Содержание
- 2. REHABILITATION FOR SHOULDER FRACTURES & SURGERIES Clavicle fractures Proximal head of humerus fractures Dr. ahmed Samir
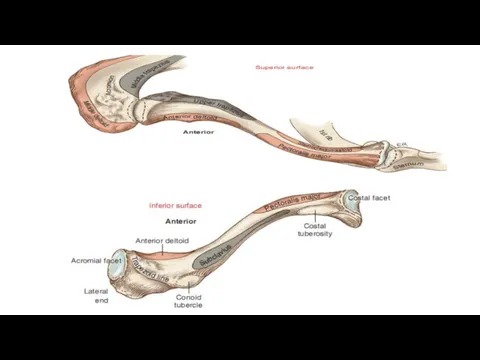
- 3. Clavicle fractures When one looks from above, it is evident that the shaft of the clavicle
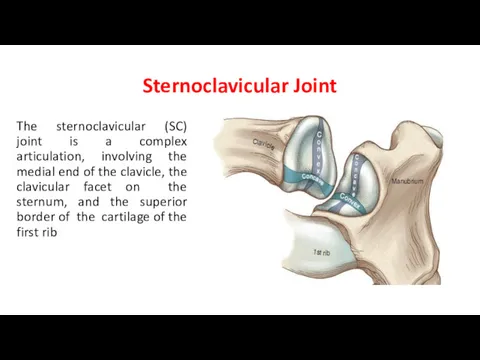
- 5. Sternoclavicular Joint The sternoclavicular (SC) joint is a complex articulation, involving the medial end of the
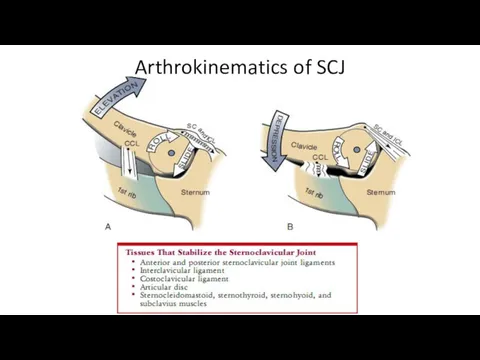
- 6. Arthrokinematics of SCJ
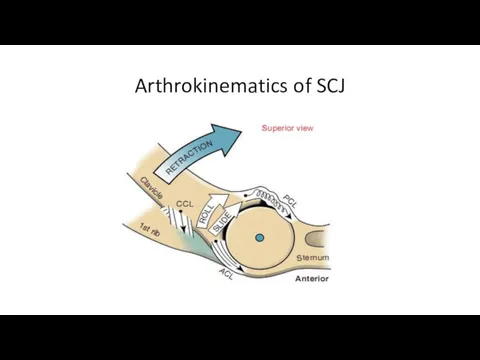
- 7. Arthrokinematics of SCJ
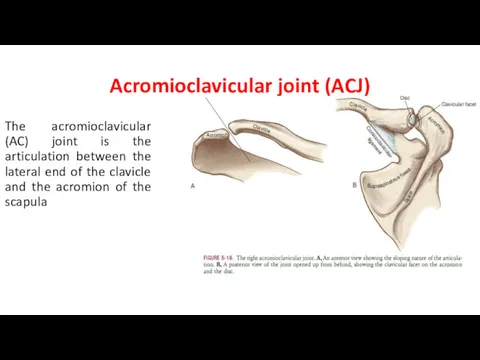
- 8. Acromioclavicular joint (ACJ) The acromioclavicular (AC) joint is the articulation between the lateral end of the
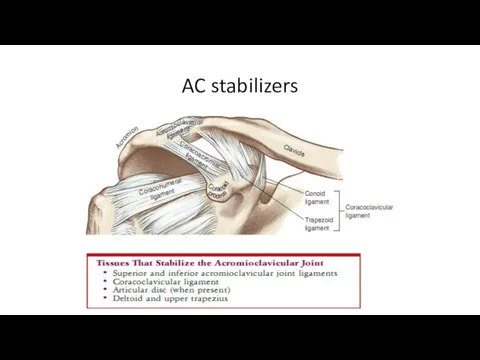
- 9. AC stabilizers
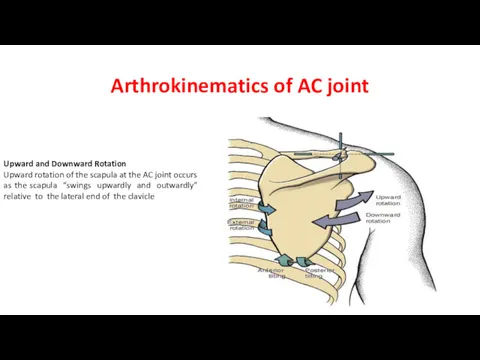
- 10. Arthrokinematics of AC joint Upward and Downward Rotation Upward rotation of the scapula at the AC
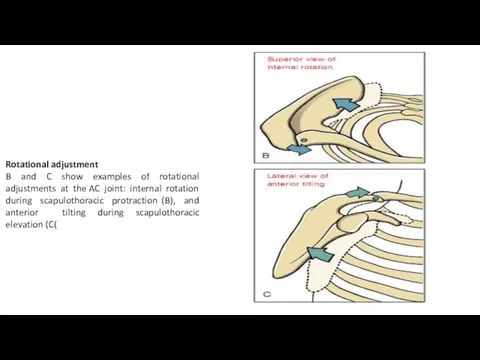
- 11. Rotational adjustment B and C show examples of rotational adjustments at the AC joint: internal rotation
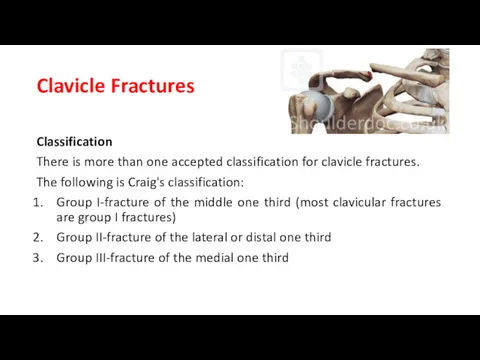
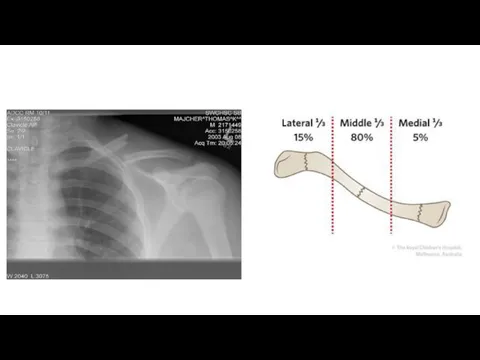
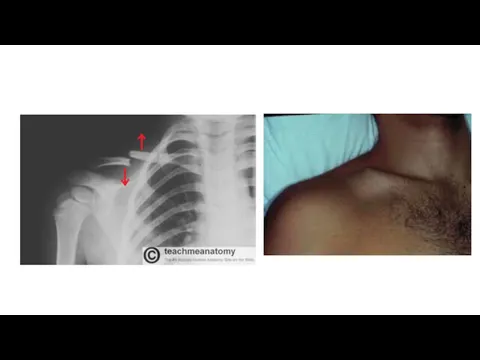
- 12. Clavicle Fractures Classification There is more than one accepted classification for clavicle fractures. The following is
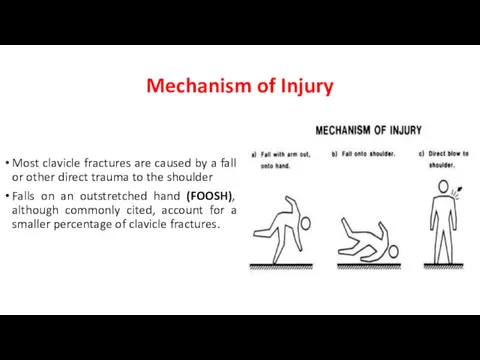
- 14. Mechanism of Injury Most clavicle fractures are caused by a fall or other direct trauma to
- 16. Treatment Goals Range of Motion Restore and improve the range of motion of the shoulder girdle.
- 17. 3. Functional Goals Improve and restore the function of the shoulder for activities of daily living
- 18. Treatment methods Sling or Supportive Immobilization This is the method of choice for most clavicle fractures.
- 19. Arm sling Figure-of-eight bracing
- 20. TREATMENT Treatment: Early to Immediate (Day of Injury to One Week) BONE HEALING Stability at fracture
- 21. Physical Examination Check for capillary refill. Sensory evaluation. The active and passive range of motion of
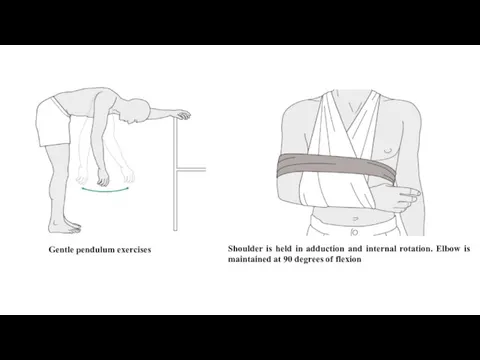
- 22. Prescription Precautions: Shoulder is held in adduction and internal rotation. Elbow is maintained at 90 degrees
- 23. Prescription Functional Activities: Personal hygiene The uninvolved extremity is used in self-care and personal hygiene. Bed
- 24. Treatment: 2 to 4 Weeks Stability at fracture site: None to minimal Stage of bone healing:
- 25. Prescription Precautions: The same as previous weeks. Range of Motion: Gentle pendulum exercises to the shoulder
- 26. Shoulder is held in adduction and internal rotation. Elbow is maintained at 90 degrees of flexion
- 27. Treatment: 4 to 6 weeks BONE HEALING Stability at fracture site: with bridging callus the fracture
- 28. Prescription Precautions: At the end of 6 weeks, once there is good callus formation and the
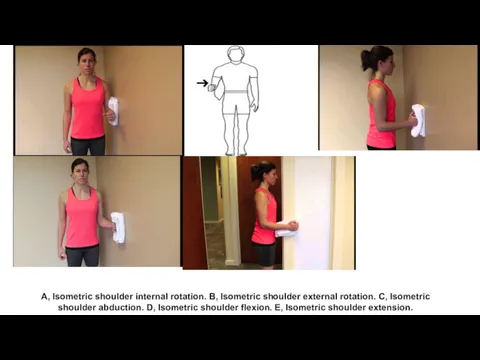
- 29. Prescription Muscle Strength: Start isometric exercises to the rotator cuff and deltoids. Functional Activities: The patient
- 30. A, Isometric shoulder internal rotation. B, Isometric shoulder external rotation. C, Isometric shoulder abduction. D, Isometric
- 31. Treatment: 6 to 8 Weeks BONE HEALING Stability at fracture site: with bridging callus the fracture
- 32. Prescription Precautions: Avoid contact sports. Range of Motion: active range of motion in all planes. Muscle
- 33. Treatment: 8 to 12 Weeks BONE HEALING Stability at fracture site: Stable. Stage of bone healing:
- 34. Prescription Precautions: Contact sports should be avoided for approximately 2 months. Range of Motion: Full ROM
- 35. Proximal Humeral Fractures Definition Fractures of the proximal end of the humerus involve the humeral head,
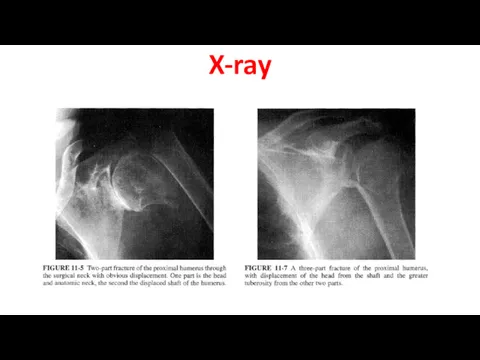
- 36. (above, left) Impacted proximal humeral fracture, also considered a one part fracture (Neer classification). A two-part
- 37. Four-part fracture of the proximal humerus. One part is the shaft, the second part the head,
- 38. X-ray
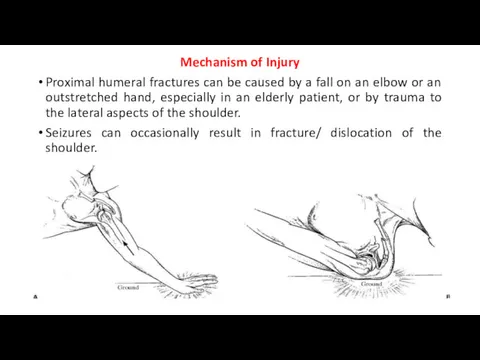
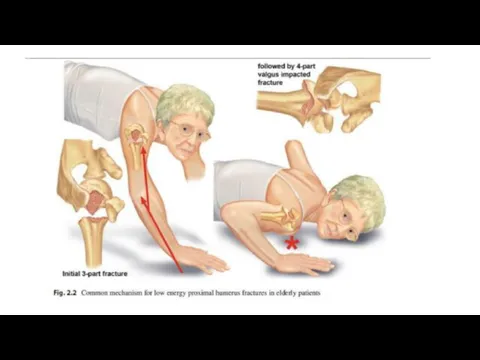
- 39. Mechanism of Injury Proximal humeral fractures can be caused by a fall on an elbow or
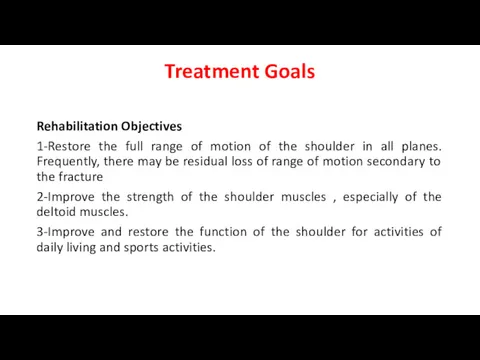
- 41. Treatment Goals Rehabilitation Objectives 1-Restore the full range of motion of the shoulder in all planes.
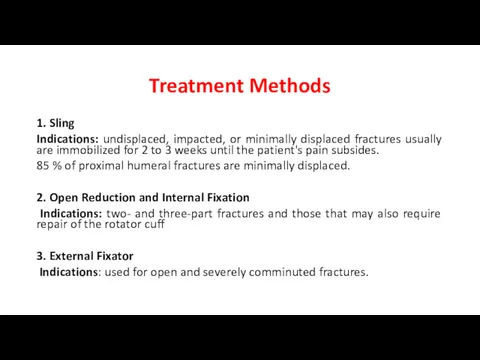
- 42. Treatment Methods 1. Sling Indications: undisplaced, impacted, or minimally displaced fractures usually are immobilized for 2
- 43. Expected Time of Bone Healing 6 to 8 weeks. Expected Duration of Rehabilitation 12 weeks to
- 44. TREATMENT Treatment: Early (Day of Injury to One Week) BONE HEALING Stability at fracture site: None.
- 45. Prescription Precautions: Avoid shoulder motion. Range of Motion: None at the shoulder and elbow. Gentle pendulum
- 46. Prescription Functional Activities: One-handed activities with the uninvolved extremity. The patient needs assistance in dressing, grooming,
- 47. Treatment: 2 to 4 Weeks BONE HEALING Stability at fracture site: None to minimal. Stage of
- 48. Applying moist heat before and ice after exercises minimizes swelling. The patient should do ball-squeezing exercises
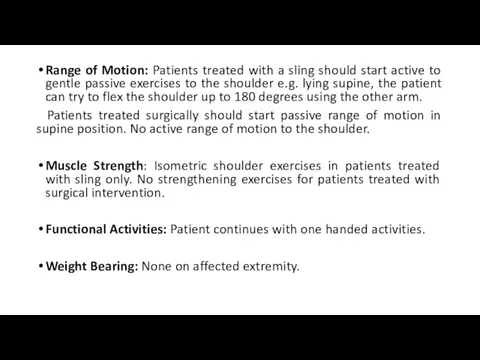
- 49. Range of Motion: Patients treated with a sling should start active to gentle passive exercises to
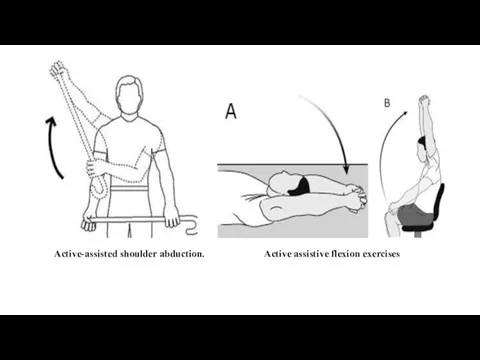
- 50. Active-assisted shoulder abduction. Active assistive flexion exercises
- 51. Treatment: 4 to 6 Weeks BONE HEALING Stability at fracture site: With bridging callus, the fracture
- 52. •Internal/external rotation-limited , Elbow-full range of motion. •Surgically treated patients may continue with passive ROM exercises.
- 53. wall-climbing exercises Codman’s pendulum.
- 54. Treatment: 6 to 8 Weeks BONE HEALING Stability at fracture site: With bridging callus, the fracture
- 55. Prescription Precautions: Avoid forced range of motion. Range of Motion: Active, active-assistive, and passive range of
- 56. Treatment: 8 to 12 Weeks BONE HEALING Stability at fracture site: stable. Stage of bone healing:
- 57. References David J. Magee, Pathology and Intervention in Musculoskeletal Rehabilitation , 2nd ed. 2016 Rehabilitation for
- 59. Скачать презентацию







 Мягкие лекарственные формы
Мягкие лекарственные формы Об утверждении Порядка оказания медицинской помощи взрослому населению по профилю анестезиология и реаниматология
Об утверждении Порядка оказания медицинской помощи взрослому населению по профилю анестезиология и реаниматология Реанимации новорожденных
Реанимации новорожденных Особенности фармакокинетики и фармакодинамики при лечении аллергий
Особенности фармакокинетики и фармакодинамики при лечении аллергий Фармакологические средства, влияющие на передачу возбуждения в холинэргических синапсах
Фармакологические средства, влияющие на передачу возбуждения в холинэргических синапсах Бронхиальная астма
Бронхиальная астма Қазақстан Республикасының электронды үкіметі. Қазақстан Республикасының электронды үкіметі порталының құрылымы және қызметі
Қазақстан Республикасының электронды үкіметі. Қазақстан Республикасының электронды үкіметі порталының құрылымы және қызметі Сахарный диабет. Заболевания щитовидной железы. Ожирение
Сахарный диабет. Заболевания щитовидной железы. Ожирение Косметический массаж
Косметический массаж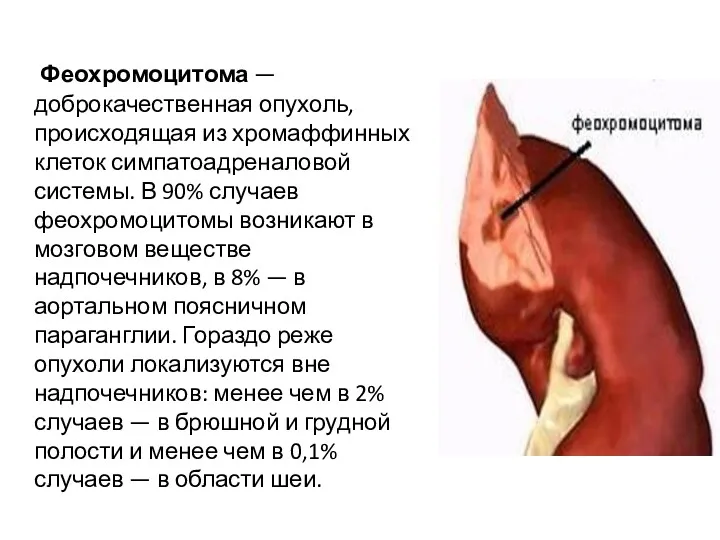 Доброкачественная опухоль феохромоцитома
Доброкачественная опухоль феохромоцитома Топографическая анатомия и оперативная хирургия тонкой и толстой кишки
Топографическая анатомия и оперативная хирургия тонкой и толстой кишки Симптомы заболеваний почек
Симптомы заболеваний почек Балалардағы бас миы мен жұлынның қатерлі ісіктері
Балалардағы бас миы мен жұлынның қатерлі ісіктері Заболевания надпочечников та гипофиза. Этиология. Патогенез. Клиника. Диагностика. Лечение
Заболевания надпочечников та гипофиза. Этиология. Патогенез. Клиника. Диагностика. Лечение Целиакия. Глютеновая энтеропатия
Целиакия. Глютеновая энтеропатия Принципы организации медицины катастроф
Принципы организации медицины катастроф Антисептики и дезинфицирующие средства. Антибактериальные химиотерапевтические средства
Антисептики и дезинфицирующие средства. Антибактериальные химиотерапевтические средства Сепсис та септичний шок
Сепсис та септичний шок Физиология пищевода. Глотание. Лекция
Физиология пищевода. Глотание. Лекция Двумерная эхокардиография
Двумерная эхокардиография Предметно-количественный учет лекарственных средств для медицинского применения
Предметно-количественный учет лекарственных средств для медицинского применения 24 марта – Всемирный день борьбы с туберкулезом
24 марта – Всемирный день борьбы с туберкулезом Физиология сердца
Физиология сердца Понятие о кариесе и его осложнениях. Хроническая стоматогенная интоксикация и сенсибилизация организма
Понятие о кариесе и его осложнениях. Хроническая стоматогенная интоксикация и сенсибилизация организма Предмет та завдання патофізіології. Методи патофізіологічних досліджень. Вчення про хворобу, етіологія і патогенез
Предмет та завдання патофізіології. Методи патофізіологічних досліджень. Вчення про хворобу, етіологія і патогенез Лимфалық ісіктер БМСК жағдайында диагнозын анықтау
Лимфалық ісіктер БМСК жағдайында диагнозын анықтау Неотложные состояния в неврологии
Неотложные состояния в неврологии Нарушение равновесия жидких сред, расстройства крово- и лимфообращения
Нарушение равновесия жидких сред, расстройства крово- и лимфообращения