Содержание
- 2. WHAT IS DIC ? Disseminated intravascular coagulation (DIC) is an acquired syndrome characterized by the intravascular
- 3. Normal Pregnancy – Hypercoagulable state. After the 1st trimester there occurs a marked increase in plasma
- 4. TYPES OF DIC ? ACUTE DIC – the physical findings are those of underlying or inciting
- 5. Amniotic fluid has been shown to be able to activate coagulation in vitro, and the degree
- 6. CHRONIC DIC- manifestation is thrombosis from excess thrombin formation , the symptoms and signs of venous
- 7. COMMON CAUSES OF DIC ACUTE DIC Abruptio Placentae Endotoxemia- septic abortions, chorioamnionitis, pyelonephritis of pregnancy. Amniotic
- 8. Vesicular mole Dextran Infusion Hemorrhagic shock due to –PPH , Cs CHRONIC DIC – IUD (
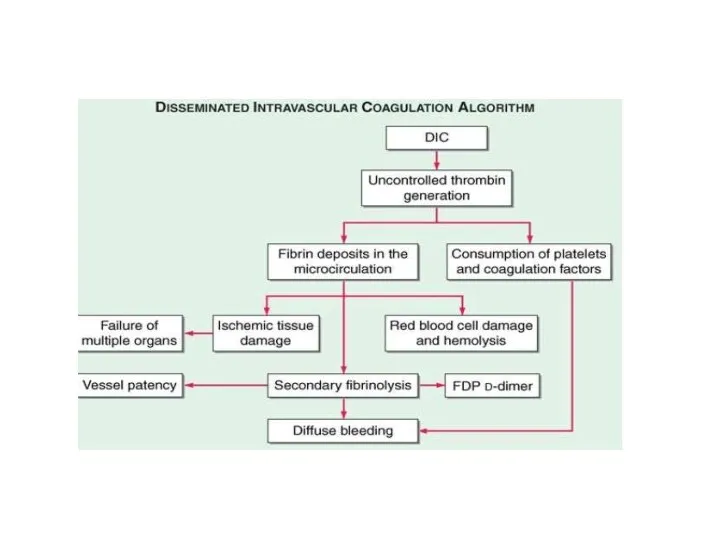
- 9. PATHOPHYSIOLOGY DIC is diagnosed in almost one-half of pregnant women with abruptio placentae, or with amniotic
- 10. PATHOPHYSIOLOGY
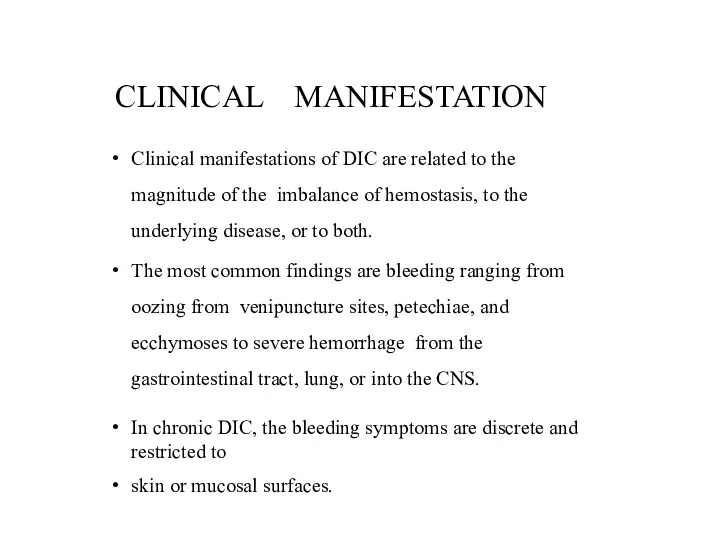
- 11. CLINICAL MANIFESTATION Clinical manifestations of DIC are related to the magnitude of the imbalance of hemostasis,
- 12. The hypercoagulability of DIC manifests as the occlusion of vessels in the microcirculation and resulting organ
- 13. Bleeding from at 3 unrelated sites is particularly suggestive of DIC. Brain- altered state of consiousness
- 14. LAB INVESTIGATIONS The laboratory investigation should include coagulation tests [aPTT, PT, thrombin time (TT)] and markers
- 15. LAB RESULTS prolongation of PT and/or aPTT platelet counts less than 100,000, or a rapid decline
- 16. DIC is an unlikely diagnosis in the presence of normal levels of FDP. The D-dimer test
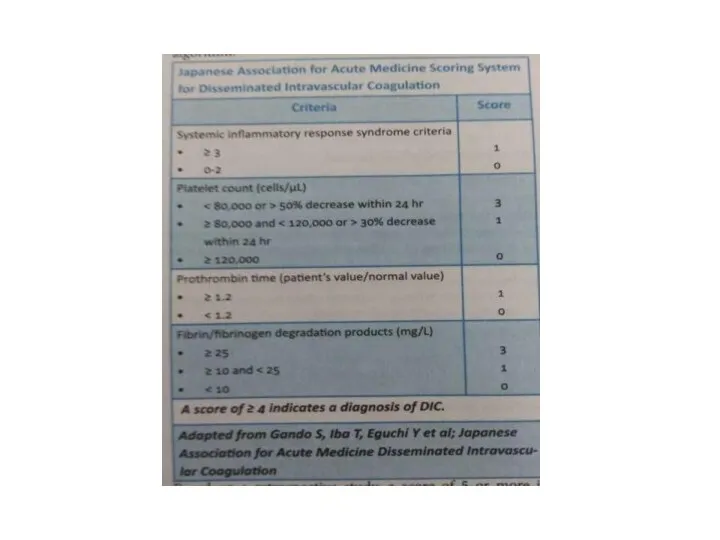
- 17. RISK ASSESSMENT Does the patient have an underlying disorder compatible with DIC? Lab coagulation tests- Platelet
- 18. Prolonged PT 6 sec = 2 point. Fibrinogen level > 1 gm/l = 0 points ,
- 20. TREATMENT The morbidity and mortality associated with DIC are primarily related to the underlying disease rather
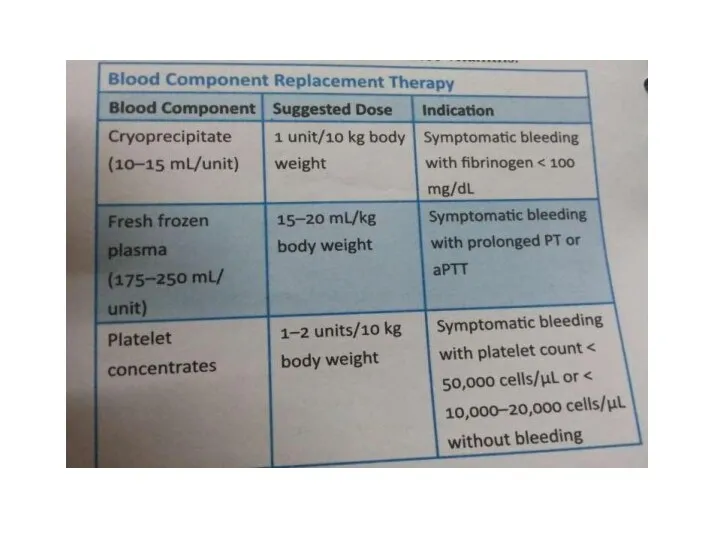
- 21. MANAGEMENT OF HEMORRHAGIC SYMPTOMS The control of bleeding in DIC patients with marked thrombocytopenia (platelet counts
- 22. The PT (>1.5 times the normal) provides a good indicator of the severity of the clotting
- 23. The transfusion must be adjusted according to the patient's clinical and laboratory evolution. Platelet concentrates at
- 24. REPLACEM ENT O F CO AG ULATI O N O R FI BRI NO LYSI S
- 25. The use of antifibrinolytic drugs, EACA, or tranexamic acid, to prevent fibrin degradation by plasmin may
- 28. Скачать презентацию
 Патофизиология печени
Патофизиология печени Язвенная болезнь желудка и ДПК
Язвенная болезнь желудка и ДПК Витамин А Ретинол
Витамин А Ретинол Скрининг дегеніміз не?
Скрининг дегеніміз не? Теория массажа
Теория массажа Диссеминированные процессы легких
Диссеминированные процессы легких Omphalocele and gastroschisis
Omphalocele and gastroschisis Всемирный день здоровья
Всемирный день здоровья Перинатальные поражения нервной системы
Перинатальные поражения нервной системы Шистосомозы. Этиологиясы. Эпидемиологиясы. Патогенезі. Классификациясы. Клиникасы. Диагностикасы. Екшеу диагностикасы. Емі
Шистосомозы. Этиологиясы. Эпидемиологиясы. Патогенезі. Классификациясы. Клиникасы. Диагностикасы. Екшеу диагностикасы. Емі Сегментарный массаж
Сегментарный массаж Токсоплазмоз. Эпидемиология. Лечение
Токсоплазмоз. Эпидемиология. Лечение Отравление техническими жидкостями
Отравление техническими жидкостями Потребность пациента в движении
Потребность пациента в движении Гломерулонефриты. Этиопатогенез, клиника, диагностика, лечение
Гломерулонефриты. Этиопатогенез, клиника, диагностика, лечение Лабораторные синдромы при заболеваниях печени и ЖВП
Лабораторные синдромы при заболеваниях печени и ЖВП СРС: Қазақстанда тағамдық уланудың таралуы
СРС: Қазақстанда тағамдық уланудың таралуы Исследование мочи
Исследование мочи Сердечно-сосудистая система: расспрос, осмотр
Сердечно-сосудистая система: расспрос, осмотр Профилактика нарушений осанки
Профилактика нарушений осанки Принципы организации медицины катастроф
Принципы организации медицины катастроф Схема описания рентгенограммы
Схема описания рентгенограммы Противоестественный задний проход и колостома
Противоестественный задний проход и колостома Неопухолевые заболевания пищевода
Неопухолевые заболевания пищевода Патанатомия СРС. Бауыр аурулары алуан түрлі
Патанатомия СРС. Бауыр аурулары алуан түрлі УЗ 26-я городская поликлиника г. Минска. Центр дружественного отношения к подросткам
УЗ 26-я городская поликлиника г. Минска. Центр дружественного отношения к подросткам Терапиялық стоматология. Тісжегіні емдеу қағидалары. Қателіктері және асқынулары, оларды жою жолдары, алдын алу
Терапиялық стоматология. Тісжегіні емдеу қағидалары. Қателіктері және асқынулары, оларды жою жолдары, алдын алу Аллергические конъюнктивиты: классификация, клиника, лечение
Аллергические конъюнктивиты: классификация, клиника, лечение