Содержание
- 2. HEART FAILURE (HF) Heart failure is a syndrome manifesting as the inability of the heart to
- 3. A state in which the heart cannot provide sufficient cardiac output to satisfy the metabolic needs
- 4. ESC GUIDELINES FOR DIAGNOSTIC AND TREATMENT OF ACUTE AND CHRONIC HF (2016) HF is a clinical
- 5. HF – is an imprecise term used to describe the pathological state that develops when the
- 6. STATISTICS HF afflicts 2,1% of population At 40 years of age, the lifetime risk of developing
- 7. Final common pathway for many cardiovascular diseases whose natural history results in symptomatic or asymptomatic left
- 8. PROGNOSIS HF is a strong predictor of the sudden cardiac death The 5-year mortality rate for
- 9. AETHIOLOGY OF HF The three major contributors are: hypertension, coronary ar tery disease, dilated cardiomyopathy, heart
- 10. RISK FACTORS Hypertension Diabetes Age Obesity Heart valve problems Unhealthy lifestyle (smoking, physical inactivity, etc.)
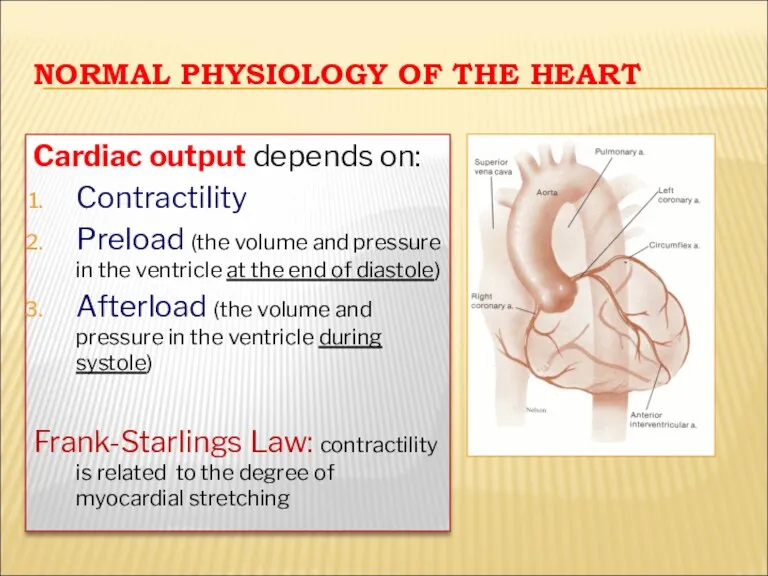
- 11. NORMAL PHYSIOLOGY OF THE HEART Cardiac output depends on: Contractility Preload (the volume and pressure in
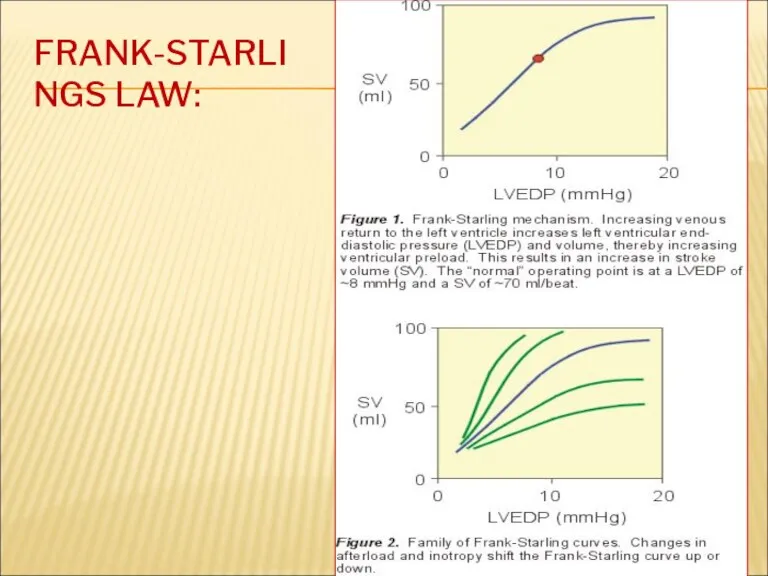
- 12. FRANK-STARLINGS LAW:
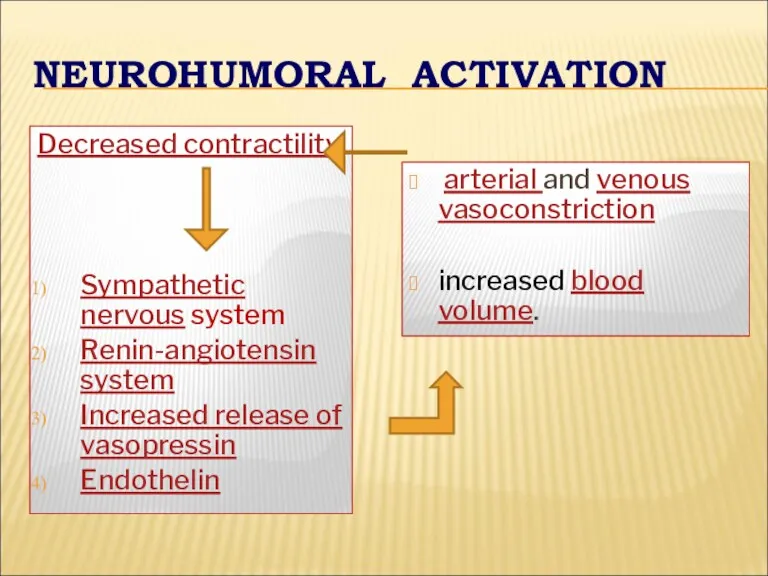
- 13. NEUROHUMORAL ACTIVATION Decreased contractility Sympathetic nervous system Renin-angiotensin system Increased release of vasopressin Endothelin arterial and
- 14. COMPENSATORY CHANGES IN HEART FAILURE Activation of СNS Activation of RAS Increased heart rate Release of
- 15. CLASSIFICATION Heart failure can be classified in several ways 1 - Acute and chronic HF 2
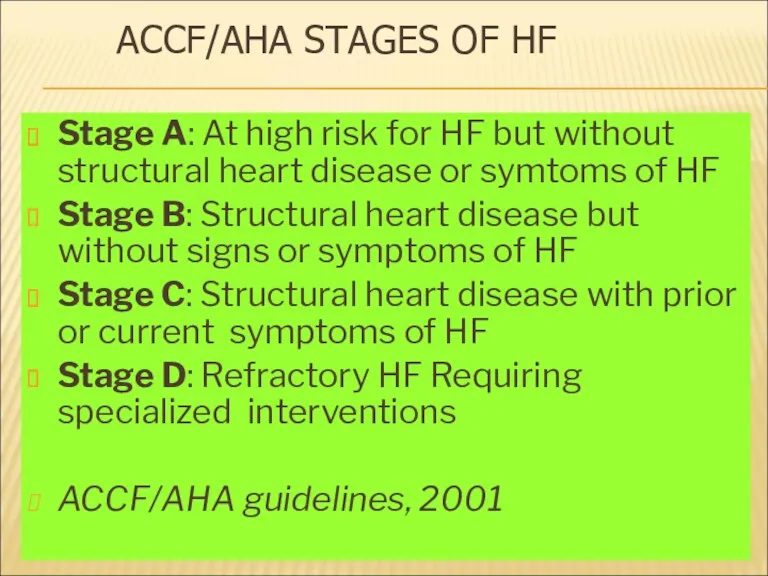
- 16. ACCF/AHA STAGES OF HF Stage A: At high risk for HF but without structural heart disease
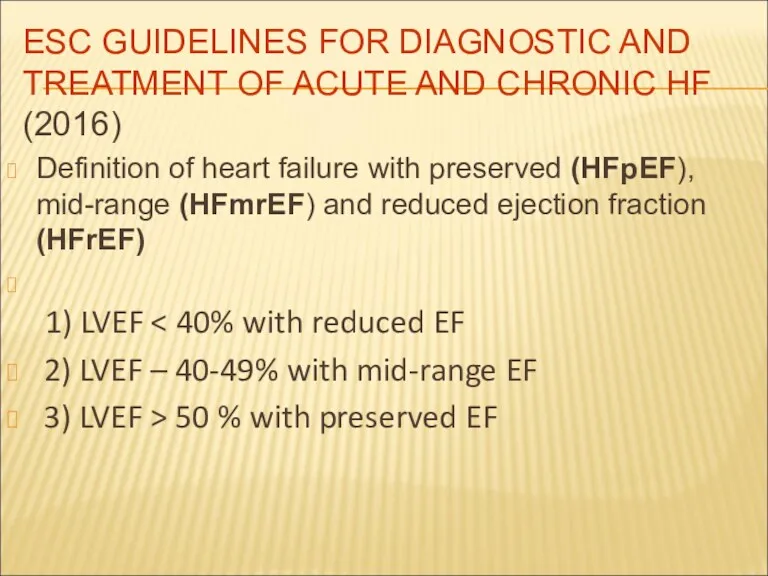
- 17. ESC GUIDELINES FOR DIAGNOSTIC AND TREATMENT OF ACUTE AND CHRONIC HF (2016) Definition of heart failure
- 18. ESC GUIDELINES FOR DIAGNOSTIC AND TREATMENT OF ACUTE AND CHRONIC HF (2016) In previous guidelines it
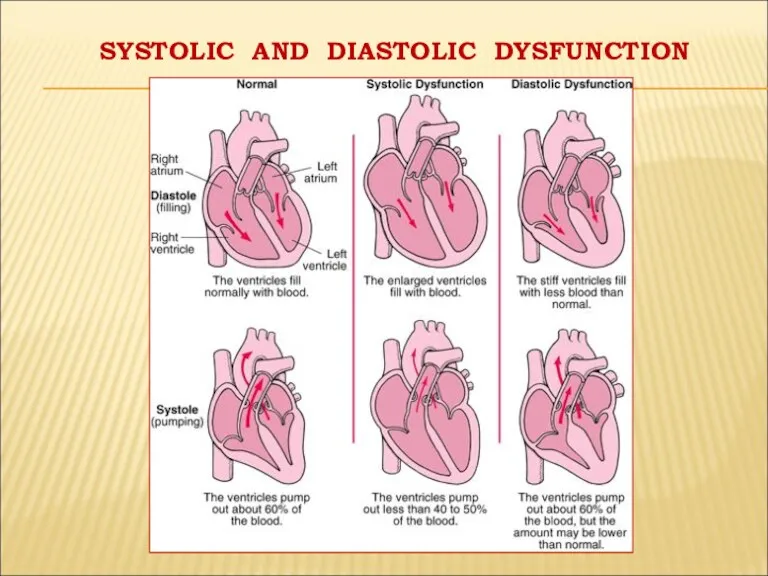
- 19. SYSTOLIC AND DIASTOLIC DYSFUNCTION
- 20. « FORWARD AND BACKWARD HF» In some patients with HF the predominant problem is an inadequate
- 21. "HIGH OUTPUT CARDIAC FAILURE” This can occur from: Severe anemia, Gram negative septicaemia, Beriberi (vitamin B1/thiamine
- 22. Decrease of pump function decrease cardiac output, heart volume per minute decrease arterial pressure increase activity
- 23. SYSTOLIC DYSFUNCTION Coronary artery disease (CAD) Dilated cardiomyopathy (DCMP) Myocarditis Anti-cancer drugs (doxorubicin) and some toxins
- 24. DIASTOLIC DYSFUNCTION Constrictive pericarditis, cardiac tamponade LV hypertrophy (hypertension) Restrictive cardiomyopathy
- 25. LEFT, RIGHT AND BIVENTRICULAR FAILURE
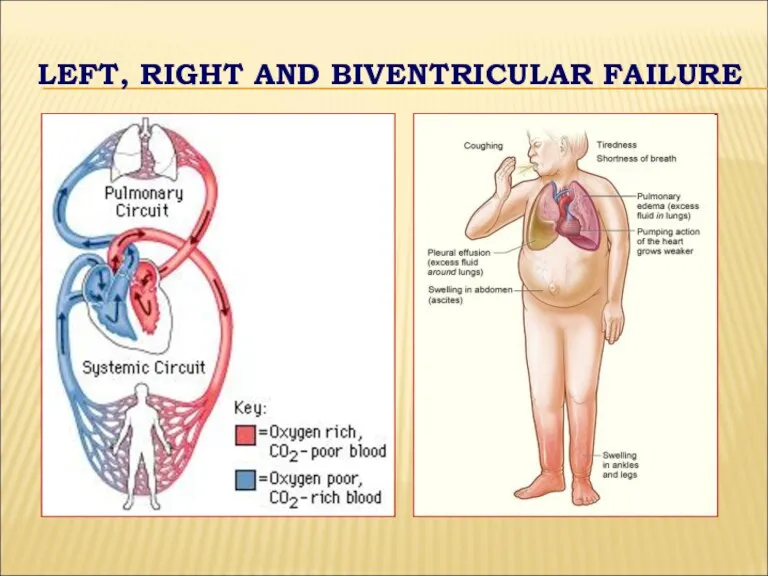
- 26. LEFT-SIDED FAILURE Dyspnea and suffocation Orthopnea Paroxysmal nocturnal dyspnea Peripheral cyanosis and coldness Tiredness, weakness, anxiety
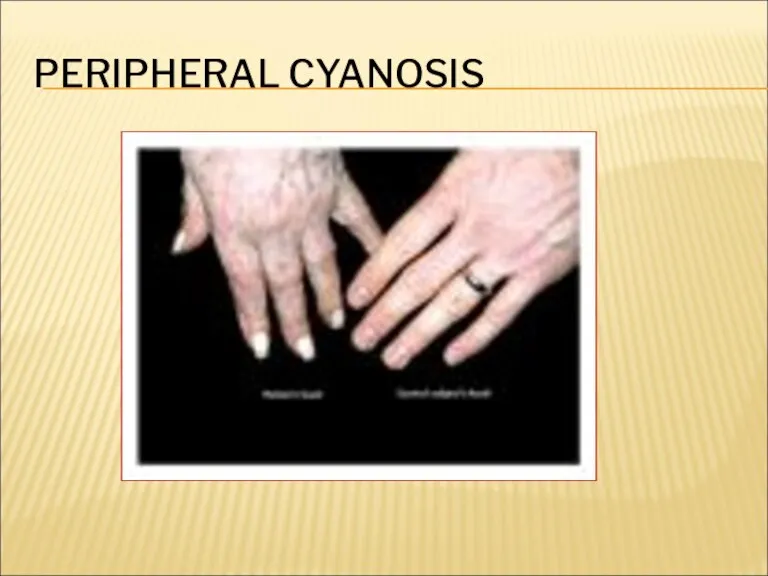
- 27. PERIPHERAL CYANOSIS
- 28. RIGHT-SIDED FAILURE Fluid accumulation and swelling (edema) in the feet, ankles, legs Hepatomegaly Enlargement of abdomen
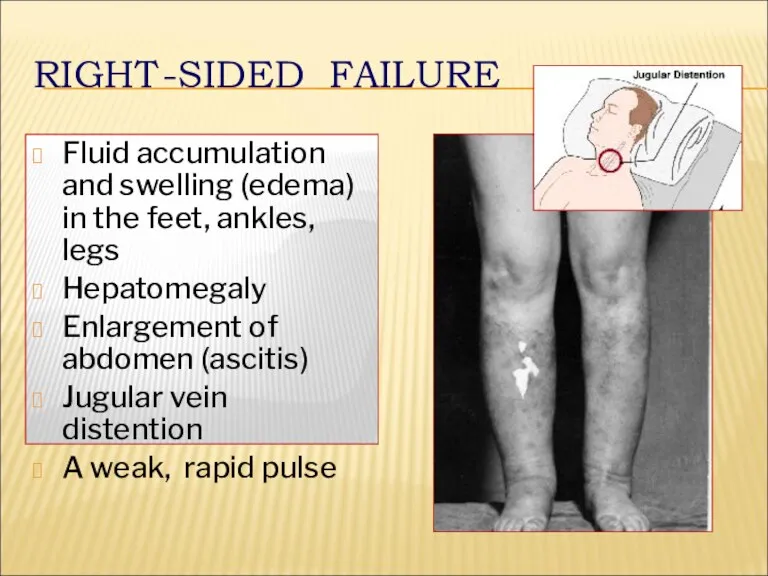
- 29. NEW YORK НЕАRT ASSOCIATION (NYHA) FUNCTIONAL CLASSIFICATION OF CHF
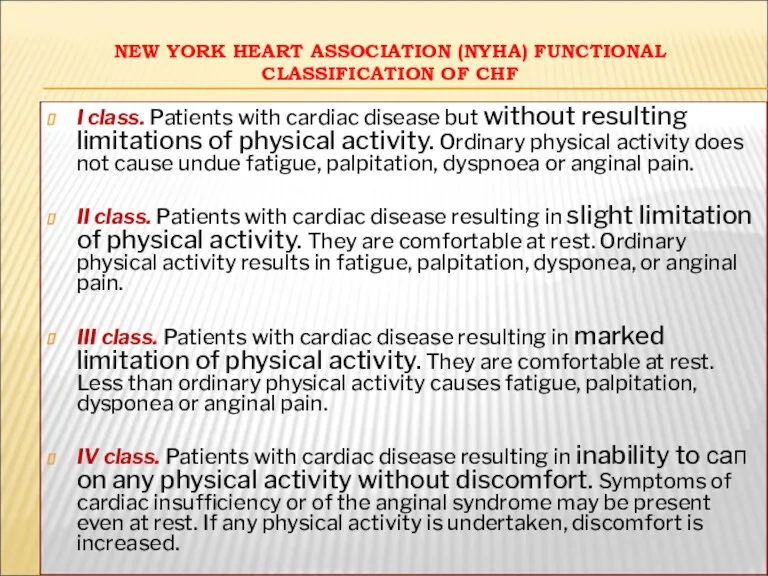
- 30. DIAGNOSIS OF HF Symptoms (underlying disease + HF) Physical examination (pulse, BP, abnormal heart sounds and
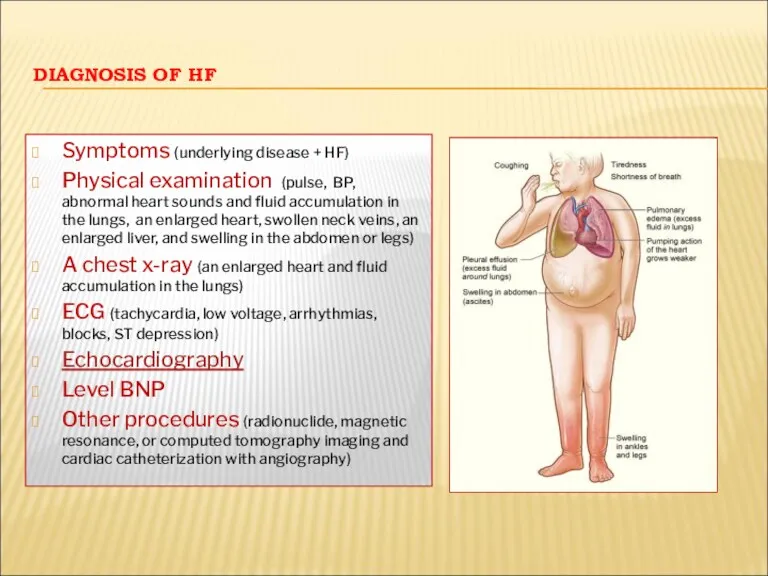
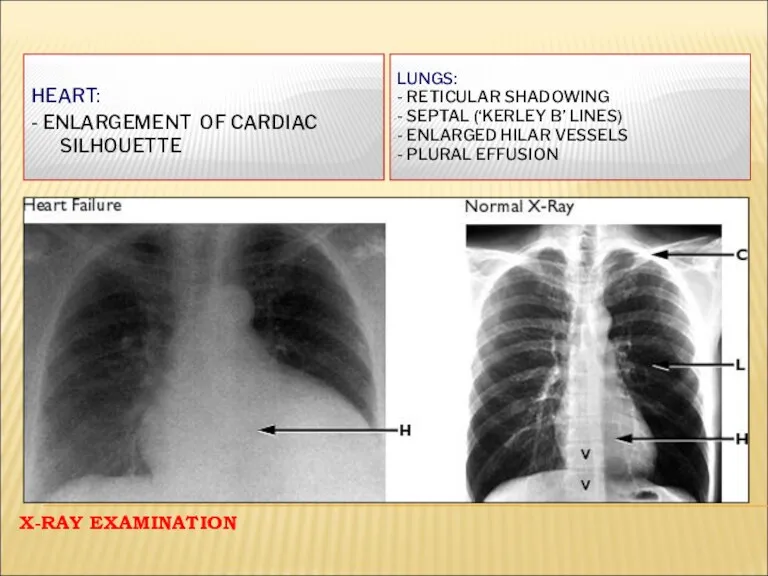
- 31. X-RAY EXAMINATION LUNGS: - RETICULAR SHADOWING - SEPTAL (‘KERLEY B’ LINES) - ENLARGED HILAR VESSELS -
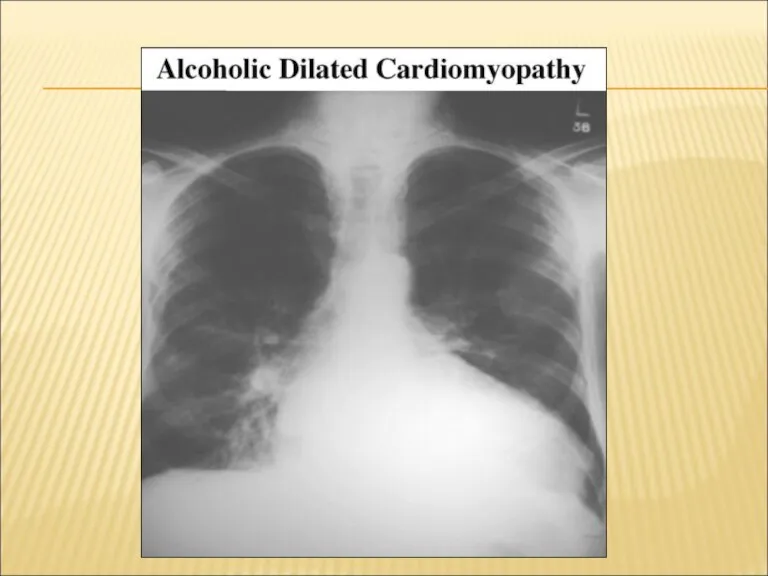
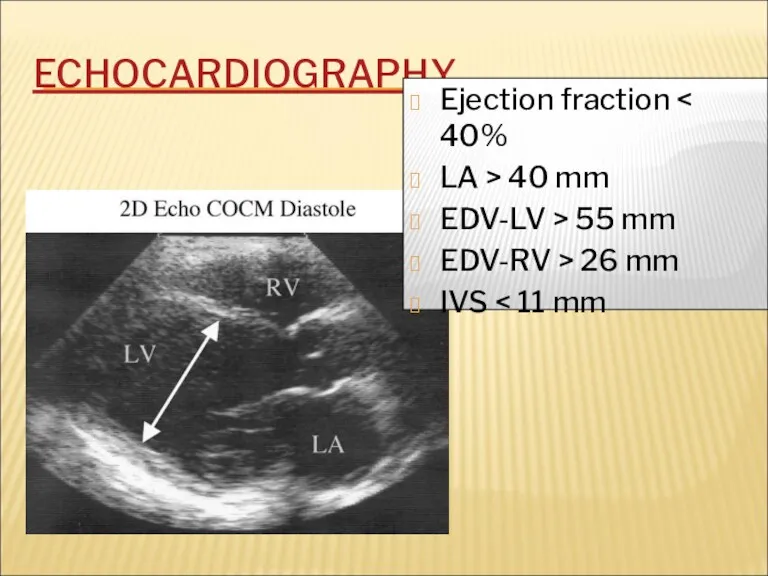
- 33. ECHOCARDIOGRAPHY Ejection fraction LA > 40 mm EDV-LV > 55 mm EDV-RV > 26 mm IVS
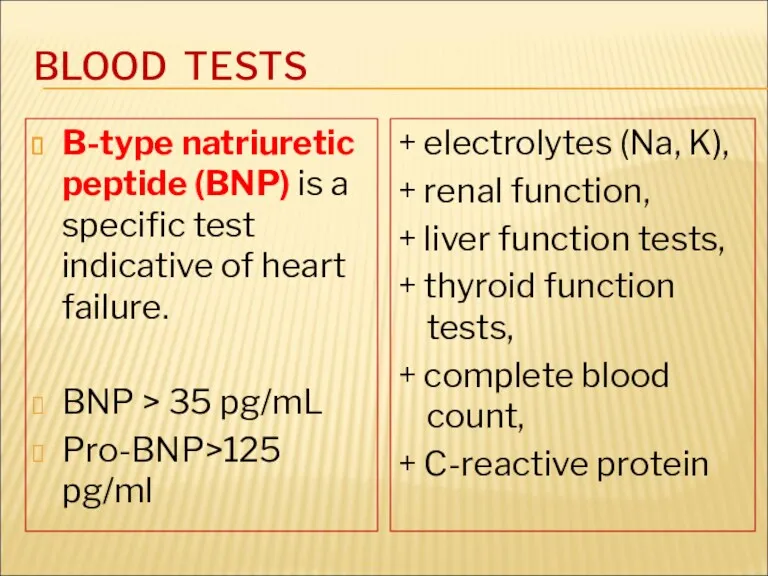
- 34. BLOOD TESTS B-type natriuretic peptide (BNP) is a specific test indicative of heart failure. BNP >
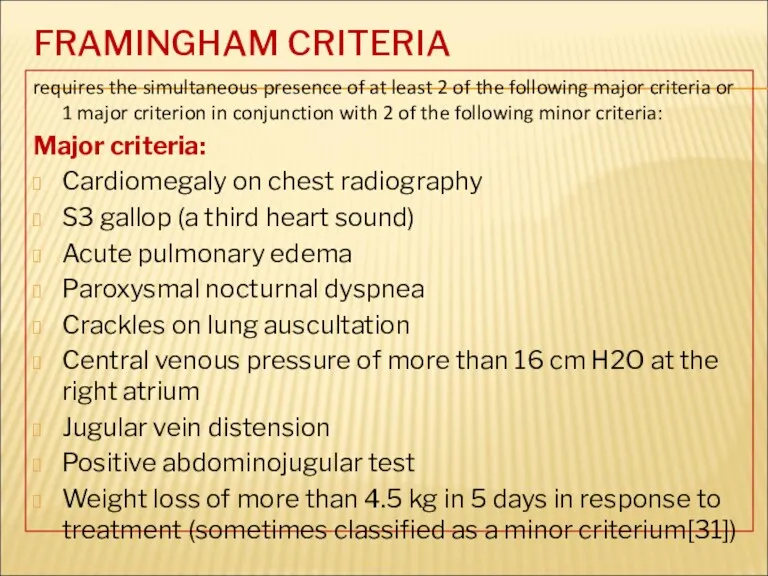
- 35. FRAMINGHAM CRITERIA requires the simultaneous presence of at least 2 of the following major criteria or
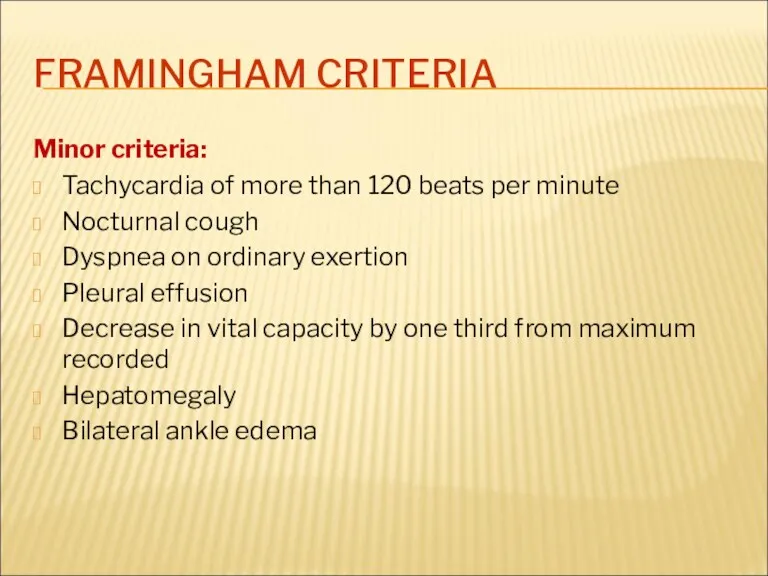
- 36. FRAMINGHAM CRITERIA Minor criteria: Tachycardia of more than 120 beats per minute Nocturnal cough Dyspnea on
- 37. THE COURSE OF CHF Symptoms of heart failure may begin suddenly, especially if the cause is
- 38. TREATMENT OF HEART FAILURE Acute and chronic management strategies in heart failure are aimed at improving
- 39. MANAGEMENT OF THE HEART FAILURE The main purposes: To reduce mortality !!! To relieve HF symptoms
- 40. GOALS OF TREATMENT To improve symptoms and quality of life To decrease likelihood of disease progression
- 41. THE MAIN PRINCIPLES OF HF MANAGEMENT To reveal and exclude triggering factors To normalise cardiac output
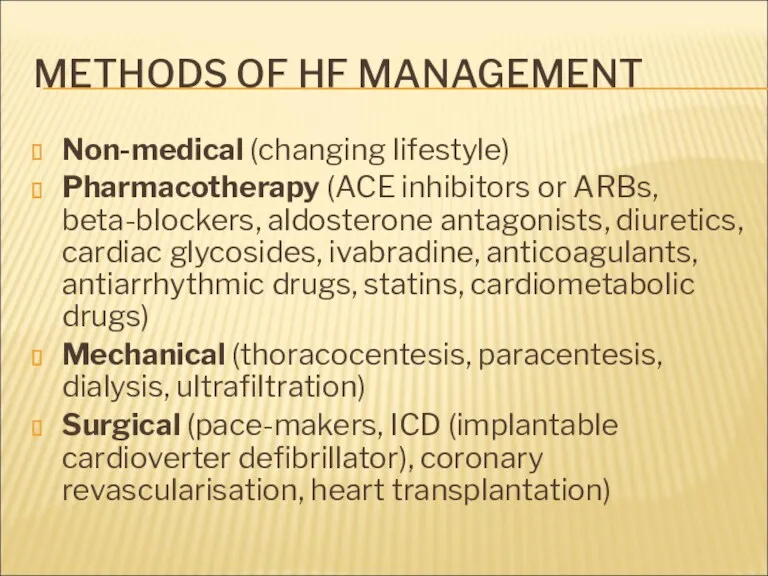
- 42. METHODS OF HF MANAGEMENT Non-medical (changing lifestyle) Pharmacotherapy (ACE inhibitors or ARBs, beta-blockers, aldosterone antagonists, diuretics,
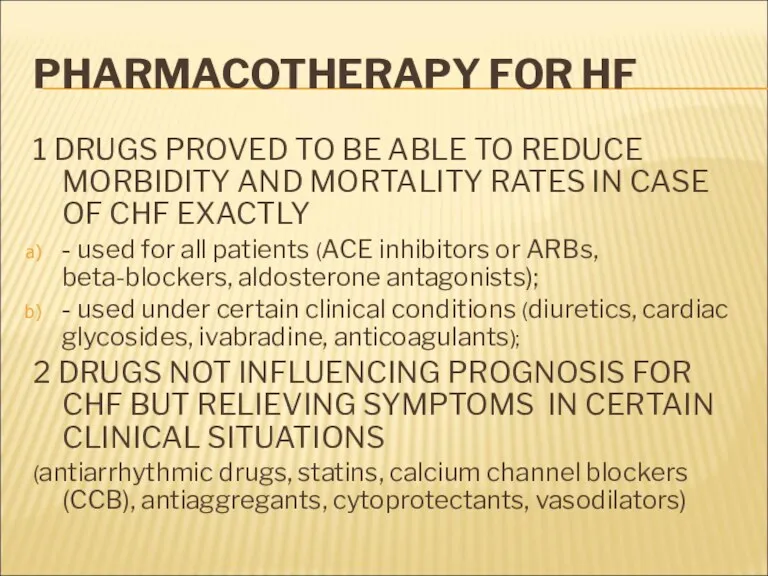
- 43. PHARMACOTHERAPY FOR HF 1 DRUGS PROVED TO BE ABLE TO REDUCE MORBIDITY AND MORTALITY RATES IN
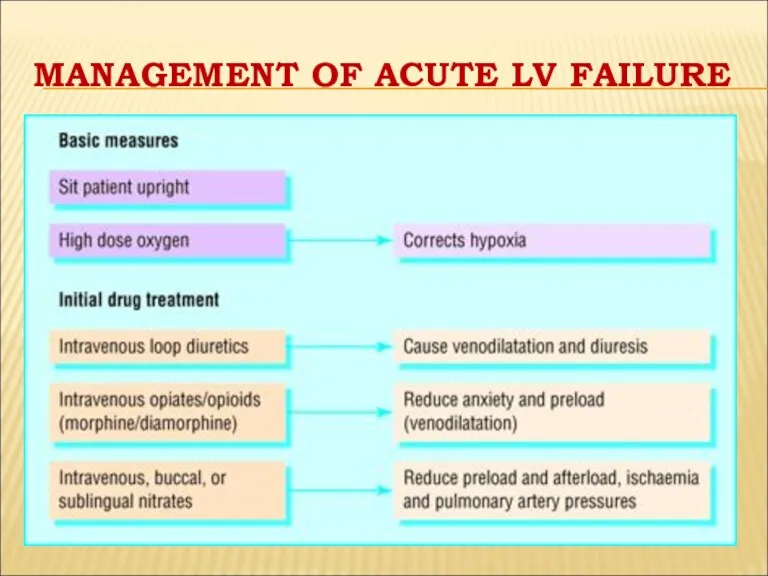
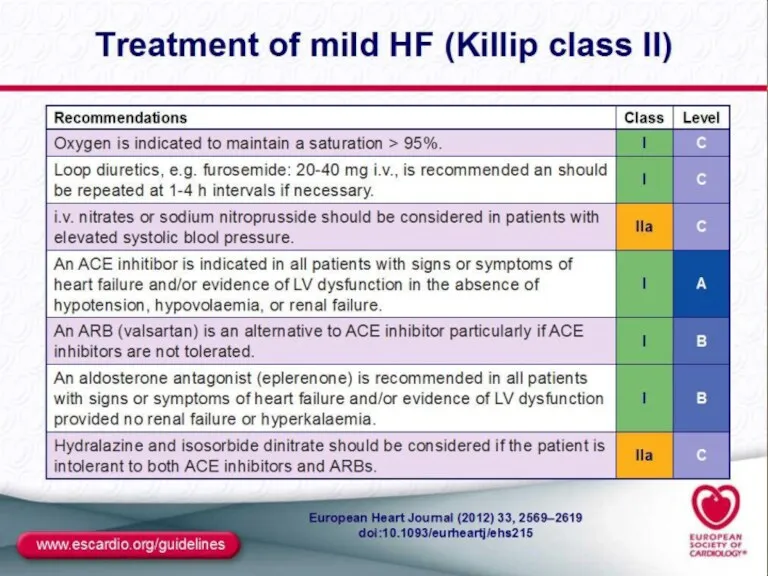
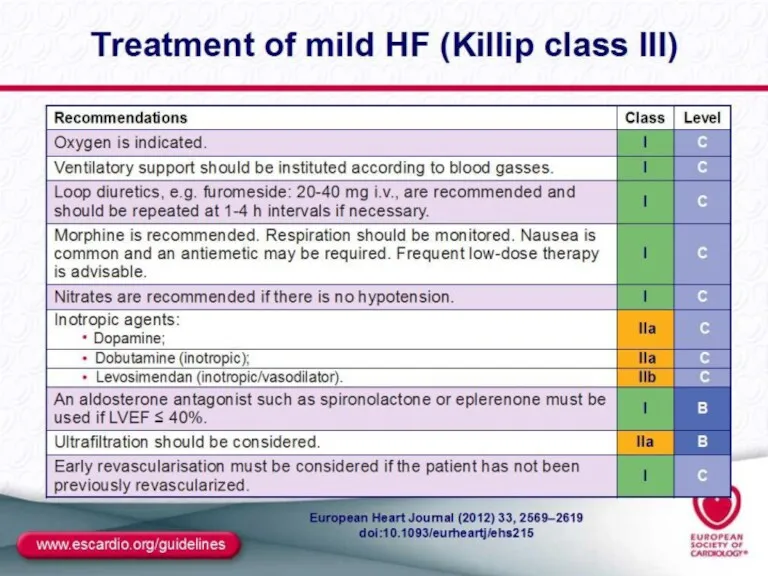
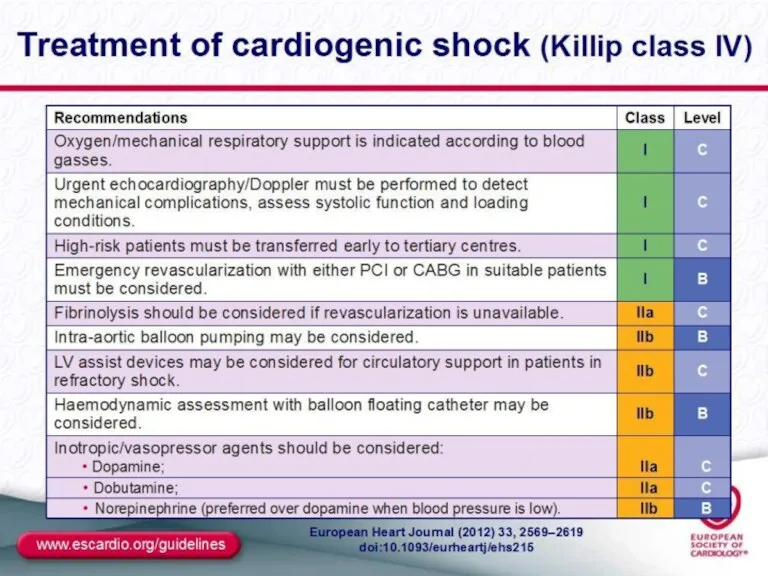
- 44. MANAGEMENT OF ACUTE LV FAILURE
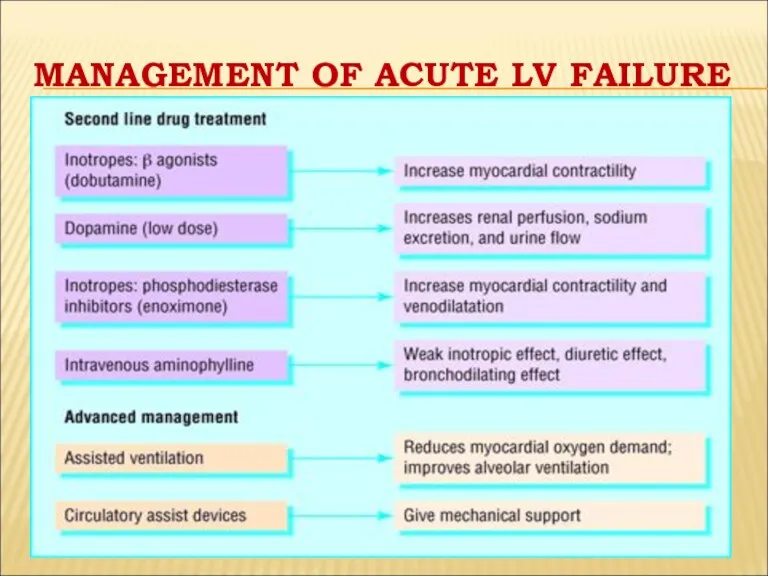
- 45. MANAGEMENT OF ACUTE LV FAILURE
- 49. GENERAL MANAGEMENT OF CHRONIC HF Education of patient and relatives Diet: decrease of salt intake, good
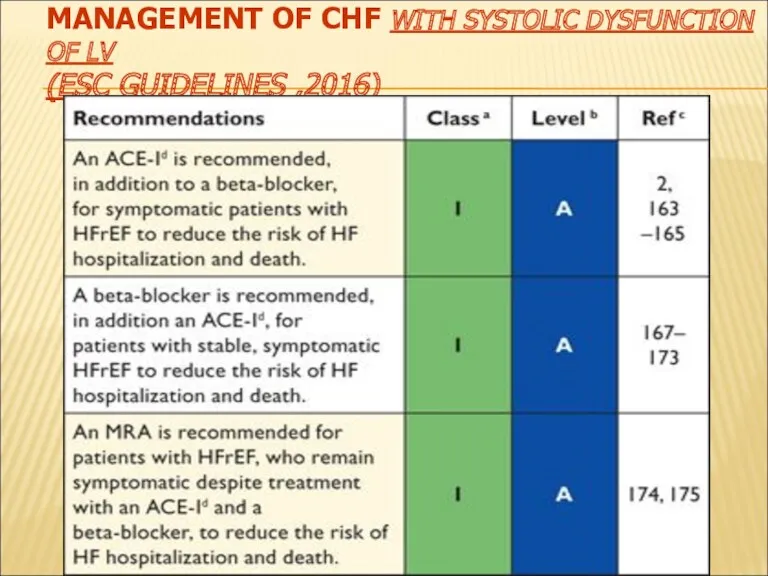
- 50. MANAGEMENT OF CHF WITH SYSTOLIC DYSFUNCTION OF LV (ESC GUIDELINES ,2016)
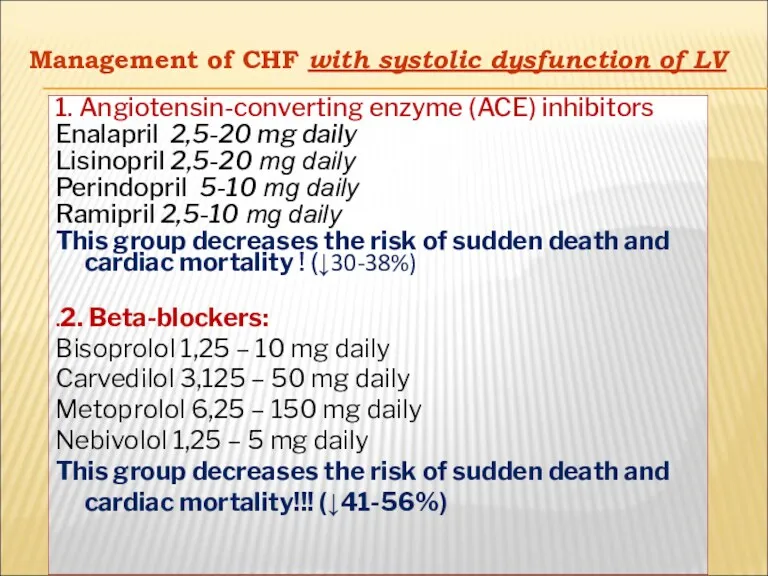
- 51. Management of CHF with systolic dysfunction of LV
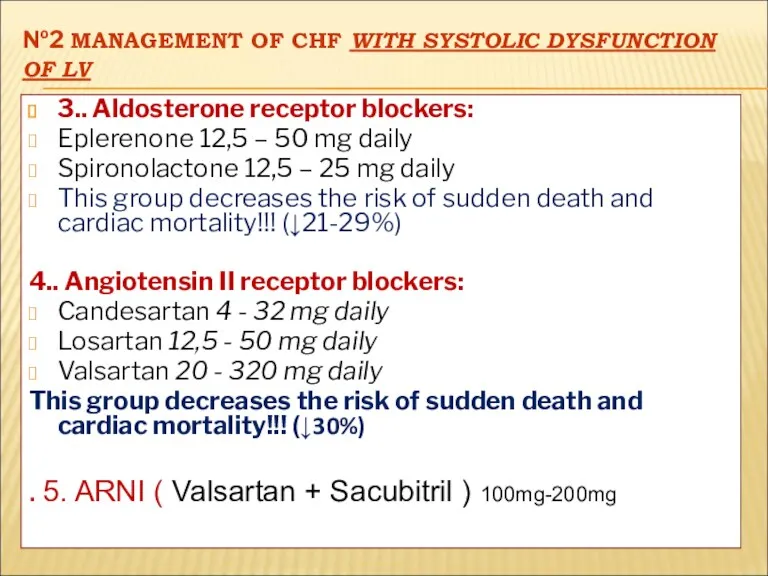
- 52. №2 MANAGEMENT OF CHF WITH SYSTOLIC DYSFUNCTION OF LV 3.. Aldosterone receptor blockers: Eplerenone 12,5 –
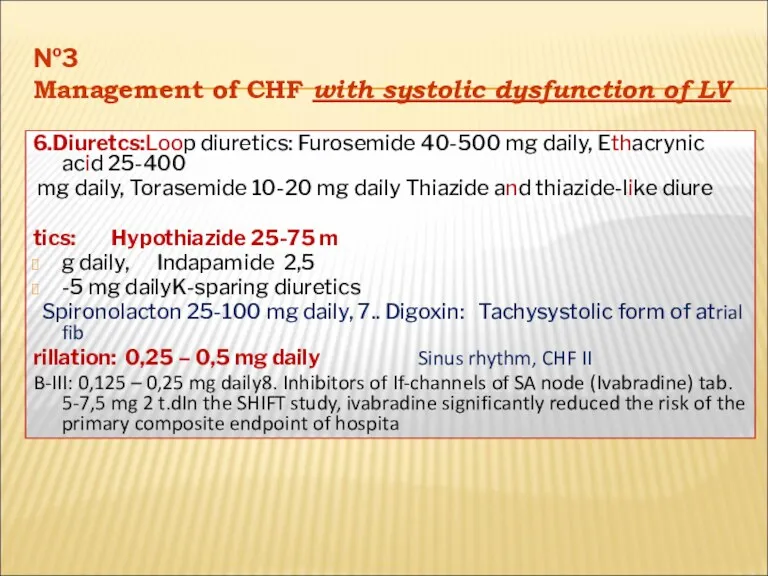
- 53. №3 Management of CHF with systolic dysfunction of LV 6.Diuretcs:Loop diuretics: Furosemide 40-500 mg daily, Ethacrynic
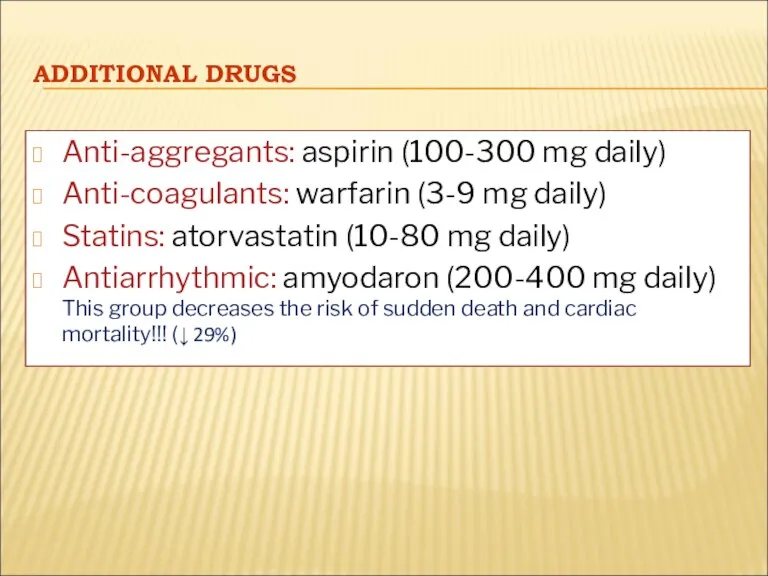
- 54. ADDITIONAL DRUGS Anti-aggregants: aspirin (100-300 mg daily) Anti-coagulants: warfarin (3-9 mg daily) Statins: atorvastatin (10-80 mg
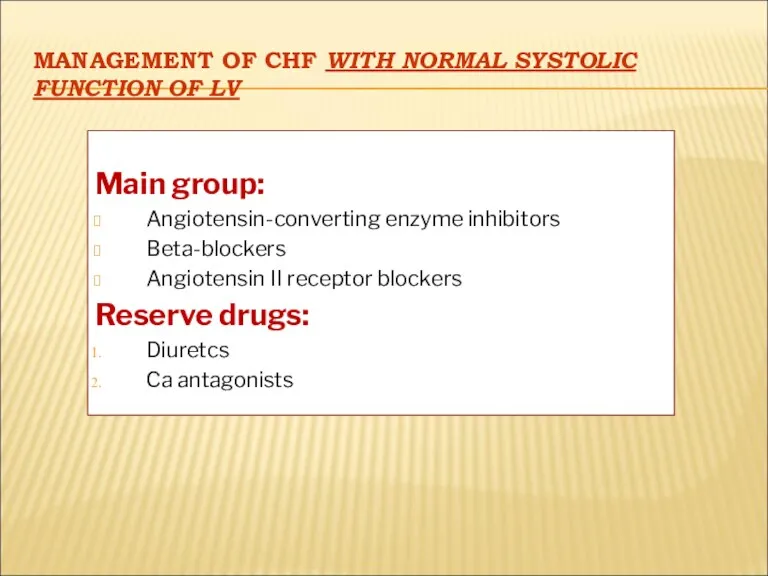
- 55. MANAGEMENT OF CHF WITH NORMAL SYSTOLIC FUNCTION OF LV Main group: Angiotensin-converting enzyme inhibitors Beta-blockers Angiotensin
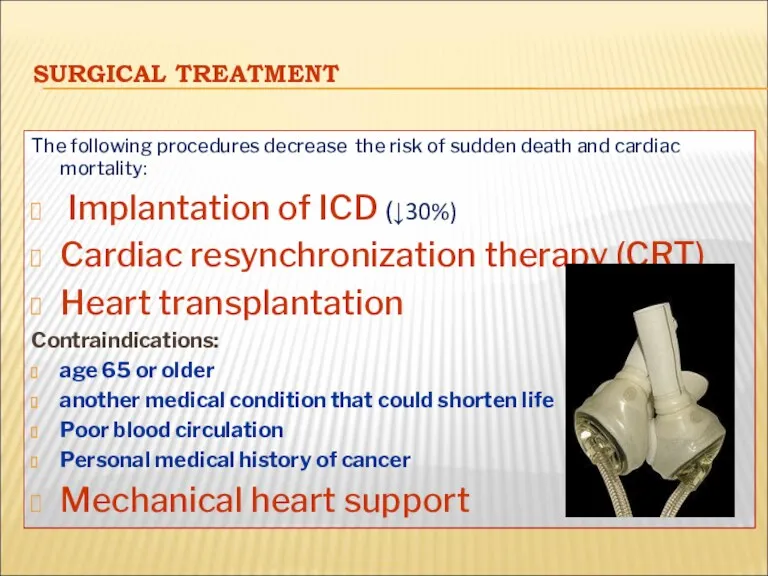
- 56. SURGICAL TREATMENT The following procedures decrease the risk of sudden death and cardiac mortality: Implantation of
- 58. Скачать презентацию
 Dental clinic
Dental clinic Воспаление. Этиологические факторы воспаления
Воспаление. Этиологические факторы воспаления Первая помощь при растяжении связок, вывихах суставов, переломах костей
Первая помощь при растяжении связок, вывихах суставов, переломах костей Тромбоз подключичной вены
Тромбоз подключичной вены Введение в пропедевтику внутренних болезней
Введение в пропедевтику внутренних болезней Дифференциальный диагноз анемий
Дифференциальный диагноз анемий Эндодонтиялық тәжірибеде лазерлі сәулені қолдан
Эндодонтиялық тәжірибеде лазерлі сәулені қолдан Введение в психиатрию, предмет, задачи, основные направления развития психиатрии
Введение в психиатрию, предмет, задачи, основные направления развития психиатрии Предраковые процессы
Предраковые процессы Психология детей с расстройствами эмоционально-волевой сферы и поведения
Психология детей с расстройствами эмоционально-волевой сферы и поведения Збудники анаеробних інфекцій
Збудники анаеробних інфекцій Неправильные положения плода (поперечное, косое). Причины. Диагностика. Ведение беременности и родов
Неправильные положения плода (поперечное, косое). Причины. Диагностика. Ведение беременности и родов Медициналық психология
Медициналық психология Современные методы фармацевтического анализа
Современные методы фармацевтического анализа Цитология (биология клетки)
Цитология (биология клетки) Питание детей с муковисцидозом
Питание детей с муковисцидозом Сальмонеллез у кошек и собак
Сальмонеллез у кошек и собак Лечение отеков до появления диуретиков
Лечение отеков до появления диуретиков Теміртапшылықты анемия
Теміртапшылықты анемия Сүйек кемігі
Сүйек кемігі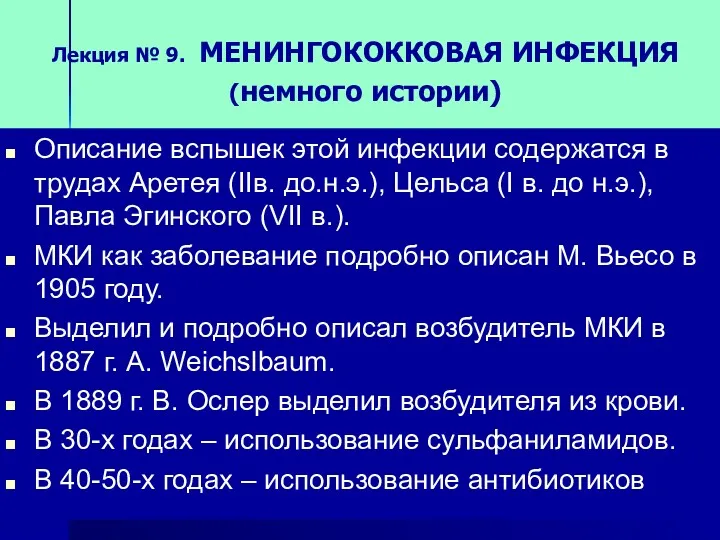 Менингококковая инфекция
Менингококковая инфекция Коронарлық жеткіліксіздік
Коронарлық жеткіліксіздік Роль иммунной системы при беременности
Роль иммунной системы при беременности Теория и организация адаптивной физической культуры
Теория и организация адаптивной физической культуры Синдром поражения миокарда
Синдром поражения миокарда Мышечная система. Скелетные мышцы
Мышечная система. Скелетные мышцы Методы определения центрального соотношения челюстей в стоматологии
Методы определения центрального соотношения челюстей в стоматологии The body’s defenses. Types of acquired immunity
The body’s defenses. Types of acquired immunity