Содержание
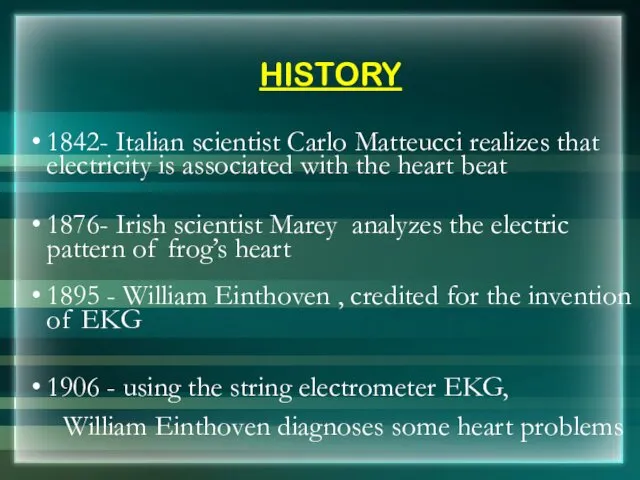
- 2. HISTORY 1842- Italian scientist Carlo Matteucci realizes that electricity is associated with the heart beat 1876-
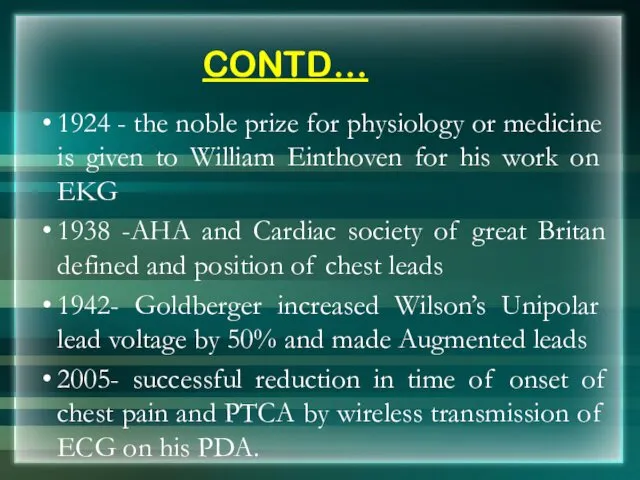
- 3. CONTD… 1924 - the noble prize for physiology or medicine is given to William Einthoven for
- 5. MODERN ECG INSTRUMENT
- 6. What is an EKG? The electrocardiogram (EKG) is a representation of the electrical events of the
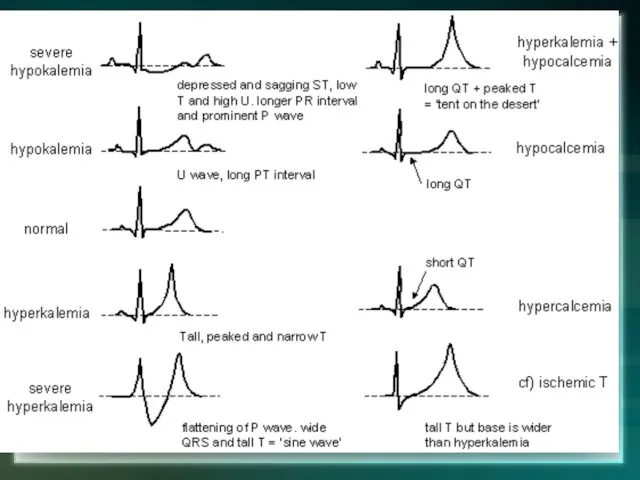
- 7. With EKGs we can identify Arrhythmias Myocardial ischemia and infarction Pericarditis Chamber hypertrophy Electrolyte disturbances (i.e.
- 8. Depolarization Contraction of any muscle is associated with electrical changes called depolarization These changes can be
- 9. Pacemakers of the Heart SA Node - Dominant pacemaker with an intrinsic rate of 60 -
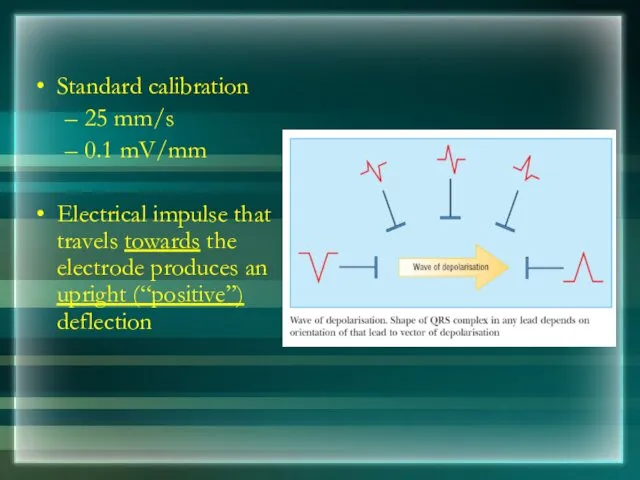
- 10. Standard calibration 25 mm/s 0.1 mV/mm Electrical impulse that travels towards the electrode produces an upright
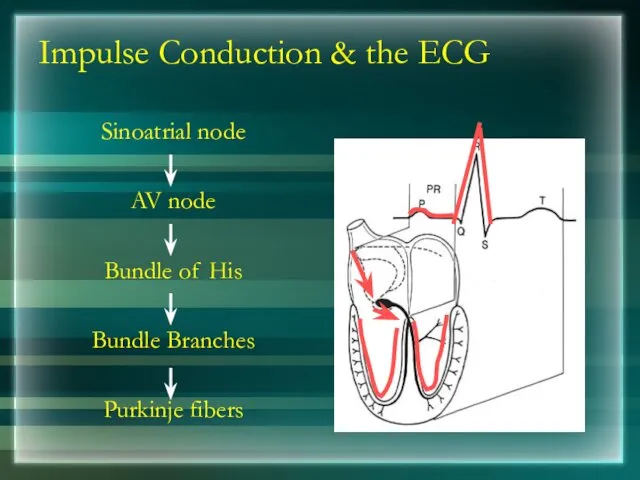
- 11. Impulse Conduction & the ECG Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers
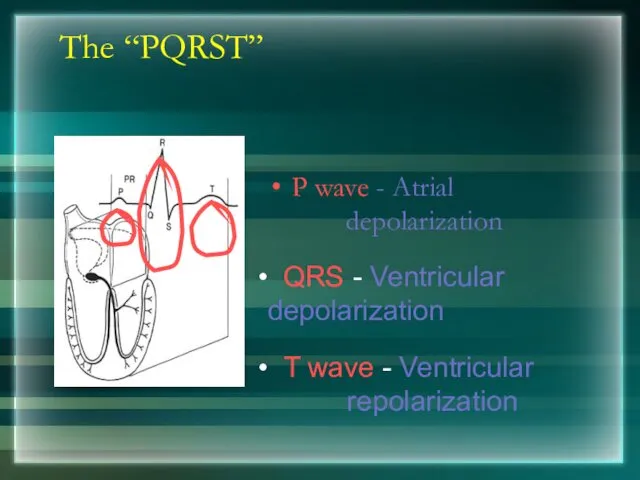
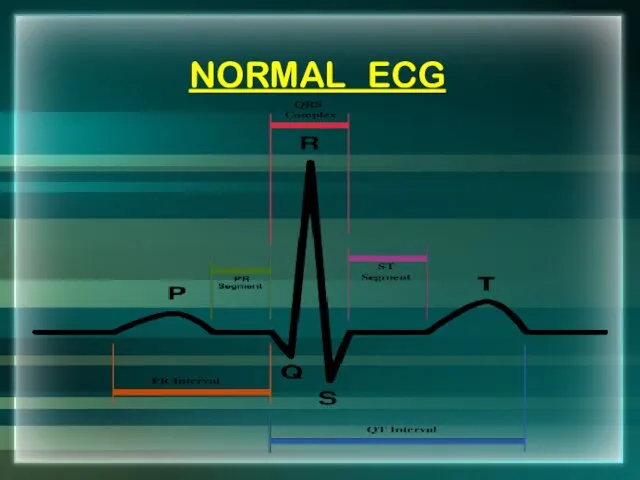
- 12. The “PQRST” P wave - Atrial depolarization T wave - Ventricular repolarization QRS - Ventricular depolarization
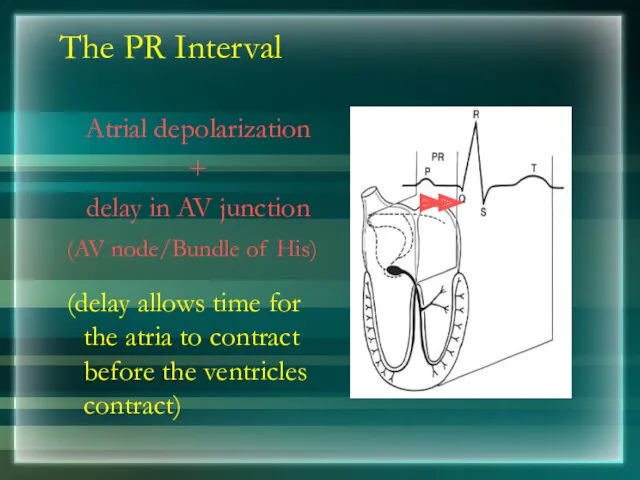
- 13. The PR Interval Atrial depolarization + delay in AV junction (AV node/Bundle of His) (delay allows
- 14. NORMAL ECG
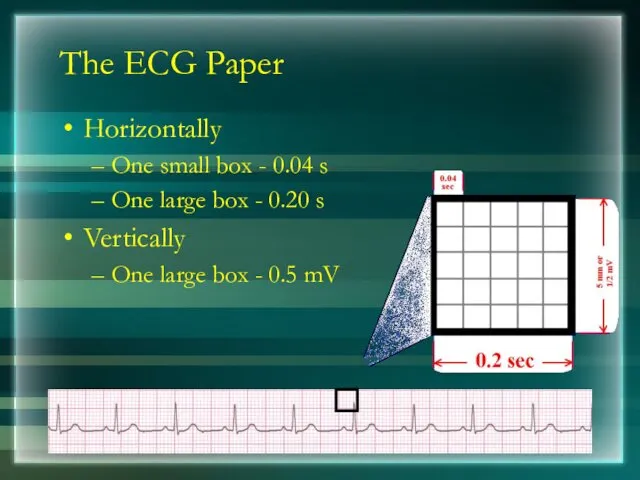
- 15. The ECG Paper Horizontally One small box - 0.04 s One large box - 0.20 s
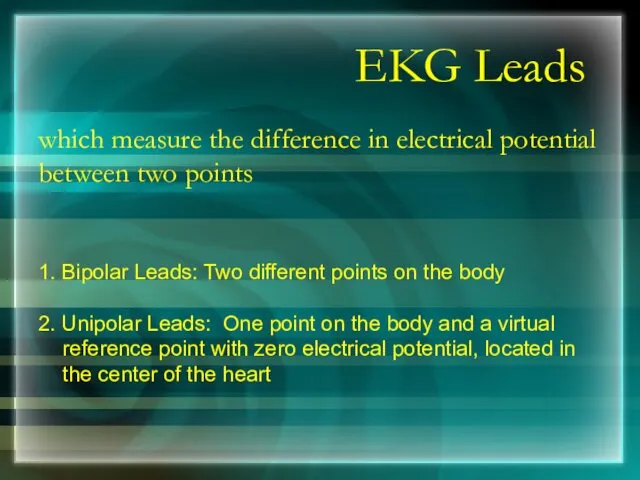
- 16. EKG Leads which measure the difference in electrical potential between two points 1. Bipolar Leads: Two
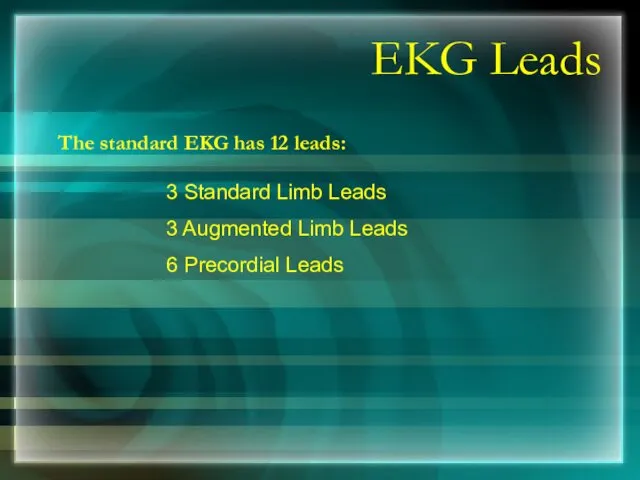
- 17. EKG Leads The standard EKG has 12 leads: 3 Standard Limb Leads 3 Augmented Limb Leads
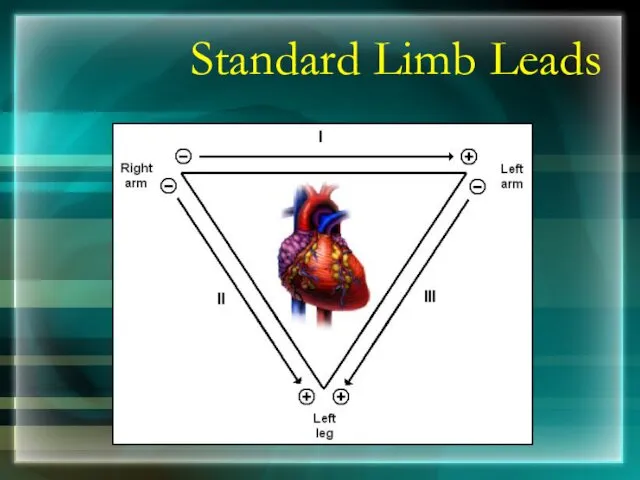
- 18. Standard Limb Leads
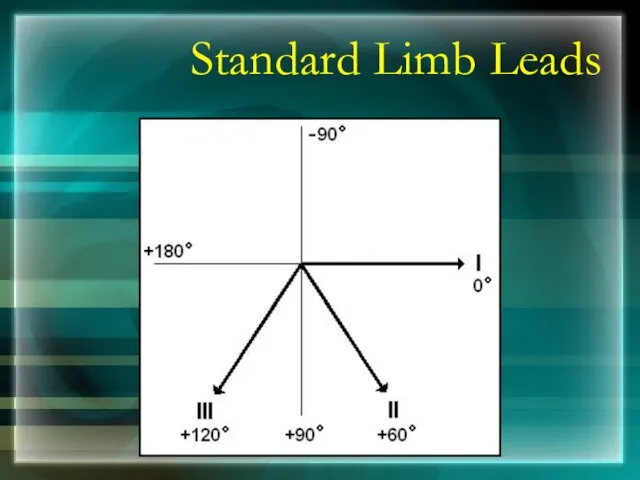
- 19. Standard Limb Leads
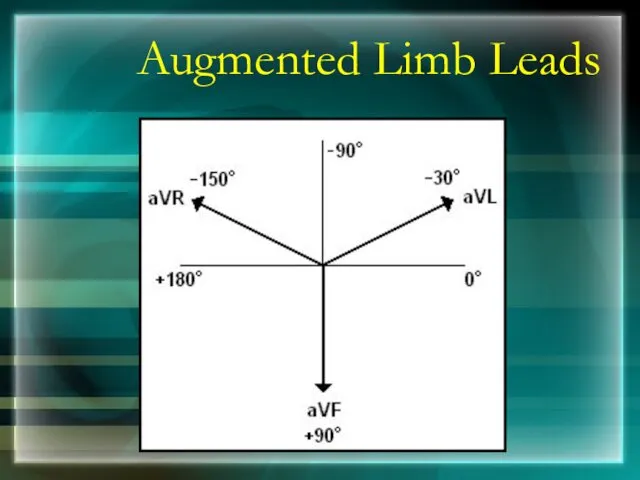
- 20. Augmented Limb Leads
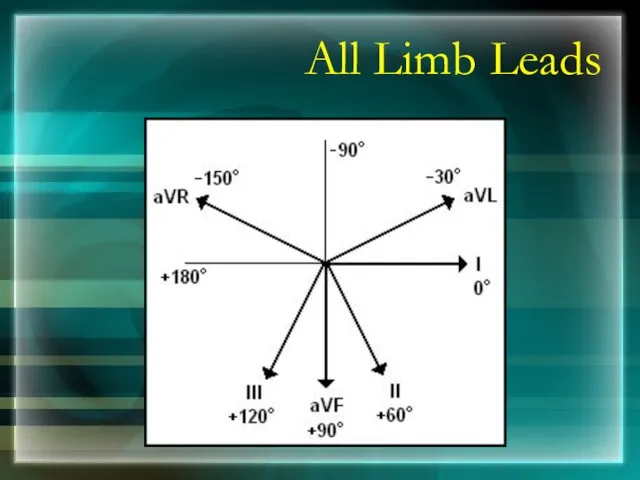
- 21. All Limb Leads
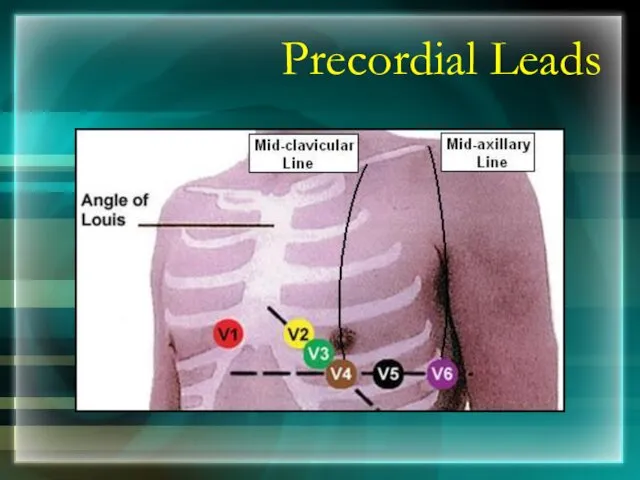
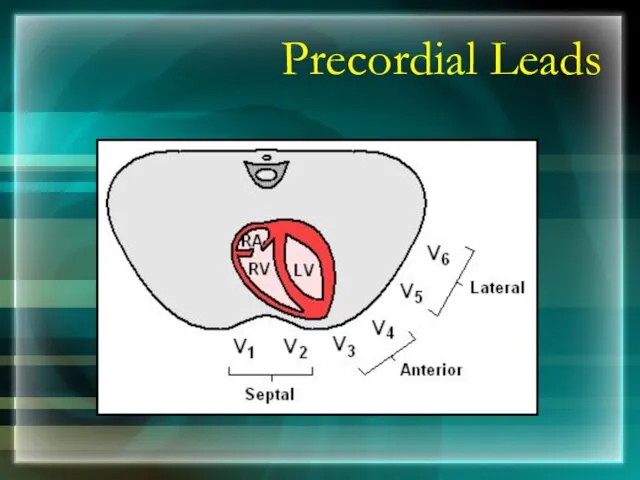
- 22. Precordial Leads
- 23. Precordial Leads
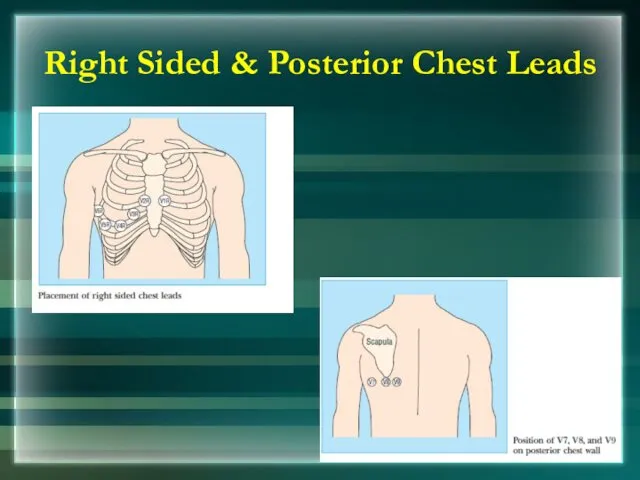
- 24. Right Sided & Posterior Chest Leads
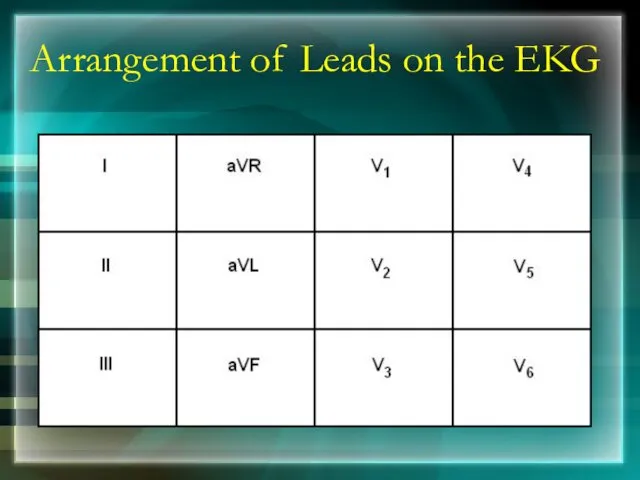
- 25. Arrangement of Leads on the EKG
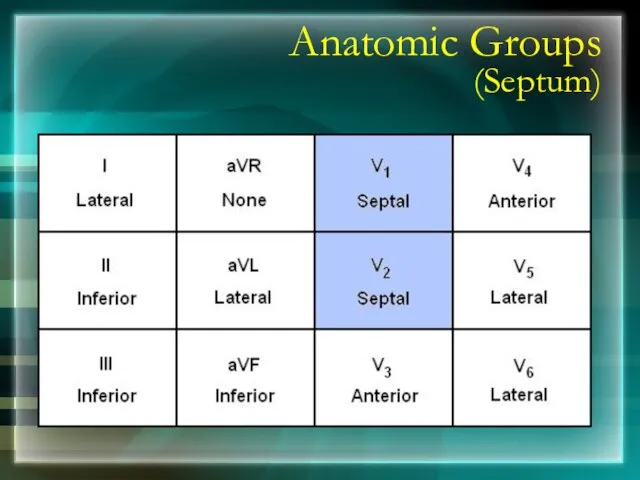
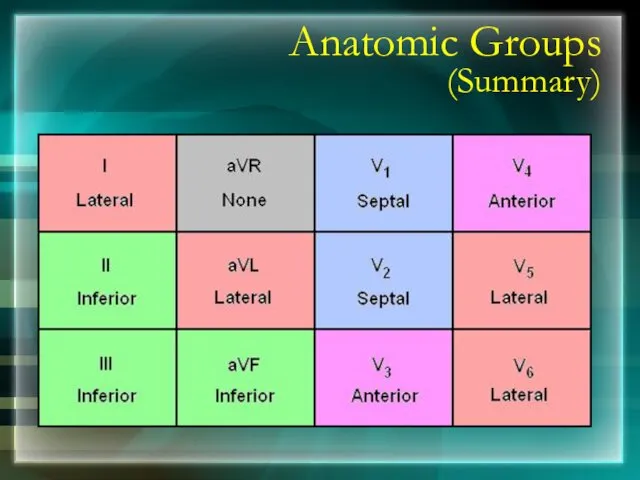
- 26. Anatomic Groups (Septum)
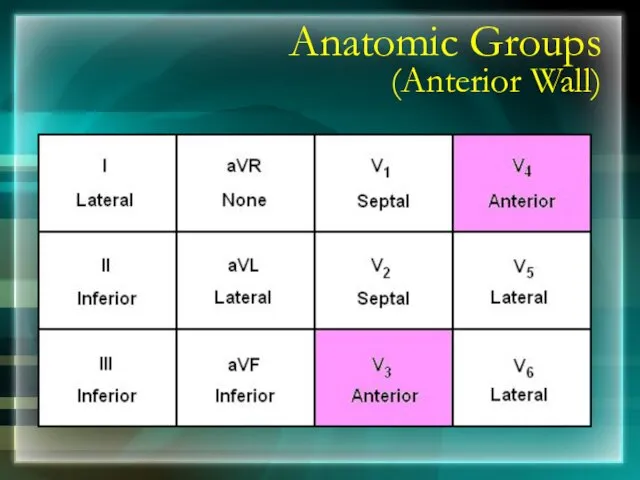
- 27. Anatomic Groups (Anterior Wall)
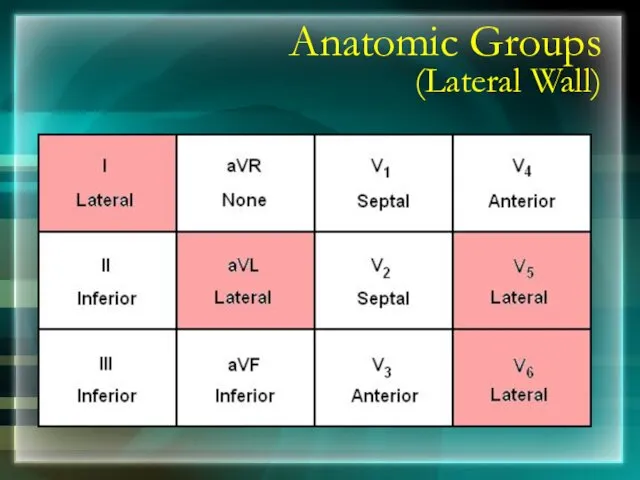
- 28. Anatomic Groups (Lateral Wall)
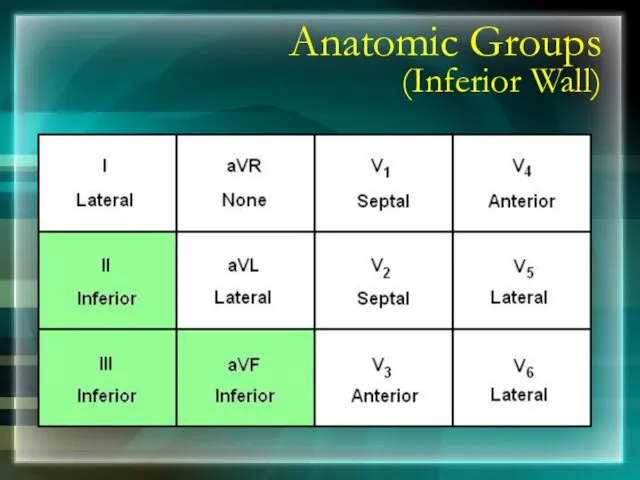
- 29. Anatomic Groups (Inferior Wall)
- 30. Anatomic Groups (Summary)
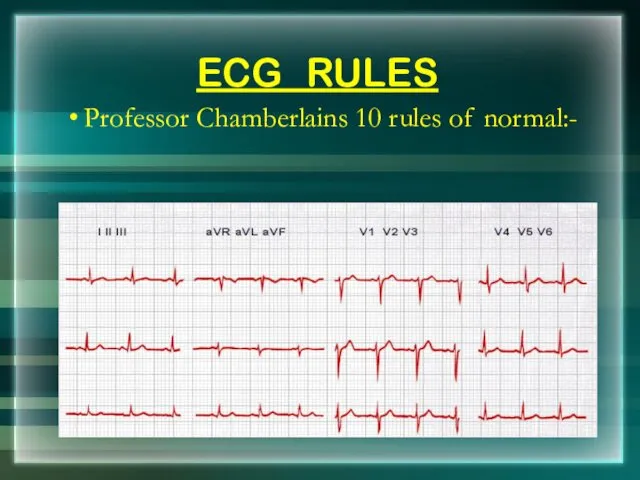
- 31. ECG RULES Professor Chamberlains 10 rules of normal:-
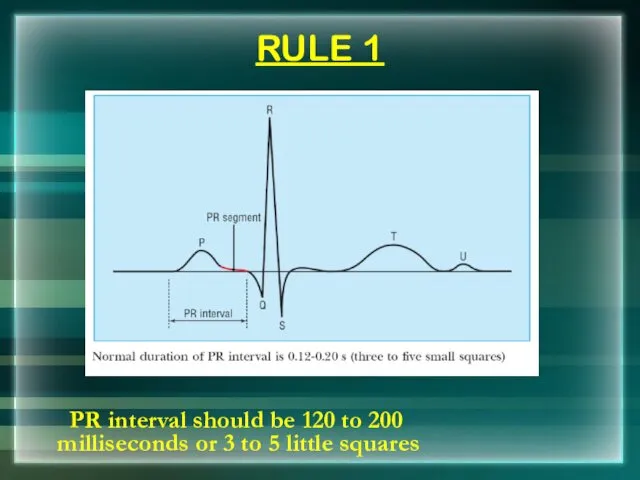
- 32. RULE 1 PR interval should be 120 to 200 milliseconds or 3 to 5 little squares
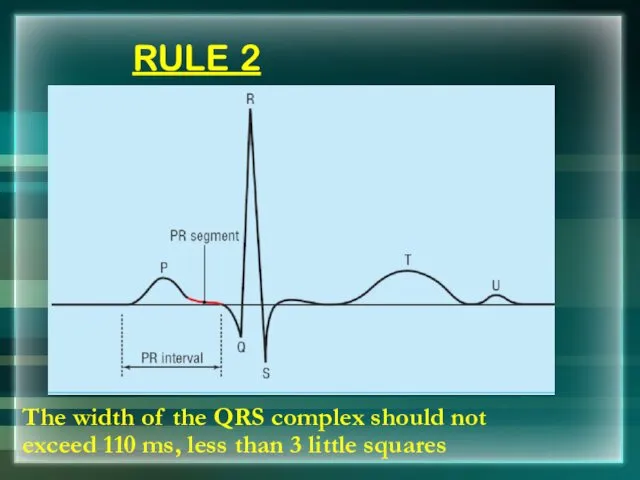
- 33. RULE 2 The width of the QRS complex should not exceed 110 ms, less than 3
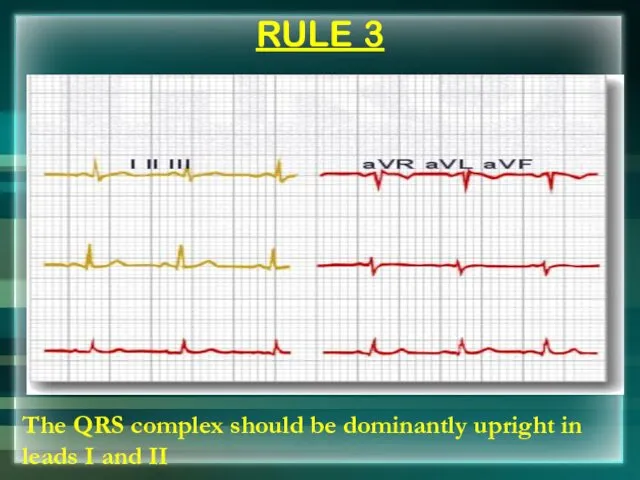
- 34. RULE 3 The QRS complex should be dominantly upright in leads I and II
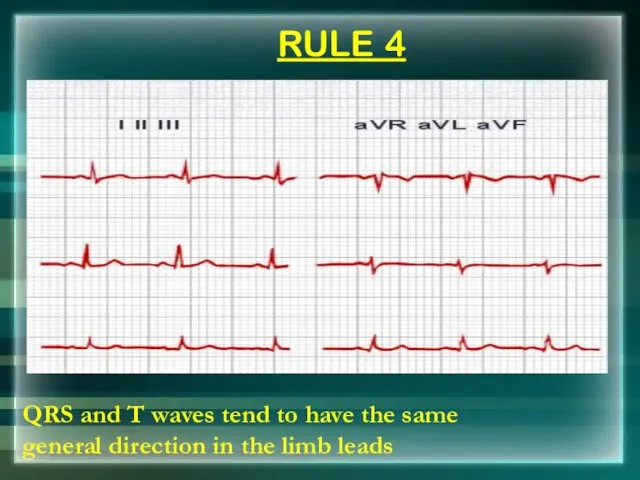
- 35. RULE 4 QRS and T waves tend to have the same general direction in the limb
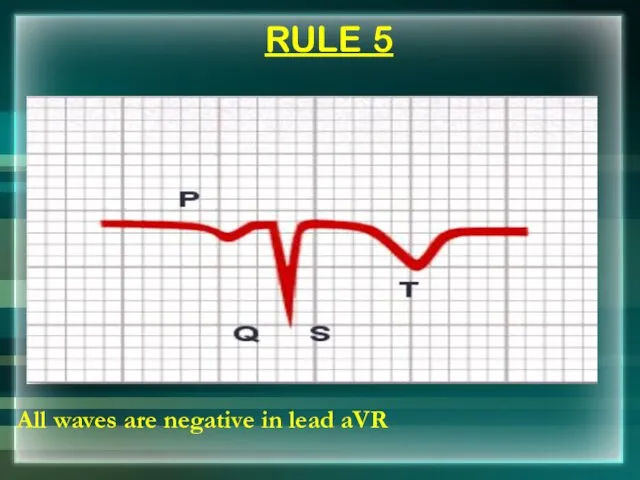
- 36. RULE 5 All waves are negative in lead aVR
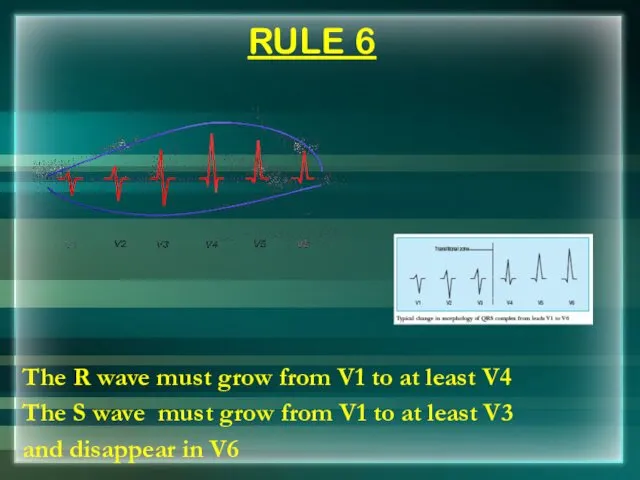
- 37. RULE 6 The R wave must grow from V1 to at least V4 The S wave
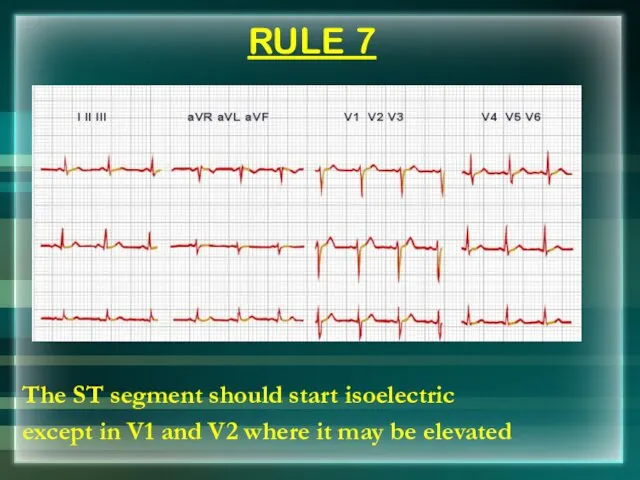
- 38. RULE 7 The ST segment should start isoelectric except in V1 and V2 where it may
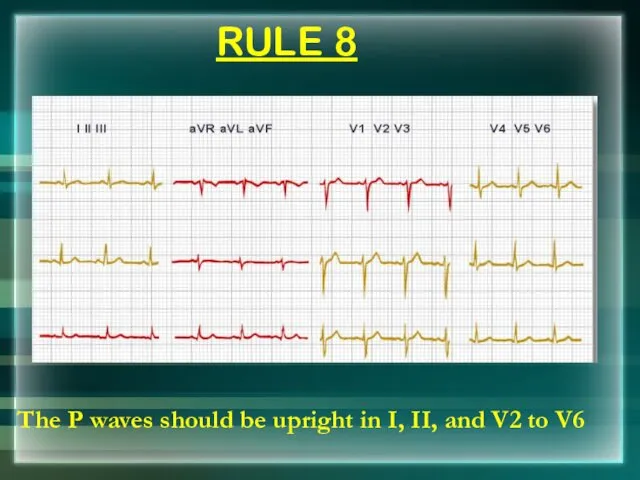
- 39. RULE 8 The P waves should be upright in I, II, and V2 to V6
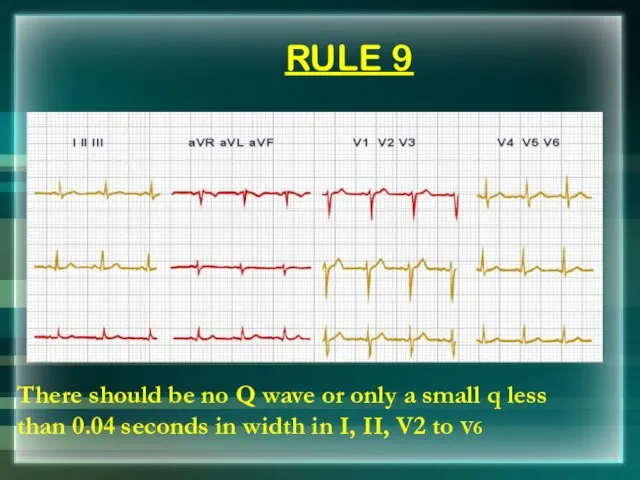
- 40. RULE 9 There should be no Q wave or only a small q less than 0.04
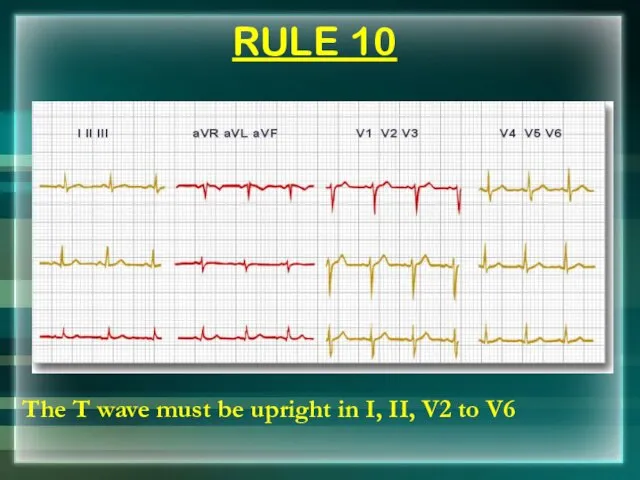
- 41. RULE 10 The T wave must be upright in I, II, V2 to V6
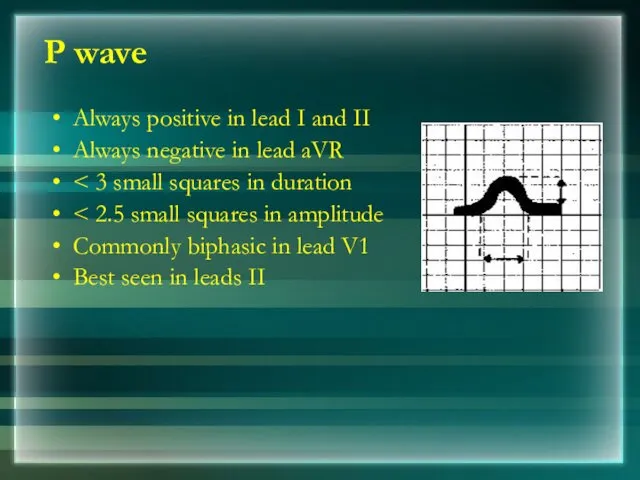
- 42. P wave Always positive in lead I and II Always negative in lead aVR Commonly biphasic
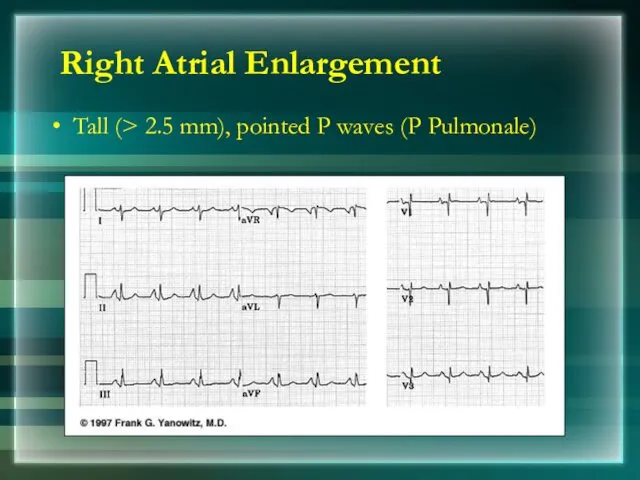
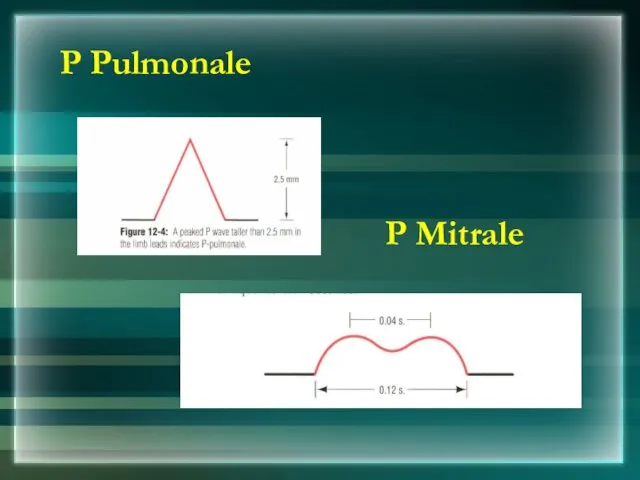
- 43. Right Atrial Enlargement Tall (> 2.5 mm), pointed P waves (P Pulmonale)
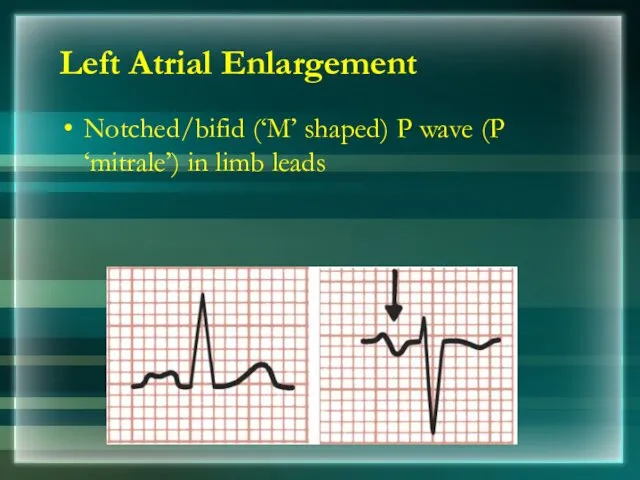
- 44. Notched/bifid (‘M’ shaped) P wave (P ‘mitrale’) in limb leads Left Atrial Enlargement
- 45. P Pulmonale P Mitrale
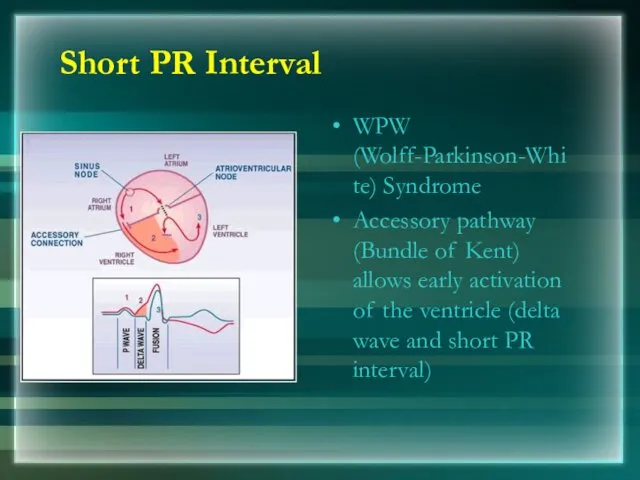
- 46. Short PR Interval WPW (Wolff-Parkinson-White) Syndrome Accessory pathway (Bundle of Kent) allows early activation of the
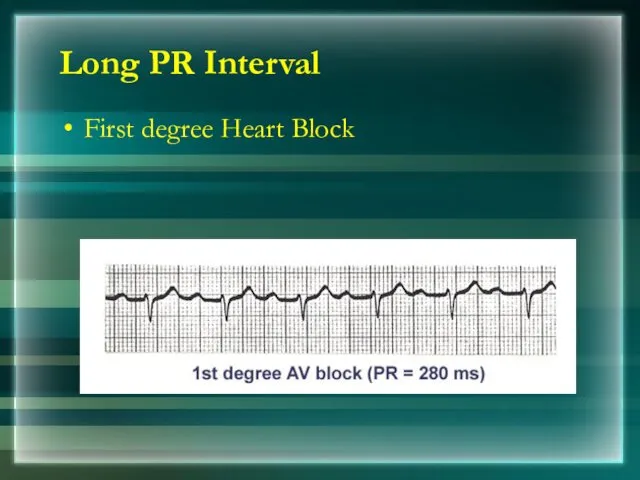
- 47. Long PR Interval First degree Heart Block
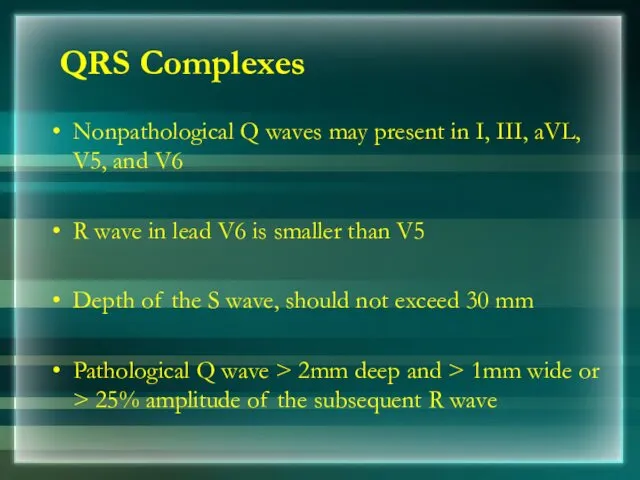
- 48. QRS Complexes Nonpathological Q waves may present in I, III, aVL, V5, and V6 R wave
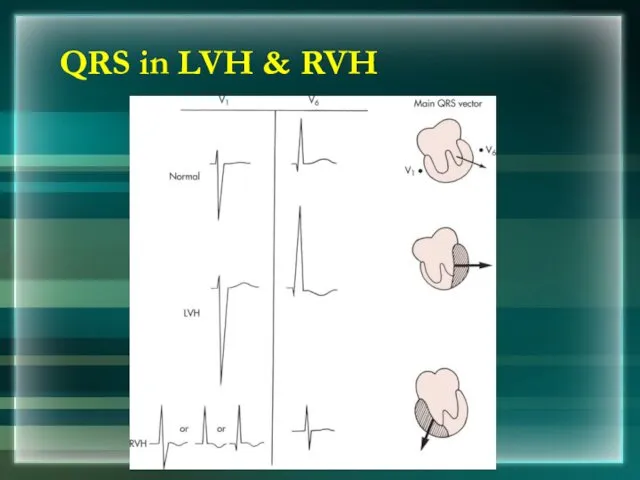
- 49. QRS in LVH & RVH
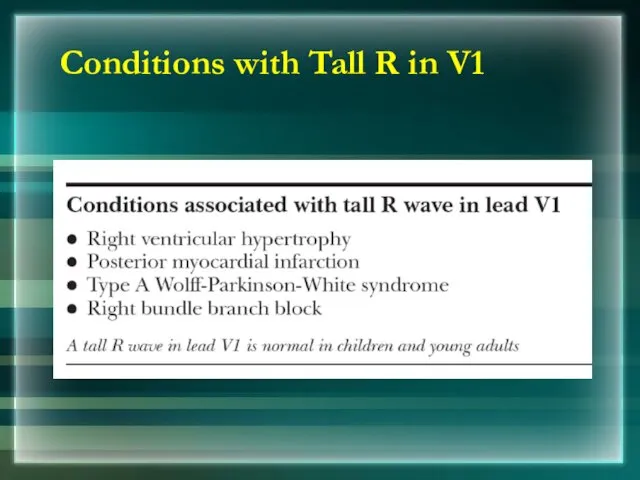
- 50. Conditions with Tall R in V1
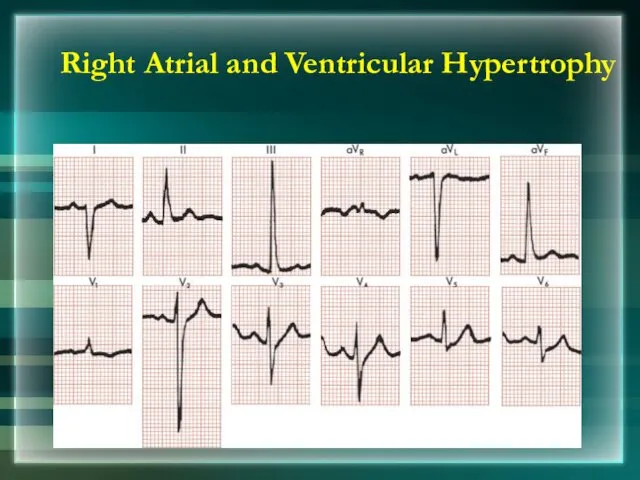
- 51. Right Atrial and Ventricular Hypertrophy
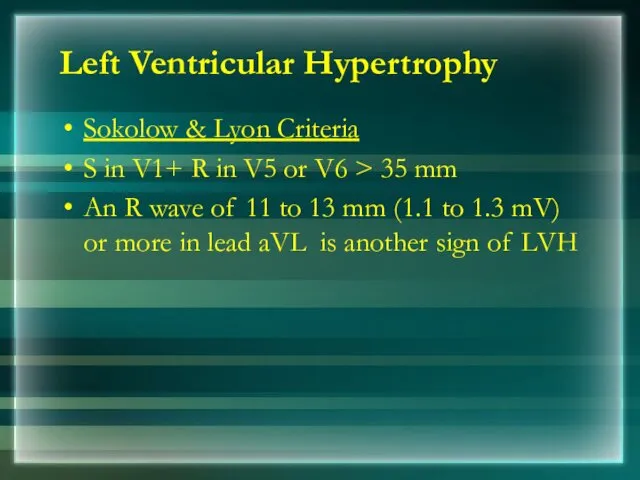
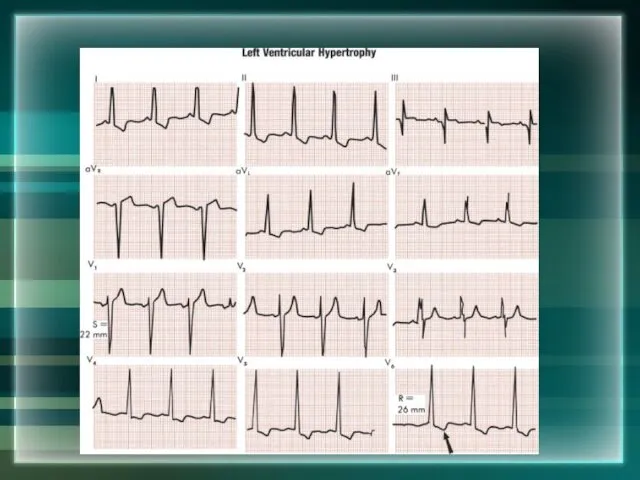
- 52. Left Ventricular Hypertrophy Sokolow & Lyon Criteria S in V1+ R in V5 or V6 >
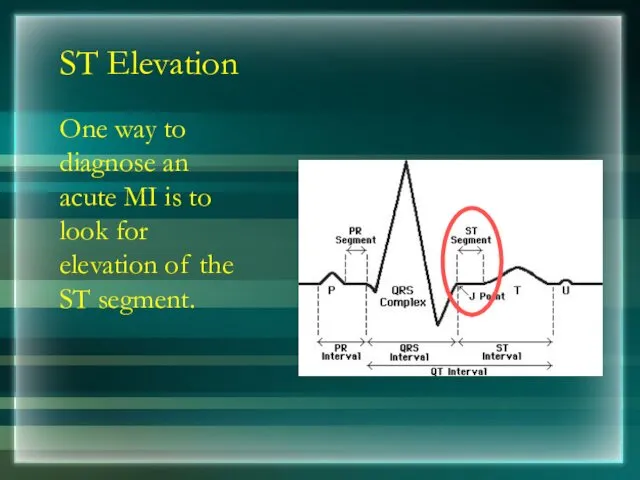
- 54. ST Segment ST Segment is flat (isoelectric) Elevation or depression of ST segment by 1 mm
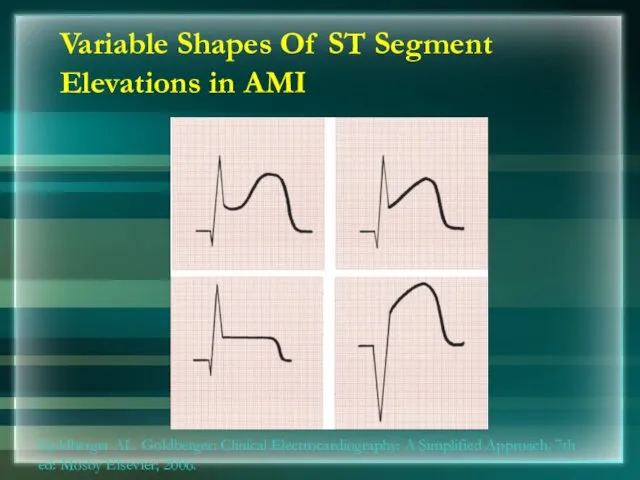
- 55. Variable Shapes Of ST Segment Elevations in AMI Goldberger AL. Goldberger: Clinical Electrocardiography: A Simplified Approach.
- 56. T wave Normal T wave is asymmetrical, first half having a gradual slope than the second
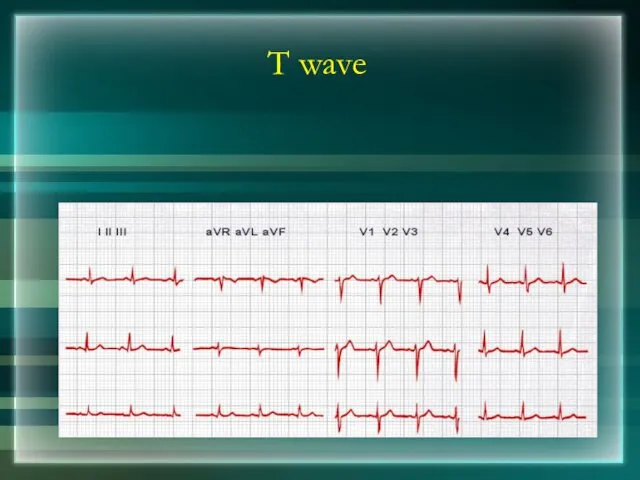
- 57. T wave
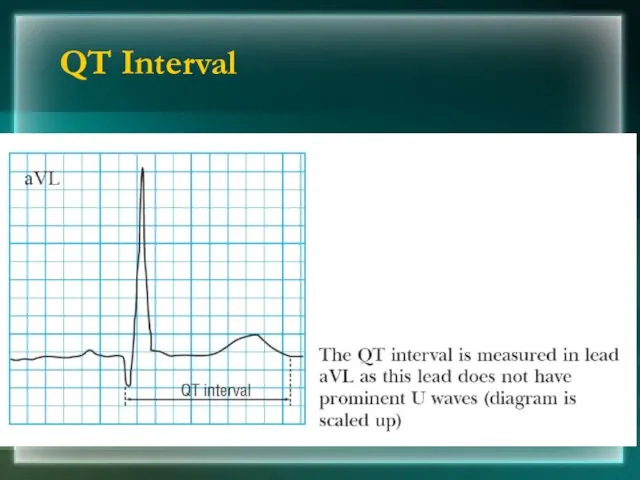
- 58. QT interval Total duration of Depolarization and Repolarization QT interval decreases when heart rate increases For
- 59. QT Interval
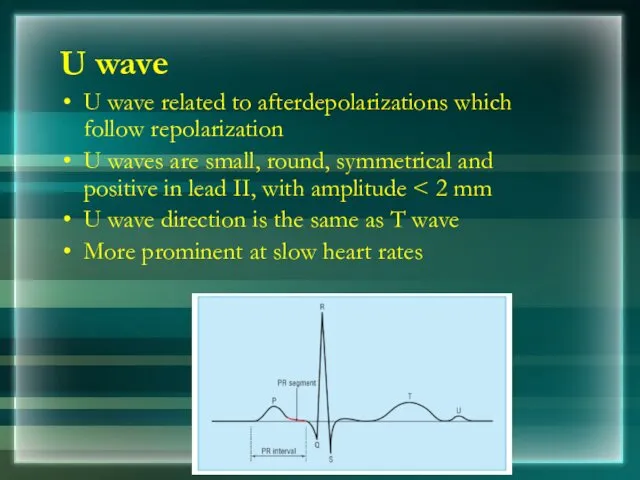
- 60. U wave U wave related to afterdepolarizations which follow repolarization U waves are small, round, symmetrical
- 61. Determining the Heart Rate Rule of 300/1500 10 Second Rule
- 62. Rule of 300 Count the number of “big boxes” between two QRS complexes, and divide this
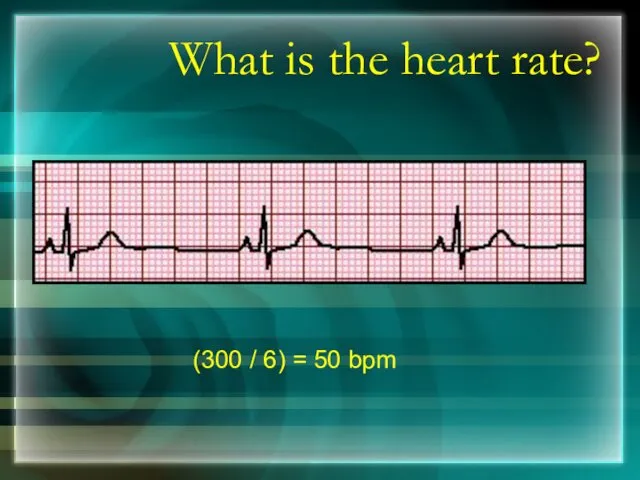
- 63. What is the heart rate? (300 / 6) = 50 bpm
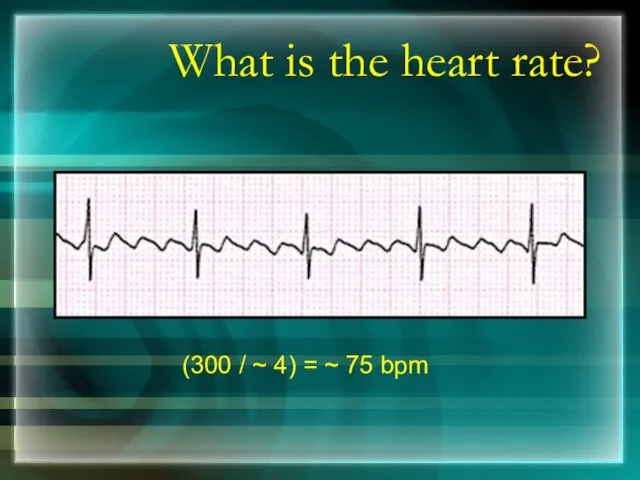
- 64. What is the heart rate? (300 / ~ 4) = ~ 75 bpm
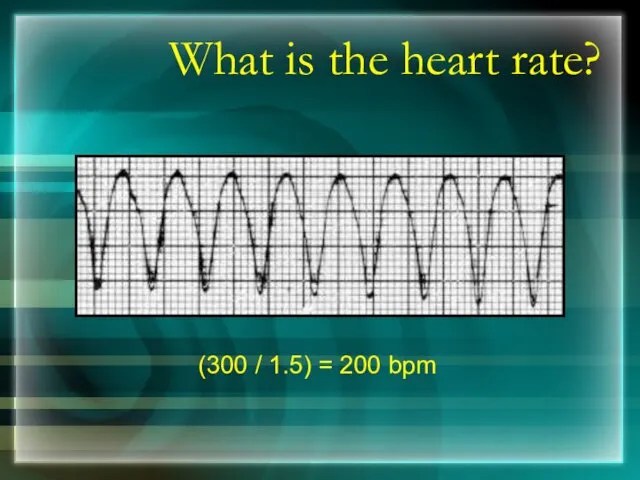
- 65. What is the heart rate? (300 / 1.5) = 200 bpm
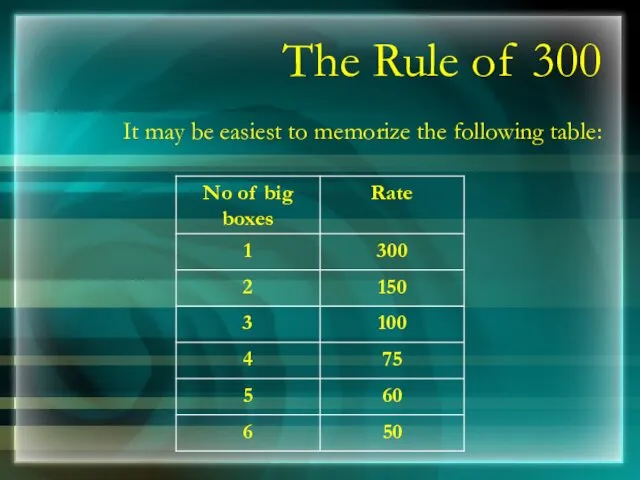
- 66. The Rule of 300 It may be easiest to memorize the following table:
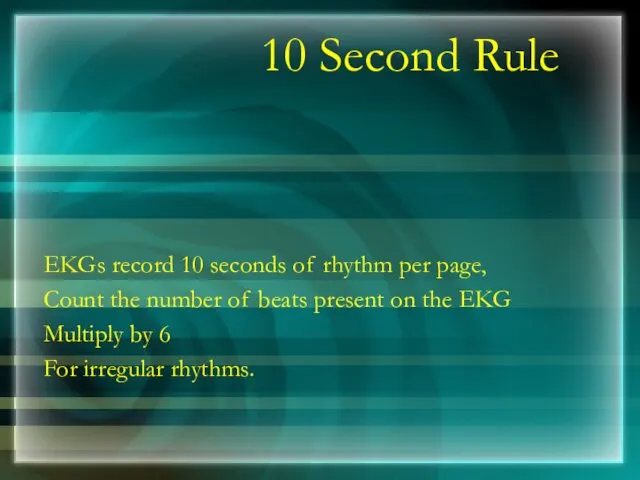
- 67. 10 Second Rule EKGs record 10 seconds of rhythm per page, Count the number of beats
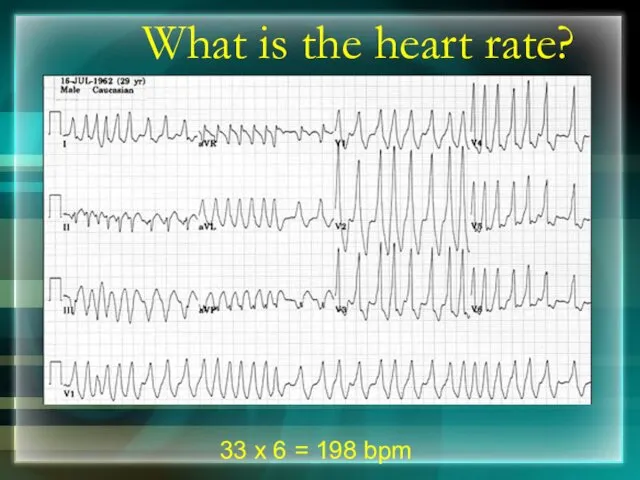
- 68. What is the heart rate? 33 x 6 = 198 bpm
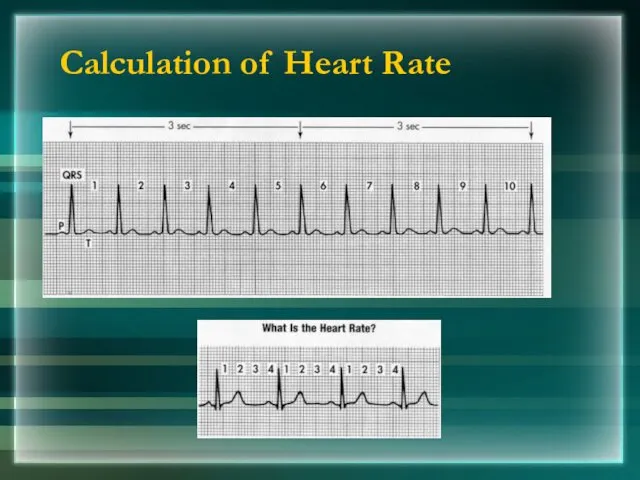
- 69. Calculation of Heart Rate
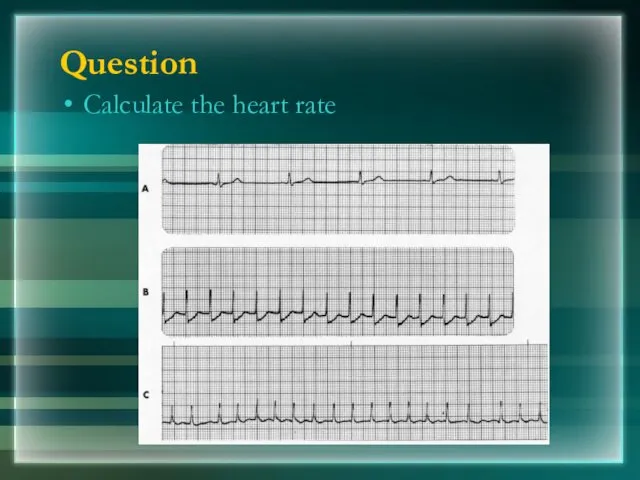
- 70. Question Calculate the heart rate
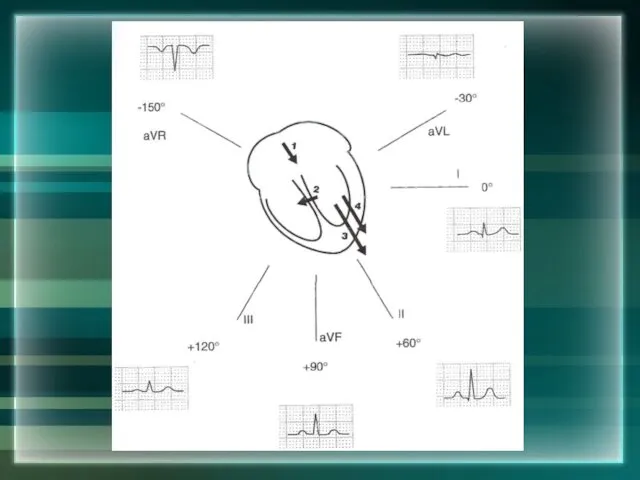
- 71. The QRS Axis The QRS axis represents overall direction of the heart’s electrical activity. Abnormalities hint
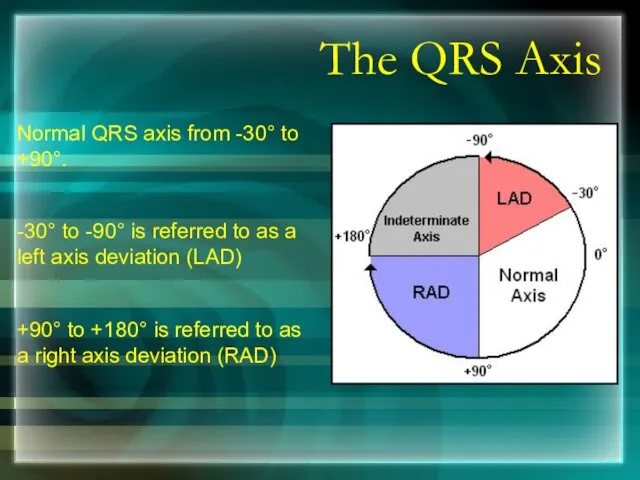
- 72. The QRS Axis Normal QRS axis from -30° to +90°. -30° to -90° is referred to
- 73. Determining the Axis The Quadrant Approach The Equiphasic Approach
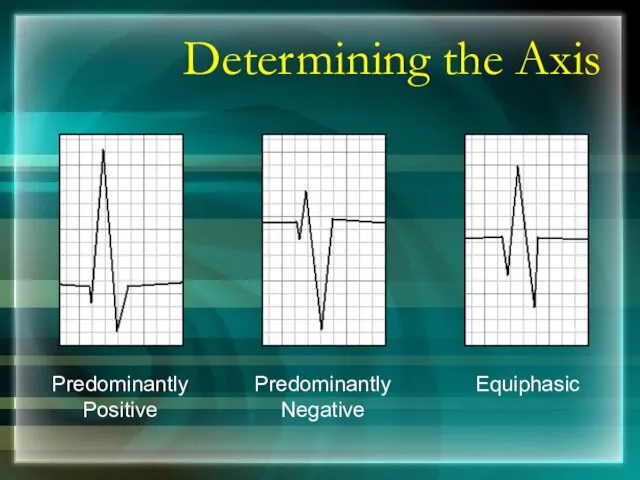
- 74. Determining the Axis Predominantly Positive Predominantly Negative Equiphasic
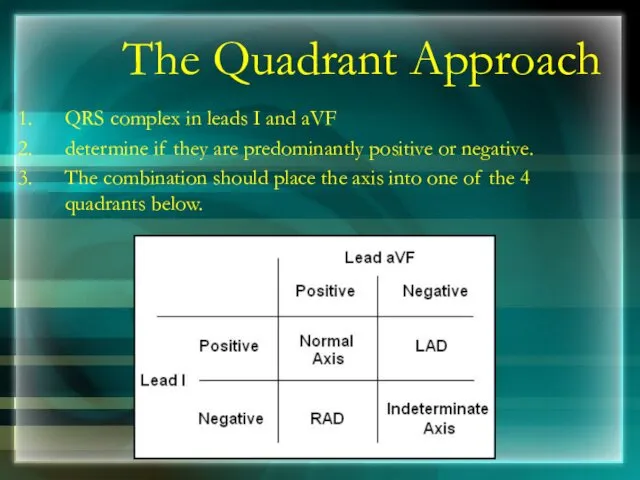
- 75. The Quadrant Approach QRS complex in leads I and aVF determine if they are predominantly positive
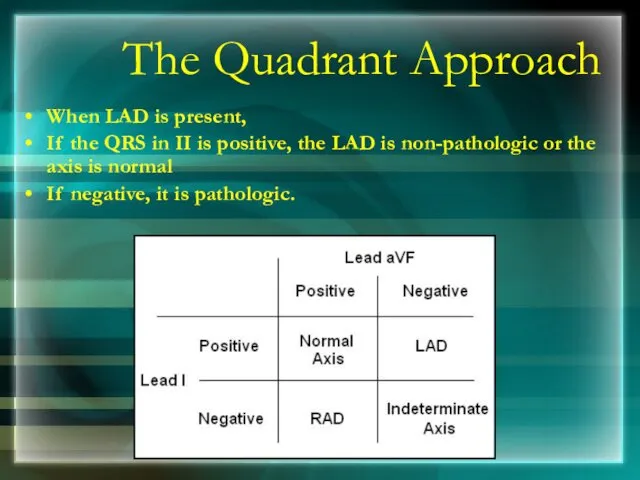
- 76. The Quadrant Approach When LAD is present, If the QRS in II is positive, the LAD
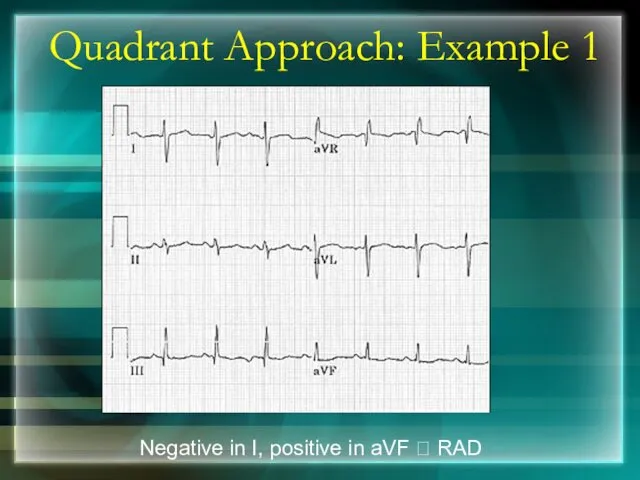
- 77. Quadrant Approach: Example 1 Negative in I, positive in aVF ? RAD
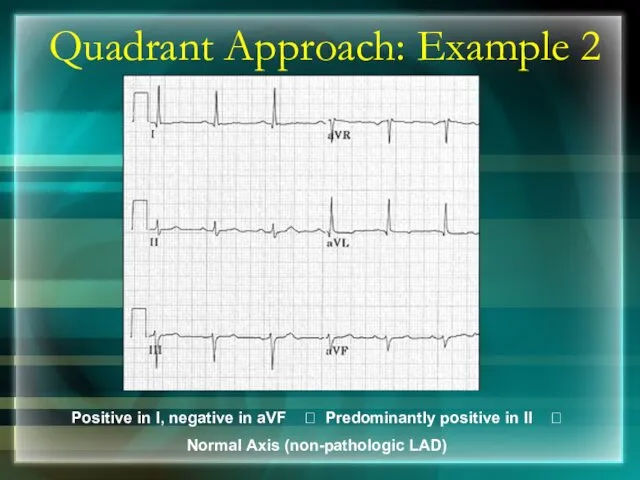
- 78. Quadrant Approach: Example 2 Positive in I, negative in aVF ? Predominantly positive in II ?
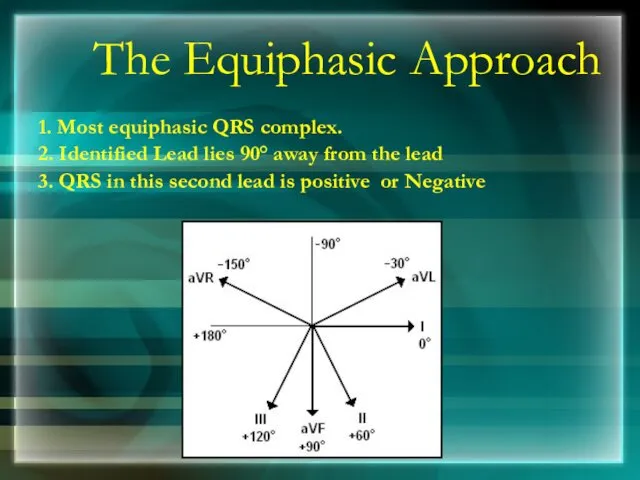
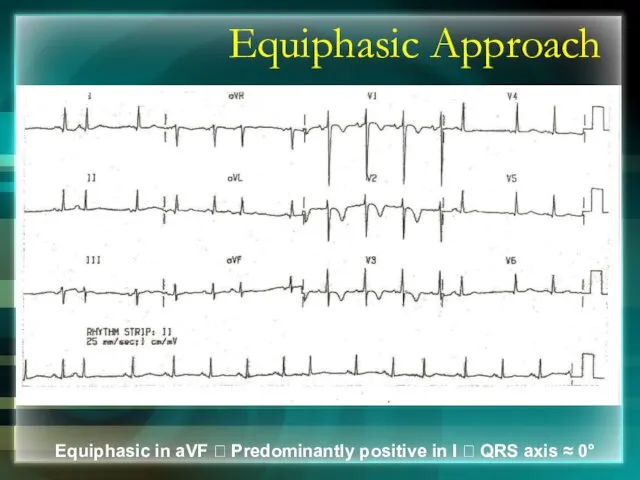
- 79. The Equiphasic Approach 1. Most equiphasic QRS complex. 2. Identified Lead lies 90° away from the
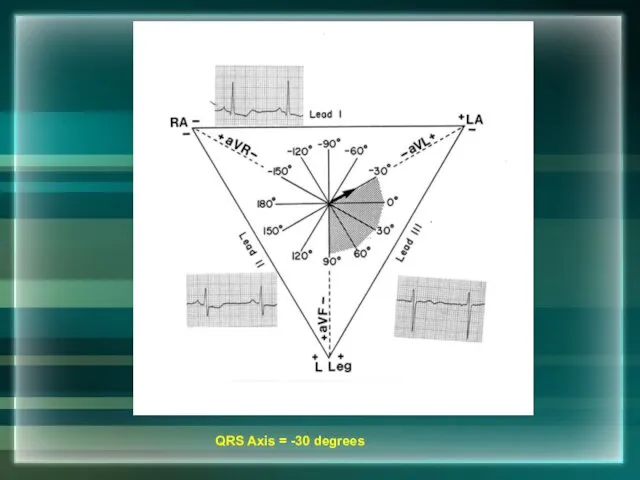
- 80. QRS Axis = -30 degrees
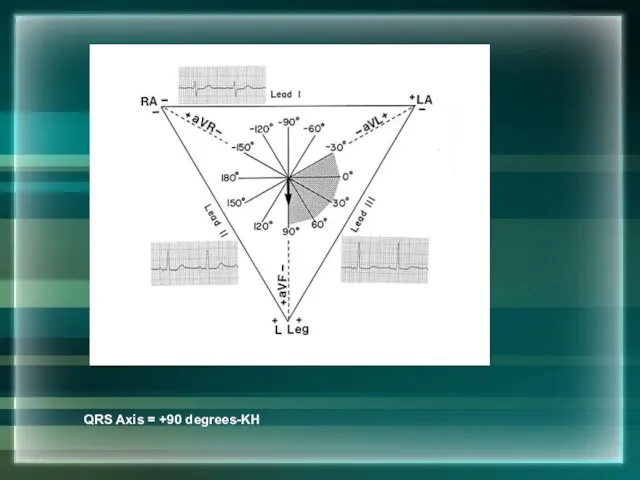
- 81. QRS Axis = +90 degrees-KH
- 83. Equiphasic Approach Equiphasic in aVF ? Predominantly positive in I ? QRS axis ≈ 0°
- 84. Thank You
- 85. BRADYARRYTHMIA Dr Subroto Mandal, MD, DM, DC Associate Professor, Cardiology
- 86. Classification Sinus Bradycardia Junctional Rhythm Sino Atrial Block Atrioventricular block
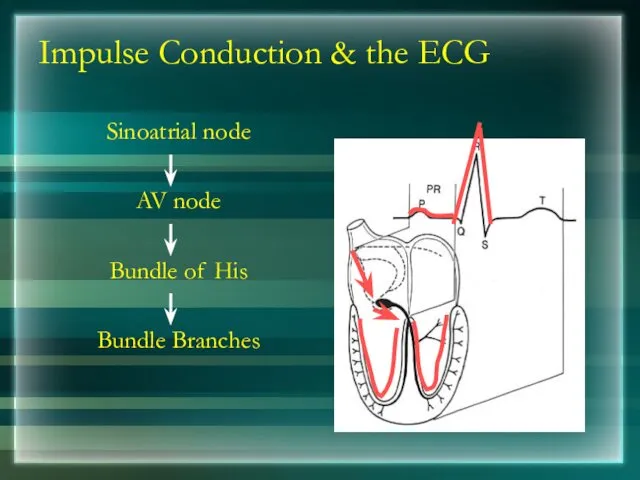
- 87. Impulse Conduction & the ECG Sinoatrial node AV node Bundle of His Bundle Branches
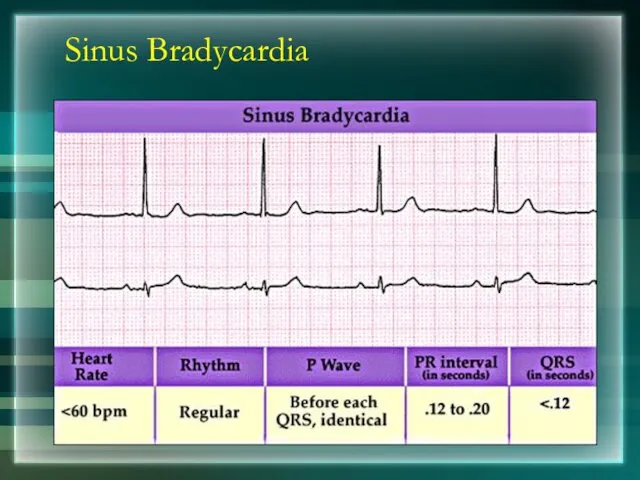
- 88. Sinus Bradycardia
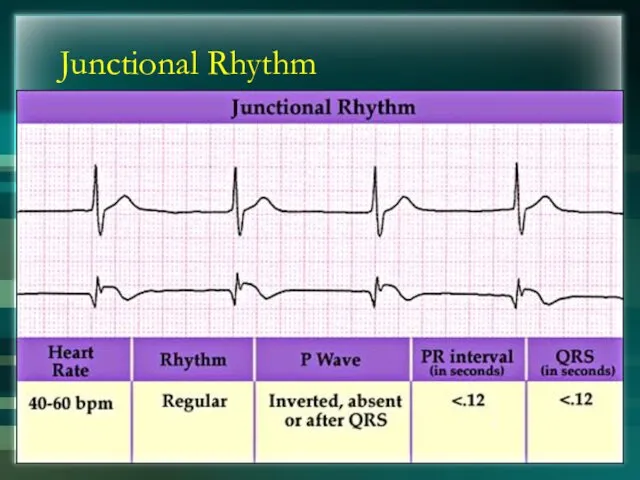
- 89. Junctional Rhythm
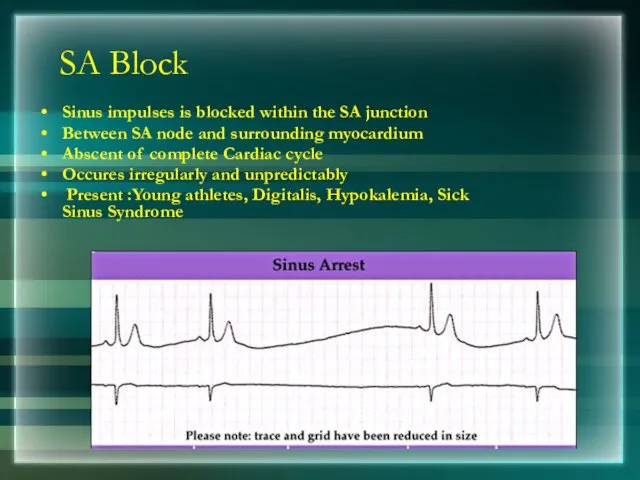
- 90. SA Block Sinus impulses is blocked within the SA junction Between SA node and surrounding myocardium
- 91. AV Block First Degree AV Block Second Degree AV Block Third Degree AV Block
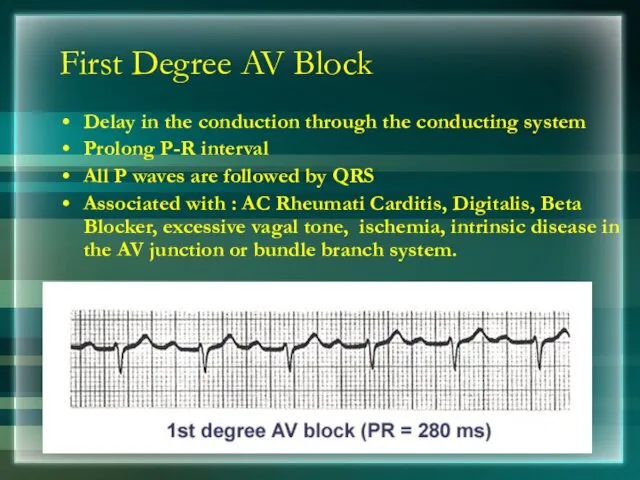
- 92. First Degree AV Block Delay in the conduction through the conducting system Prolong P-R interval All
- 93. Second Degree AV Block Intermittent failure of AV conduction Impulse blocked by AV node Types: Mobitz
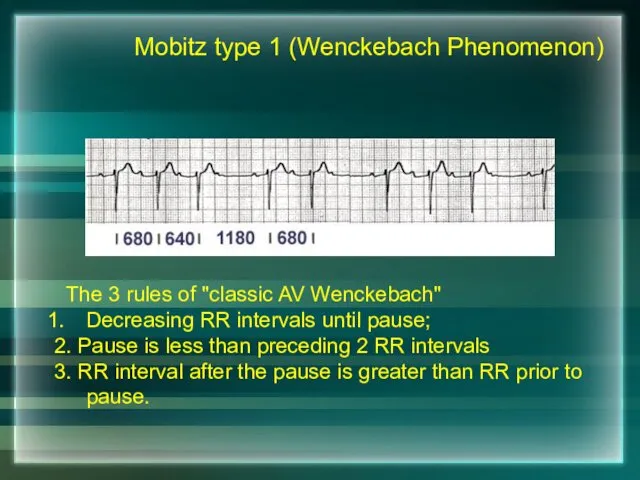
- 94. The 3 rules of "classic AV Wenckebach" Decreasing RR intervals until pause; 2. Pause is less
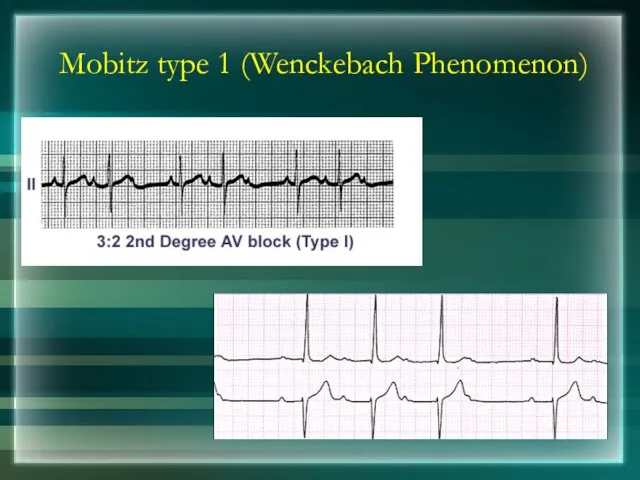
- 95. Mobitz type 1 (Wenckebach Phenomenon)
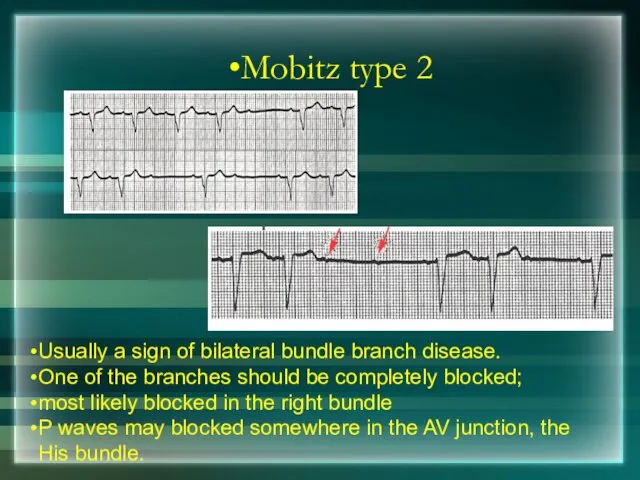
- 96. Mobitz type 2 Usually a sign of bilateral bundle branch disease. One of the branches should
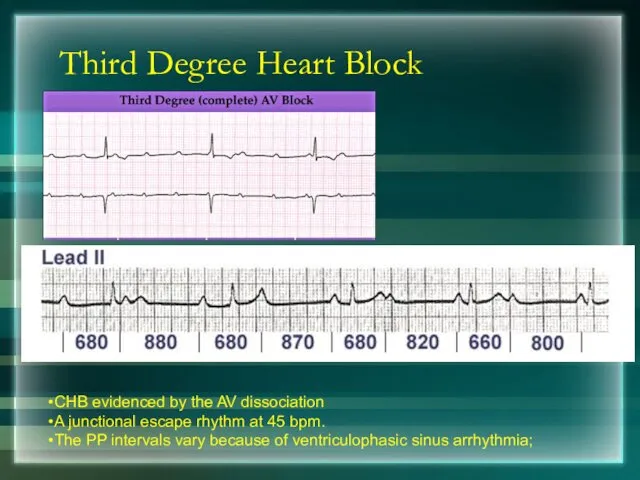
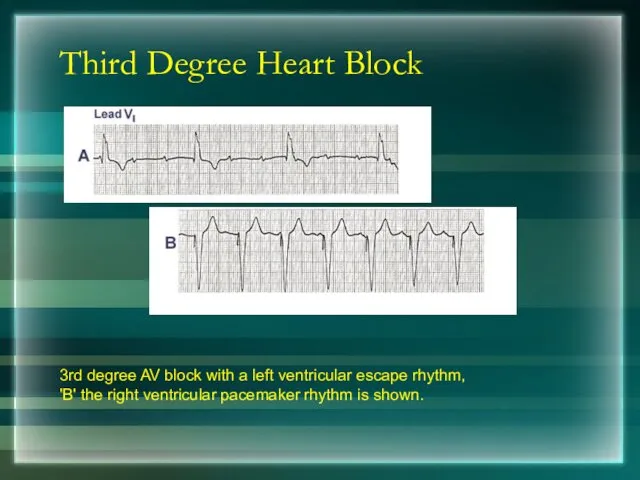
- 97. Third Degree Heart Block CHB evidenced by the AV dissociation A junctional escape rhythm at 45
- 98. Third Degree Heart Block 3rd degree AV block with a left ventricular escape rhythm, 'B' the
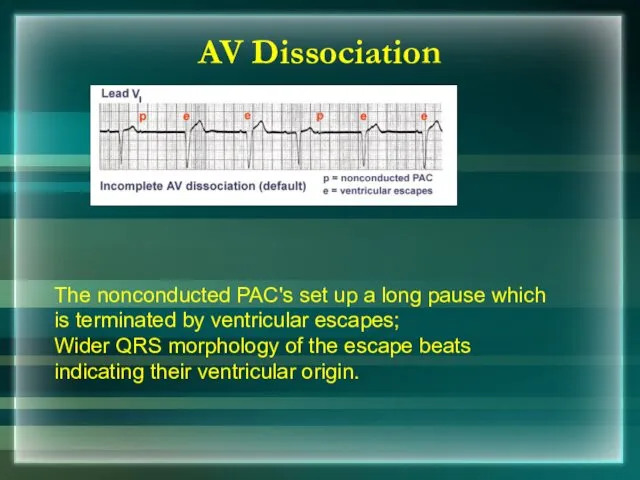
- 99. The nonconducted PAC's set up a long pause which is terminated by ventricular escapes; Wider QRS
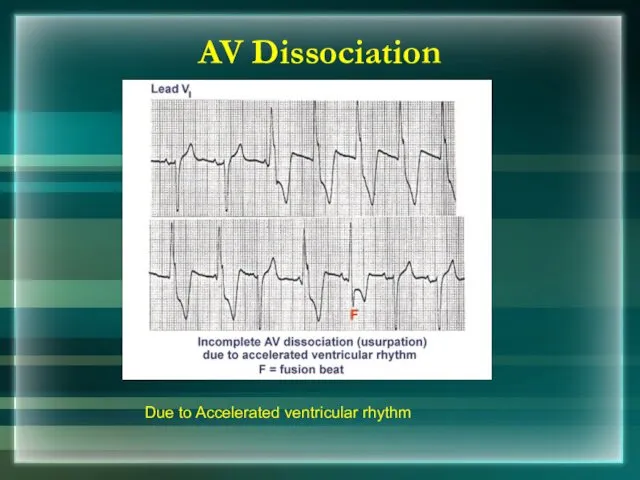
- 100. AV Dissociation Due to Accelerated ventricular rhythm
- 101. Thank You
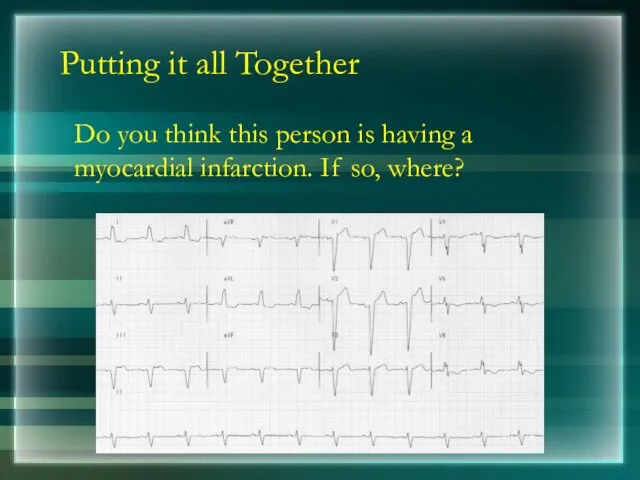
- 102. Putting it all Together Do you think this person is having a myocardial infarction. If so,
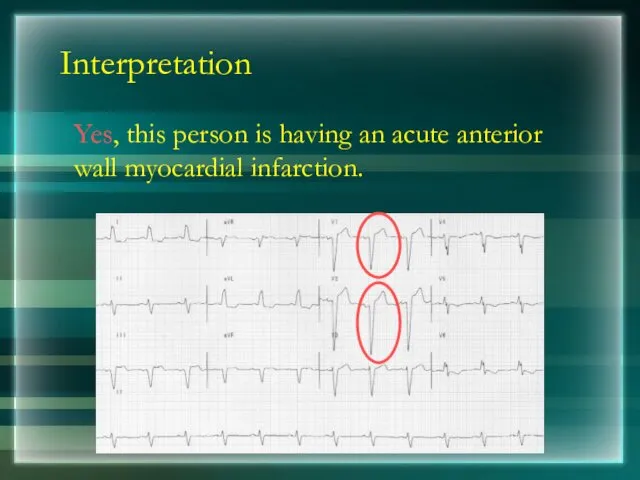
- 103. Interpretation Yes, this person is having an acute anterior wall myocardial infarction.
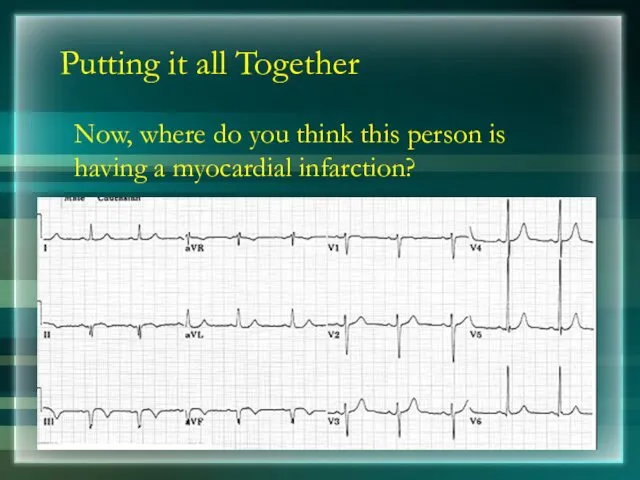
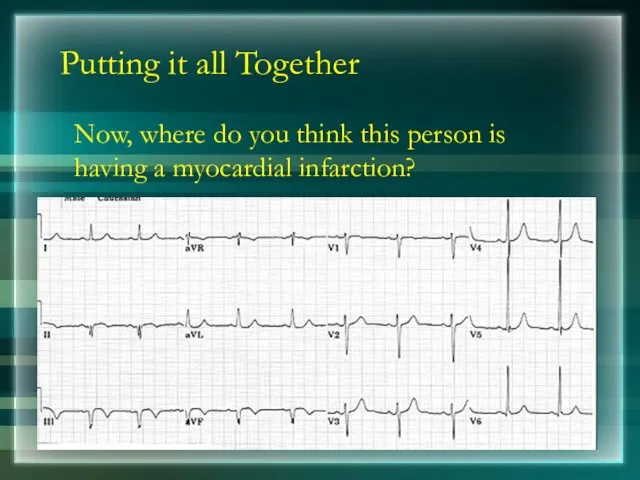
- 104. Putting it all Together Now, where do you think this person is having a myocardial infarction?
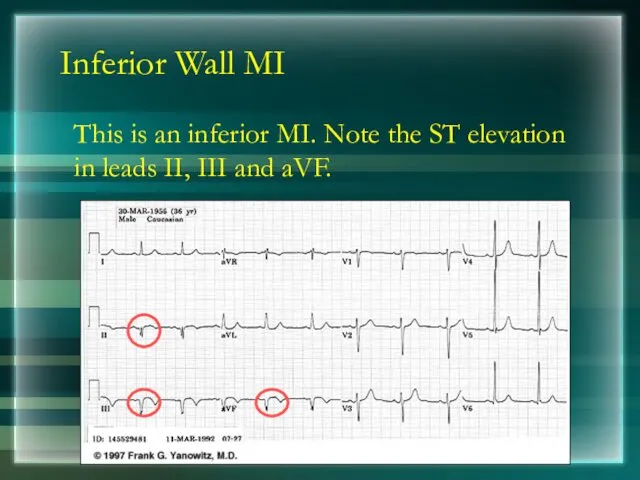
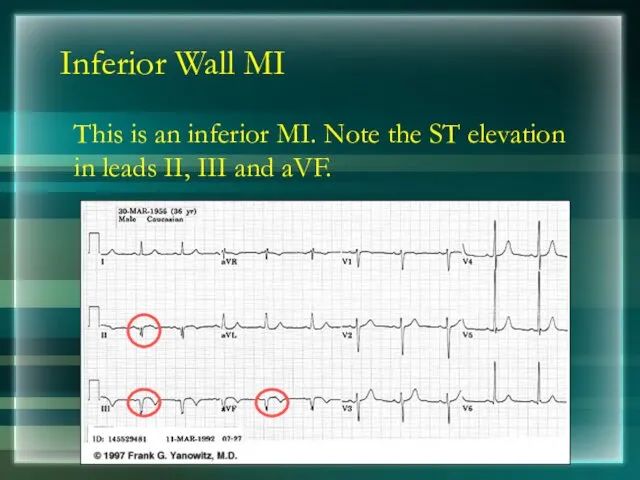
- 105. Inferior Wall MI This is an inferior MI. Note the ST elevation in leads II, III
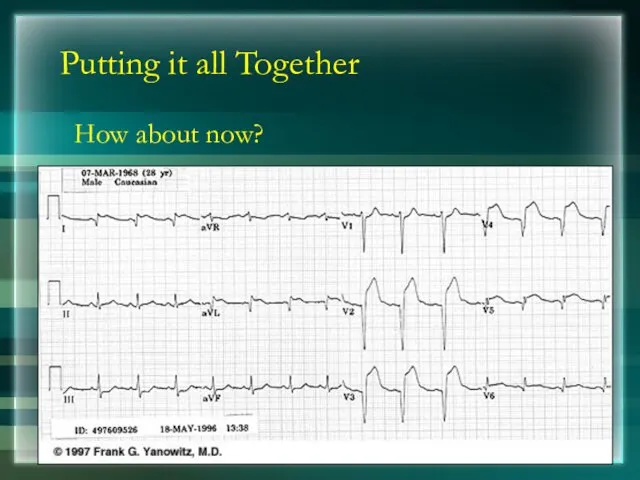
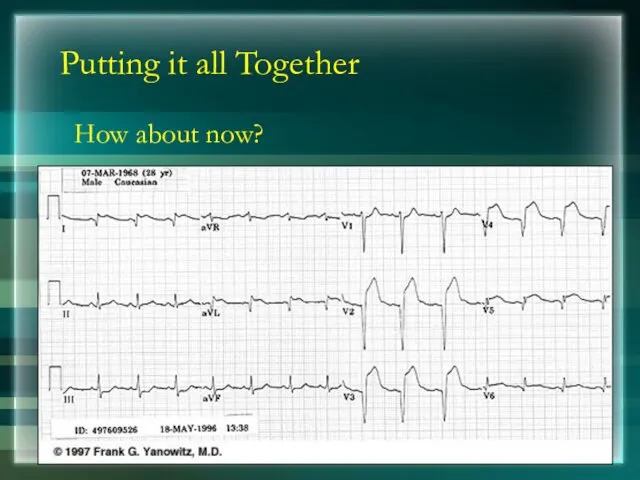
- 106. Putting it all Together How about now?
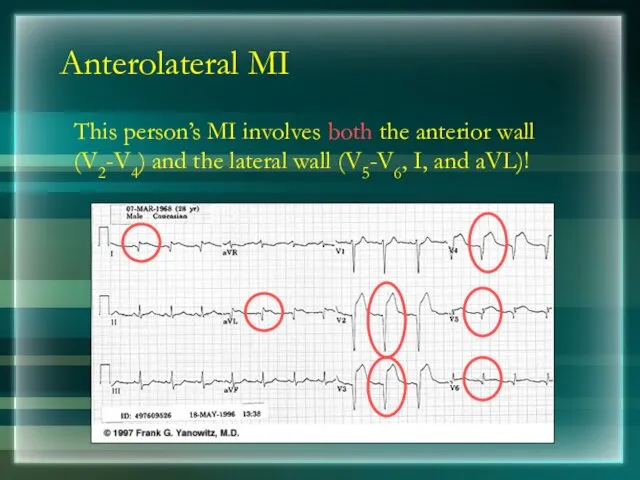
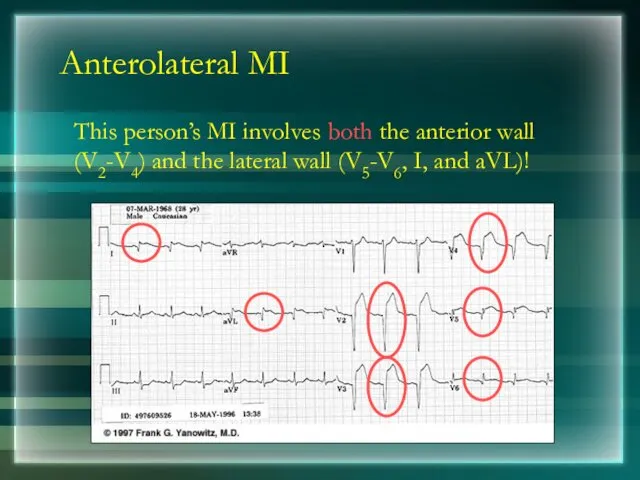
- 107. Anterolateral MI This person’s MI involves both the anterior wall (V2-V4) and the lateral wall (V5-V6,
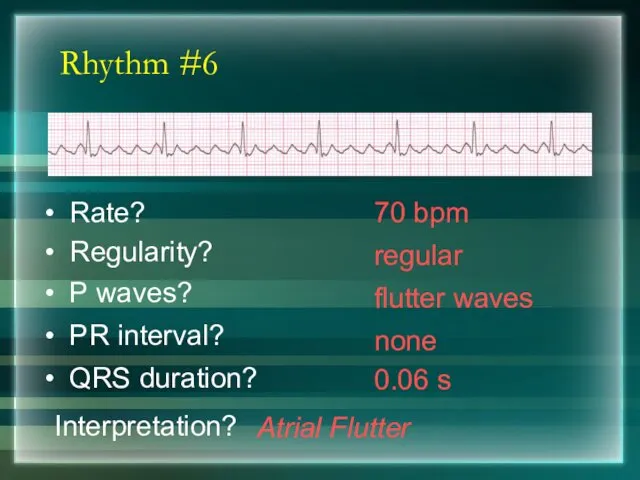
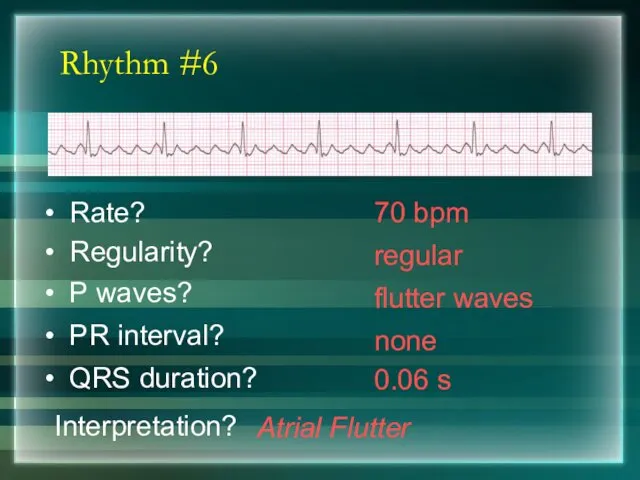
- 108. Rhythm #6 70 bpm Rate? Regularity? regular flutter waves 0.06 s P waves? PR interval? none
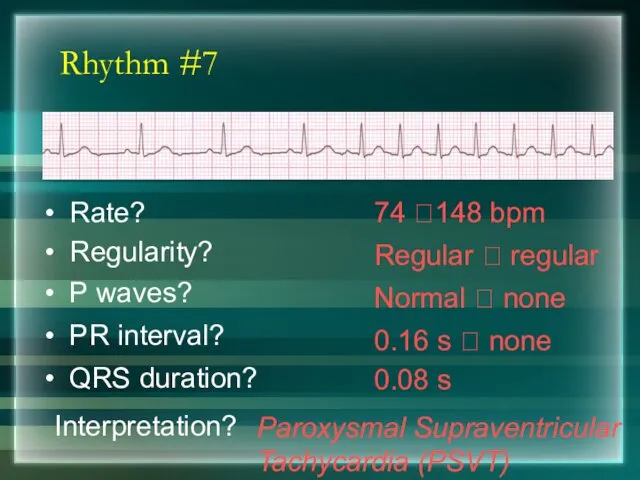
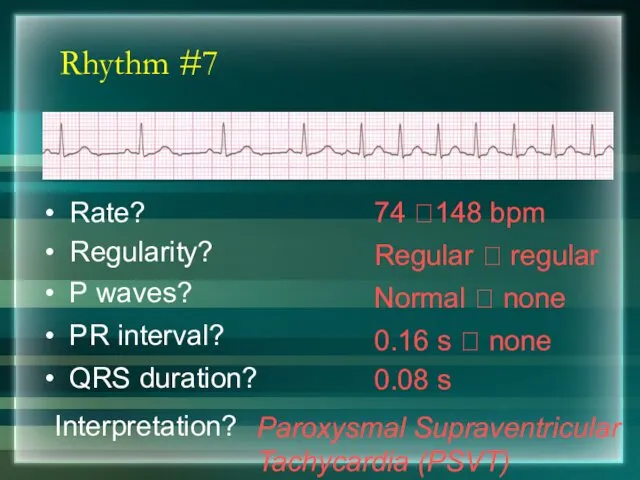
- 109. Rhythm #7 74 ?148 bpm Rate? Regularity? Regular ? regular Normal ? none 0.08 s P
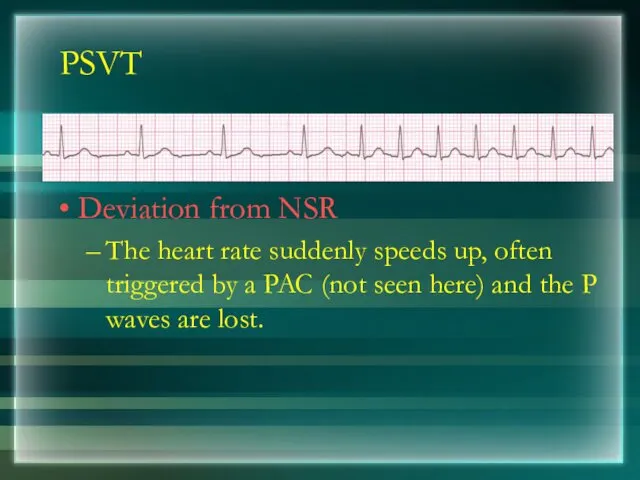
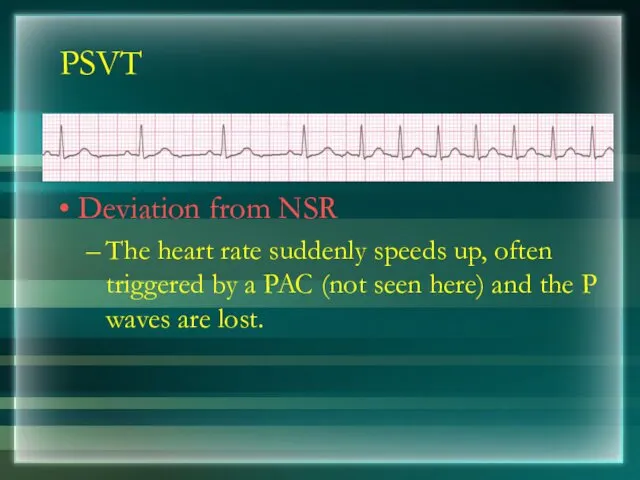
- 110. PSVT Deviation from NSR The heart rate suddenly speeds up, often triggered by a PAC (not
- 111. Ventricular Arrhythmias Ventricular Tachycardia Ventricular Fibrillation
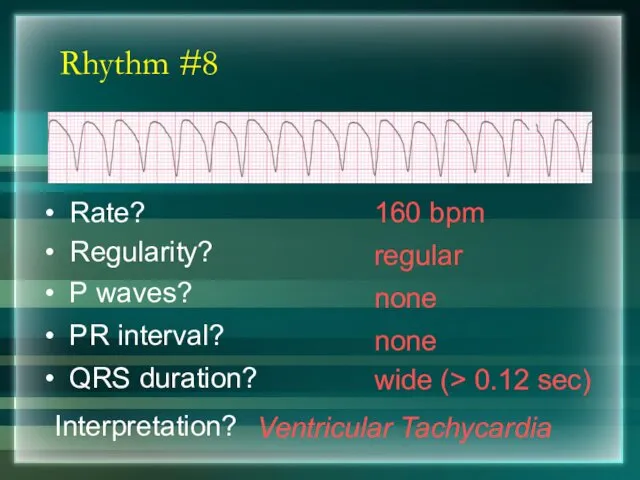
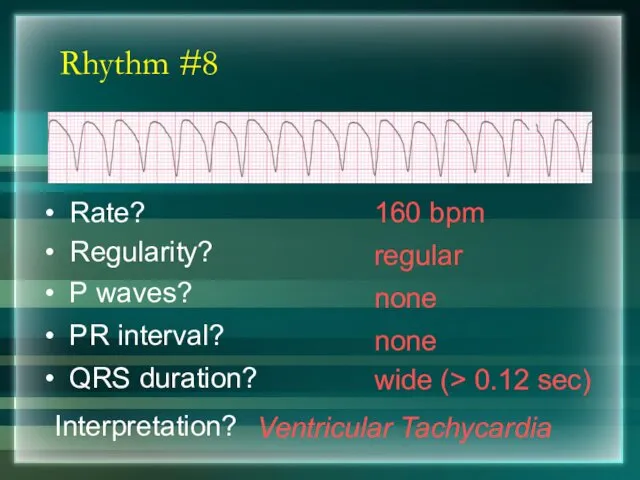
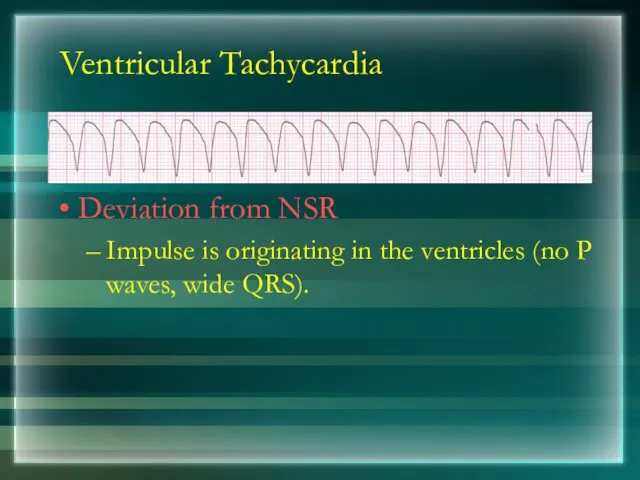
- 112. Rhythm #8 160 bpm Rate? Regularity? regular none wide (> 0.12 sec) P waves? PR interval?
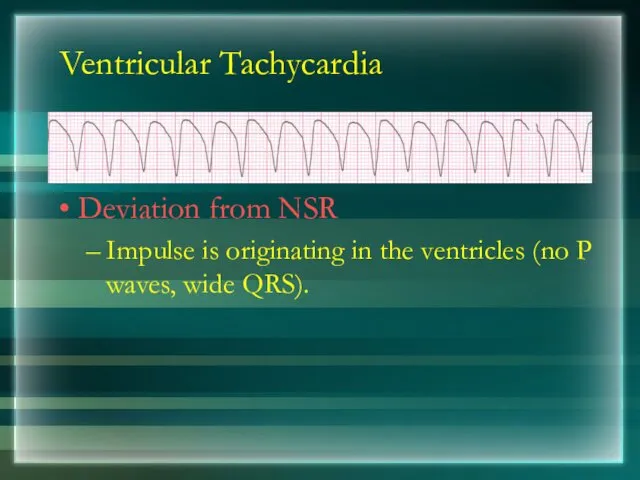
- 113. Ventricular Tachycardia Deviation from NSR Impulse is originating in the ventricles (no P waves, wide QRS).
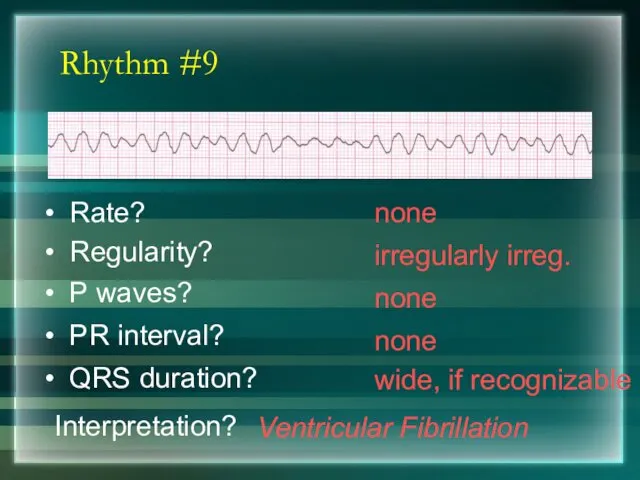
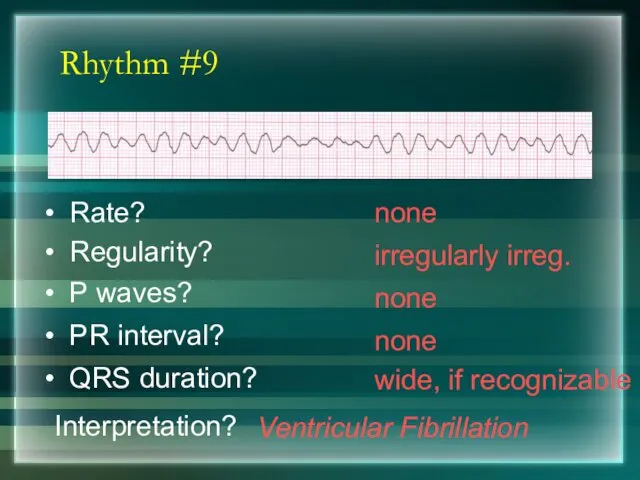
- 114. Rhythm #9 none Rate? Regularity? irregularly irreg. none wide, if recognizable P waves? PR interval? none
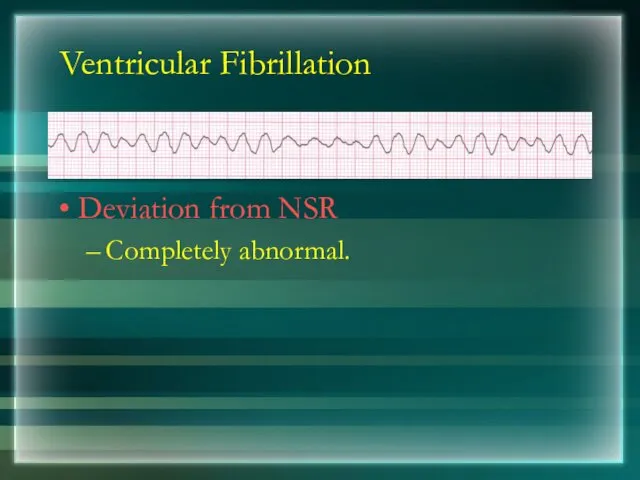
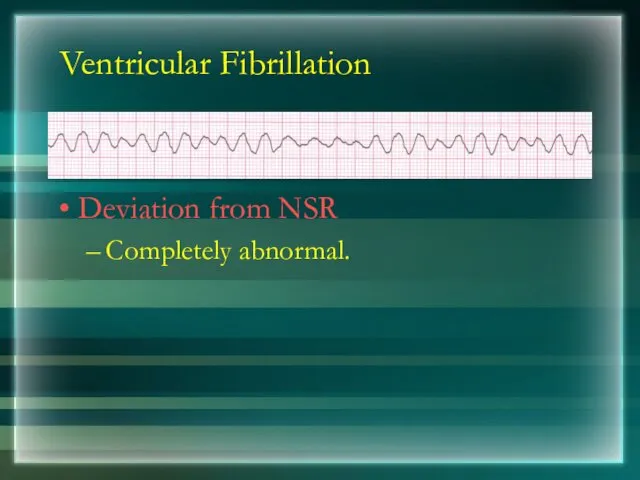
- 115. Ventricular Fibrillation Deviation from NSR Completely abnormal.
- 116. Arrhythmia Formation Arrhythmias can arise from problems in the: Sinus node Atrial cells AV junction Ventricular
- 117. SA Node Problems The SA Node can: fire too slow fire too fast Sinus Bradycardia Sinus
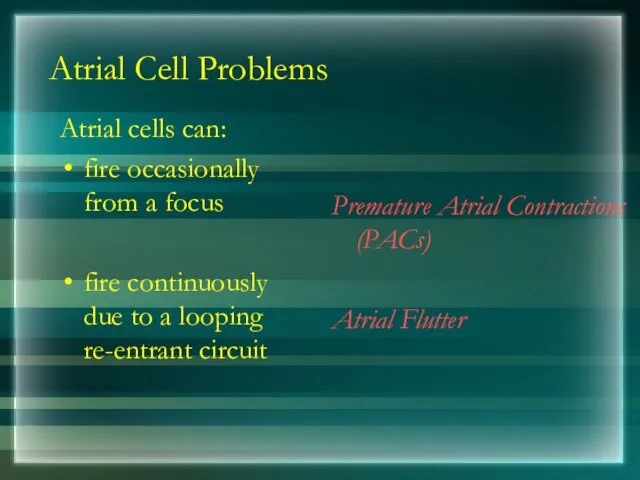
- 118. Atrial Cell Problems Atrial cells can: fire occasionally from a focus fire continuously due to a
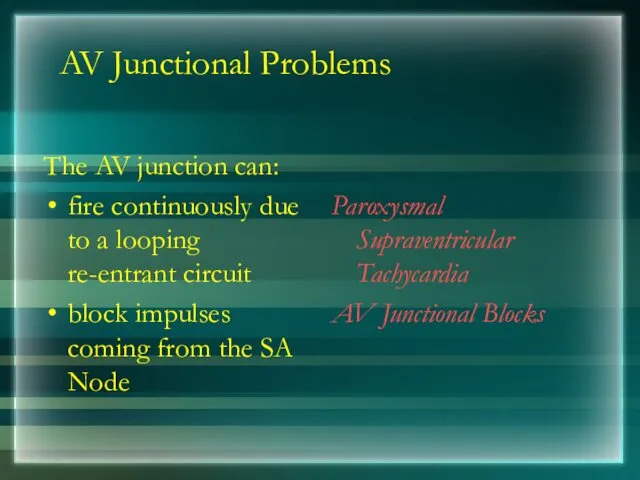
- 119. AV Junctional Problems The AV junction can: fire continuously due to a looping re-entrant circuit block
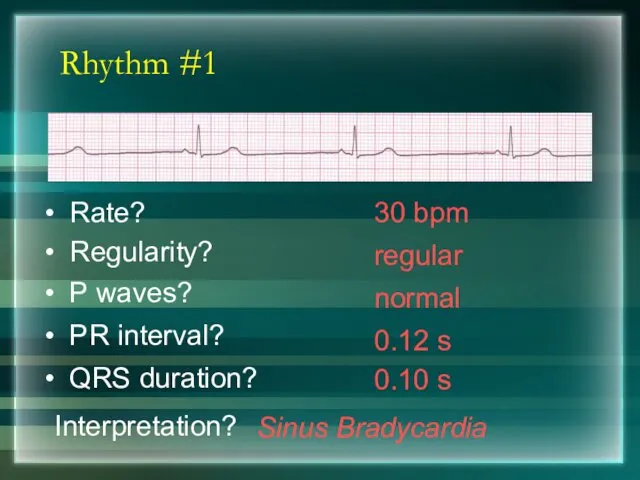
- 120. Rhythm #1 30 bpm Rate? Regularity? regular normal 0.10 s P waves? PR interval? 0.12 s
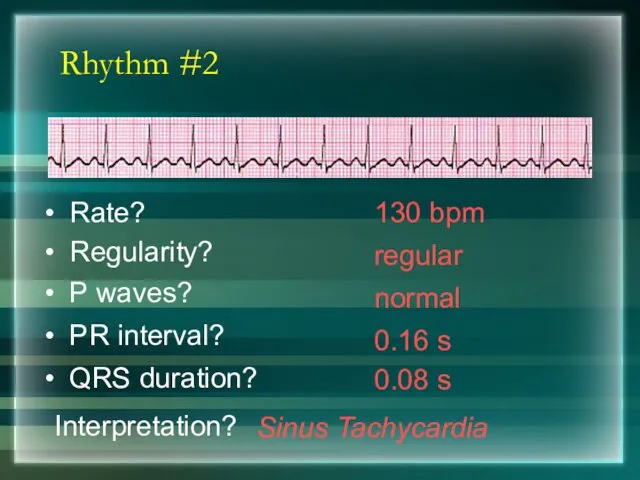
- 121. Rhythm #2 130 bpm Rate? Regularity? regular normal 0.08 s P waves? PR interval? 0.16 s
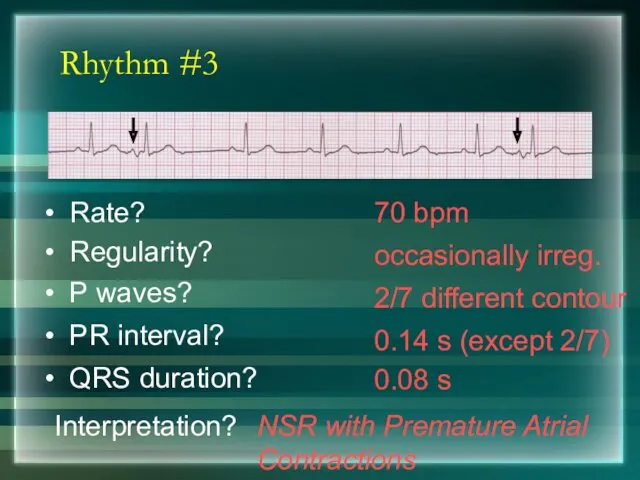
- 122. Rhythm #3 70 bpm Rate? Regularity? occasionally irreg. 2/7 different contour 0.08 s P waves? PR
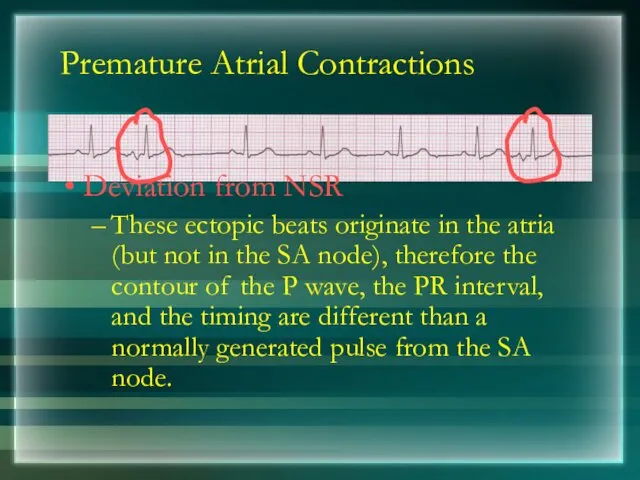
- 123. Premature Atrial Contractions Deviation from NSR These ectopic beats originate in the atria (but not in
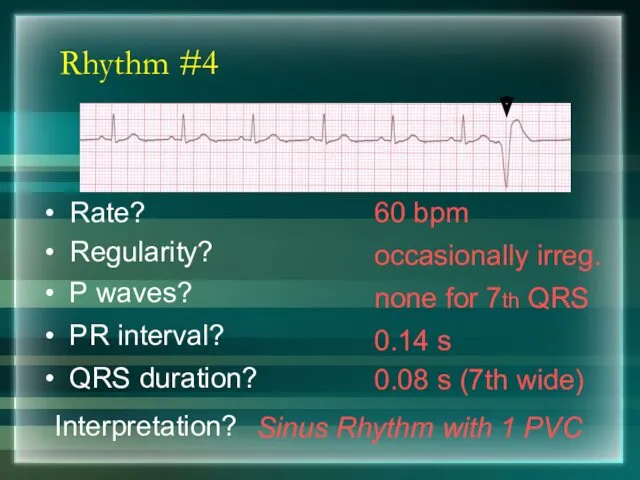
- 124. Rhythm #4 60 bpm Rate? Regularity? occasionally irreg. none for 7th QRS 0.08 s (7th wide)
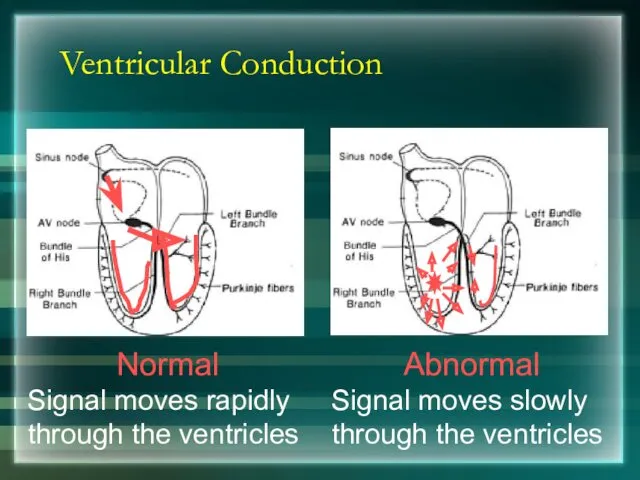
- 125. Ventricular Conduction Normal Signal moves rapidly through the ventricles Abnormal Signal moves slowly through the ventricles
- 126. AV Nodal Blocks 1st Degree AV Block 2nd Degree AV Block, Type I 2nd Degree AV
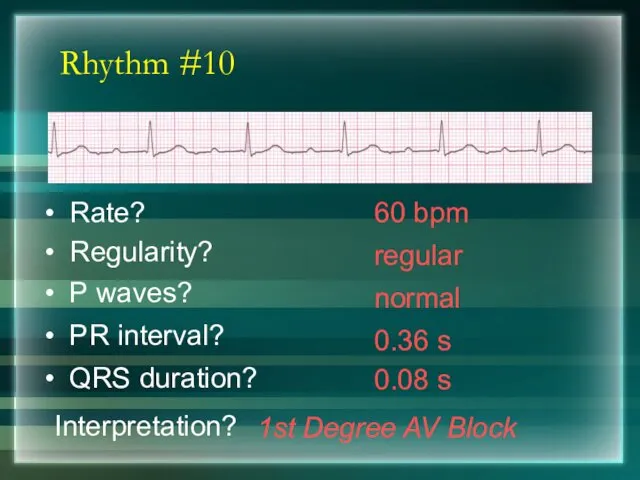
- 127. Rhythm #10 60 bpm Rate? Regularity? regular normal 0.08 s P waves? PR interval? 0.36 s
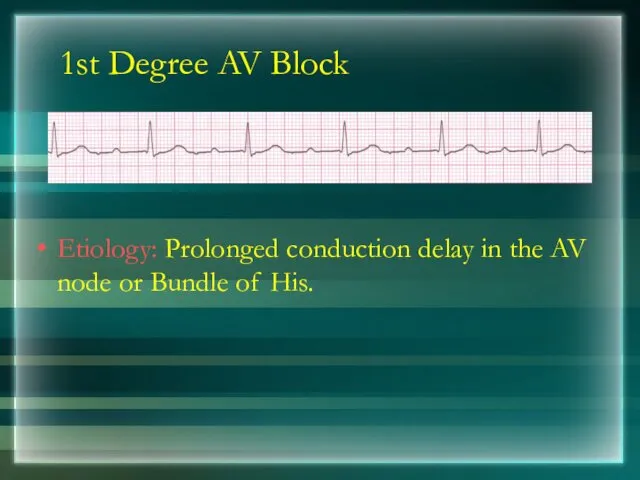
- 128. 1st Degree AV Block Etiology: Prolonged conduction delay in the AV node or Bundle of His.
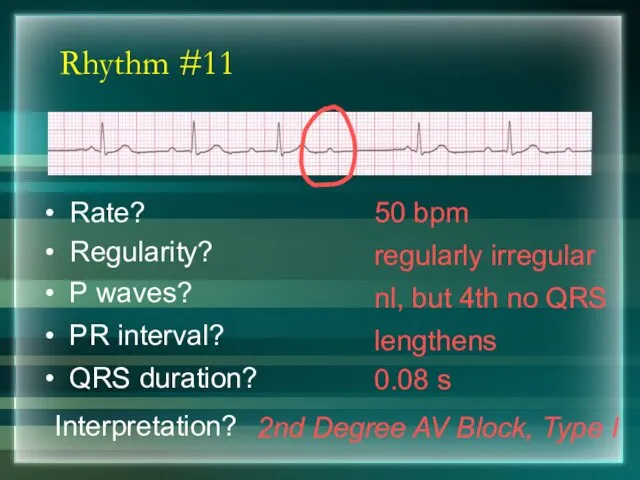
- 129. Rhythm #11 50 bpm Rate? Regularity? regularly irregular nl, but 4th no QRS 0.08 s P
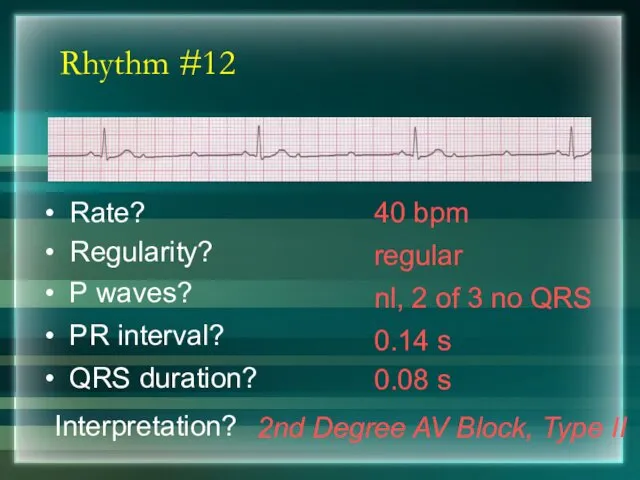
- 130. Rhythm #12 40 bpm Rate? Regularity? regular nl, 2 of 3 no QRS 0.08 s P
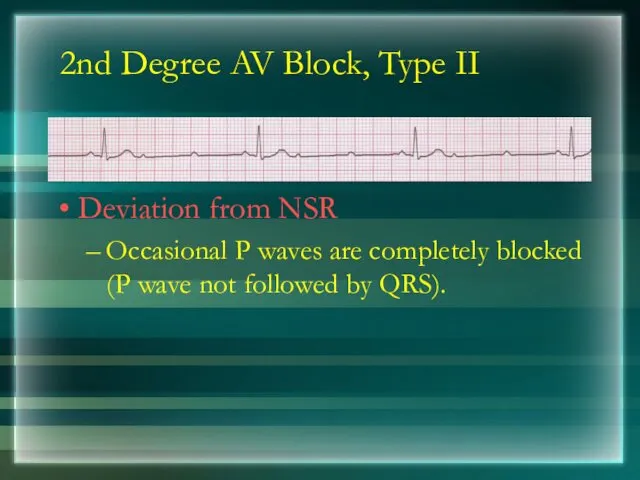
- 131. 2nd Degree AV Block, Type II Deviation from NSR Occasional P waves are completely blocked (P
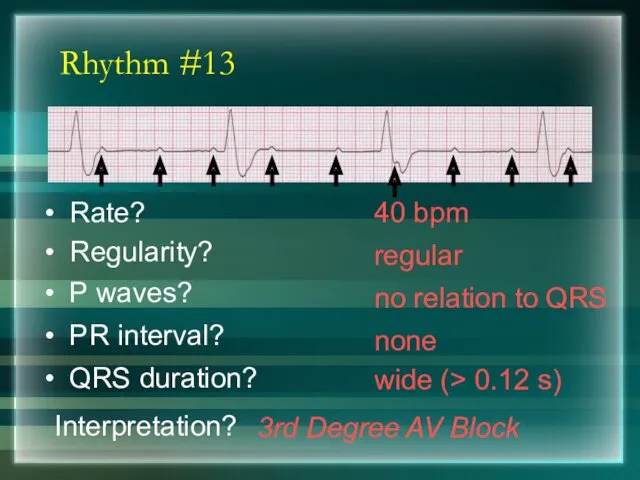
- 132. Rhythm #13 40 bpm Rate? Regularity? regular no relation to QRS wide (> 0.12 s) P
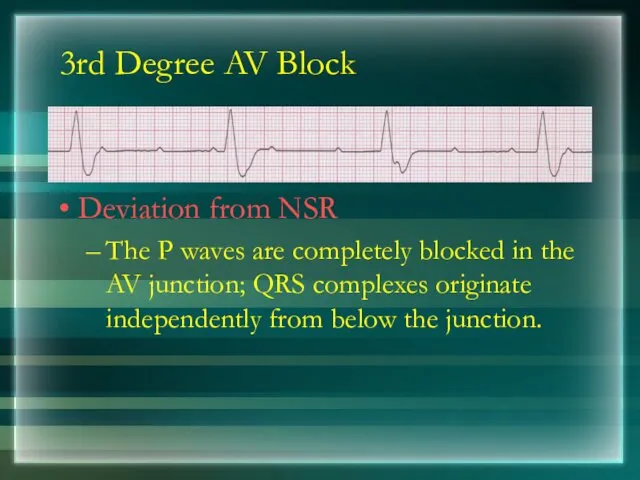
- 133. 3rd Degree AV Block Deviation from NSR The P waves are completely blocked in the AV
- 134. Supraventricular Arrhythmias Atrial Fibrillation Atrial Flutter Paroxysmal Supraventricular Tachycardia
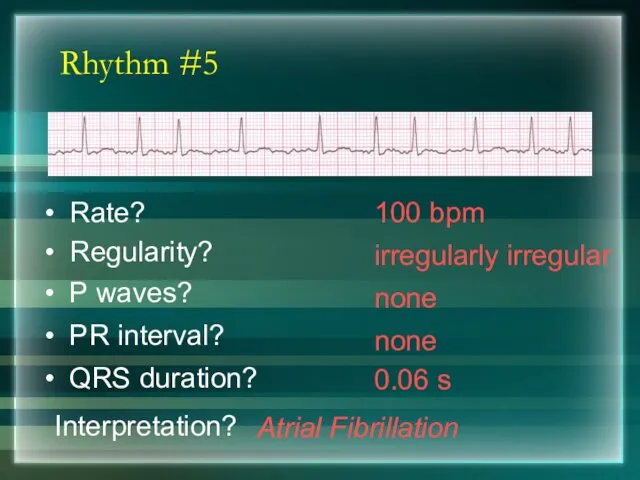
- 135. Rhythm #5 100 bpm Rate? Regularity? irregularly irregular none 0.06 s P waves? PR interval? none
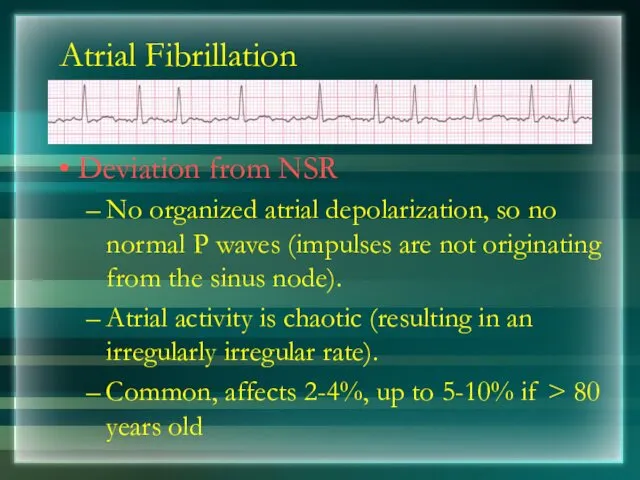
- 136. Atrial Fibrillation Deviation from NSR No organized atrial depolarization, so no normal P waves (impulses are
- 137. Rhythm #6 70 bpm Rate? Regularity? regular flutter waves 0.06 s P waves? PR interval? none
- 138. Rhythm #7 74 ?148 bpm Rate? Regularity? Regular ? regular Normal ? none 0.08 s P
- 139. PSVT Deviation from NSR The heart rate suddenly speeds up, often triggered by a PAC (not
- 140. Ventricular Arrhythmias Ventricular Tachycardia Ventricular Fibrillation
- 141. Rhythm #8 160 bpm Rate? Regularity? regular none wide (> 0.12 sec) P waves? PR interval?
- 142. Ventricular Tachycardia Deviation from NSR Impulse is originating in the ventricles (no P waves, wide QRS).
- 143. Rhythm #9 none Rate? Regularity? irregularly irreg. none wide, if recognizable P waves? PR interval? none
- 144. Ventricular Fibrillation Deviation from NSR Completely abnormal.
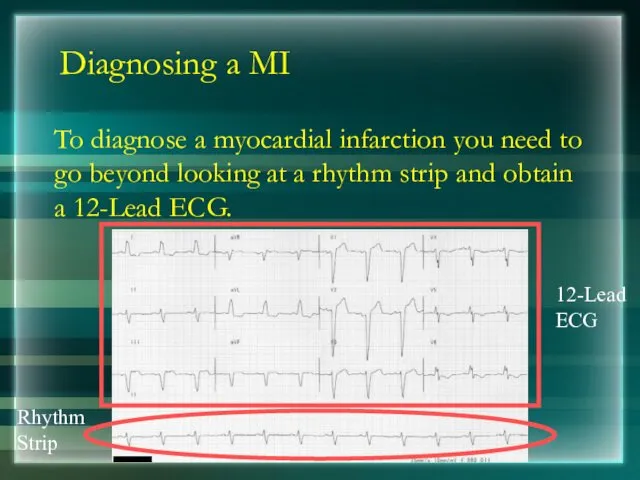
- 145. Diagnosing a MI To diagnose a myocardial infarction you need to go beyond looking at a
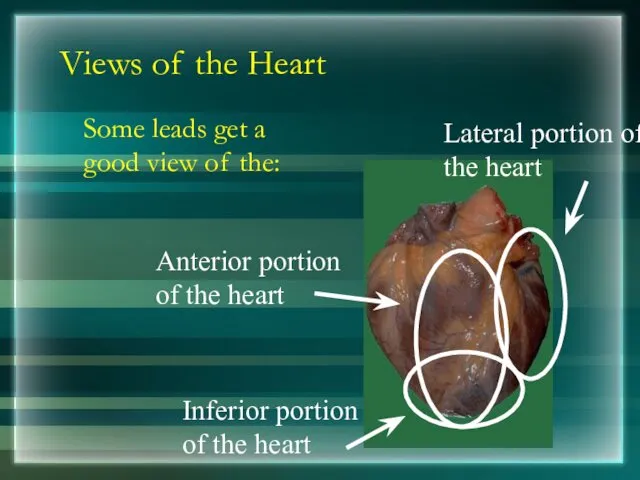
- 146. Views of the Heart Some leads get a good view of the: Anterior portion of the
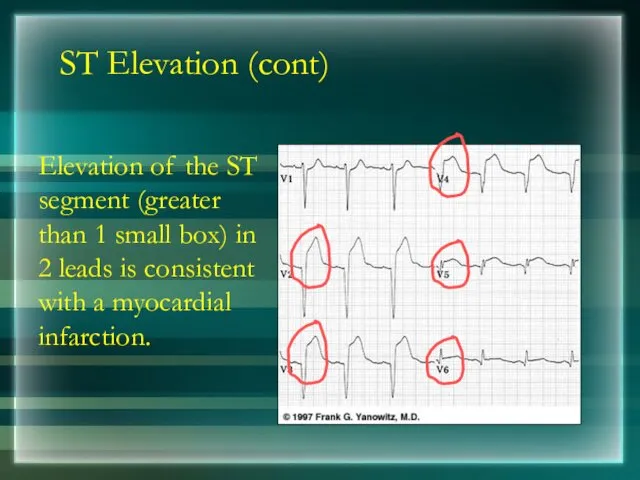
- 147. ST Elevation One way to diagnose an acute MI is to look for elevation of the
- 148. ST Elevation (cont) Elevation of the ST segment (greater than 1 small box) in 2 leads
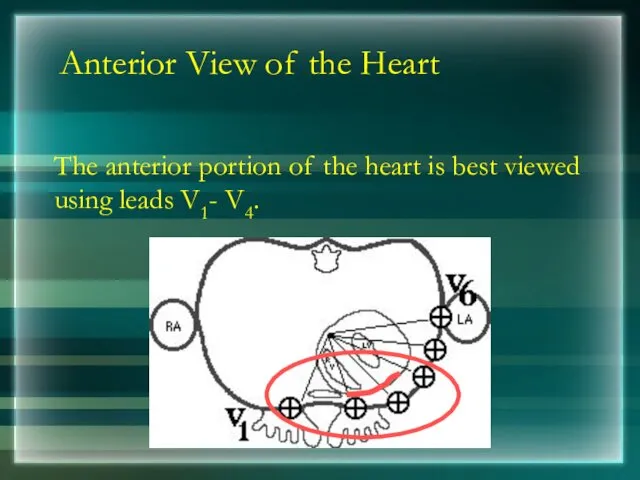
- 149. Anterior View of the Heart The anterior portion of the heart is best viewed using leads
- 150. Anterior Myocardial Infarction If you see changes in leads V1 - V4 that are consistent with
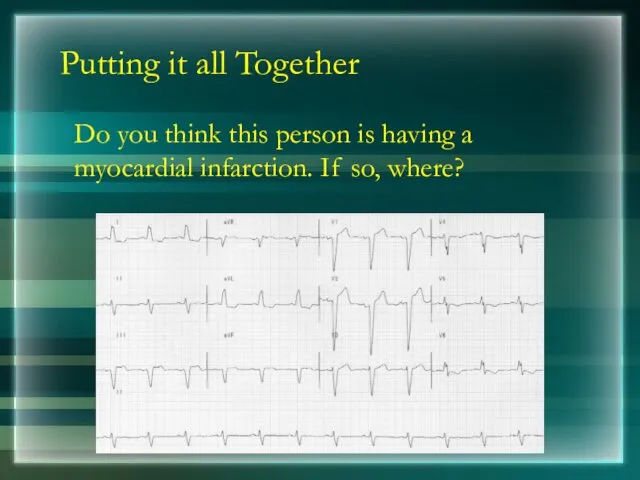
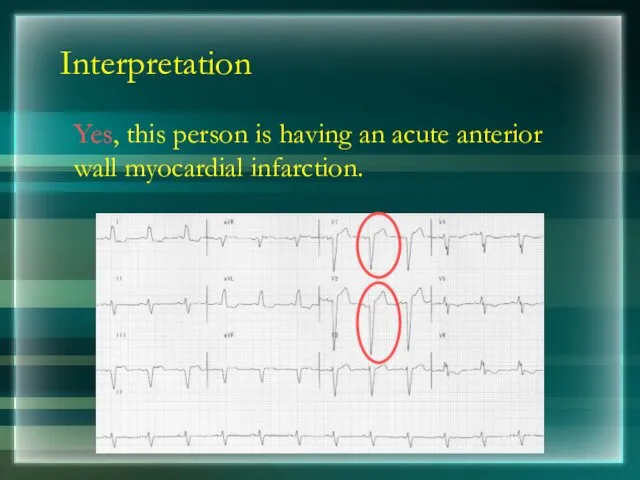
- 151. Putting it all Together Do you think this person is having a myocardial infarction. If so,
- 152. Interpretation Yes, this person is having an acute anterior wall myocardial infarction.
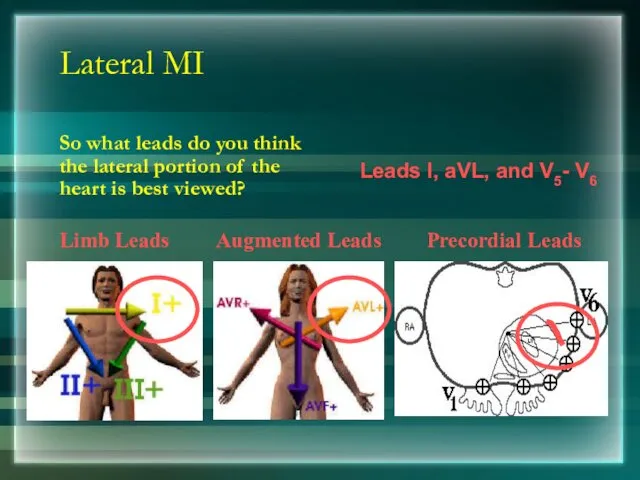
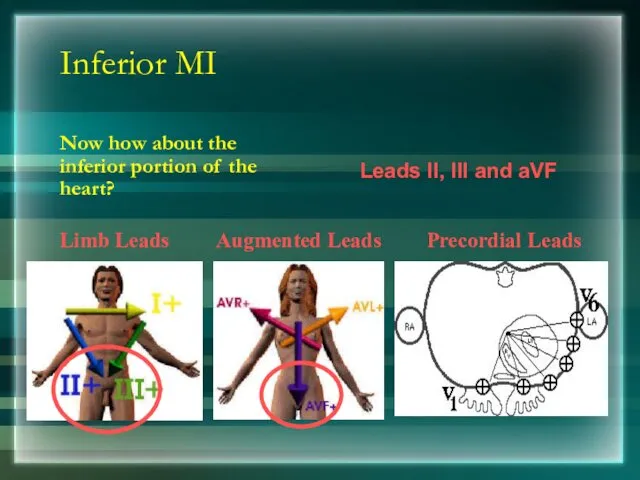
- 153. Other MI Locations Now that you know where to look for an anterior wall myocardial infarction
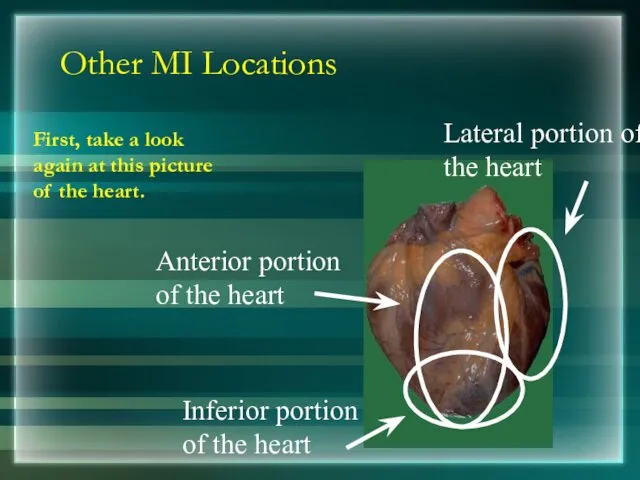
- 154. Other MI Locations First, take a look again at this picture of the heart.
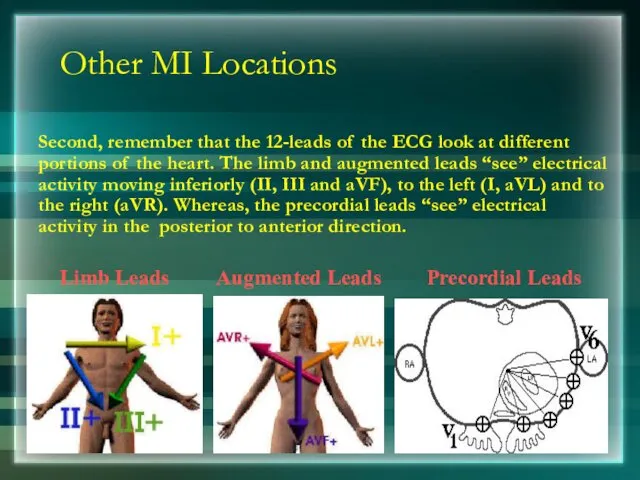
- 155. Other MI Locations Second, remember that the 12-leads of the ECG look at different portions of
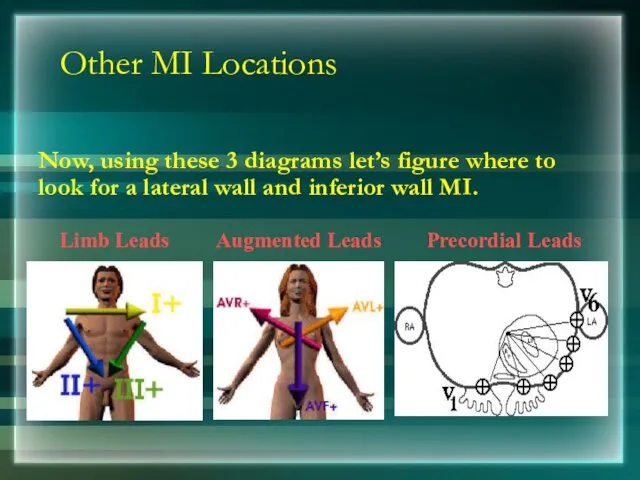
- 156. Other MI Locations Now, using these 3 diagrams let’s figure where to look for a lateral
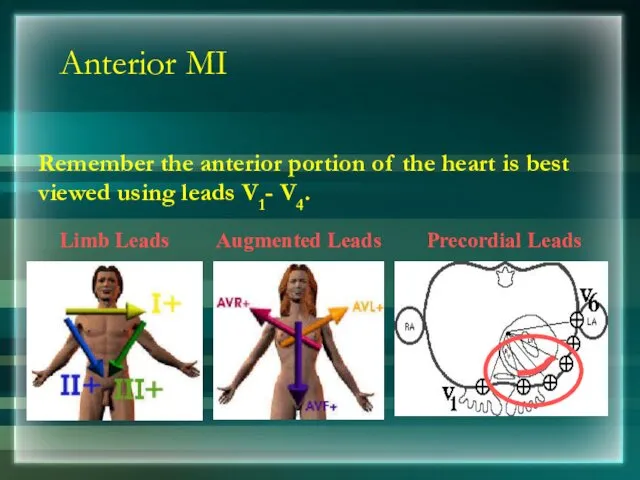
- 157. Anterior MI Remember the anterior portion of the heart is best viewed using leads V1- V4.
- 158. Lateral MI So what leads do you think the lateral portion of the heart is best
- 159. Inferior MI Now how about the inferior portion of the heart? Limb Leads Augmented Leads Precordial
- 160. Putting it all Together Now, where do you think this person is having a myocardial infarction?
- 161. Inferior Wall MI This is an inferior MI. Note the ST elevation in leads II, III
- 162. Putting it all Together How about now?
- 163. Anterolateral MI This person’s MI involves both the anterior wall (V2-V4) and the lateral wall (V5-V6,
- 164. RIGHT ATRIAL ENLARGEMENT
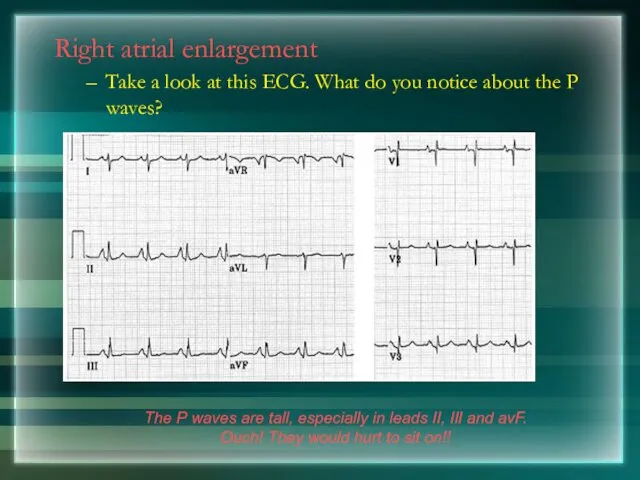
- 165. Right atrial enlargement Take a look at this ECG. What do you notice about the P
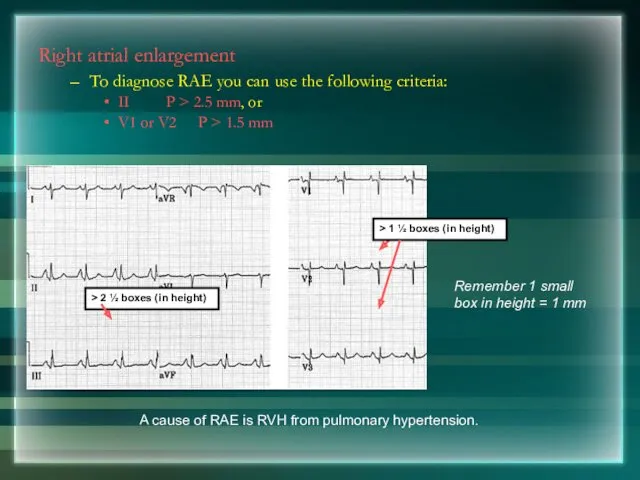
- 166. Right atrial enlargement To diagnose RAE you can use the following criteria: II P > 2.5
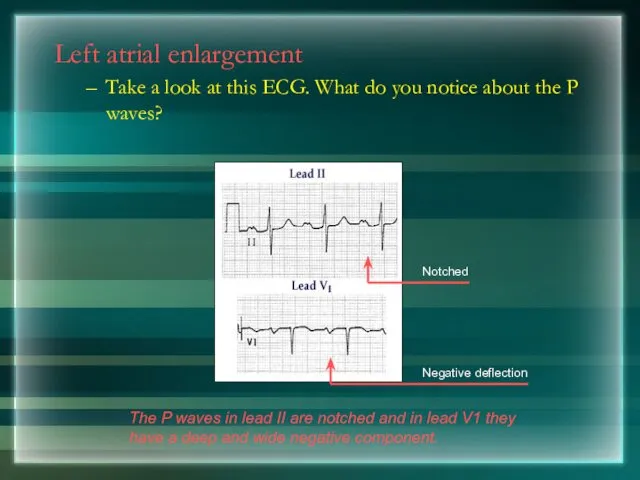
- 167. Left atrial enlargement Take a look at this ECG. What do you notice about the P
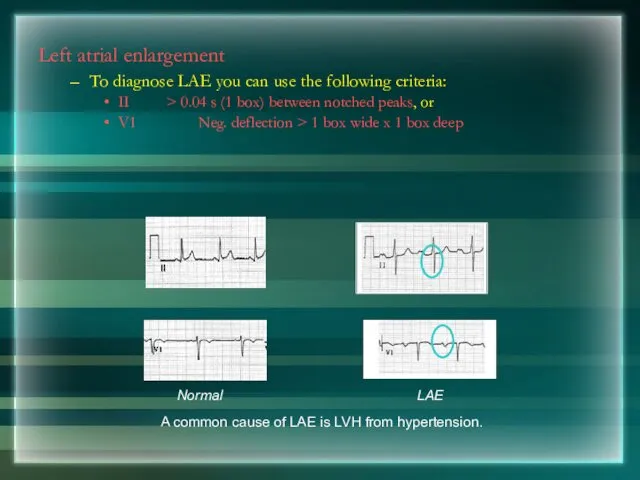
- 168. Left atrial enlargement To diagnose LAE you can use the following criteria: II > 0.04 s
- 169. Left Ventricular Hypertrophy
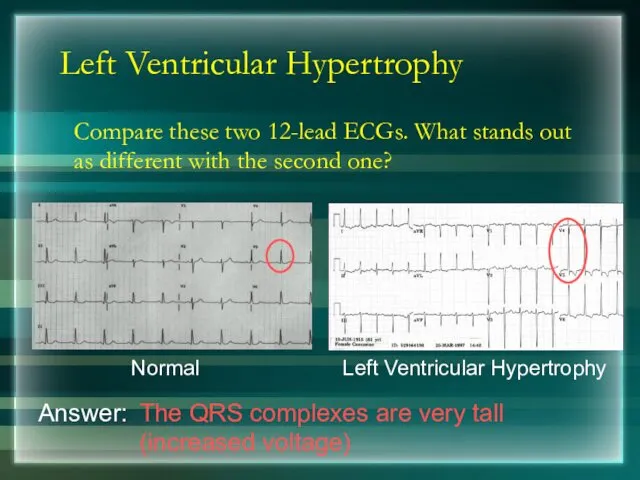
- 170. Left Ventricular Hypertrophy Compare these two 12-lead ECGs. What stands out as different with the second
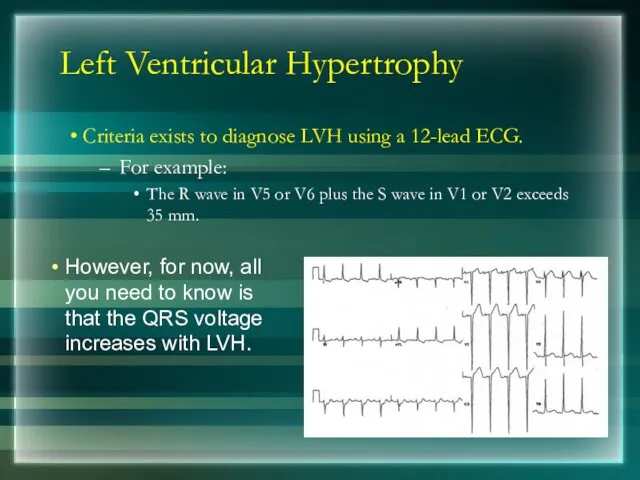
- 171. Left Ventricular Hypertrophy Criteria exists to diagnose LVH using a 12-lead ECG. For example: The R
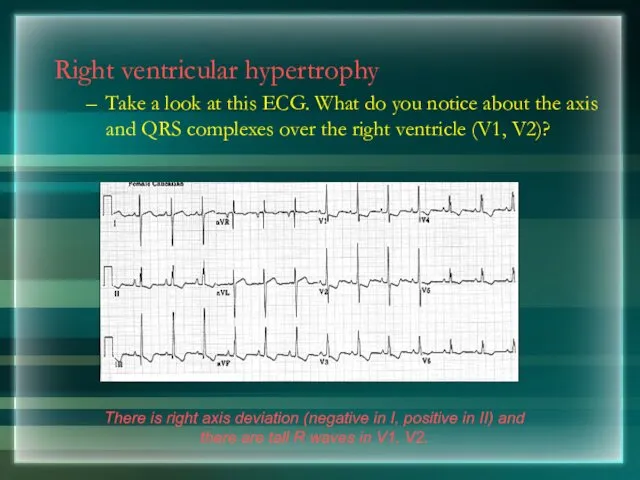
- 172. Right ventricular hypertrophy Take a look at this ECG. What do you notice about the axis
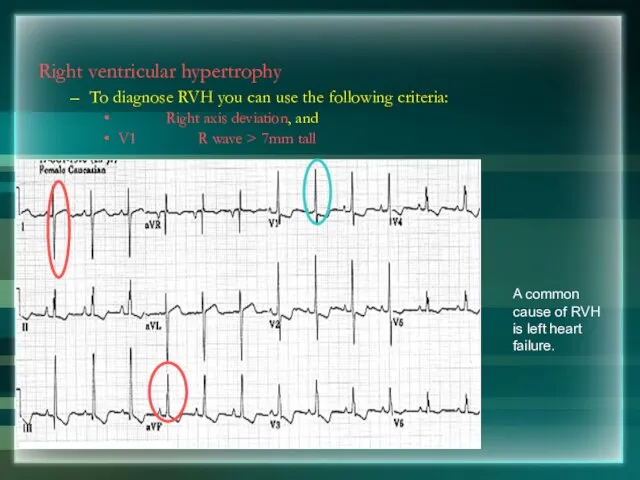
- 173. Right ventricular hypertrophy To diagnose RVH you can use the following criteria: Right axis deviation, and
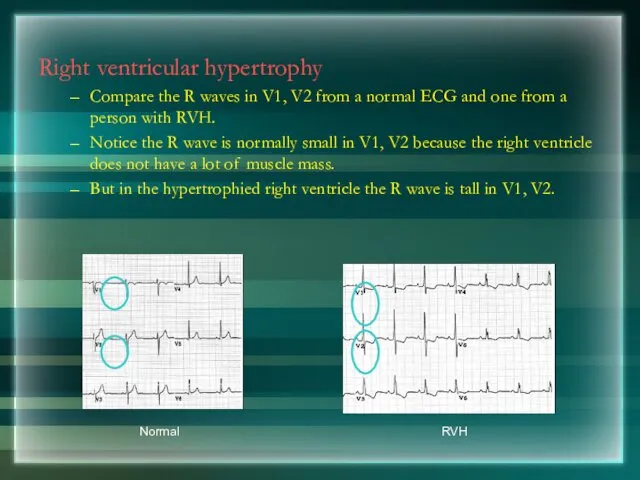
- 174. Right ventricular hypertrophy Compare the R waves in V1, V2 from a normal ECG and one
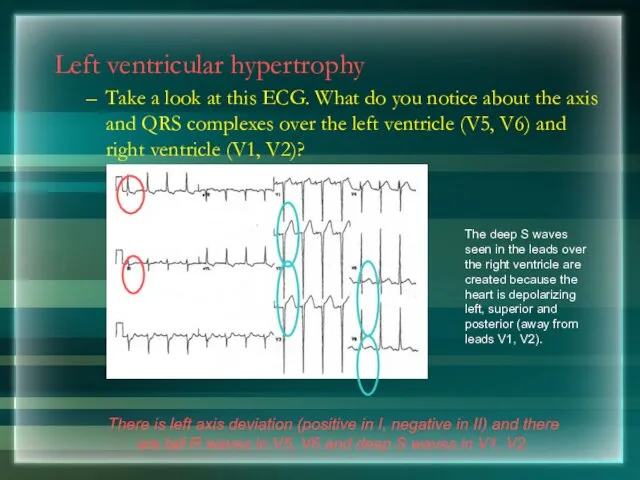
- 175. Left ventricular hypertrophy Take a look at this ECG. What do you notice about the axis
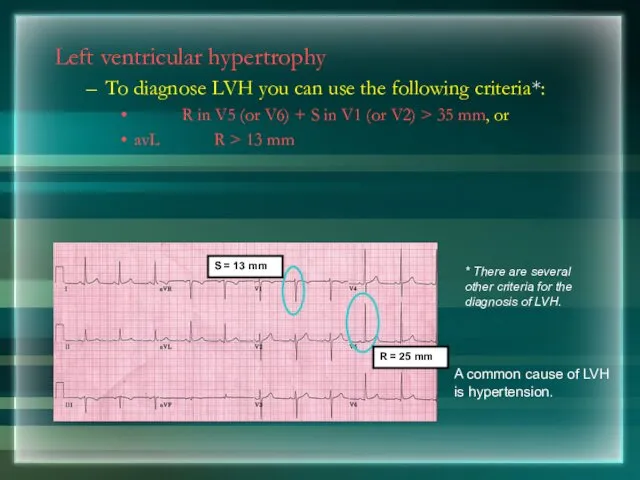
- 176. Left ventricular hypertrophy To diagnose LVH you can use the following criteria*: R in V5 (or
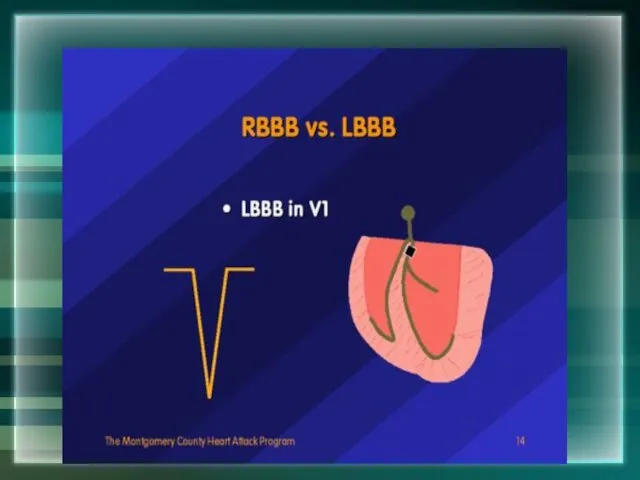
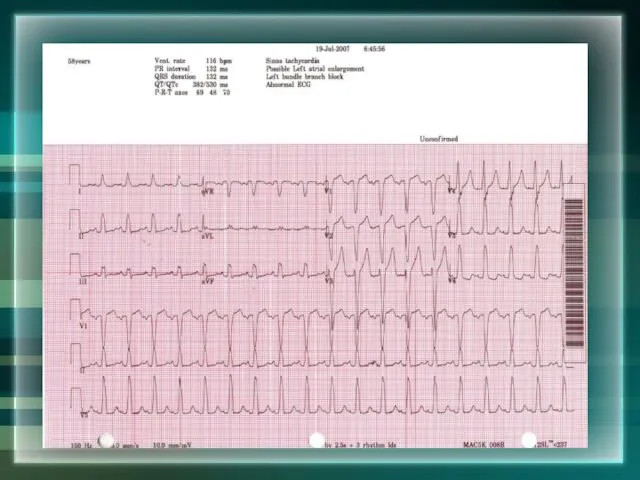
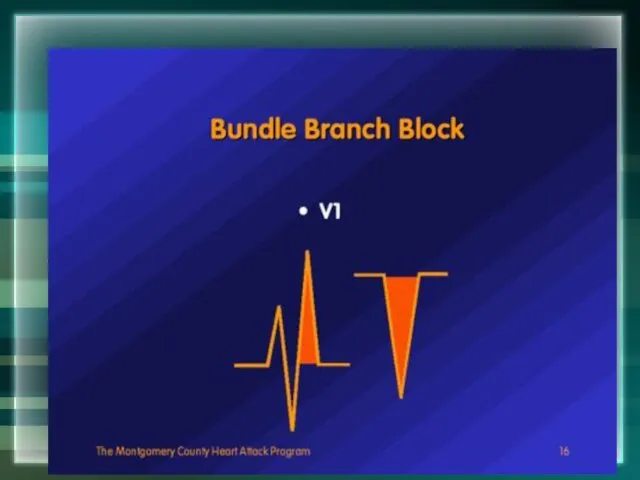
- 177. Bundle Branch Blocks
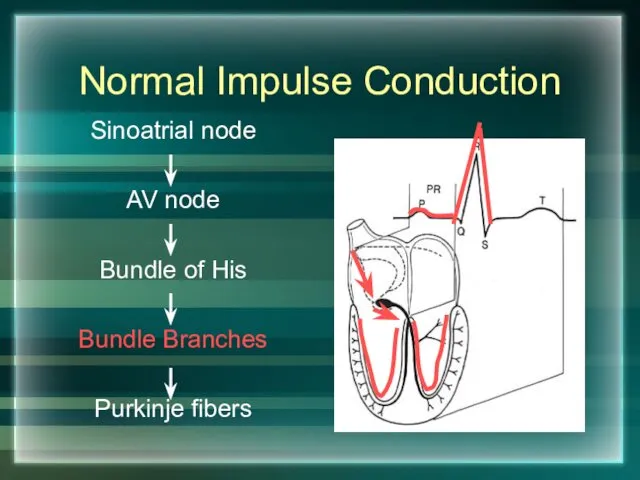
- 178. Normal Impulse Conduction Sinoatrial node AV node Bundle of His Bundle Branches Purkinje fibers
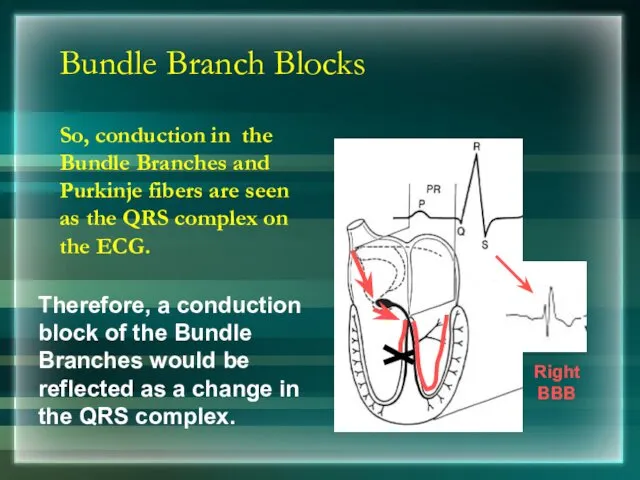
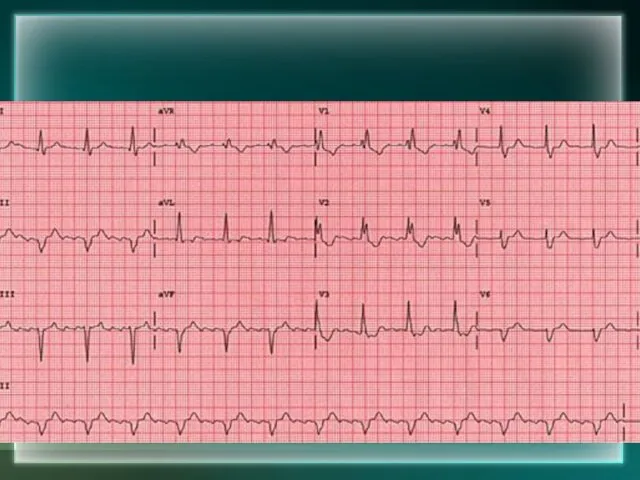
- 179. Bundle Branch Blocks So, conduction in the Bundle Branches and Purkinje fibers are seen as the
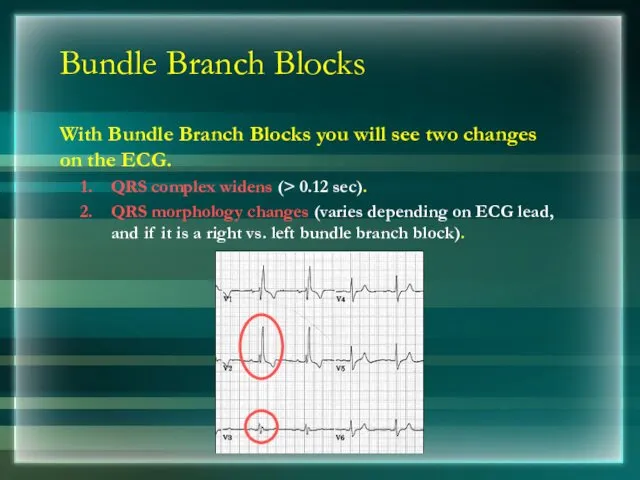
- 180. Bundle Branch Blocks With Bundle Branch Blocks you will see two changes on the ECG. QRS
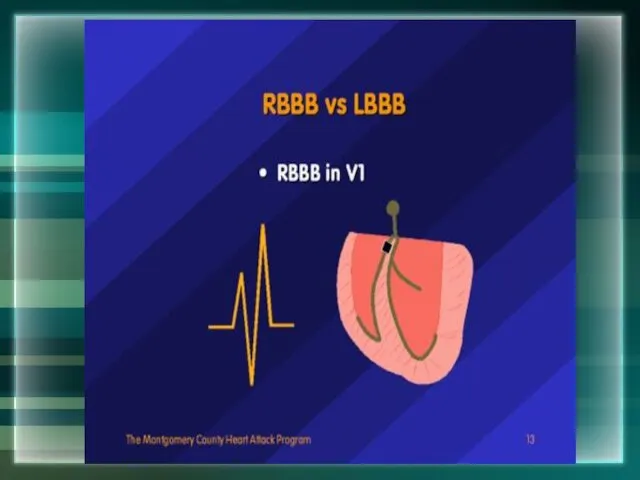
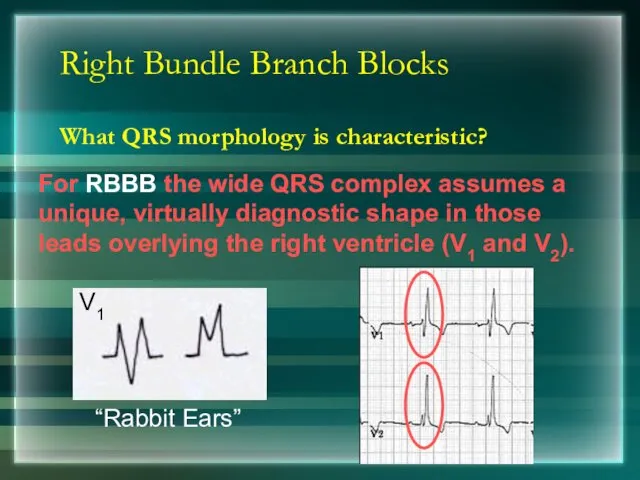
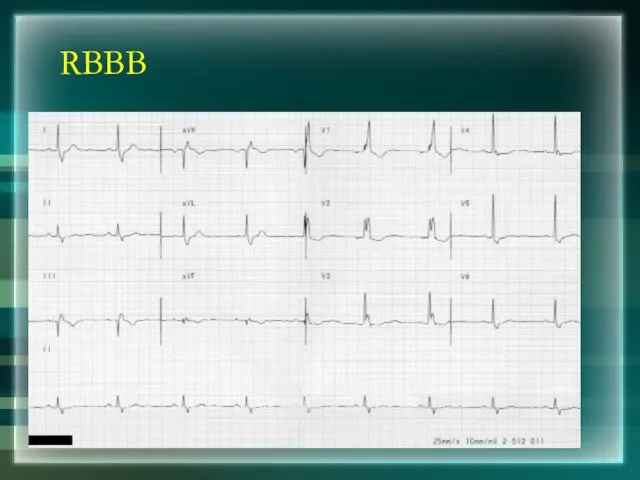
- 182. Right Bundle Branch Blocks What QRS morphology is characteristic?
- 183. RBBB
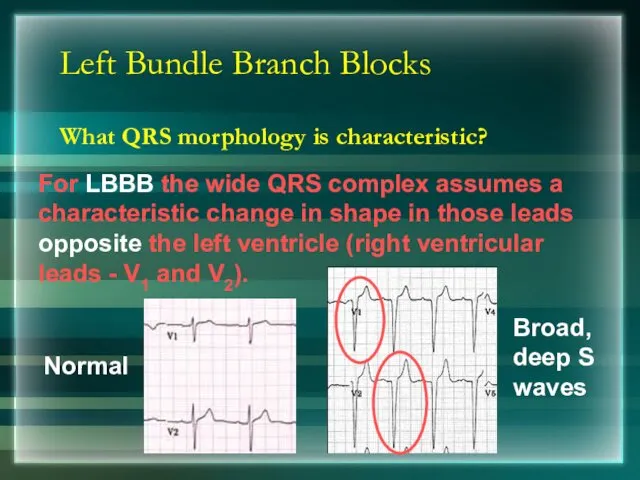
- 185. Left Bundle Branch Blocks What QRS morphology is characteristic? Normal
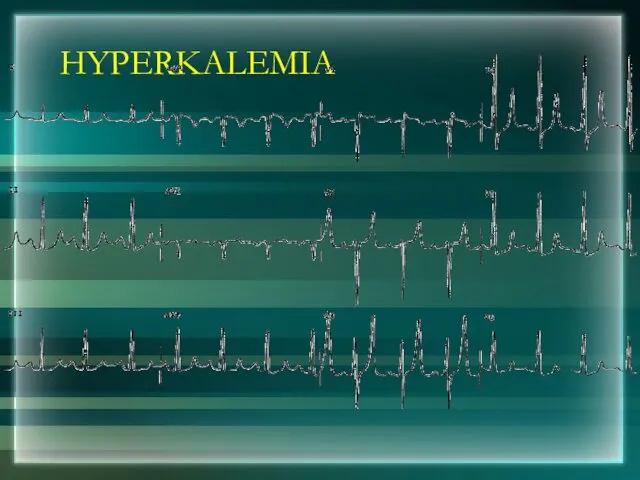
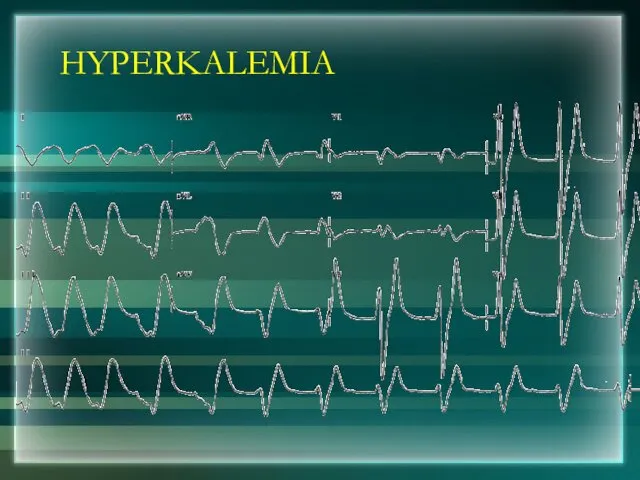
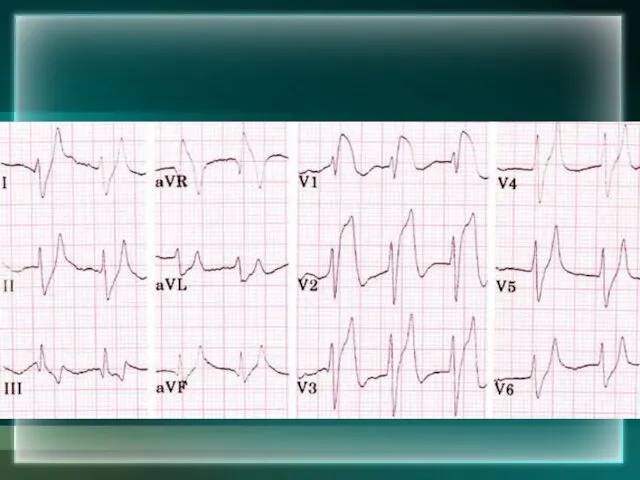
- 191. HYPERKALEMIA
- 192. HYPERKALEMIA
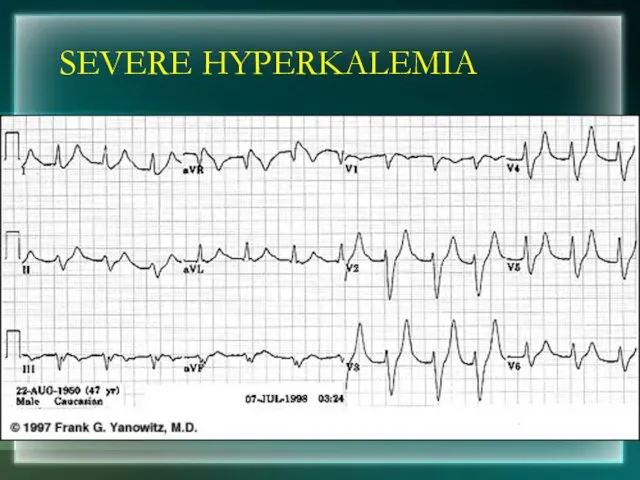
- 194. SEVERE HYPERKALEMIA
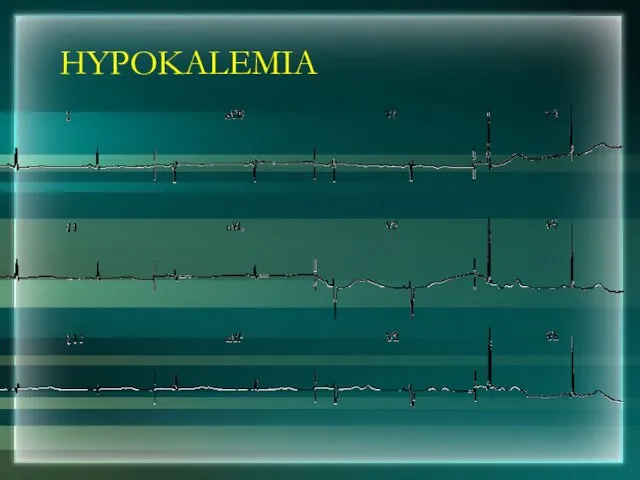
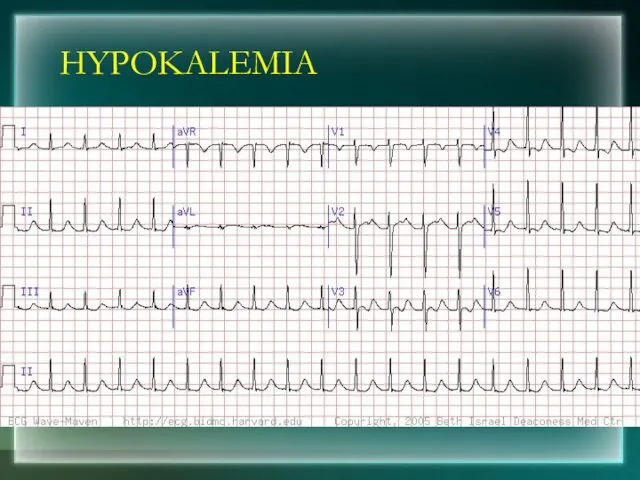
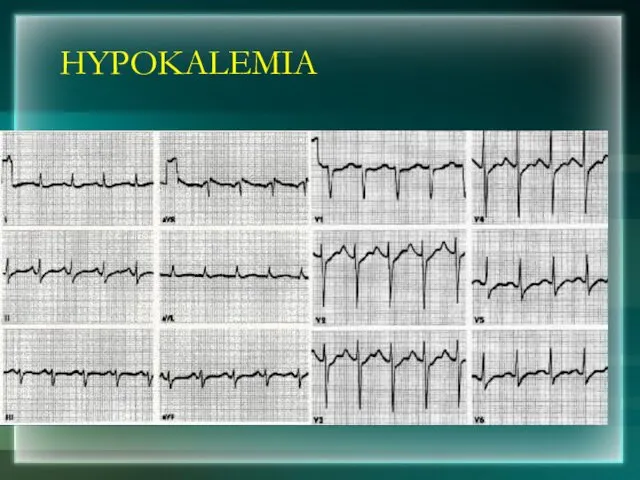
- 195. HYPOKALEMIA
- 196. HYPOKALEMIA
- 197. HYPOKALEMIA
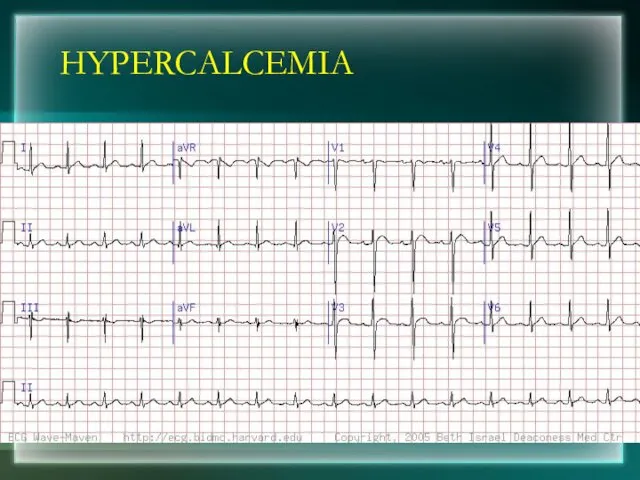
- 198. HYPERCALCEMIA
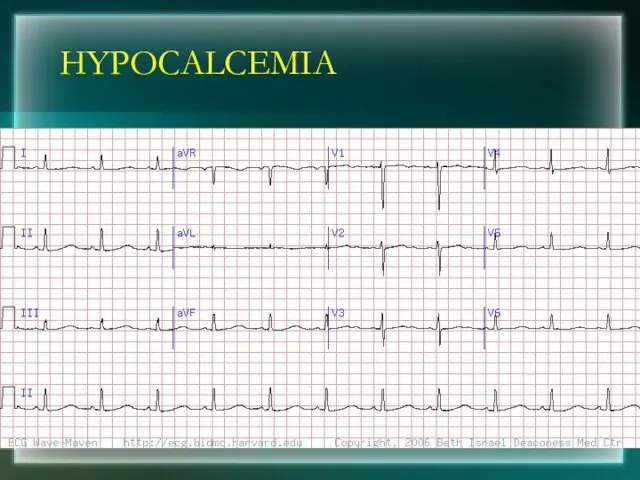
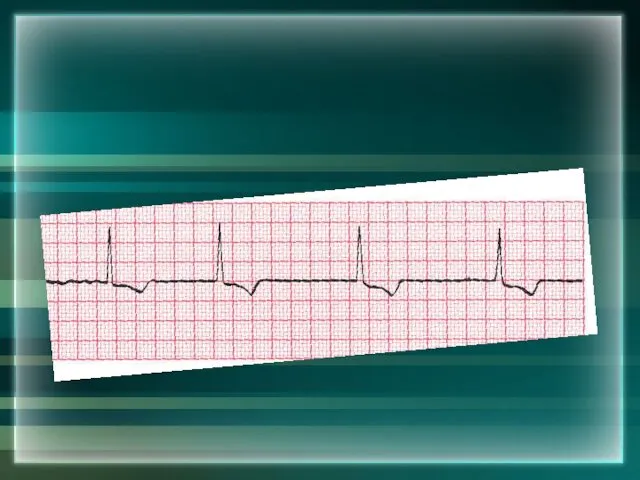
- 199. HYPOCALCEMIA
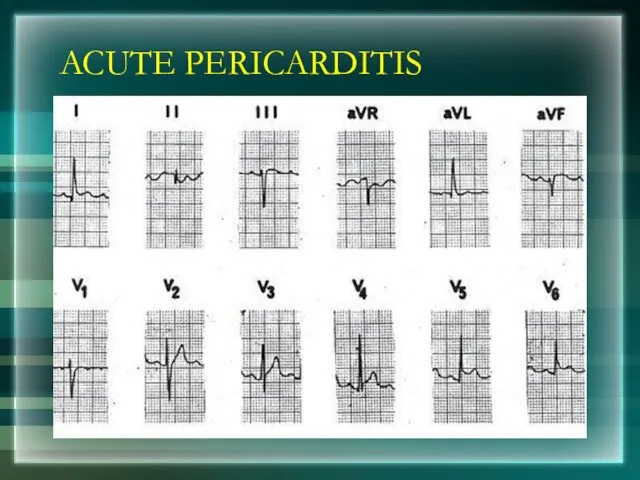
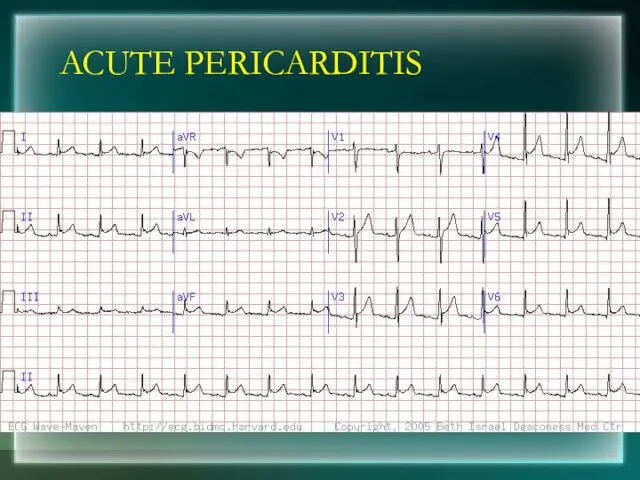
- 201. ACUTE PERICARDITIS
- 202. ACUTE PERICARDITIS
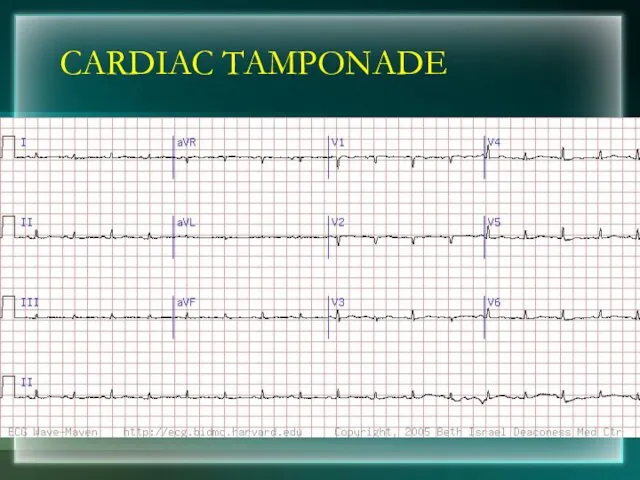
- 203. CARDIAC TAMPONADE
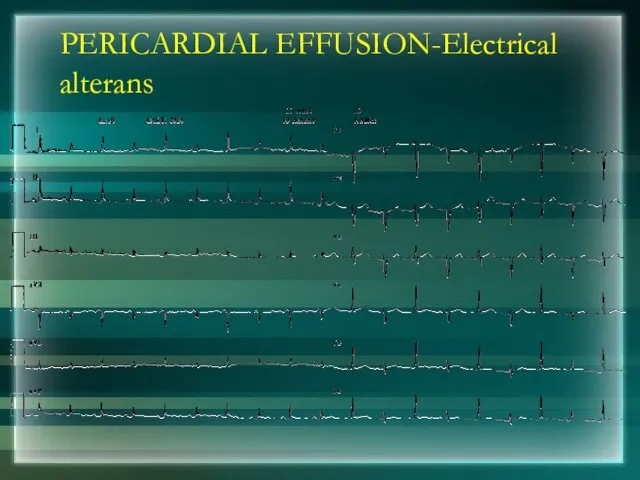
- 204. PERICARDIAL EFFUSION-Electrical alterans
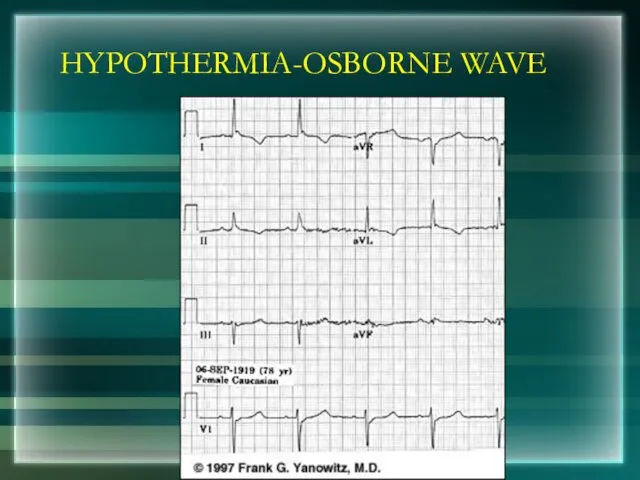
- 205. HYPOTHERMIA-OSBORNE WAVE
- 207. Скачать презентацию

 Здоровое питание. Что такое здоровое питание?
Здоровое питание. Что такое здоровое питание? Пиелонефрит. Классификация
Пиелонефрит. Классификация Лечебно-профилактический уход при заболеваниях системы кровообращения у детей в амбулаторных условиях
Лечебно-профилактический уход при заболеваниях системы кровообращения у детей в амбулаторных условиях Ангиофарм. Обзор
Ангиофарм. Обзор Желчнокаменная болезнь у детей
Желчнокаменная болезнь у детей Острые респираторные вирусные инфекции у детей
Острые респираторные вирусные инфекции у детей Основы Лечебной физической культуры
Основы Лечебной физической культуры Мутационная теория онкогенеза
Мутационная теория онкогенеза Профилактика ОРВИ и гриппа
Профилактика ОРВИ и гриппа Болезни слюнных желез
Болезни слюнных желез Эпидемиология и диагностика туберкулеза. Пробное лечение, как метод диагностики
Эпидемиология и диагностика туберкулеза. Пробное лечение, как метод диагностики Сахарный диабет
Сахарный диабет Патогенна дія хімічних та біологічних факторів на організм. Роль спадковості в патології. (Лекція 4)
Патогенна дія хімічних та біологічних факторів на організм. Роль спадковості в патології. (Лекція 4) Сұйық аққыш композиттер. Құрамы, қасиеті, артықшылығы мен кемшіліктері. Қолдану технологиясы
Сұйық аққыш композиттер. Құрамы, қасиеті, артықшылығы мен кемшіліктері. Қолдану технологиясы Санитарно-гигиеническое обследование детского дошкольного учреждения с оформлением учебного акта обследования
Санитарно-гигиеническое обследование детского дошкольного учреждения с оформлением учебного акта обследования Особенности оказания сестринской помощи семье и пациенту с заболеваниеми сердечно-сосудистой системы
Особенности оказания сестринской помощи семье и пациенту с заболеваниеми сердечно-сосудистой системы Трофобластические опухоли матки
Трофобластические опухоли матки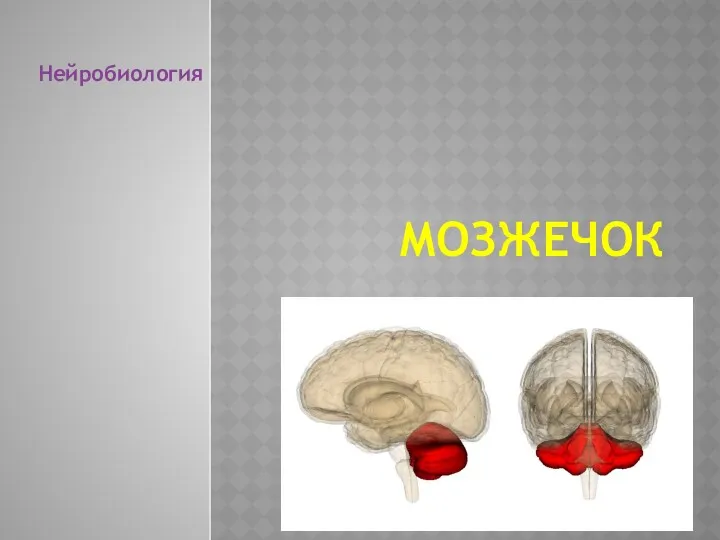 Мозжечок
Мозжечок Острая кишечная непроходимость
Острая кишечная непроходимость кесарево Нургали Гаухар
кесарево Нургали Гаухар Учение об инфекции
Учение об инфекции Вирусные диареи
Вирусные диареи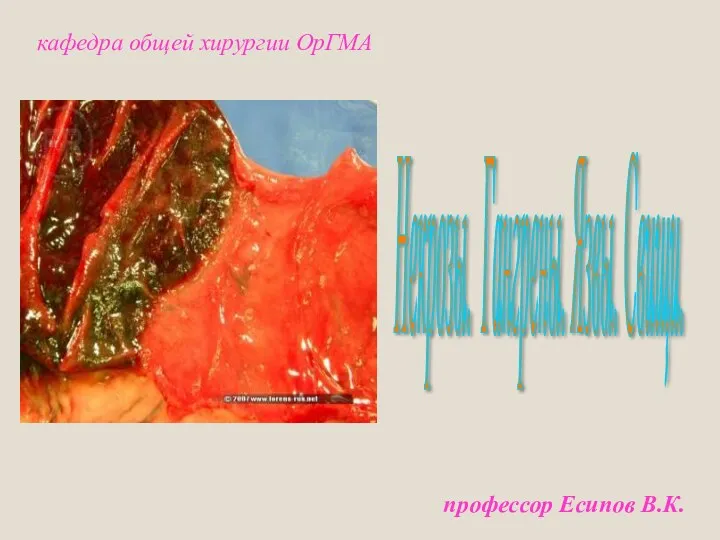 Некрозы. Гангрены. Язвы. Свищи
Некрозы. Гангрены. Язвы. Свищи Ортодонтияда иновациялық емдеу әдістері, инвизилайн (invisalign) жүйесі
Ортодонтияда иновациялық емдеу әдістері, инвизилайн (invisalign) жүйесі Очаговый туберкулез легких
Очаговый туберкулез легких Қант диабеті кезіндегі лабораториялық зерттеулер
Қант диабеті кезіндегі лабораториялық зерттеулер Здоровые дети – счастливые родители
Здоровые дети – счастливые родители Культурно-гигиенические навыки детей от 1 года до 7 лет
Культурно-гигиенические навыки детей от 1 года до 7 лет