Содержание
- 2. DIAGNOSTIC APPROACH TO COLIC IN ADULT HORSES PAIN – degree, duration, and type PULSE – rate
- 3. MEDICAL MANAGEMENT OF COLIC IN ADULT HORSES Non-steroidal anti-inflammatory drugs (NSAIDs )- Flunixin meglumine, ketoprofen, and
- 4. Decompression - gastric decompression via a nasogastric tube, cecal enterocentesis in the right paralumbar fossa Alternate
- 5. LAXATIVES – mineral oil at 0.5-1 gallon via NGT in an adult horse. magnesium sulfate (Epsom
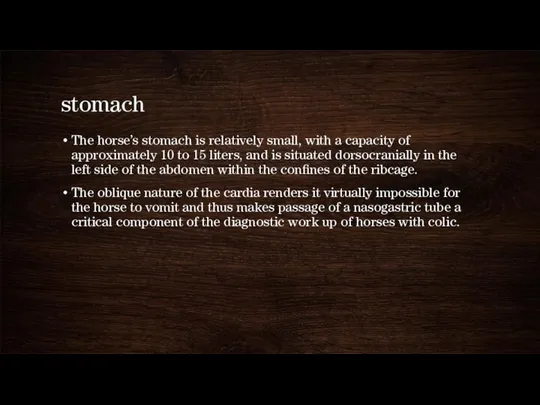
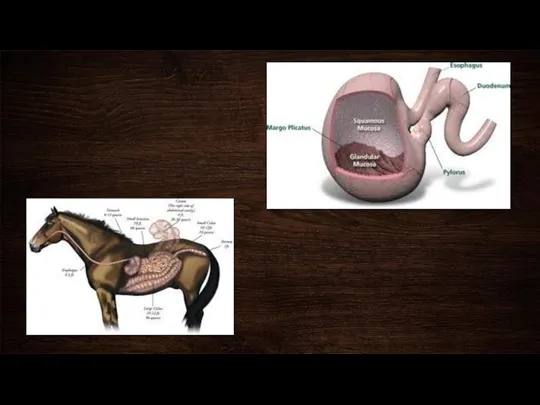
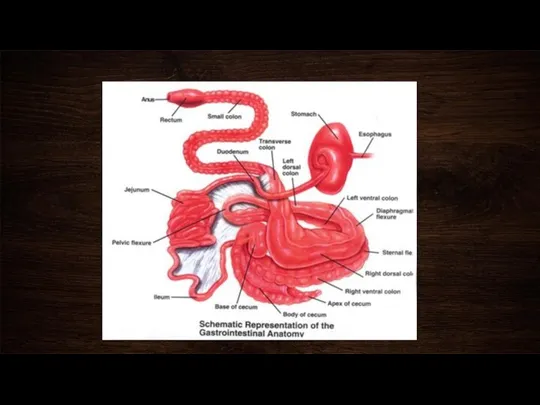
- 6. stomach The horse’s stomach is relatively small, with a capacity of approximately 10 to 15 liters,
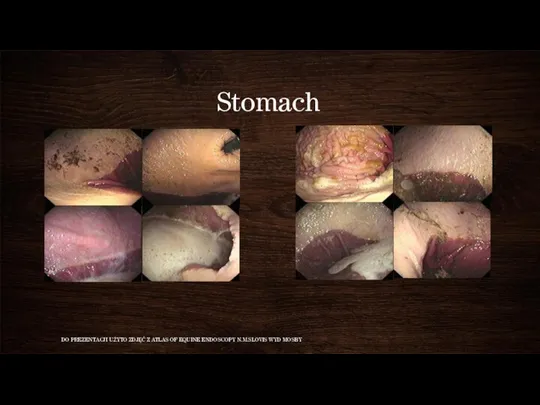
- 8. Stomach DO PREZENTACJI UŻYTO ZDJĘĆ Z ATLAS OF EQUINE ENDOSCOPY N.M.SLOVIS WYD MOSBY
- 9. Gastritis Gastritis is an inflammation and irritation of the lining of the stomach. Unlike a stomach
- 10. Acute Gastritis Acute gastritis is caused by ingesting moldy or spoiled feed, sand, chemicals and toxins,
- 11. Chronic Gastritis Chronic gastritis is associated with the long-standing ingestion of poor quality feeds or foreign
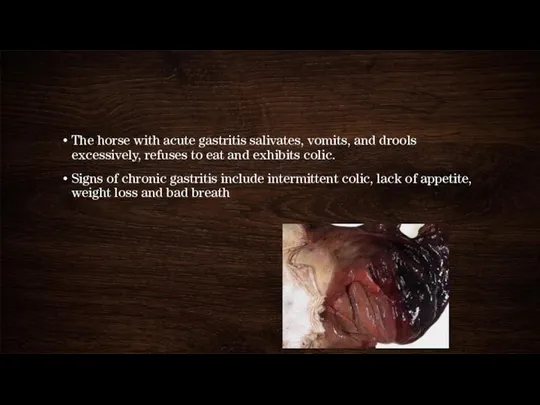
- 12. The horse with acute gastritis salivates, vomits, and drools excessively, refuses to eat and exhibits colic.
- 13. treatment H2 receptors blockers – ranitidin 6-7 mg/kg every 8 hours, cymetidin 10-20 mg/kg Proton pump
- 14. Gastric ulcers Ulcers are a common medical condition in horses and foals. It is estimated that
- 15. Stomach is divided into two distinct parts. The non-glandular portion (also called the esophageal region) is
- 16. Causes of gastric ulcers Fasting (not eating) - Horses evolved to graze, eating many small meals
- 17. Signs of gastric ulcers in horses In foals, signs of gastric ulcers include: Intermittent colic, often
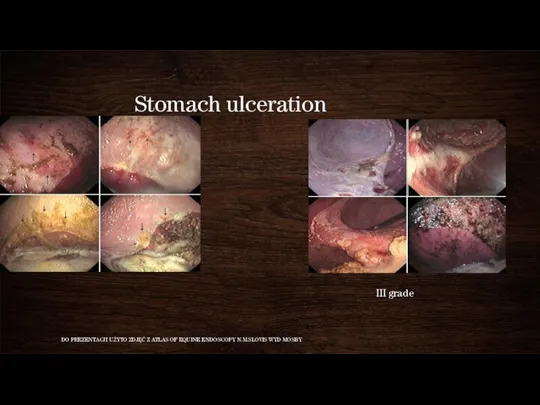
- 18. Stomach ulceration I grade DO PREZENTACJI UŻYTO ZDJĘĆ Z ATLAS OF EQUINE ENDOSCOPY N.M.SLOVIS WYD MOSBY
- 19. Treatment of gastric ulcers in horses H2 blockers: These are medications that block the action of
- 20. In addition to medications, changes in management are almost always necessary including: Increasing the amount of
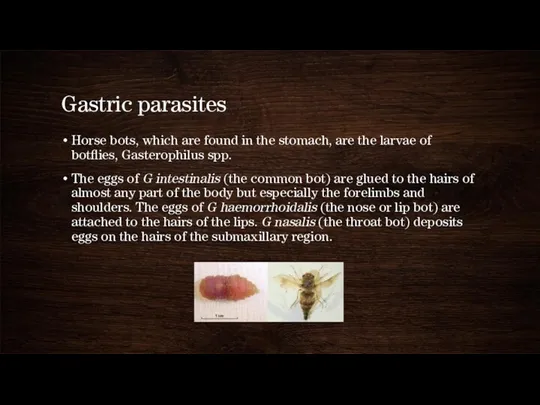
- 21. Gastric parasites Horse bots, which are found in the stomach, are the larvae of botflies, Gasterophilus
- 22. The larvae of all 3 species apparently stay embedded in the tongue or the mucosa of
- 23. Bots cause a mild gastritis, but large numbers may be present with no clinical signs. The
- 24. ATLAS OF EQUINE ENDOSCOPY N.M.SLOVIS WYD MOSBY
- 25. Gastric dilatation and rupture Gastric dilatation can be classified as primary, secondary, or idiopathic. Causes of
- 26. Secondary gastric dilatation occurs more commonly and can result from primary intestinal ileus or small or
- 27. Gastric dilation usually produces: Acute, severe colic Tachycardia Pale mucous membranes Retching Ingesta at the nares
- 28. Primary gastric dilation should be suspected : copious amounts of gastric reflux in the absence of
- 29. Gastric rupture results in septic peritonitis which will be reflected in the nature of fluid collected
- 30. treatment Gastric lavage (water or oil) Treat underlying disease
- 31. Gastric Impaction (Obstruction) Gastric impaction can result in either acute or chronic signs of colic. Although
- 32. Clinical signs The colic associated with gastric impaction varies from mild and chronic to acute and
- 33. treatment gastric lavage with water IV fluid therapy and analgesia the impacted stomach can be felt
- 34. prevention Regular dental care Ensure sugar beet nuts are adequately soaked prior to feeding Secure storage
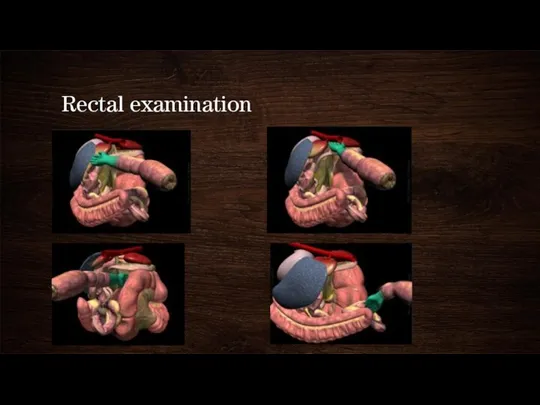
- 36. Rectal examination
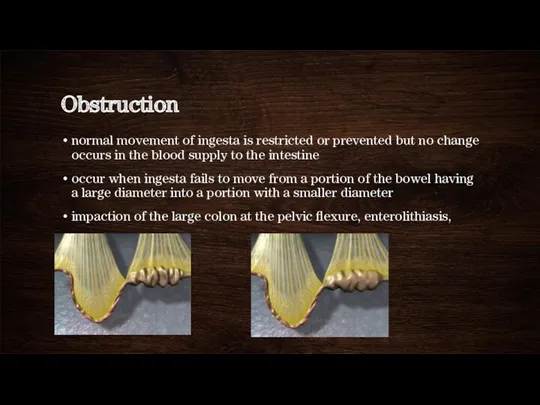
- 37. Obstruction normal movement of ingesta is restricted or prevented but no change occurs in the blood
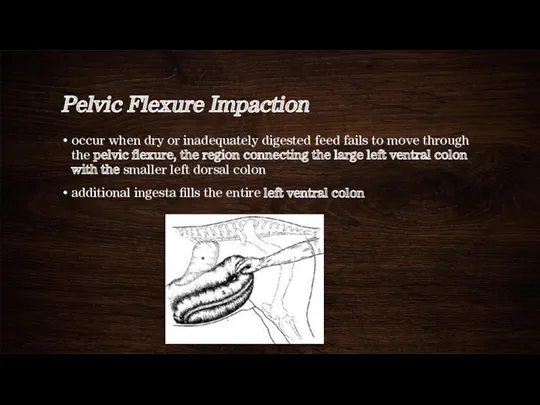
- 38. Pelvic Flexure Impaction occur when dry or inadequately digested feed fails to move through the pelvic
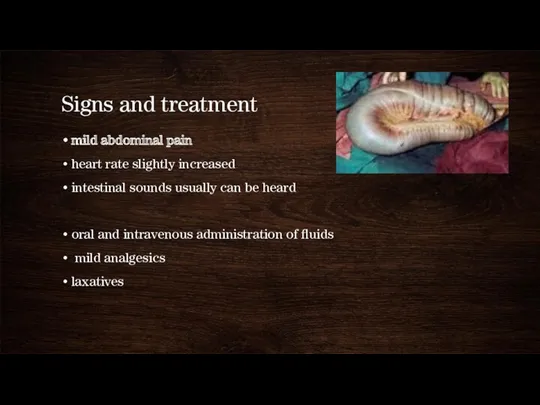
- 39. Signs and treatment mild abdominal pain heart rate slightly increased intestinal sounds usually can be heard
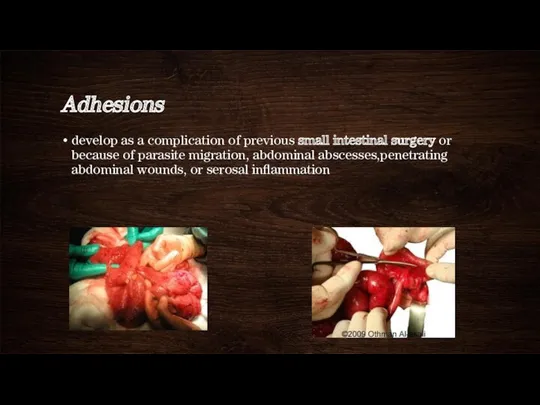
- 40. Adhesions develop as a complication of previous small intestinal surgery or because of parasite migration, abdominal
- 41. history of a gradual onset of colic and weight loss, and in many instances the pain
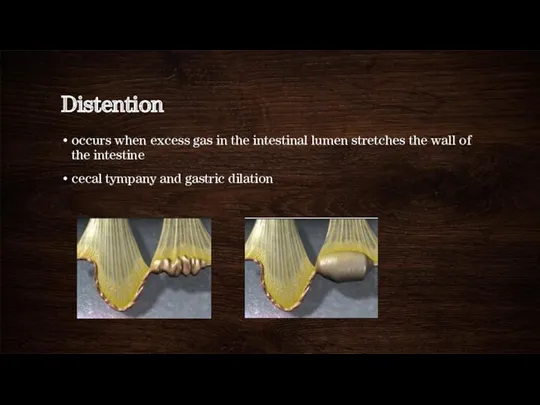
- 42. Distention occurs when excess gas in the intestinal lumen stretches the wall of the intestine cecal
- 43. Cecal Tympany occurs commonly in horses with colonic displacements, colon volvulus, or obstruction of the small
- 44. distention of the abdomen tight paralumbar fossae pain tachycardia and tachypnea high-pitched pinging sound in the
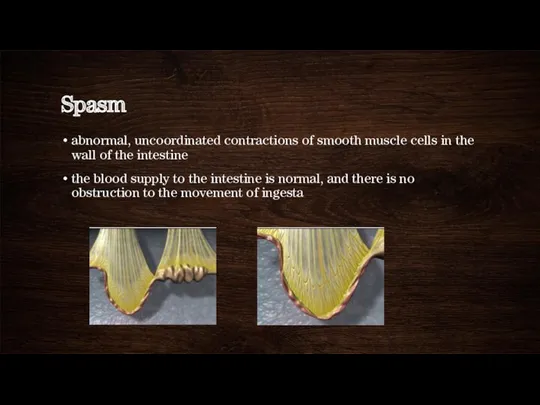
- 45. Spasm abnormal, uncoordinated contractions of smooth muscle cells in the wall of the intestine the blood
- 46. Spasmodic Colic occurs due to spasm or cramping of intestinal musculature diagnosis is based on the
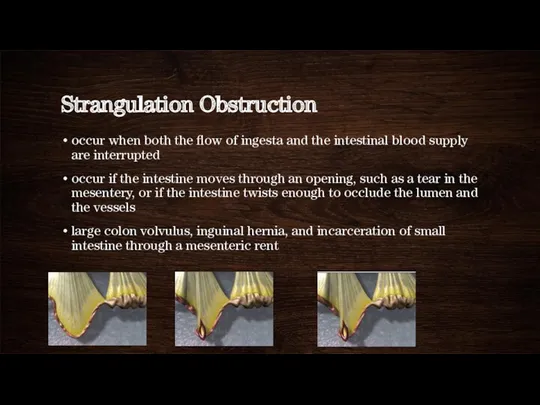
- 47. Strangulation Obstruction occur when both the flow of ingesta and the intestinal blood supply are interrupted
- 48. Small Intestinal Strangulation through Mesenteric Rent defect in the small intestinal mesentery called a mesenteric rent
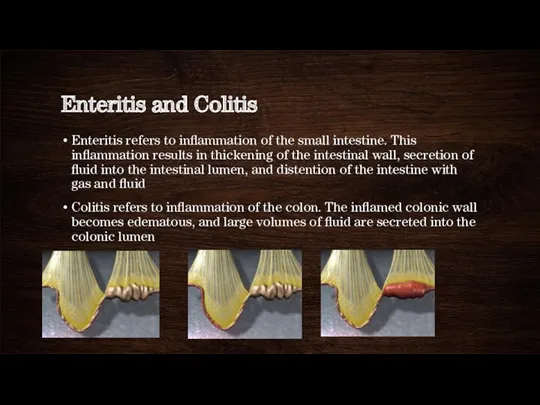
- 49. Enteritis and Colitis Enteritis refers to inflammation of the small intestine. This inflammation results in thickening
- 50. Nonstrangulating Infarction Loss of blood supply to part of the intestine in the absence of a
- 51. thromboembolism or a reduction in local blood flow secondary to parasitism postoperative Signs: chronic intermittent episodes
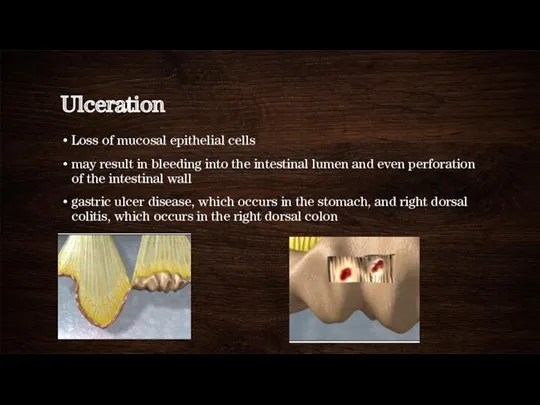
- 52. Ulceration Loss of mucosal epithelial cells may result in bleeding into the intestinal lumen and even
- 54. Скачать презентацию

 Многообразие живого мира. Уровни организации живой материи
Многообразие живого мира. Уровни организации живой материи Какую роль играет религия в жизни современного российского общества
Какую роль играет религия в жизни современного российского общества Презентация о школе
Презентация о школе Практическая работа Получение уксусной кислоты и опыты с ней
Практическая работа Получение уксусной кислоты и опыты с ней Изображение рельефа на плане местности
Изображение рельефа на плане местности Мировая религия пастафарианство
Мировая религия пастафарианство Презентация по бисероплетению
Презентация по бисероплетению как подготовить и провести интегрированный урок
как подготовить и провести интегрированный урок Презентация Згоднев
Презентация Згоднев Базовые понятия реляционных баз данных. Лекция 6
Базовые понятия реляционных баз данных. Лекция 6 Олимпийские игры От древности до современности
Олимпийские игры От древности до современности Понятие, функции, виды религии
Понятие, функции, виды религии Презентация по методической теме: Балаларда туган җиребезгә мәхәббәт, аның табигатенә карата сакчыл караш тәрбияләү һәм экологик тәрбия бирү 2011-2015 год
Презентация по методической теме: Балаларда туган җиребезгә мәхәббәт, аның табигатенә карата сакчыл караш тәрбияләү һәм экологик тәрбия бирү 2011-2015 год : Вежливость.
: Вежливость. Портфолио модели и фотографа
Портфолио модели и фотографа Прекрасные дамы Елизаветинского времени. Елизавета I и другие
Прекрасные дамы Елизаветинского времени. Елизавета I и другие Основы исторического знания
Основы исторического знания Театральные профессии
Театральные профессии Переодические и непериодические бесконечные десятичные дроби
Переодические и непериодические бесконечные десятичные дроби История метода проектов в педагогике
История метода проектов в педагогике Трансплантология - создаем нового человека
Трансплантология - создаем нового человека Тайна бумажного листа
Тайна бумажного листа Палеография эпохи феодализма
Палеография эпохи феодализма План выполнения Ремонтной программы ООО Газпром теплоэнерго наименование ДО на 2021 год
План выполнения Ремонтной программы ООО Газпром теплоэнерго наименование ДО на 2021 год Основы религиозных культур и светской этики. Родительское собрание
Основы религиозных культур и светской этики. Родительское собрание Веселый мир Оригами - презентация
Веселый мир Оригами - презентация Терехин. Герой без Золотой звезды!
Терехин. Герой без Золотой звезды! Разложение по переменным. ДМ 2. ДНФ и КНФ
Разложение по переменным. ДМ 2. ДНФ и КНФ