Содержание
- 2. Definitions Ulcer: A lesion on an epithelial surface (skin or mucous membrane) caused by superficial loss
- 3. Definitions Peptic Ulcer An ulcer of the alimentary tract mucosa, usually in the stomach or duodenum,
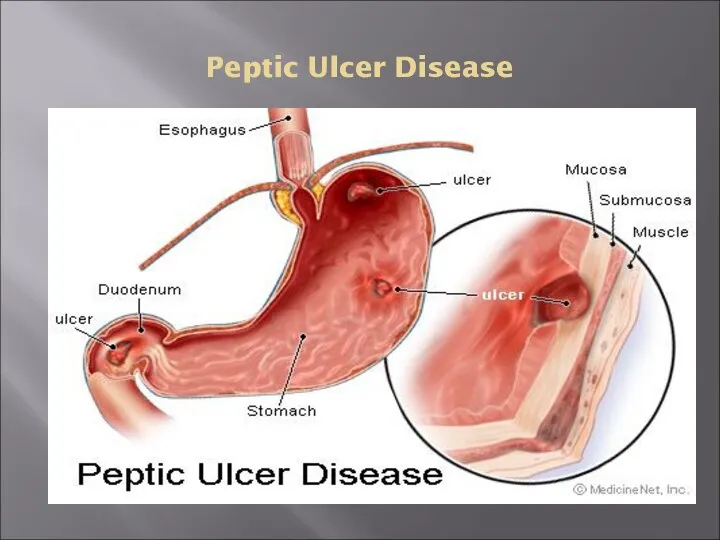
- 4. Peptic Ulcer Disease
- 5. Pathophysiology A peptic ulcer is a mucosal break, 3 mm or greater in size with depth,
- 6. Pathophysiology Two major variants in peptic ulcers are commonly encountered in the clinical practice: Duodenal Ulcer
- 7. Pathophysiology DU result from increased acid load to the duodenum due to: Increased acid secretion because
- 8. Pathophysiology DU result from increased acid load to the duodenum due to: Smoking impairing gastric mucosal
- 9. Pathophysiology GU results from the break down of gastric mucosa: Associated with gastritis affecting the body
- 10. Etiology The two most common causes of PUD are: Helicobacter pylori infection ( 70-80%) Non-steroidal anti-inflammatory
- 11. Etiology Other uncommon causes include: Gastrinoma (Gastrin secreting tumor) Stress ulceration (trauma, burns, critical illness) Viral
- 12. 1. Etiology – Helicobacter pylori
- 13. H.pylori Epidemiology One half of world’s population has H.pylori infection, with an estimated prevalence of 80-90
- 14. H.pylori as a cause of PUD The majority of PUD patients are H. pylori infected
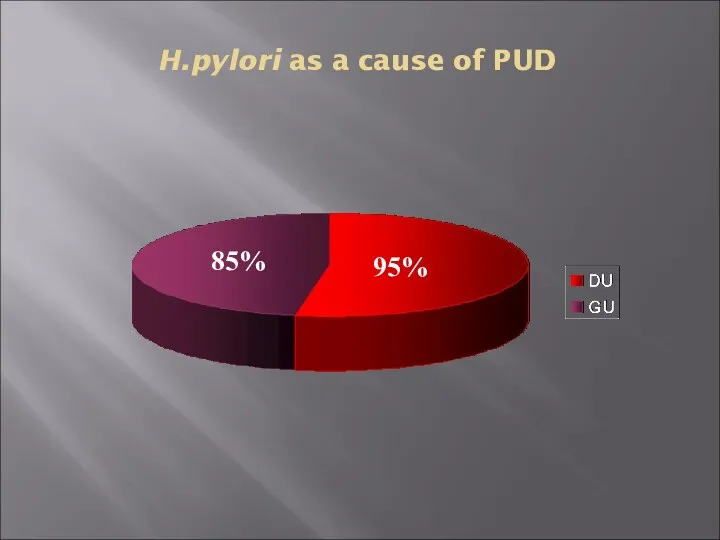
- 15. H.pylori as a cause of PUD 95% 85%
- 16. Carcinogenic effect of H. pylori H. pylori Host Factors Other environmental Factors Antral gastritis Pangastritis DU
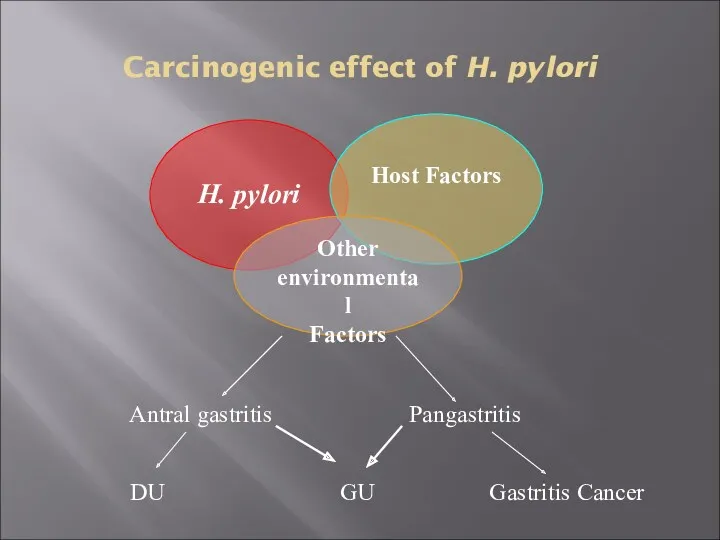
- 17. Type of NSAID & Risk of Ulcer
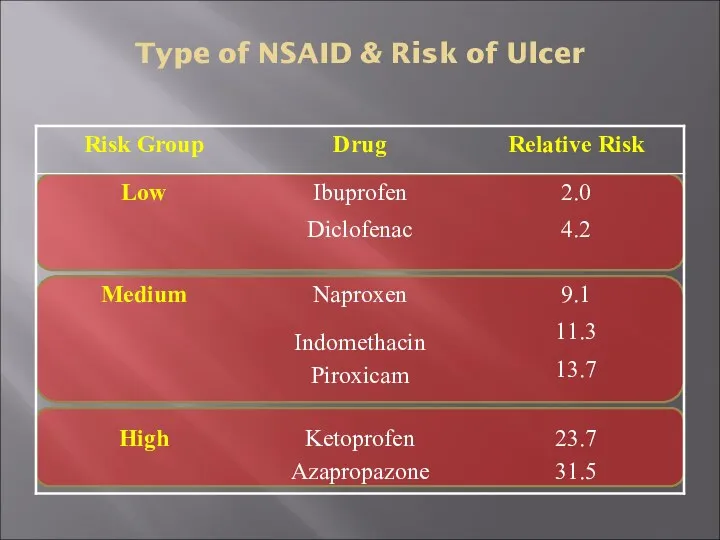
- 18. Clinical Presentation Recurrent epigastric pain (the most common symptom) Burning Occurs 1-3 hours after meals Relieved
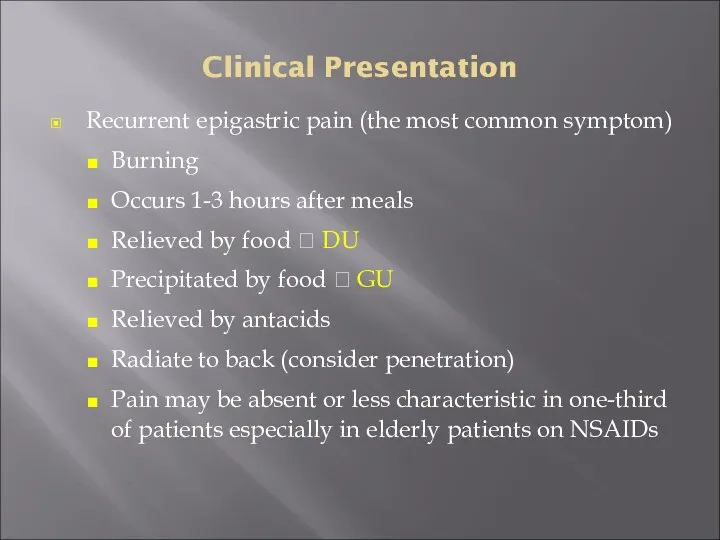
- 19. Clinical Presentation Nausea, Vomiting Dyspepsia, fatty food intolerance Chest discomfort Anorexia, weight loss especially in GU
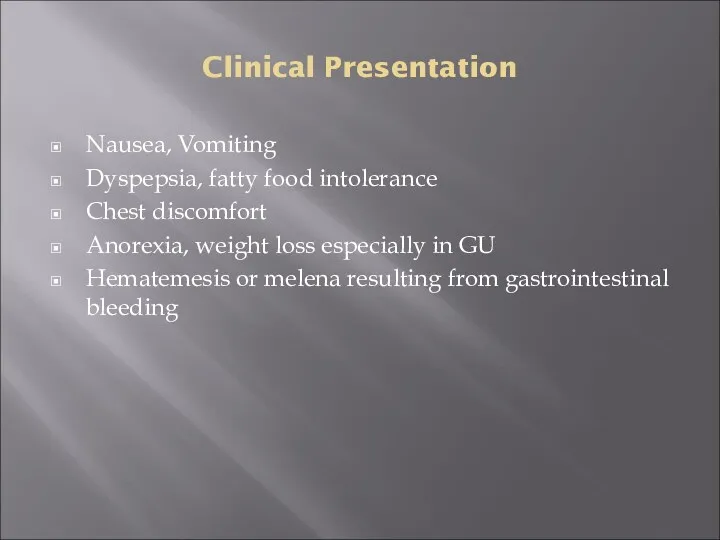
- 20. Diagnosis of PUD
- 21. Peptic Ulcer Disease Diagnosis: Diagnosis of ulcer Diagnosis of H. pylori
- 22. Diagnosis of PUD In most patients routine laboratory tests are usually unhelpful Diagnosis of PUD depends
- 23. Doudenal Ulcer on Endoscopy Doudenal Ulcer Normal doudenal bulb
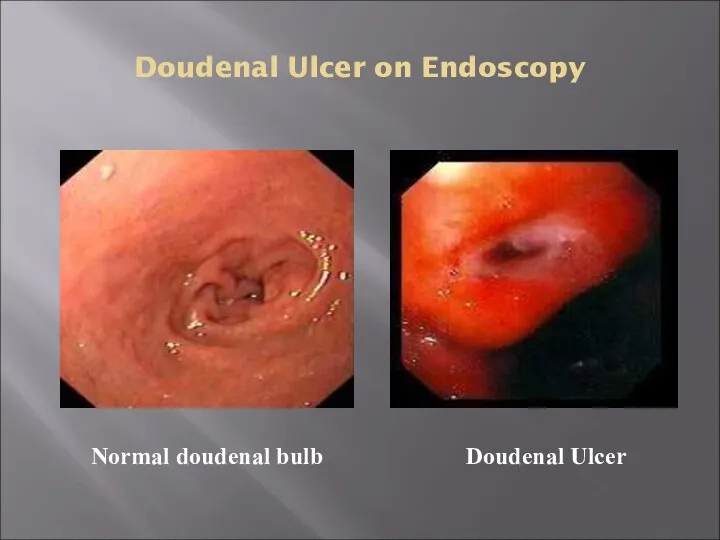
- 24. Gastric Ulcer on Endoscopy Chronic Gastric Ulcers
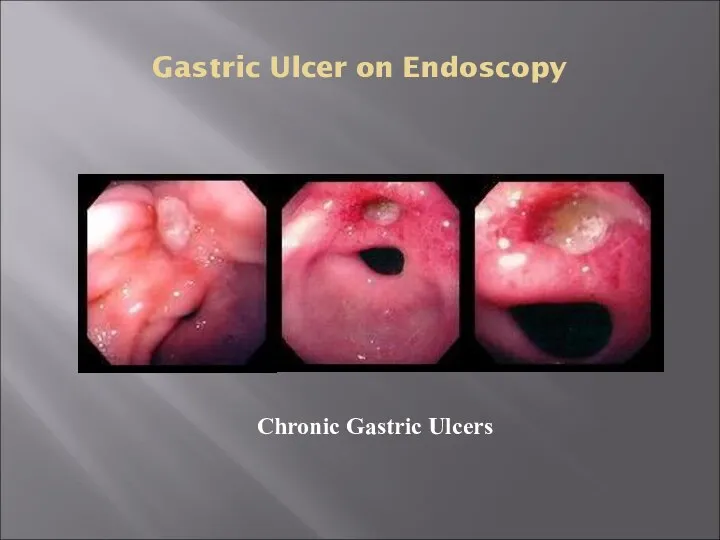
- 25. Diagnosis of H. pylori Non-invasive C13 or C14 Urea Breath Test Stool antigen test H. pylori
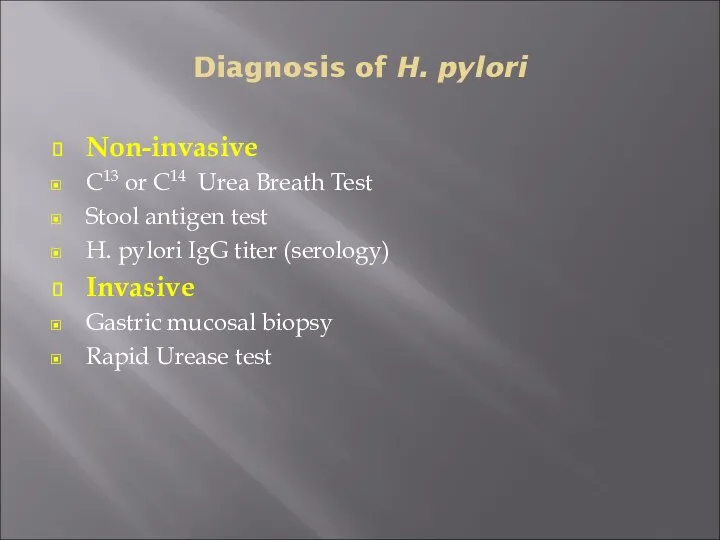
- 26. Diagnosis of H. pylori Non-invasive 1. C13 or C14 Urea Breath Test The best test for
- 27. Diagnosis of H. pylori Non-invasive Serology for H pylori Serum Antibodies (IgG) to H pylori (Not
- 28. Diagnosis of H. pylori Invasive Upper GI endoscopy Highly sensitive test Patient needs sedation Has both
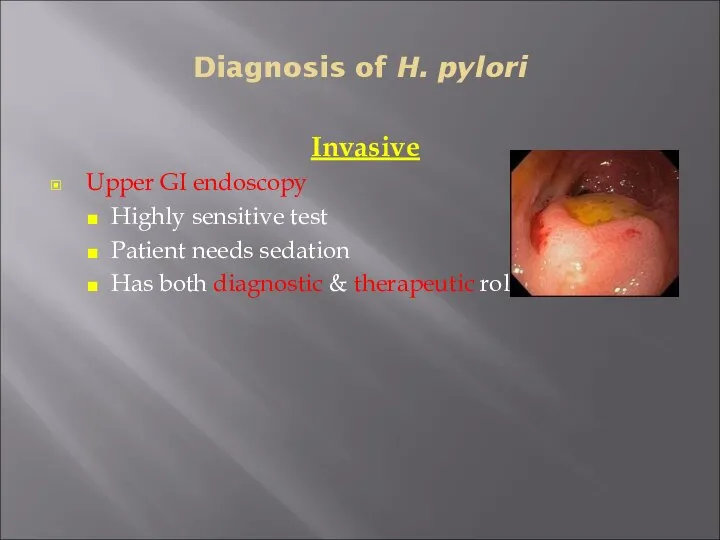
- 29. Diagnosis of H. pylori Invasive (endoscopy) Diagnostic: Detect the site and the size of the ulcer,
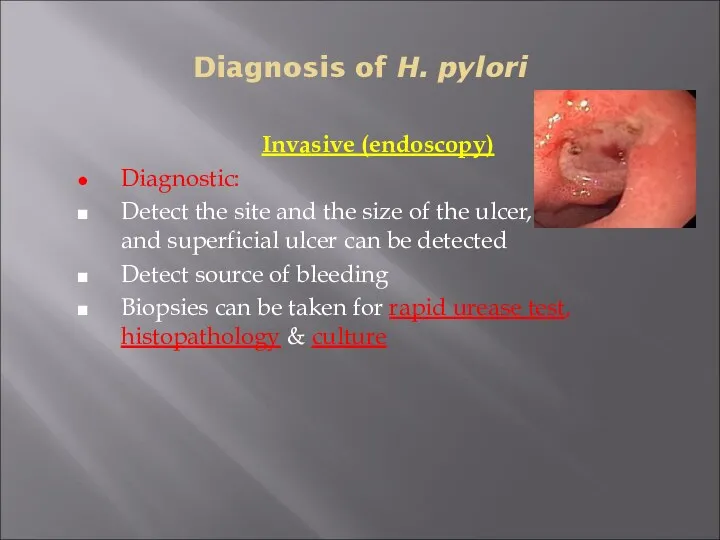
- 30. Diagnosis of H. pylori Invasive (endoscopy) Rapid urease test ( RUT) Considered the endoscopic diagnostic test
- 31. Diagnosis of H. pylori Invasive (endoscopy) * Histopathology Done if the rapid urease test result is
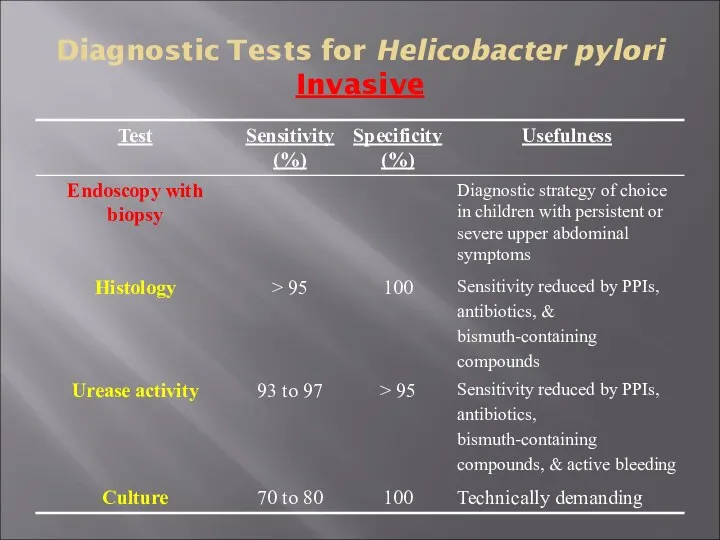
- 32. Diagnostic Tests for Helicobacter pylori Invasive
- 33. PUD – Complications Bleeding Perforation Gastric outlet or duodenal obstruction Chronic anemia
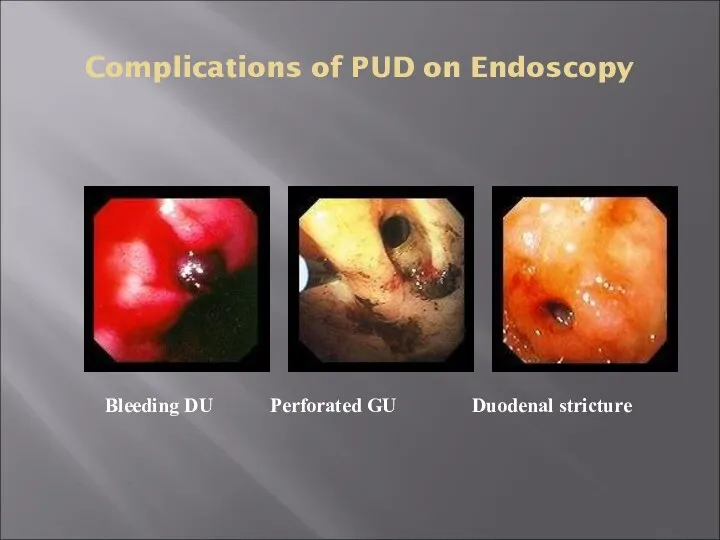
- 34. Complications of PUD on Endoscopy Bleeding DU Perforated GU Duodenal stricture
- 35. PUD Treatment
- 36. Treatment Goals Rapid relief of symptoms Healing of ulcer Preventing ulcer recurrences Reducing ulcer-related complications Reduce
- 37. General Strategy Treat complications aggressively if present Determine the etiology of ulcer Discontinue NSAID use if
- 38. General Strategy Smoking cessation should be encouraged If DU is diagnosed by endoscopy, RU testing of
- 39. Drugs Therapy H2-Receptors antagonists Proton pump inhibitors Cyto-protective agents Prostaglandin agonists Antacids Antibiotics for H. pylori
- 41. Скачать презентацию

 Противомикробные средства. Антисептики и дезинфицирующие средства
Противомикробные средства. Антисептики и дезинфицирующие средства Сосудистый шов
Сосудистый шов Анемії. Лейкози гострий і хронічний
Анемії. Лейкози гострий і хронічний Геморрагический шок в акушерстве
Геморрагический шок в акушерстве Жұқпалы аурулар эпидемиологиясы
Жұқпалы аурулар эпидемиологиясы Показания к переводу на искусственную вентиляцию легких. Параметры КЩС. Режимы вентиляции
Показания к переводу на искусственную вентиляцию легких. Параметры КЩС. Режимы вентиляции Пороки развития позвоночника
Пороки развития позвоночника Нейрофизиология. Двигательная функция ЦНС. (Лекция 8)
Нейрофизиология. Двигательная функция ЦНС. (Лекция 8) Анатомия и биомеханика ВНЧС
Анатомия и биомеханика ВНЧС Лечебно-профилактическое и лечебное питание
Лечебно-профилактическое и лечебное питание Общая фармакология
Общая фармакология Перечень действующих документов по профилактике инфекционных заболеваний
Перечень действующих документов по профилактике инфекционных заболеваний Блокады вымени
Блокады вымени Бронх обструктивті синдром
Бронх обструктивті синдром Острый гематогенный остеомиелит, эпифизарный остеомиелит
Острый гематогенный остеомиелит, эпифизарный остеомиелит Хроническая обструктивная болезнь легких
Хроническая обструктивная болезнь легких Остеология. Кости таза и нижних конечностей
Остеология. Кости таза и нижних конечностей Заболеваемость населения. Инвалидность. Физическое развитие. Социально значимые заболевания
Заболеваемость населения. Инвалидность. Физическое развитие. Социально значимые заболевания Умственная отсталость
Умственная отсталость АИТВ/ЖИТС туралы
АИТВ/ЖИТС туралы Постановка периферического венозного катетера
Постановка периферического венозного катетера Quản lí và đánh giá công nghệ y tế
Quản lí và đánh giá công nghệ y tế Острый гломерулонефрит
Острый гломерулонефрит Использование аэрозольного ингалятора флутиказона пропионата в сочетании с сальметеролом в лечении бронхиальной астмы
Использование аэрозольного ингалятора флутиказона пропионата в сочетании с сальметеролом в лечении бронхиальной астмы Синдром длительного сдавления (СДС)
Синдром длительного сдавления (СДС) Дерматомиозит. Симптомы, течение
Дерматомиозит. Симптомы, течение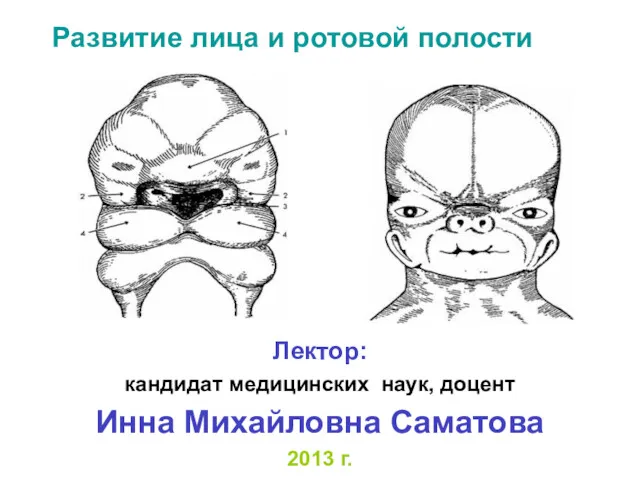 Развитие лица и ротовой полости
Развитие лица и ротовой полости Ведение беременных с бронхиальной астмой
Ведение беременных с бронхиальной астмой