Содержание
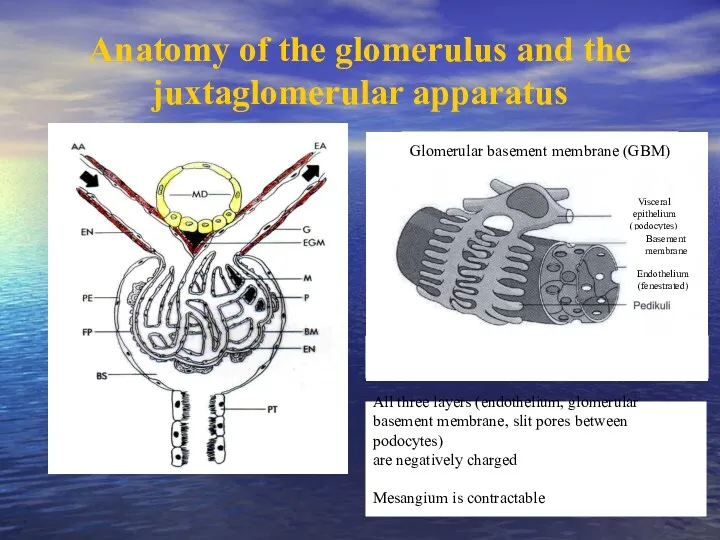
- 2. Anatomy of the glomerulus and the juxtaglomerular apparatus All three layers (endothelium, glomerular basement membrane, slit
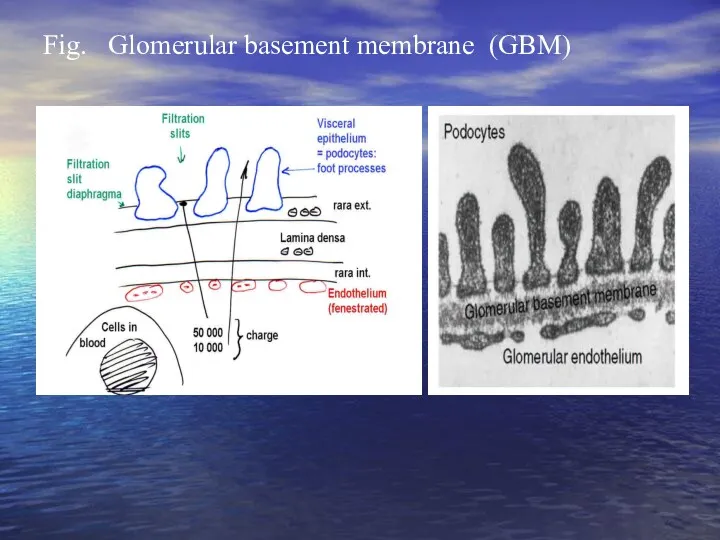
- 3. Fig. Glomerular basement membrane (GBM)
- 4. Glomerular diseases (glomerulopathy) heterogeneous group of diseases Dividing: Primary glomerulopathy Secondary glomerulopathy – can be manifestation
- 5. Immunopathologic mechanisms Damage of kidney depend on: mechanism and intensity of immune reaction collocation of antigens
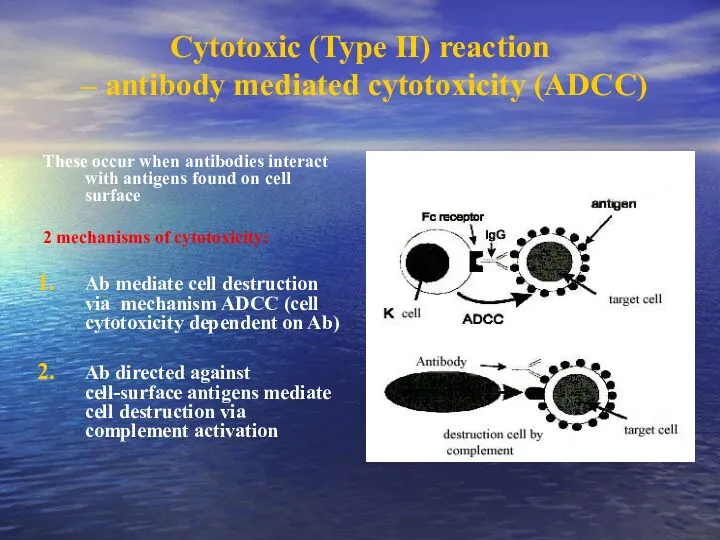
- 6. Cytotoxic (Type II) reaction – antibody mediated cytotoxicity (ADCC) These occur when antibodies interact with antigens
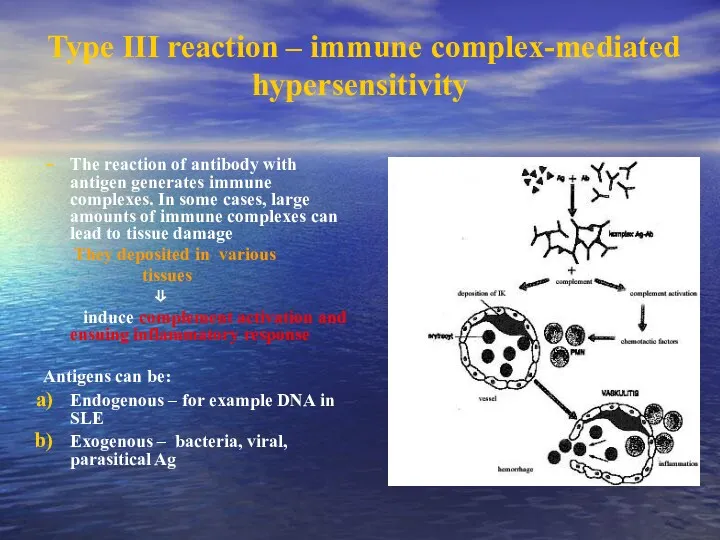
- 7. Type III reaction – immune complex-mediated hypersensitivity The reaction of antibody with antigen generates immune complexes.
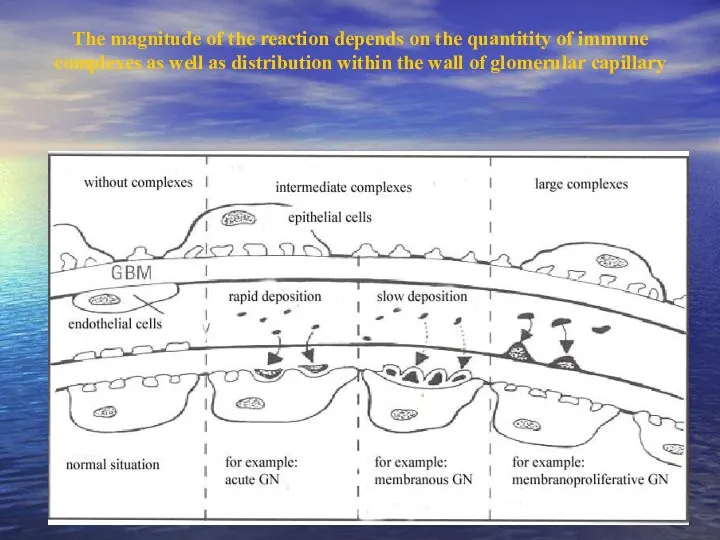
- 8. The magnitude of the reaction depends on the quantitity of immune complexes as well as distribution
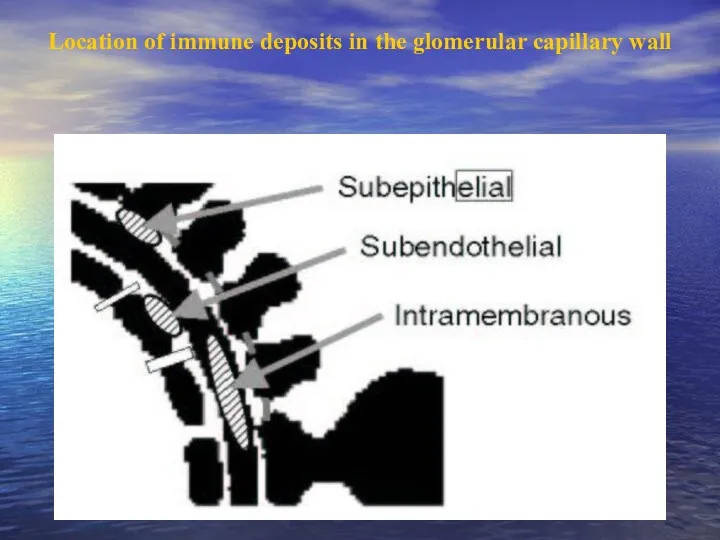
- 9. Location of immune deposits in the glomerular capillary wall
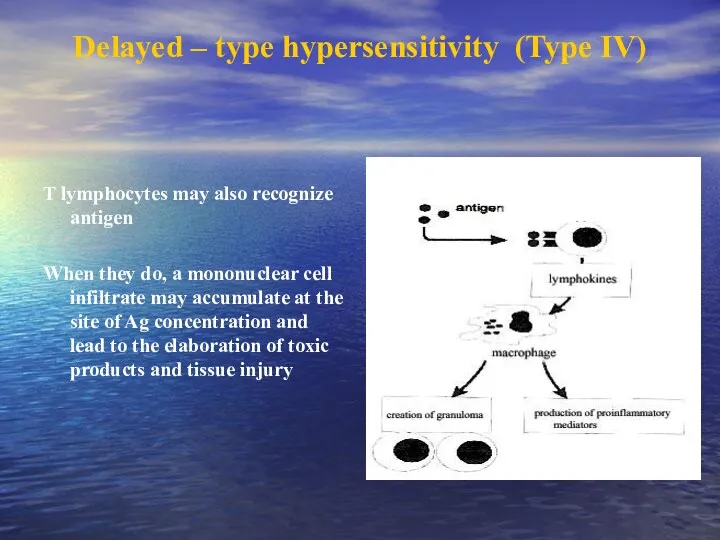
- 10. Delayed – type hypersensitivity (Type IV) T lymphocytes may also recognize antigen When they do, a
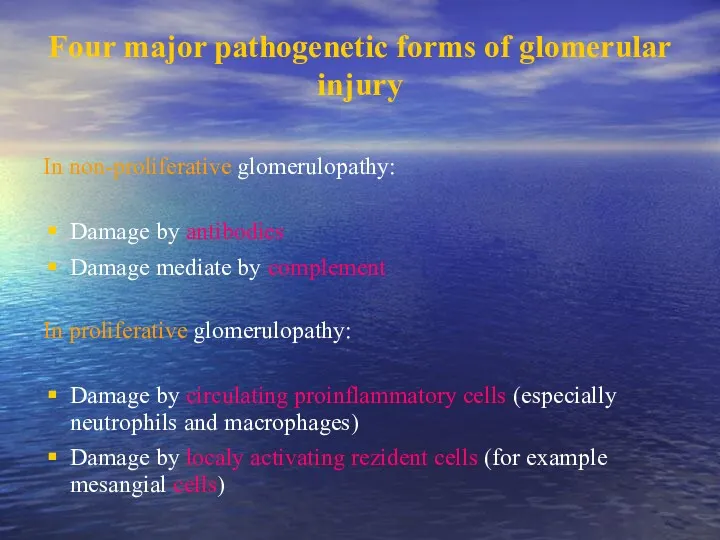
- 11. Four major pathogenetic forms of glomerular injury In non-proliferative glomerulopathy: Damage by antibodies Damage mediate by
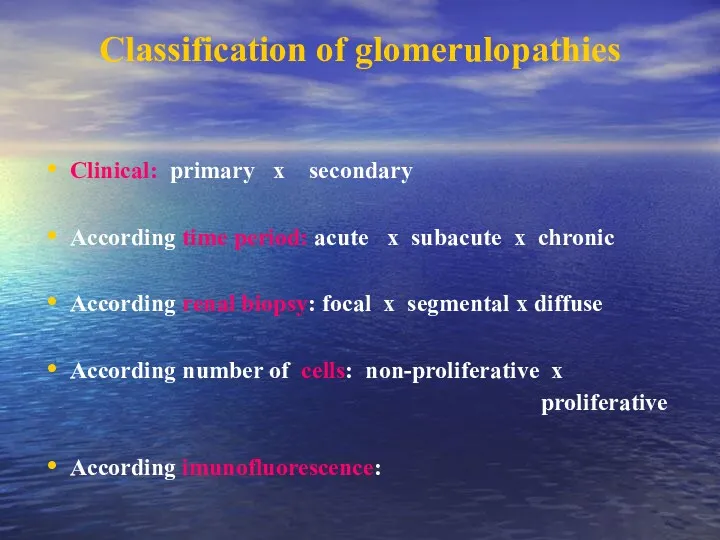
- 12. Classification of glomerulopathies Clinical: primary x secondary According time period: acute x subacute x chronic According
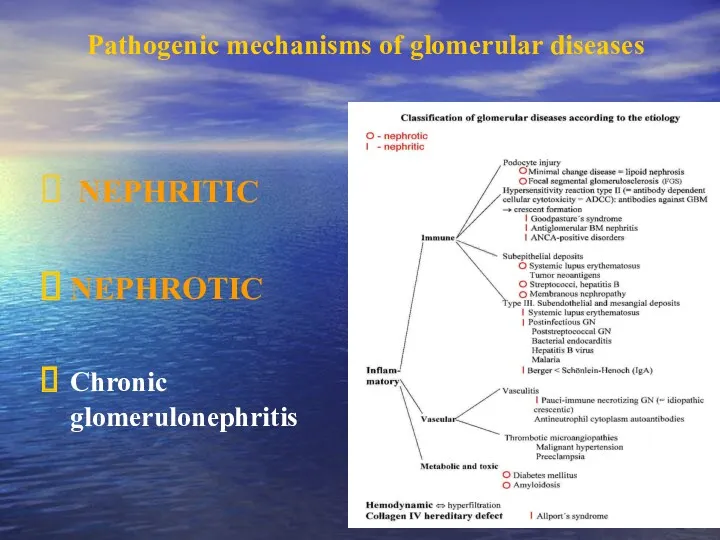
- 13. Pathogenic mechanisms of glomerular diseases NEPHRITIC NEPHROTIC Chronic glomerulonephritis
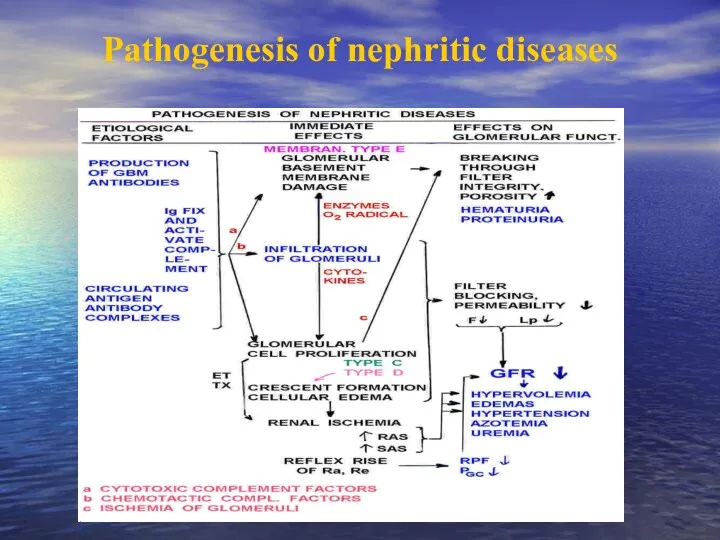
- 14. Pathogenesis of nephritic diseases
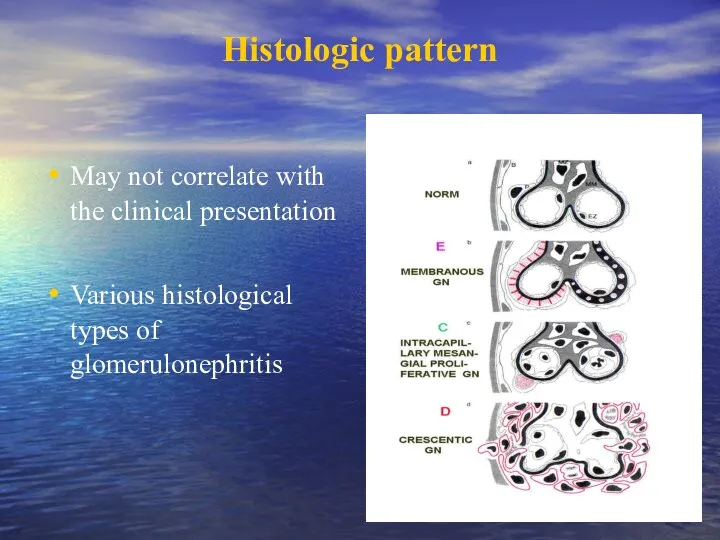
- 15. Histologic pattern May not correlate with the clinical presentation Various histological types of glomerulonephritis
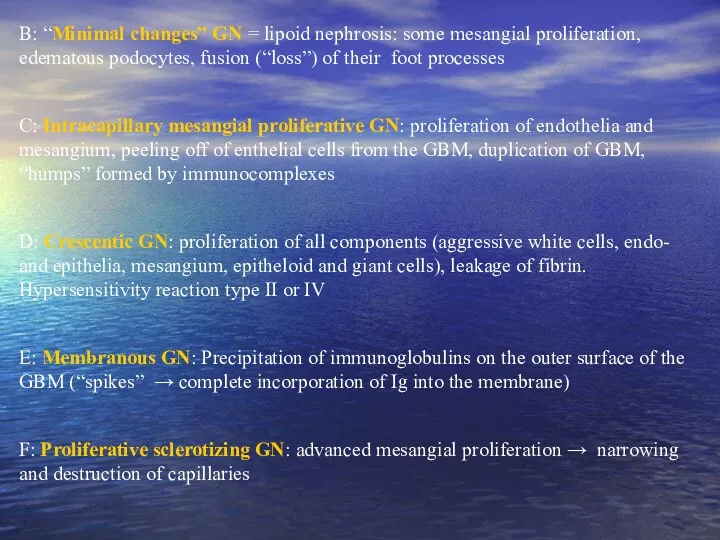
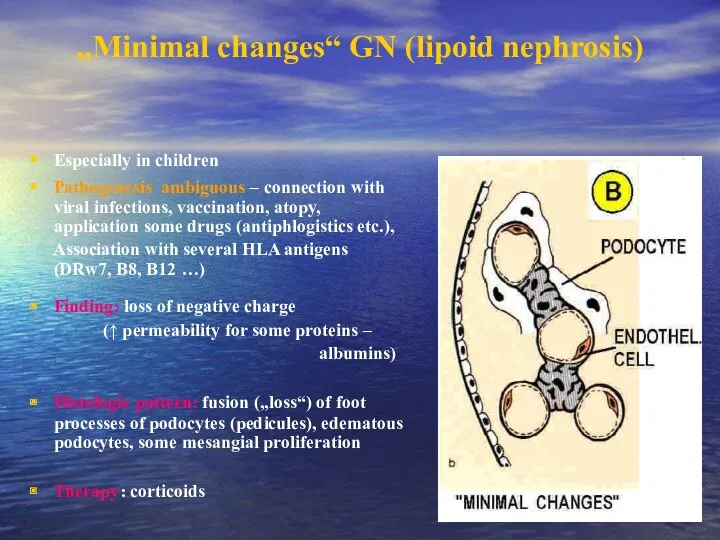
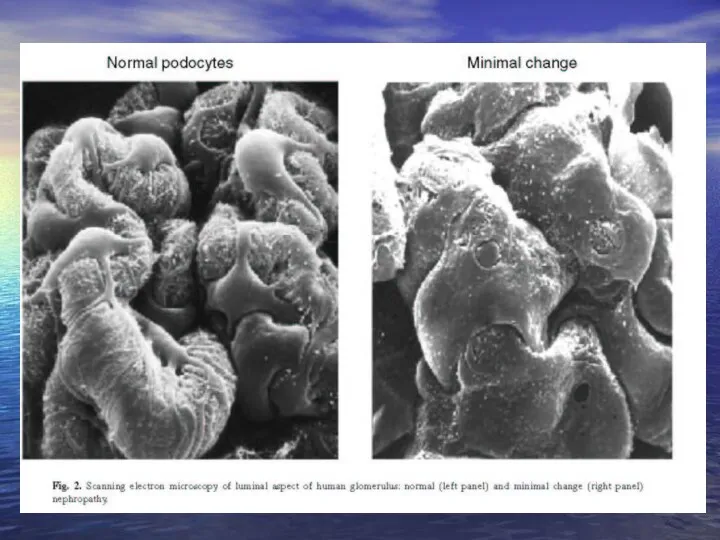
- 16. B: “Minimal changes” GN = lipoid nephrosis: some mesangial proliferation, edematous podocytes, fusion (“loss”) of their
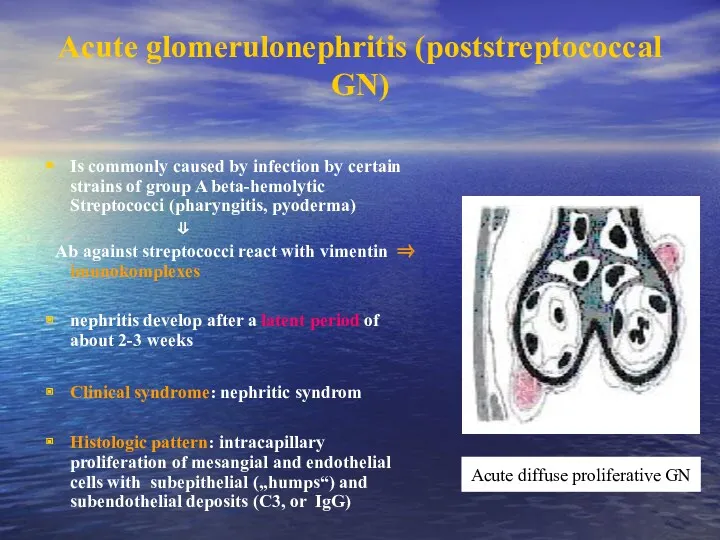
- 17. Acute glomerulonephritis (poststreptococcal GN) Is commonly caused by infection by certain strains of group A beta-hemolytic
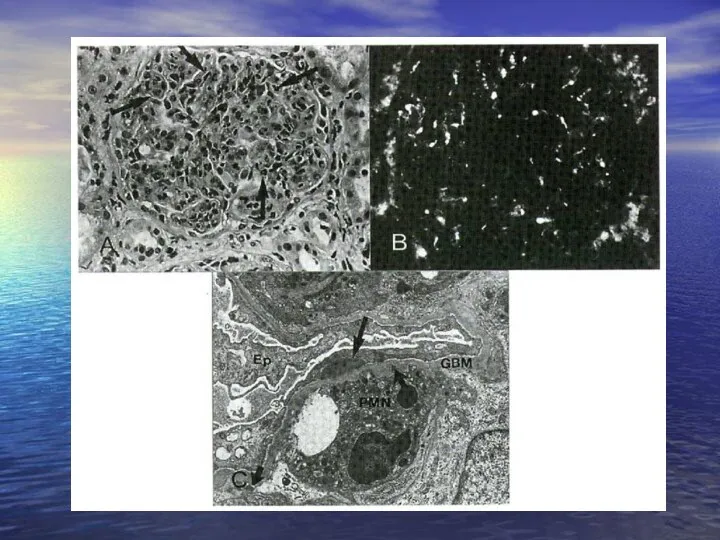
- 19. Postinfectional non-streptococcus glomerulonephritis Acute glomerulonephritis can develope also in the course of other infections: - stafylococci
- 20. Focal proliferative glomerulonephritis - different etiology: IgA nefropathy Nephritis in systemic lupus erythematodes (SLE) Nephritis in
- 21. Rapidly progressive glomerulonephritis (RPGN) Heterogeneous group of diseases, it is characterised by intense proliferation of glomerular/capsular
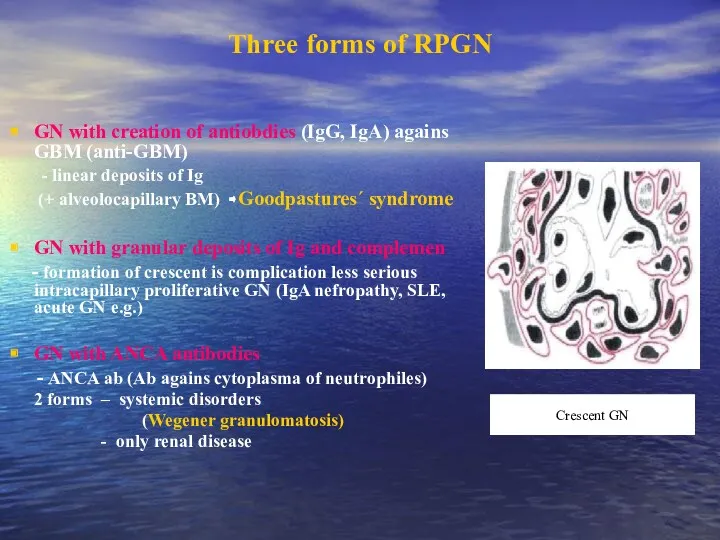
- 22. Three forms of RPGN GN with creation of antiobdies (IgG, IgA) agains GBM (anti-GBM) - linear
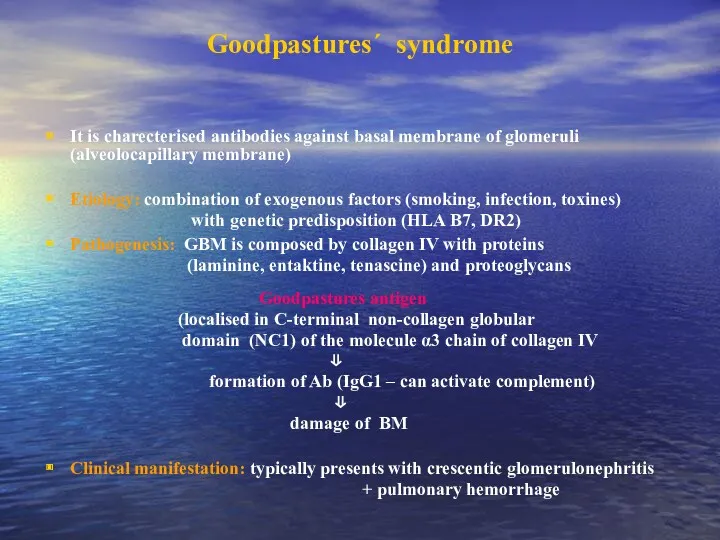
- 23. Goodpastures´ syndrome It is charecterised antibodies against basal membrane of glomeruli (alveolocapillary membrane) Etiology: combination of
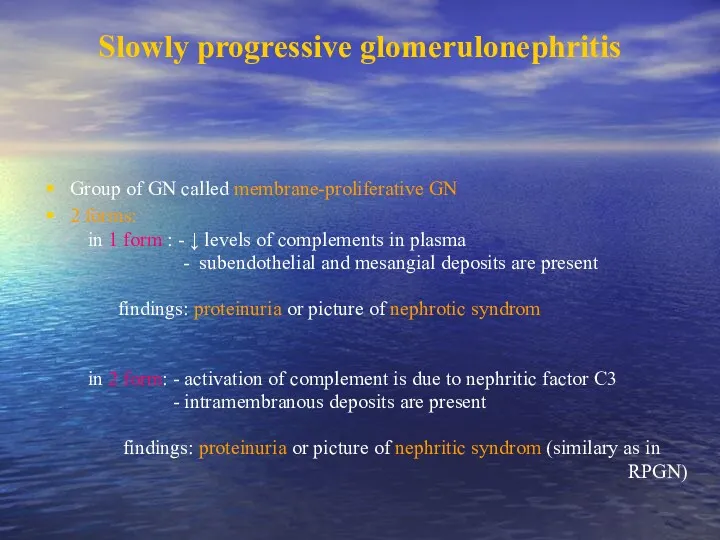
- 24. Slowly progressive glomerulonephritis Group of GN called membrane-proliferative GN 2 forms: in 1 form : -
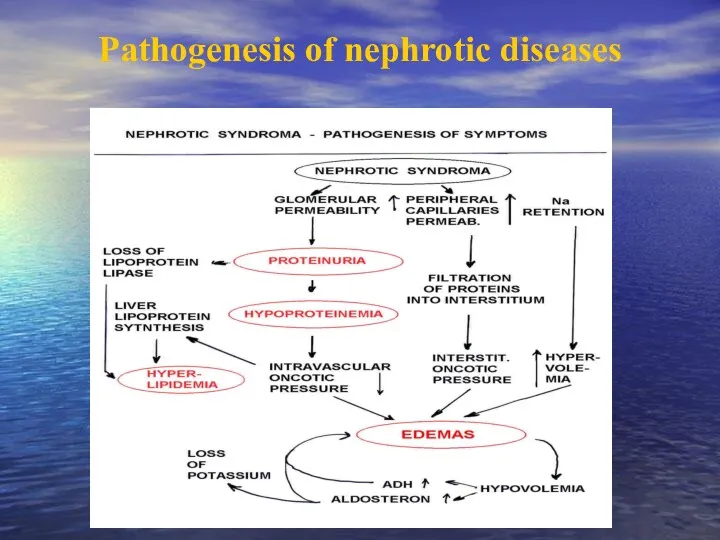
- 25. Pathogenesis of nephrotic diseases
- 26. „Minimal changes“ GN (lipoid nephrosis) Especially in children Pathogenesis ambiguous – connection with viral infections, vaccination,
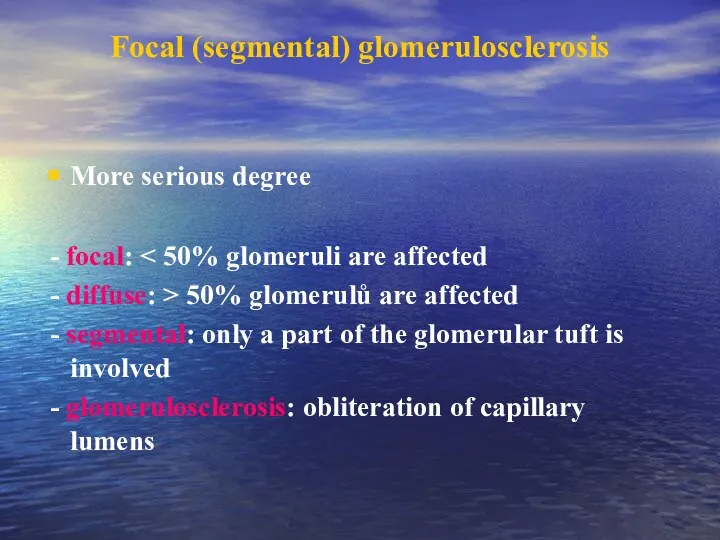
- 28. Focal (segmental) glomerulosclerosis More serious degree - focal: - diffuse: > 50% glomerulů are affected -
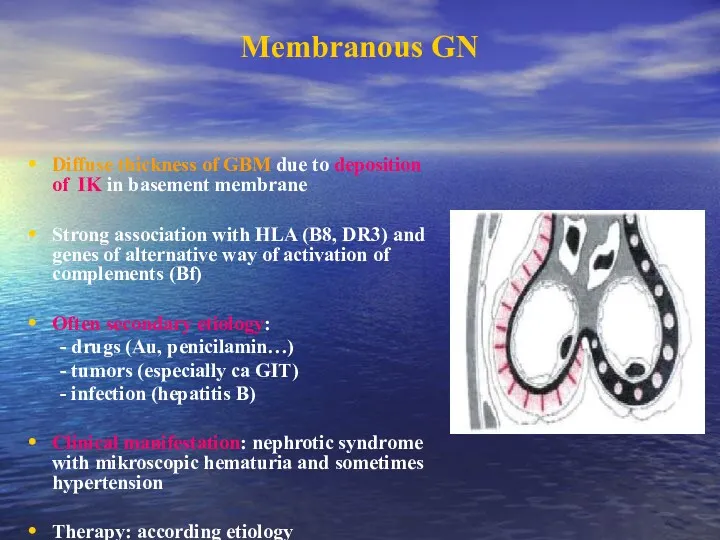
- 29. Membranous GN Diffuse thickness of GBM due to deposition of IK in basement membrane Strong association
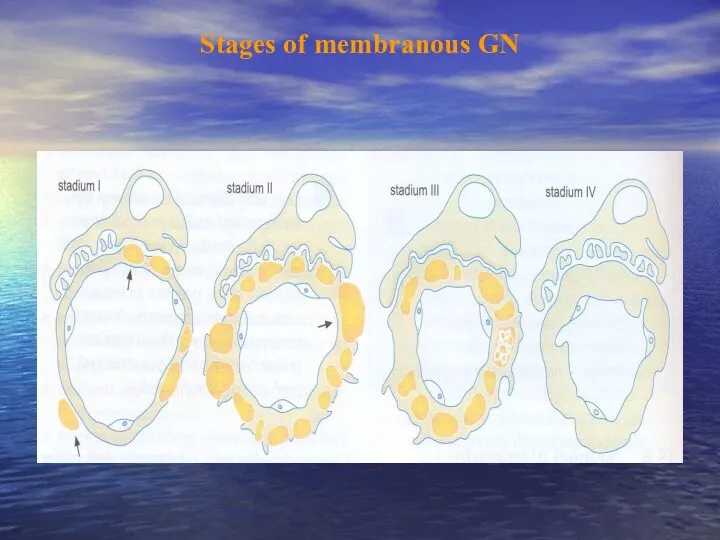
- 30. Stages of membranous GN
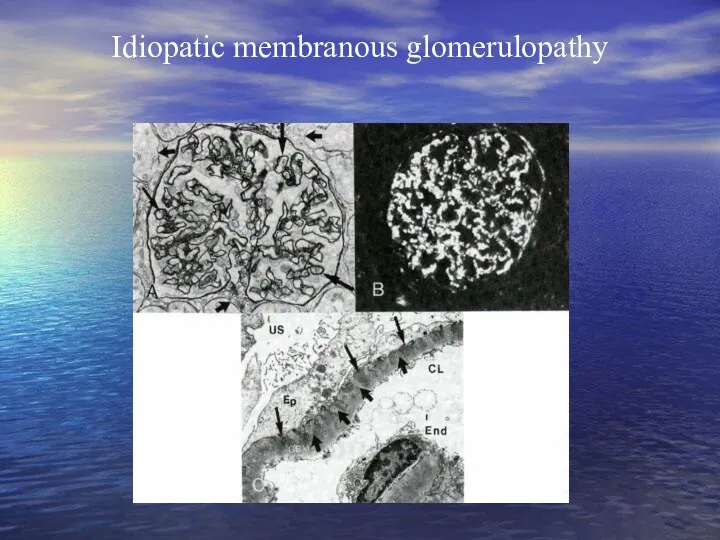
- 31. Idiopatic membranous glomerulopathy
- 32. Membranoproliferative (mesangiocapillary) glomerulopathy Is characterised by hypercellularity of the glomerular cells and basement membrane thickening 2
- 33. IgA nephropathy (Berger´s disease) Mesangioproliferative GN with deposits of IgA, event. C3 Etiology: - unknown, clinical
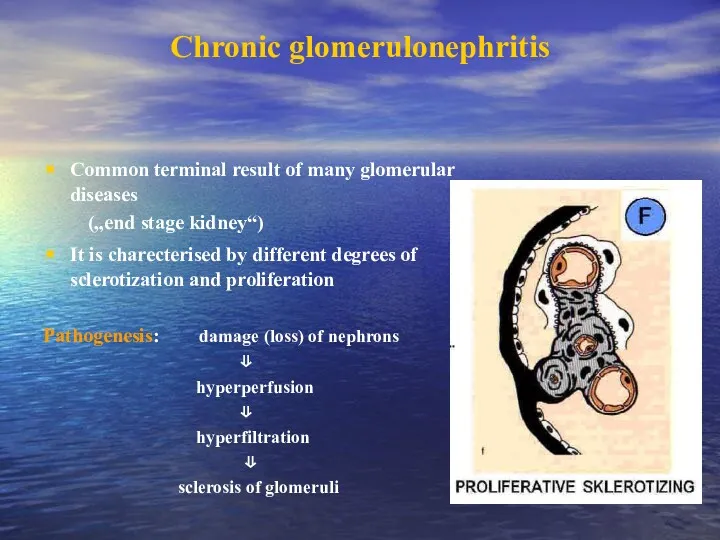
- 34. Chronic glomerulonephritis Common terminal result of many glomerular diseases („end stage kidney“) It is charecterised by
- 35. Glomerulopathy in connective tissue disorders SLE predominantly affects women, who account for 90% cases The age
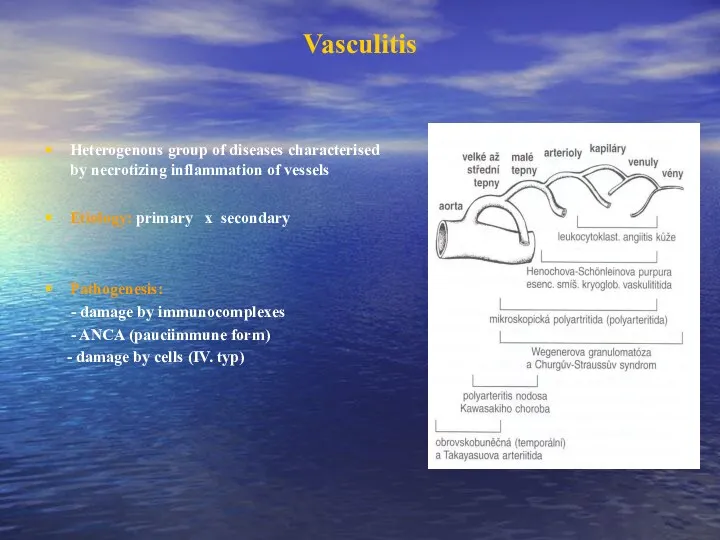
- 36. Vasculitis Heterogenous group of diseases characterised by necrotizing inflammation of vessels Etiology: primary x secondary Pathogenesis:
- 37. Henoch-Schönlein purpura systemic vasculitis affecting medium-sized vessels especially in children and younger people It is frequently
- 38. Polyarteritis nodosa is an inflammatory and necrotizing disease involving the medium-sized and small arteries throughout the
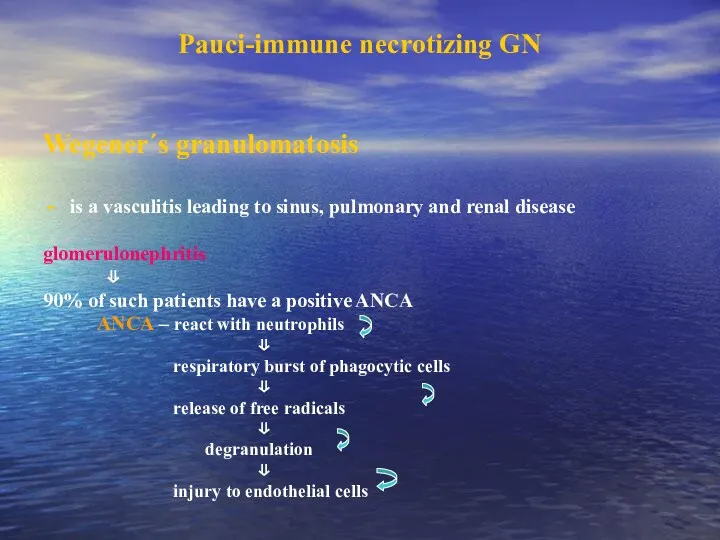
- 39. Pauci-immune necrotizing GN Wegener´s granulomatosis is a vasculitis leading to sinus, pulmonary and renal disease glomerulonephritis
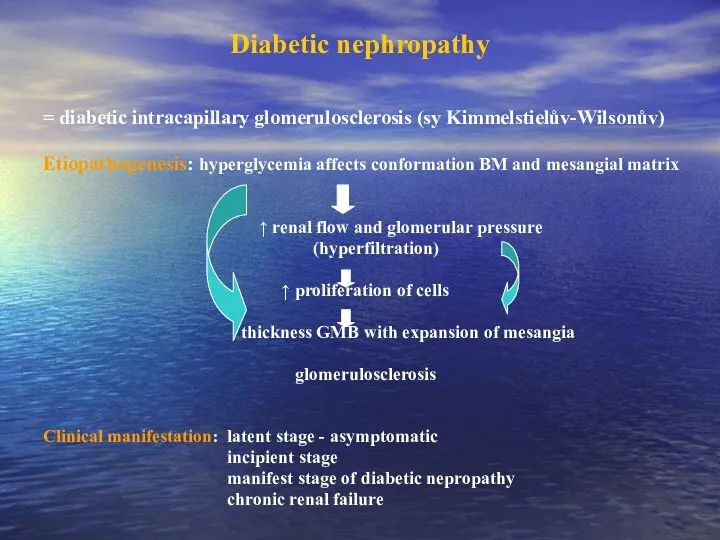
- 40. Diabetic nephropathy = diabetic intracapillary glomerulosclerosis (sy Kimmelstielův-Wilsonův) Etiopathogenesis: hyperglycemia affects conformation BM and mesangial matrix
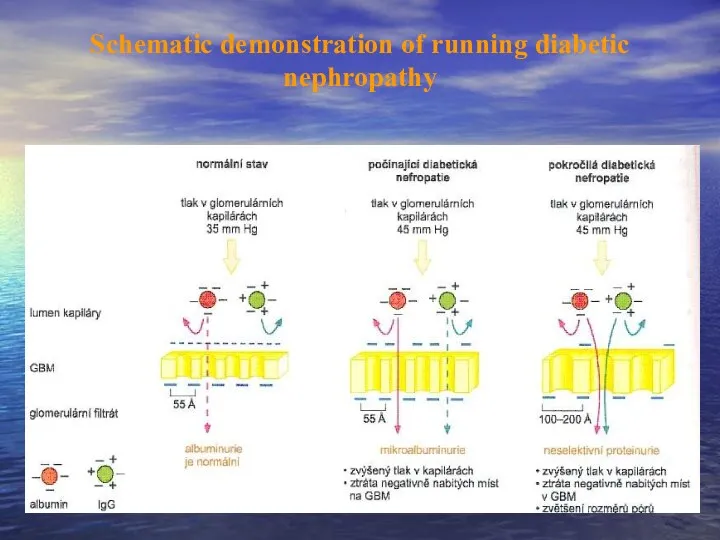
- 41. Schematic demonstration of running diabetic nephropathy
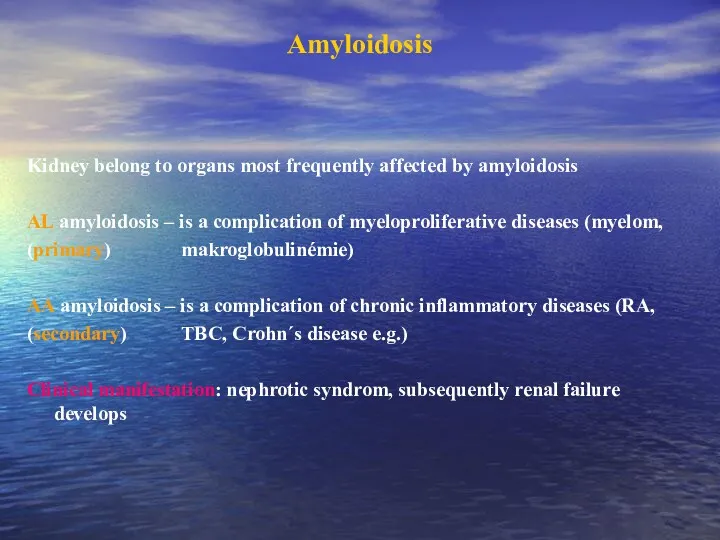
- 42. Amyloidosis Kidney belong to organs most frequently affected by amyloidosis AL amyloidosis – is a complication
- 44. Скачать презентацию

 Перикардиты. Анатомия перикарда
Перикардиты. Анатомия перикарда Спадкові захворювання нервової системи
Спадкові захворювання нервової системи ВИЧ: вопросы и ответы
ВИЧ: вопросы и ответы Нейтропении у детей
Нейтропении у детей Николай Иванович Пирогов Русский хирург и анатом
Николай Иванович Пирогов Русский хирург и анатом Информационные технологии для фармацевтов
Информационные технологии для фармацевтов Периоды детства
Периоды детства Антипсихотики (нейролептики)
Антипсихотики (нейролептики) Глобальные риски и новейшие медицинские технологии
Глобальные риски и новейшие медицинские технологии Компрессионные синдромы шейного отдела позвоночника
Компрессионные синдромы шейного отдела позвоночника Жанұямен қарым – қатынаста жеткен жетістіктерді және қиыншылықтарды талдау
Жанұямен қарым – қатынаста жеткен жетістіктерді және қиыншылықтарды талдау Інсульт. Причини, симптоми інсульту, перша допомога, поради
Інсульт. Причини, симптоми інсульту, перша допомога, поради Крон ауруы
Крон ауруы Pancreatic Cancer
Pancreatic Cancer Особенности фармакокинетики и фармакодинамики при лечении аллергий
Особенности фармакокинетики и фармакодинамики при лечении аллергий ИБС. Стенокардия
ИБС. Стенокардия Нәрестелердің асфиксиясы
Нәрестелердің асфиксиясы Опухолевый рост
Опухолевый рост Кілегейлі қабықтар мен мүшелерде эпителий тінінің мамандануы
Кілегейлі қабықтар мен мүшелерде эпителий тінінің мамандануы Нарушения сна у младенцев и детей раннего возраста
Нарушения сна у младенцев и детей раннего возраста Анастезия задних верхних и нижнего луночкого нерва по П.М. Егорову
Анастезия задних верхних и нижнего луночкого нерва по П.М. Егорову Токсикология фосфорорганических соединений (ФОС)
Токсикология фосфорорганических соединений (ФОС) Анатомо-фізіологічні особливості сечовидільної системи у дітей
Анатомо-фізіологічні особливості сечовидільної системи у дітей Өлім, өлім белгілері
Өлім, өлім белгілері Ми қыртысының анатомиялық-гистологиялық құрылымы
Ми қыртысының анатомиялық-гистологиялық құрылымы Воспалительные процессы органов женской половой системы специфической этиологии
Воспалительные процессы органов женской половой системы специфической этиологии Болезнь Крона
Болезнь Крона Respiratory system
Respiratory system