Содержание
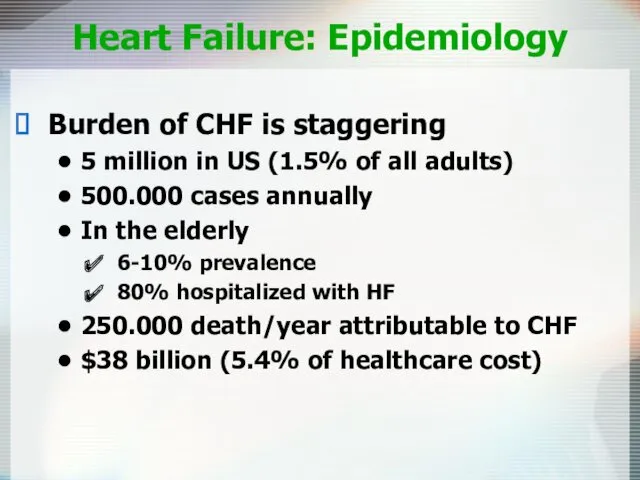
- 2. Heart Failure: Epidemiology Burden of CHF is staggering 5 million in US (1.5% of all adults)
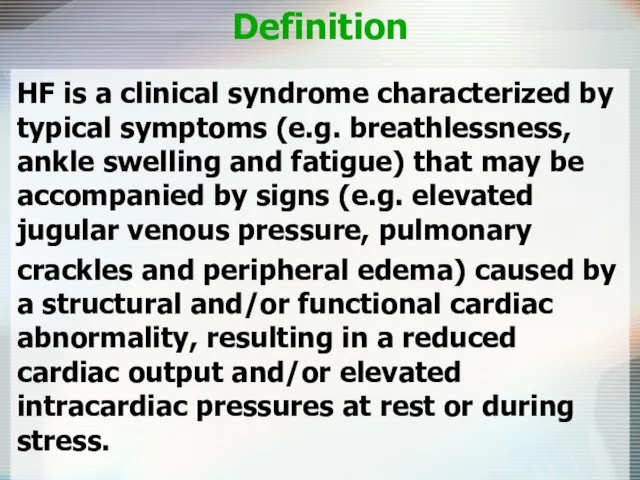
- 3. Definition HF is a clinical syndrome characterized by typical symptoms (e.g. breathlessness, ankle swelling and fatigue)
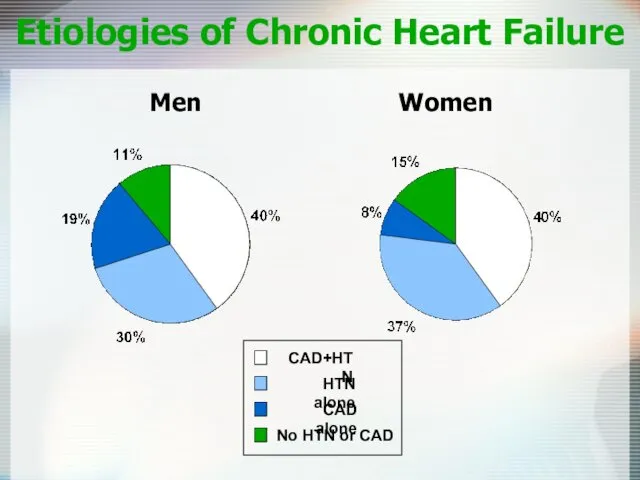
- 5. Etiologies of Chronic Heart Failure Men Women
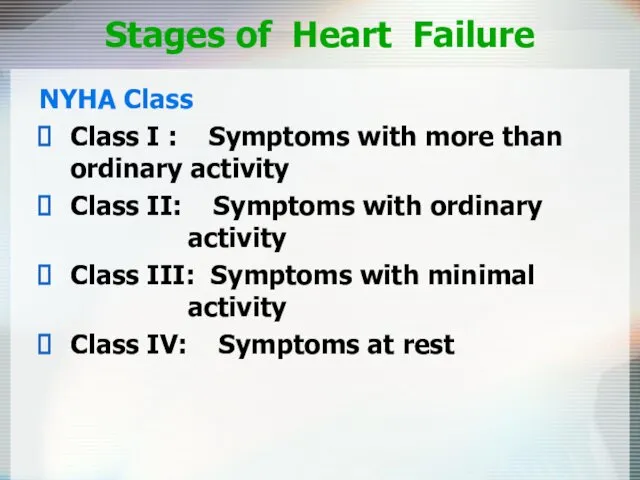
- 6. Stages of Heart Failure NYHA Class Class I : Symptoms with more than ordinary activity Class
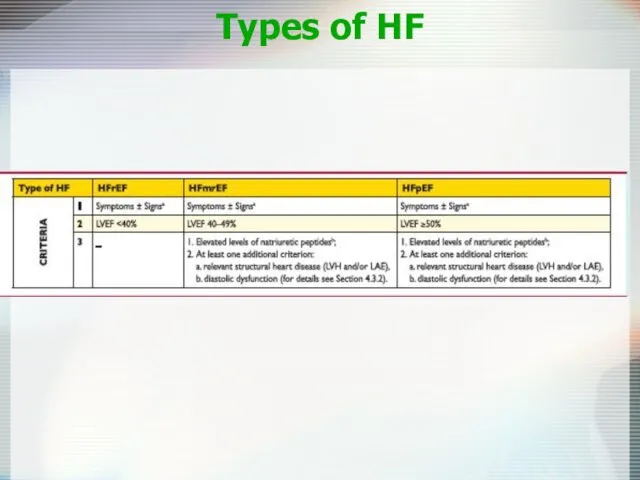
- 7. Types of HF
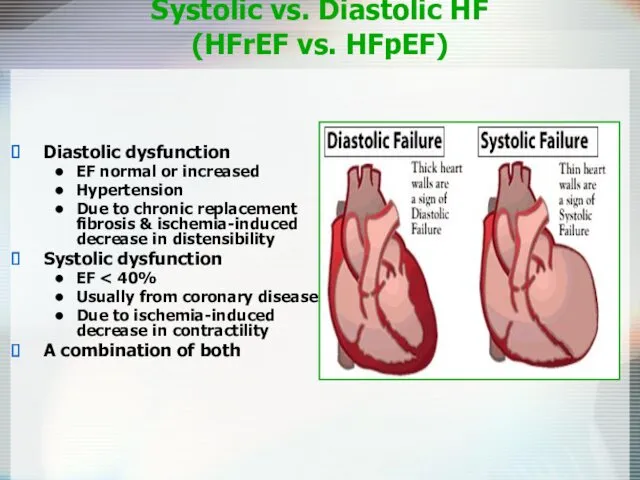
- 8. Systolic vs. Diastolic HF (HFrEF vs. HFpEF) Diastolic dysfunction EF normal or increased Hypertension Due to
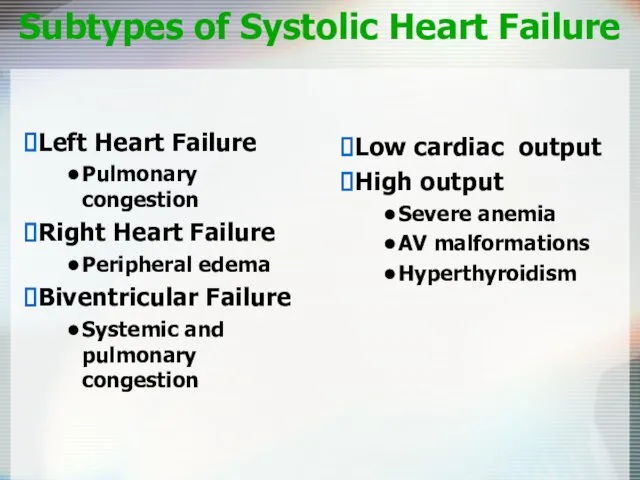
- 9. Subtypes of Systolic Heart Failure Low cardiac output High output Severe anemia AV malformations Hyperthyroidism Left
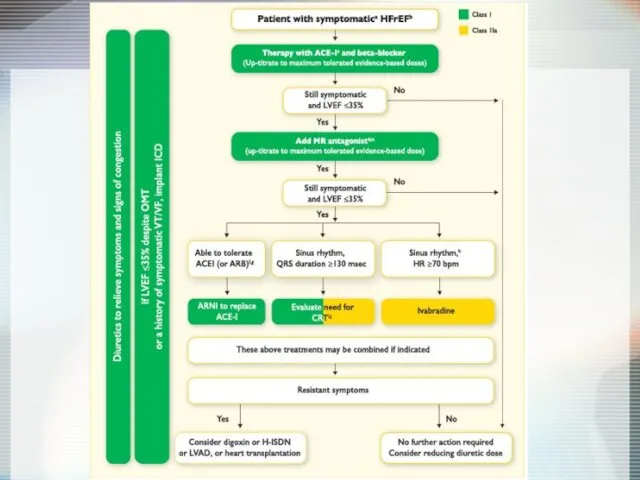
- 10. Principles of Treatment Systolic HF ↓ Preload ↓ Afterload ↑ Inotropism ↓ Neurohumoral activity ACE-I, β-blockers,
- 11. Management of Heart Failure Therapies ACE-Inhibitors Beta Blockers Aldactone Diuretics Digoxin Recent non-Pharmacological Advances Sudden death
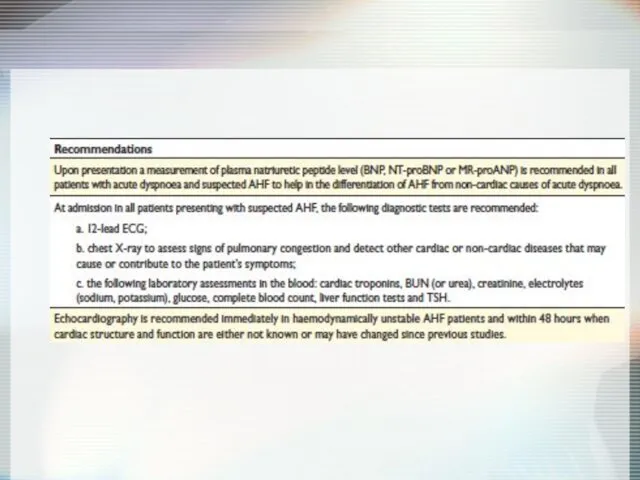
- 12. Diagnosis of HF Anamnesis Chest X-Ray ECG Echocardiography Cardiac catheterization: coronary angiography and Rt heart catheterization
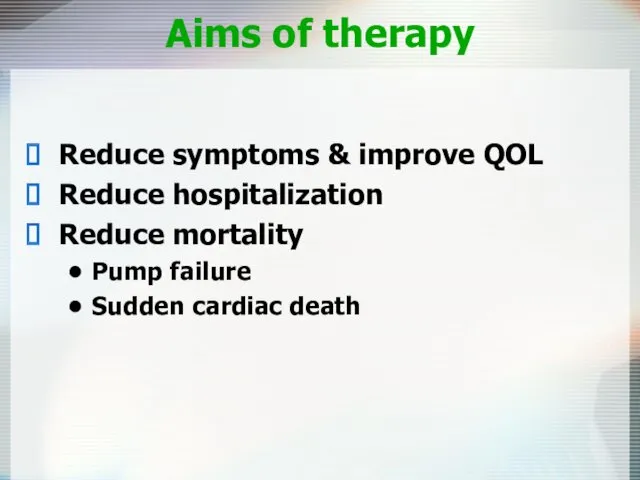
- 14. Aims of therapy Reduce symptoms & improve QOL Reduce hospitalization Reduce mortality Pump failure Sudden cardiac
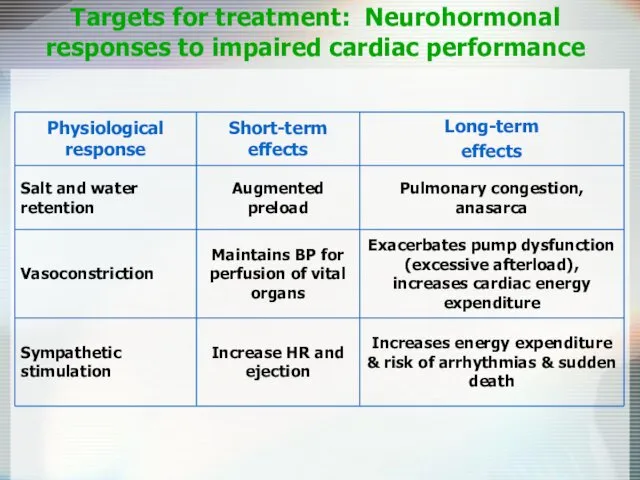
- 15. Targets for treatment: Neurohormonal responses to impaired cardiac performance
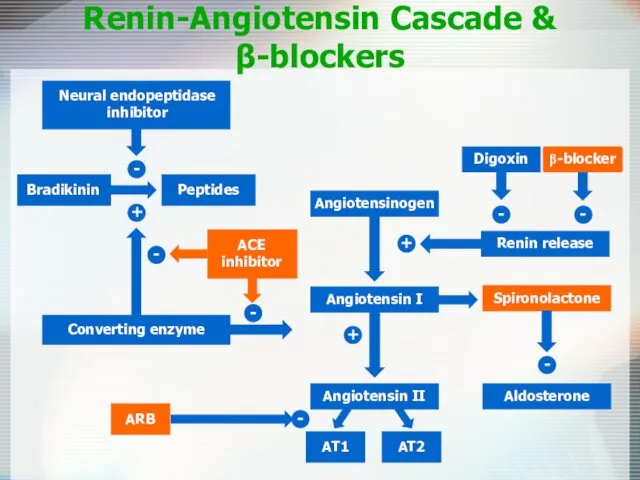
- 16. Renin-Angiotensin Cascade & β-blockers Angiotensinogen Angiotensin II AT1 AT2 Aldosterone - + + Spironolactone - -
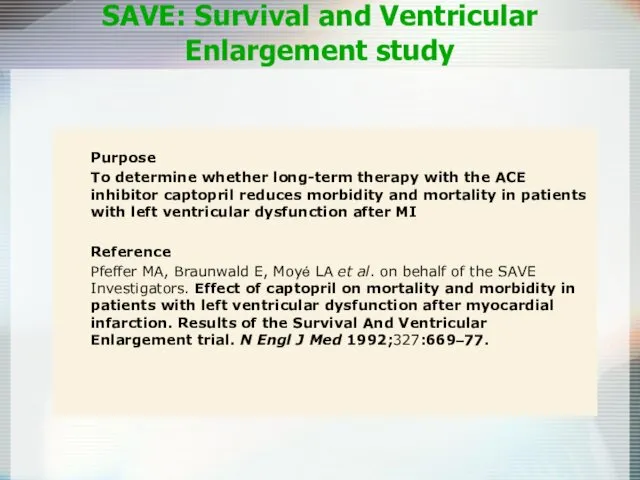
- 17. Purpose To determine whether long-term therapy with the ACE inhibitor captopril reduces morbidity and mortality in
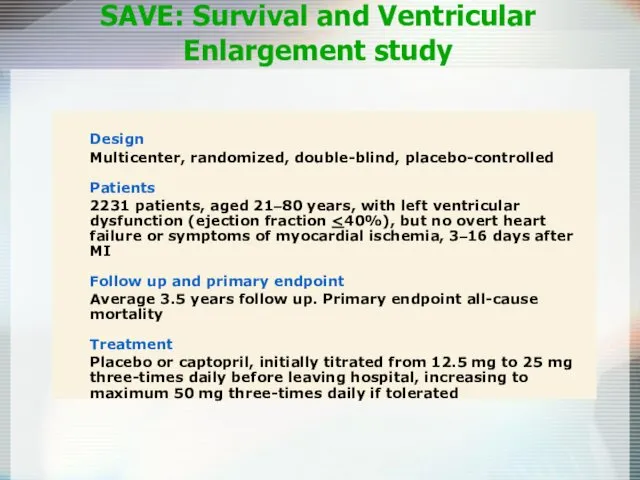
- 18. Design Multicenter, randomized, double-blind, placebo-controlled Patients 2231 patients, aged 21–80 years, with left ventricular dysfunction (ejection
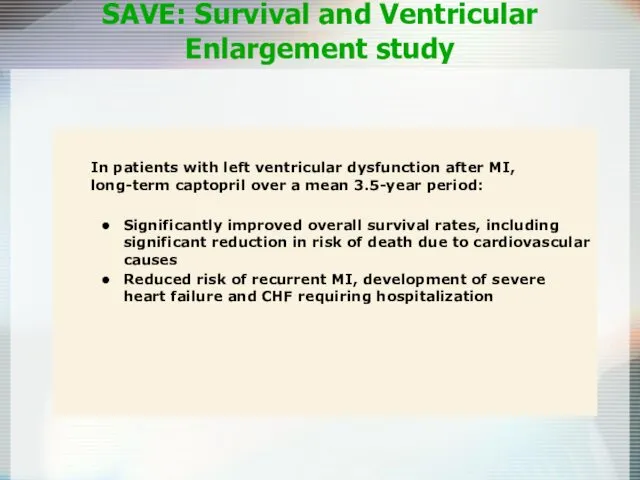
- 19. In patients with left ventricular dysfunction after MI, long-term captopril over a mean 3.5-year period: Significantly
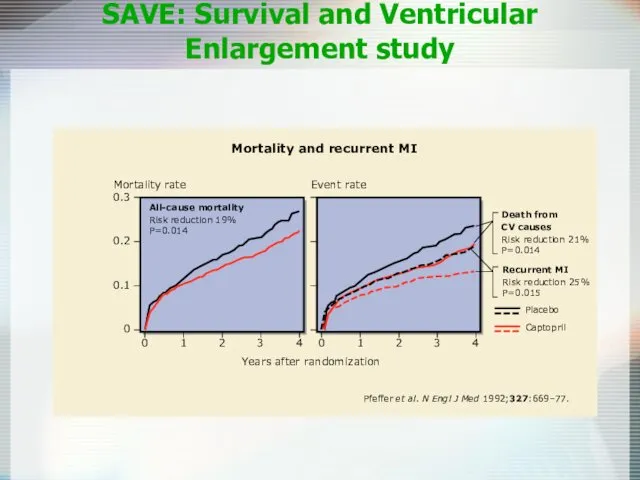
- 20. 0 0 1 2 4 3 0.3 0.2 0.1 Mortality and recurrent MI Years after randomization
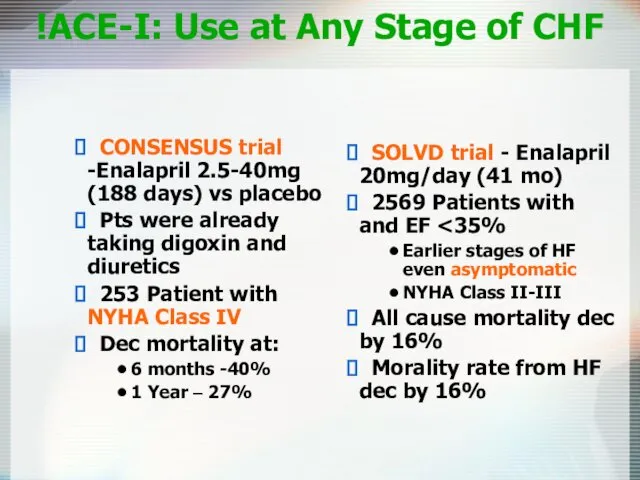
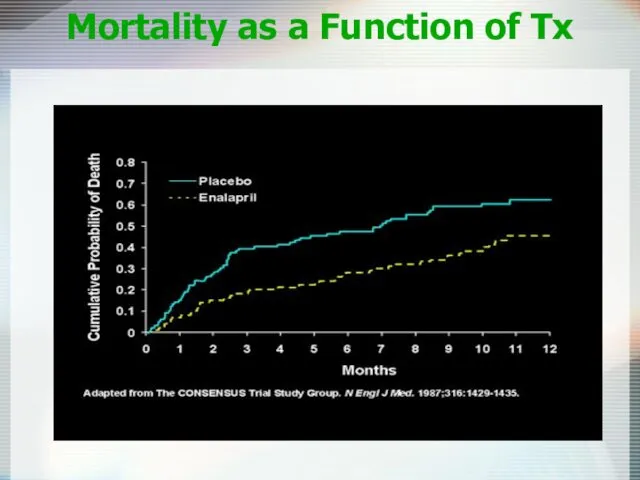
- 21. ACE-I: Use at Any Stage of CHF! SOLVD trial - Enalapril 20mg/day (41 mo) 2569 Patients
- 22. Mortality as a Function of Tx
- 23. Angiotensin-Receptor Blockers Comparable to ACE inhibitors Reduce all-cause mortality Suitable alternative for patient with adverse events
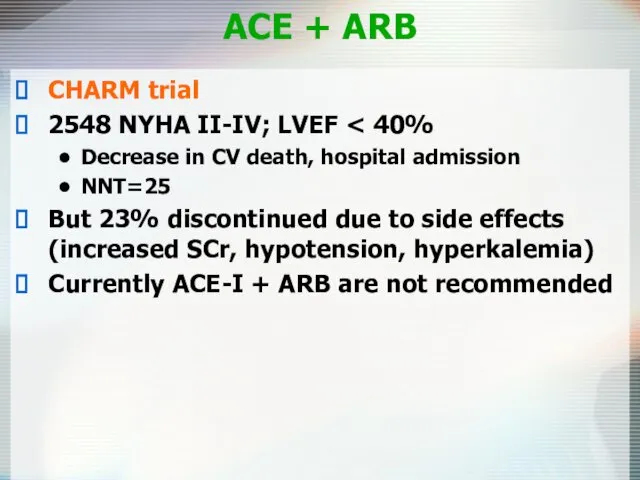
- 24. ACE + ARB CHARM trial 2548 NYHA II-IV; LVEF Decrease in CV death, hospital admission NNT=25
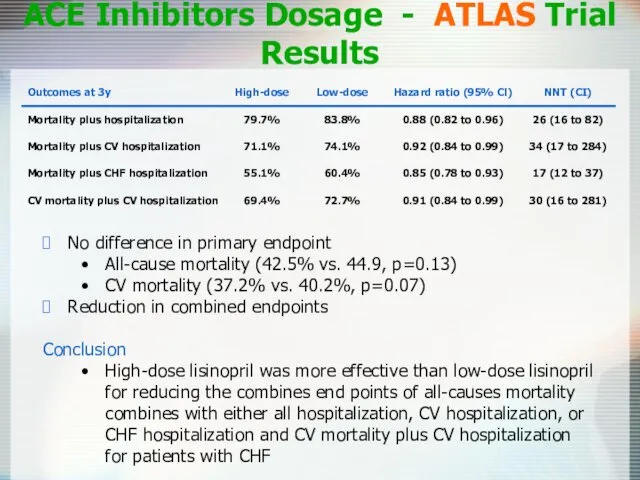
- 25. ACE Inhibitors Dosage - ATLAS Trial Results No difference in primary endpoint All-cause mortality (42.5% vs.
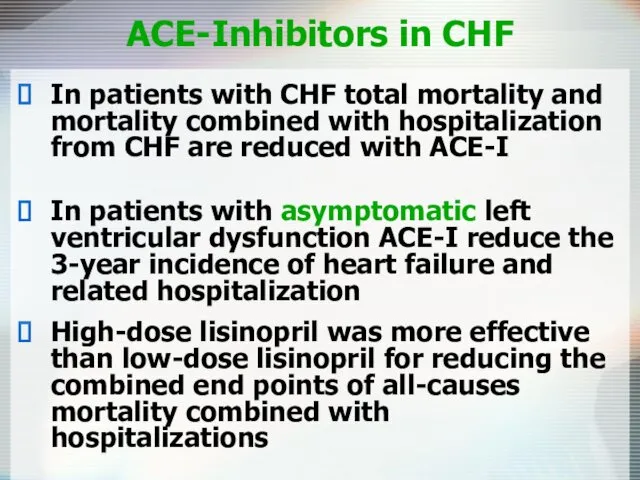
- 26. ACE-Inhibitors in CHF In patients with CHF total mortality and mortality combined with hospitalization from CHF
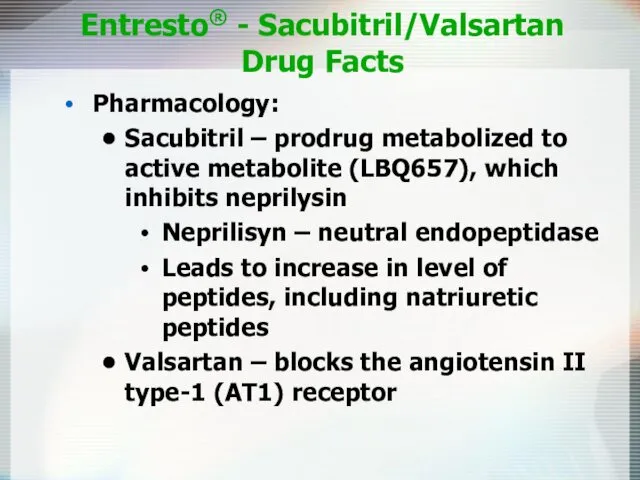
- 27. Entresto® - Sacubitril/Valsartan Drug Facts Pharmacology: Sacubitril – prodrug metabolized to active metabolite (LBQ657), which inhibits
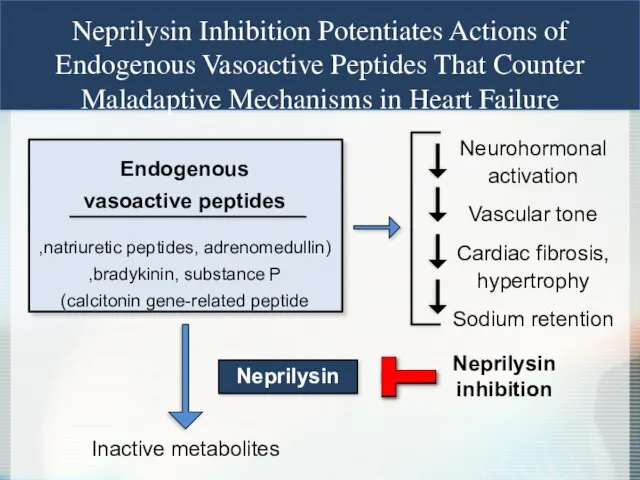
- 28. Neprilysin Inhibition Potentiates Actions of Endogenous Vasoactive Peptides That Counter Maladaptive Mechanisms in Heart Failure Endogenous
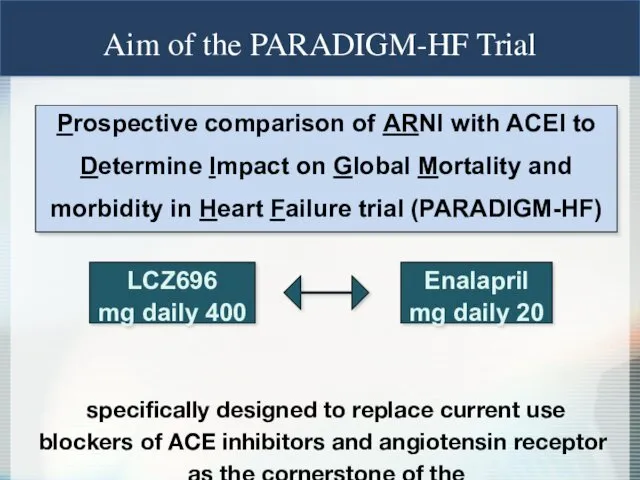
- 29. Prospective comparison of ARNI with ACEI to Determine Impact on Global Mortality and morbidity in Heart
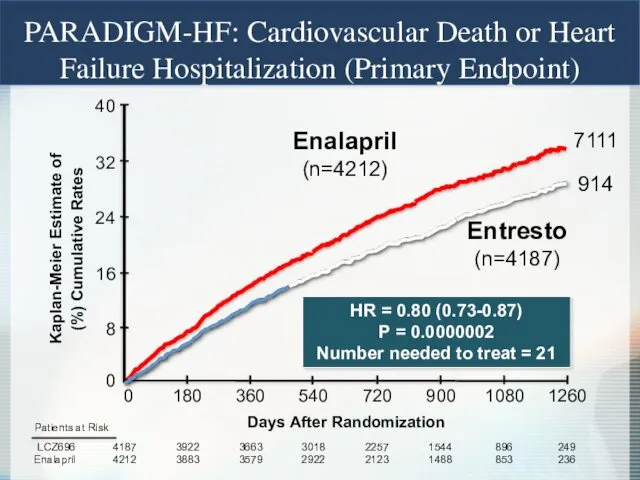
- 30. 0 16 32 40 24 8 Enalapril (n=4212) 360 720 1080 0 180 540 900 1260
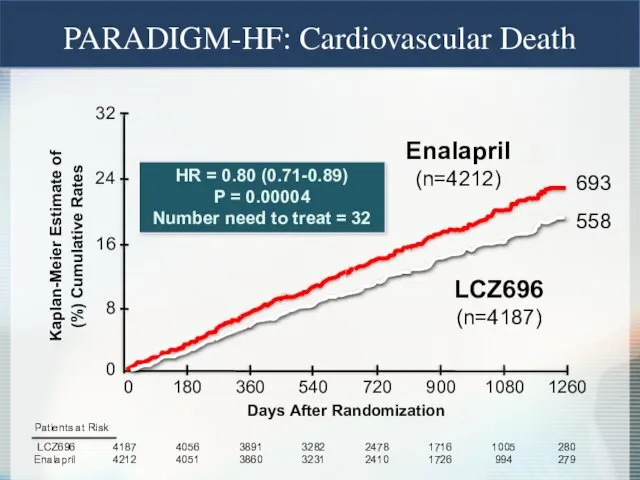
- 31. Enalapril (n=4212) LCZ696 (n=4187) HR = 0.80 (0.71-0.89) P = 0.00004 Number need to treat =
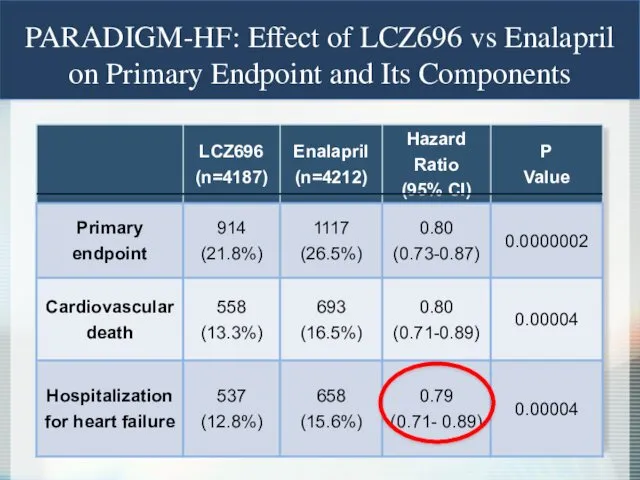
- 32. PARADIGM-HF: Effect of LCZ696 vs Enalapril on Primary Endpoint and Its Components
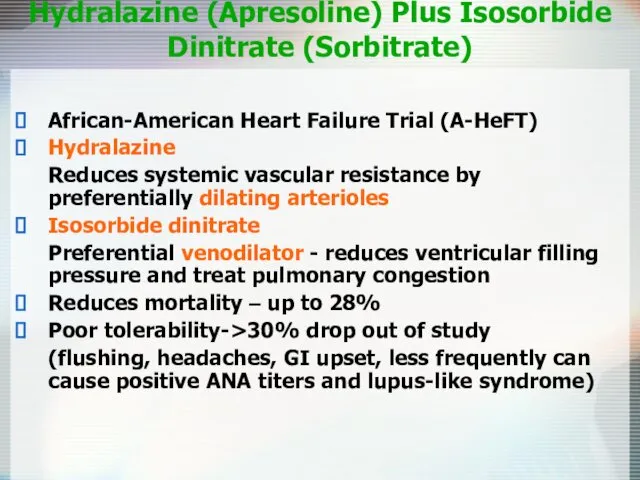
- 33. Hydralazine (Apresoline) Plus Isosorbide Dinitrate (Sorbitrate) African-American Heart Failure Trial (A-HeFT) Hydralazine Reduces systemic vascular resistance
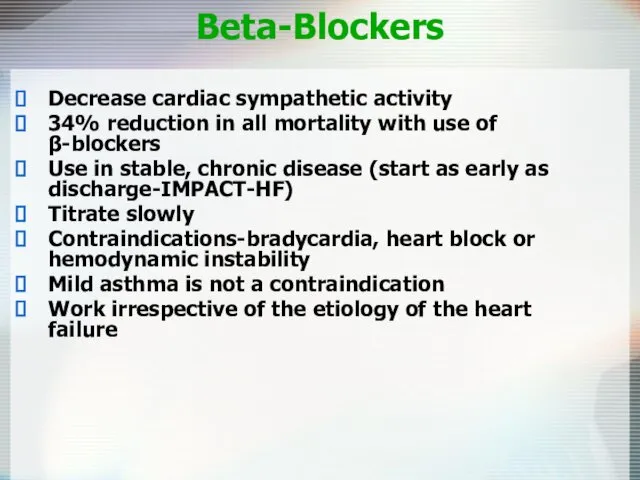
- 34. Beta-Blockers Decrease cardiac sympathetic activity 34% reduction in all mortality with use of β-blockers Use in
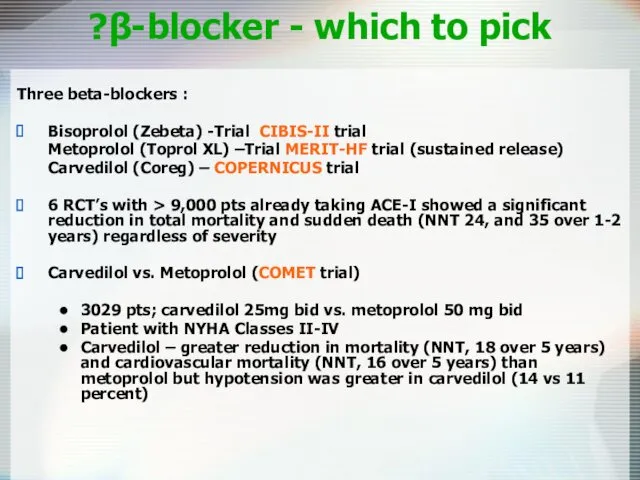
- 35. β-blocker - which to pick? Three beta-blockers : Bisoprolol (Zebeta) -Trial CIBIS-II trial Metoprolol (Toprol XL)
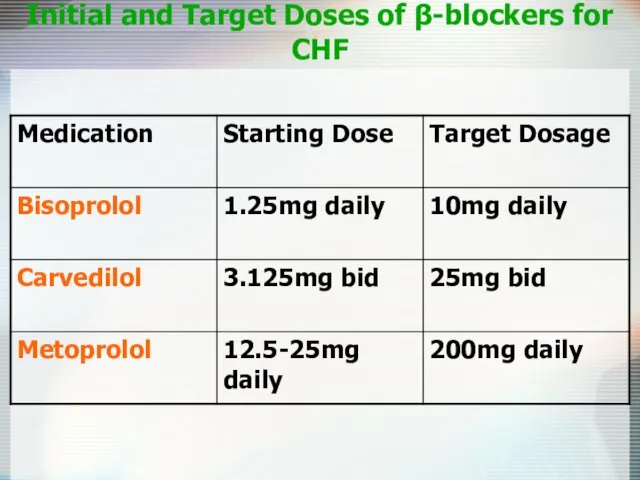
- 36. Initial and Target Doses of β-blockers for CHF
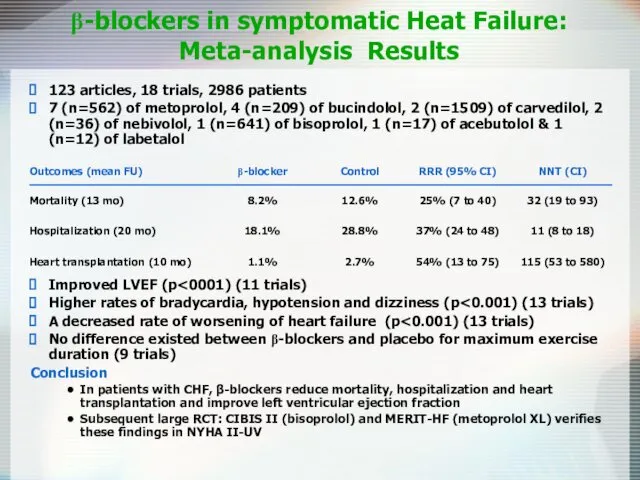
- 37. β-blockers in symptomatic Heat Failure: Meta-analysis Results 123 articles, 18 trials, 2986 patients 7 (n=562) of
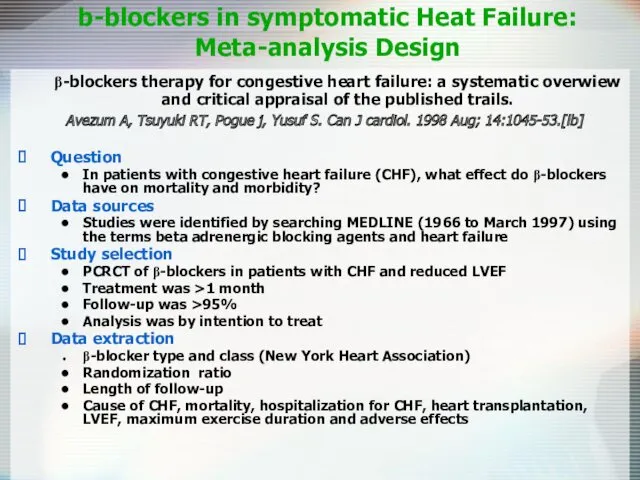
- 38. β-blockers therapy for congestive heart failure: a systematic overwiew and critical appraisal of the published trails.
- 39. Digoxin May relieve symptoms, does not reduce mortality Pts taking digoxin are less likely to be
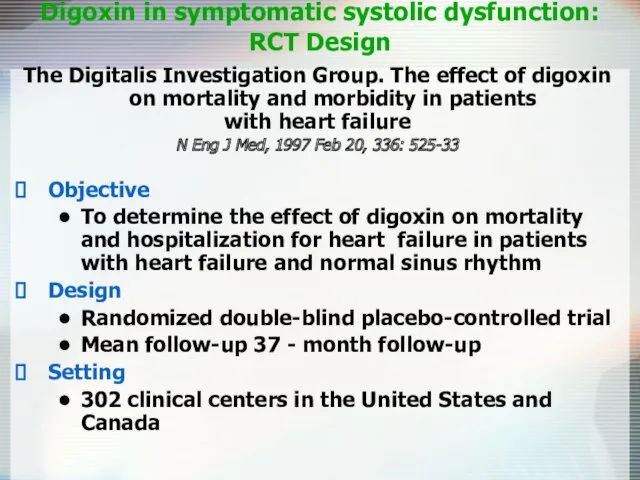
- 40. The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart
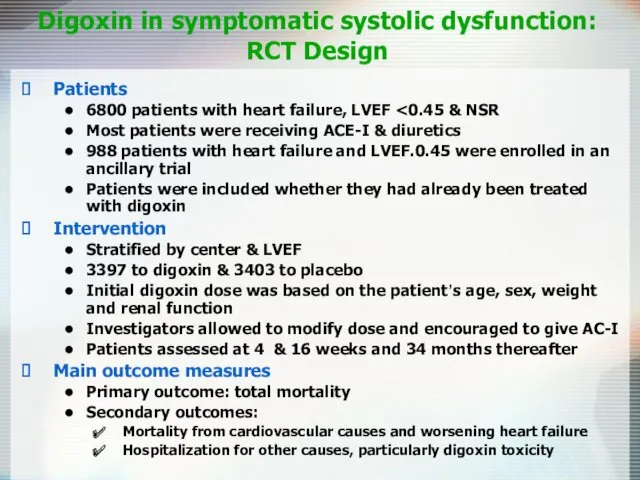
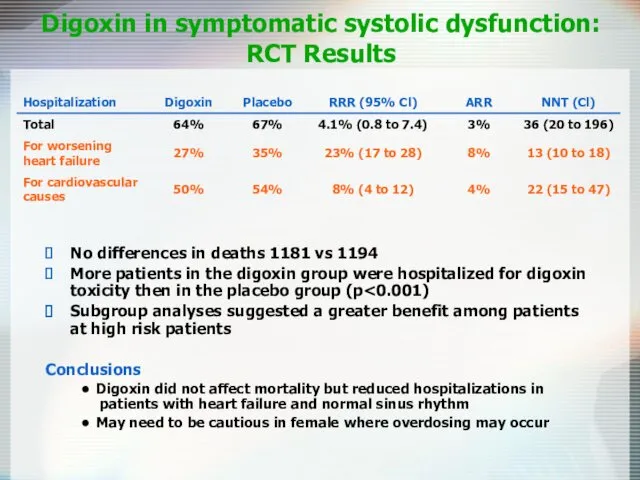
- 41. Digoxin in symptomatic systolic dysfunction: RCT Design Patients 6800 patients with heart failure, LVEF Most patients
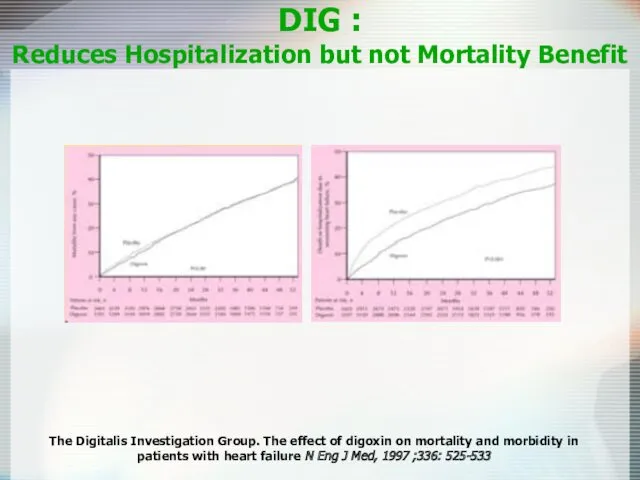
- 42. DIG : Reduces Hospitalization but not Mortality Benefit The Digitalis Investigation Group. The effect of digoxin
- 43. Digoxin in symptomatic systolic dysfunction: RCT Results No differences in deaths 1181 vs 1194 More patients
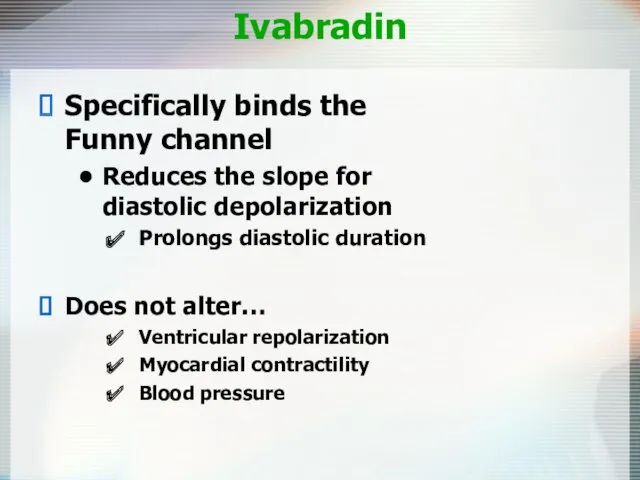
- 44. Ivabradin Specifically binds the Funny channel Reduces the slope for diastolic depolarization Prolongs diastolic duration Does
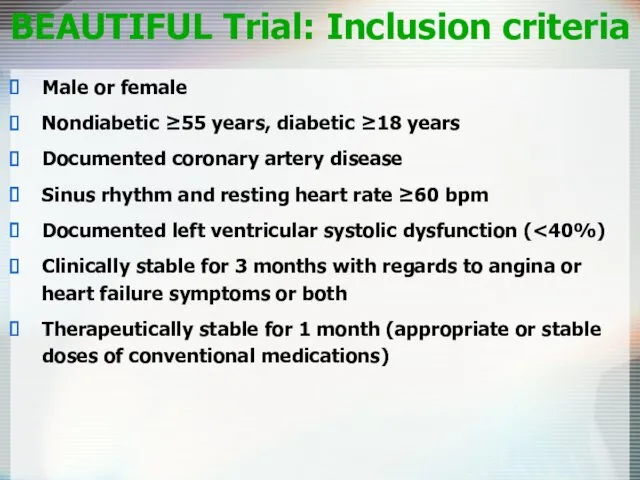
- 45. BEAUTIFUL Trial: Inclusion criteria Male or female Nondiabetic ≥55 years, diabetic ≥18 years Documented coronary artery
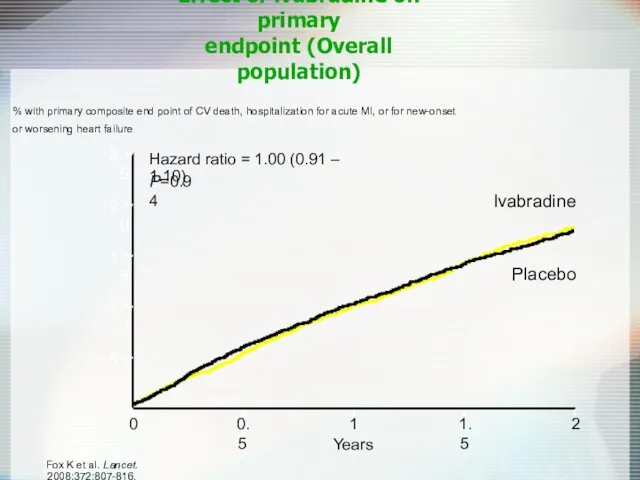
- 46. Effect of ivabradine on primary endpoint (Overall population) % with primary composite end point of CV
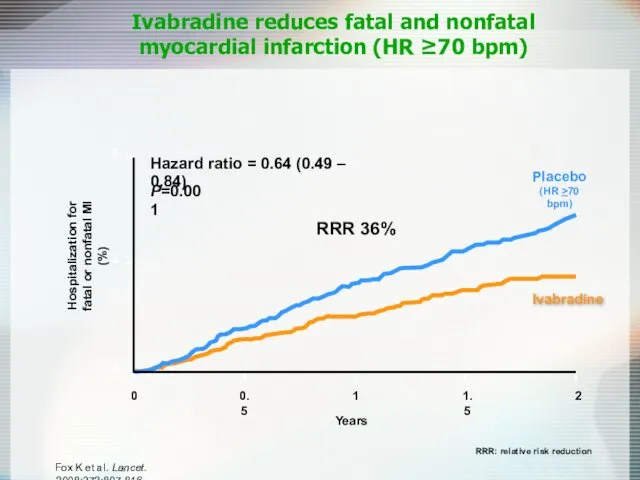
- 47. Ivabradine reduces fatal and nonfatal myocardial infarction (HR ≥70 bpm) Hospitalization for fatal or nonfatal MI
- 48. Ivabradine In patients with coronary artery disease and left ventricular dysfunction, those with a heart rate
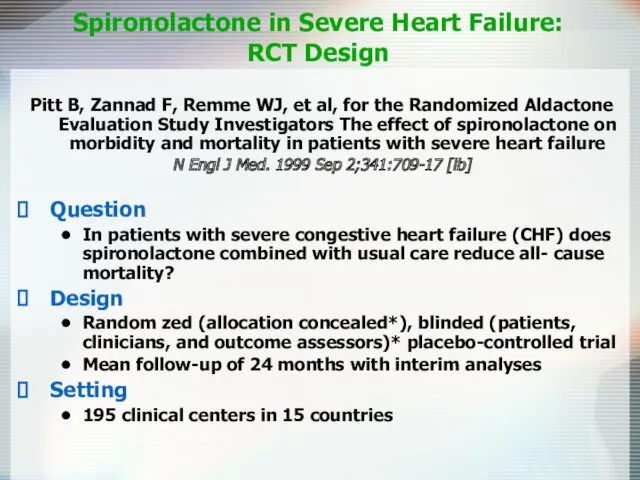
- 49. Spironolactone in Severe Heart Failure: RCT Design Pitt B, Zannad F, Remme WJ, et al, for
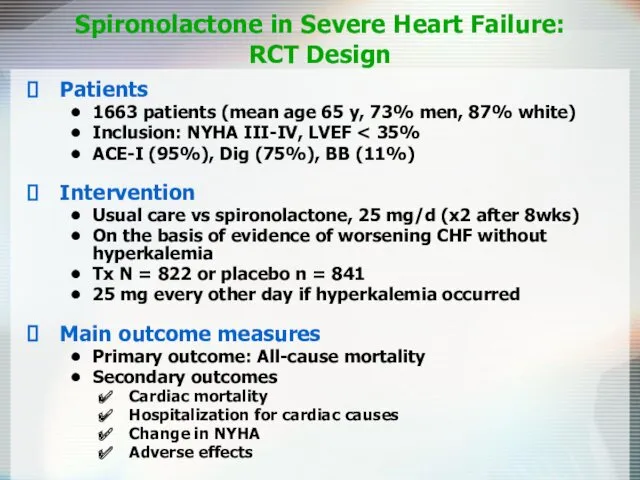
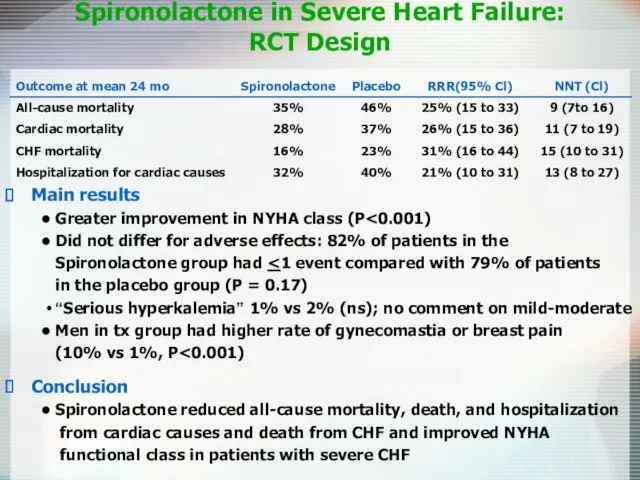
- 50. Spironolactone in Severe Heart Failure: RCT Design Patients 1663 patients (mean age 65 y, 73% men,
- 51. Spironolactone in Severe Heart Failure: RCT Design Main results Greater improvement in NYHA class (P Did
- 52. Eplerenone Post-AMI Heart Failure Efficacy and Survival Study EPHESUS Trial
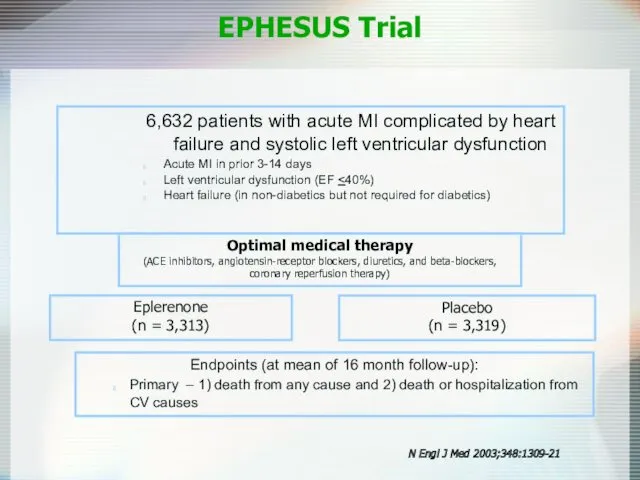
- 53. Eplerenone (n = 3,313) Placebo (n = 3,319) Endpoints (at mean of 16 month follow-up): Primary
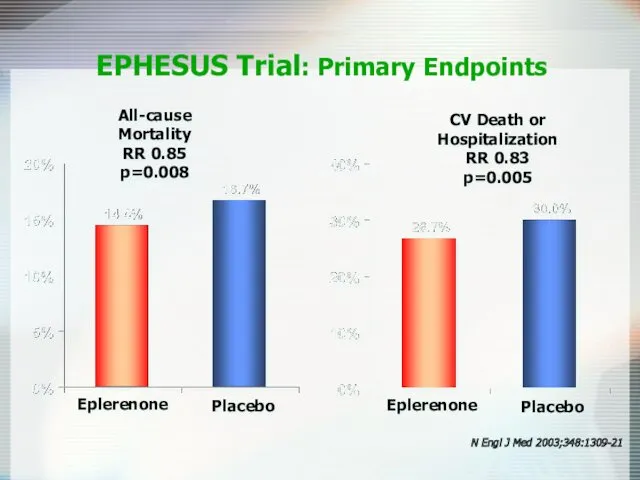
- 54. All-cause Mortality RR 0.85 p=0.008 EPHESUS Trial: Primary Endpoints CV Death or Hospitalization RR 0.83 p=0.005
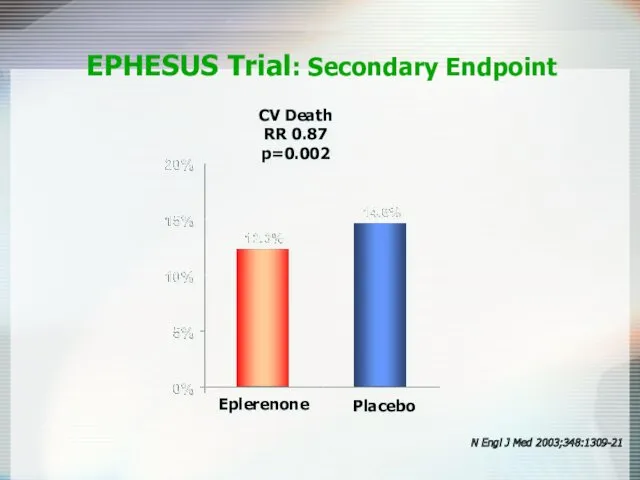
- 55. CV Death RR 0.87 p=0.002 EPHESUS Trial: Secondary Endpoint N Engl J Med 2003;348:1309-21 Eplerenone Placebo
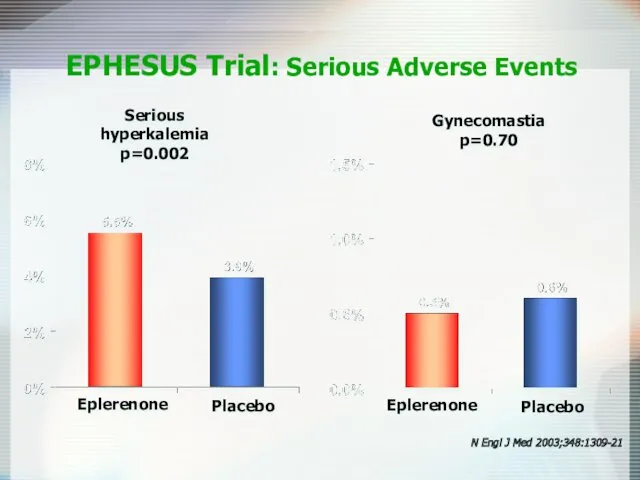
- 56. Serious hyperkalemia p=0.002 EPHESUS Trial: Serious Adverse Events Gynecomastia p=0.70 Eplerenone Placebo N Engl J Med
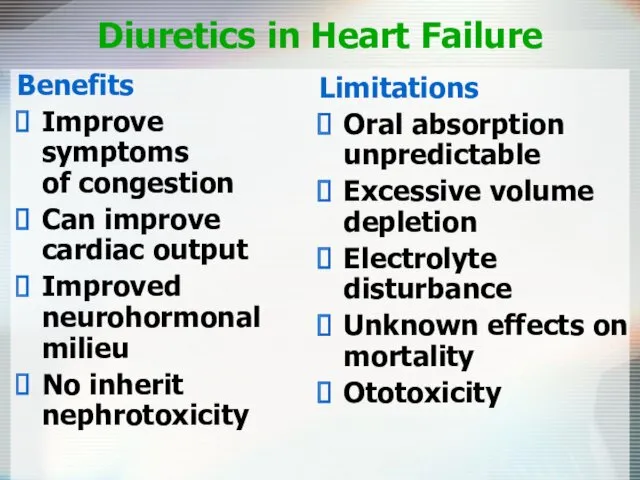
- 57. Loop Diuretics Mainstay of symptomatic treatment Improve fluid retention Increase exercise tolerance No effects on morbidity
- 58. Diuretics in Heart Failure Benefits Improve symptoms of congestion Can improve cardiac output Improved neurohormonal milieu
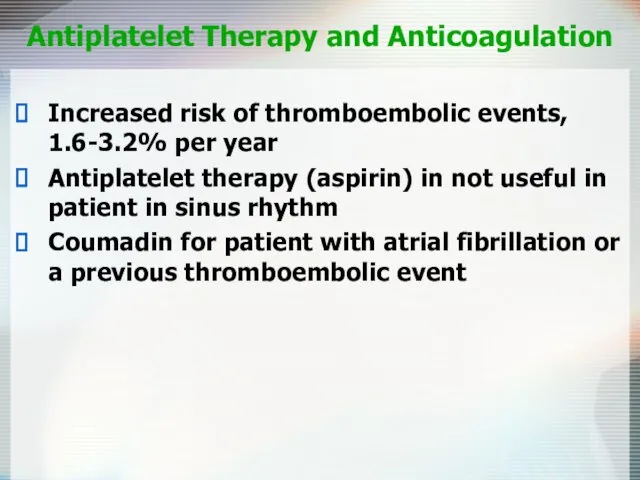
- 59. Antiplatelet Therapy and Anticoagulation Increased risk of thromboembolic events, 1.6-3.2% per year Antiplatelet therapy (aspirin) in
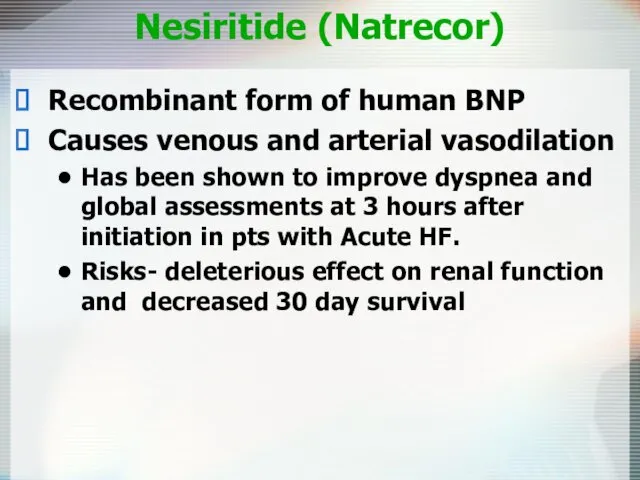
- 60. Nesiritide (Natrecor) Recombinant form of human BNP Causes venous and arterial vasodilation Has been shown to
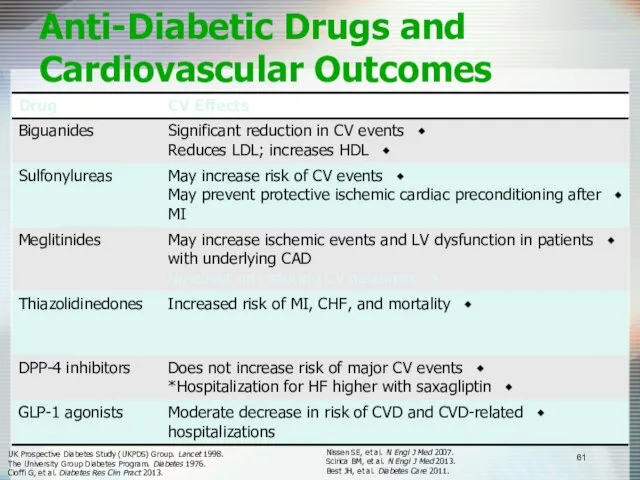
- 61. Anti-Diabetic Drugs and Cardiovascular Outcomes UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998. The University Group
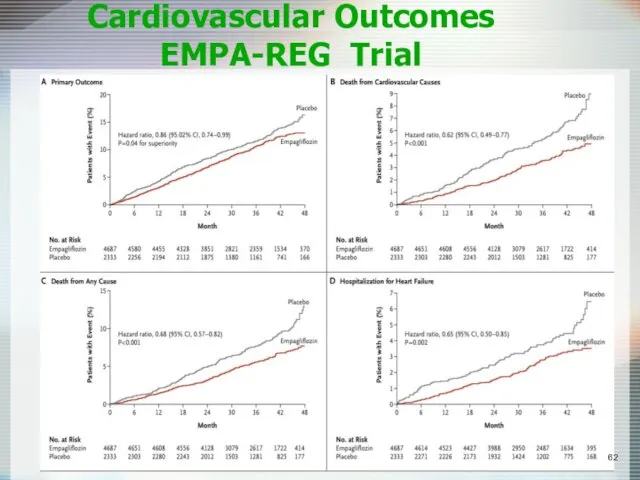
- 62. Cardiovascular Outcomes EMPA-REG Trial
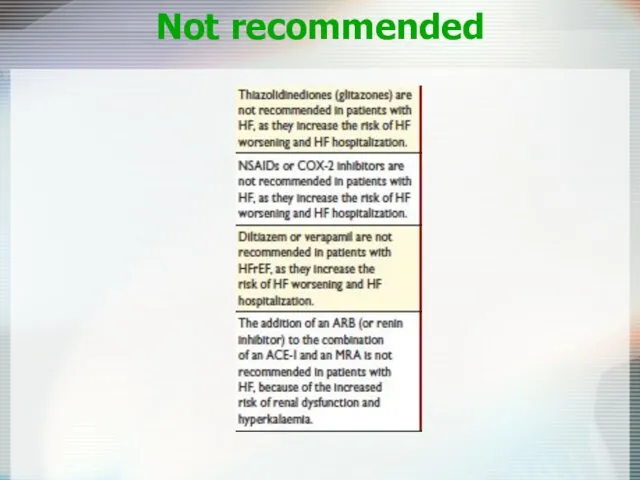
- 63. Not recommended
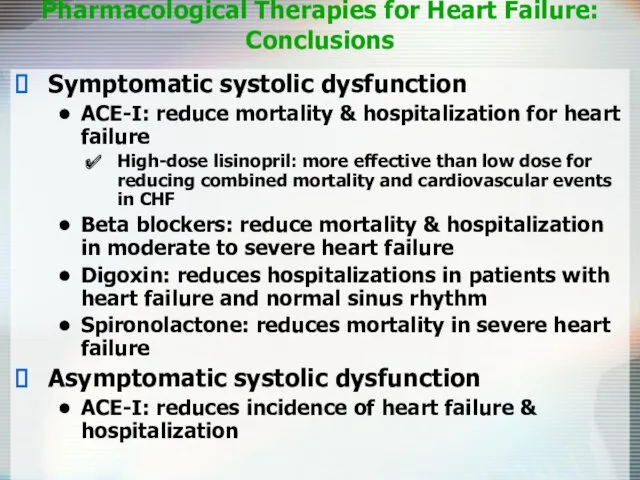
- 64. Pharmacological Therapies for Heart Failure: Conclusions Symptomatic systolic dysfunction ACE-I: reduce mortality & hospitalization for heart
- 65. Device Therapy Implantable Cardioverter-Defibrillators (ICD) Cardiac Resynchronization Therapy (CRT) Left Ventricular Assist Devices (LVAD)
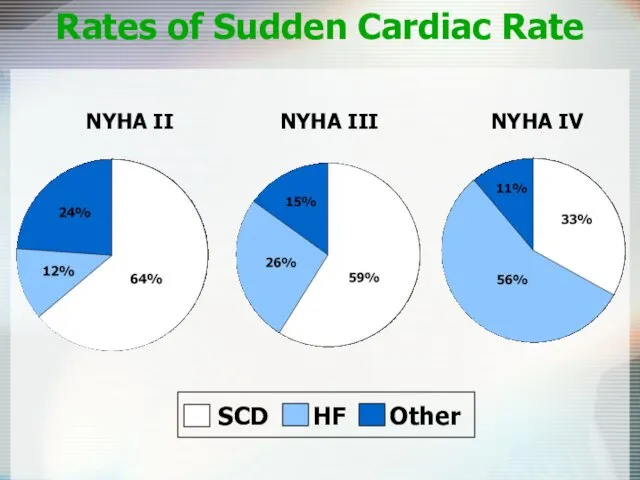
- 66. Rates of Sudden Cardiac Rate NYHA II NYHA III NYHA IV
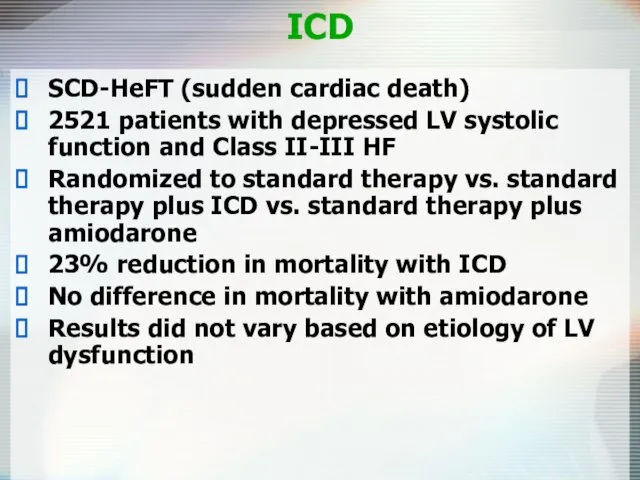
- 67. ICD SCD-HeFT (sudden cardiac death) 2521 patients with depressed LV systolic function and Class II-III HF
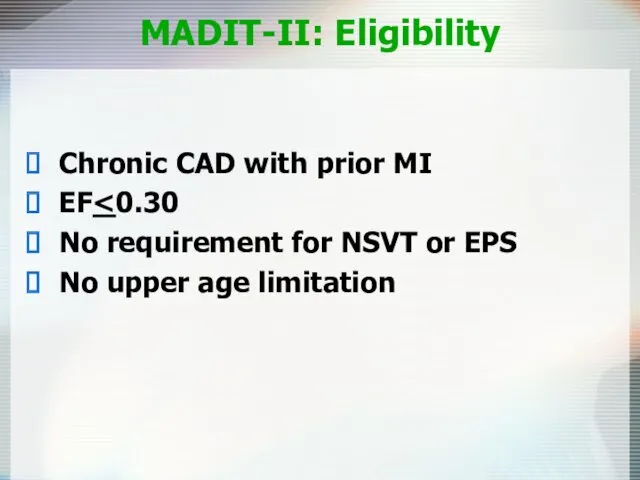
- 68. MADIT-II: Eligibility Chronic CAD with prior MI EF No requirement for NSVT or EPS No upper
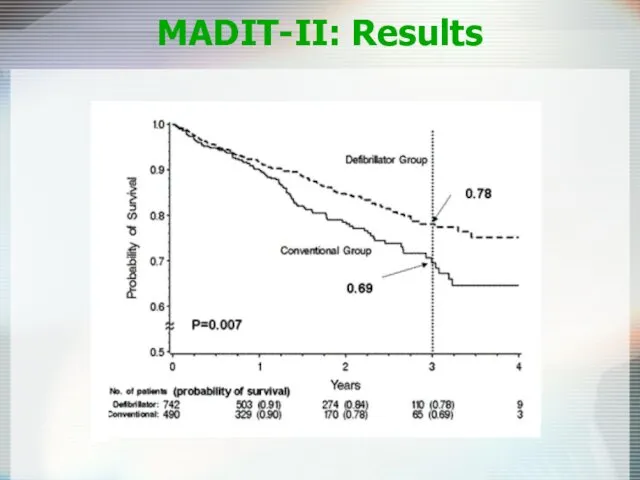
- 69. MADIT-II: Results
- 70. ICD Recommended in pts with EF Survival with good functional capacity is anticipated for > 1
- 71. Cardiac Resynchronization Therapy Patient Indications CRT device: Moderate to severe HF (NYHA Class III/IV) patients Symptomatic
- 72. CRT COMPANION trial 1520 patients, most with class III-IV HF, QRS duration >120 ms Randomized in
- 73. Conclusions ACE inhibitors improve symptoms in CCF (CONSENSUS) and reduce mortality even in asymptomatic patients with
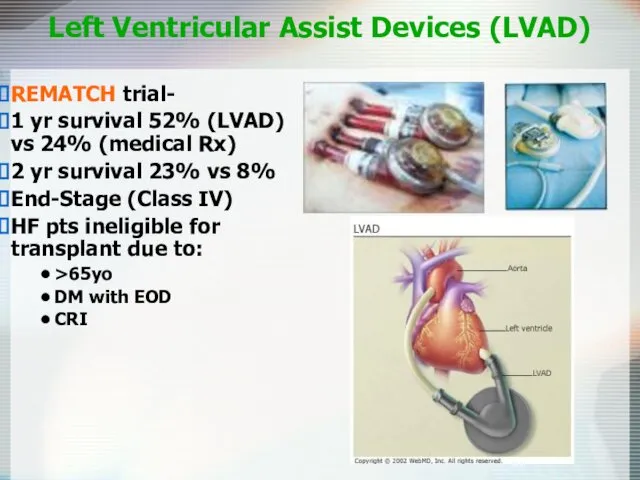
- 74. Left Ventricular Assist Devices (LVAD) REMATCH trial- 1 yr survival 52% (LVAD) vs 24% (medical Rx)
- 75. Diastolic Dysfunction 20-40% of presenting CHF syndrome Risk of death lower than systolic dysfunction Dx: Doppler
- 76. Diastolic Dysfunction Acute Management is the SAME Chronic Management is CONTROVERSIAL Diuretics-dec fluid volume CCB-promote left
- 77. Heart Failure: More than just drugs Dietary counseling Patient education Physical activity Medication compliance Aggressive follow-up
- 80. Скачать презентацию
 Компоненты и основные этапы общей анестезии. Классификация видов обезболивания
Компоненты и основные этапы общей анестезии. Классификация видов обезболивания Хирургическая рана. Процесс заживления раны и его нарушения
Хирургическая рана. Процесс заживления раны и его нарушения Жоғарғы тыныс жолдарының аурулары. Ринит. Трахеит. Ларингит
Жоғарғы тыныс жолдарының аурулары. Ринит. Трахеит. Ларингит Заболевания желудка и двенадцатиперсной кишки. Лекция №3
Заболевания желудка и двенадцатиперсной кишки. Лекция №3 Колоректальный рак
Колоректальный рак Наркотики и беременность
Наркотики и беременность Көктамырға егу жасау техникасы жəне қан алу
Көктамырға егу жасау техникасы жəне қан алу Анестезиология и реаниматология. Введение в дисциплину
Анестезиология и реаниматология. Введение в дисциплину Терморегуляция организма. Закаливание
Терморегуляция организма. Закаливание Психотропные средства. Нейролептики. Транквилизакторы. Седативные средства
Психотропные средства. Нейролептики. Транквилизакторы. Седативные средства Папулосквамозні та бульозні дерматози
Папулосквамозні та бульозні дерматози Атопический дерматит
Атопический дерматит Гормоны
Гормоны Синдром эмоционального выгорания. Распространенность синдрома
Синдром эмоционального выгорания. Распространенность синдрома Травматизм. Виды травматизма. Травматический токсикоз. Травмы головы, груди, живота
Травматизм. Виды травматизма. Травматический токсикоз. Травмы головы, груди, живота Функциональные пробы и тесты, применяемые для оценки функционального состояния организма
Функциональные пробы и тесты, применяемые для оценки функционального состояния организма Основы эпидемиологии, инфекционные заболевания
Основы эпидемиологии, инфекционные заболевания Бактериальный вагиноз при беременности
Бактериальный вагиноз при беременности Ас қорыту жүйесі. Сүт тістерінің құрылыс ерекшелігі. Тіс алмасу
Ас қорыту жүйесі. Сүт тістерінің құрылыс ерекшелігі. Тіс алмасу Балалардағы хейлиттер
Балалардағы хейлиттер Миома матки
Миома матки Предмет и задачи патофизиологии
Предмет и задачи патофизиологии Процессы адаптации и компенсации. Регенерация и репарация. Склероз
Процессы адаптации и компенсации. Регенерация и репарация. Склероз Хроническая обструктивная болезнь легких
Хроническая обструктивная болезнь легких Одонтогенные флегмоны челюстно-лицевой области
Одонтогенные флегмоны челюстно-лицевой области Основные законы гемодинамики и их математическое выражение
Основные законы гемодинамики и их математическое выражение Weight Loss Challenge. Бросьте вызов лишнему весу. Углеводы, сахар и гликемический индекс
Weight Loss Challenge. Бросьте вызов лишнему весу. Углеводы, сахар и гликемический индекс Рак мочевого пузыря
Рак мочевого пузыря