Содержание
- 2. Terminology: The word shock ( "choc " in French and "shock " in English) is translated
- 3. Shock - critical condition which develops as a result of impact on the body a factor
- 4. Shock is not a disease entities, it decompensation syndrome, which is accompanied by a variety of
- 7. Physiological constants Blood volume (CBV) - 70 ml / kg (males 70-75, 65-70 women). Distribution of
- 8. Classification According to the basic link of pathogenesis are 4 kinds of shock: hypovolemic cardiogenic obstructive
- 9. 1.Hypovolemic- it is based on reduction of CBV. These include: hemorrhagic, traumatic shock, burn shock, dehydration
- 12. Keep in mind that, regardless of the primary cause, in the final phases of the shock
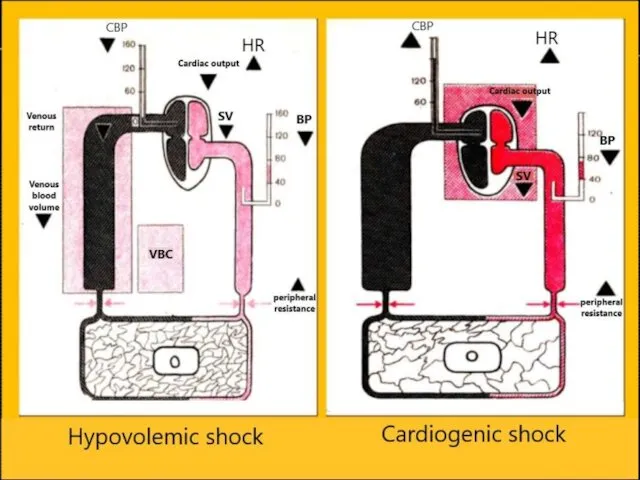
- 13. Hypovolemic shock
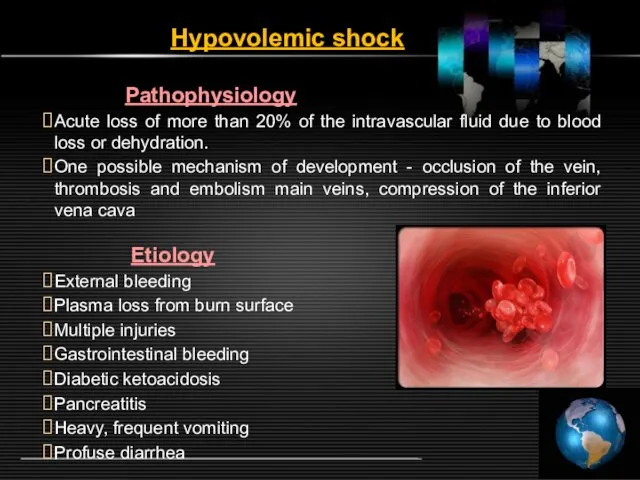
- 14. Hypovolemic shock Pathophysiology Acute loss of more than 20% of the intravascular fluid due to blood
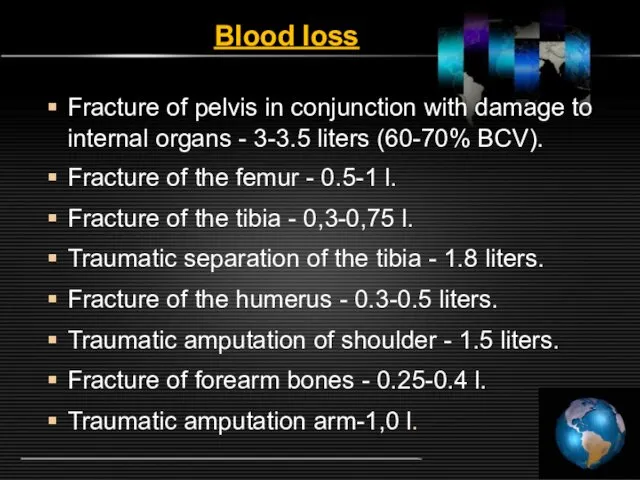
- 15. Blood loss Fracture of pelvis in conjunction with damage to internal organs - 3-3.5 liters (60-70%
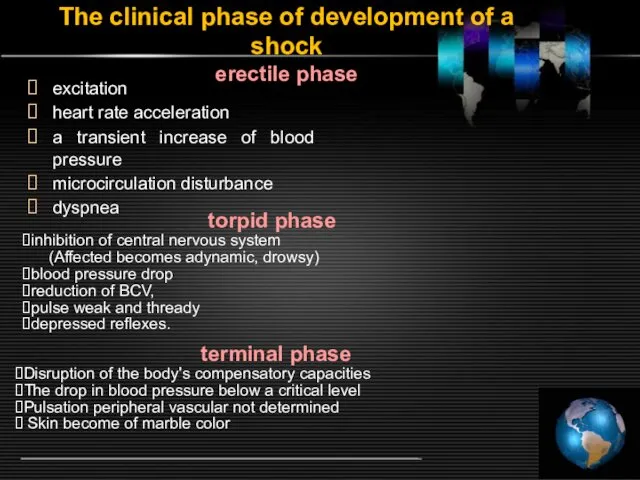
- 16. The clinical phase of development of a shock erectile phase excitation heart rate acceleration a transient
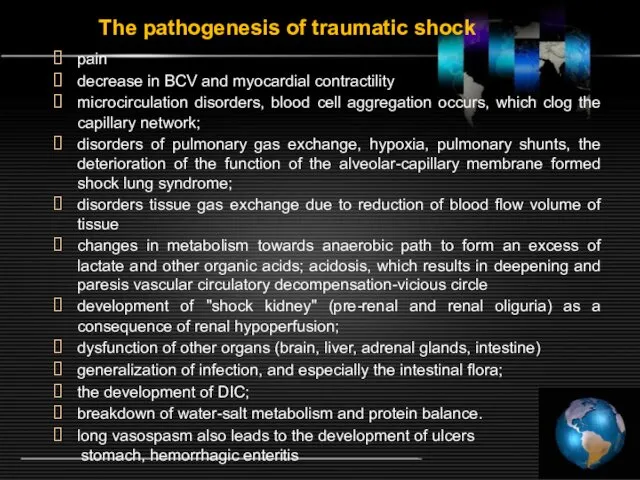
- 17. The pathogenesis of traumatic shock pain decrease in BCV and myocardial contractility microcirculation disorders, blood cell
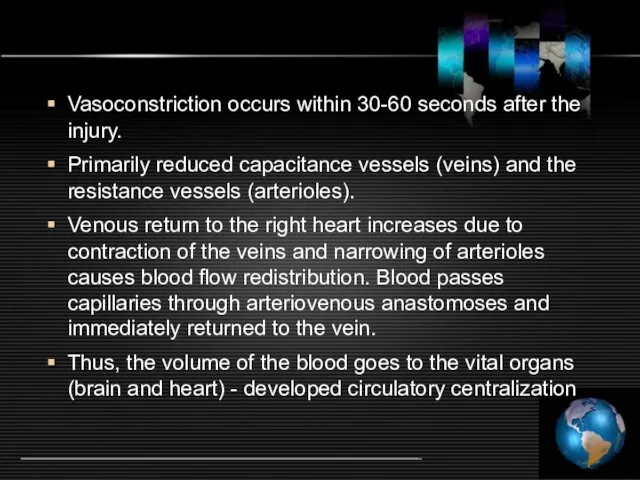
- 18. Vasoconstriction occurs within 30-60 seconds after the injury. Primarily reduced capacitance vessels (veins) and the resistance
- 19. Next compensation mechanism that develops within the first hour - interstitial fluid enters to the bloodstream.
- 20. Total effects ADH and RAAS leads to a decrease in diuresis. Retention of water and salts
- 21. Hemodynamics and survey data fizikalgo low CVP Low cardiac output High peripheral vascular resistance Jugular veins
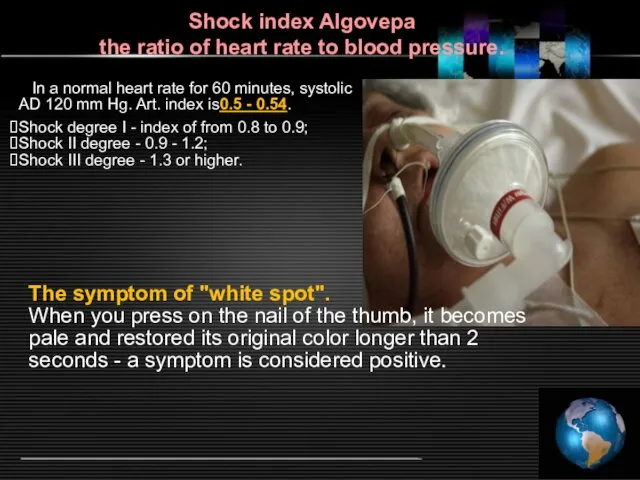
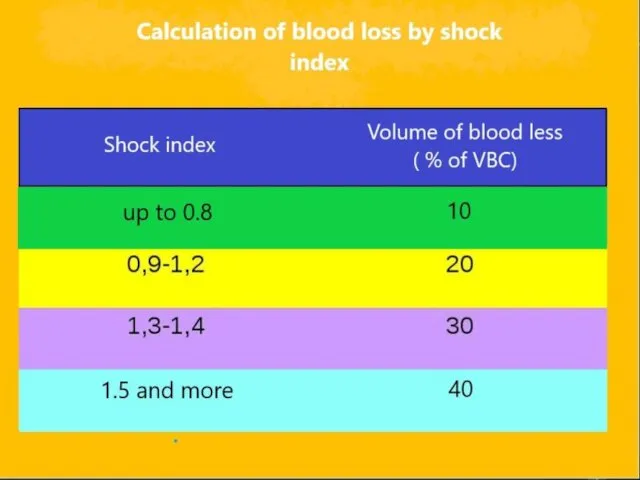
- 22. Shock index Algovepa the ratio of heart rate to blood pressure.
- 24. "Small" signs of shock pale skin conjunctival pallor cold sticky sweat mouth dryness thirst a symptom
- 25. Reduction of hemoglobin, hematocrit, red blood cells in peripheral blood does not develop immediately (the need
- 26. Stages of shock I st- compensated - loss of 20% of BCV - systolic BP 90-100
- 27. III st- decompensated reversible - loss of 30-40% of BCV - systolic BP 50-70 mmHg, pulse
- 28. Treatment of hemorrhagic and traumatic shock
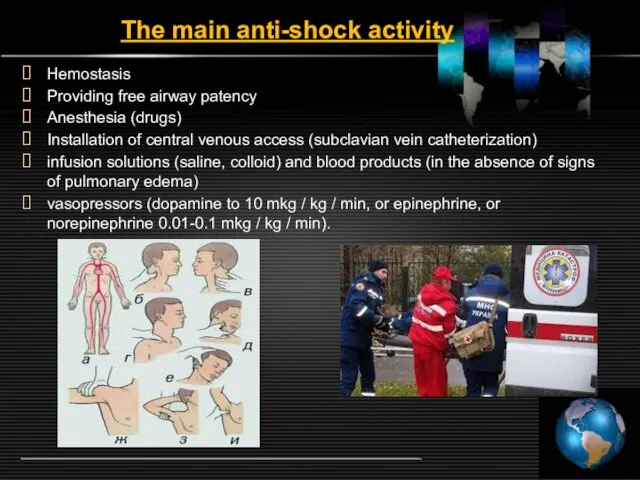
- 29. The main anti-shock activity Hemostasis Providing free airway patency Anesthesia (drugs) Installation of central venous access
- 30. Prehospital aid Partially revised the tactics of infusion-transfusion therapy in the prehospital phase. If bleeding is
- 31. Adequate consciousness, sufficient diuresis (30 ml / hr), the absence of a severe tachycardia and hyperventilation,
- 32. When a shock is suspected: identify the specific cause and severity of the condition carry out
- 33. General principles of treatment The basis of any treatment of hypovolemic shock is fluid resuscitation, i.e
- 34. Following questions need to be decided before planning treatment where what how much and in what
- 35. Crystalloid infusion solutions or colloids and crystalloids simultaneously insert at the beginning. If rapid infusion in
- 36. Blood transfusion, especially red blood cell mass is advisable to begin only after the full recovery
- 37. Classification of plasma substitutes
- 38. Crystalloid solutions: drugs with low molecular weight quickly leave the bloodstream and move into the interstitial
- 39. 2. The colloid plasma expanders This solution of high molecular weight, which for a long time
- 40. Hydroxyethyl starch derivatives: low MW (130,000) It belongs to the pharmacological group "Tetrastarch "- Voluven®, Volyutenz
- 41. Algorithms infusion-transfusion therapy for different amounts of blood loss 1.Blood loss up to 10% VBC does
- 42. 4.Defitsit VBC 20-30% - synthetic colloids, crystalloids plasma expanders. The ratio of colloids - crystalloids 1:
- 43. In the treatment of traumatic shock should not forget the need for adequate immobilization and full
- 44. Clinic of shock depends on the reasons that cause shock and localization of the injury. Traumatic
- 45. Criteria of efficiency antishock therapy 1. In patients without cardiac disease: Mean blood pressure> 60 mm
- 46. Pathophysiology Reducing the stroke volume of the heart with the defeat: - violation of the contractile
- 47. Hemodynamics and physical examination data High CVP Low cardiac output High peripheral vascular resistance Jugular venous
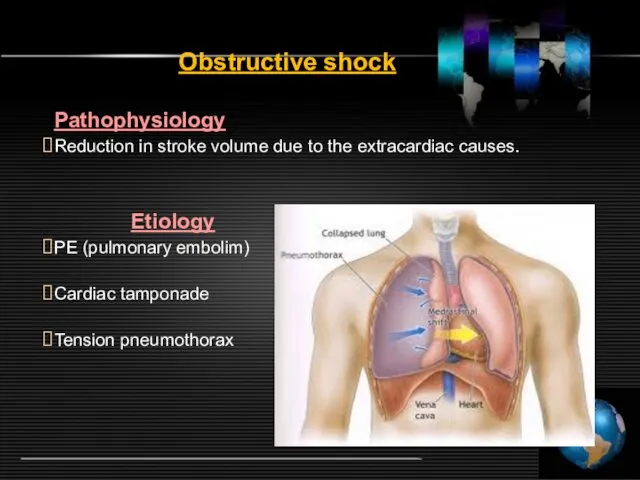
- 48. Obstructive shock Pathophysiology Reduction in stroke volume due to the extracardiac causes. Etiology PE (pulmonary embolim)
- 49. Hemodynamics and physical examination data High or Low CVP Low cardiac output High peripheral vascular resistance
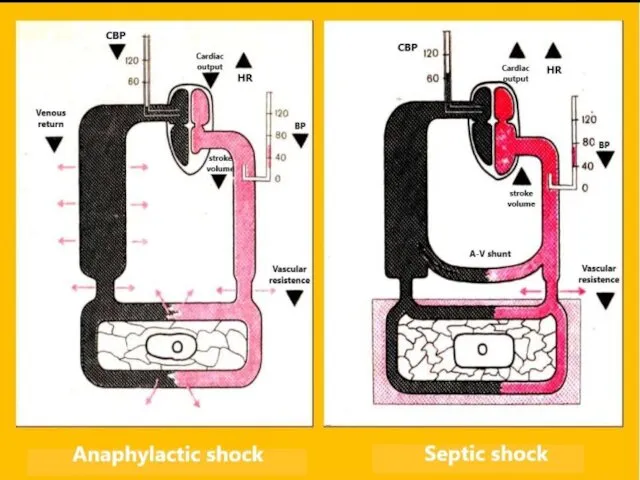
- 50. Distributive shock Pathophysiology A significant reduction in peripheral vascular resistance with redistribution intravascular volume due to
- 51. Hemodynamics and physical examination data Low CVP Increased cardiac output Low resistance peripheral vessels Lack of
- 52. Symptoms of shock Decreased blood pressure; Increased heart rate >90 beats per minute, the pulse becomes
- 53. The adult patients compensate state of shock principally by decrease systemic vascular resistance, increase cardiac contractility
- 54. Anaphylactic shock or anaphylaxis - acute generalized allergic reaction of immediate type, the state dramatically increased
- 55. One of the most dangerous complications of drug allergy, ends in 10-20% of cases, lethal. The
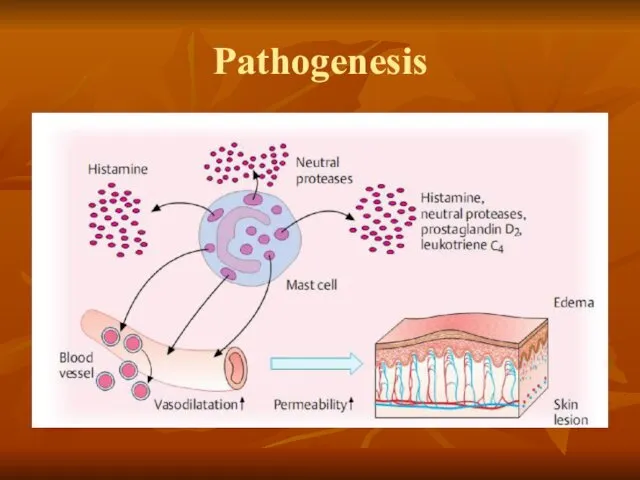
- 56. Pathogenesis
- 57. Etiology Medication. The introduction of blood products. Food products (eggs, coffee, cocoa, chocolate, strawberry, fish, milk,
- 58. Clinical symptoms 1. Initial period develops within 3-30 minutes after allergen exposure (medication, food, insect sting
- 59. Clinical symptoms 2. The period of clinical manifestation characterized by loss of consciousness, decrease of blood
- 60. clinical symptoms 3. Output period of shock usually lasts 3-4 weeks. Patients have weakness, headache, memory
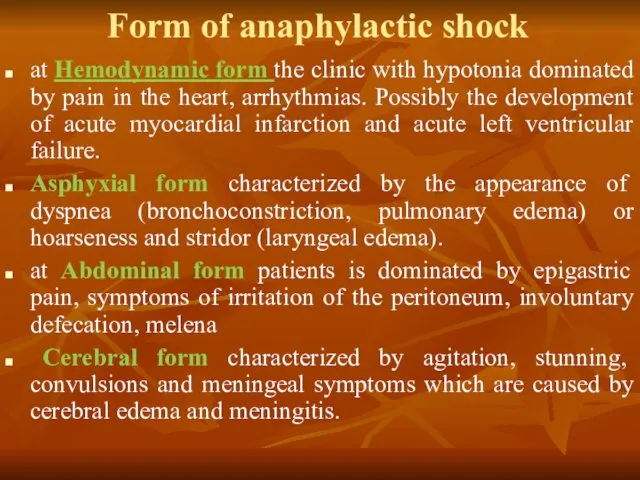
- 61. Form of anaphylactic shock at Hemodynamic form the clinic with hypotonia dominated by pain in the
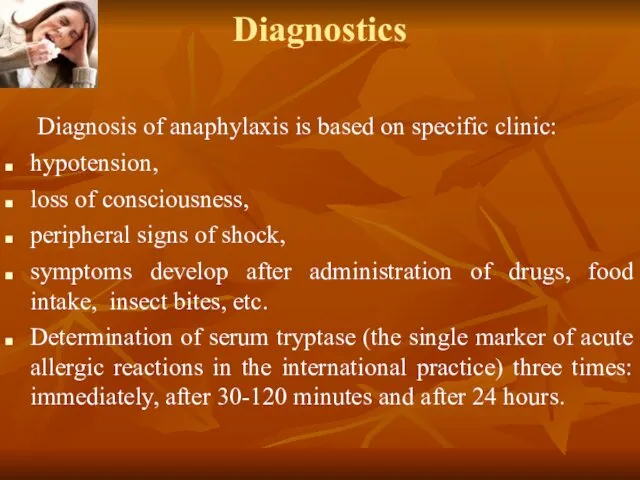
- 62. Diagnostics Diagnosis of anaphylaxis is based on specific clinic: hypotension, loss of consciousness, peripheral signs of
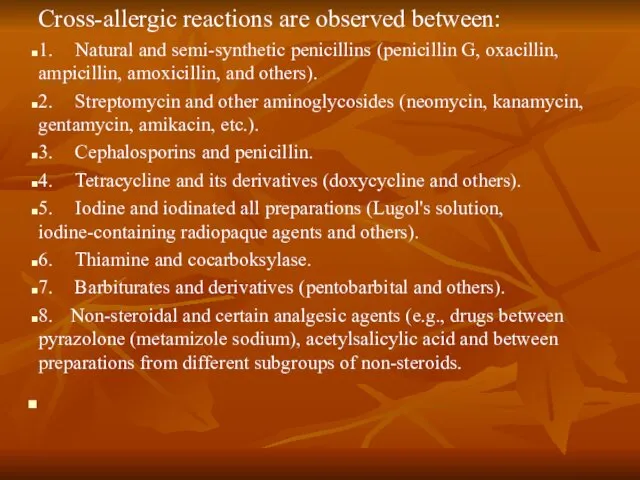
- 63. Cross-allergic reactions are observed between: 1. Natural and semi-synthetic penicillins (penicillin G, oxacillin, ampicillin, amoxicillin, and
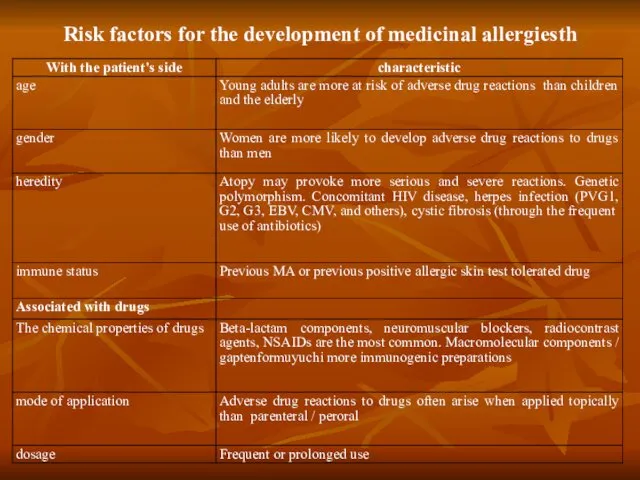
- 64. Risk factors for the development of medicinal allergiesth
- 65. First aid 90% of allergic reactions developed within 10 minutes after drug application.
- 66. Tourniquet on the limb does not overlap! The injection site is not pricked around!
- 67. Priority treatment Epinephrine (adrenaline) may save the patient's life, therefore, should be immediately administered as first-line
- 68. The second line of treatment It should suspend trigger anaphylactic reactions Providing the correct body position
- 69. In severe shock is necessary to transfer the patient on mechanical ventilation with increased concentration of
- 70. In cases of a significant tachycardia (> 120 beats / minute) tachyarrhythmia or blood pressure may
- 71. According to modern views the introduction of chloride or calcium gluconate, was widely practiced before can
- 72. H1 blockers and systemic H2 receptor can alleviate the symptoms of cutaneous anaphylaxis (infusion - H1-receptor
- 73. Patients who exhibit respiratory failure should be carefully inspected for at least 6-8 hours; patients who
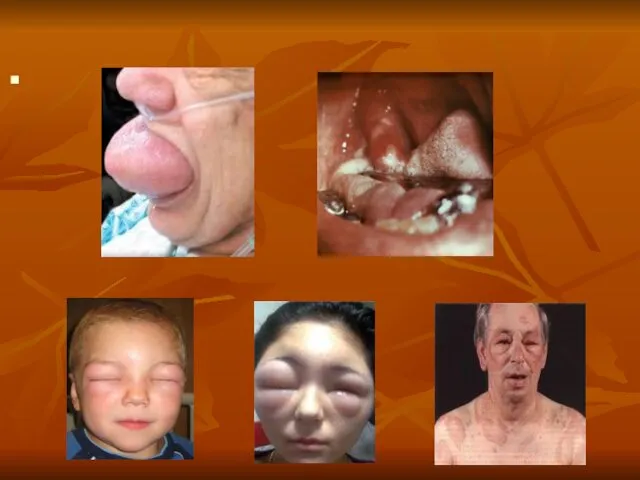
- 75. allergic urticaria
- 76. allergic urticaria
- 78. Скачать презентацию











 ПРЕЗЕНТАЦИЯ: РАЗВИТИЕ ИГРОВОЙ ДЕЯТЕЛЬНОСТИ ДЕТЕЙ ДОШКОЛЬНОГО ВОЗРАСТА
ПРЕЗЕНТАЦИЯ: РАЗВИТИЕ ИГРОВОЙ ДЕЯТЕЛЬНОСТИ ДЕТЕЙ ДОШКОЛЬНОГО ВОЗРАСТА Строение периферического отдела скелета животных
Строение периферического отдела скелета животных Описание климата по климатограммам
Описание климата по климатограммам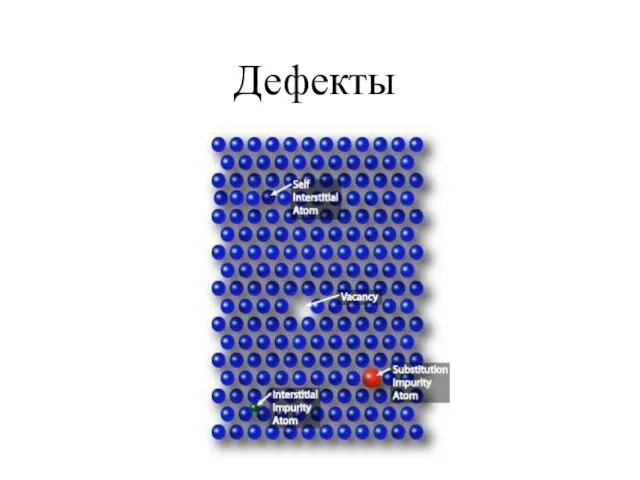 Кристаллизация Осмия. Дефекты. Поликристаллы
Кристаллизация Осмия. Дефекты. Поликристаллы Обструктивные уропатии
Обструктивные уропатии Строение атома
Строение атома 12 ИЮНЯ ДЕНЬ РОССИИ
12 ИЮНЯ ДЕНЬ РОССИИ Предмет и метод экономической теории
Предмет и метод экономической теории Урок естествознания 10 класс Традиции и революции в естествознании. Религиозная традиция
Урок естествознания 10 класс Традиции и революции в естествознании. Религиозная традиция Школы менеджмента
Школы менеджмента Взаимодействие с родителями в процессе обучения ребёнка мелкой моторики.
Взаимодействие с родителями в процессе обучения ребёнка мелкой моторики. Классификация инноваций
Классификация инноваций Минералы Урала
Минералы Урала презентация Реакции обмена
презентация Реакции обмена Атмосфера. Ветер
Атмосфера. Ветер Презентация Фосфор
Презентация Фосфор Электропитание и электроснабжение нетяговых потребителей
Электропитание и электроснабжение нетяговых потребителей Презентация Трудности адаптации ребенка в 5 классе
Презентация Трудности адаптации ребенка в 5 классе Северная война 1700-1721
Северная война 1700-1721 Разработка мобильных приложений на 1С и организация взаимодействия через Интернет
Разработка мобильных приложений на 1С и организация взаимодействия через Интернет Второстепенные члены предложения. Повторение и систематизация материала
Второстепенные члены предложения. Повторение и систематизация материала Развитию речи у детей старшего дошкольного возраста на тему: Здравствуй, лето!
Развитию речи у детей старшего дошкольного возраста на тему: Здравствуй, лето! Кільватерне прискорення частинок в плазмі (plasma wakefield acceleration)
Кільватерне прискорення частинок в плазмі (plasma wakefield acceleration) Апаптоз патофизилогиясы
Апаптоз патофизилогиясы Презентация Кабинет педагога-психолога
Презентация Кабинет педагога-психолога Трипілля – Кукутені. Загадки унікальної культури
Трипілля – Кукутені. Загадки унікальної культури Русская архитектура XVI - XVII веков
Русская архитектура XVI - XVII веков Портфолио Натальи Рудяковой. Маркетолог
Портфолио Натальи Рудяковой. Маркетолог