Содержание
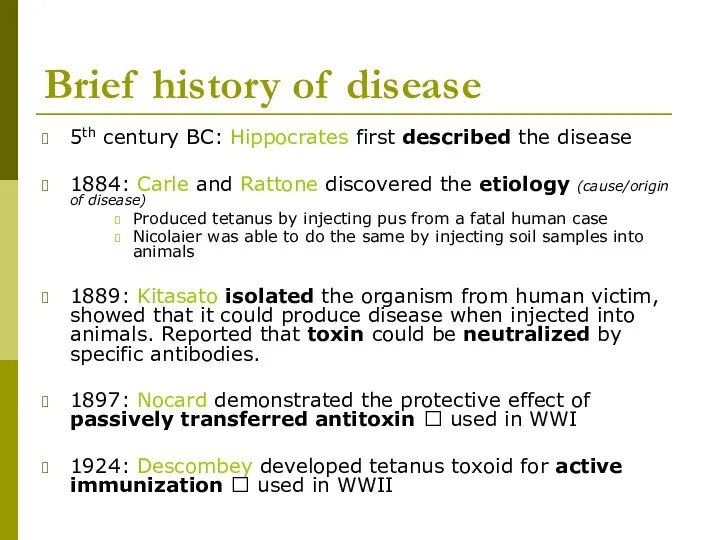
- 2. Brief history of disease 5th century BC: Hippocrates first described the disease 1884: Carle and Rattone
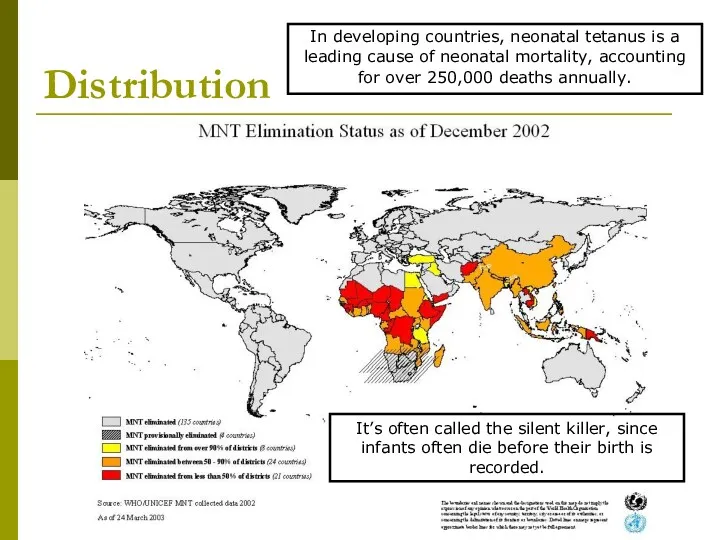
- 3. Distribution In developing countries, neonatal tetanus is a leading cause of neonatal mortality, accounting for over
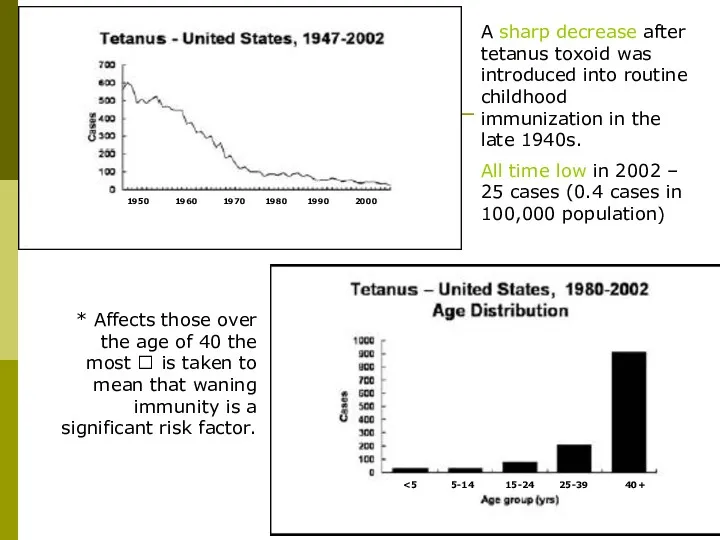
- 4. 1950 5-14 15-24 25-39 40+ A sharp decrease after tetanus toxoid was introduced into routine childhood
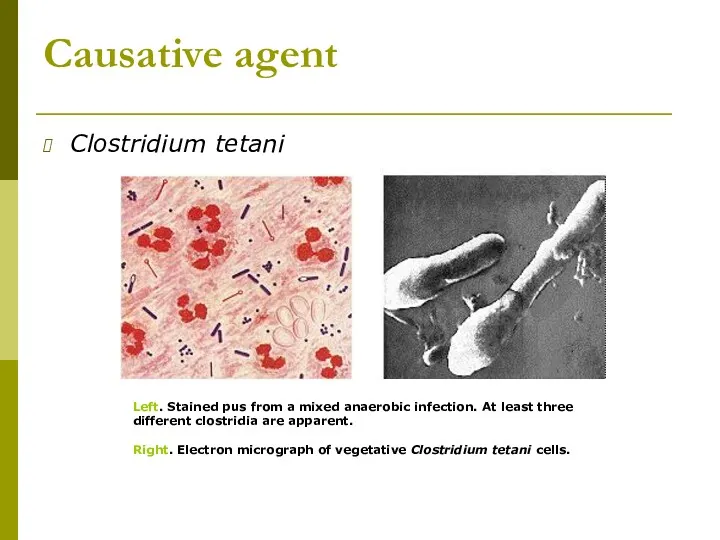
- 5. Causative agent Clostridium tetani Left. Stained pus from a mixed anaerobic infection. At least three different
- 6. Morphology & Physiology Relatively large, Gram-positive, rod-shaped bacteria Spore-forming, anaerobic. Found in soil, especially heavily-manured soils,
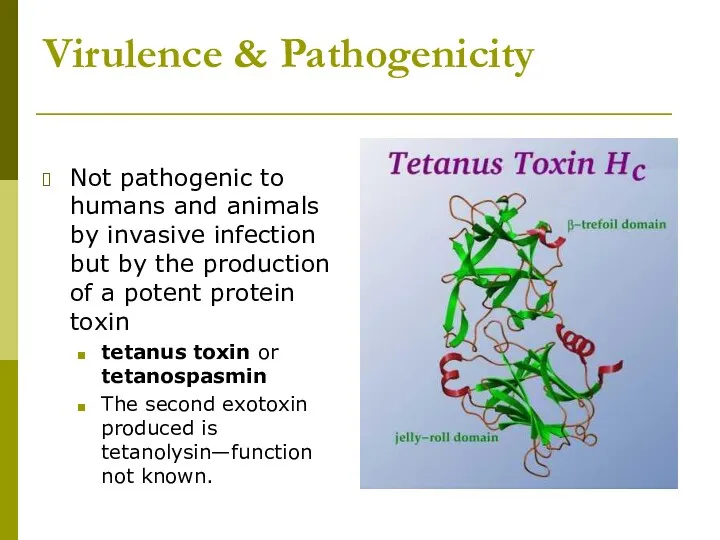
- 7. Virulence & Pathogenicity Not pathogenic to humans and animals by invasive infection but by the production
- 8. Tetanus toxin Produced when spores germinate and vegetative cells grow after gaining access to wounds. The
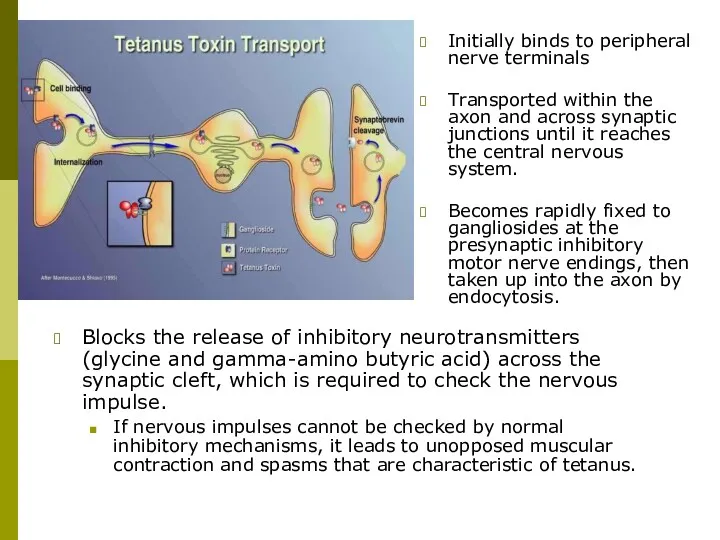
- 9. Initially binds to peripheral nerve terminals Transported within the axon and across synaptic junctions until it
- 10. Methods of transmission C. tetani can live for years as spores in animal feces and soil.
- 11. Symptoms Tetanic seizures (painful, powerful bursts of muscle contraction) if the muscle spasms affect the larynx
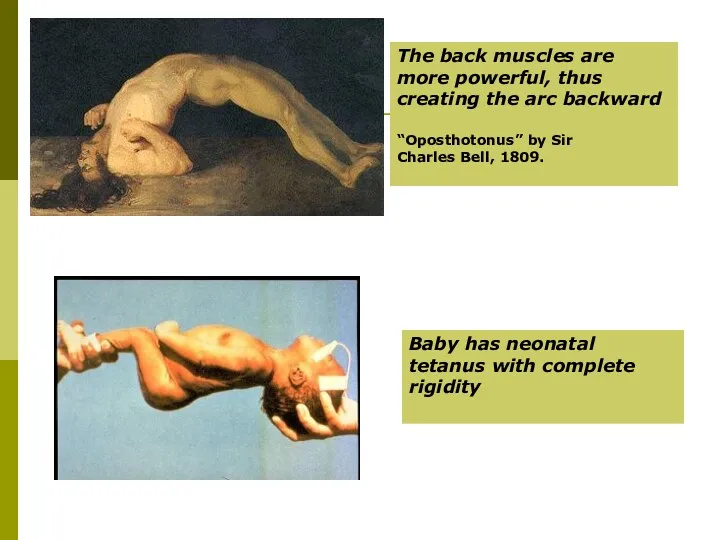
- 12. The back muscles are more powerful, thus creating the arc backward “Oposthotonus” by Sir Charles Bell,
- 13. Types of tetanus: local, cephalic, generalized, neonatal Incubation period: 3-21 days, average 8 days. Uncommon types:
- 14. Most common types: Generalized tetanus descending pattern: lockjaw ? stiffness of neck ? difficulty swallowing ?
- 15. Methods of diagnosis Based on the patient’s account and physical findings that are characteristic of the
- 16. Clinical treatment If treatment is not sought early, the disease is often fatal. The bacteria are
- 17. Method of prevention - immunization A person recovering from tetanus should begin active immunization with tetanus
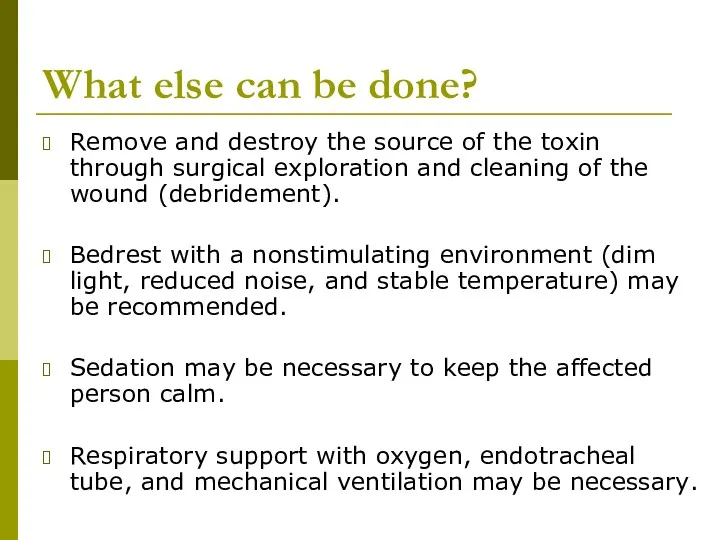
- 18. What else can be done? Remove and destroy the source of the toxin through surgical exploration
- 20. Скачать презентацию
 Геморрагический васкулит
Геморрагический васкулит Гипертонический криз
Гипертонический криз Кіші жас балалардығы жедел аппендицттің ағымының ерекшелігі
Кіші жас балалардығы жедел аппендицттің ағымының ерекшелігі Физикалық қауіпті және зиянды өндірістік факторлар
Физикалық қауіпті және зиянды өндірістік факторлар Оценка собственного физического развития
Оценка собственного физического развития Гигиеническая оценка микроклимата помещения
Гигиеническая оценка микроклимата помещения Механическая желтуха
Механическая желтуха Питание и беременность
Питание и беременность Абсцессы и флегмоны скуловой области
Абсцессы и флегмоны скуловой области Эфференттік иннервацияға әсер ететін заттар. Холинергиялық заттар. Адренергиялық заттар
Эфференттік иннервацияға әсер ететін заттар. Холинергиялық заттар. Адренергиялық заттар Ведение беременности и родов при синдроме портальной гипертензии
Ведение беременности и родов при синдроме портальной гипертензии Лейкоз ауруы кезіндегі зертханалық әдістер
Лейкоз ауруы кезіндегі зертханалық әдістер A clinical case of Renal cell carcinoma
A clinical case of Renal cell carcinoma Сведения о медицинской организации. Форма № 30
Сведения о медицинской организации. Форма № 30 Ризикована поведінка
Ризикована поведінка История неврологии
История неврологии Гепатомегалия и гепатолиенальный синдром. Лечение хронических гепатитов, циррозов печени
Гепатомегалия и гепатолиенальный синдром. Лечение хронических гепатитов, циррозов печени 20231213_9klass_immunitet
20231213_9klass_immunitet Болезнь Лайма
Болезнь Лайма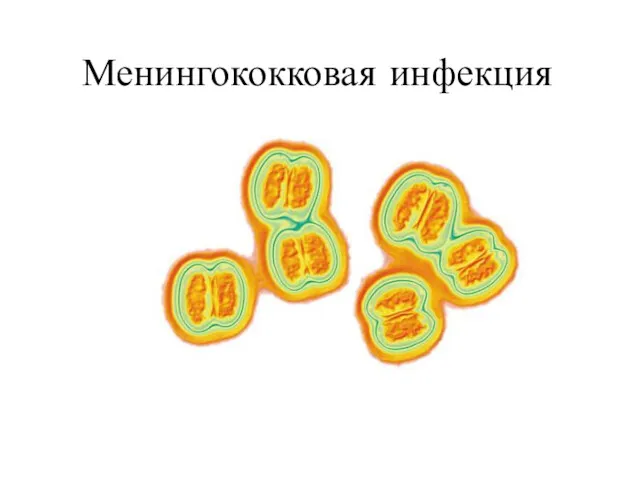 Менингококковая инфекция
Менингококковая инфекция Массаж при нарушениях развития центральной нервной системы. ДЦП
Массаж при нарушениях развития центральной нервной системы. ДЦП Элементы возрастной психологии и их учет в деятельности врача
Элементы возрастной психологии и их учет в деятельности врача Десмургия
Десмургия Жарақат және жарақат түрлері
Жарақат және жарақат түрлері Организация инфекционного контроля и инфекционной безопасности пациентов и медперсонала на примере отделения терапевтического
Организация инфекционного контроля и инфекционной безопасности пациентов и медперсонала на примере отделения терапевтического История болезни: множественная миома матки. Полип эндометрия
История болезни: множественная миома матки. Полип эндометрия Балаларда ас корыту жуйесі бұзылыстарының семиотикасы мен синдромдары
Балаларда ас корыту жуйесі бұзылыстарының семиотикасы мен синдромдары Суд над наркотиками
Суд над наркотиками