Clinical and serologic differences of hemolytic disease among ABO and Rh
sensibilisation
1. a - и b –agglutinins normally exists in blood serum of mother and capable to penetrate fetus. Rh antibodies normally are absent both in mother and fetus.
2. Anti-A and Anti-B being full agglutinins as other antibodies could penetrate placenta whereas full Rh antibodies couldn’t penetrate it.
3. Fetus tissues in “extractors”( people who reveals A and B substances not only in blood but in humors as well) and in “non-extractors” contains both A and B substances which is usually neutralizes anti-A and anti-B antibodies. Rh –antibodies doesn’t neutralizes by the tissue antibodies therefore their infiltration of Rh positive fetus causes hemolysis. This very characteristic differential feature of ABO antibodies leads to hemolytic disease development without previous sesibilisation as mother blood already consists of a and b agglutinins.
 Технико-экономический анализ деятельности Свердловской дистанции электроснабжения. Разработка мероприятий по снижению издержек
Технико-экономический анализ деятельности Свердловской дистанции электроснабжения. Разработка мероприятий по снижению издержек Нравственная культура личности
Нравственная культура личности Треугольник. Равенство и подобие треугольников
Треугольник. Равенство и подобие треугольников 1_fevralya_dlya_DO
1_fevralya_dlya_DO Скульптура первой половины XIX века
Скульптура первой половины XIX века Основы физиологии труда и комфортные условия жизнедеятельности
Основы физиологии труда и комфортные условия жизнедеятельности презентация к курсу История и культура Санкт- Петербурга
презентация к курсу История и культура Санкт- Петербурга Мультимедийная викторина Природа родного края
Мультимедийная викторина Природа родного края Эталоны единиц величин бесконтактных средств измерений температуры
Эталоны единиц величин бесконтактных средств измерений температуры Разминки-пятиминутки
Разминки-пятиминутки Формирование универсальных учебных действий на уроках в начальной школе
Формирование универсальных учебных действий на уроках в начальной школе Завершающий период Великой Отечественной войны
Завершающий период Великой Отечественной войны Сүйек-буын туберкулезі
Сүйек-буын туберкулезі Презентация: Стихийные природные явления России
Презентация: Стихийные природные явления России Чрезвычайные ситуации экологического характера
Чрезвычайные ситуации экологического характера Архітектура комп'ютера
Архітектура комп'ютера Социально-коммуникативное развитие НОД Путешествие в весенний лес-1 младшая группа
Социально-коммуникативное развитие НОД Путешествие в весенний лес-1 младшая группа Урок географии в 7 классе коррекционной школы VIII вида на тему Животный мир тундры
Урок географии в 7 классе коррекционной школы VIII вида на тему Животный мир тундры Wall Calendar 2017: NASA
Wall Calendar 2017: NASA Оздоровительная физическая культура и ее формы. Влияние оздоровительной физической культуры на организм человека
Оздоровительная физическая культура и ее формы. Влияние оздоровительной физической культуры на организм человека Презентации к урокам
Презентации к урокам Правила поведения за столом. Занятие 1.
Правила поведения за столом. Занятие 1. Презентация Метод учебного проекта
Презентация Метод учебного проекта Новый фитнес с бассейном
Новый фитнес с бассейном Древний Китай
Древний Китай Lubrication
Lubrication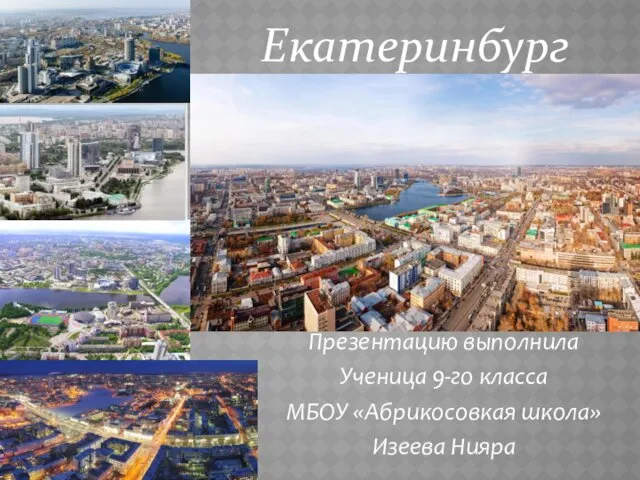 Административный центр Уральского федерального округа Екатеринбург
Административный центр Уральского федерального округа Екатеринбург Окислительно-восстановительные процессы и реакции
Окислительно-восстановительные процессы и реакции