goal as tolerated by
- 41. Caloric Value of Lipids Calories from Lipid (10 kcal/g) Maximum fat oxidation occurs when intravenous lipid
- 42. Precautions For Neonates Restrict the dose of lipids in minimum amounts that will provide only the
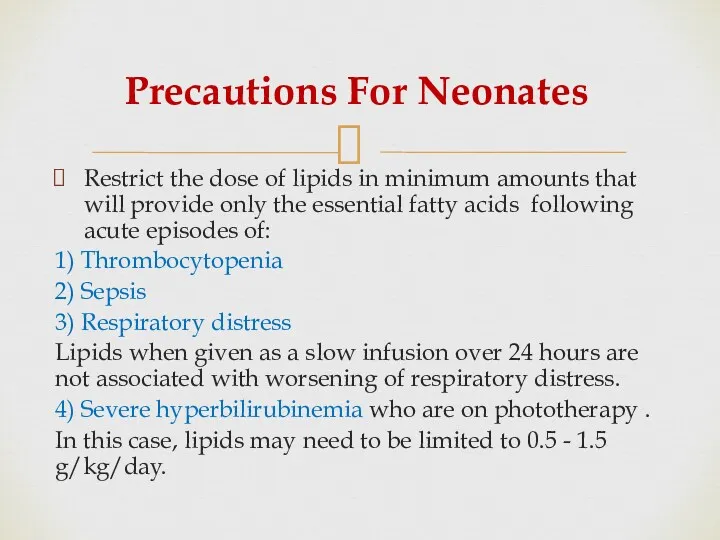
- 43. Potential complications and risks of providing IV Lipids Hyperlipidemia. Potential increased risk or exacerbation of chronic
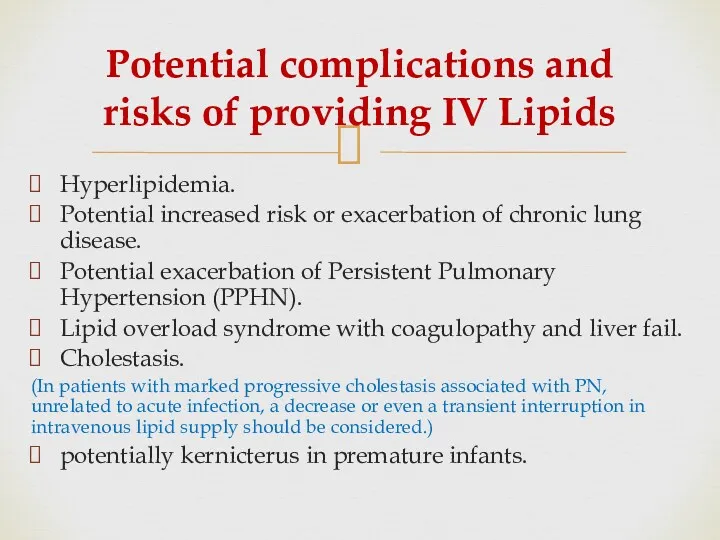
- 44. Monitoring Plasma clearance of infused triglycerides can be assessed by measurement of plasma triglyceride concentrations. Checking
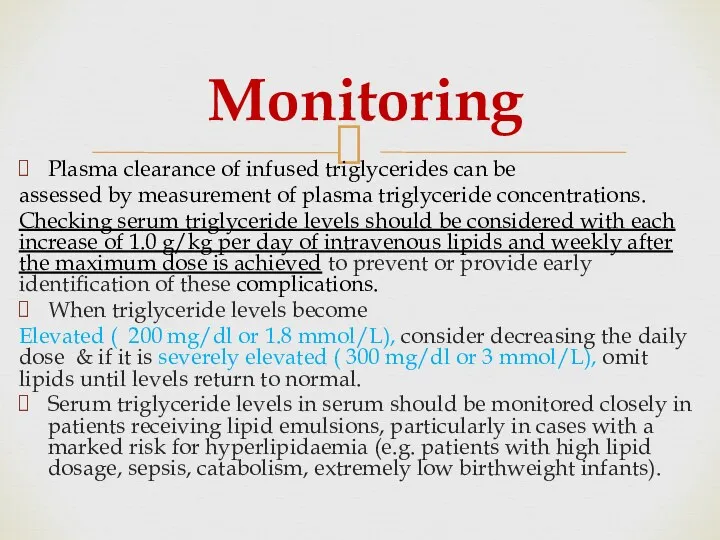
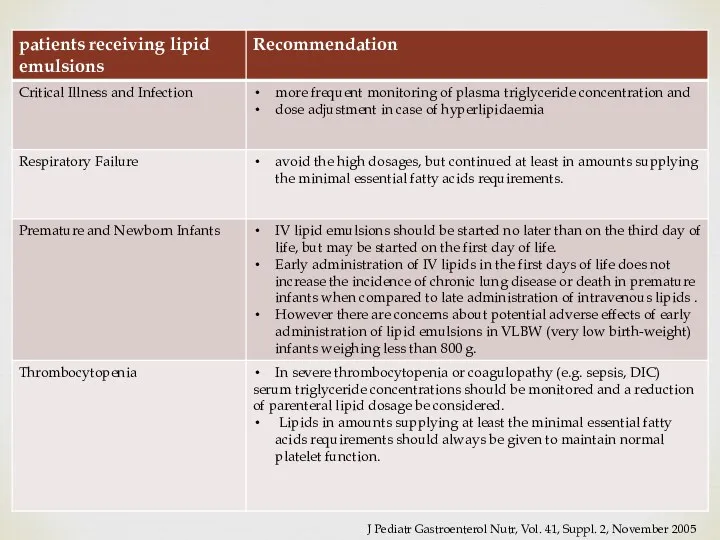
- 45. J Pediatr Gastroenterol Nutr, Vol. 41, Suppl. 2, November 2005
- 46. 5. Determine Carbohydrates Requirements Dextrose is major immediate energy source . Several body tissues depend mainly
- 47. Recommended parenteral glucose supply (g/kg/day) Estimation of carbohydrates requirements It is important, especially when prescribing PN
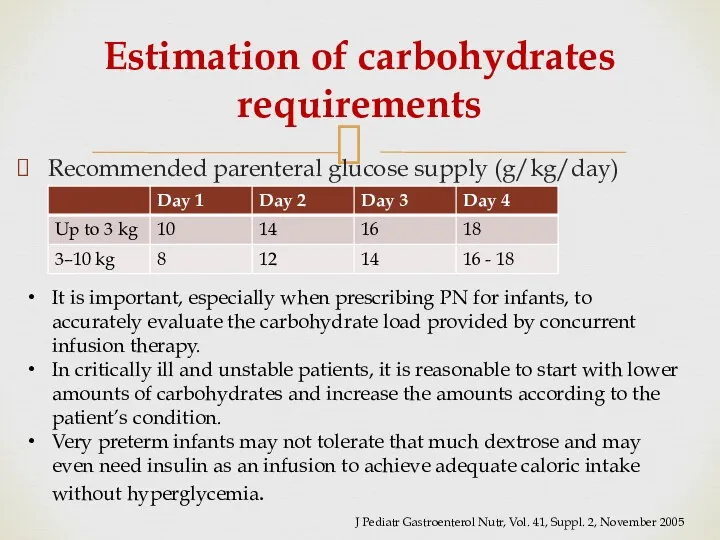
- 48. Carbohydrates Requirements need to be adapted according to Age and clinical situation (e.g. malnutrition, acute illness,
- 49. Regimen of Carbohydrate Administration For neonates: Begin with GIR 4-8 mg/kg/min in preterm 4-6 mg/kg/min in
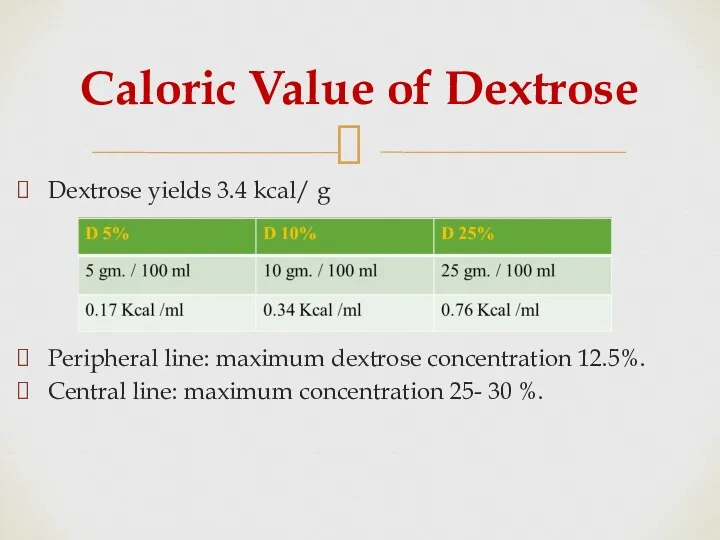
- 50. Caloric Value of Dextrose Dextrose yields 3.4 kcal/ g Peripheral line: maximum dextrose concentration 12.5%. Central
- 51. Potential complications Hyperglycemia or hypoglycemia. Glycosuria and potential osmotic diuresis. Cholestasis and/or hepatic steatosis (usually from
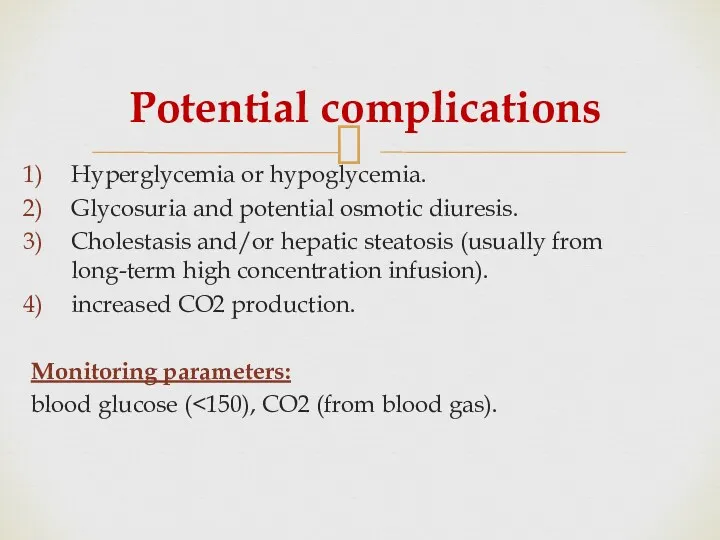
- 52. Managing Hyperglycemia in Neonates If hyperglycemia develops: ↓GIR insulin may improve glucose tolerance . Do not
- 53. 6. Estimate a Daily Maintenance amount of Electrolytes Vitamins & Trace elements
- 54. A) Electrolytes Initial PN solutions may be started without added electrolytes. Add electrolytes gradually as the
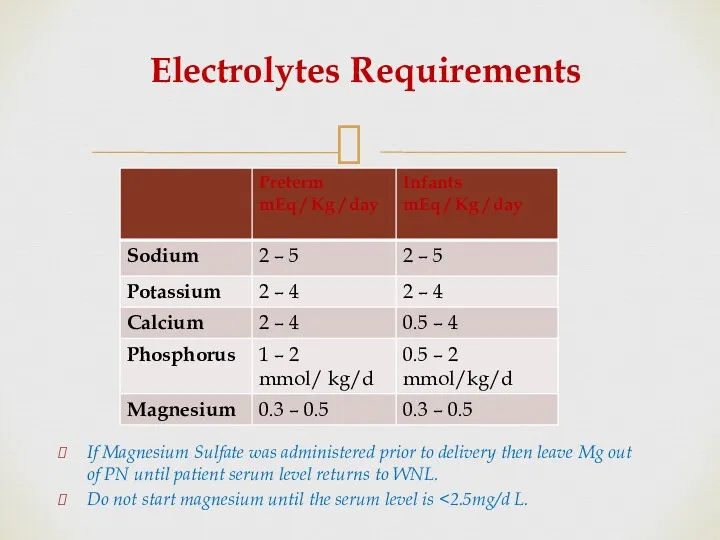
- 55. Electrolytes Requirements If Magnesium Sulfate was administered prior to delivery then leave Mg out of PN
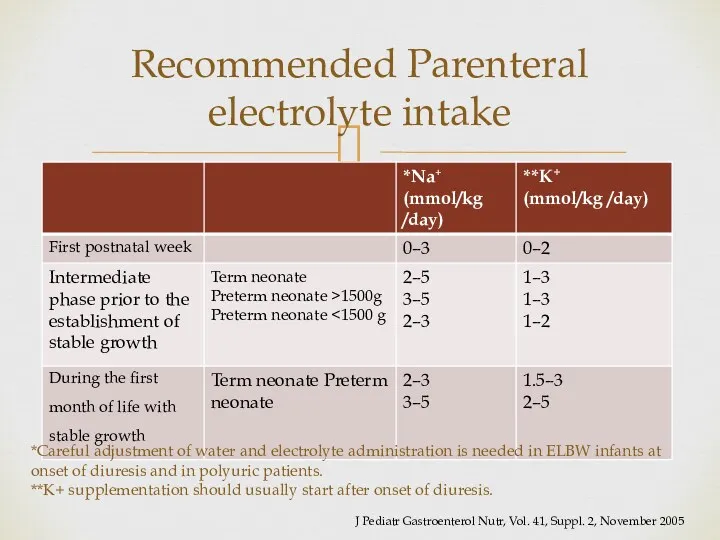
- 56. Recommended Parenteral electrolyte intake *Careful adjustment of water and electrolyte administration is needed in ELBW infants
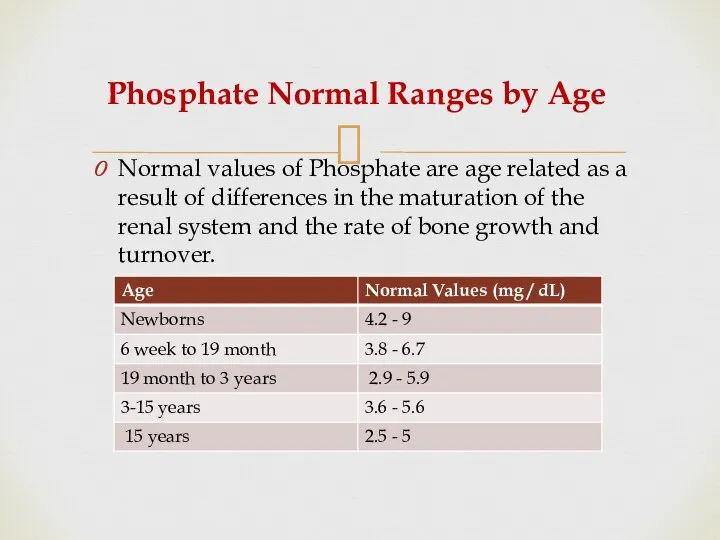
- 57. Phosphate Normal Ranges by Age Normal values of Phosphate are age related as a result of
- 58. B) Trace Elements Standard trace elements contain selenium, chromium, copper , manganese , and zinc. Neonates
- 59. Trace Elements Requirements
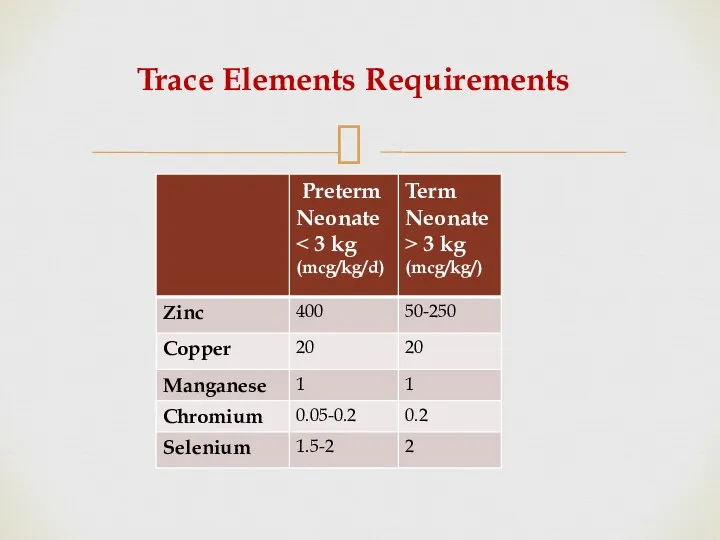
- 60. Pediatrace® Dose: 1 ml/ kg/ day for Premature, Infant & Children with a weight
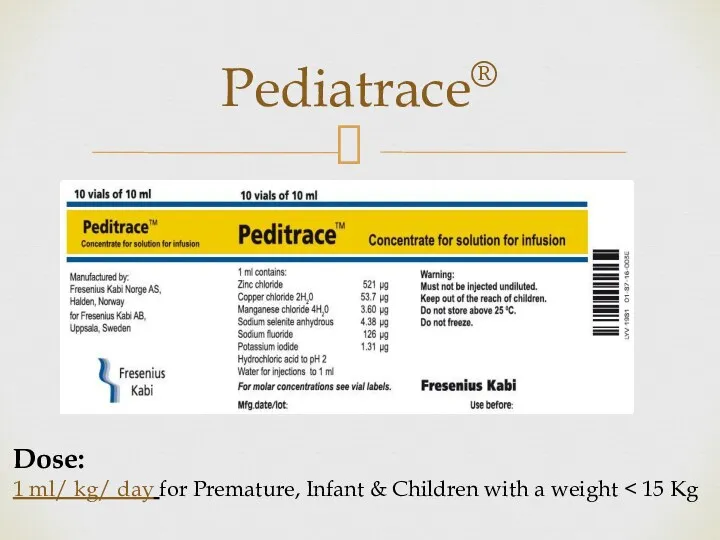
- 61. C) Vitamins Requirements Similar to trace elements, multivitamins are often standard in PN unless requested otherwise.
- 62. Medication Additives in PN Generally, medications should not be added to PN if it can be
- 63. PN Complications Short term Complications 1- Catheter-related infections 2- Catheter insertion complications 3-Peripheral Thrombophlebitis 4-Gut atrophy
- 64. Short term Complications Continue 7. Refeeding syndrome can occur in acutely or chronically malnourished patients by
- 65. Long term Complications 1-Hepatobiliary Disorders (includes steatosis, cholestasis, and gallbladder stones) 2-Osteoporosis & osteomalacia associated with
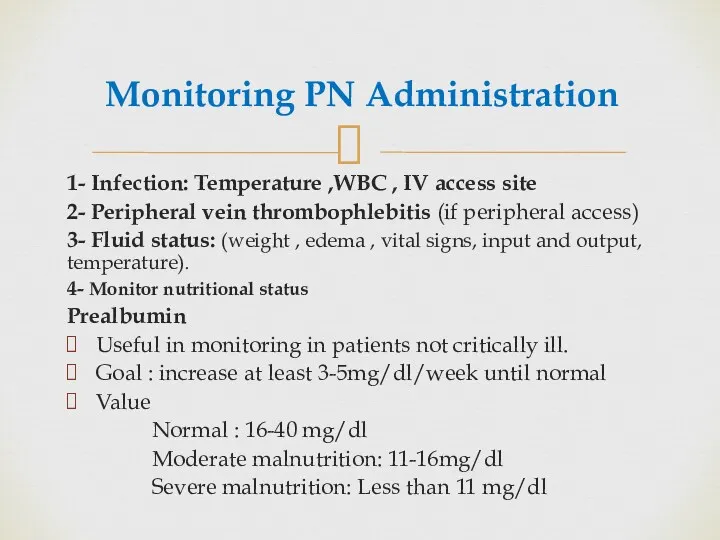
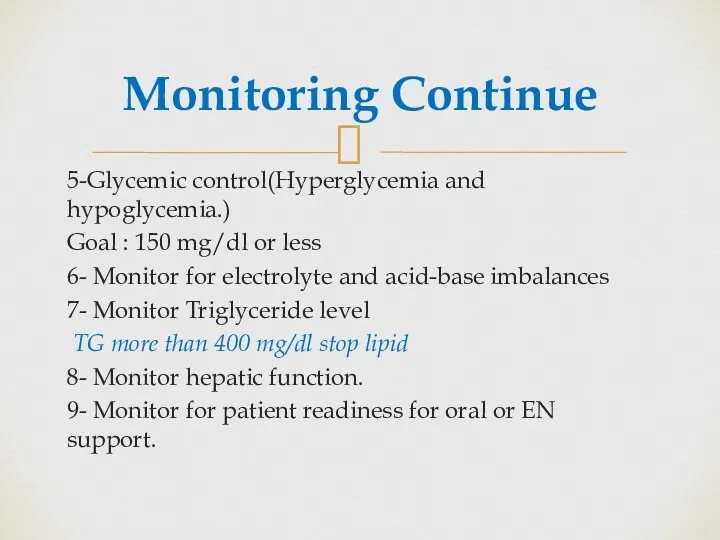
- 66. Monitoring PN Administration 1- Infection: Temperature ,WBC , IV access site 2- Peripheral vein thrombophlebitis (if
- 67. Monitoring Continue 5-Glycemic control(Hyperglycemia and hypoglycemia.) Goal : 150 mg/dl or less 6- Monitor for electrolyte
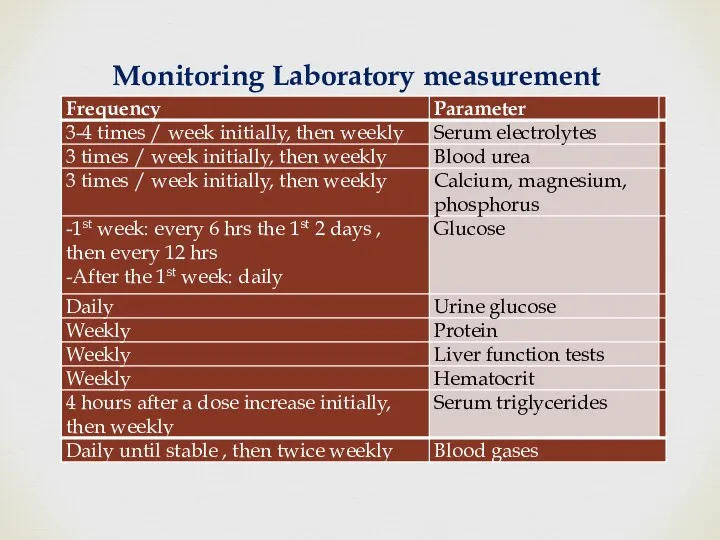
- 68. Monitoring Laboratory measurement
- 69. Transition to Oral or Enteral Nutrition When initiating enteral or oral nutrition , monitor for glucose,
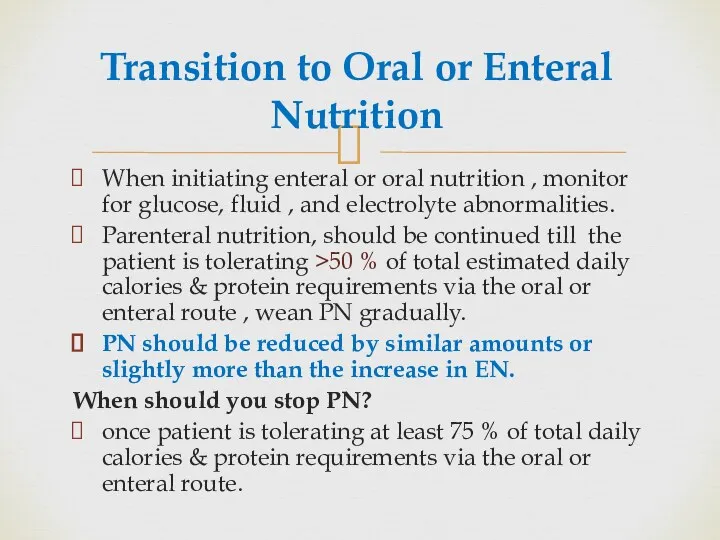
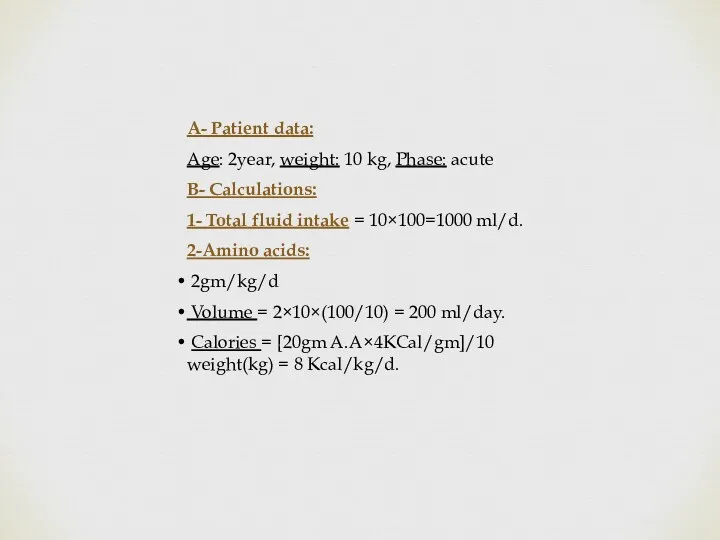
- 71. A- Patient data: Age: 2year, weight: 10 kg, Phase: acute B- Calculations: 1- Total fluid intake
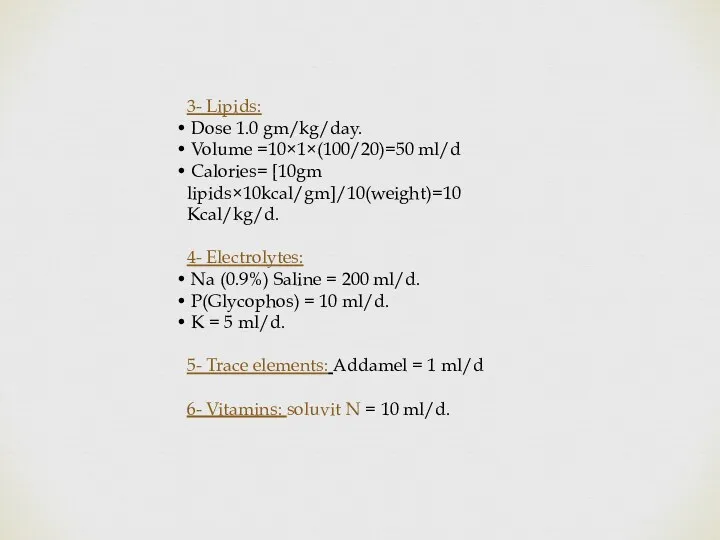
- 72. 3- Lipids: Dose 1.0 gm/kg/day. Volume =10×1×(100/20)=50 ml/d Calories= [10gm lipids×10kcal/gm]/10(weight)=10 Kcal/kg/d. 4- Electrolytes: Na (0.9%)
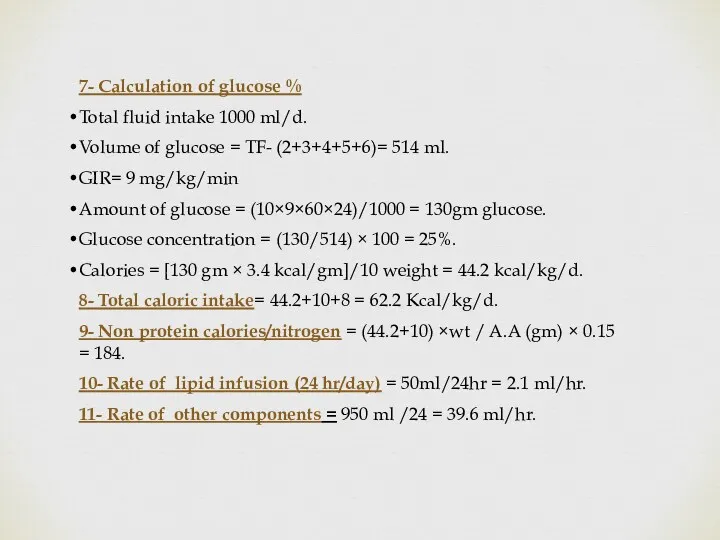
- 73. 7- Calculation of glucose % Total fluid intake 1000 ml/d. Volume of glucose = TF- (2+3+4+5+6)=
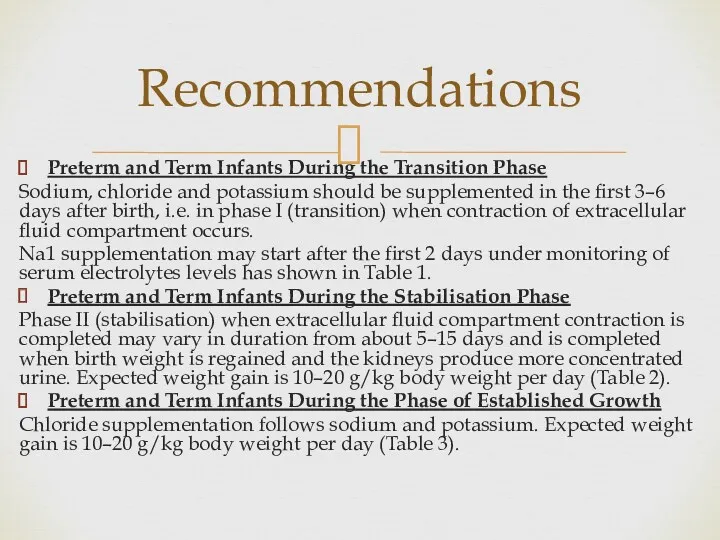
- 74. Preterm and Term Infants During the Transition Phase Sodium, chloride and potassium should be supplemented in
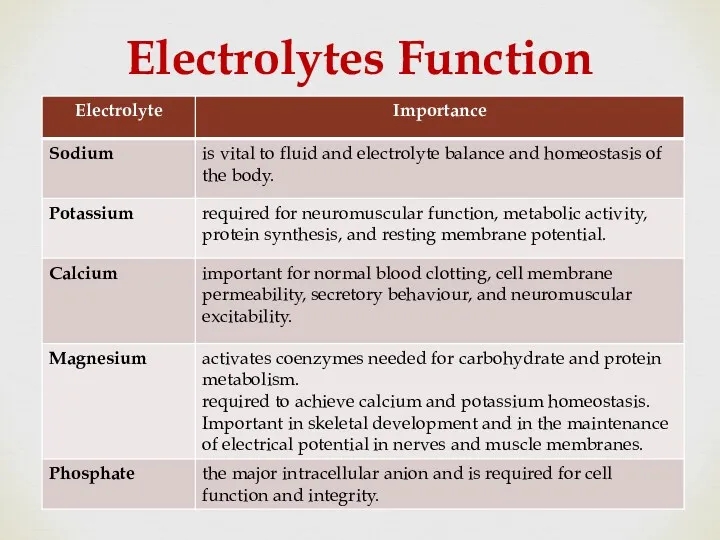
- 75. Electrolytes Function
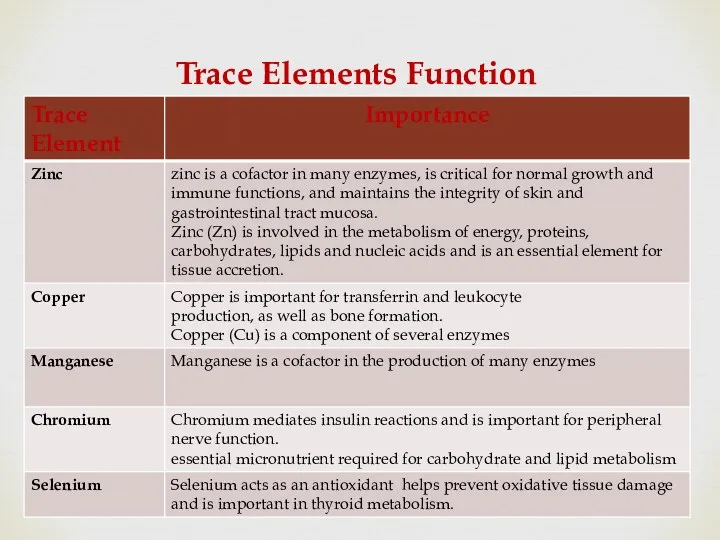
- 76. Trace Elements Function
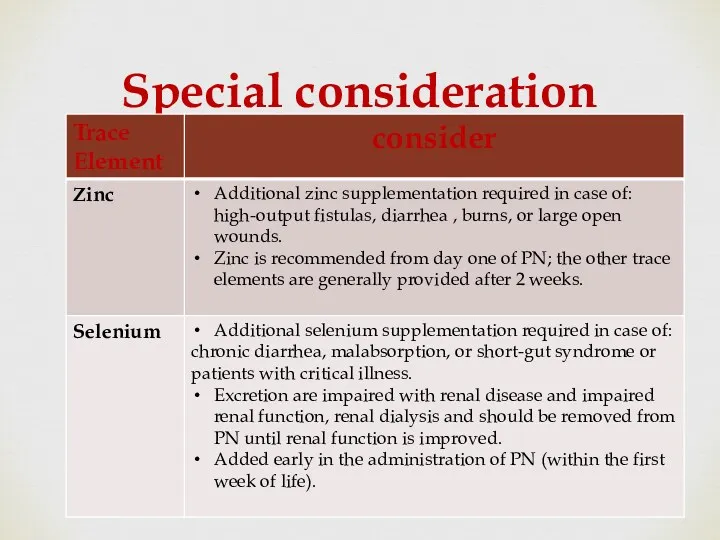
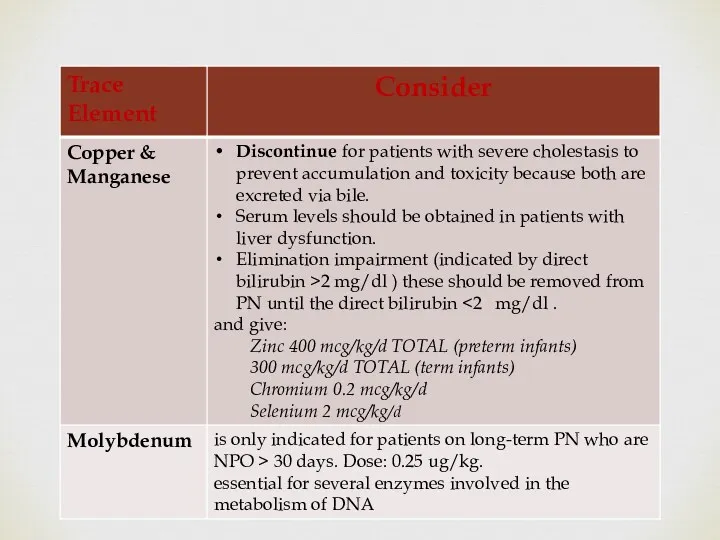
- 77. Special consideration
- 79. Medication Additives Continue Heparin: may be added to the TPN solutions in (0.5 - 1 unit/mL
- 80. There is no proven benefit of heparin for the prevention of thrombotic occlusion of CVC’s under
- 81. Medication Additives Continue Carnitine Should be added if a patient continues to require PN after 10
- 82. Medication Additives Continue H2 antagonist such as famotidine or ranitidine, may be added to the daily
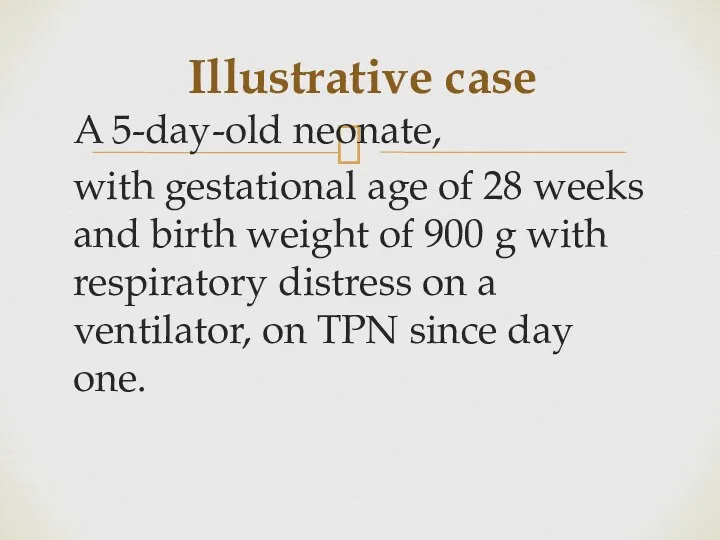
- 83. Illustrative case A 5-day-old neonate, with gestational age of 28 weeks and birth weight of 900
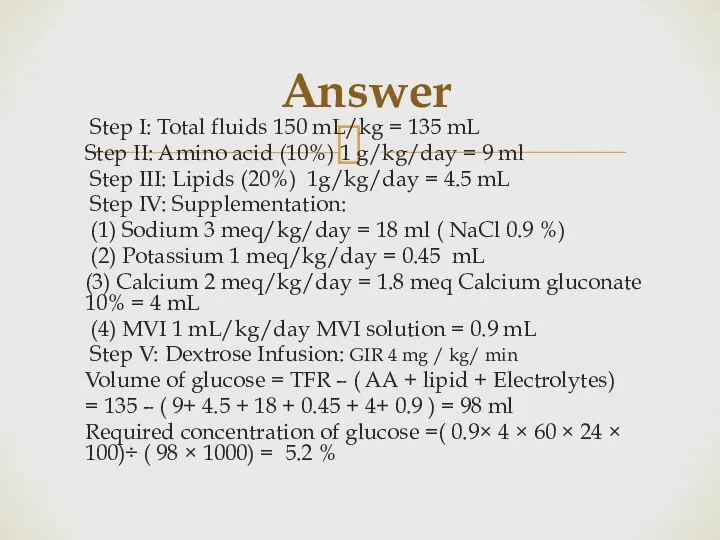
- 84. Answer Step I: Total fluids 150 mL/kg = 135 mL Step II: Amino acid (10%) 1
- 86. Скачать презентацию

 Перикардиты. Анатомия перикарда
Перикардиты. Анатомия перикарда Спадкові захворювання нервової системи
Спадкові захворювання нервової системи ВИЧ: вопросы и ответы
ВИЧ: вопросы и ответы Нейтропении у детей
Нейтропении у детей Николай Иванович Пирогов Русский хирург и анатом
Николай Иванович Пирогов Русский хирург и анатом Информационные технологии для фармацевтов
Информационные технологии для фармацевтов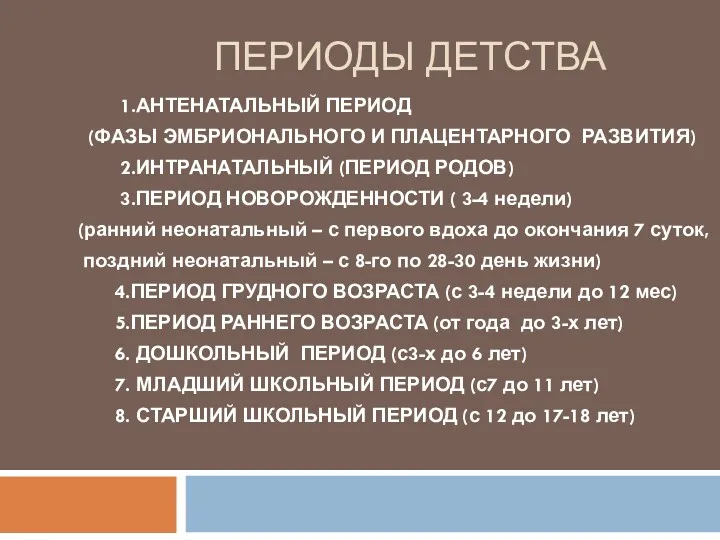 Периоды детства
Периоды детства Антипсихотики (нейролептики)
Антипсихотики (нейролептики) Глобальные риски и новейшие медицинские технологии
Глобальные риски и новейшие медицинские технологии Компрессионные синдромы шейного отдела позвоночника
Компрессионные синдромы шейного отдела позвоночника Жанұямен қарым – қатынаста жеткен жетістіктерді және қиыншылықтарды талдау
Жанұямен қарым – қатынаста жеткен жетістіктерді және қиыншылықтарды талдау Інсульт. Причини, симптоми інсульту, перша допомога, поради
Інсульт. Причини, симптоми інсульту, перша допомога, поради Крон ауруы
Крон ауруы Pancreatic Cancer
Pancreatic Cancer Особенности фармакокинетики и фармакодинамики при лечении аллергий
Особенности фармакокинетики и фармакодинамики при лечении аллергий ИБС. Стенокардия
ИБС. Стенокардия Нәрестелердің асфиксиясы
Нәрестелердің асфиксиясы Опухолевый рост
Опухолевый рост Кілегейлі қабықтар мен мүшелерде эпителий тінінің мамандануы
Кілегейлі қабықтар мен мүшелерде эпителий тінінің мамандануы Нарушения сна у младенцев и детей раннего возраста
Нарушения сна у младенцев и детей раннего возраста Анастезия задних верхних и нижнего луночкого нерва по П.М. Егорову
Анастезия задних верхних и нижнего луночкого нерва по П.М. Егорову Токсикология фосфорорганических соединений (ФОС)
Токсикология фосфорорганических соединений (ФОС) Анатомо-фізіологічні особливості сечовидільної системи у дітей
Анатомо-фізіологічні особливості сечовидільної системи у дітей Өлім, өлім белгілері
Өлім, өлім белгілері Ми қыртысының анатомиялық-гистологиялық құрылымы
Ми қыртысының анатомиялық-гистологиялық құрылымы Воспалительные процессы органов женской половой системы специфической этиологии
Воспалительные процессы органов женской половой системы специфической этиологии Болезнь Крона
Болезнь Крона Respiratory system
Respiratory system