Содержание
- 2. The aim of treatment The aims of treating tuberculosis in adults are: to eliminate the clinical
- 3. The complex treatment of pulmonary tuberculosis patients includes: antimycobacterial therapy - pathogenetic treatment - colapsotherapy and
- 4. Principles of treatment of patient with tuberculosis 1. Complexity is combination of specific and non-specific, as
- 5. Principles of treatment of patient with tuberculosis 3. Biphasic treatment of tuberculosis. First intensive phase is
- 6. Principles of treatment of patient with tuberculosis 4. Individual treatment of patient with tuberculosis is based
- 7. Principles of treatment of patient with tuberculosis 5. Long-term and continued treatment, which should last for
- 8. Principles of treatment of patient with tuberculosis 7. Controlled chemotherapy means that all medication should be
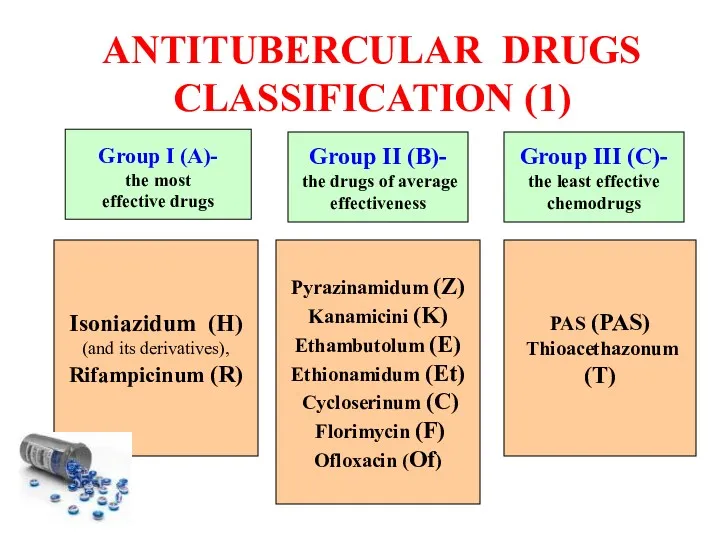
- 9. ANTITUBERCULAR DRUGS CLASSIFICATION (1) Isoniazidum (H) (and its derivatives), Rifampicinum (R) Pyrazinamidum (Z) Kanamicini (K) Ethambutolum
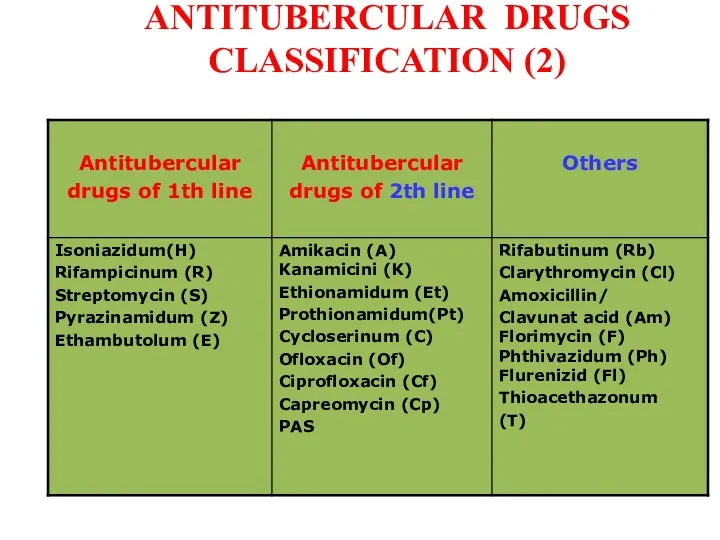
- 10. ANTITUBERCULAR DRUGS CLASSIFICATION (2)
- 11. ANTITUBERCULAR DRUGS CLASSIFICATION (3) Group 1: First-line oral agents • Pyrazinamide (Z) • Ethambutol (E) •
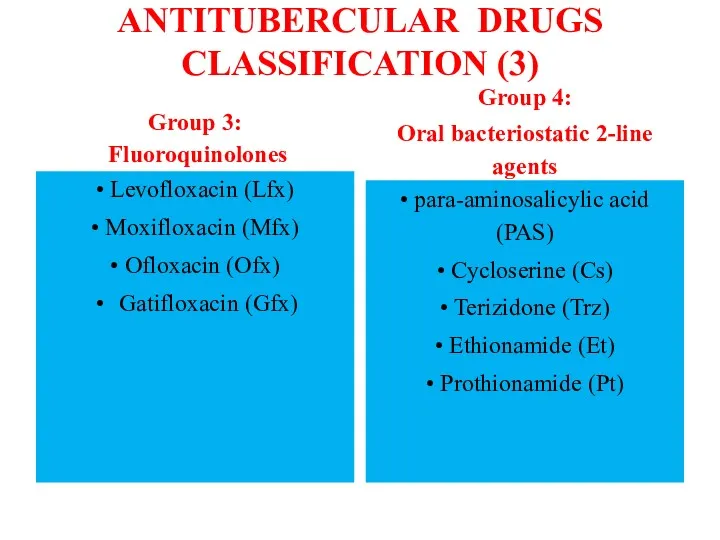
- 12. ANTITUBERCULAR DRUGS CLASSIFICATION (3) Group 3: Fluoroquinolones • Levofloxacin (Lfx) • Moxifloxacin (Mfx) • Ofloxacin (Ofx)
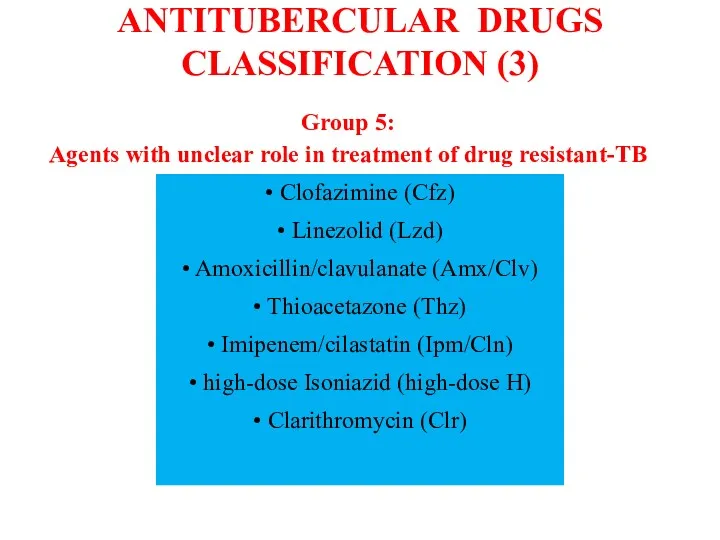
- 13. ANTITUBERCULAR DRUGS CLASSIFICATION (3) Group 5: Agents with unclear role in treatment of drug resistant-TB •
- 14. Isoniazid (H) H is a pro-drug that requires processing by the bacterial catalase-peroxidase to become active.
- 15. Isoniazid (H) Pharmacokinetics H is readily absorbed from the gastrointestinal tract or following intramuscular injections. Peak
- 16. Isoniazid (H) Toxicity H is well tolerated at recommended doses, although slow acetylators can accumulate higher
- 17. Rifampicin (R) Structure and general properties R inhibits gene transcription, by interacting with the beta subunit
- 18. Rifampicin (R) Pharmacokinetics This drug is readily absorbed from the gastrointestinal tract (food may delay or
- 19. Rifampicin (R) Toxicity R is well tolerated, although adverse effects may arise during intermittent therapy or
- 20. Ethambutol (E) E is only active against dividing mycobacteria, being bacteriostatic. Since E affects the biosynthesis
- 21. Ethambutol (E) Pharmacokinetics E is given orally, as it is well absorbed in the gastrointestinal tract
- 22. Ethambutol (E) Toxicity E produces retrobulbar neuritis with a reduction in visual acuity, constriction of visual
- 23. Pyrazinamide (Z) Z is a bactericidal drug active only against M. tuberculosis, having no in vitro
- 24. Pyrazinamide (Z) Pharmacokinetics Z is given orally and is readily absorbed from the gastrointestinal tract. Serum
- 25. Pyrazinamide (Z) Toxicity Z is hepatotoxic in a dose-dependent manner. Following a daily dose of 3
- 26. Streptomycin (S) Structure and general properties S, an antibiotic produced by some strains of Streptomyces griseous,
- 27. Streptomycin (S) Pharmacokinetics S, like most aminoglycosides, is poorly absorbed from the gastrointestinal tract, and therefore
- 28. Streptomycin (S) Toxicity Like most aminoglycosides, S has ototoxic effects affecting vestibular rather than auditory (cochlear)
- 29. Other drugs against tuberculosis Drugs in this group are interesting for one or more of the
- 30. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 31. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 32. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 33. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 34. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 35. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 36. WHO definitions of TB cases recommended for use since March 2013 and that were used in
- 37. WHO definitions of TB cases recommended for use since March 2013 and that were used in
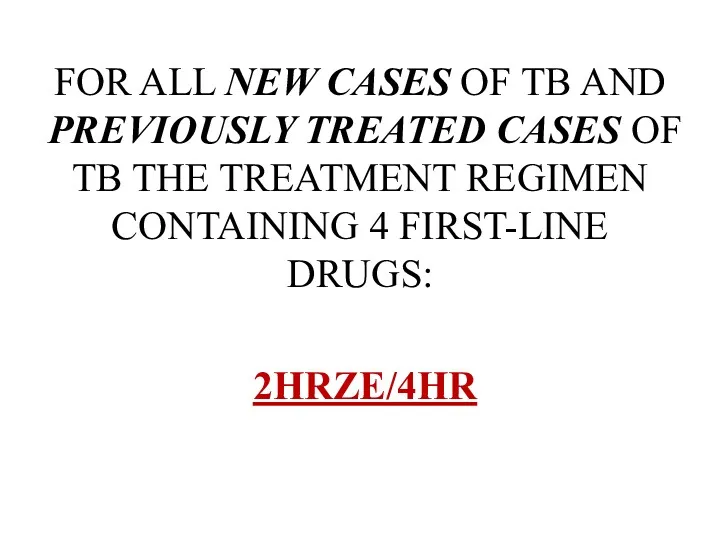
- 38. FOR ALL NEW CASES OF TB AND PREVIOUSLY TREATED CASES OF TB THE TREATMENT REGIMEN CONTAINING
- 39. Treatment of mono- or poly-resistant non-multidrug-resistant tuberculosis These patients are relatively easy to treat and cure
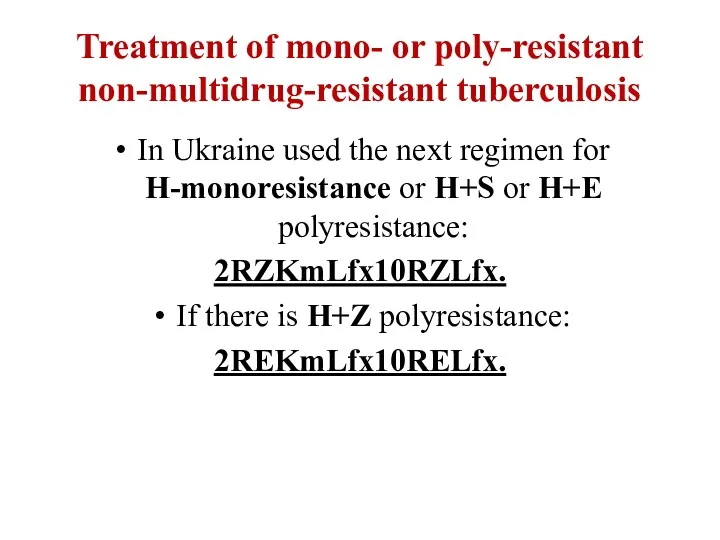
- 40. Treatment of mono- or poly-resistant non-multidrug-resistant tuberculosis In Ukraine used the next regimen for H-monoresistance or
- 41. Treatment of mono- or poly-resistant non-multidrug-resistant tuberculosis A completely different situation exists in patients with R
- 42. COMMON DRUG SIDE EFFECTS
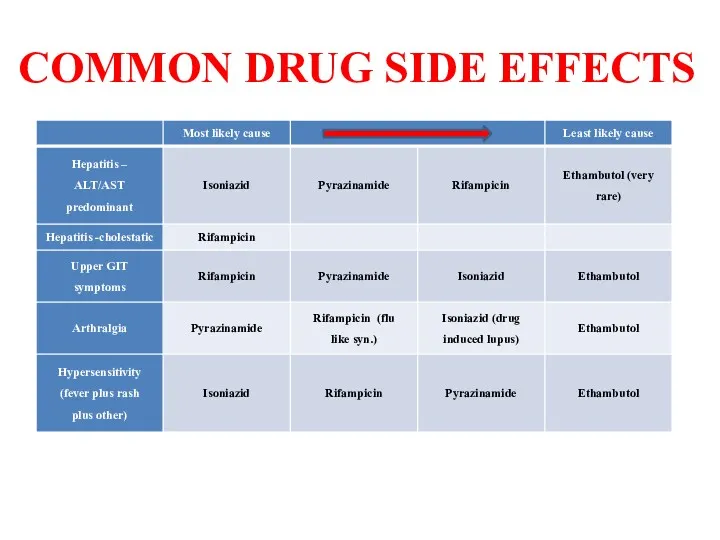
- 43. MANAGEMENT OF SIDE EFFECTS Management of cutaneous reactions If a patient develops itching without a rash
- 44. MANAGEMENT OF SIDE EFFECTS Management of drug-induced hepatitis If it is thought that the liver disease
- 45. MANAGEMENT OF SIDE EFFECTS Management of drug-induced hepatitis Once drug-induced hepatitis has resolved, the drugs are
- 46. MANAGEMENT OF SIDE EFFECTS Management of drug-induced hepatitis Alternative regimens depend on which drug is implicated
- 47. TREATMENT OF EXTRAPULMONARY TUBERCULOSIS Bone and joint TB Standard course therapy (5EHRZ, 4 HR) is sufficient
- 48. SURGICAL TREATMENT Absolute indications for surgery in TB treatment: – a high probability of failure of
- 49. SURGICAL TREATMENT Emergency indications (that is, without surgery death is imminent and unavoidable) include: – profuse
- 50. SURGICAL TREATMENT Urgent indications include: – irreversible TB progression, despite adequate anti-TB chemotherapy – recurrent haemoptysis
- 51. SURGICAL TREATMENT the majority of authors define the elective indications listed here: – localized forms of
- 52. Surgery should be seriously considered when: the disease is sufficiently localized to allow surgery; the remaining
- 53. Types of operations 1. lung resections of different size wedge resection segmentectomy lobectomy and bilobectomy combined
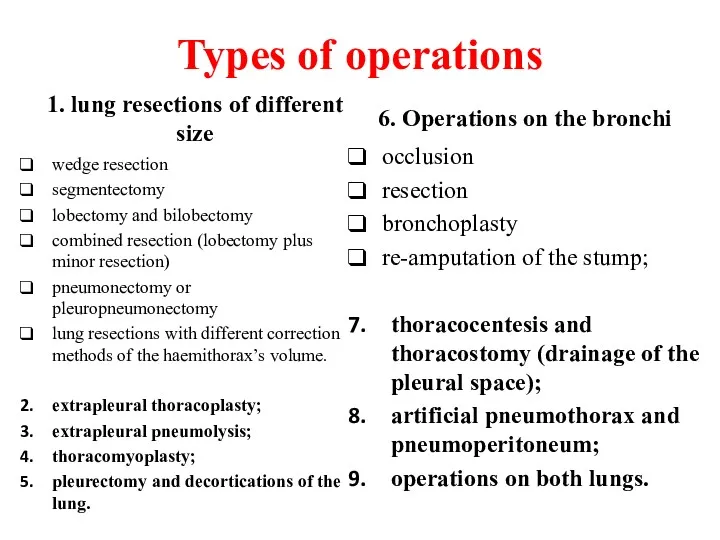
- 54. PATHOGENETIC TREATMENT OF TUBERCULOSIS It is aimed at solving the following tasks: Decreasing exudative pneumonic phenomena
- 55. PATHOGENETIC TREATMENT OF TUBERCULOSIS The following methods of rational therapy are applied to realize these tasks:
- 56. PATHOGENETIC TREATMENT OF TUBERCULOSIS The following methods of rational therapy are applied to realize these tasks:
- 57. PATHOGENETIC TREATMENT OF TUBERCULOSIS Laser Therapy This has also been tried as an adjunct to chemotherapy
- 58. PATHOGENETIC TREATMENT OF TUBERCULOSIS Gene Therapy The decoding of the human genome provides another fascinating aspect
- 59. PATHOGENETIC TREATMENT OF TUBERCULOSIS Role of Steroids The adjuvant use of corticosteroids in DR-TB patients has
- 60. PATHOGENETIC TREATMENT OF TUBERCULOSIS Other drugs Inhibitors of proteolytic enzymes (Contrical 10000 in 200ml of the
- 61. PATHOGENETIC TREATMENT OF TUBERCULOSIS Other drugs The tracheobronchial tree sanation occupies one of the most prominent
- 62. Criteria of effectiveness in the treatment of tuberculosis patients are: 1) the disappearance of clinical and
- 64. Скачать презентацию


 Грипп и другие ОРВИ. Ангины, дифференциальная диагностика, лечение, профилактика
Грипп и другие ОРВИ. Ангины, дифференциальная диагностика, лечение, профилактика Вакцинация
Вакцинация Соединительнотканные дисплазии сердца. Этиология. Патогенез. Клинико-диагностические и дифференциально-диагностические критерии
Соединительнотканные дисплазии сердца. Этиология. Патогенез. Клинико-диагностические и дифференциально-диагностические критерии Центр ФГБУ Федеральный центр сердечно-сосудистой хирургии (г.Пенза)
Центр ФГБУ Федеральный центр сердечно-сосудистой хирургии (г.Пенза) Эпилепсия. Определение
Эпилепсия. Определение Принцип ЭКГ
Принцип ЭКГ Влияние питания на здоровій рост и развитие ребенка
Влияние питания на здоровій рост и развитие ребенка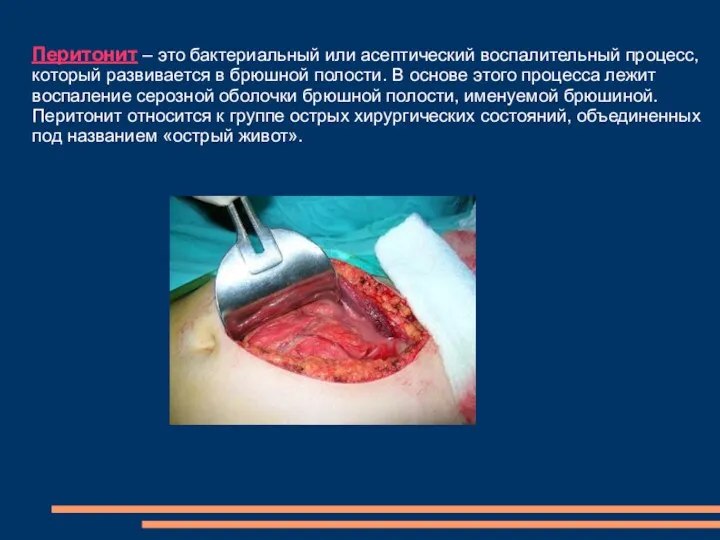 Перитонит. Причины бактериальных перитонитов
Перитонит. Причины бактериальных перитонитов Гострі екзогенні отруєння
Гострі екзогенні отруєння Жіночий таз. Плід як об'єкт родів. Акушерська термінологія
Жіночий таз. Плід як об'єкт родів. Акушерська термінологія Врожденный и приобретенный иммунитет. Клеточные и гуморальные механизмы
Врожденный и приобретенный иммунитет. Клеточные и гуморальные механизмы Антикоагулянтная терапия у больных ишемическим инсультом
Антикоагулянтная терапия у больных ишемическим инсультом Роль медицинского персонала в уходе за детьми
Роль медицинского персонала в уходе за детьми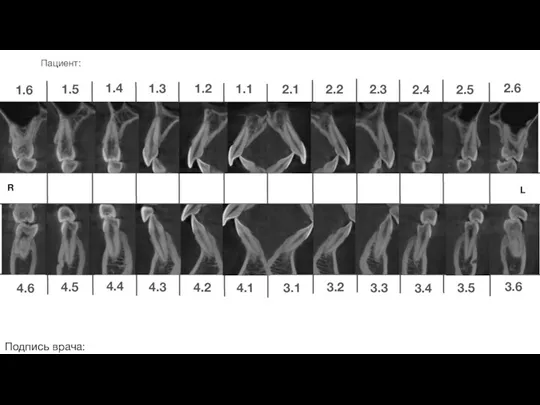 Ортодонтическое лечение. Стоматология
Ортодонтическое лечение. Стоматология Требования по заполнению направления на медико-социальную экспертизу
Требования по заполнению направления на медико-социальную экспертизу Жақ-бет аймағы жарақаттанған науқастарға көмек көрсету
Жақ-бет аймағы жарақаттанған науқастарға көмек көрсету Pulmonary tuberculosis. Passive Voice. Past and Present Tenses
Pulmonary tuberculosis. Passive Voice. Past and Present Tenses Отруйність спиртів та їх згубна дія на організм людини
Отруйність спиртів та їх згубна дія на організм людини Период молочных зубов
Период молочных зубов Иммунитет. Лекция №2
Иммунитет. Лекция №2 Высшие мозговые функции и их нарушения. Гнозис и праксис
Высшие мозговые функции и их нарушения. Гнозис и праксис Adult Nursing Care I
Adult Nursing Care I Эволюция представлений о сепсисе. Сепсис-3. Современная концепция патогенеза сепсиса
Эволюция представлений о сепсисе. Сепсис-3. Современная концепция патогенеза сепсиса Метод лактаційної аменореї
Метод лактаційної аменореї Удаление дивертикула Меккеля. Болезнь Гиршпрунга
Удаление дивертикула Меккеля. Болезнь Гиршпрунга Желтуха новорожденных
Желтуха новорожденных Заманауи карпулалық анестетиктер. Түрлері. Клинико-фармакологиялық мінездемесі
Заманауи карпулалық анестетиктер. Түрлері. Клинико-фармакологиялық мінездемесі Общие принципы интенсивной терапии острой дыхательной недостаточности Показания к ИВЛ
Общие принципы интенсивной терапии острой дыхательной недостаточности Показания к ИВЛ