Слайд 2
DEFINITION
Shock it is a severe disturbance of hemodynamic in which the
circulatory system fails to maintain adequate perfusion of vital organ.
Traumatic shock is characterized by severe tissue. damage, such as multiple fractures, severe contusions, or burns.
Слайд 3
SHOCK IN TRAUMA
Classification
Hypovolemic
Distributive
Cardiogenic
Слайд 4
HYPOVOLEMIC SHOCK
MOST COMMON CAUSE OF SHOCK IN THE TRAUMA PATIENT
DUE TO
HEMORRHAGE ( LOSS OF RBCS IMPAIRS OXYGEN TRANSPORTATION
IN ANY TRAUMA PATIENT WITH SHOCK, ASSUME HAEMORRHAGE IS CAUSE UNTIL PROVEN OTHERWISE
Слайд 5
DISTRIBUTIVE SHOCK
NEUROGENIC SHOCK
DECREASED SYSTEMIC VASCULAR RESISTANCE DUE TO VASODILATION
MOST
COMMON CAUSE IN SPINAL CORD INJURY
Слайд 6
CARDIOGENIC SHOCK
INTRINSIC
BLUNT CARDIAC TRAUMA LEADING TO MUSCLE DAMAGE AND DYSRHYTHMIA
VALVULAR DISCRUPTION
EXTRINSIC
PERICARDIAL TAMPONADE
TENSION PNEUMOTHORAX
Слайд 7
TRAUMATIC SHOCK MECHANISM
Microcirculation –Systemic vascular resistance rises to maintain a
level of systemic pressure that is adequate for perfusion of the heart and brain at the expense of other tissue. Arteriolar vascular smooth cells has both α- and β–adrenergic receptors. Norepinephrine release - acting on α 1 -receptors as vasoconstrictor - is the fundamental compensatory response in shock. –Reduced filtration because of decreased capillary surface area across which filtration occurs.
Consequence: increased interstitial and intravascular volume at the expense of intracellular volume.
Слайд 8
TRAUMATIC SHOCK MECHANISM
Cellular response –Decline of intracellular high energy phosphate
stores (decreased amount of ATP) because of the mitochondrial dysfunction.
Consequences: Accumulation of hydrogen ions, lactate (products of anaerobic metabolism) As shock progresses, these vasodilatation metabolites cause further hypotension and hypo perfusion
Слайд 9
TRAUMATIC SHOCK MECHANISM
Cardiovascular response –Decreased ventricular filling (decreased preload). The
increased heart rate is a useful but limited compensatory mechanism to maintain the adequate stroke volume –Impaired myocardial contractility which reduces the stroke volume –Elevated systemic vascular resistance (except of hyper dynamic stage of septic shock) increases the afterload
Слайд 10
TRAUMATIC SHOCK MECHANISM
Pulmonary response –Increased pulmonary vascular resistance (particularly in
septic shock) –Tachypnoe, but restricted ventilation, reduced functional residual capacity – atelectasis. –Acute respiratory distress syndrome characterized by noncardiogenic pulmonary oedema secondary to pulmonary capillary endothelial and alveolar epithelial injury
Слайд 11
TRAUMATIC SHOCK MECHANISM
Renal response –Consequences of hypo perfusion: reduced renal
blood flow, increased afferent arteriolar resistance – reduced glomerular filtration rate together with the increased aldosterone and vasopressin production will cause reduced urine volume –Acute tubular necrosis as a result of interaction of shock, sepsis and administration of nephrotoxic agents
Слайд 12
TRAUMATIC SHOCK MECHANISM
Inflammatory responses –Activation of an extensive network of
proinflammatory mediator systems plays a significant role in the progression of shock and contributes to the development of organ injury Activation of classic and alternative pathways of complement cascade causing cell damage Activation of coagulation cascade causes microvascular thrombosis Tumour necrosis factor-α, produced by activated macrophages contributes to hypotension, lactic acidosis, and respiratory failure IL-8 upregulate adhesion molecules on the neutrophil to enhance aggregation, and damage to the vascular endothelium Increased Thromboxane A 2 levels is potent vasoconstrictor that contributes to the pulmonary hypertension
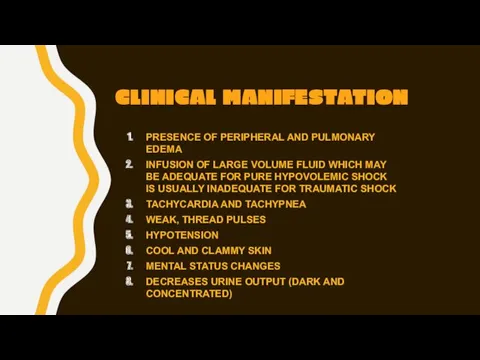
Слайд 13
CLINICAL MANIFESTATION
PRESENCE OF PERIPHERAL AND PULMONARY EDEMA
INFUSION OF LARGE
VOLUME FLUID WHICH MAY BE ADEQUATE FOR PURE HYPOVOLEMIC SHOCK IS USUALLY INADEQUATE FOR TRAUMATIC SHOCK
TACHYCARDIA AND TACHYPNEA
WEAK, THREAD PULSES
HYPOTENSION
COOL AND CLAMMY SKIN
MENTAL STATUS CHANGES
DECREASES URINE OUTPUT (DARK AND CONCENTRATED)
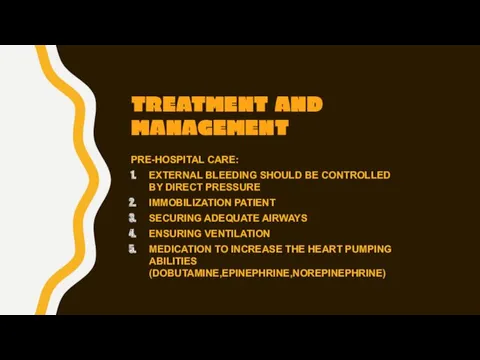
Слайд 14
TREATMENT AND MANAGEMENT
PRE-HOSPITAL CARE:
EXTERNAL BLEEDING SHOULD BE CONTROLLED BY DIRECT PRESSURE
IMMOBILIZATION PATIENT
SECURING ADEQUATE AIRWAYS
ENSURING VENTILATION
MEDICATION TO INCREASE THE HEART PUMPING ABILITIES (DOBUTAMINE,EPINEPHRINE,NOREPINEPHRINE)
 Презентация Мой класс- это мое отражение
Презентация Мой класс- это мое отражение Времена группы Continuous
Времена группы Continuous Произведения М.Ю. Лермонтова в творчестве М. Врубеля
Произведения М.Ю. Лермонтова в творчестве М. Врубеля Вейвлеты при анализе скважинных данных
Вейвлеты при анализе скважинных данных Отчет о создании развивающей среды.
Отчет о создании развивающей среды. Антуан де Сент-Экзюпери
Антуан де Сент-Экзюпери Автоматизация смешения светлых нефтепродуктов
Автоматизация смешения светлых нефтепродуктов Купола над белым безмолвием.
Купола над белым безмолвием. Искусство 16 века в Нидерландах и Германии. (Тема 7)
Искусство 16 века в Нидерландах и Германии. (Тема 7) Творческий проект здоровые зубы - всякому любы
Творческий проект здоровые зубы - всякому любы Будущий мужчина, или Как правильно воспитывать мальчика (консультация для родителей)
Будущий мужчина, или Как правильно воспитывать мальчика (консультация для родителей) Графический интерфейс операционных систем
Графический интерфейс операционных систем Игра Подбери одежду по сезону
Игра Подбери одежду по сезону Колокола в музыке
Колокола в музыке Тема 1. Место и роль вооруженных сил Российской Федерации в структуре государства
Тема 1. Место и роль вооруженных сил Российской Федерации в структуре государства Хищные звери
Хищные звери Лекция 5__
Лекция 5__ Скульпту́ра. Объект изображения в скульптуре
Скульпту́ра. Объект изображения в скульптуре Значение и употребление глаголов в речи
Значение и употребление глаголов в речи Асептика и антисептика
Асептика и антисептика ВКР: Проект мини-цеха производства колбасных изделий и полуфабрикатов мощностью 1,5 т/смену
ВКР: Проект мини-цеха производства колбасных изделий и полуфабрикатов мощностью 1,5 т/смену Оригами Сонобе
Оригами Сонобе Презентация по технологии Портрет в сырной рамке
Презентация по технологии Портрет в сырной рамке Москва во главе объединения русских земель
Москва во главе объединения русских земель Шаблон Россия
Шаблон Россия Разработка проекта наладки РТК на базе станка с ЧПУ на обработку детали Шестерня VIII оси 1к62-02-119
Разработка проекта наладки РТК на базе станка с ЧПУ на обработку детали Шестерня VIII оси 1к62-02-119 Мое портфолио Диск Диск
Мое портфолио Диск Диск 20002
20002