Содержание
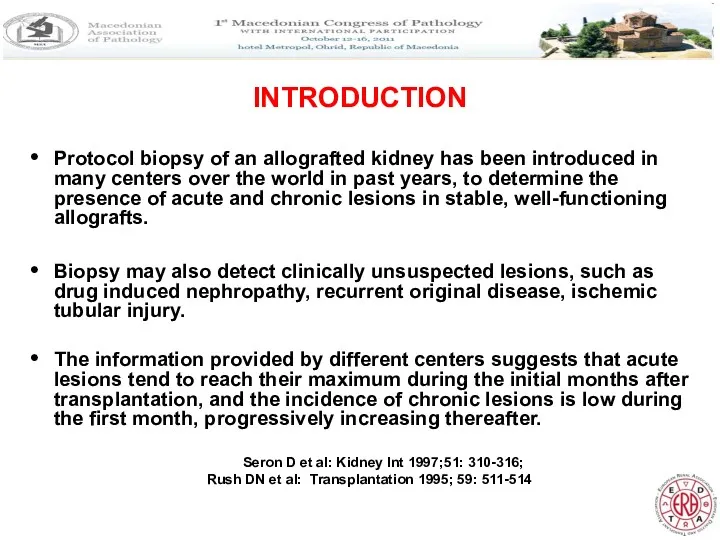
- 2. INTRODUCTION Protocol biopsy of an allografted kidney has been introduced in many centers over the world
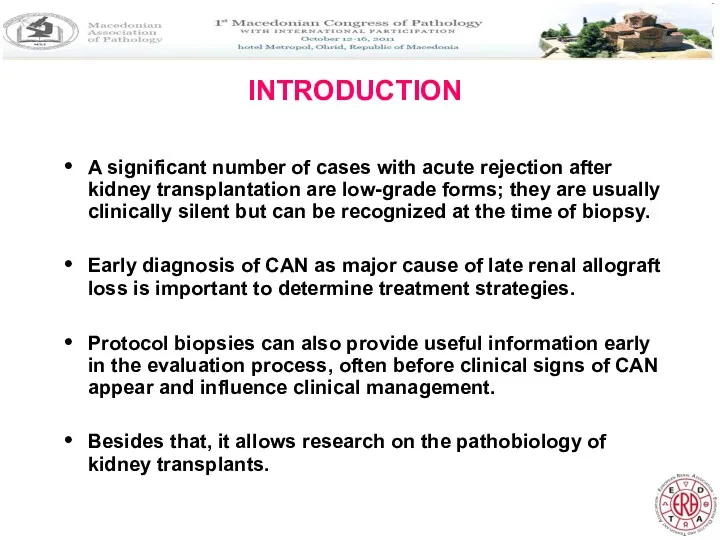
- 3. INTRODUCTION A significant number of cases with acute rejection after kidney transplantation are low-grade forms; they
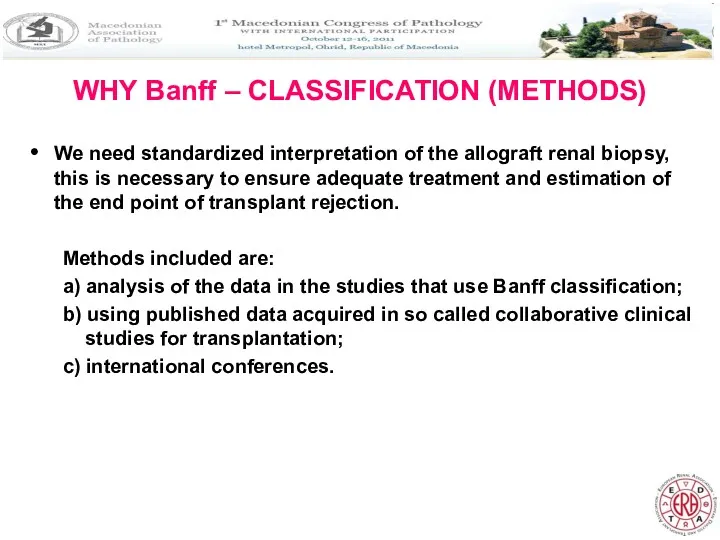
- 4. WHY Banff – CLASSIFICATION (METHODS) We need standardized interpretation of the allograft renal biopsy, this is
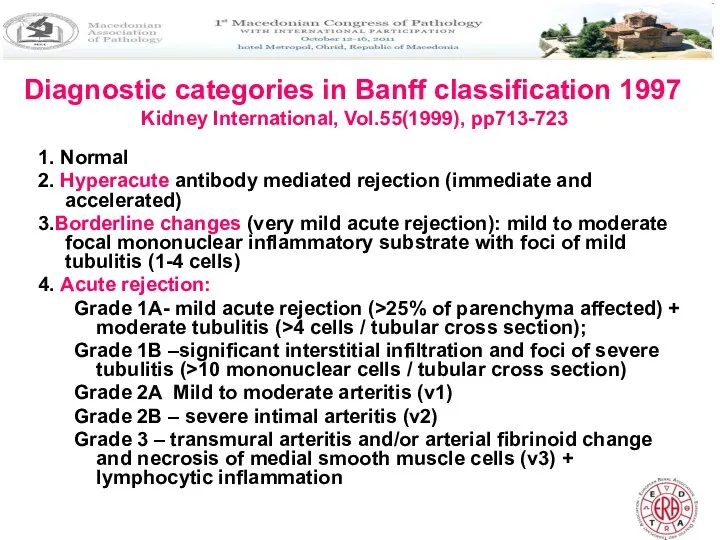
- 5. Diagnostic categories in Banff classification 1997 Kidney International, Vol.55(1999), pp713-723 1. Normal 2. Hyperacute antibody mediated
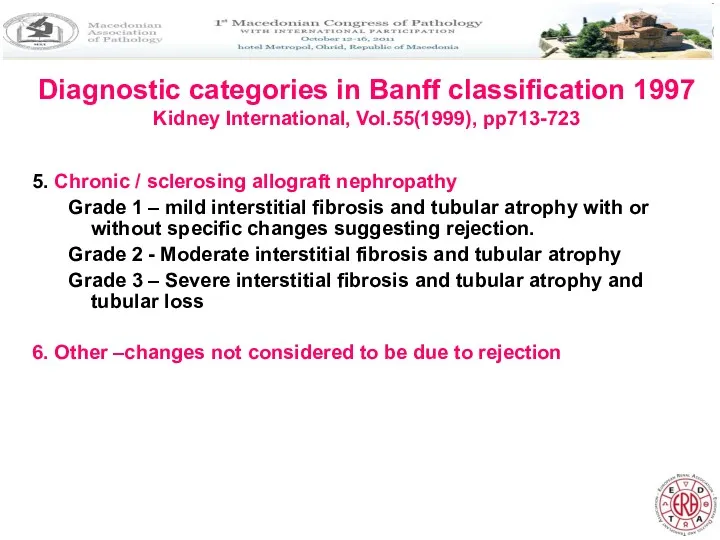
- 6. Diagnostic categories in Banff classification 1997 Kidney International, Vol.55(1999), pp713-723 5. Chronic / sclerosing allograft nephropathy
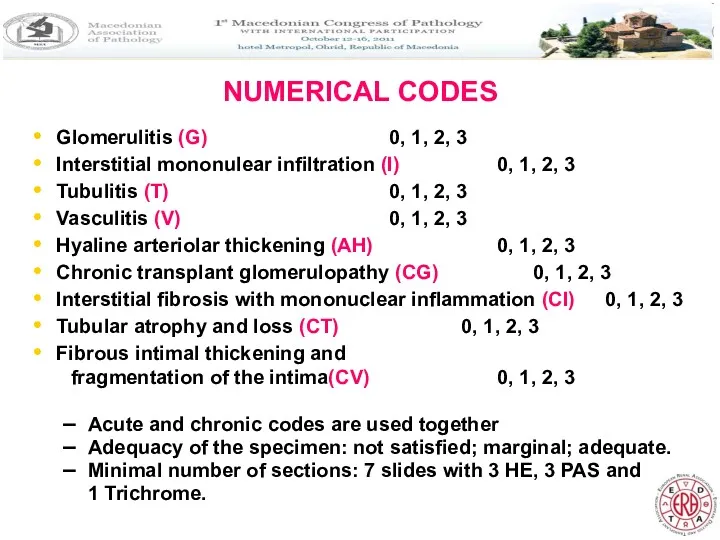
- 7. NUMERICAL CODES Glomerulitis (G) 0, 1, 2, 3 Interstitial mononulear infiltration (I) 0, 1, 2, 3
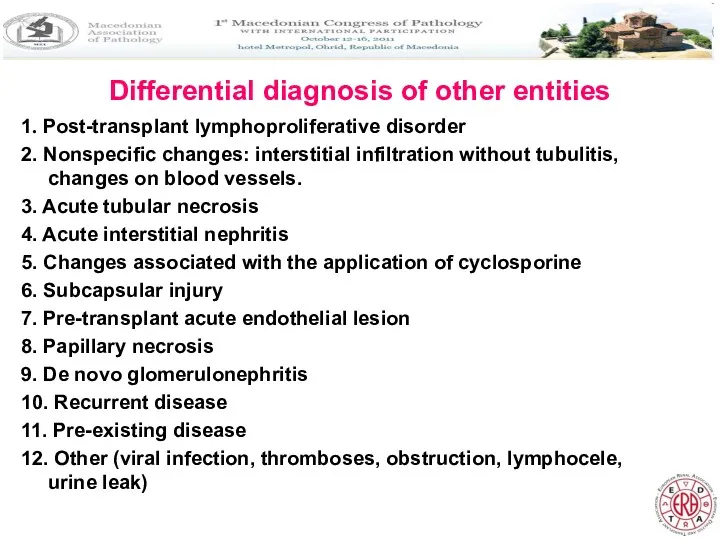
- 8. Differential diagnosis of other entities 1. Post-transplant lymphoproliferative disorder 2. Nonspecific changes: interstitial infiltration without tubulitis,
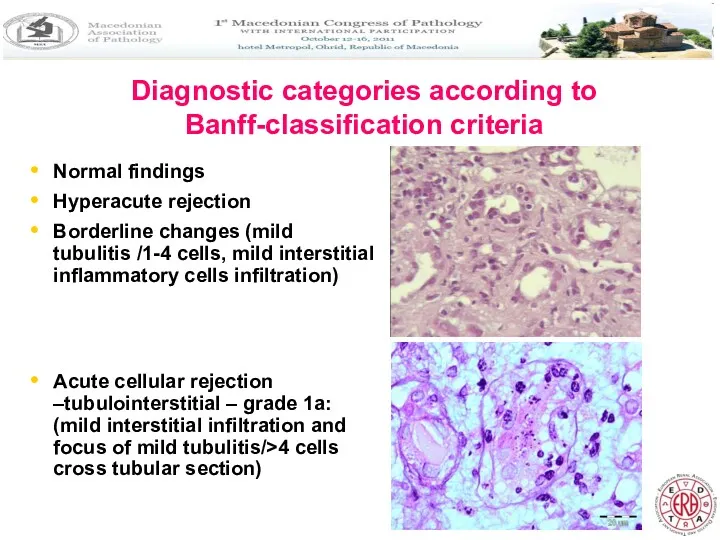
- 9. Diagnostic categories according to Banff-classification criteria Normal findings Hyperacute rejection Borderline changes (mild tubulitis /1-4 cells,
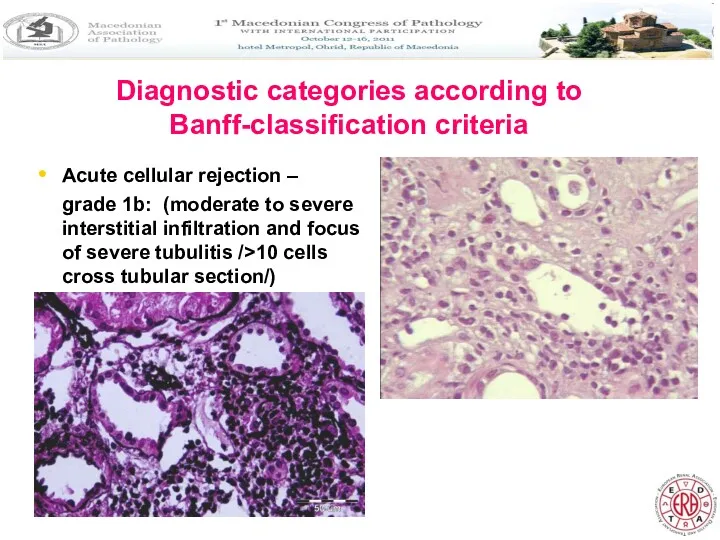
- 10. Diagnostic categories according to Banff-classification criteria Acute cellular rejection – grade 1b: (moderate to severe interstitial
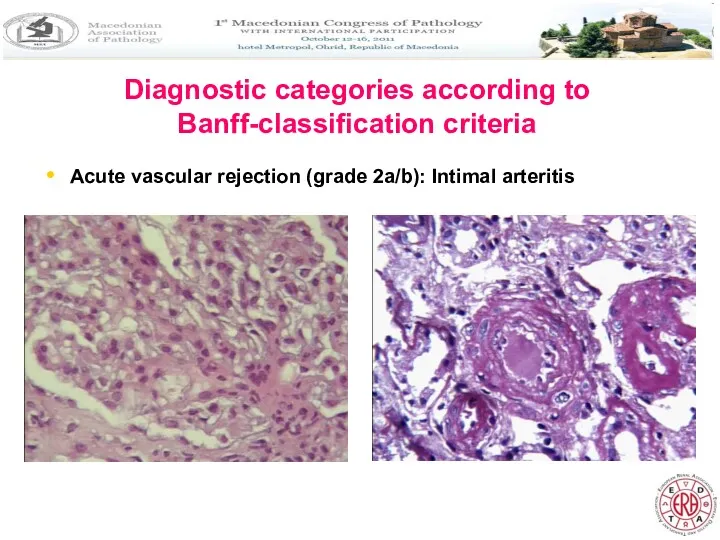
- 11. Diagnostic categories according to Banff-classification criteria Acute vascular rejection (grade 2a/b): Intimal arteritis
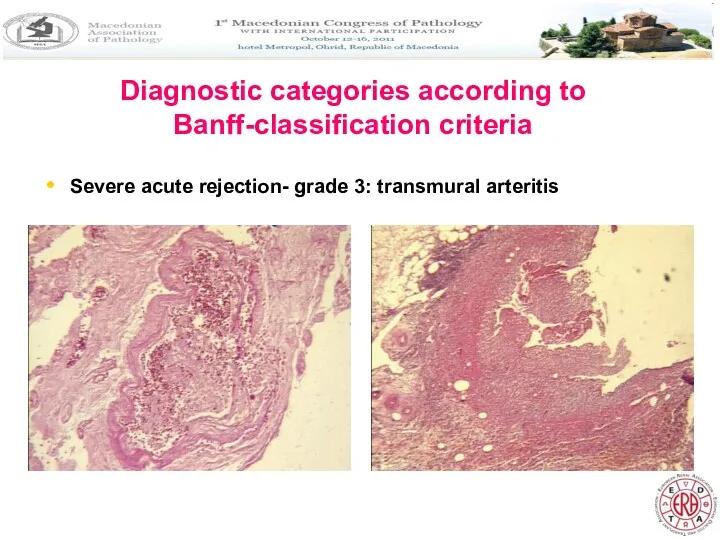
- 12. Diagnostic categories according to Banff-classification criteria Severe acute rejection- grade 3: transmural arteritis
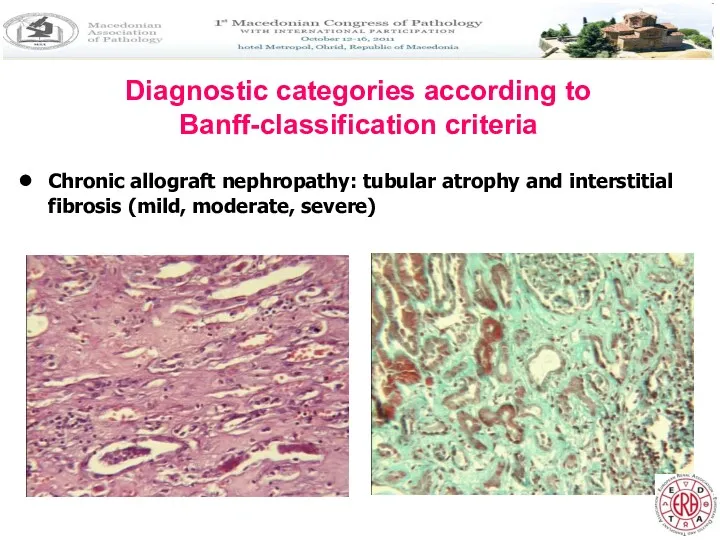
- 13. Diagnostic categories according to Banff-classification criteria Chronic allograft nephropathy: tubular atrophy and interstitial fibrosis (mild, moderate,
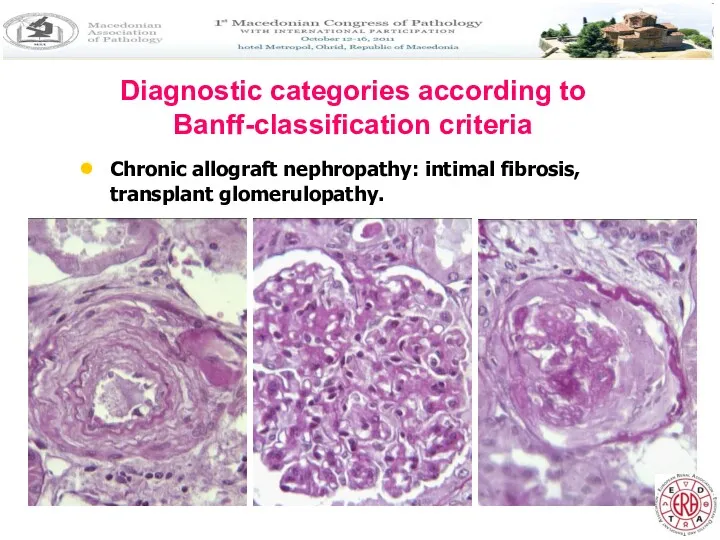
- 14. Diagnostic categories according to Banff-classification criteria Chronic allograft nephropathy: intimal fibrosis, transplant glomerulopathy.
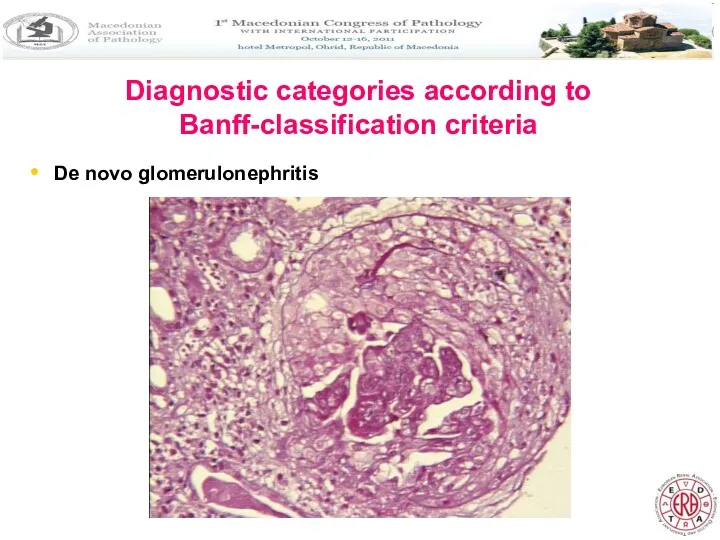
- 15. Diagnostic categories according to Banff-classification criteria De novo glomerulonephritis
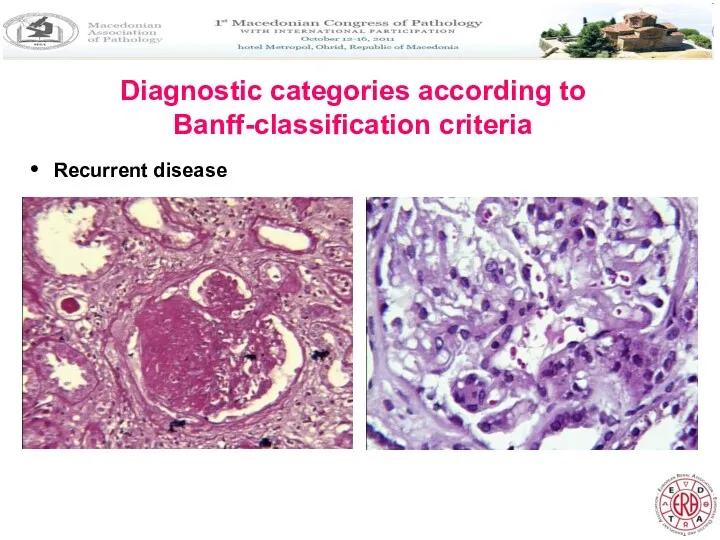
- 16. Diagnostic categories according to Banff-classification criteria Recurrent disease
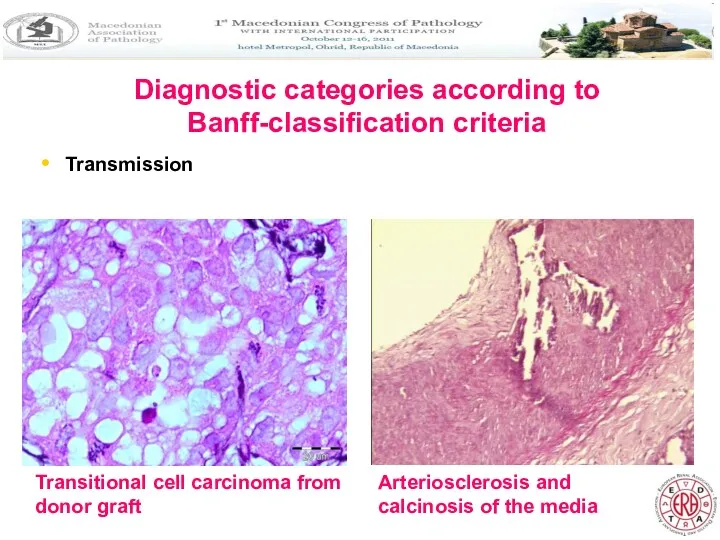
- 17. Diagnostic categories according to Banff-classification criteria Transmission Transitional cell carcinoma from donor graft Arteriosclerosis and calcinosis
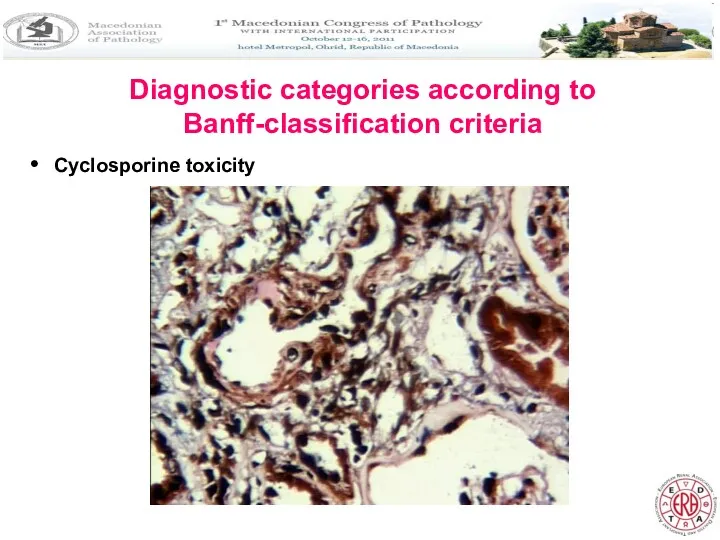
- 18. Diagnostic categories according to Banff-classification criteria Cyclosporine toxicity
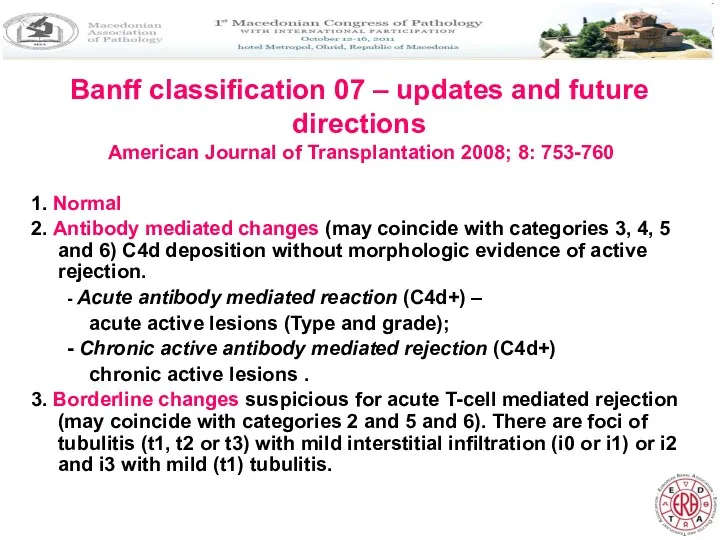
- 19. Banff classification 07 – updates and future directions American Journal of Transplantation 2008; 8: 753-760 1.
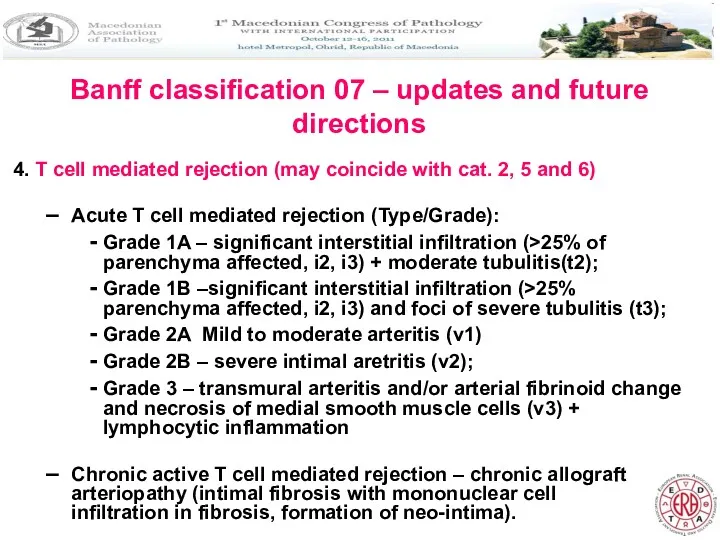
- 20. Banff classification 07 – updates and future directions 4. T cell mediated rejection (may coincide with
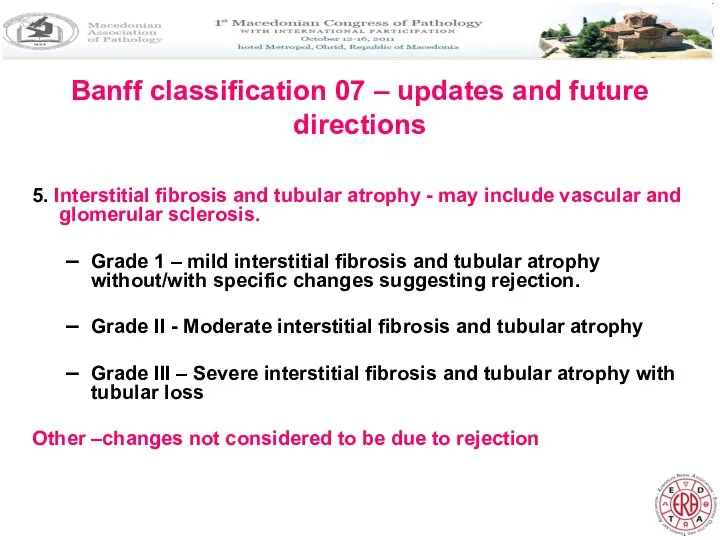
- 21. Banff classification 07 – updates and future directions 5. Interstitial fibrosis and tubular atrophy - may
- 22. Banff classification 07 – updates and future directions American Journal of Transplantation 2008; 8: 753-760 1.
- 23. INTRODUCTION In Macedonia, most cases usually underwent biopsy at the time of graft dysfunction. A study
- 24. MATERIALS AND METHODS A total of 28 paired biopsy specimens from allografted kidneys performed at 1
- 25. MATERIALS AND METHODS The immunosuppressive regimen consisted of methylprednisolone and Daclizumab as induction therapy, and cyclosporine,
- 26. RESULTS The mean age of the recipients was 35.2+/-8.3 years Male to female ratio was 3/1.
- 27. RESULTS Signs of acute rejection were found in 13/28 (46,4%) and 12/28 (42,8%) cases, at 1
- 28. RESULTS It is of interest that in three cases there were signs of cyclosporine nephrotoxicity, although
- 29. RESULTS Immunohistochemical study for cell proliferation by Ki 67 showed greater proliferative index in the second
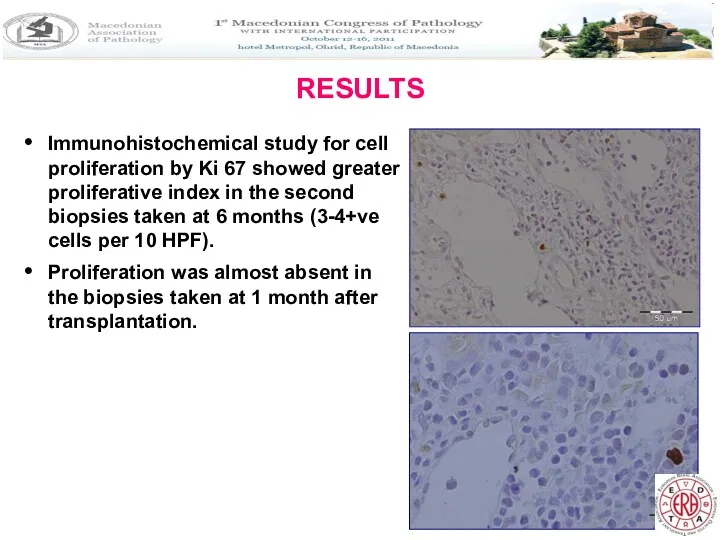
- 30. RESULTS Evaluation of the apoptosis showed significant number of cells that expressed apoptosis markers (>30 cells
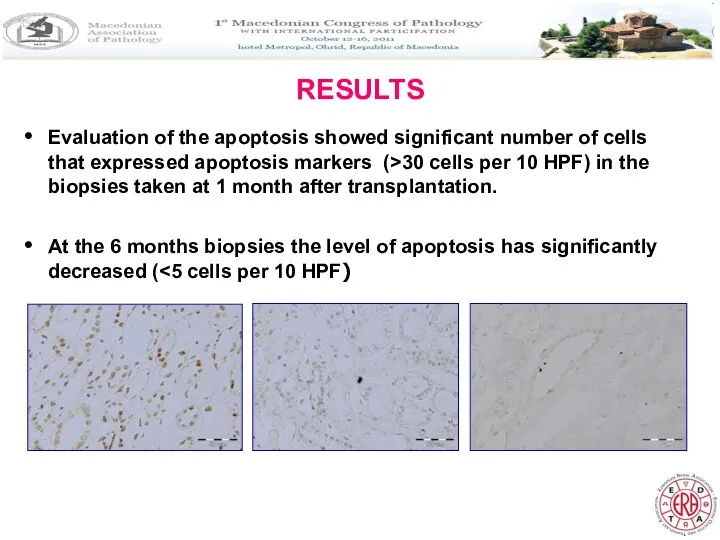
- 31. DISCUSSION We demonstrated histopathological findings in grafted kidneys, which clinically showed adquate renal function at the
- 32. DISCUSSION Study of protocol biopsies from stable grafts had revealed an unexpectedly strong correlation between the
- 33. DISCUSSION Findings of recurrent disease and cyclosporine nephrotoxicity are important because of the further treatment strategy
- 34. CONCLUSION AND RECOMMENDATIONS There are three possible stategies: 1. No biopsy: This is the default position
- 35. CONCLUSION AND RECOMMENDATIONS There are three possible strategies: 2. Biopsies in high-risk individuals: Although it is
- 36. CONCLUSION AND RECOMMENDATIONS There are three possible strategies: 3. Universal biopsy policy: Protocol biopsies are valuable
- 37. CONCLUSION AND RECOMMENDATIONS SCR results in chronic tubulointerstitial damage, impaired renal dysfunction and reduced graft survival.
- 39. Скачать презентацию
 Заболевания молочной железы. Воспалительные заболевания. Опухоли молочной железы
Заболевания молочной железы. Воспалительные заболевания. Опухоли молочной железы Менингит. Менингококкты инфекция
Менингит. Менингококкты инфекция Психосоматическая проблема
Психосоматическая проблема Сучасні тенденції діагностики та лікуваня раку передміхурової залози
Сучасні тенденції діагностики та лікуваня раку передміхурової залози Качество медпомощи в организациях ПМСП
Качество медпомощи в организациях ПМСП Поражения слизистой оболочки полости рта у детей, обусловленные аллергией
Поражения слизистой оболочки полости рта у детей, обусловленные аллергией Воспалительные заболевания женских половых органов
Воспалительные заболевания женских половых органов Терминальные состояния. Реанимация
Терминальные состояния. Реанимация Лапароскопия. Лапароскопическая диагностика
Лапароскопия. Лапароскопическая диагностика Причини порушення прохідності дихальних шляхів
Причини порушення прохідності дихальних шляхів Лучевая терапия
Лучевая терапия Открытый артериальный проток
Открытый артериальный проток Всемирный день иммунитета
Всемирный день иммунитета Кислотно-щелочное состояние
Кислотно-щелочное состояние Травма слезных органов
Травма слезных органов Биологическая (таргетная) терапия в ревматологии
Биологическая (таргетная) терапия в ревматологии The use of lasers in medicine
The use of lasers in medicine Характеристика фаз психогенных реакций при ЧС
Характеристика фаз психогенных реакций при ЧС Инородные тела верхних дыхательных путей у взрослых
Инородные тела верхних дыхательных путей у взрослых Сестринский процесс при дискинезии желчевыводящих путей. Сестринский процесс при хроническом холецистите
Сестринский процесс при дискинезии желчевыводящих путей. Сестринский процесс при хроническом холецистите Диспансерное наблюдение детей с ССЗ на педиатрическом участке
Диспансерное наблюдение детей с ССЗ на педиатрическом участке Современные методы визуальной диагностики в ревматологии. Показания и противопоказания
Современные методы визуальной диагностики в ревматологии. Показания и противопоказания Инфекционно-аллергическое заболевание туберкулез
Инфекционно-аллергическое заболевание туберкулез Противоаллергические средства
Противоаллергические средства Профилактика гриппа и других ОРВИ, менингококковой инфекции
Профилактика гриппа и других ОРВИ, менингококковой инфекции !! 378512
!! 378512 Бронх демікпесі
Бронх демікпесі Основи та стереотипи класичного менеджменту стосовно системи медичної допомоги населенню. Тема 1
Основи та стереотипи класичного менеджменту стосовно системи медичної допомоги населенню. Тема 1