Содержание
- 2. Biological Therapy in Psychiatry Anatoly Kreinin MD, PhD Director of Psychiatric Department, Tirat Carmel Mental Health
- 3. Mental Health Care Pre-1930’s
- 4. Before we begin… “It should be made clear that all psychotropic drugs can be safe or
- 5. What is a ‘drug’? A very vague term all ingested substances alter bodily function ‘drug’ is
- 6. HISTORY OF ANTIPSYCHOTICS Anti-psychotics were discovered accidentally by a French naval surgeon, Henri Laborit. Laborit was
- 7. Treatment Before Drugs Came into Play King Saul – vine, music-therapy Patients were kept isolated from
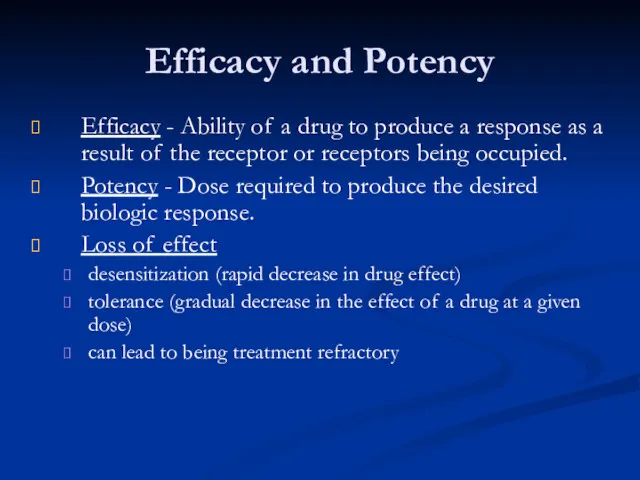
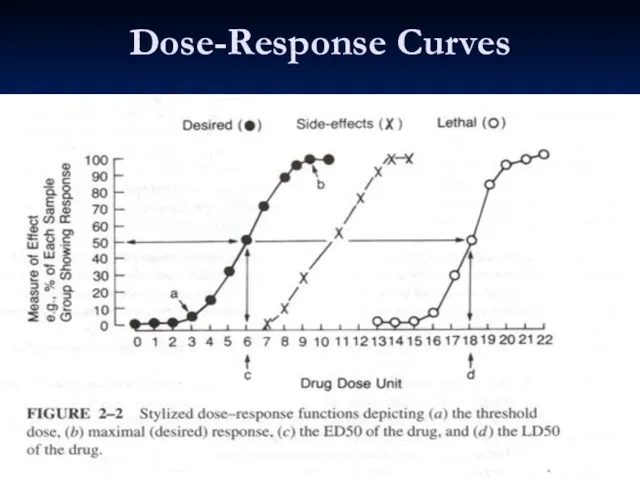
- 9. Efficacy and Potency Efficacy - Ability of a drug to produce a response as a result
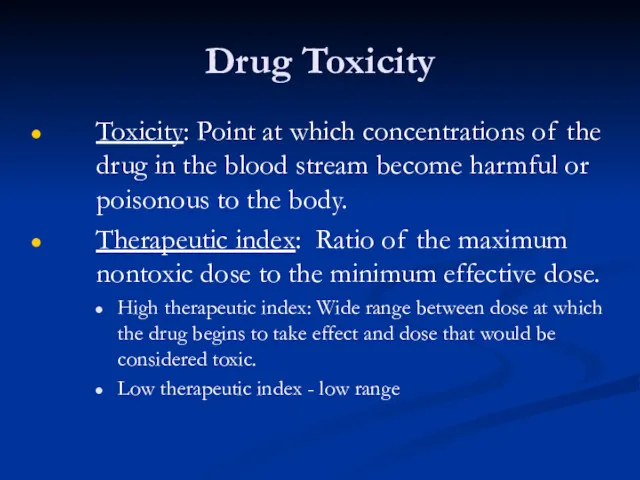
- 10. Drug Toxicity Toxicity: Point at which concentrations of the drug in the blood stream become harmful
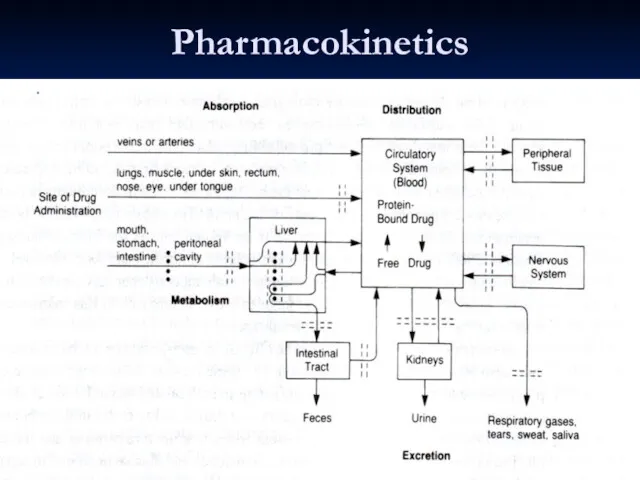
- 11. Absorption From site of administration into the plasma Oral - (tablet and liquid) (Table 8-3) Most
- 12. Pharmacokinetics: How the Body Acts on the Drug Absorption Distribution Metabolism Elimination
- 13. Bioavailability Amount of drug that reaches systemic circulation unchanged Often used to compare one drug to
- 14. Distribution Amount of drug found in various tissues, especially the intended ones. Psychiatric drugs must pass
- 15. Crossing the Blood Brain Barrier Passive diffusion Drug must dissolve in the structure of the cell
- 16. Metabolism Process by which the drug is altered and broken down into smaller substances (metabolites) that
- 17. Elimination Clearance: Total amount of blood, serum, or plasma from which a drug is completely removed
- 18. Dosing and Steady State Dosing: Administration of medication over time, so that therapeutic levels can be
- 19. Pharmacokinetics: Cultural Considerations 9% of whites - genetically defective P-4502D6 Asian descent Metabolize ethanol to produce
- 20. Phases of Drug Treatment Initiation Stabilization Maintenance Discontinuation
- 21. Tolerance & Dependence Tolerance – state of decreased sensitivity to the drug as a result of
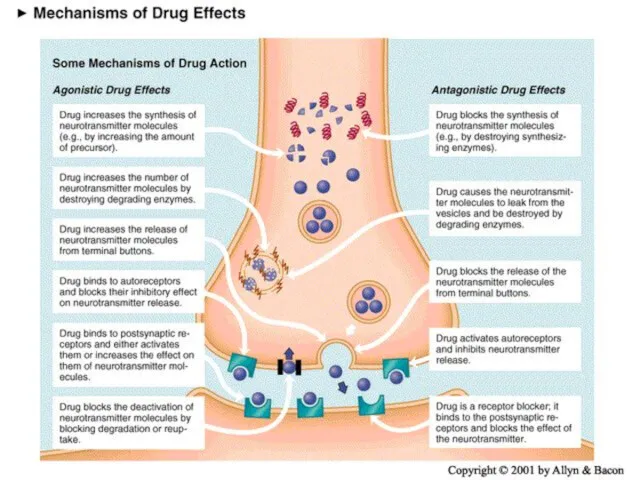
- 22. Receptors Types of Action Agonist: same biologic action Antagonist: opposite effect Interactions with a receptor Selectivity:
- 23. Ion Channels Drugs can block or open the ion channels Example: benzodiazepine drugs facilitate GABA in
- 24. Enzymes Enzymes catalyze specific biochemical reactions within cells and are targets for some drugs. Monoamine oxidase
- 25. Carrier Proteins Transport neurotransmitters across cell membranes Medications may block or inhibit this transport. Example: antidepressants
- 26. Being a neurotransmitter: What does it take? Exists presynaptically Synthesis enzymes exist presynaptically Released in response
- 27. Neurotransmitters 80 plus chemical substances that provide communication between cells. Some of these are actually NTs
- 28. All psychoactive drugs act centrally (i.e. on the brain) The vast majority of drug actions are
- 29. Neurotransmitters have 7 actions Synthesized Stored Enzymatically destroyed if not stored Exocytosis Termination of release via
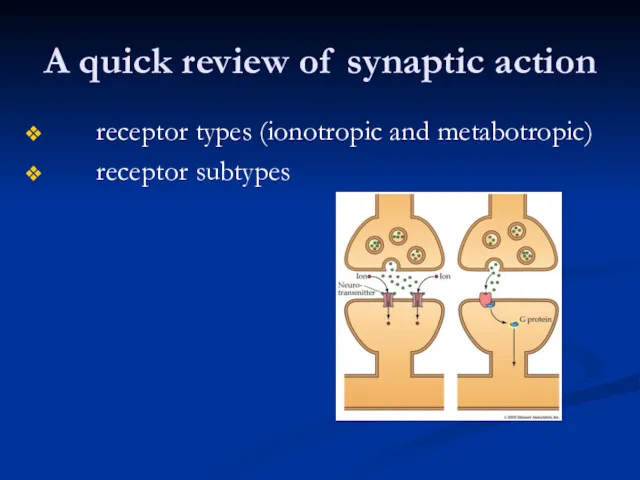
- 30. A quick review of synaptic action receptor types (ionotropic and metabotropic) receptor subtypes
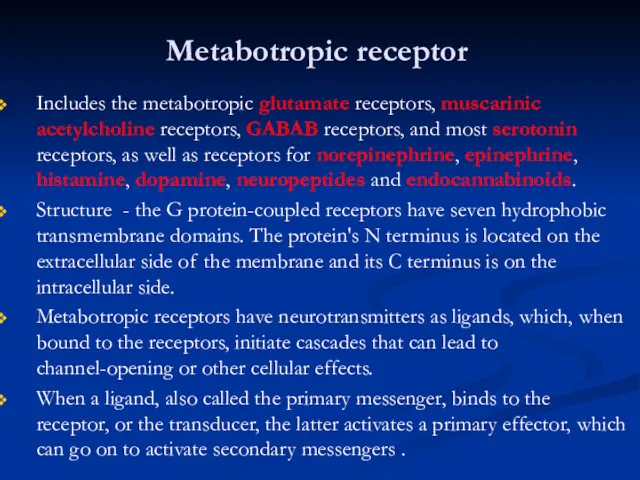
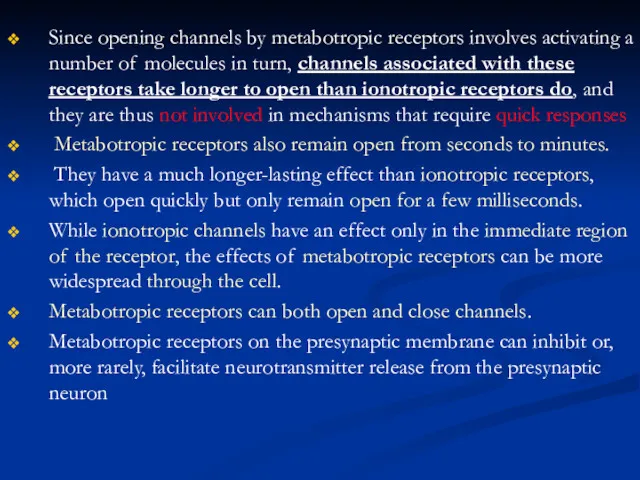
- 31. Metabotropic receptor Includes the metabotropic glutamate receptors, muscarinic acetylcholine receptors, GABAB receptors, and most serotonin receptors,
- 32. Since opening channels by metabotropic receptors involves activating a number of molecules in turn, channels associated
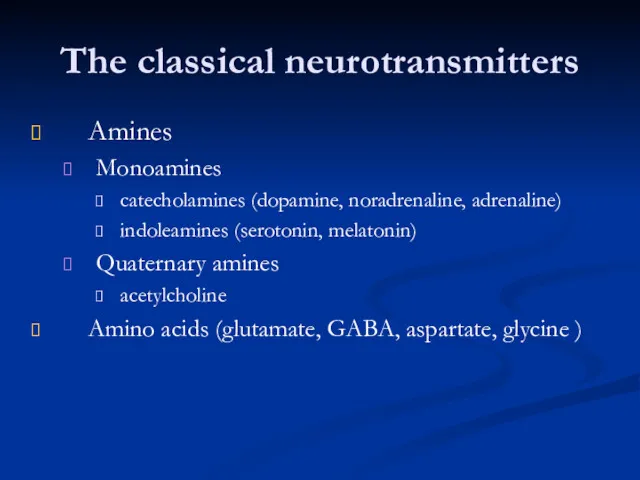
- 33. The classical neurotransmitters Amines Monoamines catecholamines (dopamine, noradrenaline, adrenaline) indoleamines (serotonin, melatonin) Quaternary amines acetylcholine Amino
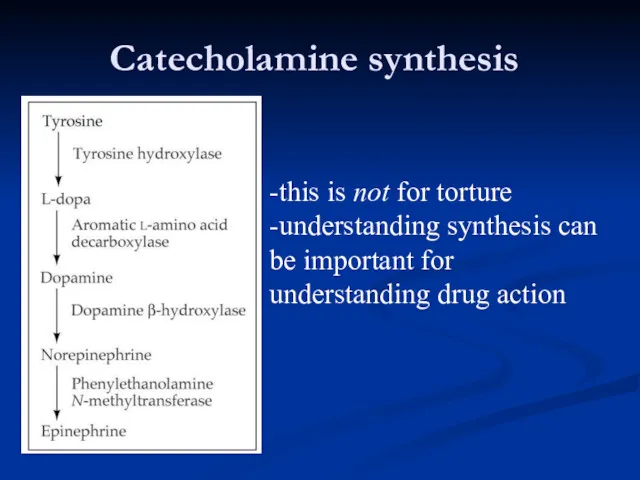
- 34. Catecholamine synthesis -this is not for torture -understanding synthesis can be important for understanding drug action
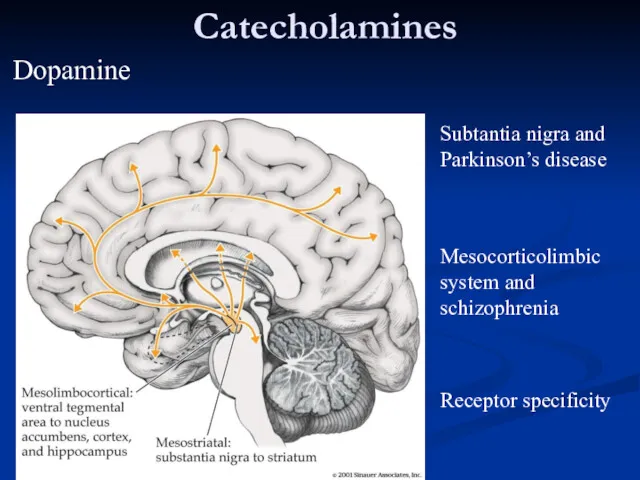
- 35. Catecholamines Subtantia nigra and Parkinson’s disease Mesocorticolimbic system and schizophrenia Receptor specificity Dopamine
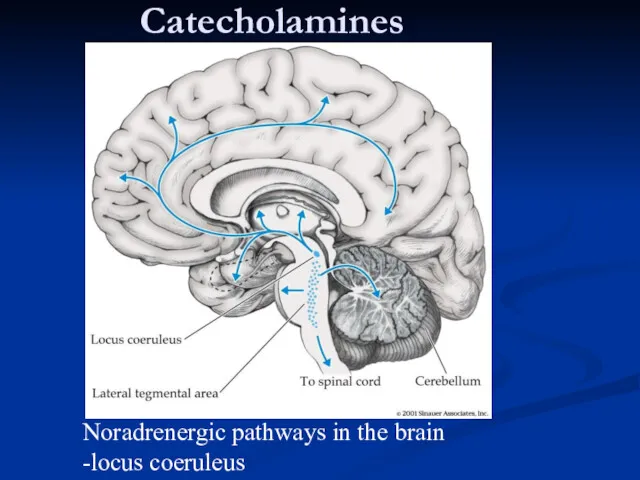
- 36. Catecholamines Noradrenergic pathways in the brain -locus coeruleus
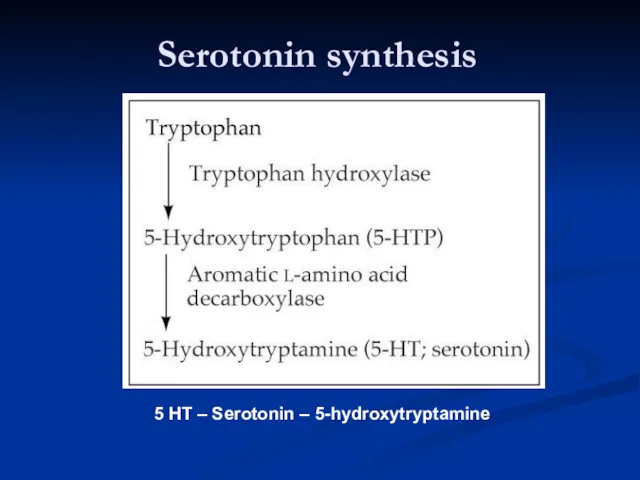
- 37. Serotonin synthesis 5 HT – Serotonin – 5-hydroxytryptamine
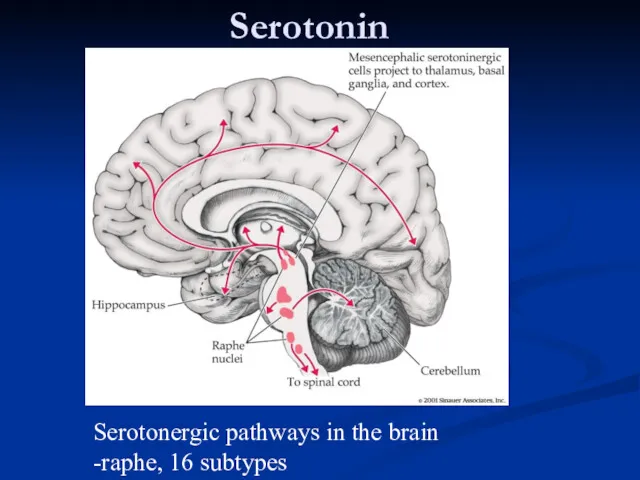
- 38. Serotonin Serotonergic pathways in the brain -raphe, 16 subtypes
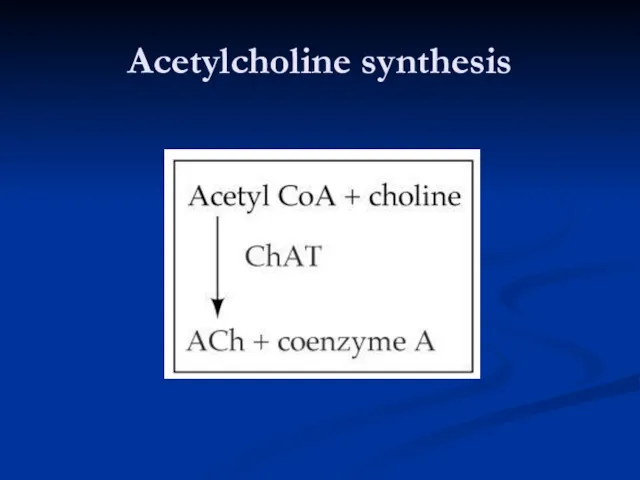
- 39. Acetylcholine synthesis
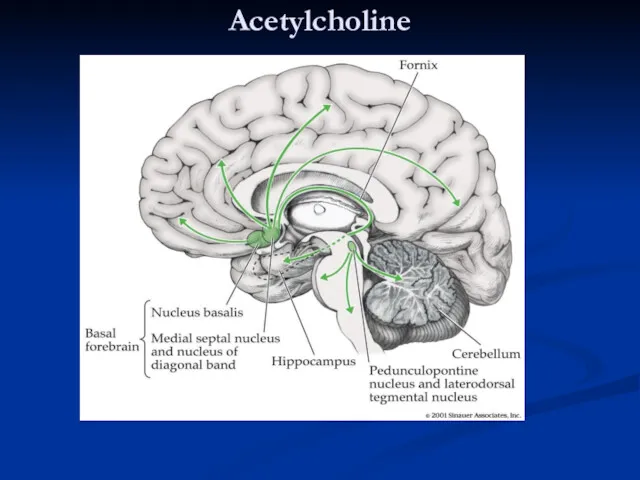
- 40. Acetylcholine Cholinergic pathways in the brain -basal forebrain, neuromuscular junction
- 41. Amino acids: The workhorses of the neurotransmitter family Glutamate - the primary excitatory neurotransmitter in brains
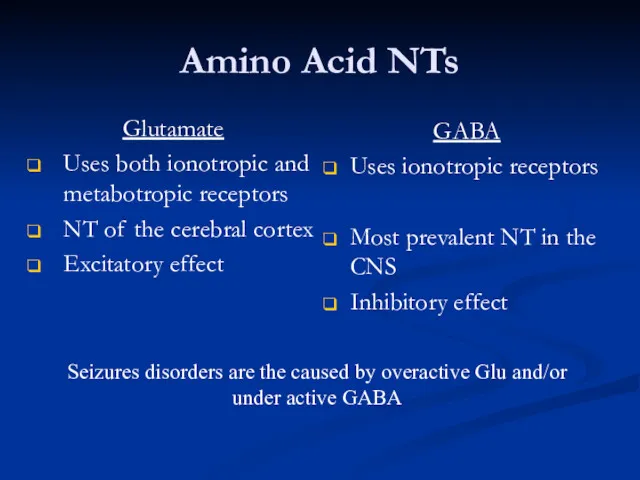
- 42. Amino Acid NTs Glutamate Uses both ionotropic and metabotropic receptors NT of the cerebral cortex Excitatory
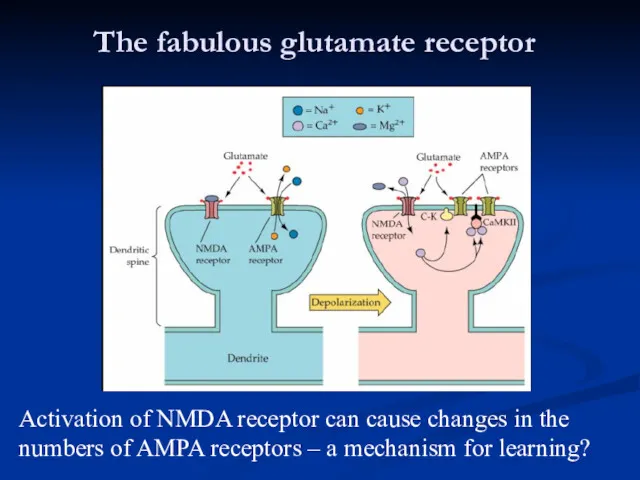
- 43. The fabulous glutamate receptor Activation of NMDA receptor can cause changes in the numbers of AMPA
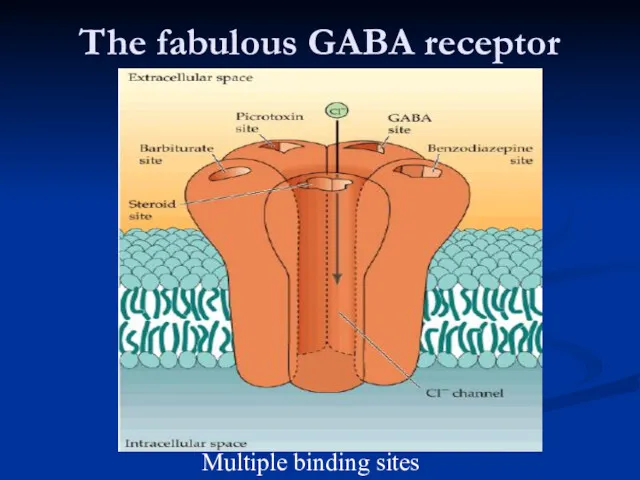
- 44. The fabulous GABA receptor Multiple binding sites
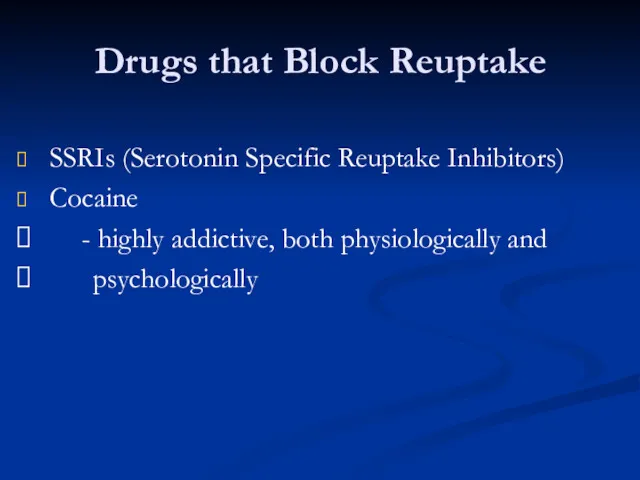
- 45. Drugs that Block Reuptake SSRIs (Serotonin Specific Reuptake Inhibitors) Cocaine - highly addictive, both physiologically and
- 46. Dose-Response Curves
- 47. Pharmacokinetics Blood Brain Barrier Blocks many chemicals in general circulation from entering the brain The capillaries
- 48. Pharmacokinetics
- 49. Pharmacokinetics Liver P450 Enzymes Everything absorbed from the GI tract passes through the liver before entering
- 50. Pharmacokinetics Liver P450 Enzymes (cont.) Levels of the ~50 P450 enzymes in humans can vary widely
- 51. Basic classification of drug actions Agonists stimulate or activate antagonists prevent
- 52. Ways that drugs can agonize Stimulate release receptor binding inhibition of reuptake inhibition of deactivation promote
- 53. Ways that drugs can antagonize Block release receptor blocker prevent synthesis
- 54. Schizophrenia Affects about 1/100 people Begins in 20’s Often triggered by stress, illness, etc. but there’s
- 55. Symptoms of schizophrenia Positive symptoms -hallucinations, delusions, paranoia Negative symptoms -lack of emotion, energy, directedness
- 56. Schizophrenia Pathophysiology No consistent neuropathology or biomarkers for schizophrenia ? Increased dopamine in mesolimbic pathways causes
- 57. Schizophrenia Antipsychotics Typical / Conventional antipsychotics Atypical antipsychotics
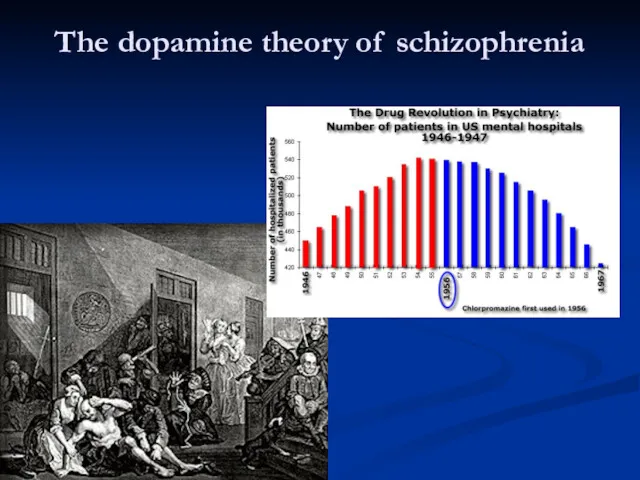
- 58. The dopamine theory of schizophrenia
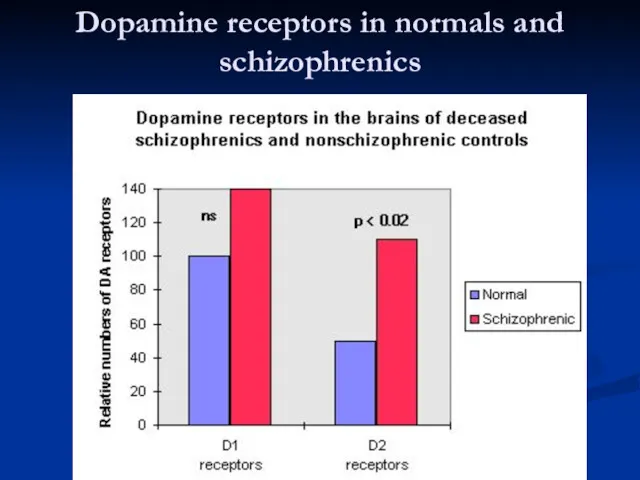
- 59. Dopamine receptors in normals and schizophrenics
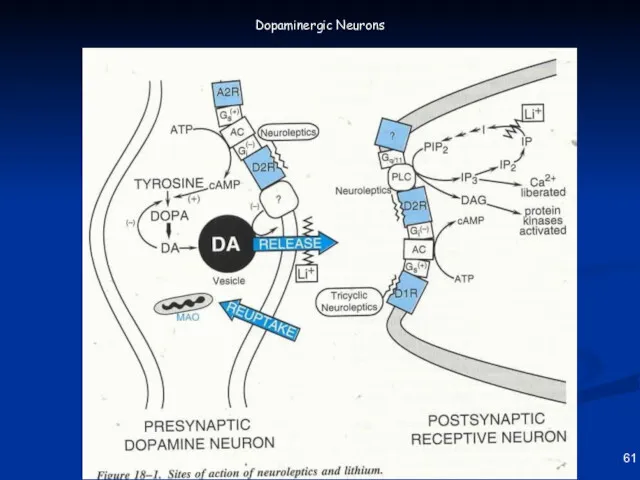
- 60. 61 Dopaminergic Neurons
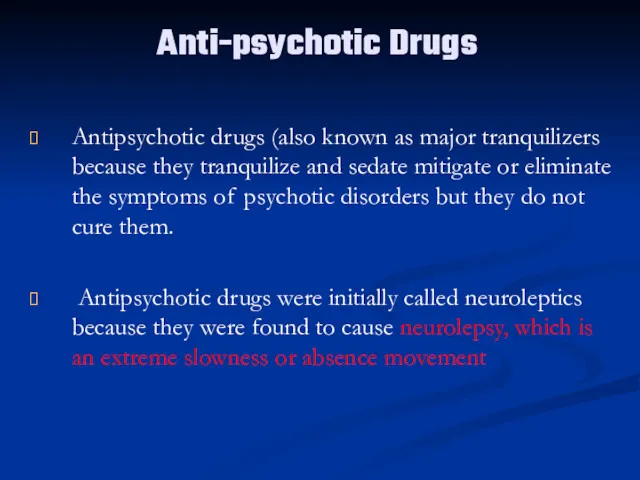
- 61. Anti-psychotic Drugs Antipsychotic drugs (also known as major tranquilizers because they tranquilize and sedate mitigate or
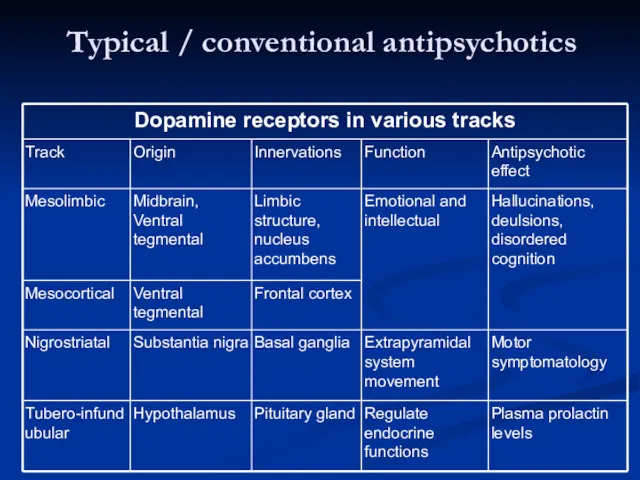
- 62. Typical / conventional antipsychotics
- 63. Typical / conventional antipsychotics Mechanism of action Blocks receptors for dopamine, acetylcholine, histamine and norepinephrine Current
- 64. Typical / conventional antipsychotics Properties Effective in reducing positive symptoms during acute episodes and in preventing
- 65. Typical / conventional antipsychotics Potency All have same ability to relieve symptoms of psychosis Differ from
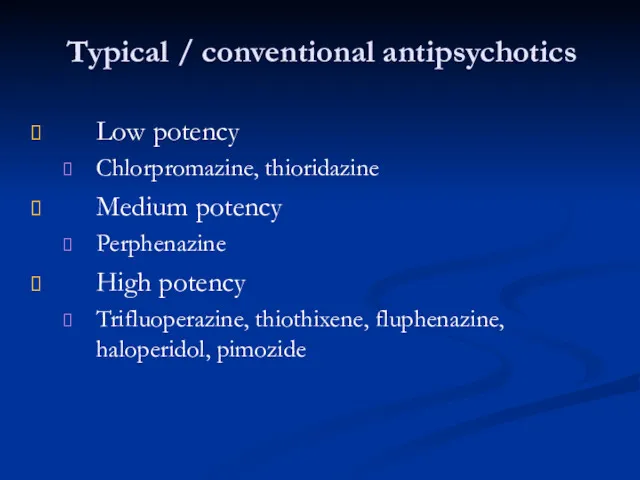
- 66. Typical / conventional antipsychotics Low potency Chlorpromazine, thioridazine Medium potency Perphenazine High potency Trifluoperazine, thiothixene, fluphenazine,
- 67. BRAIN AREAS INVOLVED IN ANTIPSYCHOTIC TREATMENT The oversimplified version of what brain areas are involved in
- 68. BRAIN AREAS INVOLVED IN SCHIZOPHRENIA 4 DOPAMINE PATHWAYS There are four dopamine pathways in the brain:
- 69. Dopamine Pathways Nigrostriatal Chronic blockade can cause Potentially irreversible movement disorder “Tardive Dyskinesia”
- 70. Dopamine Pathways Mesocortical May be associated with both positive and negative symptoms Blockade may help reduce
- 71. Dopamine Pathways Tuberoinfundibular Blockade produces galactorrhea Dopamine = PIF (prolactin inhibiting factor)
- 72. Dopamine Pathways Summary Four dopamine pathways Appears that blocking dopamine receptors in only one of them
- 73. Dopaminergic D2 Blockade Possible Clinical Consequences Extrapyramidal movement disorders Endocrine changes Sexual dysfunction
- 74. Histamine H1 Blockade Possible Clinical Consequences Sedation, drowsiness Weight gain Hypotension
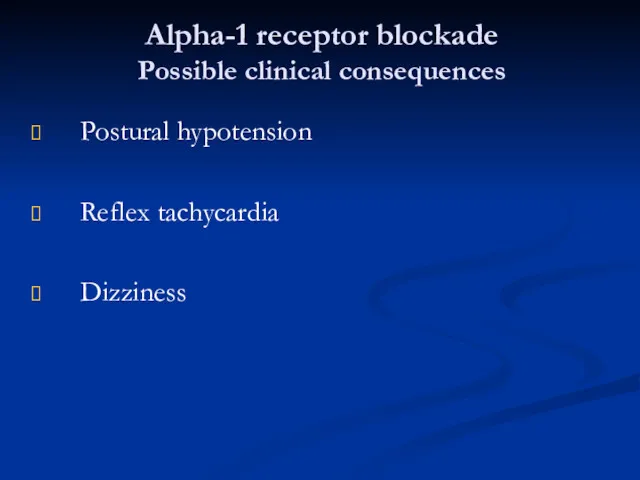
- 75. Alpha-1 receptor blockade Possible clinical consequences Postural hypotension Reflex tachycardia Dizziness
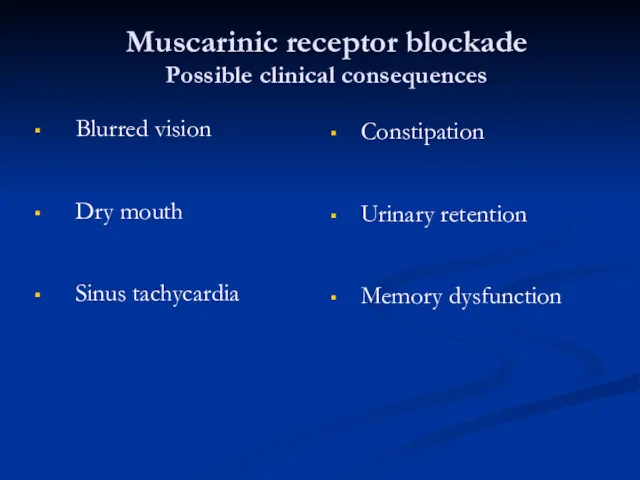
- 76. Muscarinic receptor blockade Possible clinical consequences Blurred vision Dry mouth Sinus tachycardia Constipation Urinary retention Memory
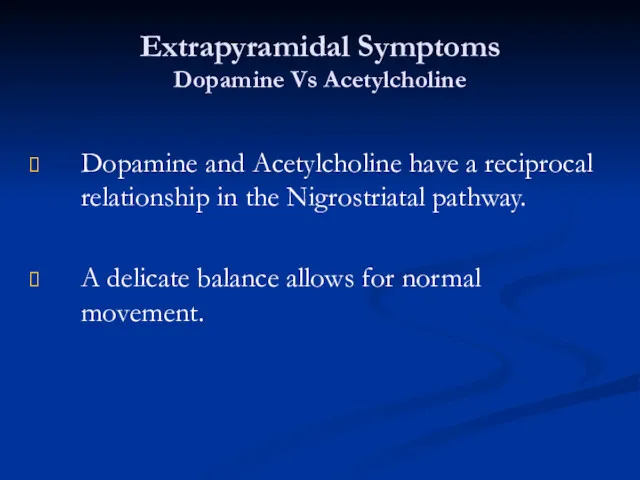
- 77. Extrapyramidal Symptoms Dopamine Vs Acetylcholine Dopamine and Acetylcholine have a reciprocal relationship in the Nigrostriatal pathway.
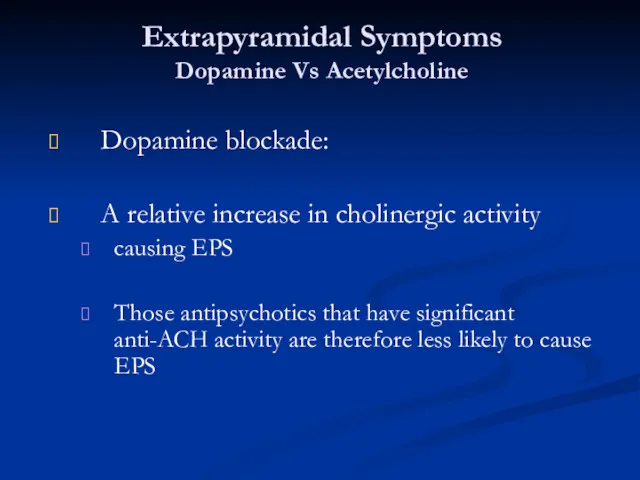
- 78. Extrapyramidal Symptoms Dopamine Vs Acetylcholine Dopamine blockade: A relative increase in cholinergic activity causing EPS Those
- 79. Extrapyramidal Symptoms Dopamine Vs Acetylcholine When high potency antipsychotics are chosen, we often prescribe anti-ACH medication
- 80. Neurological Side Effects: Dystonic Reactions: Uncoordinated spastic movements of muscle groups Trunk, tongue, face Akinesia: Decreased
- 81. Neurological Side Effects: Tremors: Fine movement (shaking) of the extremities Akathisia: Restlessness Pacing May result in
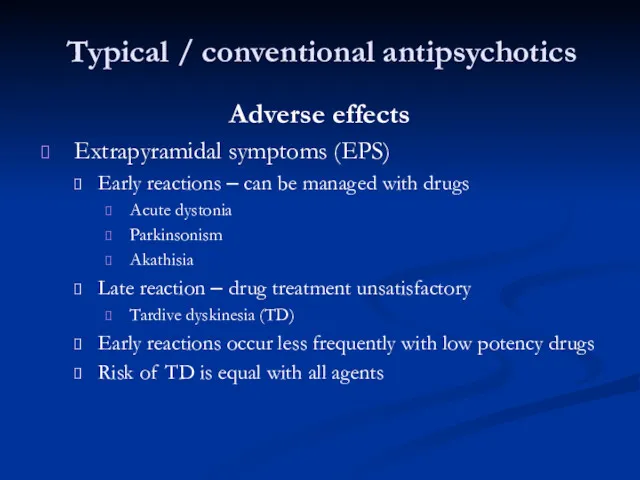
- 82. Typical / conventional antipsychotics Adverse effects Extrapyramidal symptoms (EPS) Early reactions – can be managed with
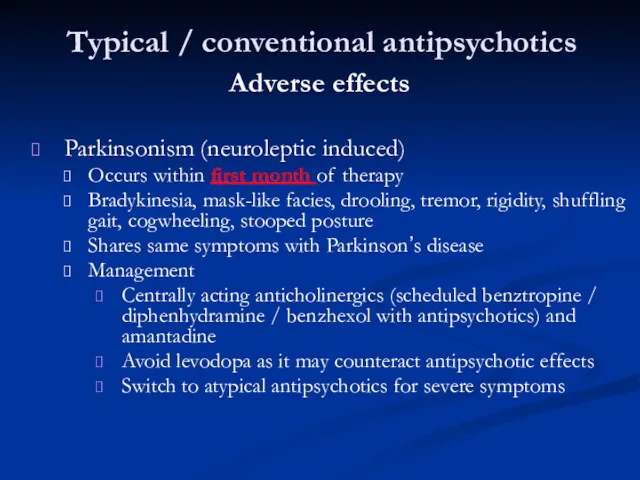
- 83. Typical / conventional antipsychotics Adverse effects Parkinsonism (neuroleptic induced) Occurs within first month of therapy Bradykinesia,
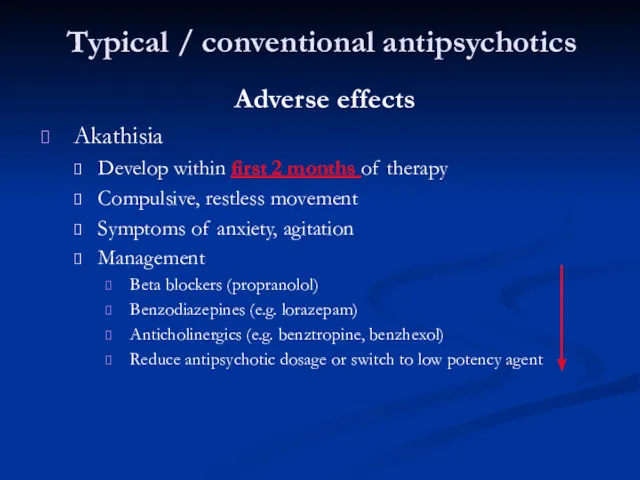
- 84. Typical / conventional antipsychotics Adverse effects Akathisia Develop within first 2 months of therapy Compulsive, restless
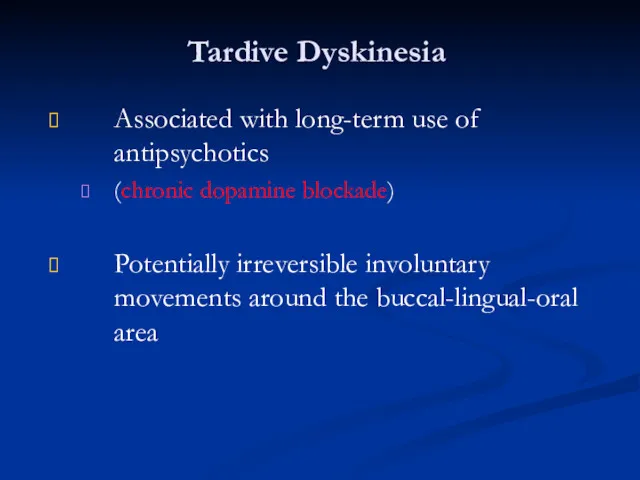
- 85. Tardive Dyskinesia Associated with long-term use of antipsychotics (chronic dopamine blockade) Potentially irreversible involuntary movements around
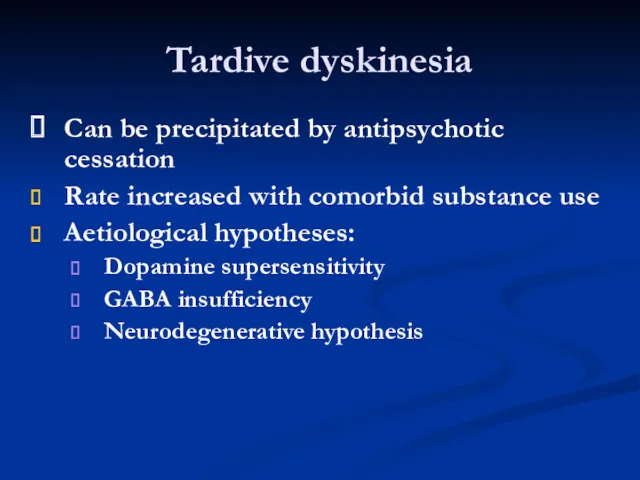
- 86. Tardive dyskinesia Can be precipitated by antipsychotic cessation Rate increased with comorbid substance use Aetiological hypotheses:
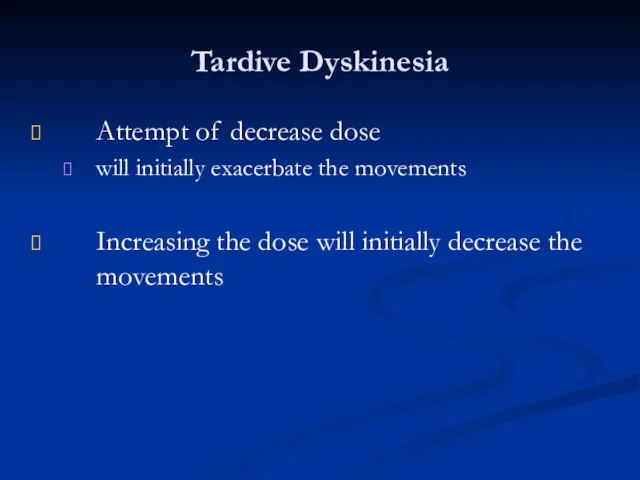
- 87. Tardive Dyskinesia Attempt of decrease dose will initially exacerbate the movements Increasing the dose will initially
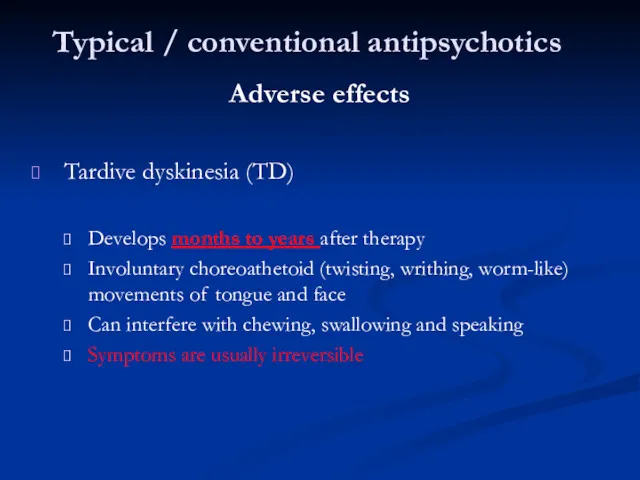
- 88. Typical / conventional antipsychotics Adverse effects Tardive dyskinesia (TD) Develops months to years after therapy Involuntary
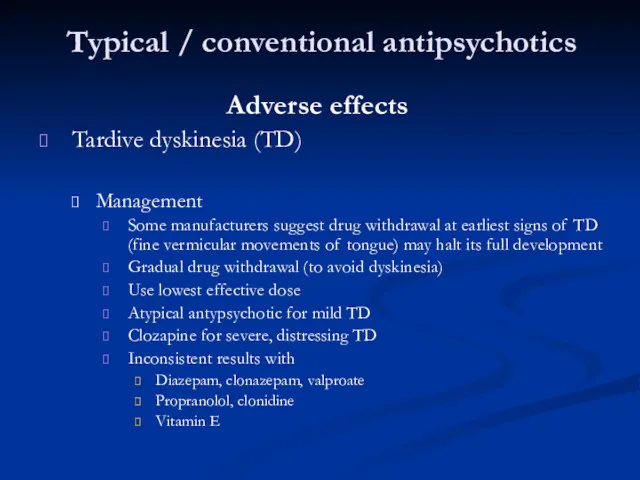
- 89. Typical / conventional antipsychotics Adverse effects Tardive dyskinesia (TD) Management Some manufacturers suggest drug withdrawal at
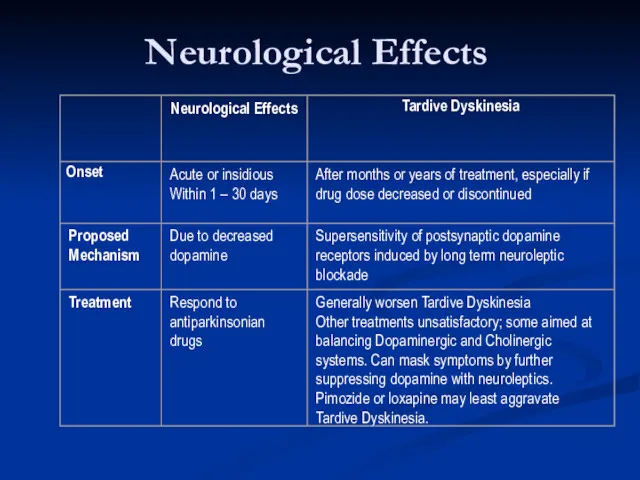
- 90. Neurological Effects
- 92. Скачать презентацию

 Лучевая диагностика остеоартрозов и артрозоартритов
Лучевая диагностика остеоартрозов и артрозоартритов Гипертермический синдром
Гипертермический синдром Клинический случай
Клинический случай Показания и противопоказания переливания крови. Способы, виды, методы переливания. Осложнения и профилактика
Показания и противопоказания переливания крови. Способы, виды, методы переливания. Осложнения и профилактика Развитие органов кроветворения и иммунной защиты
Развитие органов кроветворения и иммунной защиты Физика и метафизика смерти
Физика и метафизика смерти Доказательная медицина в сестринском деле. Концепция доказательной медицины. Основные понятия
Доказательная медицина в сестринском деле. Концепция доказательной медицины. Основные понятия Закрытые и открытые повреждения грудной клетки и ее органов
Закрытые и открытые повреждения грудной клетки и ее органов Особенности конструирования зубных протезов при опоре на имплантаты. Принципы выбора рациональных структур имплантатов
Особенности конструирования зубных протезов при опоре на имплантаты. Принципы выбора рациональных структур имплантатов Ветеринарная вирусология. Вирус европейской чумы свиней
Ветеринарная вирусология. Вирус европейской чумы свиней ботулизм
ботулизм Листериялар. Морфологиясы, физиологиясы, листериялардың антигендері. Экологиясы. Әйелдер патологиясындағы ролі
Листериялар. Морфологиясы, физиологиясы, листериялардың антигендері. Экологиясы. Әйелдер патологиясындағы ролі Энцефалопатия Балалардың церебралдық салдары
Энцефалопатия Балалардың церебралдық салдары Ортопедическое лечение при заболеваниях пародонта
Ортопедическое лечение при заболеваниях пародонта Коморбидные формы ВИЧ-инфекции
Коморбидные формы ВИЧ-инфекции Эпилепсия. Диагностика и лечение
Эпилепсия. Диагностика и лечение Биохимия почек и мочи. (Лекция 10)
Биохимия почек и мочи. (Лекция 10) Неспецифический язвенный колит
Неспецифический язвенный колит Симтоматология гастритов, язвенной болезни желудка и двенадцатиперстной кишки. Заболевания тонкого и толстого кишечника
Симтоматология гастритов, язвенной болезни желудка и двенадцатиперстной кишки. Заболевания тонкого и толстого кишечника Функциональная анатомия органов мужской половой системы
Функциональная анатомия органов мужской половой системы Faberlic - Expert. Домашняя альтернатива салонным процедурам
Faberlic - Expert. Домашняя альтернатива салонным процедурам Дорсопатия - дегенеративно-дистрофические заболевания позвоночника и околопозвоночных тканей
Дорсопатия - дегенеративно-дистрофические заболевания позвоночника и околопозвоночных тканей Желтуха новорожденных
Желтуха новорожденных Әйелдер консультациясы және отбасын жоспарлау орталықтарында жас ата-аналар мектебінің жұмысына қатысып есеп жазу
Әйелдер консультациясы және отбасын жоспарлау орталықтарында жас ата-аналар мектебінің жұмысына қатысып есеп жазу Сердечно-сосудистая недостаточность у новорожденных детей
Сердечно-сосудистая недостаточность у новорожденных детей Расстройства ощущений и восприятия
Расстройства ощущений и восприятия Приобретённые пороки сердца
Приобретённые пороки сердца Жүкті әйелді антенаталды бақылау, физиологиялық жүктілікті бақылау, босануға психологиялық дайындық
Жүкті әйелді антенаталды бақылау, физиологиялық жүктілікті бақылау, босануға психологиялық дайындық