Содержание
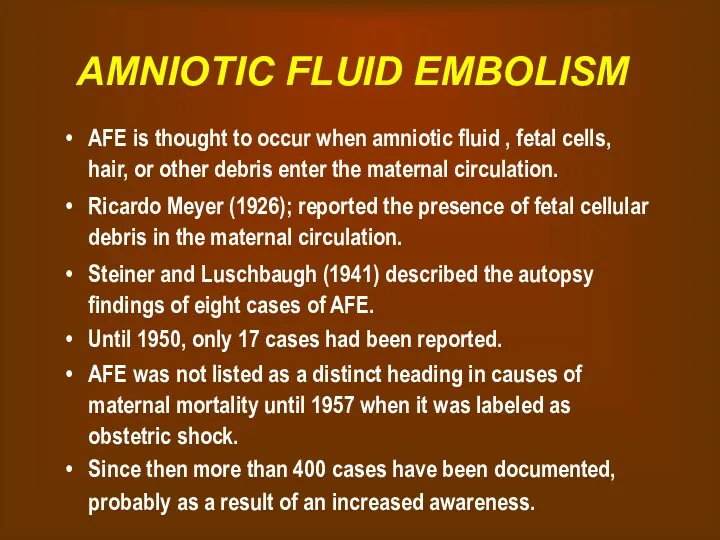
- 2. AMNIOTIC FLUID EMBOLISM AFE is thought to occur when amniotic fluid , fetal cells, hair, or
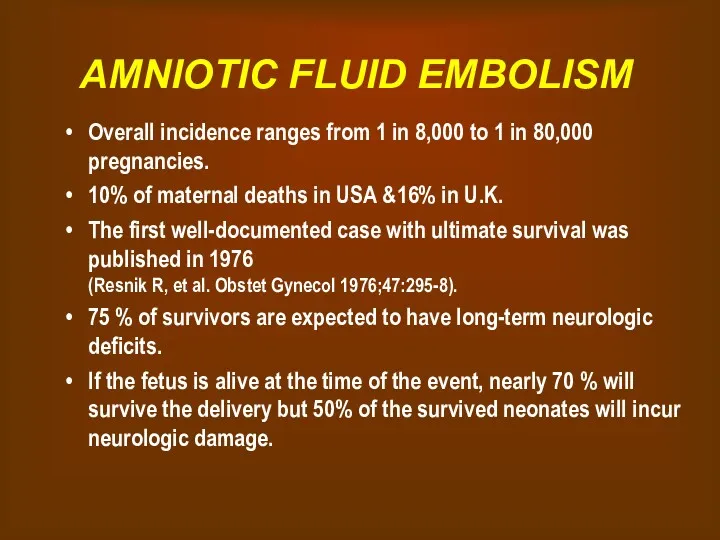
- 3. AMNIOTIC FLUID EMBOLISM Overall incidence ranges from 1 in 8,000 to 1 in 80,000 pregnancies. 10%
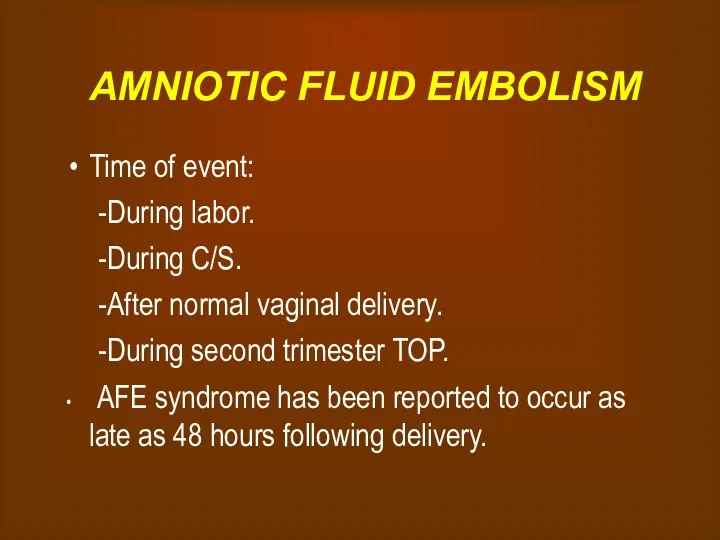
- 4. AMNIOTIC FLUID EMBOLISM Time of event: During labor. During C/S. After normal vaginal delivery. During second
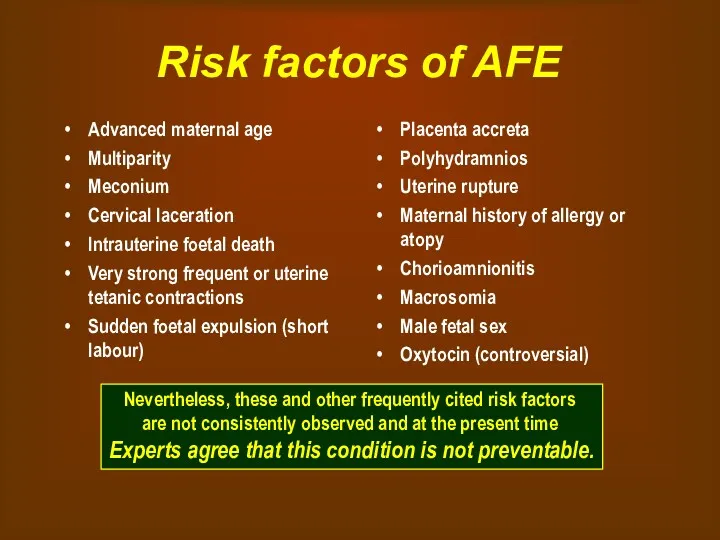
- 5. Risk factors of AFE Advanced maternal age Multiparity Meconium Cervical laceration Intrauterine foetal death Very strong
- 6. Experimental AFE The cardiorespiratory effects of acute intravascular injection of amniotic fluid have been studied in
- 7. Experimental AFE Intravascular injection of amniotic fluid in rhesus monkeys failed to produce cardiovascular changes similar
- 8. Pathophysiology - Poorly understood. - Cotton (1996), has proposed a biphasic model. Phase 1: Amniotic fluid
- 9. Pathophysiology The similar homodynamic derangements seen with AFE syndrome , anaphylactic, and septic shock have led
- 10. Pathophysiology Measurement of tryptase ( a degranulation product of mast cells released with histamine during anaphylactic
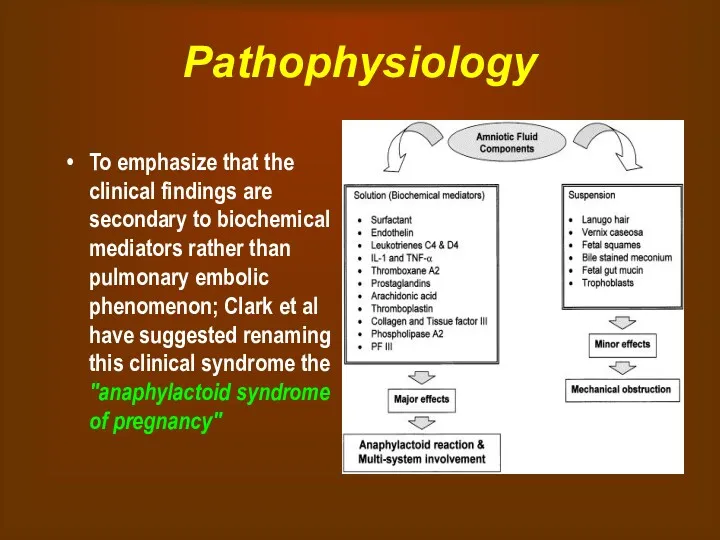
- 11. Pathophysiology To emphasize that the clinical findings are secondary to biochemical mediators rather than pulmonary embolic
- 12. Clinical presentation The classic clinical presentation of the syndrome has been described by five signs that
- 13. Clinical presentation A sudden drop in O2 saturation can be the initial indication of AFE during
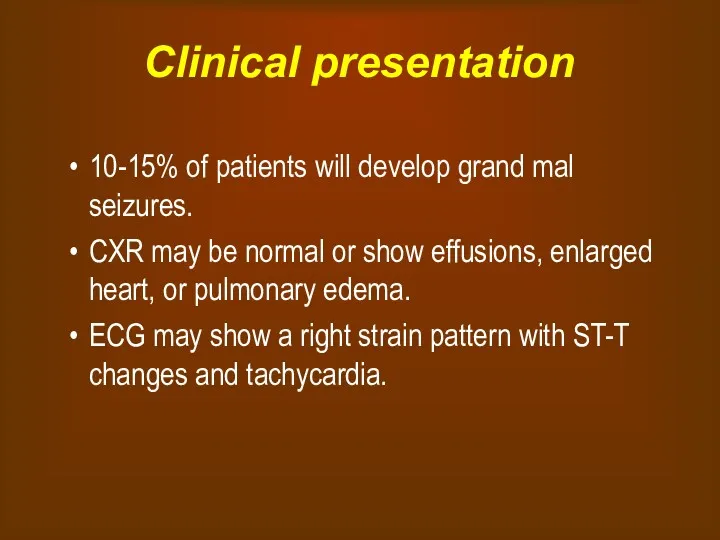
- 14. Clinical presentation 10-15% of patients will develop grand mal seizures. CXR may be normal or show
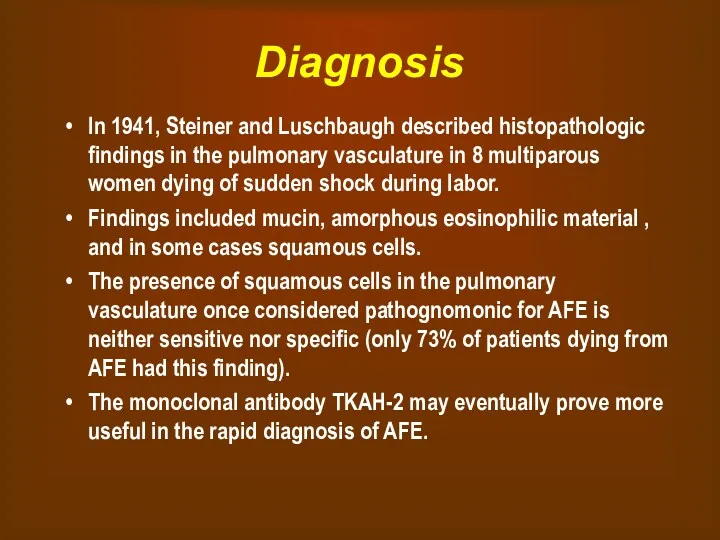
- 15. Diagnosis In 1941, Steiner and Luschbaugh described histopathologic findings in the pulmonary vasculature in 8 multiparous
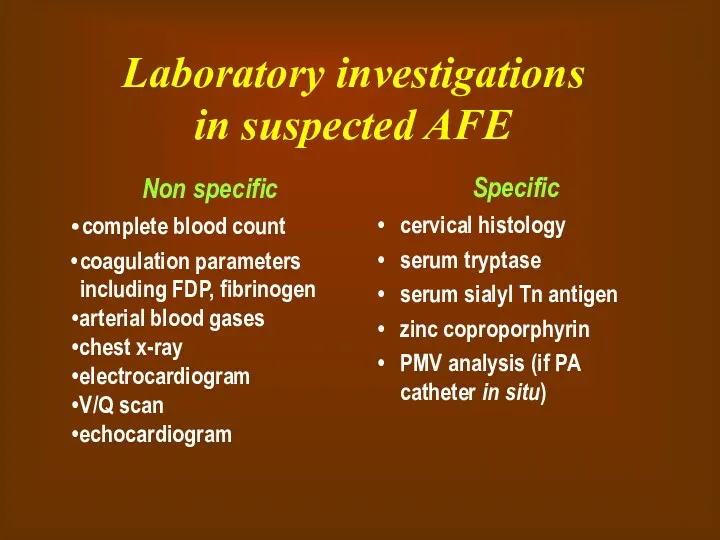
- 16. Laboratory investigations in suspected AFE Non specific complete blood count coagulation parameters including FDP, fibrinogen arterial
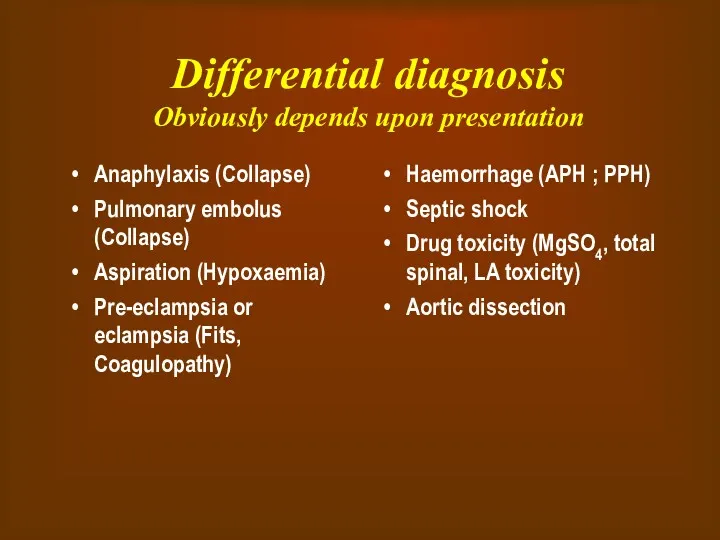
- 17. Differential diagnosis Obviously depends upon presentation Anaphylaxis (Collapse) Pulmonary embolus (Collapse) Aspiration (Hypoxaemia) Pre-eclampsia or eclampsia
- 18. Management of AFE GOALS OF MANAGEMENT: Restoration of cardiovascular and pulmonary equilibrium Maintain systolic blood pressure
- 19. Management of AFE As intubation and CPR may be required it is necessary to have easy
- 20. Management of AFE Treat hypotension, increase the circulating volume and cardiac output with crystalloids. After correction
- 21. Management of AFE In the ICU To assess the effectiveness of treatment and resuscitation, it is
- 22. Management of AFE In the ICU Central venous pressure monitoring is important to diagnose right ventricular
- 23. Management of AFE Coagulopathy DIC results in the depletion of fibrinogen, platelets, and coagulation factors, especially
- 24. Restoration of uterine tone Uterine atony is best treated with massage, uterine packing, and oxytocin or
- 25. Sympathomimetic Vasopressor agent Dopamine Dopamine increases myocardial contractility and systolic BP with little increase in diastolic
- 26. Maternal Mortality in AFE Maternal death usually occurs in one of three ways: (1) sudden cardiac
- 27. Further issues in the Management Transfer: Transfer to a level 3 hospital may be required once
- 28. Medical/Legal Pitfalls Failure to respond emergently is a pitfall. AFE is a clinical diagnosis. Steps must
- 29. SUMMARY AFE is a sudden and unexpected rare but life threatining complication of pregnancy. It has
- 31. Скачать презентацию
 Державна санітарно-епідеміологічна експертиза, як елемент соціально-гігієнічного моніторингу. Основні положення та організація
Державна санітарно-епідеміологічна експертиза, як елемент соціально-гігієнічного моніторингу. Основні положення та організація Операции на органах шеи
Операции на органах шеи Физиология паращитовидных желёз
Физиология паращитовидных желёз Повреждения и заболевания мочеполовых органов
Повреждения и заболевания мочеполовых органов Хирург Н.Н. Бурденко
Хирург Н.Н. Бурденко Арбовирусты инфекциялар. Кенелік энцефалит вирусы
Арбовирусты инфекциялар. Кенелік энцефалит вирусы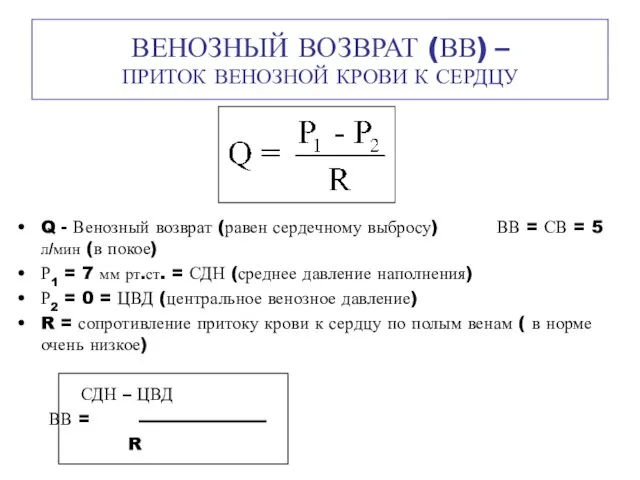 Венозный возврат (ВВ) – приток венозной крови к сердцу
Венозный возврат (ВВ) – приток венозной крови к сердцу Шум и вибрация
Шум и вибрация Алкогольный цирроз
Алкогольный цирроз Возрастные особенности системы крови и иммунитета
Возрастные особенности системы крови и иммунитета Неврозы
Неврозы Противоаритмические лекарственные средства
Противоаритмические лекарственные средства Здоровье на работе. Что должен знать о ВИЧ/СПИДе каждый?
Здоровье на работе. Что должен знать о ВИЧ/СПИДе каждый? Гигиена аптечных заведений
Гигиена аптечных заведений Гиперчувствительность. Иммунодефициты. Аутоиммунные процессы
Гиперчувствительность. Иммунодефициты. Аутоиммунные процессы Послеродовые депрессии
Послеродовые депрессии Аллергия. Стоматология
Аллергия. Стоматология 84-я Всероссийская научная конференция студентов и молодых ученых. Отчет. Секция: Общая хирургия
84-я Всероссийская научная конференция студентов и молодых ученых. Отчет. Секция: Общая хирургия Клинико-экономические исследования
Клинико-экономические исследования Химиотерапевтические лекарственные препараты, макролиды и азалиды
Химиотерапевтические лекарственные препараты, макролиды и азалиды Пороки сердца
Пороки сердца Асқорыту жолдарының қатерлі және қатерсіз ісіктері
Асқорыту жолдарының қатерлі және қатерсіз ісіктері Мировые демографические показатели рождаемость, смертность в развитых и развивающихся странах. Демографическая ситуация в Росси
Мировые демографические показатели рождаемость, смертность в развитых и развивающихся странах. Демографическая ситуация в Росси Классификация геморрагического васкулита
Классификация геморрагического васкулита Белки
Белки ЦМК СД в акушерстве и гинекологии ,
ЦМК СД в акушерстве и гинекологии , Medical Education in Japan
Medical Education in Japan Заболевания органов пищеварения у пожилых людей
Заболевания органов пищеварения у пожилых людей