Содержание
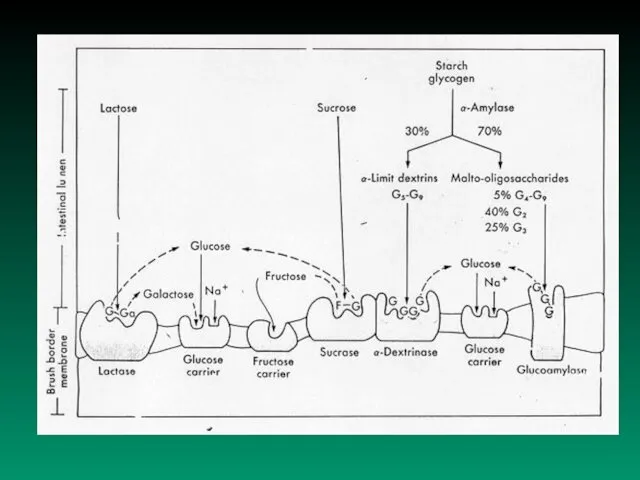
- 2. A. Physiologic remarks: Carbohydrates are present in food in various forms: 1. simple sugars - monosaccharides
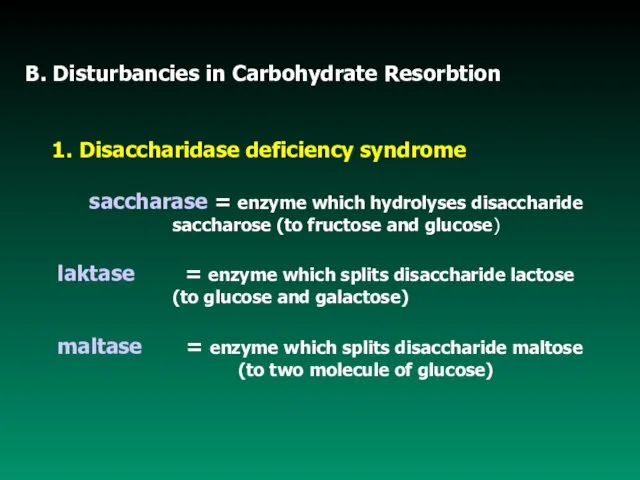
- 5. B. Disturbancies in Carbohydrate Resorbtion 1. Disaccharidase deficiency syndrome saccharase = enzyme which hydrolyses disaccharide saccharose
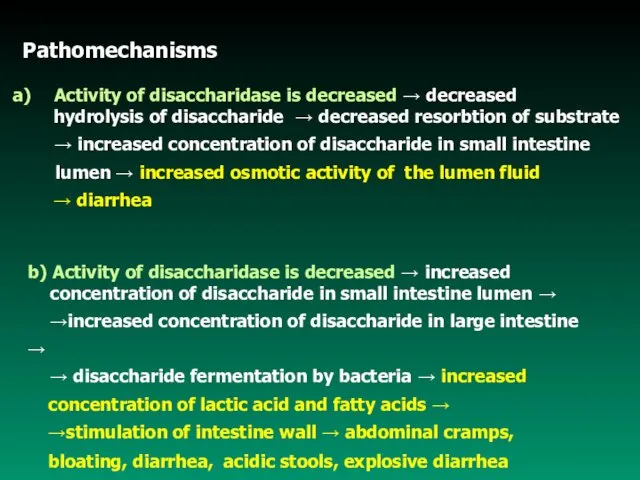
- 6. Pathomechanisms Activity of disaccharidase is decreased → decreased hydrolysis of disaccharide → decreased resorbtion of substrate
- 7. Lactase deficiency syndrome Causes of lactase deficiency: - genetic defect (primary) - secondary to a wide
- 8. Causes of secondary lactase deficiency: - nontropical (celiac disease)and tropical sprue, - regional enteritis, - viral
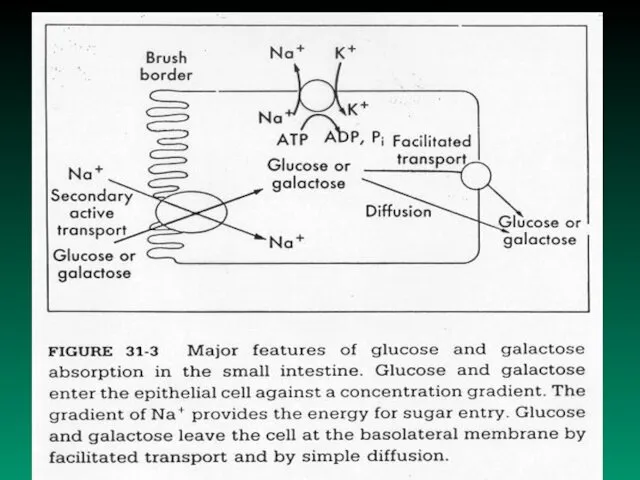
- 9. Monosaccharides malabsorbtion Small intestine ability to resorb glucose and galactose is decreased Cause: Specific transport system
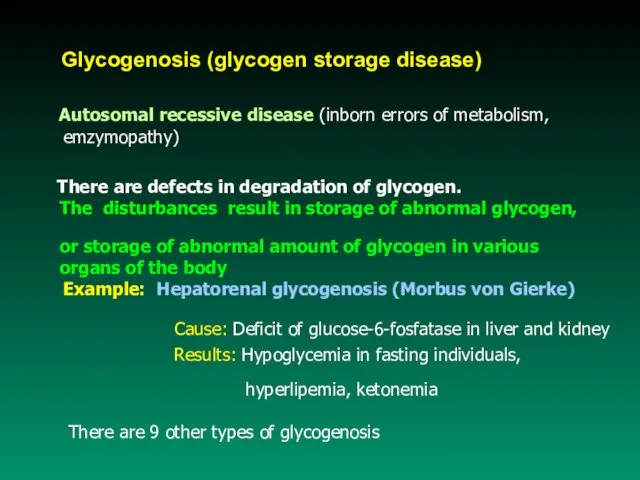
- 10. Glycogenosis (glycogen storage disease) Autosomal recessive disease (inborn errors of metabolism, emzymopathy) There are defects in
- 12. DIABETES MELLITUS DIABETES MELLITUS DM – complex chronic metabolic disorder leading to multiorgan complications Main pathophysiological
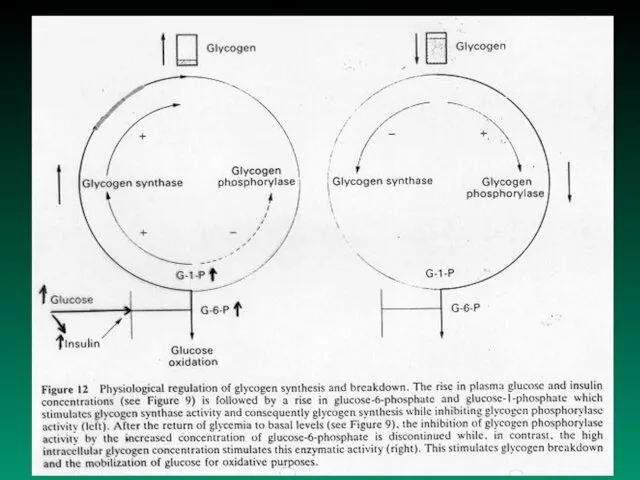
- 13. Regulation of the blood glucose level depends on liver: 1. extracting glucose from blood 2. synthesizing
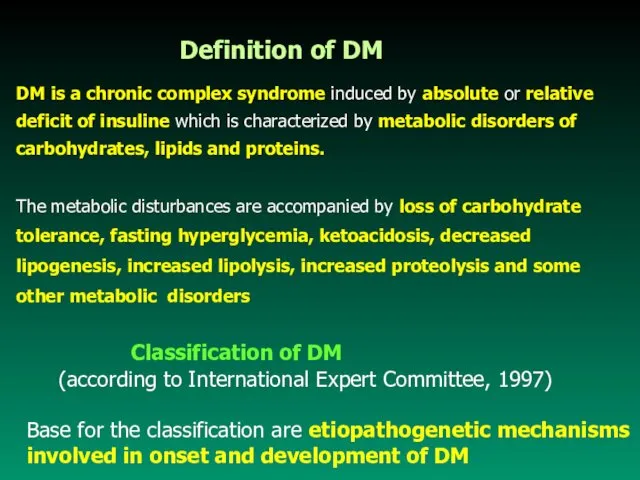
- 14. DM is a chronic complex syndrome induced by absolute or relative deficit of insuline which is
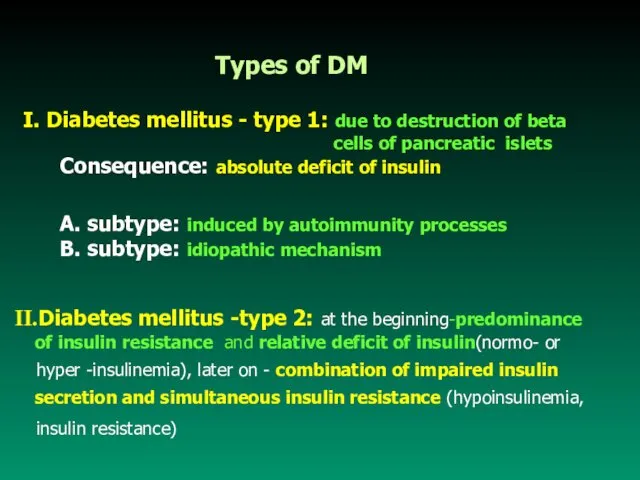
- 15. I. Diabetes mellitus - type 1: due to destruction of beta cells of pancreatic islets Consequence:
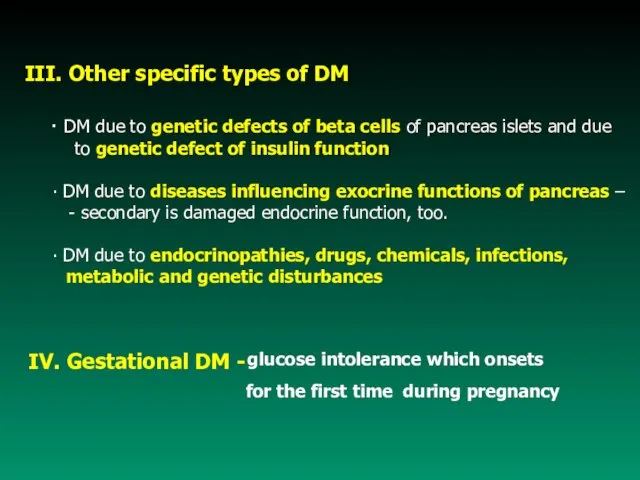
- 16. IV. Gestational DM - III. Other specific types of DM ∙ DM due to genetic defects
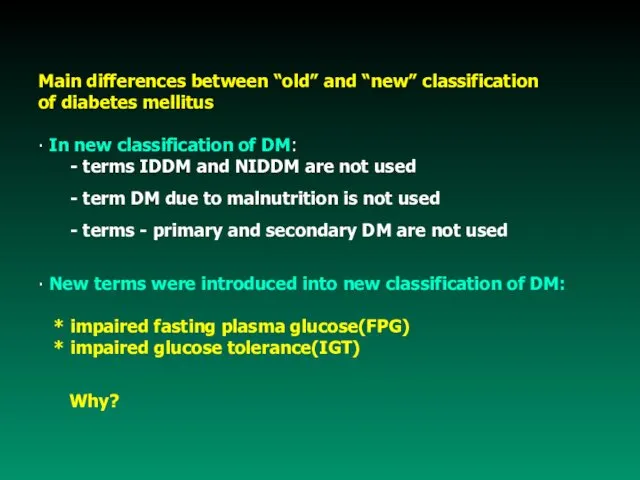
- 17. Main differences between “old” and “new” classification of diabetes mellitus ∙ In new classification of DM:
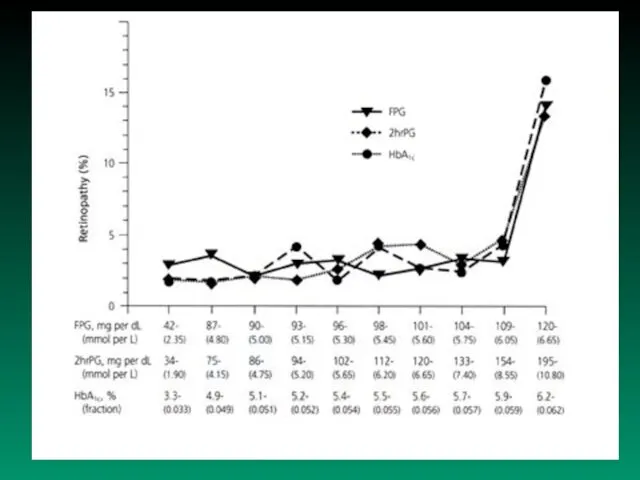
- 19. ∙ Normal fasting value of plasmatic glucose concentration: ● Normal value of PGTT – blood glucose
- 20. ∙ Impaired fasting plasma glucose: ≥ 6.1 but ∙ Impaired glucose tolerance (IGT): Glucose tolerance test
- 21. Syndrome X (metabolic X syndrome) - frequently occurs in people suffering form visceral obesity Characteristic features:
- 22. Insuline Resistance (IR) IR is one of the mechanisms involved in pathogenesis of IGT and DM,
- 23. 3. defective signal transduction (from the receptor to the plasma of cell) 4. postreceptor defect 5.
- 24. Etiopathogenesis of DM Type 1 DM - characteristics - it is most typical in individuals under
- 25. Evidence suggest that type 1 DM is caused by a gradual process of autoimmune destruction of
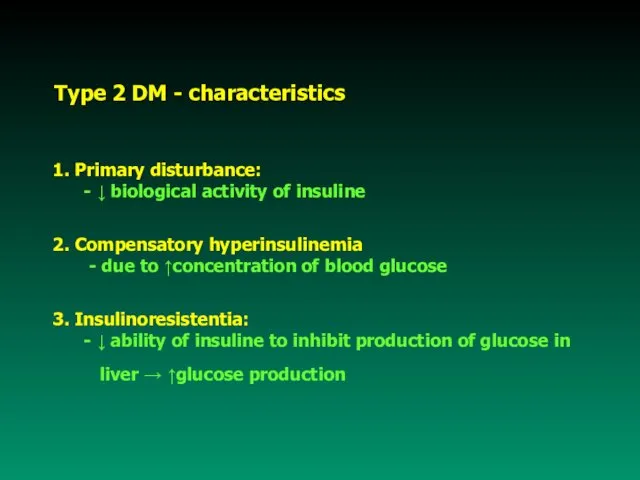
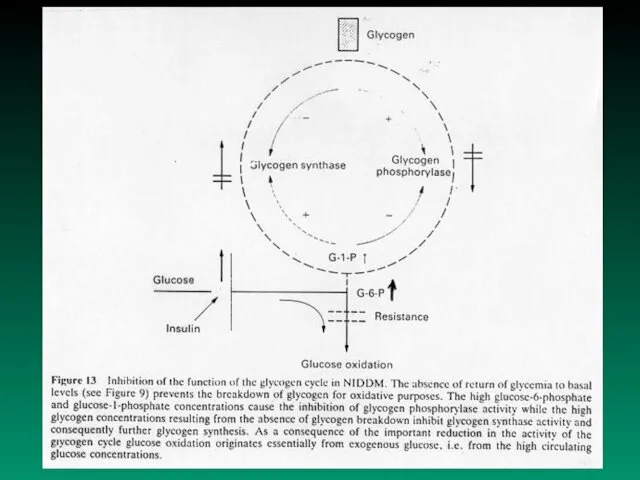
- 26. Type 2 DM - characteristics 1. Primary disturbance: - ↓ biological activity of insuline 2. Compensatory
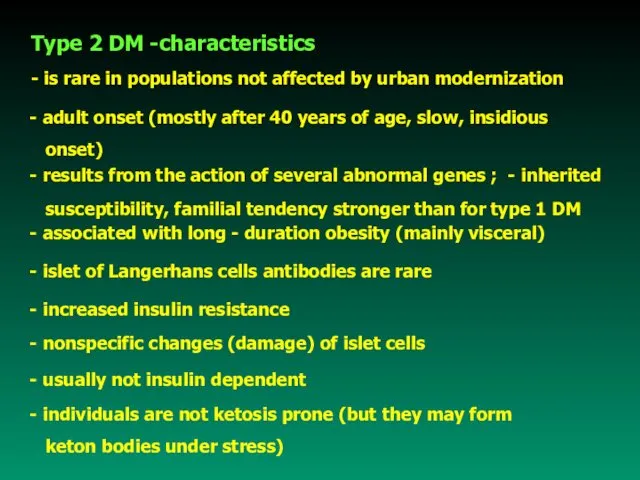
- 27. Type 2 DM -characteristics - is rare in populations not affected by urban modernization - adult
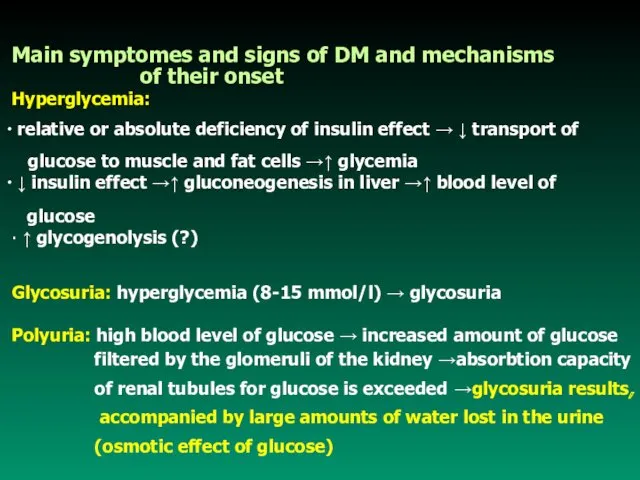
- 29. Main symptomes and signs of DM and mechanisms of their onset Hyperglycemia: relative or absolute deficiency
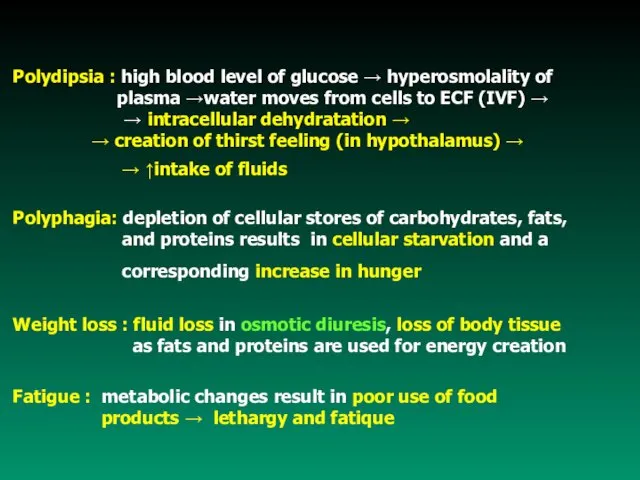
- 30. Polydipsia : high blood level of glucose → hyperosmolality of plasma →water moves from cells to
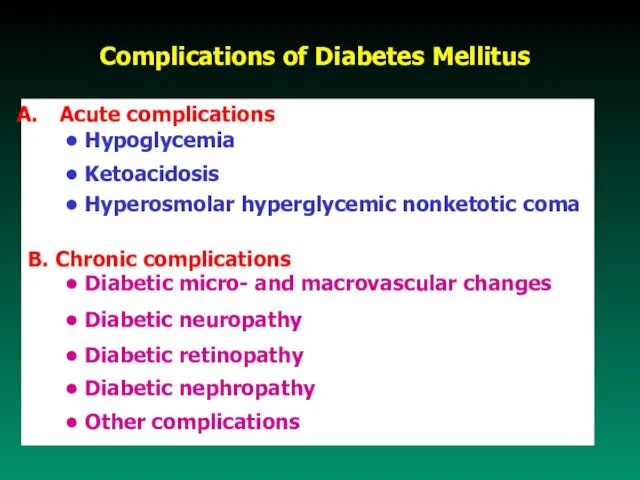
- 31. Complications of Diabetes Mellitus Acute complications • Hypoglycemia • Ketoacidosis • Hyperosmolar hyperglycemic nonketotic coma B.
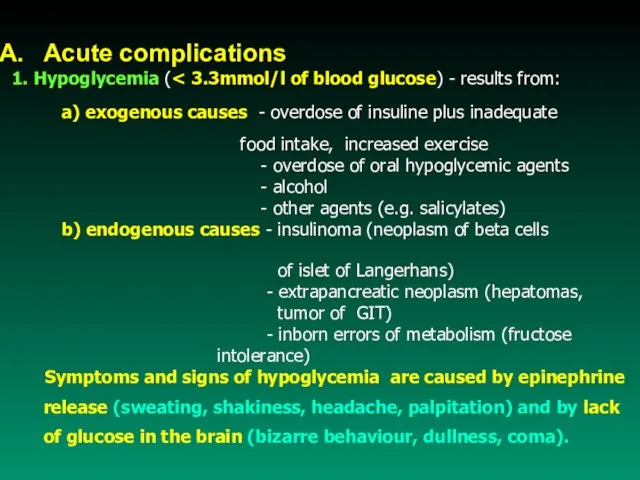
- 32. Acute complications 1. Hypoglycemia ( a) exogenous causes - overdose of insuline plus inadequate food intake,
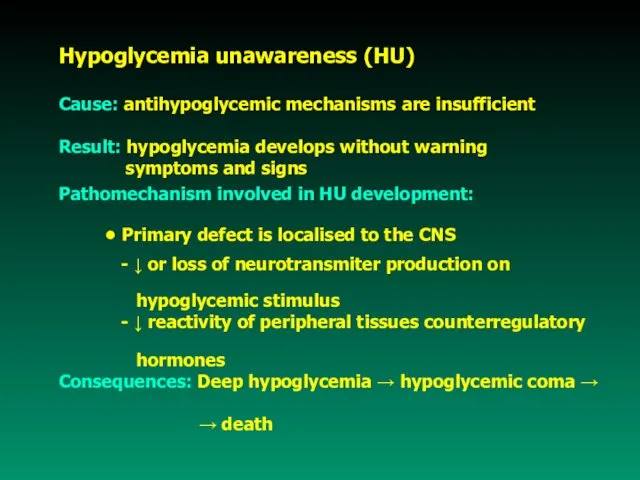
- 33. Hypoglycemia unawareness (HU) Cause: antihypoglycemic mechanisms are insufficient Result: hypoglycemia develops without warning symptoms and signs
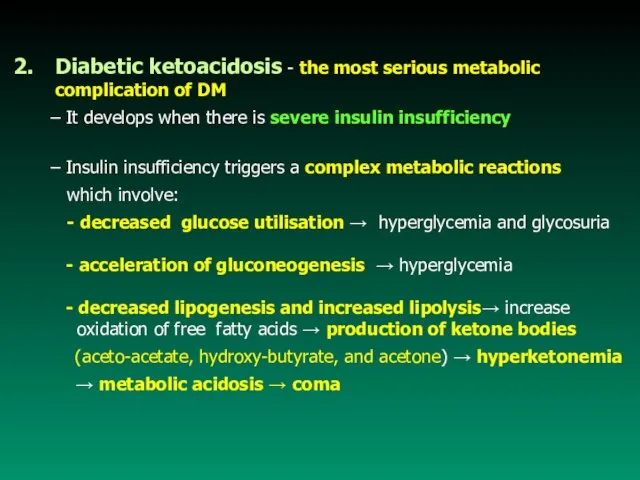
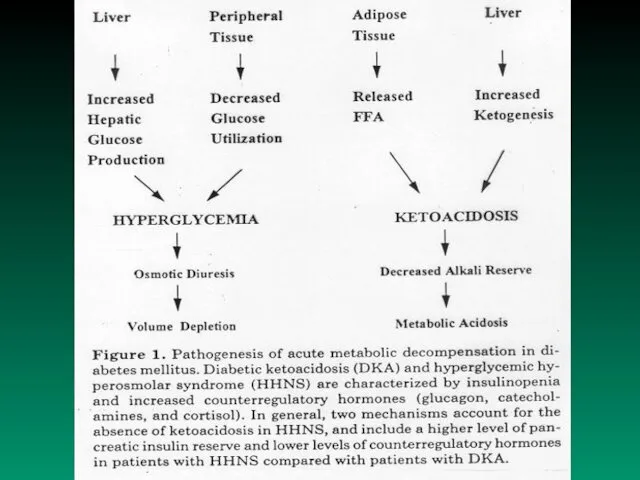
- 34. Diabetic ketoacidosis - the most serious metabolic complication of DM – It develops when there is
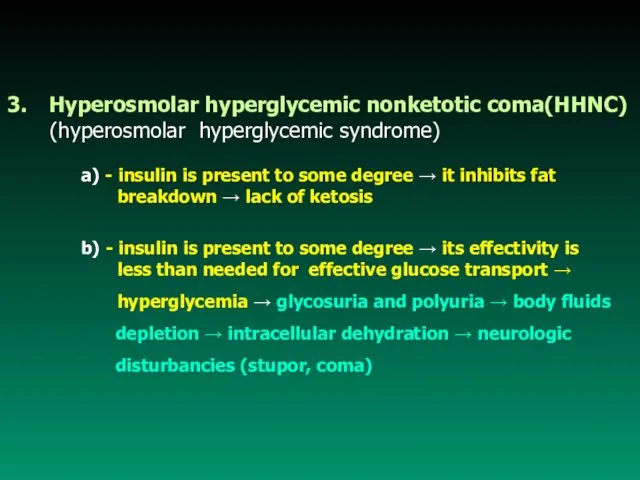
- 35. Hyperosmolar hyperglycemic nonketotic coma(HHNC) (hyperosmolar hyperglycemic syndrome) a) - insulin is present to some degree →
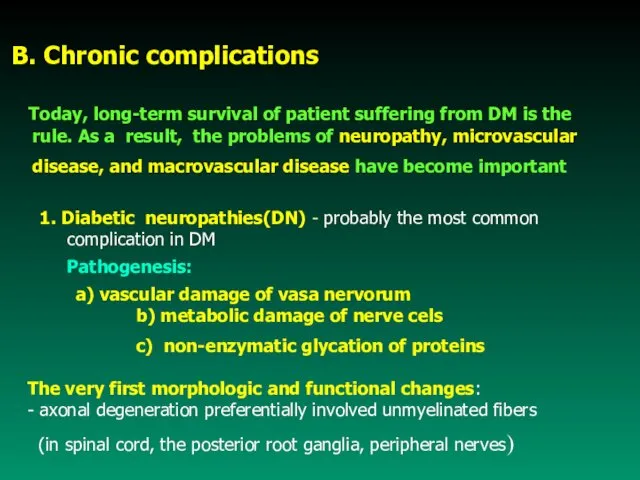
- 37. B. Chronic complications Today, long-term survival of patient suffering from DM is the rule. As a
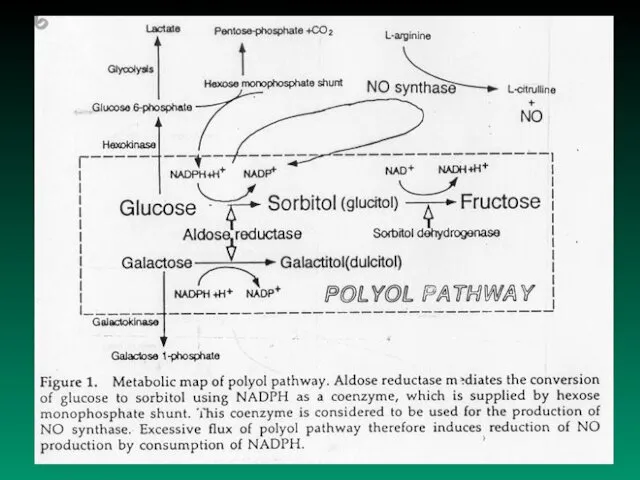
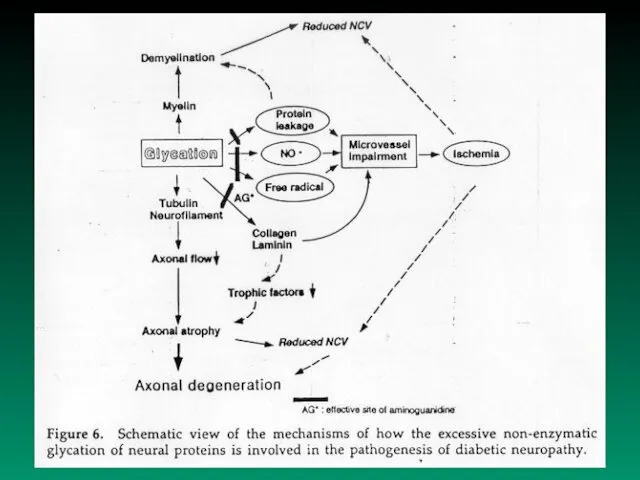
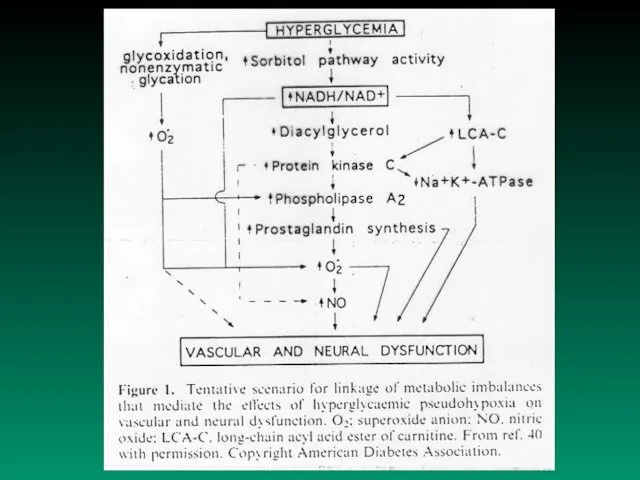
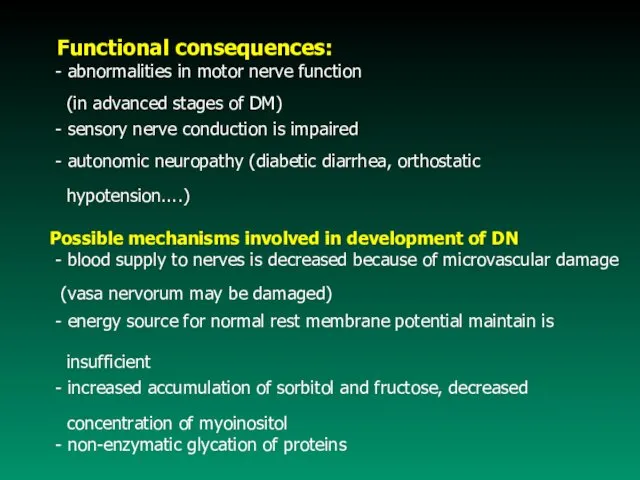
- 41. Functional consequences: - abnormalities in motor nerve function (in advanced stages of DM) - sensory nerve
- 42. Main functions of vascular endotelium • regulates vascular tone and permeability • regulates the balance between
- 43. Microvascular disease - specific lesion of DM that affect capillaries and arterioles of the retina, renal
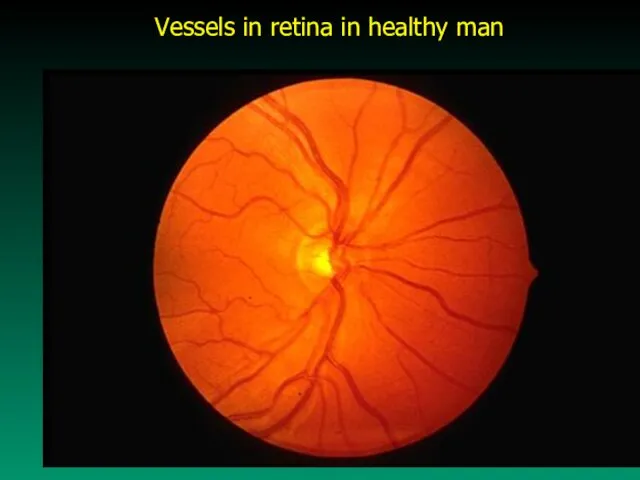
- 44. Vessels in retina in healthy man
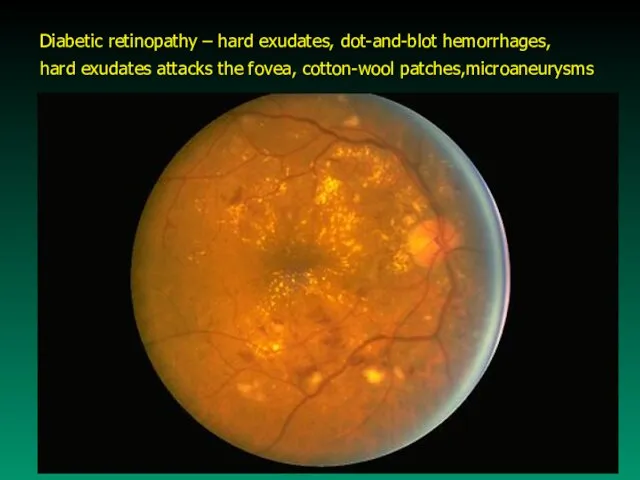
- 45. Diabetic retinopathy – hard exudates, dot-and-blot hemorrhages, hard exudates attacks the fovea, cotton-wool patches,microaneurysms
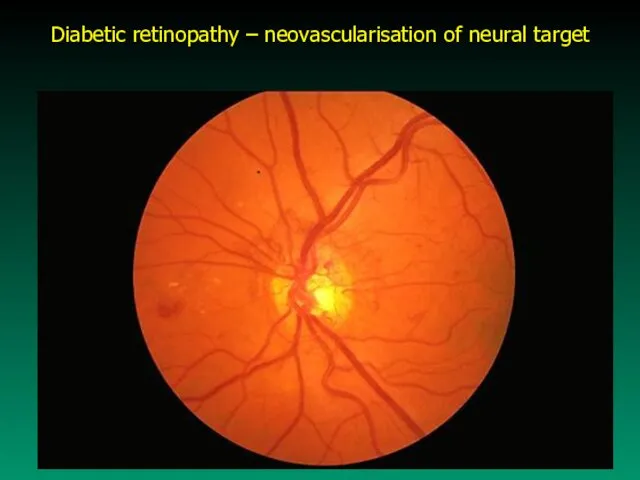
- 46. Diabetic retinopathy – neovascularisation of neural target
- 47. b) Nephropathy - it is the result of glomerular changes caused by DM Pathologic processes involved
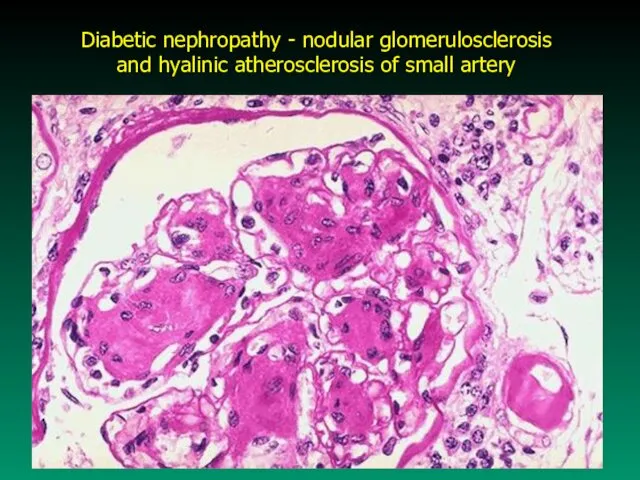
- 48. Diabetic nephropathy - nodular glomerulosclerosis and hyalinic atherosclerosis of small artery
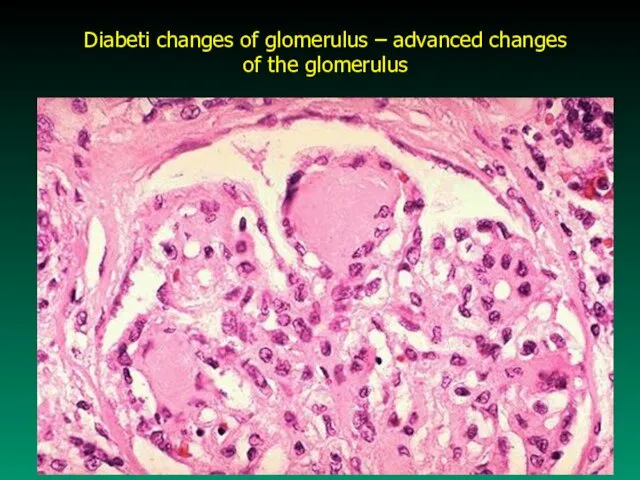
- 49. Diabeti changes of glomerulus – advanced changes of the glomerulus
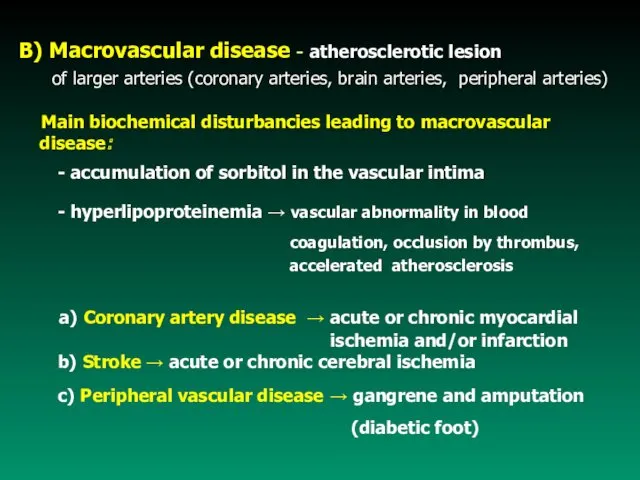
- 50. B) Macrovascular disease - atherosclerotic lesion of larger arteries (coronary arteries, brain arteries, peripheral arteries) Main
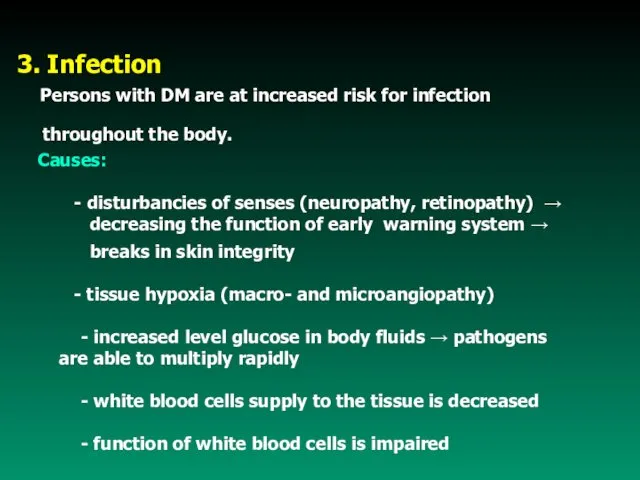
- 53. 3. Infection Persons with DM are at increased risk for infection throughout the body. Causes: -
- 55. Скачать презентацию


 Правила снятия ЭКГ. Подготовка пациента к ЭКГ. Какие датчики бывают и как их устанавливать
Правила снятия ЭКГ. Подготовка пациента к ЭКГ. Какие датчики бывают и как их устанавливать Оценка клинического протокола с помощью AGREE
Оценка клинического протокола с помощью AGREE Болезнь Паркинсона
Болезнь Паркинсона Ликбез на тему ВИЧ/СПИД
Ликбез на тему ВИЧ/СПИД TLR-рецепторы
TLR-рецепторы Ограничение жизнедеятельности и социальная недостаточность при бронхоэктатической болезни у детей
Ограничение жизнедеятельности и социальная недостаточность при бронхоэктатической болезни у детей Лекция 2. Морфология крови
Лекция 2. Морфология крови Профілактика анемії у дітей
Профілактика анемії у дітей Гормон мелатонин
Гормон мелатонин Өндірістік ортадағы жұмыс орнын қорғаудың қазіргі кездегі мәселелері
Өндірістік ортадағы жұмыс орнын қорғаудың қазіргі кездегі мәселелері Взаимосвязь всех видов обмена веществ. Лекция № 3
Взаимосвязь всех видов обмена веществ. Лекция № 3 Основы маркетинга и менеджмента в ортопедической стоматологии
Основы маркетинга и менеджмента в ортопедической стоматологии Спирограмманы тіркеу және түсіндіру
Спирограмманы тіркеу және түсіндіру Классификация, мониторирование, лечение бронхиальной астмы у детей
Классификация, мониторирование, лечение бронхиальной астмы у детей Аномальные маточные кровотечения. Оценка ТФД, гормональные исследования в диагностике функциональных нарушений РС
Аномальные маточные кровотечения. Оценка ТФД, гормональные исследования в диагностике функциональных нарушений РС Лучевое исследование желудо-чнокишечного тракта, органов брюшной полости и мочеполовой системы. (Часть 1)
Лучевое исследование желудо-чнокишечного тракта, органов брюшной полости и мочеполовой системы. (Часть 1) Острый панкреатит
Острый панкреатит Миома матки
Миома матки Разбор клинического случая
Разбор клинического случая Виды массажа
Виды массажа Лекарственные препараты, влияющие на свертываемость крови
Лекарственные препараты, влияющие на свертываемость крови Faculty of clinical psychology. Perm state medical university named after E.A. Wagner
Faculty of clinical psychology. Perm state medical university named after E.A. Wagner Органы кроветворения и иммунной защиты
Органы кроветворения и иммунной защиты Гипоплазия эмали: этиология, патогенез, клиника, диагностика, лечение. Наследственные пороки развития твердых тканей зубов
Гипоплазия эмали: этиология, патогенез, клиника, диагностика, лечение. Наследственные пороки развития твердых тканей зубов Классификация энцефалитов. Аутоиммунные энцефалиты
Классификация энцефалитов. Аутоиммунные энцефалиты Типовые нарушения обмена белков и нуклеиновых кислот
Типовые нарушения обмена белков и нуклеиновых кислот Онтогенез -II. Постнатальный период индивидуального развития. Регенерация. Трансплантация. Опухолевый рост
Онтогенез -II. Постнатальный период индивидуального развития. Регенерация. Трансплантация. Опухолевый рост Копия история болезни Девятковской
Копия история болезни Девятковской