Содержание
- 3. Cardiomyopathy (CM) is defined by WHO as ‘a disease of the myocardium associated with cardiac dysfunction’
- 4. The prognosis is poor. 40% of children presenting with symptomatic CM in the USA either receive
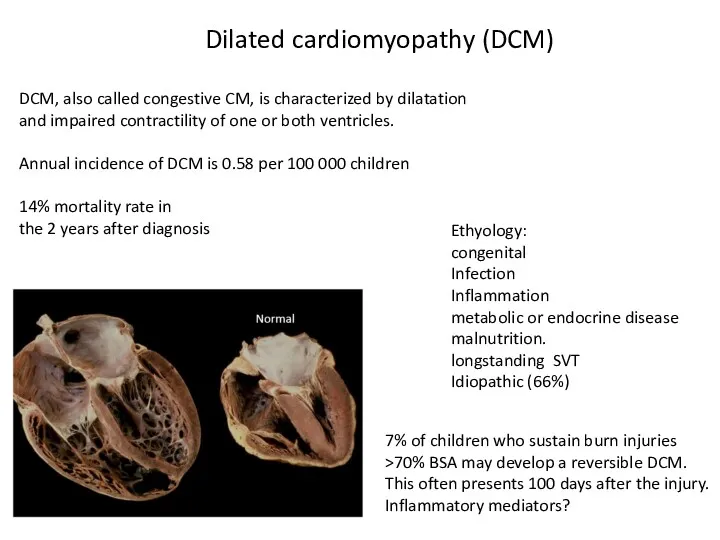
- 5. Dilated cardiomyopathy (DCM) DCM, also called congestive CM, is characterized by dilatation and impaired contractility of
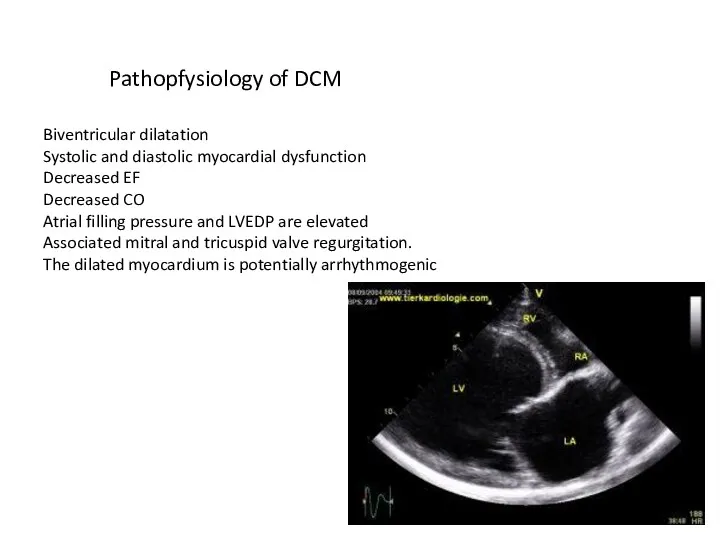
- 6. Pathopfysiology of DCM Biventricular dilatation Systolic and diastolic myocardial dysfunction Decreased EF Decreased CO Atrial filling
- 7. Preanesthetic management of DCM The enlarged heart ? extrinsic airway compression at the origin of the
- 8. Anesthetic management of DCM Optimization of coronary perfusion Maintain adequate diastolic pressure Adequate preload Maintenance of
- 9. Hypertrophic cardiomyopathy HCM More common in adults, the incidence is low in children (5/1,000,000). As patients
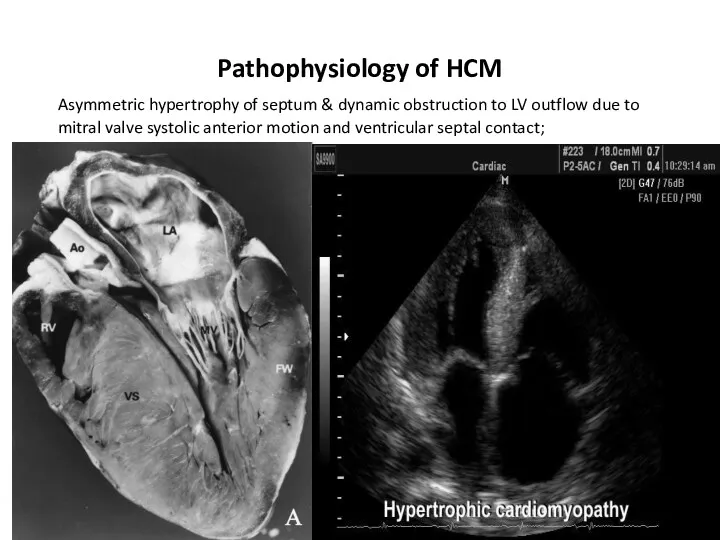
- 10. Pathophysiology of HCM Asymmetric hypertrophy of septum & dynamic obstruction to LV outflow due to mitral
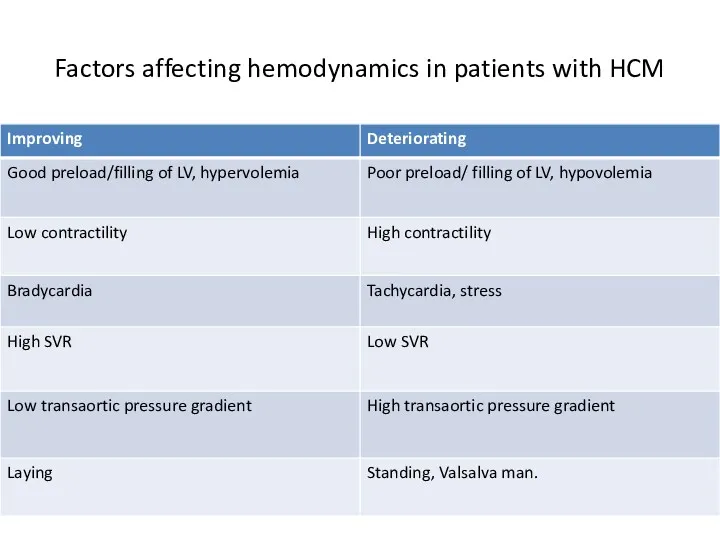
- 12. Factors affecting hemodynamics in patients with HCM
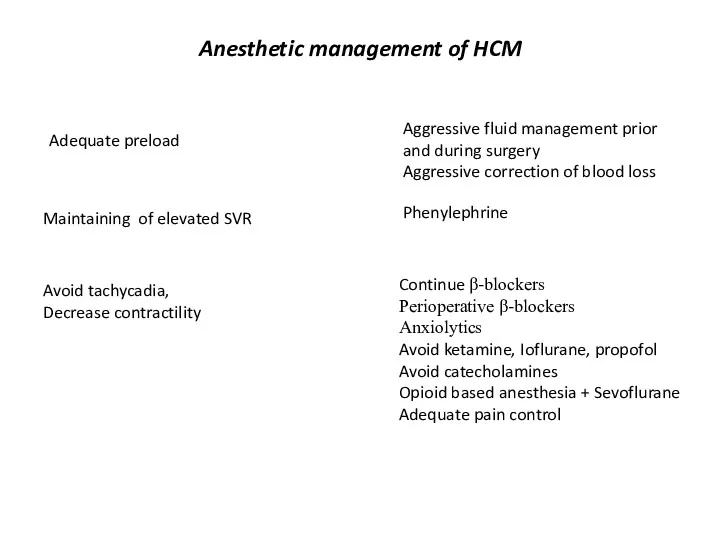
- 13. Anesthetic management of HCM Maintaining of elevated SVR Phenylephrine Adequate preload Aggressive fluid management prior and
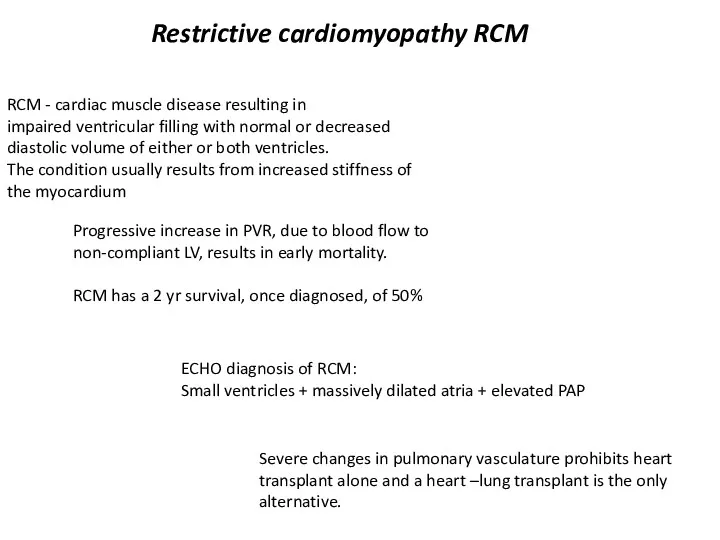
- 14. Restrictive cardiomyopathy RCM RCM - cardiac muscle disease resulting in impaired ventricular filling with normal or
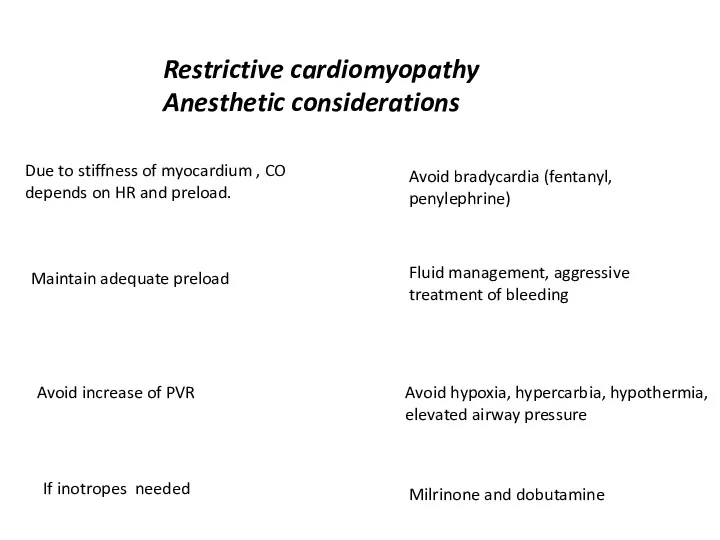
- 15. Restrictive cardiomyopathy Anesthetic considerations Due to stiffness of myocardium , CO depends on HR and preload.
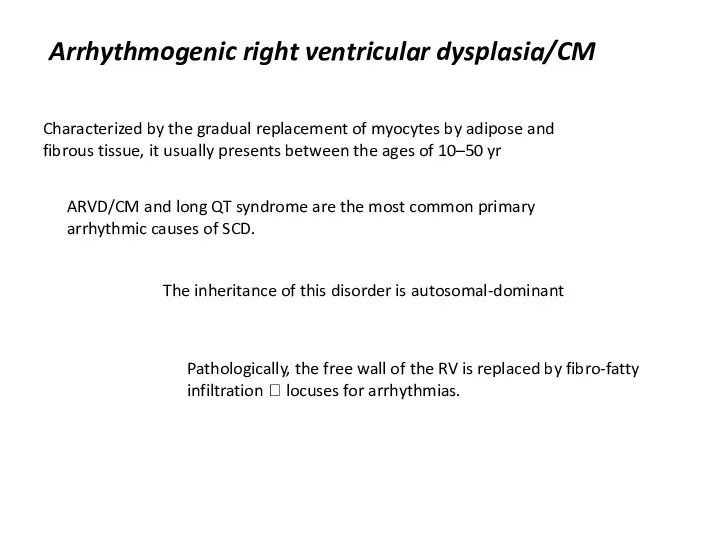
- 16. Arrhythmogenic right ventricular dysplasia/CM Characterized by the gradual replacement of myocytes by adipose and fibrous tissue,
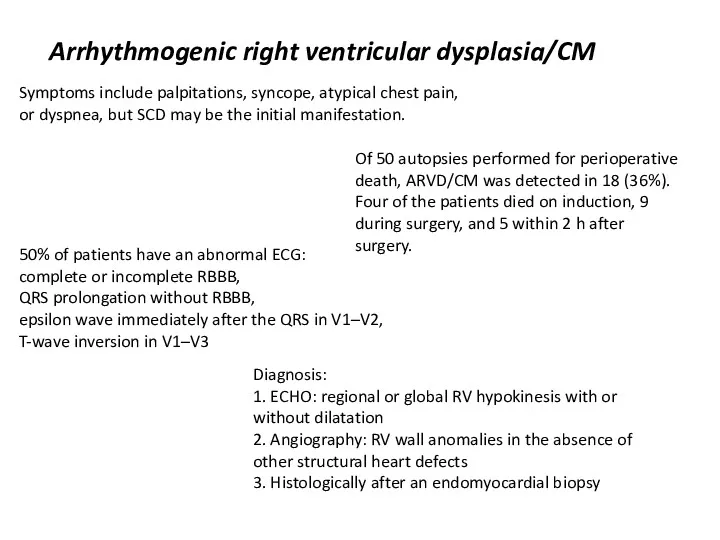
- 17. Arrhythmogenic right ventricular dysplasia/CM Symptoms include palpitations, syncope, atypical chest pain, or dyspnea, but SCD may
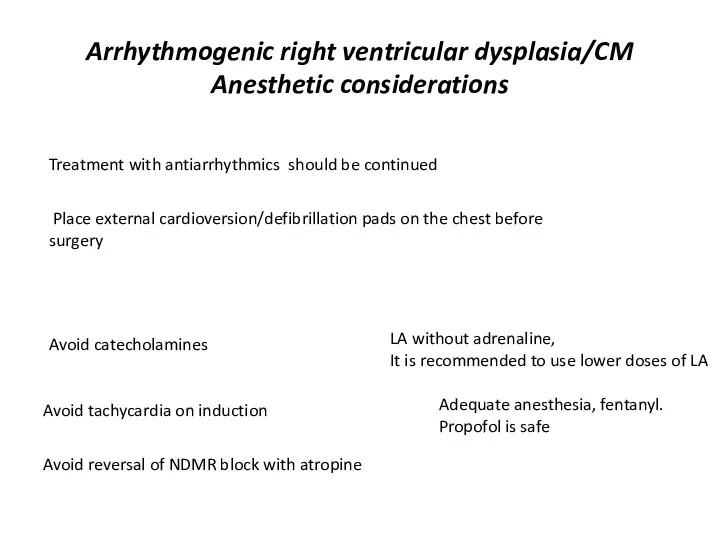
- 18. Arrhythmogenic right ventricular dysplasia/CM Anesthetic considerations Avoid catecholamines LA without adrenaline, It is recommended to use
- 20. Скачать презентацию

 Медицина в походе
Медицина в походе Пароксизмальная тахикардия
Пароксизмальная тахикардия Операции на органах шеи
Операции на органах шеи Сестринский процесс при подготовке больных к операции
Сестринский процесс при подготовке больных к операции Сочетанная травма груди и живота
Сочетанная травма груди и живота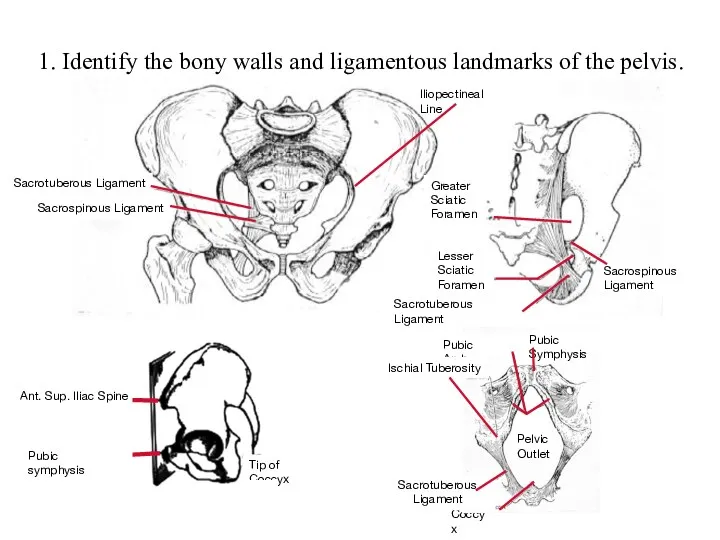 Identify the bony walls and ligamentous landmarks of the pelvis
Identify the bony walls and ligamentous landmarks of the pelvis БМСК жағдайында көмек көрсету қағидалары
БМСК жағдайында көмек көрсету қағидалары Нозокомиальные инфекции – от теории к практике
Нозокомиальные инфекции – от теории к практике Жедел аппендицит
Жедел аппендицит Хронические нагноительные заболевания легких
Хронические нагноительные заболевания легких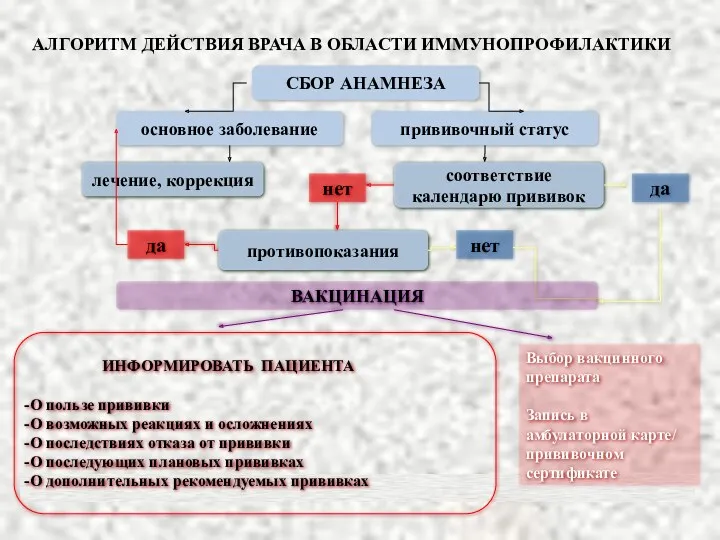 Алгоритм действия врача в области иммунопрофилактики
Алгоритм действия врача в области иммунопрофилактики Врожденный гипотиреоз
Врожденный гипотиреоз Гипотиреоз
Гипотиреоз Недоношенный ребенок – особенности ухода. Ранняя реабилитация недоношенного новорожденного
Недоношенный ребенок – особенности ухода. Ранняя реабилитация недоношенного новорожденного Балалардағы ауыз қуысы шырышты қабығының жіті және созылмалы кандидозы. Клиникасы, емі
Балалардағы ауыз қуысы шырышты қабығының жіті және созылмалы кандидозы. Клиникасы, емі ГОБУЗ ЦРБ ЗАТО г. Североморск
ГОБУЗ ЦРБ ЗАТО г. Североморск 1 декабря – Всемирный день борьбы со СПИДом
1 декабря – Всемирный день борьбы со СПИДом Спирография. Спирограмма
Спирография. Спирограмма Обращение товаров аптечного ассортимента (ТАА) на фармацевтическом рынке. Классификация ТАА. Фармацевтическое товароведение
Обращение товаров аптечного ассортимента (ТАА) на фармацевтическом рынке. Классификация ТАА. Фармацевтическое товароведение Поведенческие расстройства, связанные с физиологическими нарушениями. (Тема 3)
Поведенческие расстройства, связанные с физиологическими нарушениями. (Тема 3) Недоношенные дети
Недоношенные дети Терапиялық стоматология. Шыныталшықты штифттер. Құрамы, касиеттері. Қолдану көрсеткіштері және қолдану технологиясы
Терапиялық стоматология. Шыныталшықты штифттер. Құрамы, касиеттері. Қолдану көрсеткіштері және қолдану технологиясы День донора в Общественной палате Российской Федерации
День донора в Общественной палате Российской Федерации Кариес зубов. Причины и механизм образования. Основные теории и гипотезы кариеса (Миллер, Лукомский, Энтин, Шарпенак, Боровский)
Кариес зубов. Причины и механизм образования. Основные теории и гипотезы кариеса (Миллер, Лукомский, Энтин, Шарпенак, Боровский) Нәрестелердің асфиксиясы
Нәрестелердің асфиксиясы Алкогольдің адам организміне зияны
Алкогольдің адам организміне зияны Фармакологическая группа: сердечные гликозиды
Фармакологическая группа: сердечные гликозиды Анализ работы фельдшерско - акушерских пунктов Кировской области, 2016
Анализ работы фельдшерско - акушерских пунктов Кировской области, 2016