Содержание
- 2. Objectives Mood, affect, mood disorders (mood D/O’s) Nosology, epidemiology, treatment (tx) of: Major depressive disorder (MDD)
- 3. Mood - The subjective sense indicates the long, deep and constant feeling that affects a person,
- 4. Mood - The subjective sense indicates the long, deep and constant feeling that affects a person,
- 5. Mood v. Affect “mood” a sustained emotional attitude typically garnered through pt self-report “affect” the way
- 6. Major Depressive Disorder
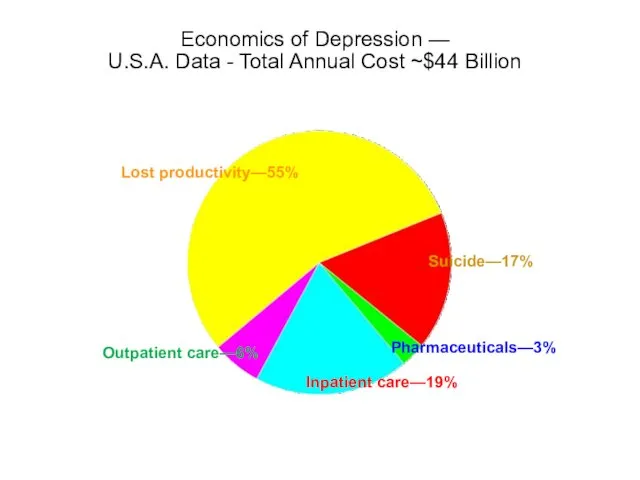
- 7. Economics of Depression — U.S.A. Data - Total Annual Cost ~$44 Billion 9 Lost productivity—55% Suicide—17%
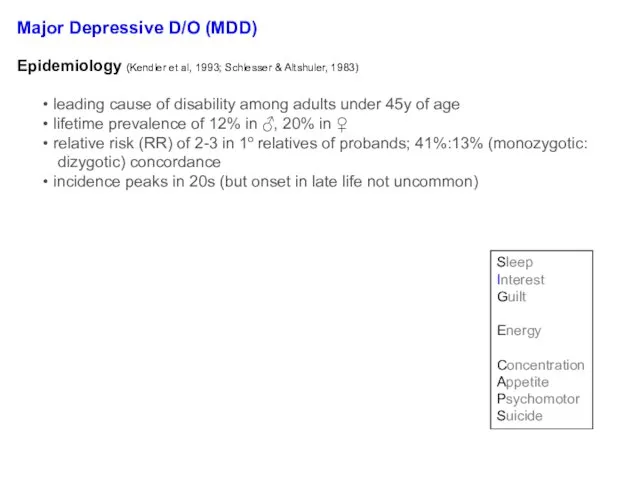
- 8. Major Depressive D/O (MDD) Diagnosis req’s ≥1 major depressive episode (MDE) MDE = ≥2wks of signif
- 9. Question: When does a major depressive episode (MDE) ≠ Major Depressive Disorder?
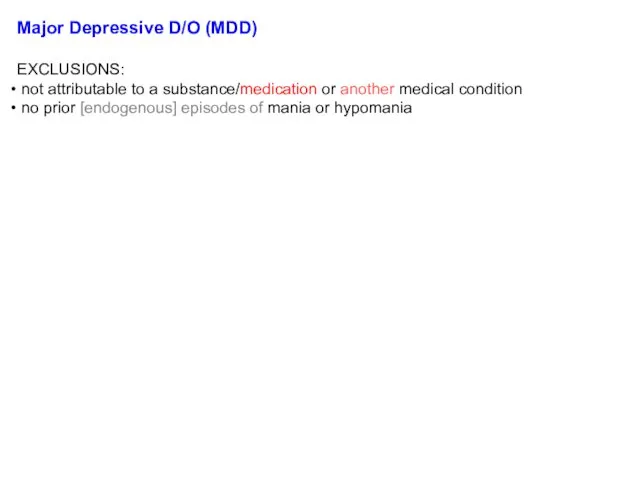
- 10. Major Depressive D/O (MDD) EXCLUSIONS: not attributable to a substance/medication or another medical condition no prior
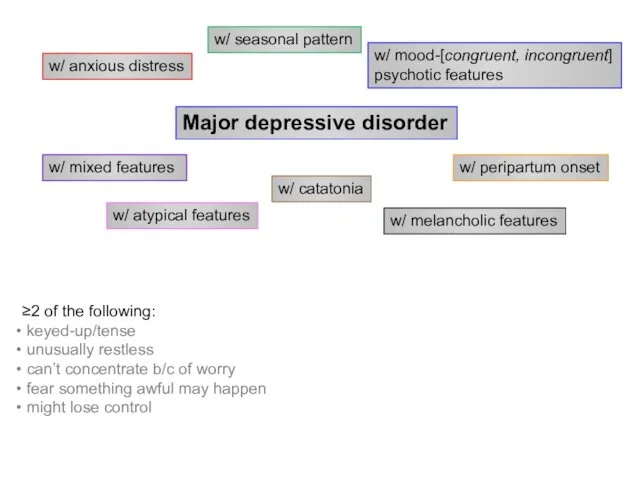
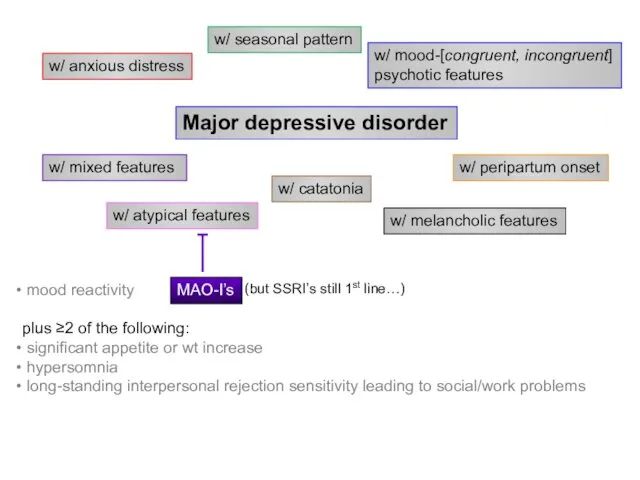
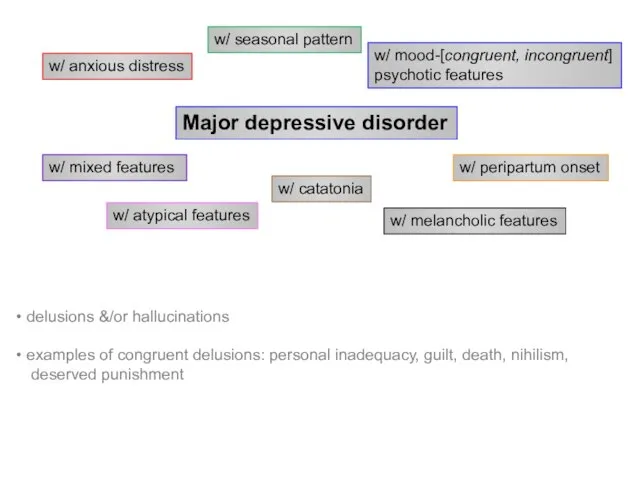
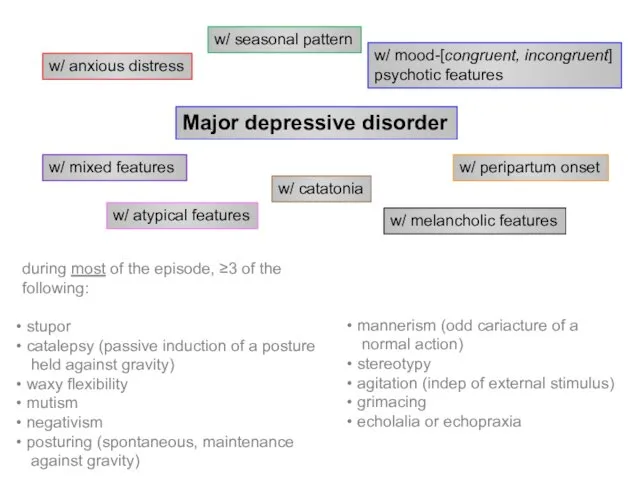
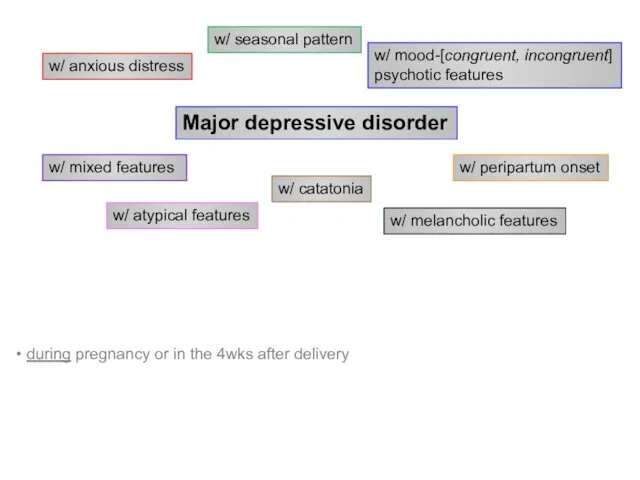
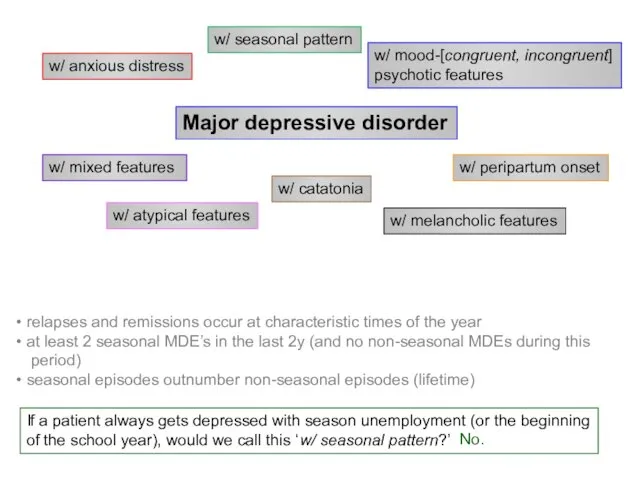
- 11. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
- 12. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
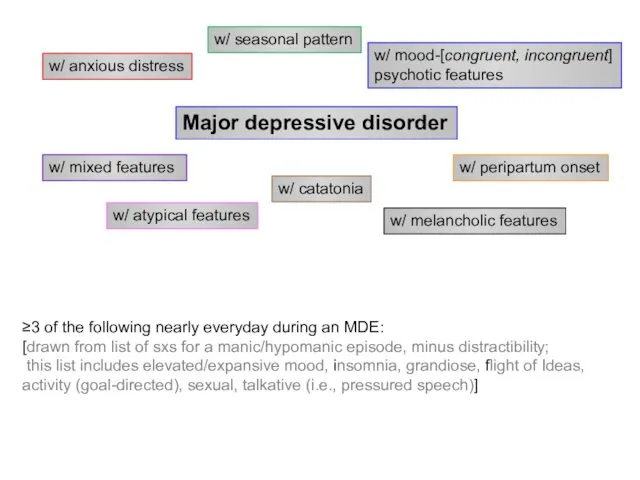
- 13. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
- 14. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
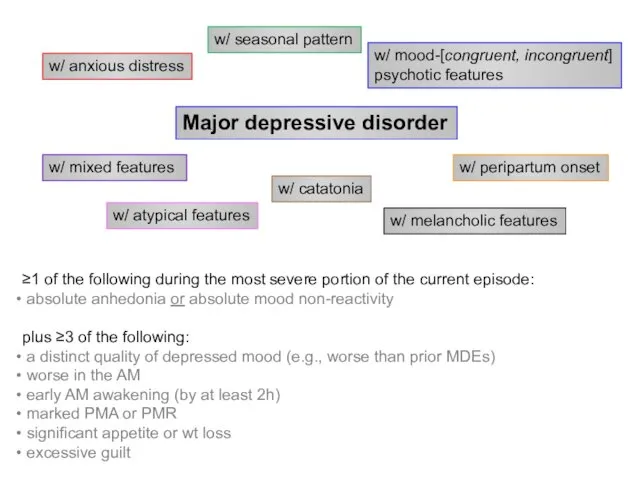
- 15. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
- 16. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
- 17. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
- 18. Major depressive disorder w/ anxious distress w/ mixed features w/ atypical features w/ melancholic features w/
- 19. Belmaker RH and Agam G, NEJM 2008, 358:55-68 iproniazid (1957) imipramine (1959)
- 20. Question: Do antidepressants have additional actions besides inhibition of reuptake transporters? “…the Zoloft cartoon” from: http://gifsoup.com/webroot/animatedgifs/50426_o.gif;
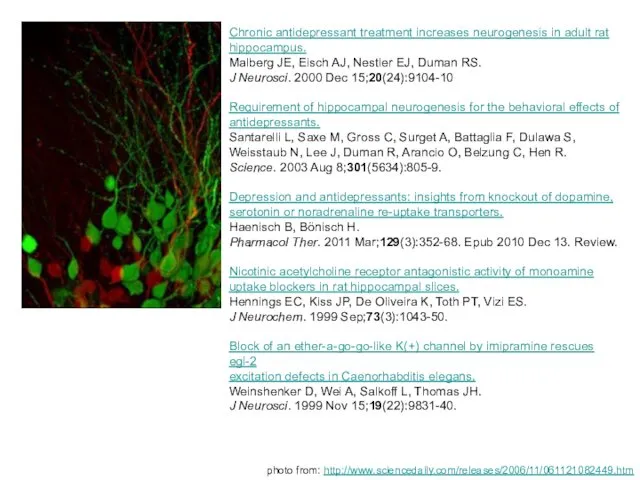
- 21. Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus. Malberg JE, Eisch AJ, Nestler EJ, Duman
- 22. Subsequent hypotheses about MDD altered glutamatergic transmission ↓’d GABAergic transmission monoamine-Ach imbalance disruption of endogenous opioid
- 23. Key brain areas involved in regulation of mood (A) Ventromedial prefrontal cortex (VMPFC)1 Modulates pain and
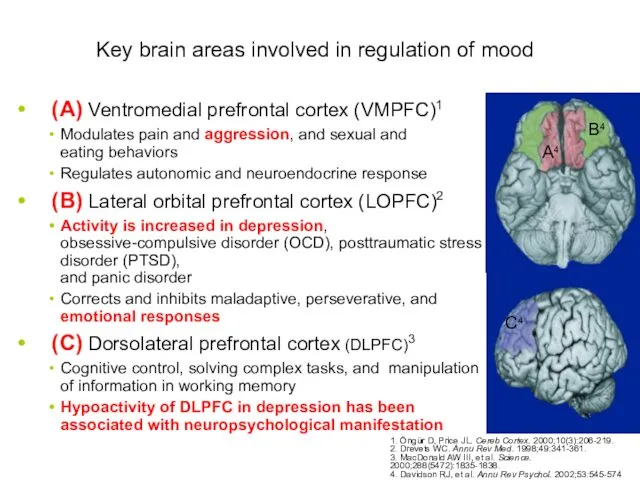
- 24. Key brain areas involved in regulation of mood (cont.) (A) Amygdala: regulates cortical arousal and neuroendocrine
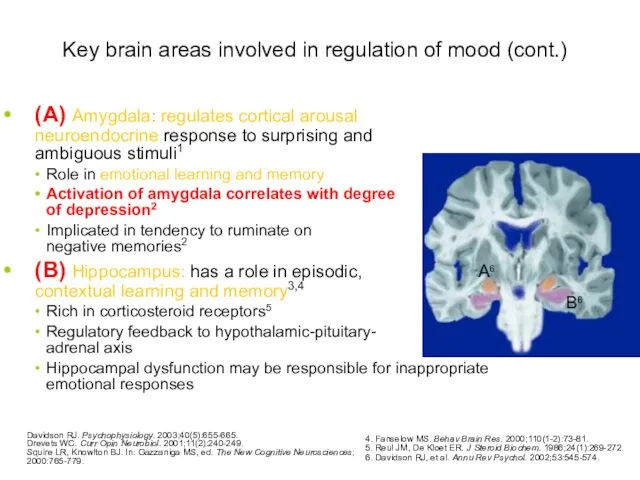
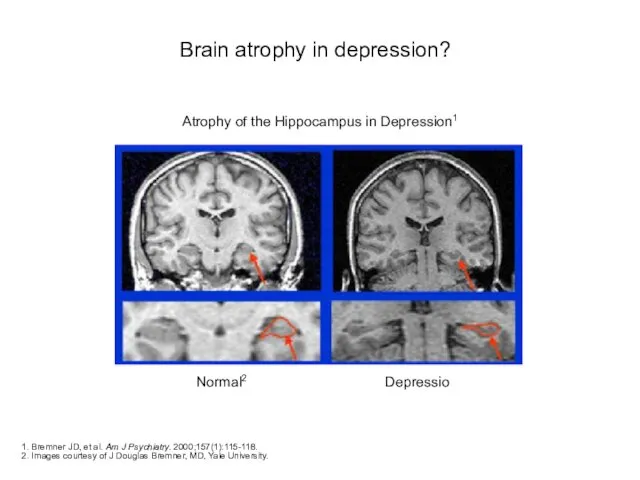
- 25. Brain atrophy in depression? 1. Bremner JD, et al. Am J Psychiatry. 2000;157(1):115-118. 2. Images courtesy
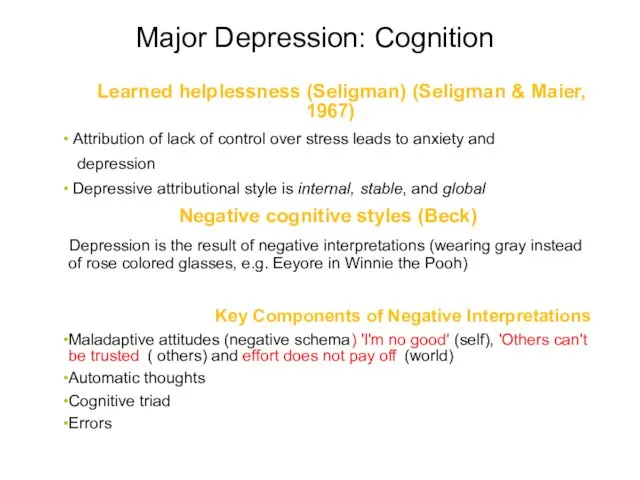
- 26. Major Depression: Cognition Learned helplessness (Seligman) (Seligman & Maier, 1967) Attribution of lack of control over
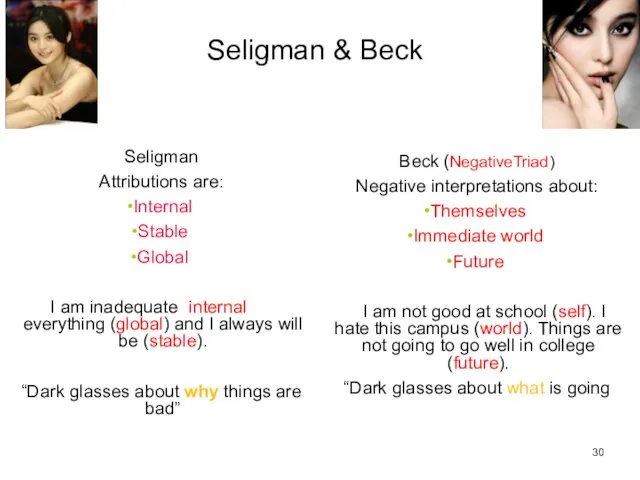
- 27. Seligman & Beck Seligman Attributions are: Internal Stable Global I am inadequate (internal) at everything (global)
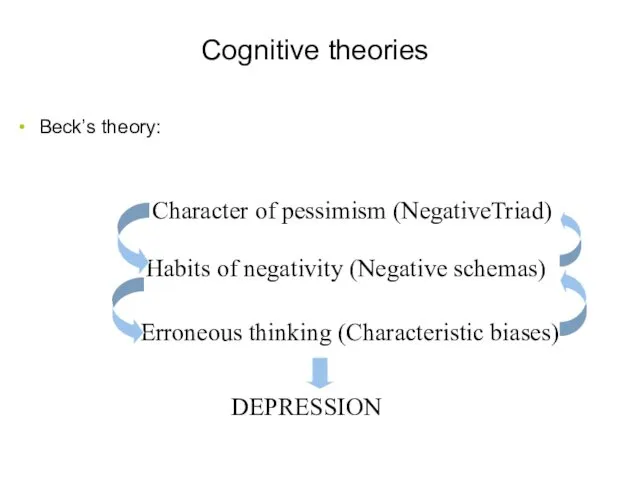
- 28. Cognitive theories Beck’s theory: 31 Character of pessimism (NegativeTriad) Habits of negativity (Negative schemas) Erroneous thinking
- 29. Characteristic biases Arbitrary inference Selective abstraction Overgeneralization Magnification and minimization 32
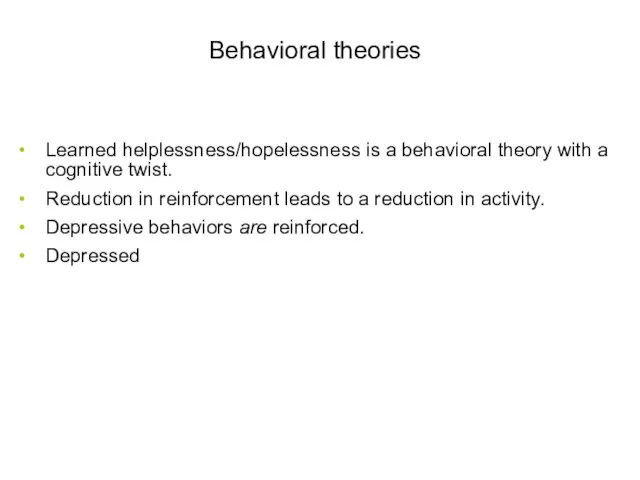
- 30. Behavioral theories Learned helplessness/hopelessness is a behavioral theory with a cognitive twist. Reduction in reinforcement leads
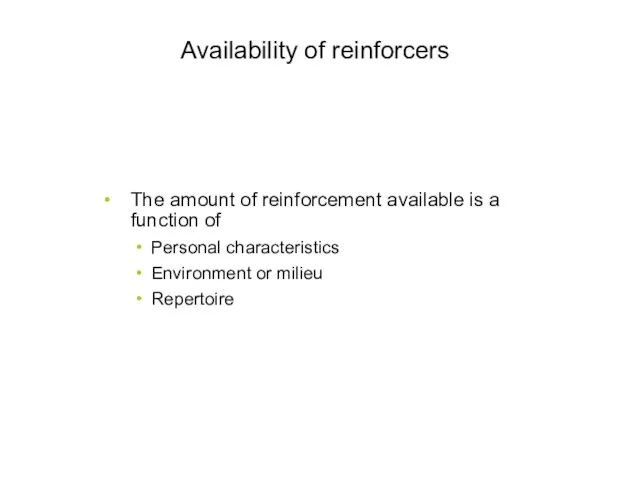
- 31. Availability of reinforcers The amount of reinforcement available is a function of Personal characteristics Environment or
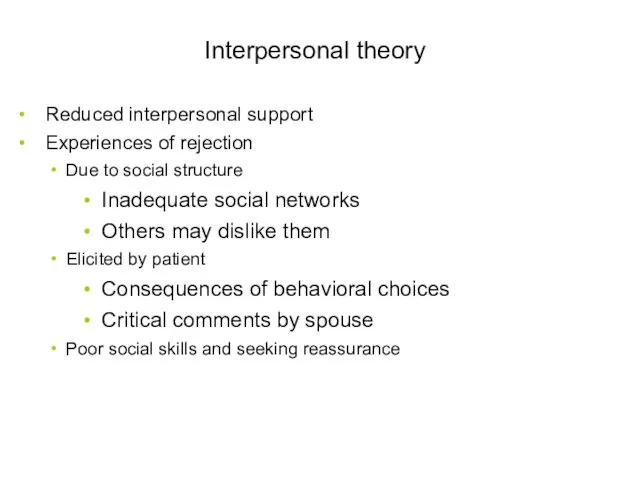
- 32. Interpersonal theory Reduced interpersonal support Experiences of rejection Due to social structure Inadequate social networks Others
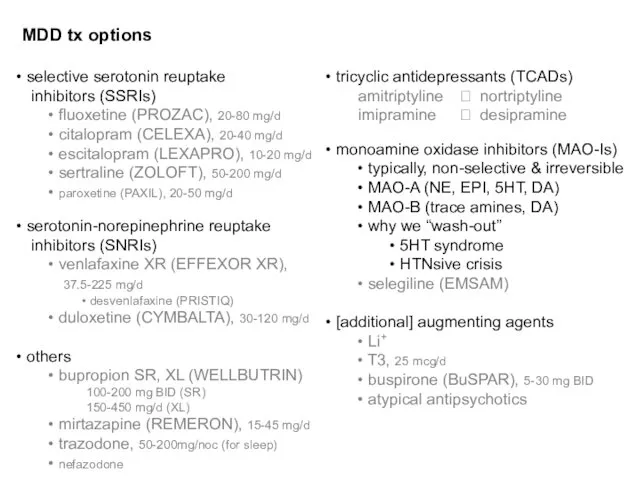
- 33. MDD tx options selective serotonin reuptake inhibitors (SSRIs) fluoxetine (PROZAC), 20-80 mg/d citalopram (CELEXA), 20-40 mg/d
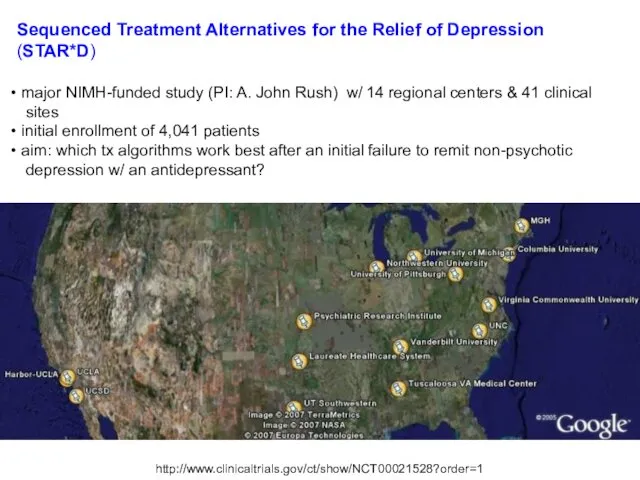
- 34. Sequenced Treatment Alternatives for the Relief of Depression (STAR*D) major NIMH-funded study (PI: A. John Rush)
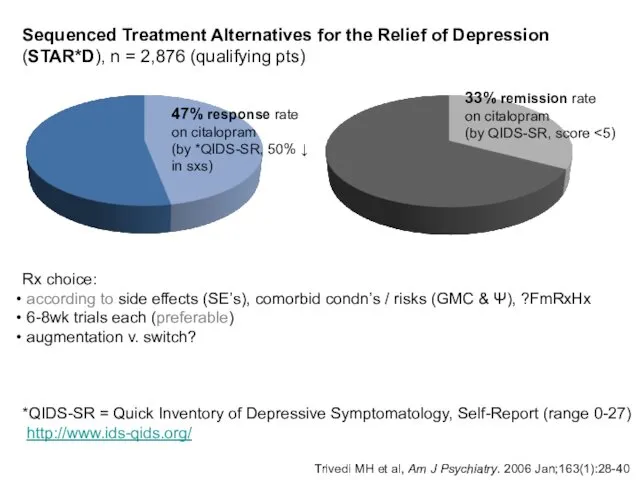
- 35. Trivedi MH et al, Am J Psychiatry. 2006 Jan;163(1):28-40 47% response rate on citalopram (by *QIDS-SR,
- 36. MDD tx options Ψtherapy cognitive bx therapy (CBT) interpersonal therapy (IPT) psychodynamic therapy interventional Ψ electroconvulsive
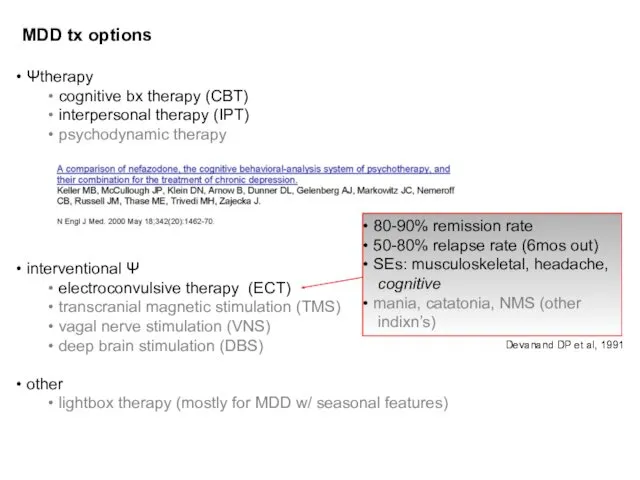
- 37. Major Depressive D/O (MDD) NATURAL HISTORY (Frank E and Thase ME, 1999 & DSM-5) recovery usually
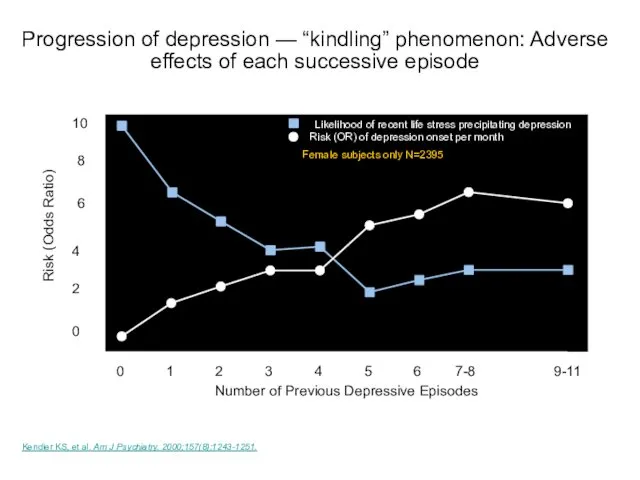
- 38. Kendler KS, et al. Am J Psychiatry. 2000;157(8):1243-1251. Number of Previous Depressive Episodes 10 Risk (Odds
- 39. Persistent depressive disorder (dysthymia) 2y of depressed mood (1y in children/adolescents) most of the day, more
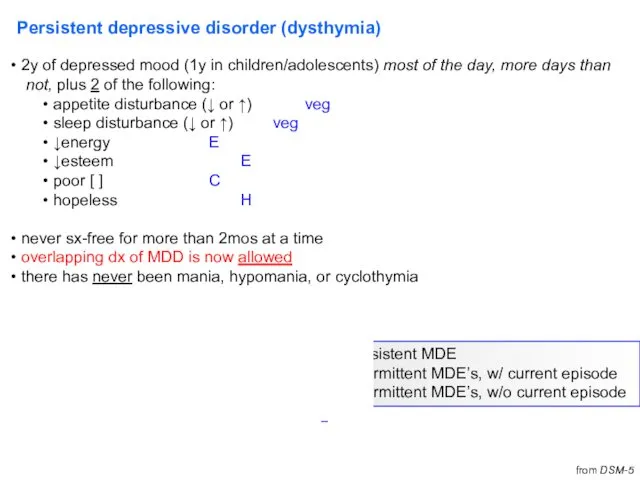
- 40. Persistent depressive disorder (dysthymia) may be more treatment-resistant (TxR) than straightforward MDD EPIDEMIOLOGY lifetime prevalence =
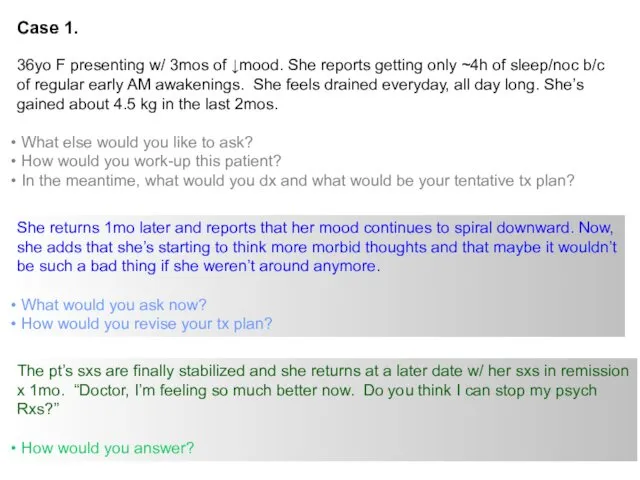
- 41. Case 1. 36yo F presenting w/ 3mos of ↓mood. She reports getting only ~4h of sleep/noc
- 42. Premenstrual dysphoric d/o Criterion A. In most menstrual cycles, ≥5 sxs in the final week before
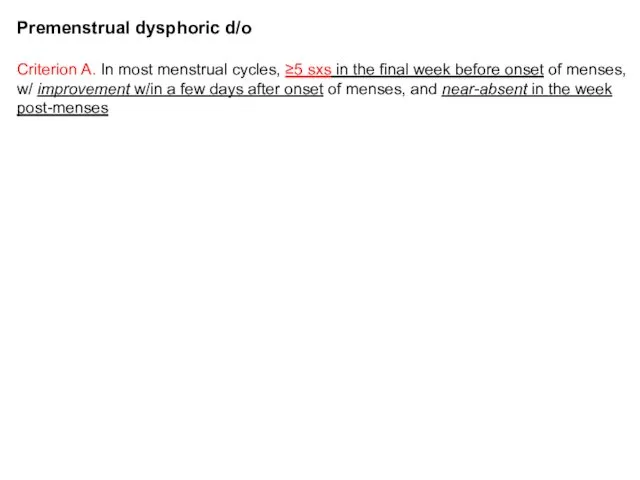
- 43. Premenstrual dysphoric d/o (M)ood (labile &/or irritable &/or anxious) Sleep Interest Body Energy Concentration Appetite Out
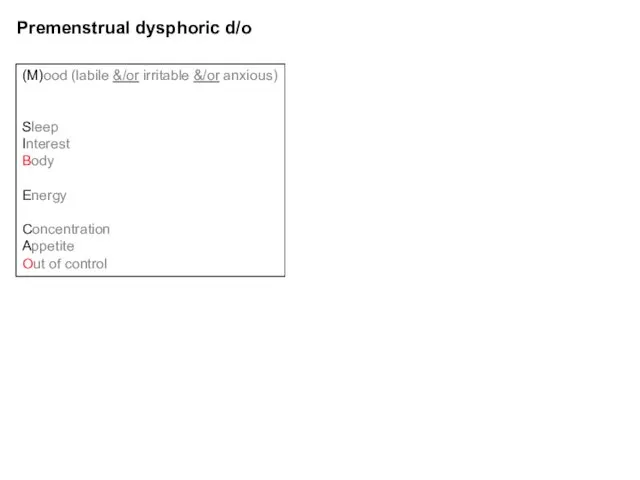
- 44. Disruptive mood dysregulation disorder *severe recurrent temper outbursts (verbal or behavior) grossly disproportionate to the situation
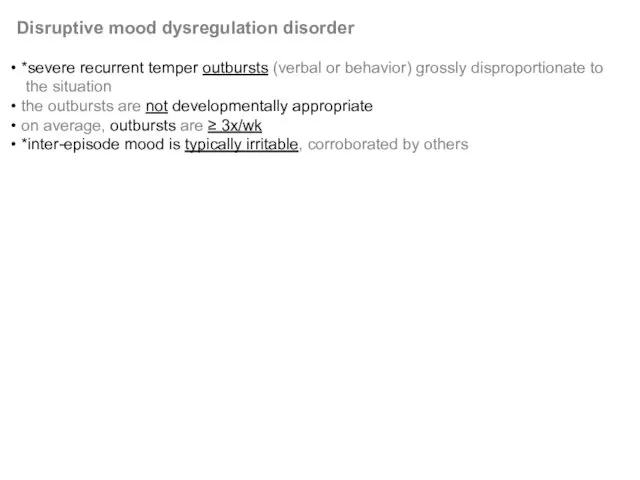
- 45. Bipolar disorder
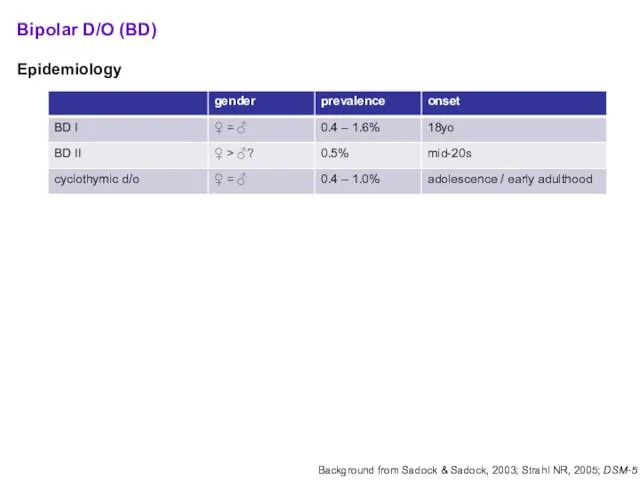
- 46. Bipolar D/O (BD) Epidemiology Diagnostic criteria: BD I ≥ 1 manic episode MDE is neither sufficient
- 47. Bipolar D/O (BD) Manic episode: elevated mood & ≥1wk of at least 3 of the following
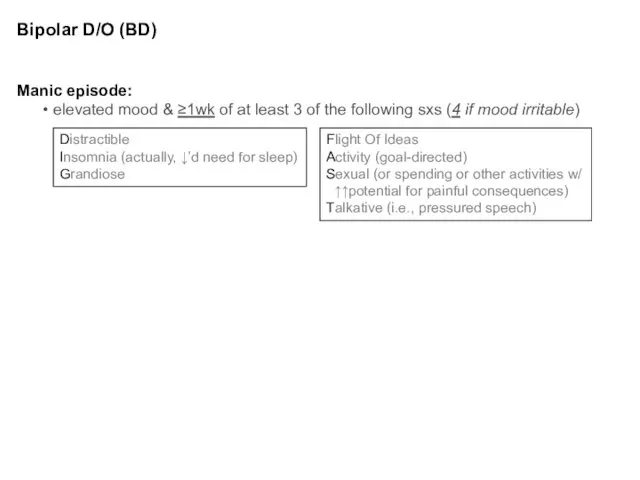
- 48. Bipolar Disorder (BD) EXCLUSIONS: another medical cause substance/medication causes SPECIFIERS: same as w/ MDD plus: rapid
- 49. Bipolar Disorder (BD) MORE on ‘w/ mixed features’… IF full criteria met for both poles, the
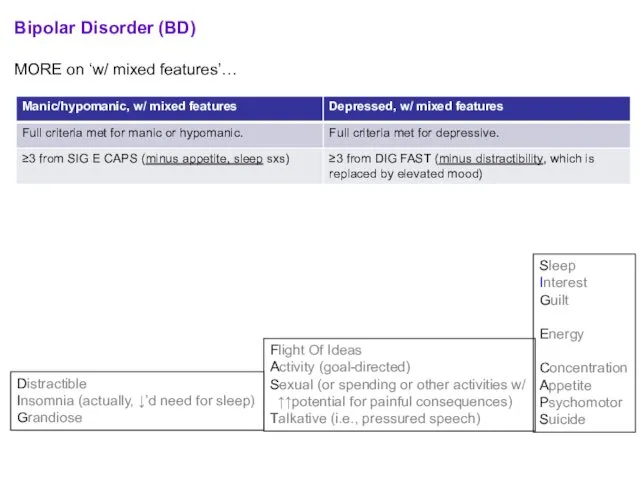
- 50. Case 1 - continued Prior hx to date: 36yo F w/ 3mos of depressed mood tx’d
- 51. Case 1 - continued Is manic switch a real concern? mood stabilizer = primarily Li+, VPA,
- 52. Biology of Bipolar D/O (BD) failure of linkage studies Janice Egeland – 2 decades of work
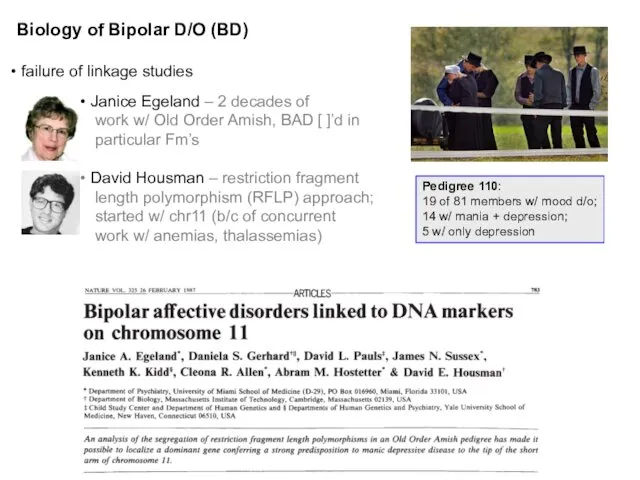
- 53. *’s 2 accompanying papers (same issue of Nature) unable to replicate chr11 assocn’s in independent pedigrees
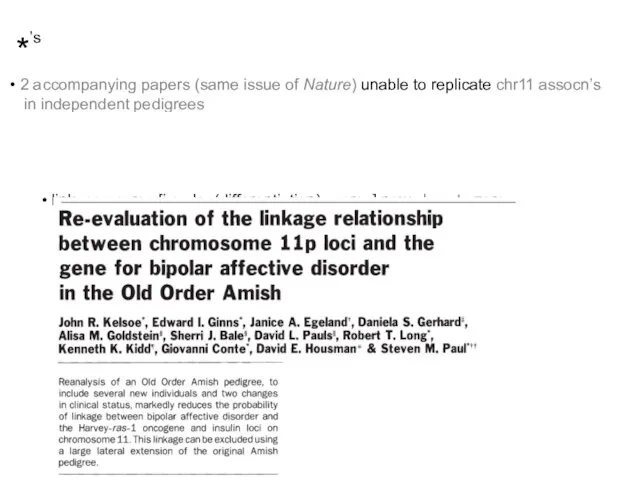
- 54. Linkage studies 6q (LOD 4.19 narrow), 8q (LOD 3.40 broad) (still hold-up in meta-analyses – e.g.,
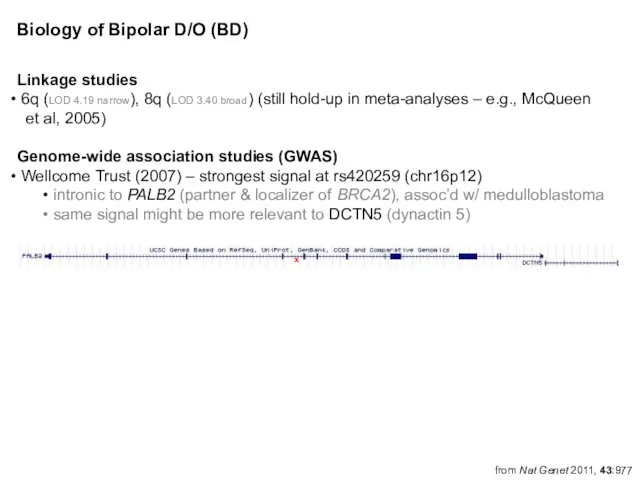
- 55. More on select GWA-identified candidates CACNA1C α1 subunit of a voltage-dependent Ca2+ channel per citations in
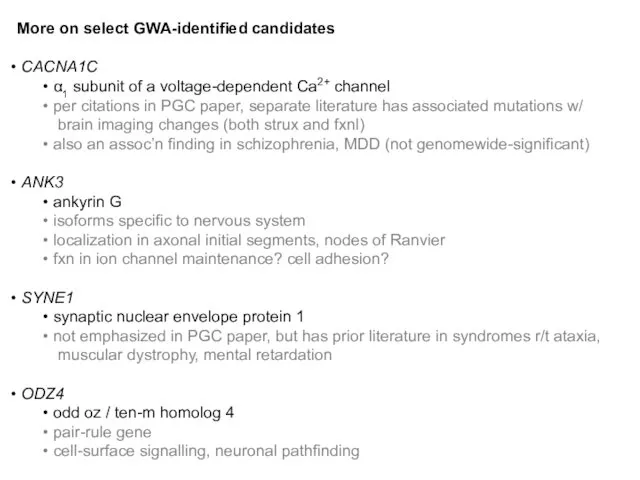
- 56. Bipolar Disorder (BD) – treatment The old standard: mood stabilizer + reuptake blocker Debunked: gabapentin (NEURONTIN)
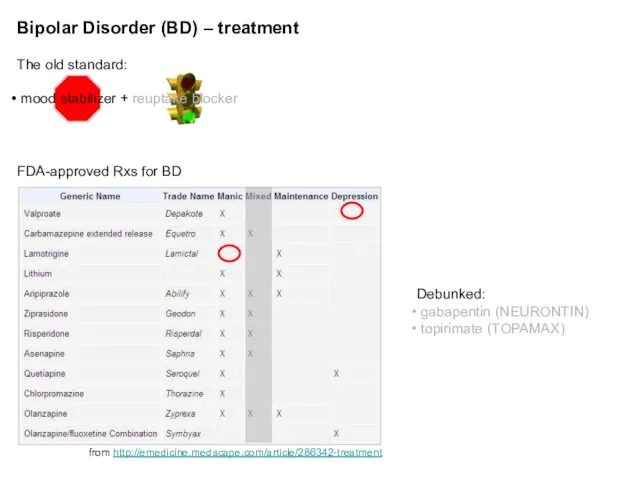
- 57. John Cade. Ψist at a provincial hospital in Australia figured mania was 2/2 an abnormally secreted
- 58. Bipolar Disorder (BD) – treatment (cont’d) Li+ v. Depakote / valproate (VPA) (Bowden CL, 2001) Li+
- 59. Bipolar Disorder (BD) – treatment (cont’d) How many agents to use? combination tx often helpful in
- 60. Bipolar Disorder (BD) – natural history 60% of manic episodes immediately precede an MDE MDE’s usually
- 61. Cyclothymic D/O 2y of fluctuating mood (1y in children, adolescents) hypomanic symptoms (but NOT episodes) dysthymic
- 62. Differential diagnosis
- 63. Phenocopies and gray areas… Anxiety D/O’s (esp. GAD, PTSD) Schizoaffective D/O Delirium Dementia Personality D/O’s Substance/Medication-induced
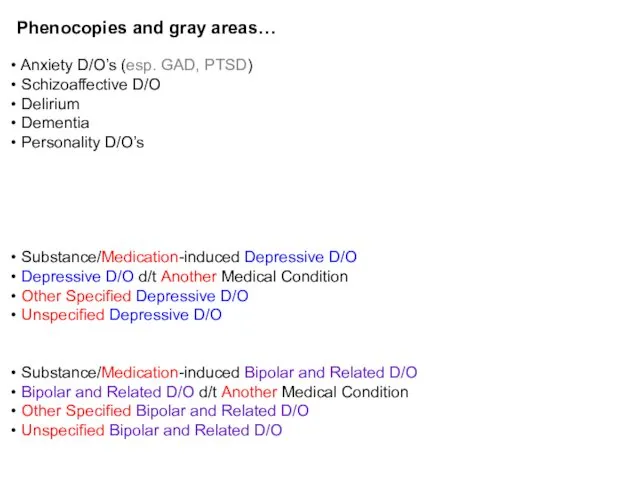
- 64. Depressive, Bipolar & Related D/O d/t a Another Medical Condition Endocrine (e.g., thyroid, hypothalamic-pituitary-adrenal/HPA) Neurologic (e.g.,
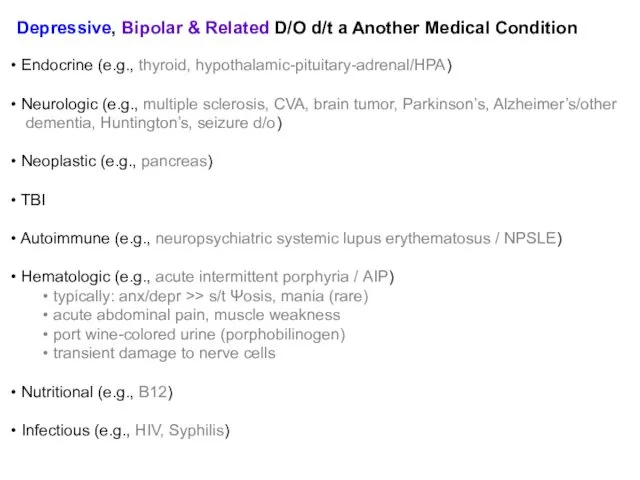
- 65. Substance/Medication-induced Depressive, Bipolar & Related D/O ILLICITS can be from intoxication or withdrawal phases EtOH –
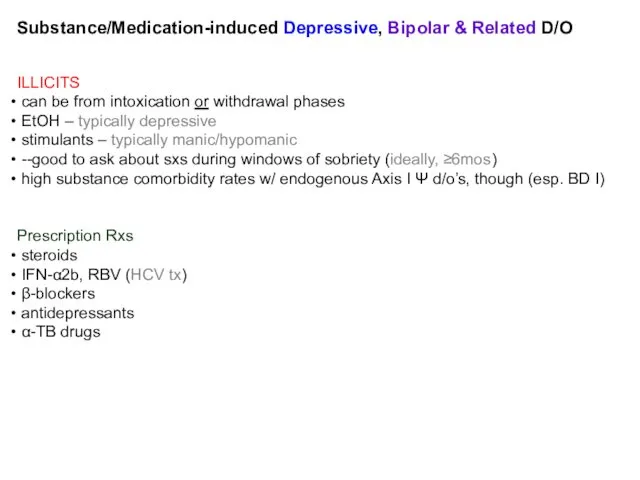
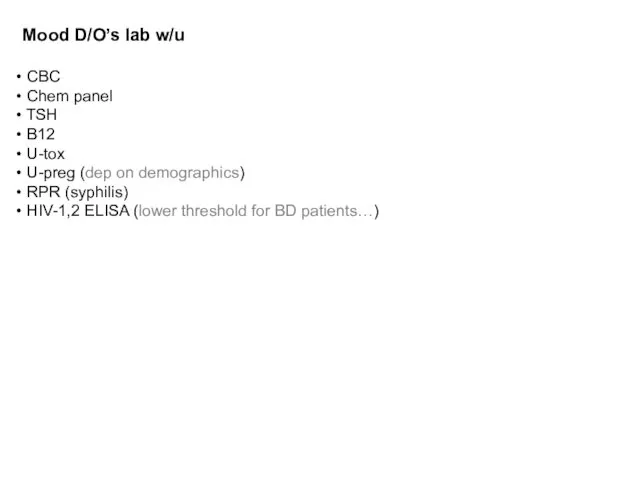
- 66. Mood D/O’s lab w/u CBC Chem panel TSH B12 U-tox U-preg (dep on demographics) RPR (syphilis)
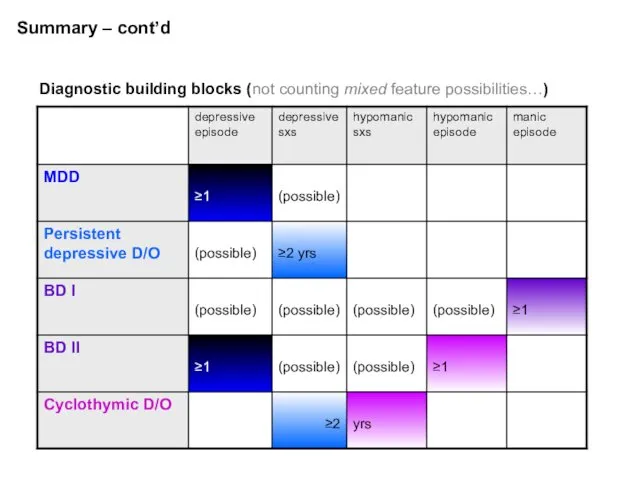
- 67. Summary – cont’d Diagnostic building blocks (not counting mixed feature possibilities…)
- 68. 5 Myths and Facts About Suicide Myth #1: People who talk about killing themselves rarely commit
- 69. 5 Myths and Facts About Suicide Myth #2: The suicidal person wants to die and feels
- 70. 5 Myths and Facts About Suicide Myth # 3: If you ask someone about their suicidal
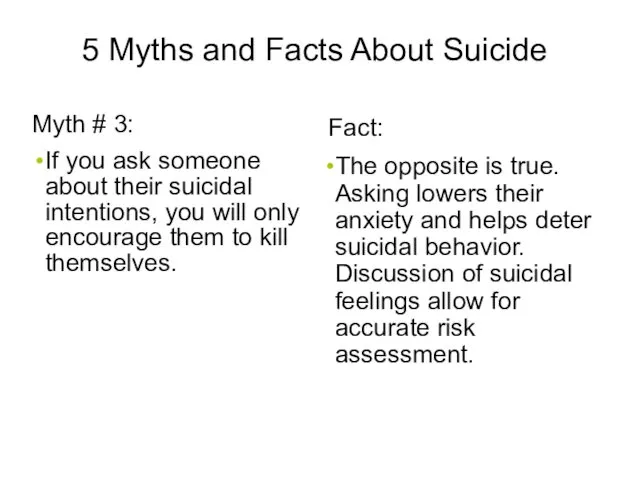
- 71. 5 Myths and Facts About Suicide Myth # 4: All suicidal people are deeply depressed. 43
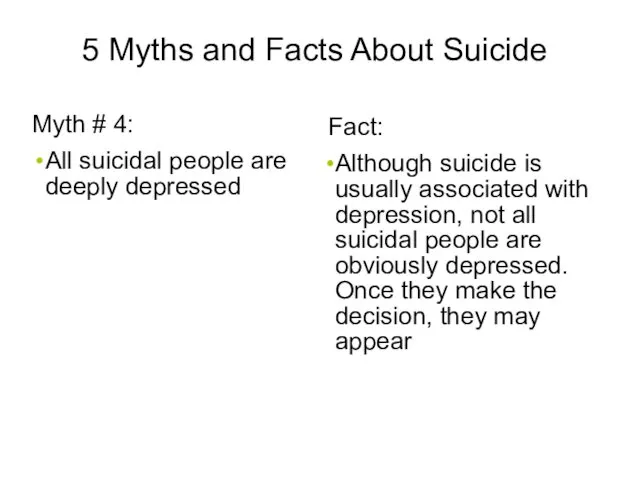
- 72. 5 Myths and Facts About Suicide Myths # 5: Suicidal people rarely seek medical attention. 44
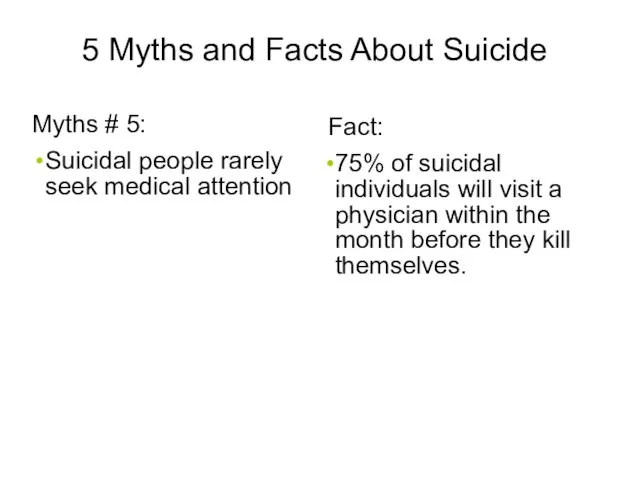
- 73. Socio-demographic Risk Factors Male > 60 years Widowed or Divorced White or Native American Living alone
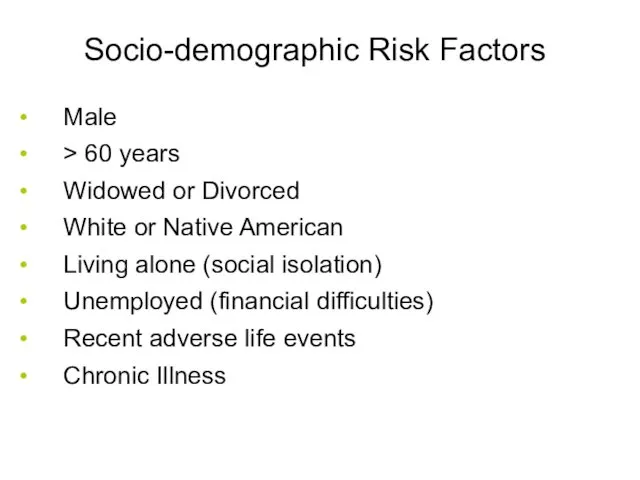
- 74. Clinical Risk Factors Previous Attempts Clinical depression or schizophrenia Substance Abuse Feelings of hopelessness Severe anxiety,
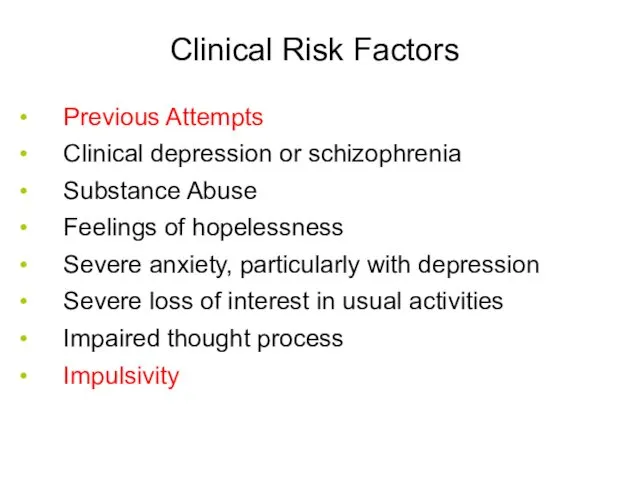
- 75. Suicide:Treatment Problem-solving Cognitive behavioral therapy Coping skills Stress reduction 47
- 76. Additional case presentations
- 77. Case 2. 18yo M high school student who was BIB his parents to the ER after
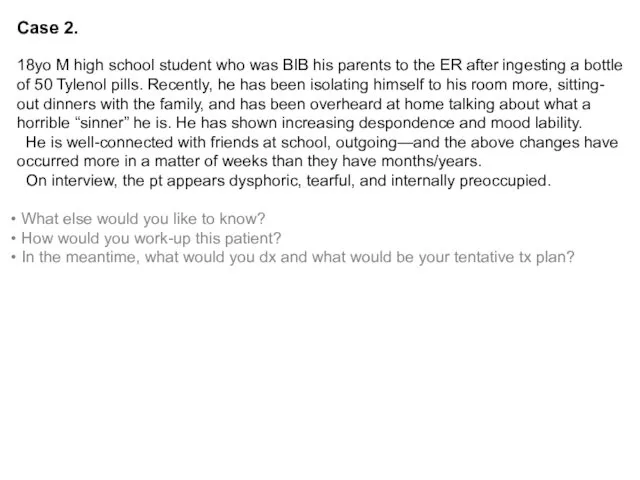
- 78. Case 3. 50yo F, under-employed and barely hanging-on with temp agency work, comes in for her
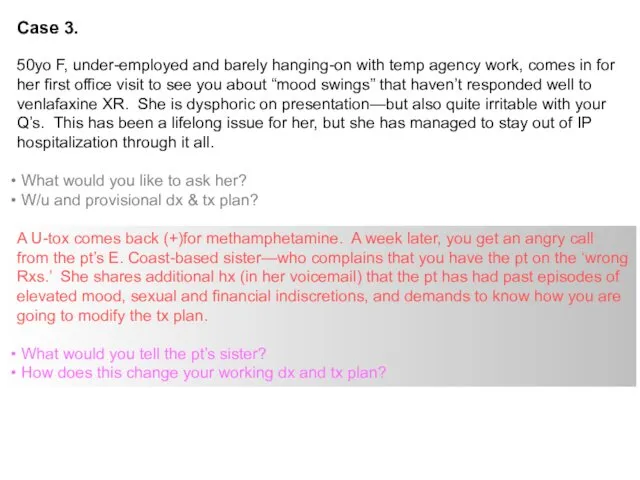
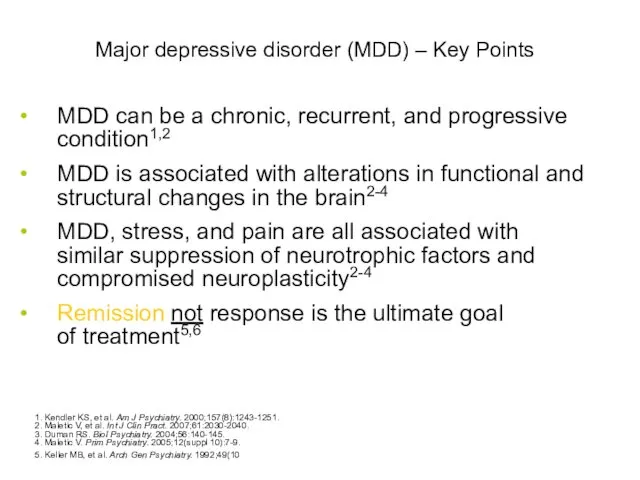
- 80. Major depressive disorder (MDD) – Key Points MDD can be a chronic, recurrent, and progressive condition1,2
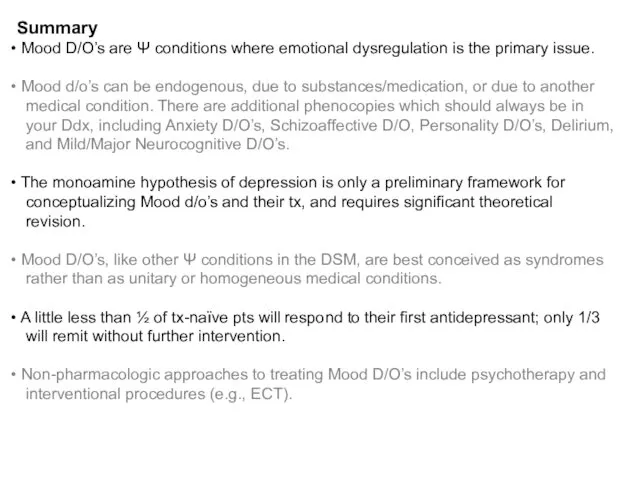
- 81. Summary Mood D/O’s are Ψ conditions where emotional dysregulation is the primary issue. Mood d/o’s can
- 83. Скачать презентацию
 Эмоциональная сфера дошкольников в подготовительной группе
Эмоциональная сфера дошкольников в подготовительной группе Struktura zachowań rekreacyjnych od koncepcji systemu do struktury rekreacji. (Wykład 2)
Struktura zachowań rekreacyjnych od koncepcji systemu do struktury rekreacji. (Wykład 2) Особенности личностного своеобразия детей с нарушением речи и коммуникации
Особенности личностного своеобразия детей с нарушением речи и коммуникации Как быть англичанином
Как быть англичанином Критерии готовности к школе
Критерии готовности к школе Иллюзии
Иллюзии Theories of personality
Theories of personality Психолого-педагогическое сопровождение участников образовательной деятельности на этапе подготовки к итоговой аттестации
Психолого-педагогическое сопровождение участников образовательной деятельности на этапе подготовки к итоговой аттестации Навички для психологічного відновлення
Навички для психологічного відновлення Как преодолеть стресс
Как преодолеть стресс Дизайн-мышление педагога дополнительного образования
Дизайн-мышление педагога дополнительного образования Этические особенности работы психолога с детьми и подростками
Этические особенности работы психолога с детьми и подростками Что такое – обида?
Что такое – обида? Мотивация. Общая характеристика учебной мотивации
Мотивация. Общая характеристика учебной мотивации Қиял дегеніміз
Қиял дегеніміз Управление стрессами
Управление стрессами Психодрама. Создание и развитие психодрамы
Психодрама. Создание и развитие психодрамы Конфликтные ситуации в деятельности вожатого и их разрешение. Возрастные особенности детей
Конфликтные ситуации в деятельности вожатого и их разрешение. Возрастные особенности детей Медиативные навыки: инструментарий медиатора
Медиативные навыки: инструментарий медиатора Мышление в психическом развитии. Лекция 6
Мышление в психическом развитии. Лекция 6 Темперамент и выбор профессии
Темперамент и выбор профессии Психологія пам’яті
Психологія пам’яті Общение как специфический вид деятельности
Общение как специфический вид деятельности Катализаторы креативности
Катализаторы креативности Отношение пожилых к старости
Отношение пожилых к старости Введение в психологию. Предмет, задачи и методы психологии
Введение в психологию. Предмет, задачи и методы психологии Жесты и мимика как невербальные средства общения
Жесты и мимика как невербальные средства общения Эмпирические исследования познавательных процессов. ОПП- 2
Эмпирические исследования познавательных процессов. ОПП- 2