Содержание
- 2. Frequency 67% occur in males Young adults (20-29 yr) Children > 50 years of age fewest
- 3. INCIDENCE Approx. one million burn patients/annually in the United States 3-5% cases are life-threatening 60,000 hospitalized
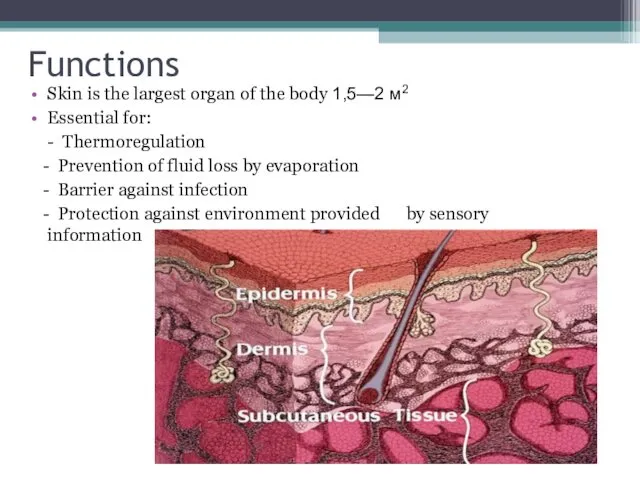
- 4. Functions Skin is the largest organ of the body 1,5—2 м2 Essential for: - Thermoregulation -
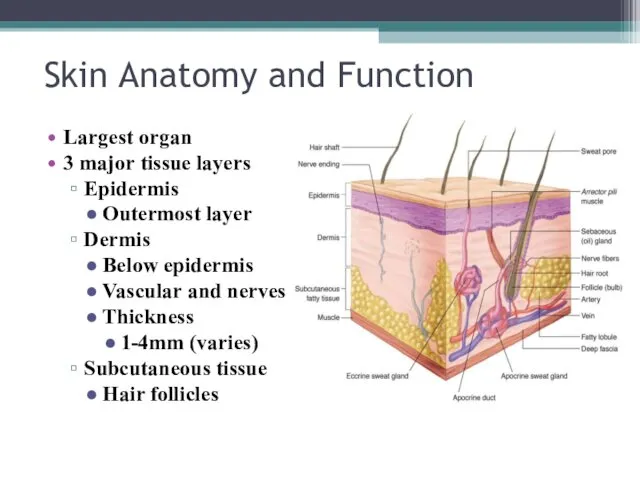
- 5. Skin Anatomy and Function Largest organ 3 major tissue layers Epidermis Outermost layer Dermis Below epidermis
- 6. Types of burn injuries Thermal: direct contact with heat (flame, scald, contact) Electrical A.C. – alternating
- 7. Classification Burns are classified by depth, type and extent of injury Every aspect of burn treatment
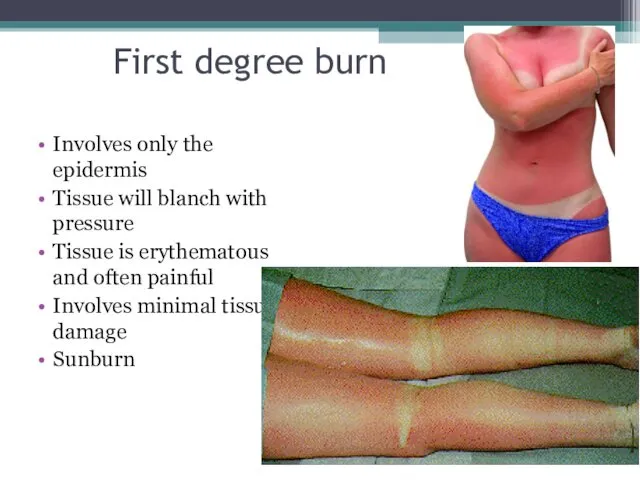
- 8. First degree burn Involves only the epidermis Tissue will blanch with pressure Tissue is erythematous and
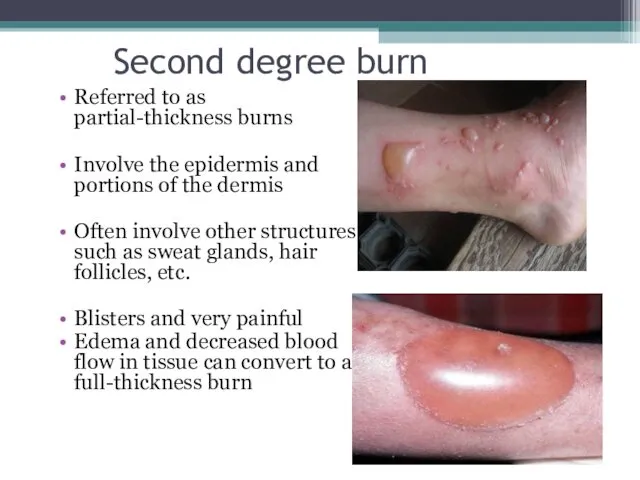
- 9. Second degree burn Referred to as partial-thickness burns Involve the epidermis and portions of the dermis
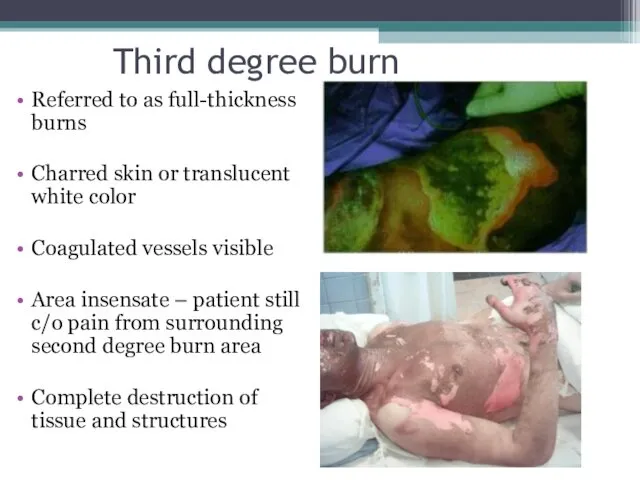
- 10. Third degree burn Referred to as full-thickness burns Charred skin or translucent white color Coagulated vessels
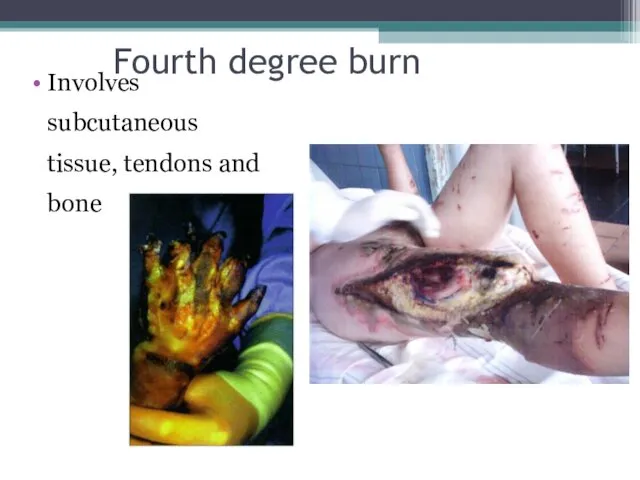
- 11. Fourth degree burn Involves subcutaneous tissue, tendons and bone
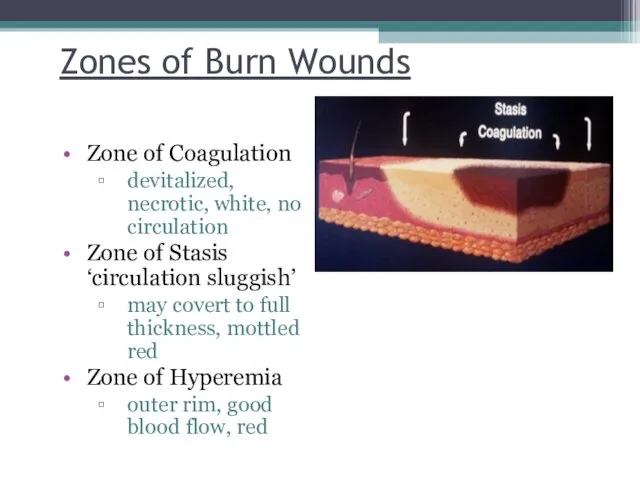
- 12. Zones of Burn Wounds Zone of Coagulation devitalized, necrotic, white, no circulation Zone of Stasis ‘circulation
- 13. Burn extent % BSA involved morbidity Burn extent is calculated only on individuals with second and
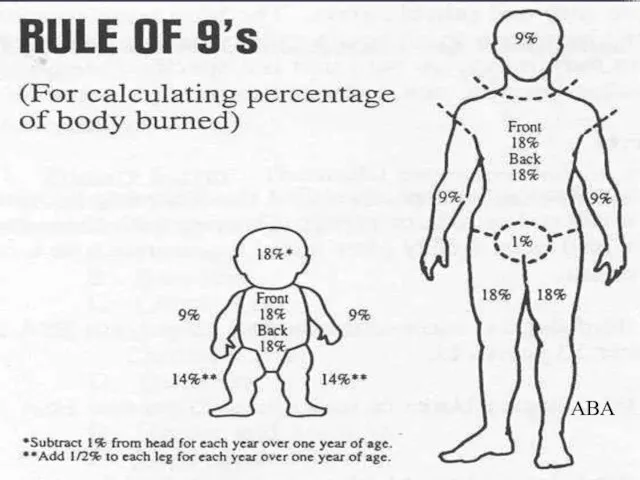
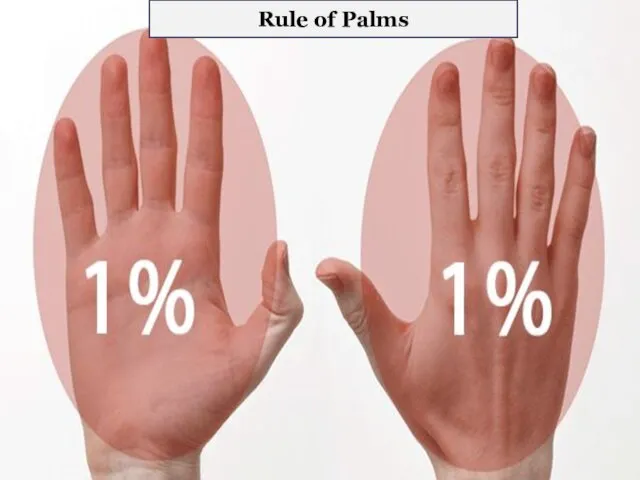
- 14. Measurement charts Rule of Nines: Quick estimate of percent of burn Rule of Palms: Good for
- 15. Rule of 9s ABA
- 16. Rule of Palms
- 17. Lab studies Severe burns: CBC Chemistry profile Coagulation profile creatine phosphokinase and urine myoglobin (with electrical
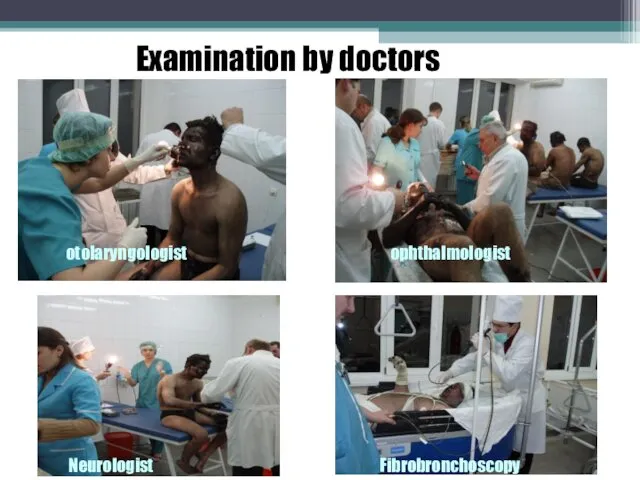
- 18. otolaryngologist Neurologist ophthalmologist Fibrobronchoscopy Examination by doctors
- 19. Imaging studies X-Ray Plain Films / CT scan: Dependent upon history and physical findings
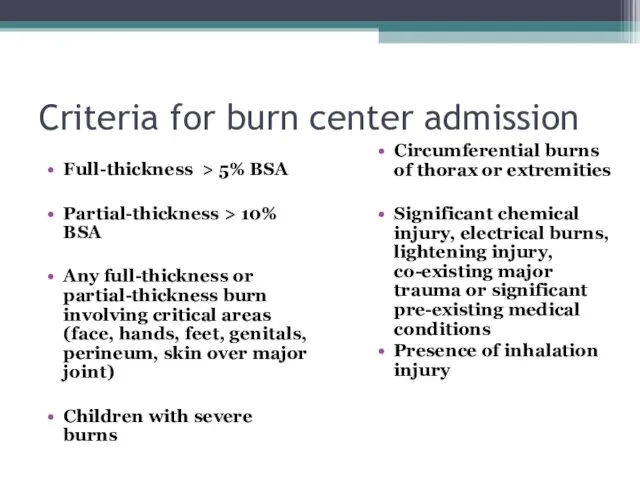
- 20. Criteria for burn center admission Full-thickness > 5% BSA Partial-thickness > 10% BSA Any full-thickness or
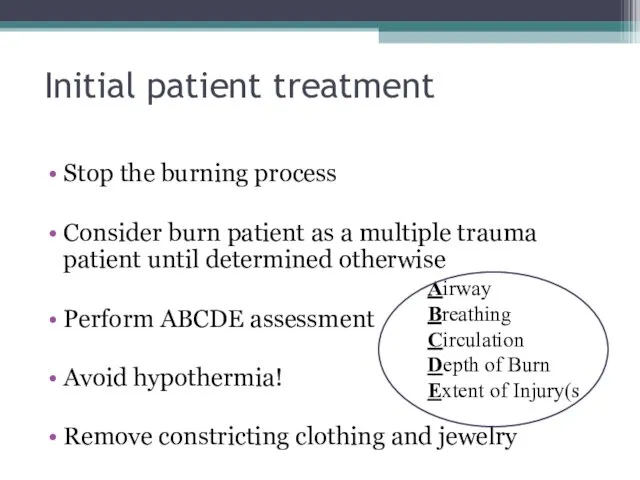
- 21. Initial patient treatment Stop the burning process Consider burn patient as a multiple trauma patient until
- 22. Details of the incident Cause of the burn Time of injury Place of the occurrence (closed
- 23. Care of small burns What can YOU do?
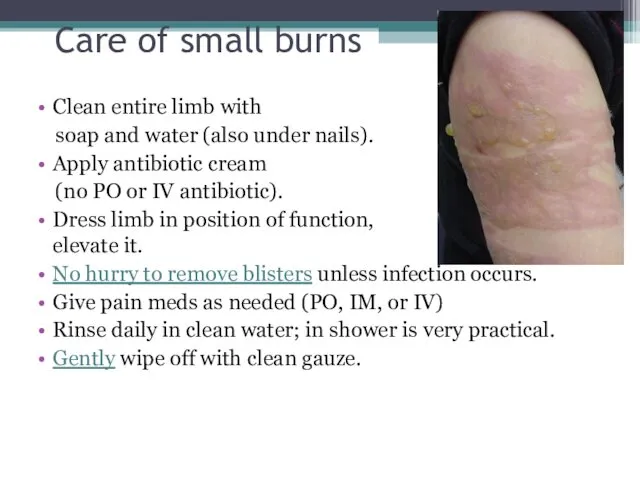
- 24. Care of small burns Clean entire limb with soap and water (also under nails). Apply antibiotic
- 25. Blisters In the pre-hospital setting, there is no hurry to remove blisters. Leaving the blister intact
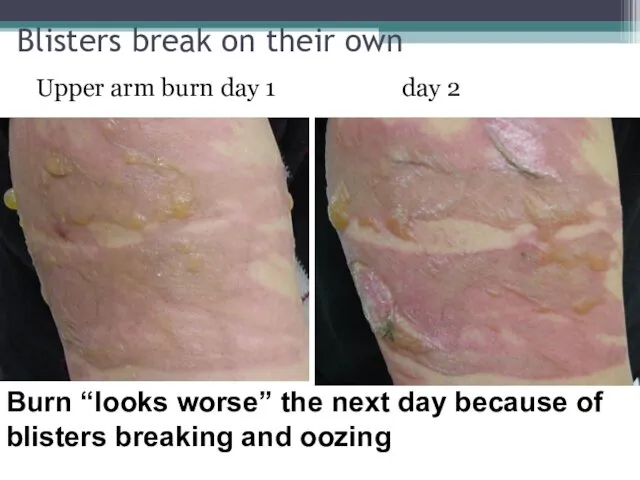
- 26. Blisters break on their own Upper arm burn day 1 day 2 Burn “looks worse” the
- 27. Upper arm burn Blisters show probable partial thickness burn. Area without blister might be deeper partial
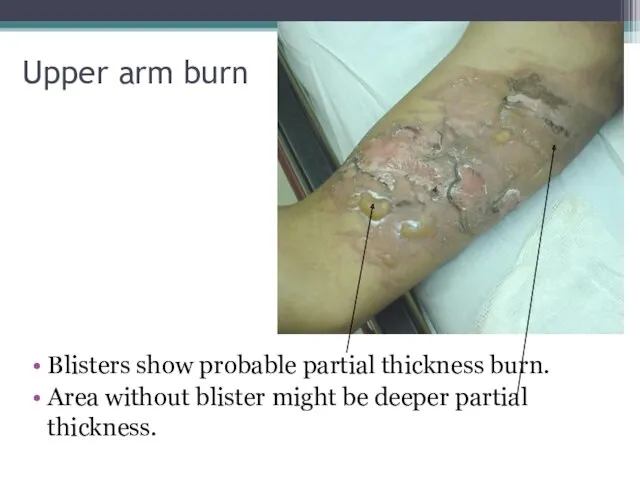
- 28. Debride blister using simple instruments
- 29. After debridement
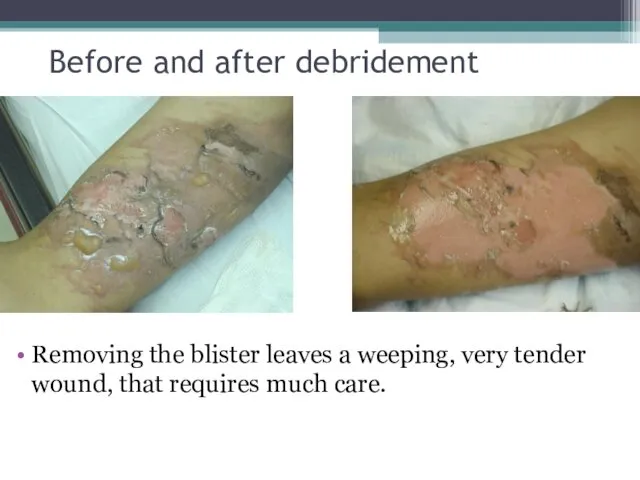
- 30. Before and after debridement Removing the blister leaves a weeping, very tender wound, that requires much
- 31. Silver sulfadiazene
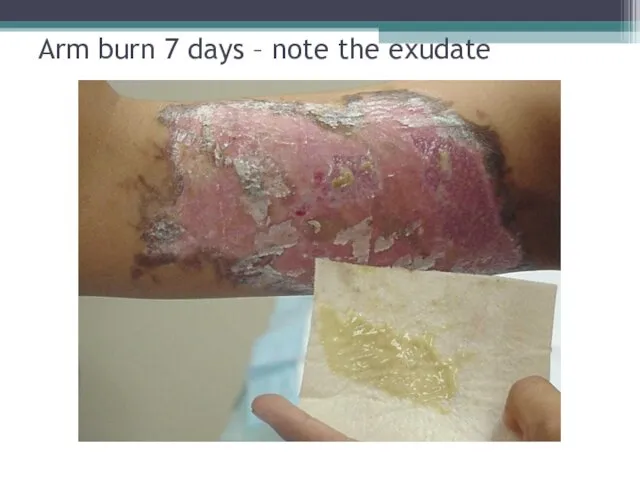
- 32. Arm burn 7 days – note the exudate
- 33. Burns of special areas of the body Face Mouth Neck Hands and feet Genitalia
- 34. Face Be VERY concerned for the airway!! Eyelids, lips and ears often swell. In fact, they
- 35. Hands and feet This is rather deep and might require grafting. But initial management is basic.
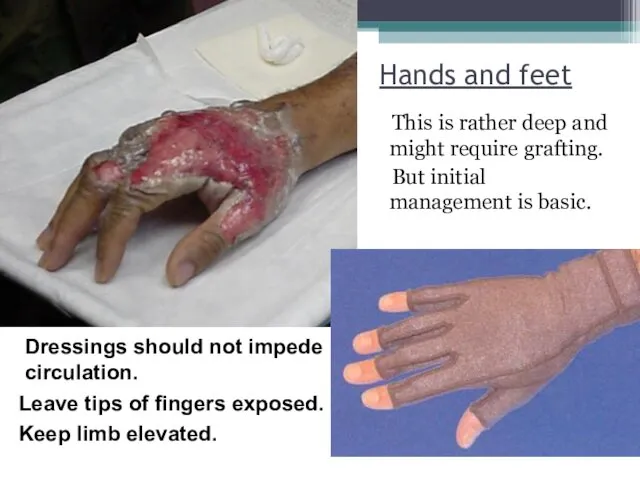
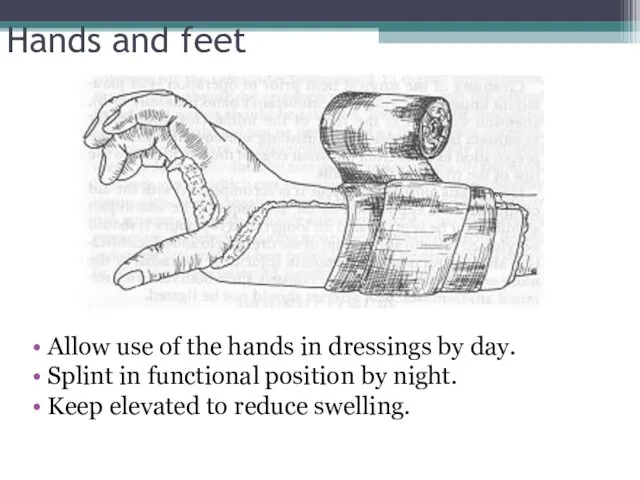
- 36. Hands and feet Allow use of the hands in dressings by day. Splint in functional position
- 37. Hands and feet Fingers might develop contractures if active measures are not taken to prevent them.
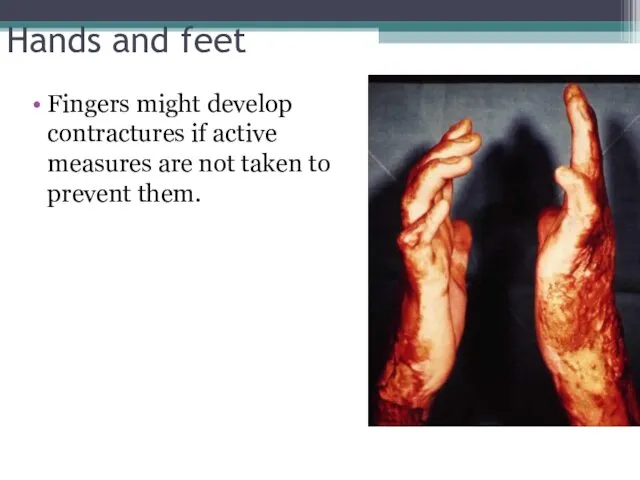
- 38. Genitalia Shower daily, rinse off old cream, apply new cream. Insert Foley catheter if unable to
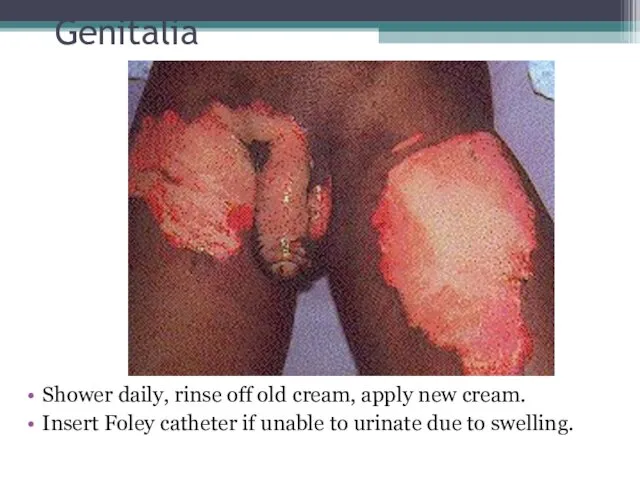
- 39. Large Burns
- 40. Causes of death in burn patients Airway Facial edema, and/or airway edema Breathing Toxic inhalation (CO,
- 41. Edema Formation Amount of edema can be immense (even without facial burns) Depression of mental status
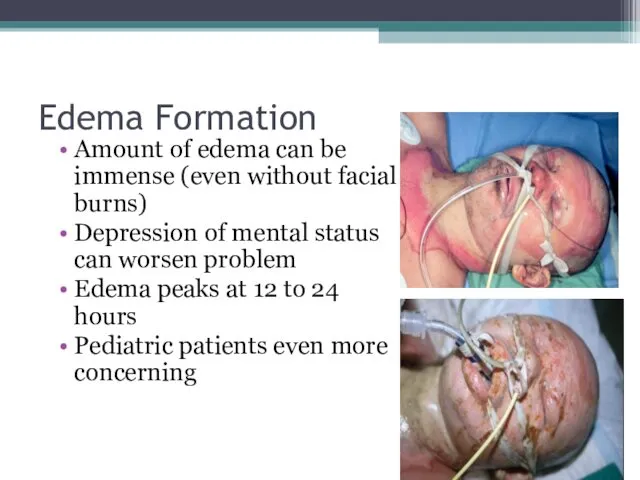
- 42. Causes of death in burn patients Circulation: “failure of resuscitation” Cardiovascular collapse, or acute MI Acute
- 43. Patients with larger burns First assess CBA’s “Disability” (brief neuro exam) Later Examine rest of patient
- 44. Airway considerations Upper airway injury (above the glottis): Area buffers the heat of smoke – thermal
- 45. Criteria for intubation Changes in voice Wheezing / labored respirations Excessive, continuous coughing Altered mental status
- 46. Ventilatory therapies Rapid Sequence Intubation Pain Management, Sedation and Paralysis PEEP (positive end expiratory pressure) High
- 47. Ventilatory therapies Burn patients with Acute respiratory distress syndrome (ARDS) requiring PEEP (positive end expiratory pressure)
- 48. Circumferential burns of the chest Eschar - burned, inflexible, necrotic tissue Compromises ventilatory motion Escharotomy may
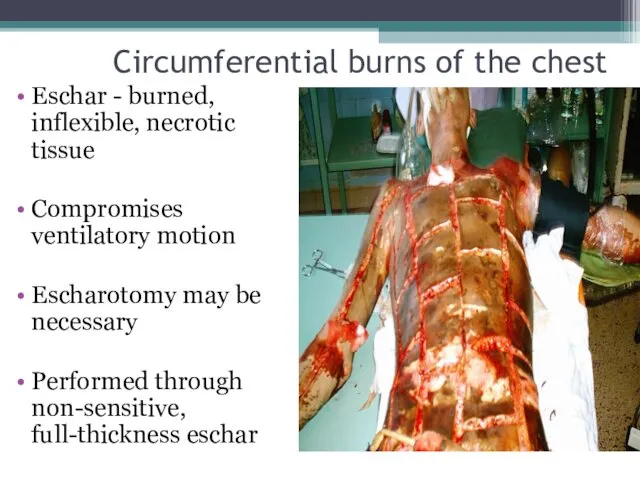
- 49. Carbon Monoxide Intoxication Carbon monoxide has a binding affinity for hemoglobin which is 210-240 times greater
- 50. Signs and Symptoms of Carbon Monoxide Intoxication Usually symptoms not present until 15% of the hemoglobin
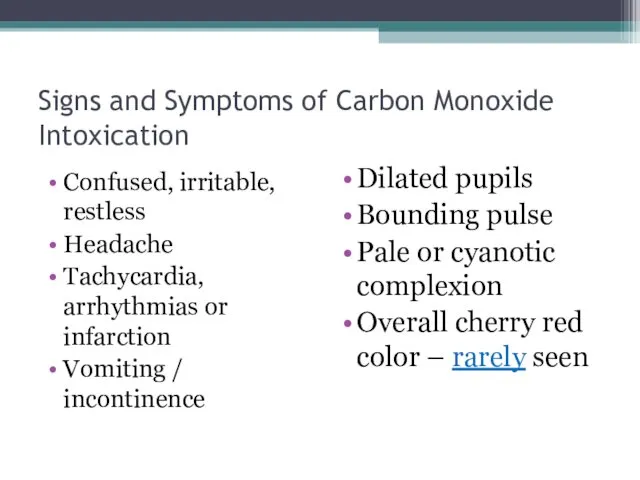
- 51. Signs and Symptoms of Carbon Monoxide Intoxication Confused, irritable, restless Headache Tachycardia, arrhythmias or infarction Vomiting
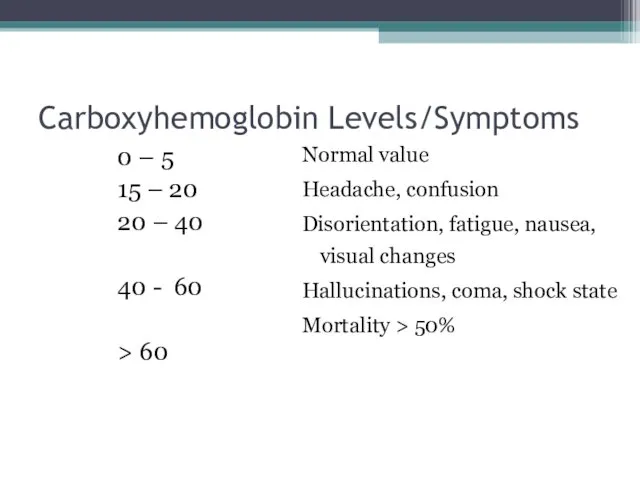
- 52. Carboxyhemoglobin Levels/Symptoms 0 – 5 15 – 20 20 – 40 40 - 60 > 60
- 53. Management of Carbon Monoxide Intoxication Remove patient from source of exposure. Administer 100% high flow oxygen
- 54. Circulation considerations Formation of edema is the greatest initial volume loss Burns 30% or Edema is
- 55. Circulation considerations Capillary permeability increased Protein molecules are now able to cross the membrane Reduced intravascular
- 56. Circulation considerations Loss of plasma volume is greatest during the first 4 – 6 hours, decreasing
- 57. Fluid resuscitation Goal: Maintain perfusion to vital organs Based on the TBSA, body weight and whether
- 58. Fluid resuscitation Lactated Ringers - preferred solution Contains Na+ - restoration of Na+ loss is essential
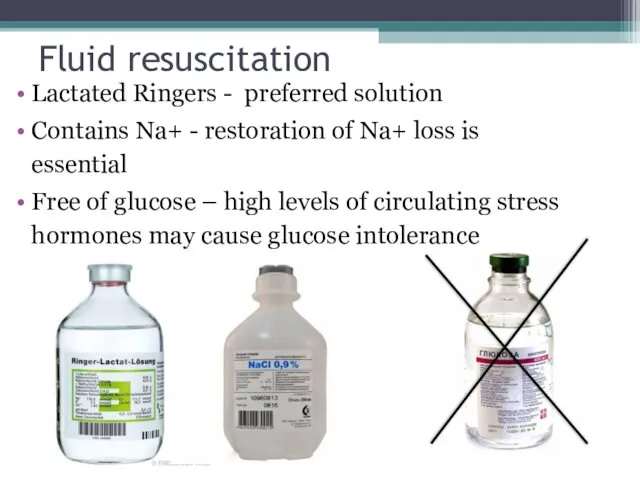
- 59. Fluid resuscitation Burned patients have large insensible fluid losses Fluid volumes may increase in patients with
- 60. Fluid resuscitation Fluid requirement calculations for infusion rates are based on the time from injury, not
- 61. Assessing adequacy of resuscitation Peripheral blood pressure: may be difficult to obtain Urine Output: Best indicator
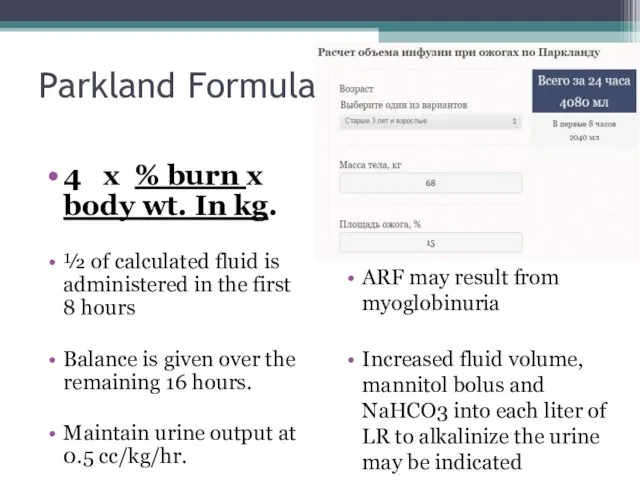
- 62. Parkland Formula 4 x % burn x body wt. In kg. ½ of calculated fluid is
- 63. Effects of hypothermia Hypothermia may lead to acidosis/coagulopathy Hypothermia causes peripheral vasoconstriction and impairs oxygen delivery
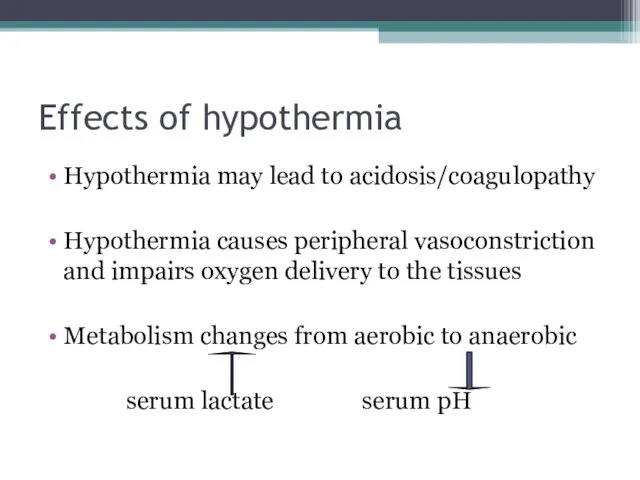
- 64. Prevention of hypothermia Cover patients with a dry sheet – keep head covered Pre-warm trauma room
- 65. Pain management Adequate analgesia imperative! DOC: Morphine Sulfate Dose: Adults: 0.1 – 0.2 mg/kg IVP Children:
- 66. Antibiotics Prophylactic antibiotics are not indicated in the early postburn period.
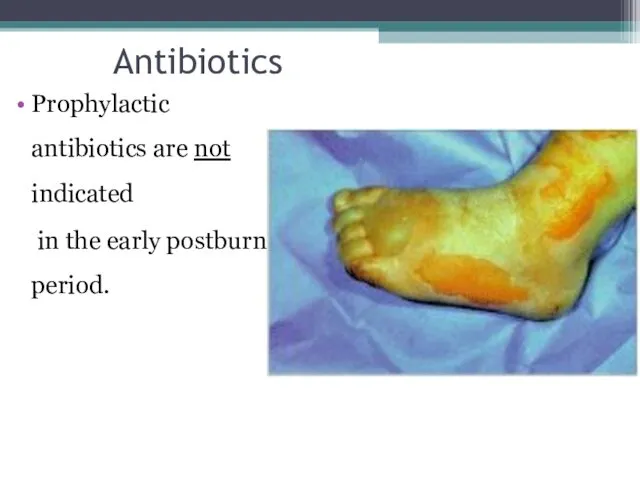
- 67. Other considerations Check tetanus status – administer Td as appropriate Debride and treat open blisters or
- 68. Electrical burns: are thermal injuries resulting from high intensity heat. The skin injury area may appear
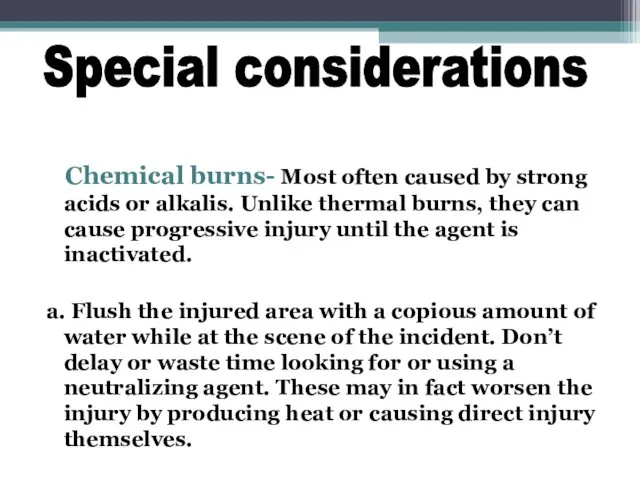
- 69. Chemical burns- Most often caused by strong acids or alkalis. Unlike thermal burns, they can cause
- 70. Burn Injury: Summary Many risk factors age dependent Pediatricians primary role: prevention High risk of multiple
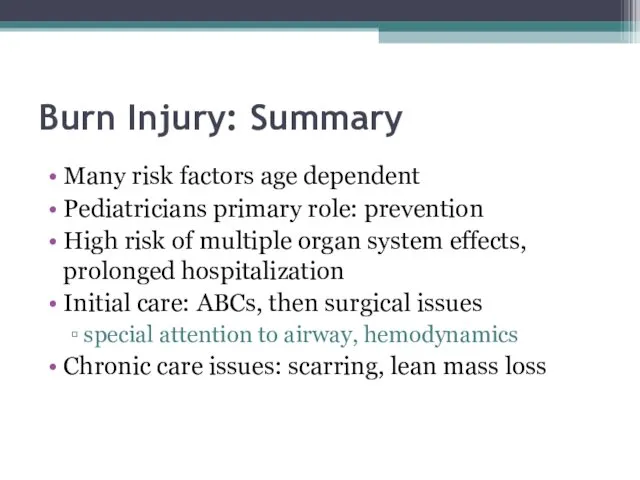
- 72. Скачать презентацию



 Медициналық технологияны бағалау бойынша жұмыс:практикалық сұрақтар
Медициналық технологияны бағалау бойынша жұмыс:практикалық сұрақтар Микрохирургическое отделение. Объемно-планировочные решения зданий
Микрохирургическое отделение. Объемно-планировочные решения зданий Нерв жүйесі ауруларын диагностикалаудың нейровизуализациялық әдістері
Нерв жүйесі ауруларын диагностикалаудың нейровизуализациялық әдістері Гемостаз. Механизмы и патология
Гемостаз. Механизмы и патология Электрокардиография. Электрофизиологические основы ЭКГ
Электрокардиография. Электрофизиологические основы ЭКГ Вирусные гепатиты А, В, С, Д и Е
Вирусные гепатиты А, В, С, Д и Е Диареи у детей
Диареи у детей Национальные клинические руководства в Казахстане: история развития, структура и внедрения
Национальные клинические руководства в Казахстане: история развития, структура и внедрения Психотропные средства
Психотропные средства Ботулизм (ихтиизм)
Ботулизм (ихтиизм) Патология красной крови. Диагностика анемий. Терминология. Классификация
Патология красной крови. Диагностика анемий. Терминология. Классификация Выбор препарата 1-ой линии терапии для лечения больных распространённым почечно-клеточным раком
Выбор препарата 1-ой линии терапии для лечения больных распространённым почечно-клеточным раком Лечебная физическая культура
Лечебная физическая культура Патология терморегуляции. Лекция № 8
Патология терморегуляции. Лекция № 8 Понятие боли
Понятие боли Ревматоидный артрит
Ревматоидный артрит Биохимия костной ткани. Лекция № 4
Биохимия костной ткани. Лекция № 4 Паренхиматозные дистрофии
Паренхиматозные дистрофии ВИЧ-инфекция. Классификация, клиника, лечение
ВИЧ-инфекция. Классификация, клиника, лечение Периферическая венозная катетеризация
Периферическая венозная катетеризация Жүйке жүйесі мен тері жабындыларының туа біткен ақаулары
Жүйке жүйесі мен тері жабындыларының туа біткен ақаулары Современные подходы к лечению хронической сердечной недостаточности
Современные подходы к лечению хронической сердечной недостаточности Клиническая анатомия слабых мест передней брюшной стенки и диафрагмы
Клиническая анатомия слабых мест передней брюшной стенки и диафрагмы Ветеринарно-санітарна оцінка риби при філометроїдозі
Ветеринарно-санітарна оцінка риби при філометроїдозі Личная гигиена младшего школьника
Личная гигиена младшего школьника Действие массажа на кожу
Действие массажа на кожу Группа компаний Росгосстрах. Программа страхования Международная медицинская помощь
Группа компаний Росгосстрах. Программа страхования Международная медицинская помощь Защитные функции антител
Защитные функции антител