Содержание
- 2. Plan 1. The concept of hospital infections 2. Pathogens of nosocomial infections 3 The properties of
- 3. infectious disease resulting from: Patients infected in hospital; infection of medical personnel, who working in health
- 4. By nosocomial infections DOES NOT include: case of patient in hospital in the incubation period; cases
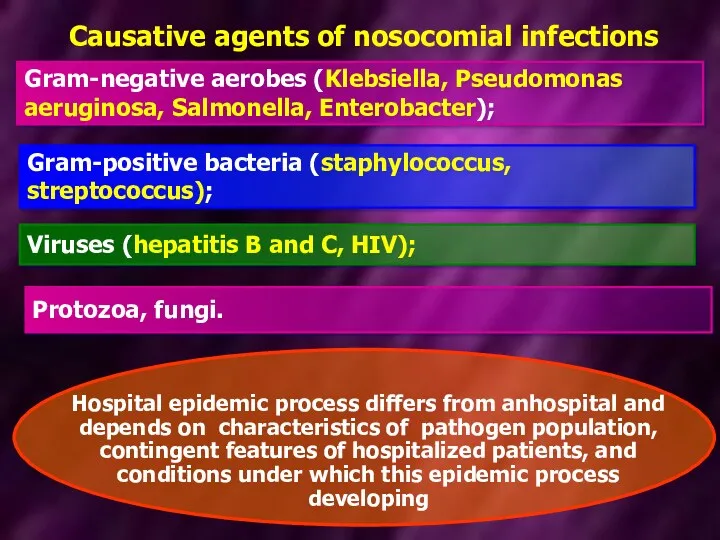
- 5. Causative agents of nosocomial infections Gram-negative aerobes (Klebsiella, Pseudomonas aeruginosa, Salmonella, Enterobacter); Gram-positive bacteria (staphylococcus, streptococcus);
- 6. Preventive measures for the prevention of introduction of community-acquired pathogens in hospital For hospitalization is necessary
- 7. CHARACTERISTICS OF HOSPITAL bacterial pathogens are resistant to adverse environmental factors: UV rays, dryness (hospital strains
- 8. CHARACTERISTICS OF HOSPITAL bacterial pathogens have multidrug-resistant to antibiotics (hospital strains of Klebsiella and Staphylococci resistant
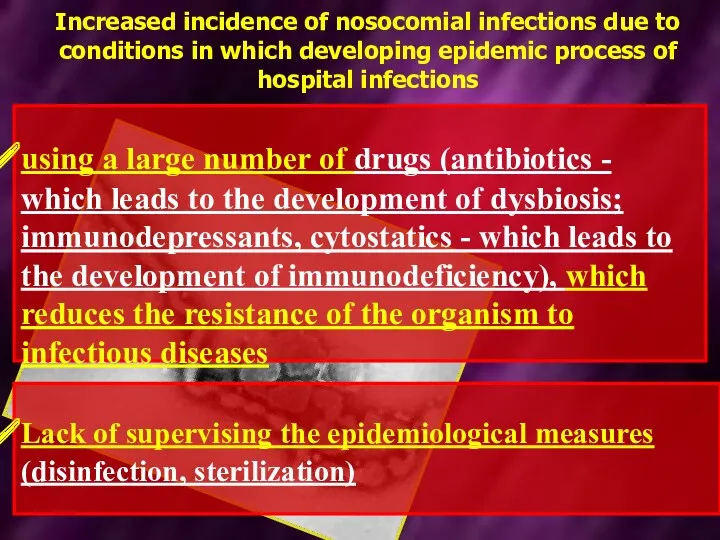
- 9. Increased incidence of nosocomial infections due to conditions in which developing epidemic process of hospital infections
- 10. Increased incidence of nosocomial infections due to conditions in which developing epidemic process of hospital infections
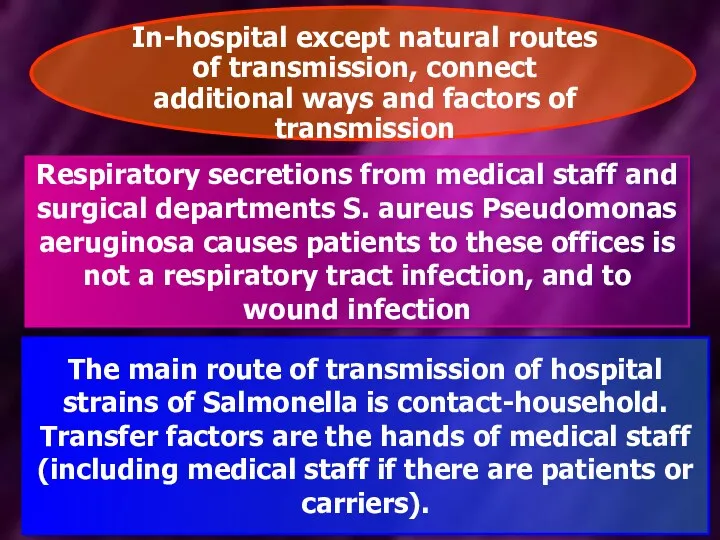
- 11. Respiratory secretions from medical staff and surgical departments S. aureus Pseudomonas aeruginosa causes patients to these
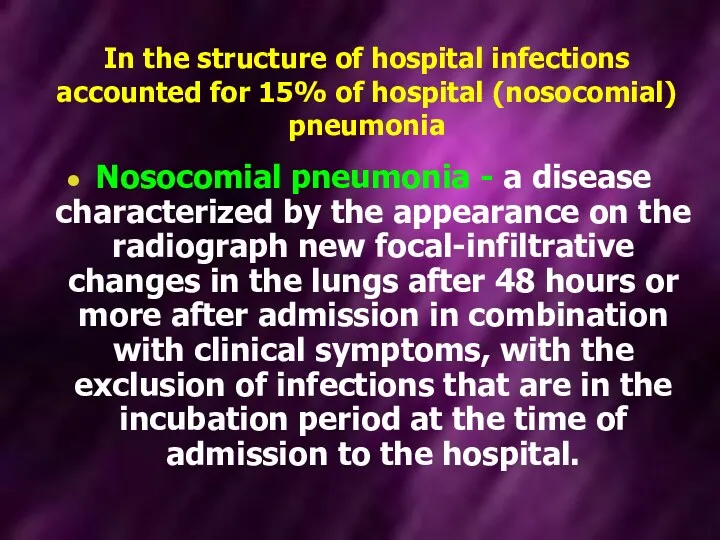
- 12. In the structure of hospital infections accounted for 15% of hospital (nosocomial) pneumonia Nosocomial pneumonia -
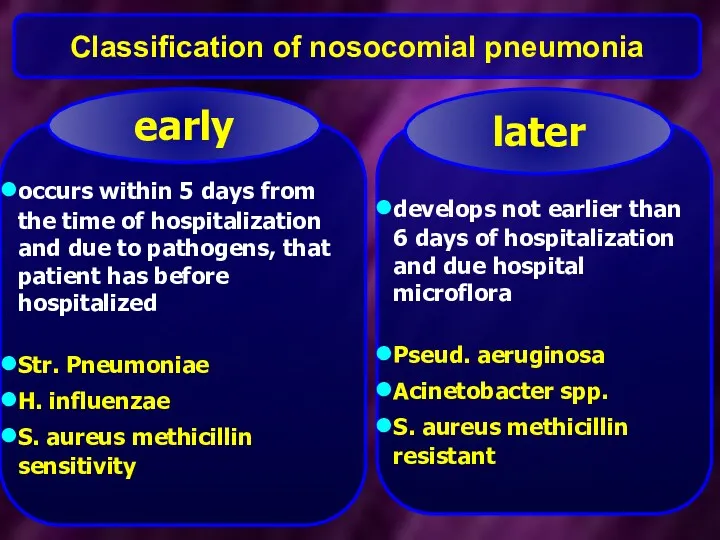
- 13. Classification of nosocomial pneumonia occurs within 5 days from the time of hospitalization and due to
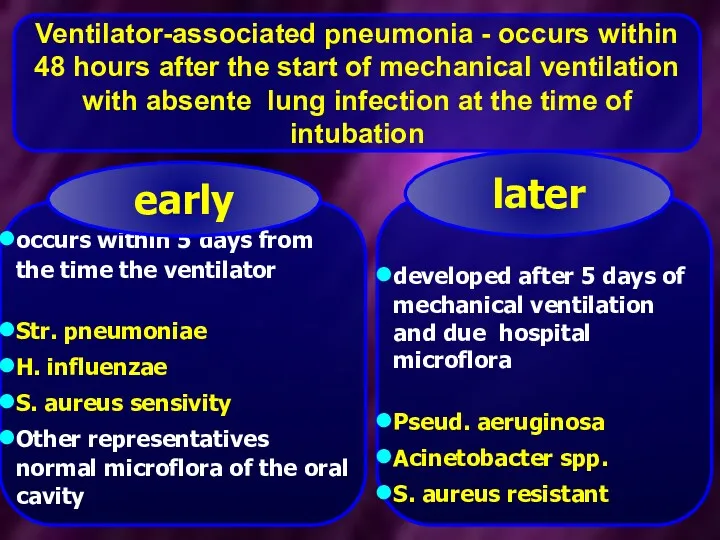
- 14. Ventilator-associated pneumonia - occurs within 48 hours after the start of mechanical ventilation with absente lung
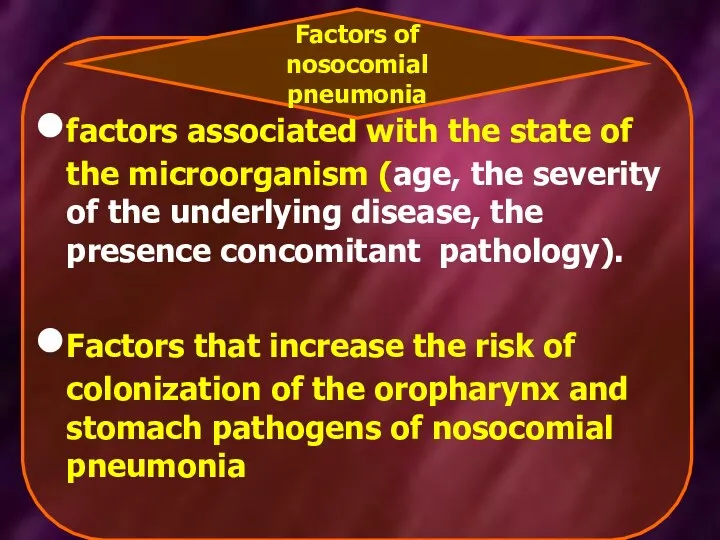
- 15. factors associated with the state of the microorganism (age, the severity of the underlying disease, the
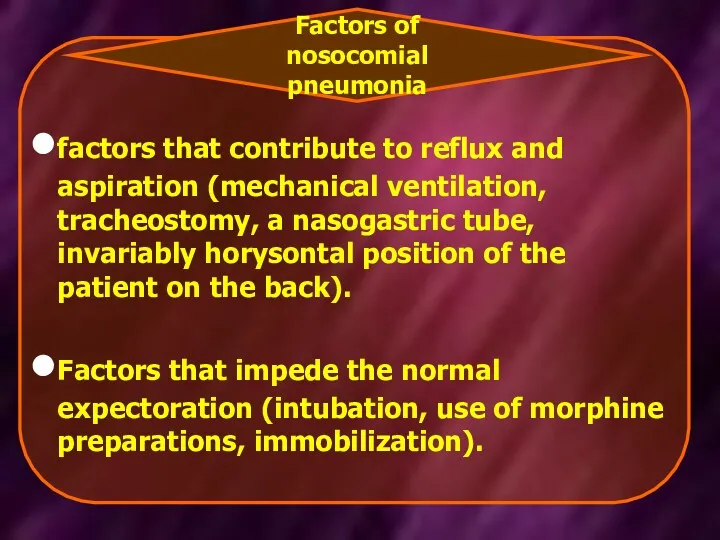
- 16. factors that contribute to reflux and aspiration (mechanical ventilation, tracheostomy, a nasogastric tube, invariably horysontal position
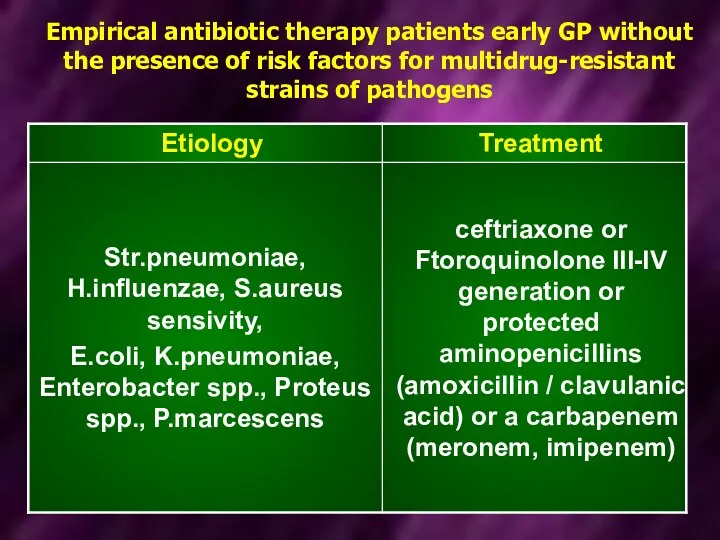
- 17. Empirical antibiotic therapy patients early GP without the presence of risk factors for multidrug-resistant strains of
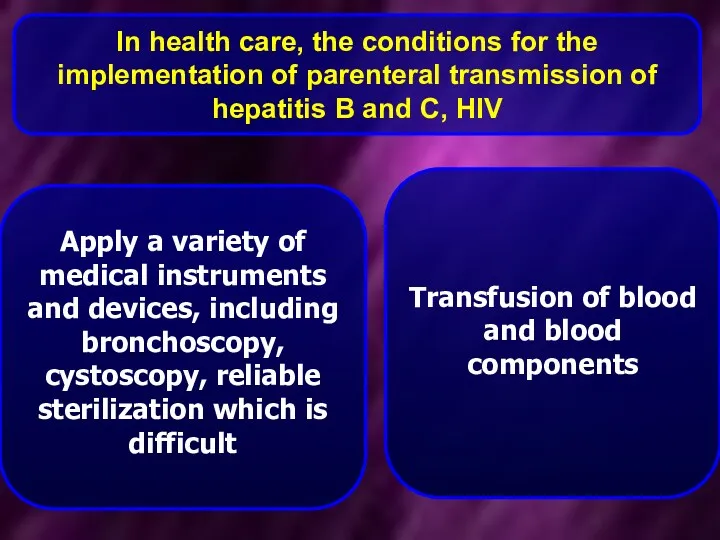
- 18. In health care, the conditions for the implementation of parenteral transmission of hepatitis B and C,
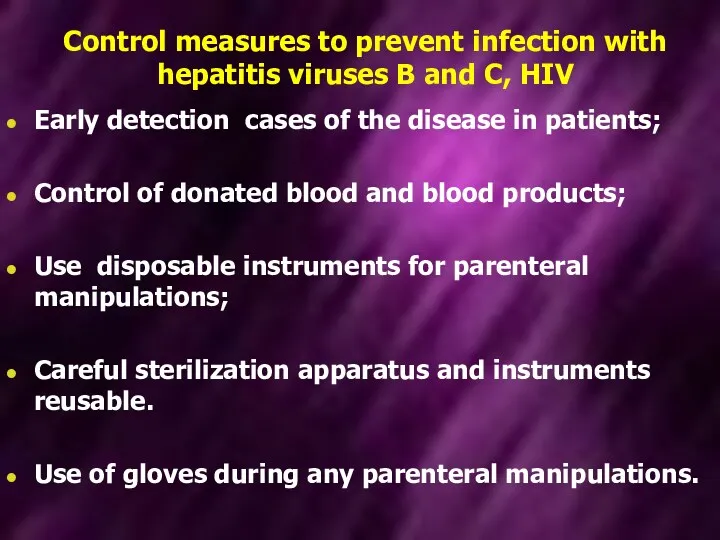
- 19. Control measures to prevent infection with hepatitis viruses B and C, HIV Early detection cases of
- 20. HIV infection any damage of skin, mucous membranes nurses, pollution of their biomaterial patients during help
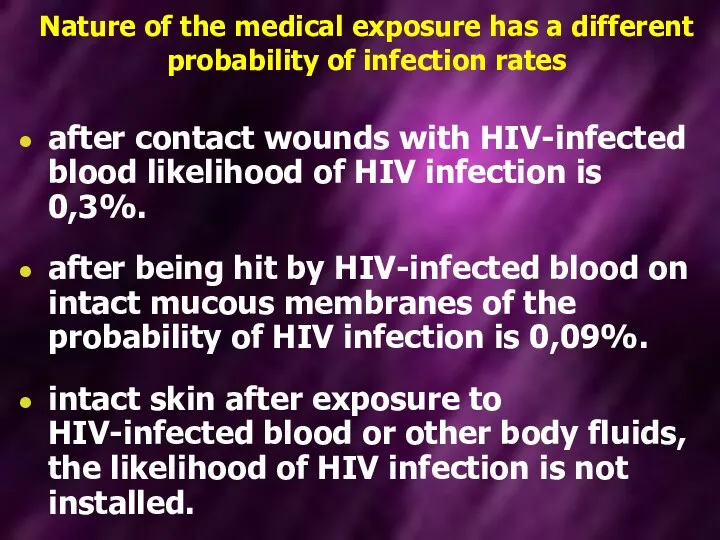
- 21. Nature of the medical exposure has a different probability of infection rates after contact wounds with
- 22. Conducting post-exposure prophylaxis (PEP) Order from 05.11.2013 № 955 - A short course of antiretroviral drugs
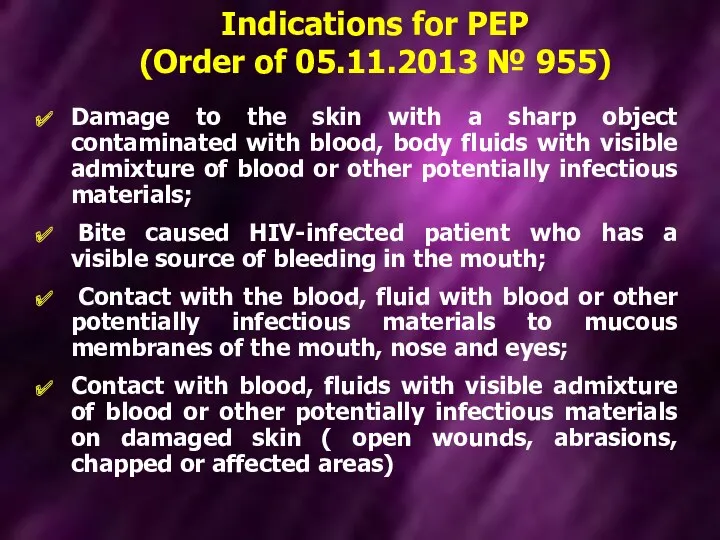
- 23. Damage to the skin with a sharp object contaminated with blood, body fluids with visible admixture
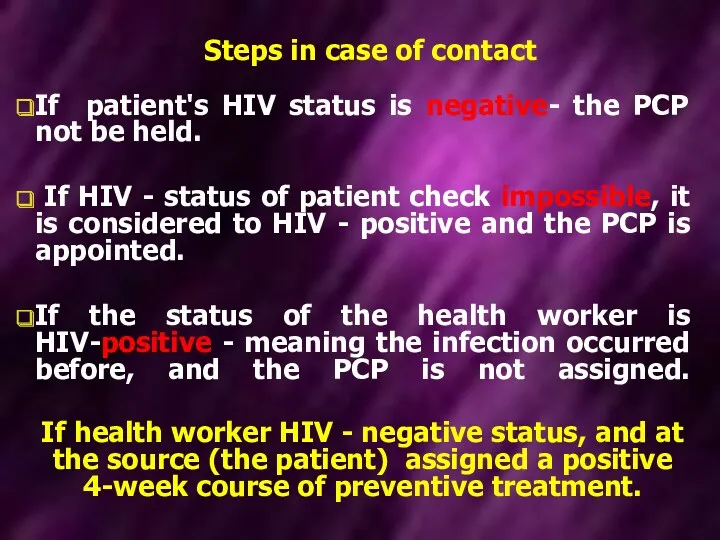
- 24. Steps in case of contact If patient's HIV status is negative- the PCP not be held.
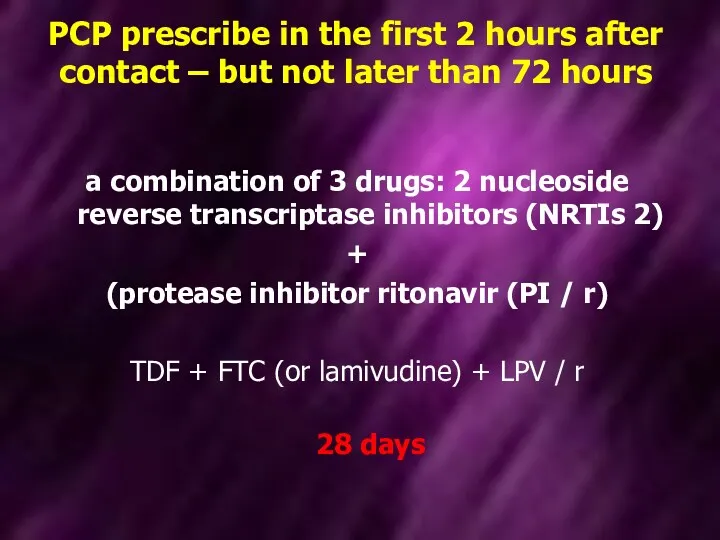
- 25. PCP prescribe in the first 2 hours after contact – but not later than 72 hours
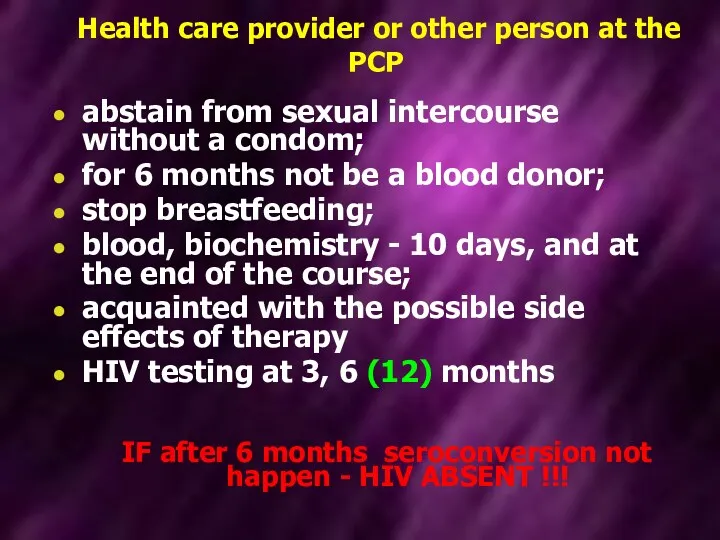
- 26. Health care provider or other person at the PCP abstain from sexual intercourse without a condom;
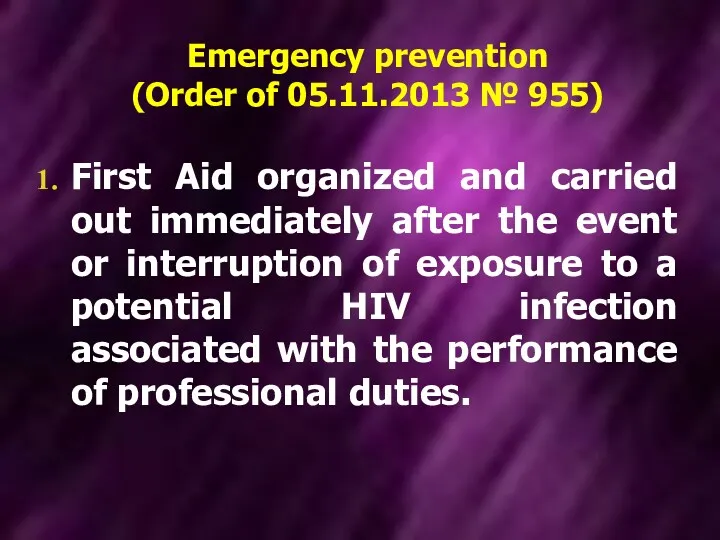
- 27. Emergency prevention (Order of 05.11.2013 № 955) First Aid organized and carried out immediately after the
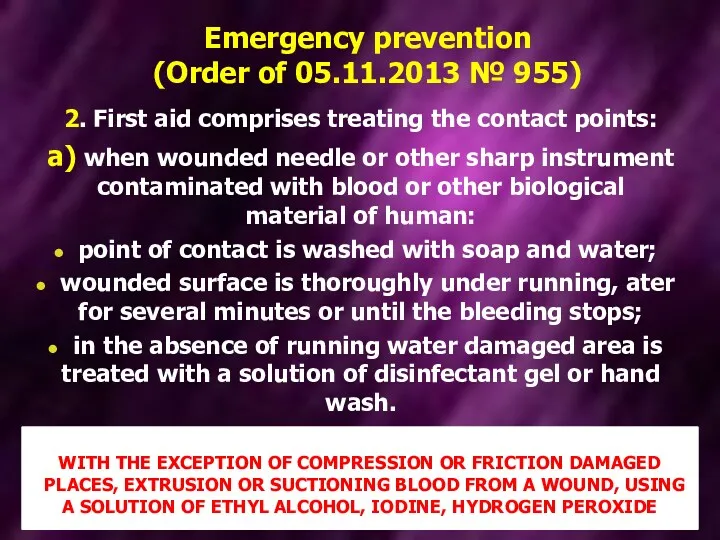
- 28. Emergency prevention (Order of 05.11.2013 № 955) 2. First aid comprises treating the contact points: а)
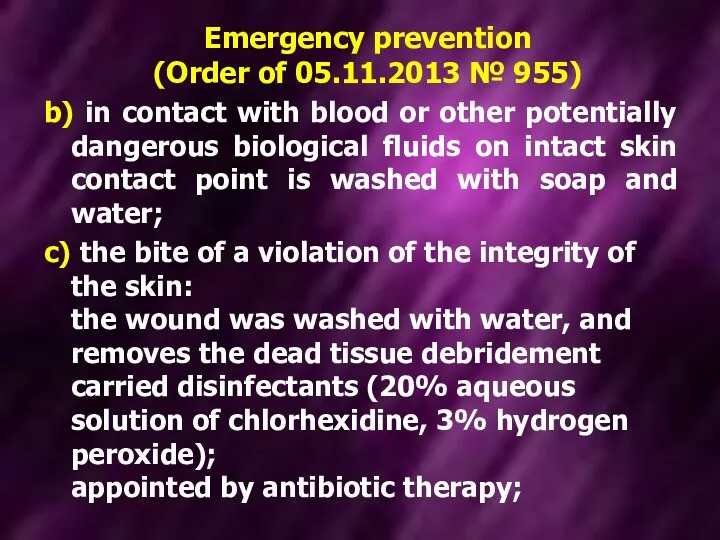
- 29. Emergency prevention (Order of 05.11.2013 № 955) b) in contact with blood or other potentially dangerous
- 30. Emergency prevention (Order of 05.11.2013 № 955) d) After contact with blood or other potentially dangerous
- 31. Emergency prevention (Order of 05.11.2013 № 955) e) when blood or other potentially dangerous biological fluids
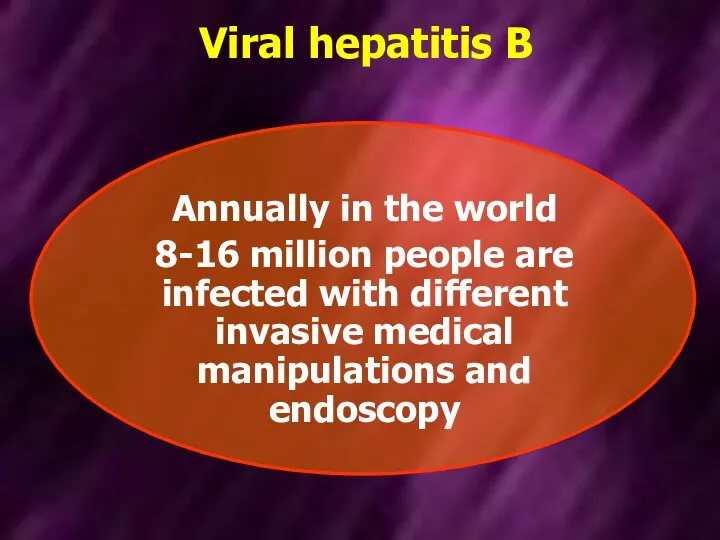
- 32. Viral hepatitis B Annually in the world 8-16 million people are infected with different invasive medical
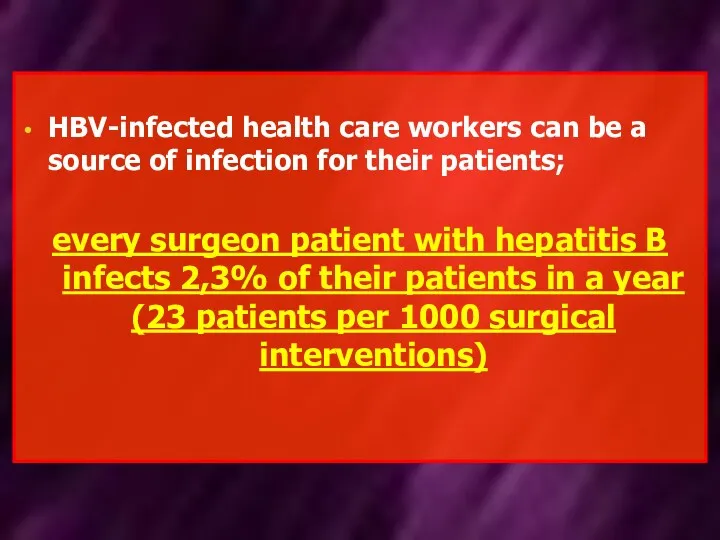
- 33. HBV-infected health care workers can be a source of infection for their patients; every surgeon patient
- 34. Viral hepatitis В Indications for plan vaccination: Medical workers; military personnel, firemen; staff and patients of
- 35. Viral hepatitis В Indications for plan vaccination: people who use drugs intravenously, HIV-infected, persons who frequently
- 36. Vaccines, registered in Ukraine, for the prevention of hepatitis B containing recombinant antigen HBs 1) Heberbiovac
- 37. Viral hepatitis В CONTRAINDICATIONS -universal for all vaccines; -Pregnancy and lactation -NOT are contraindications. The vaccine
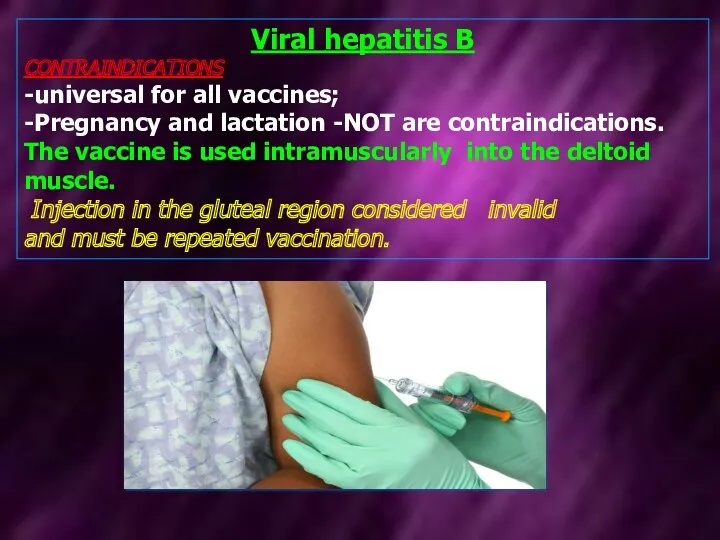
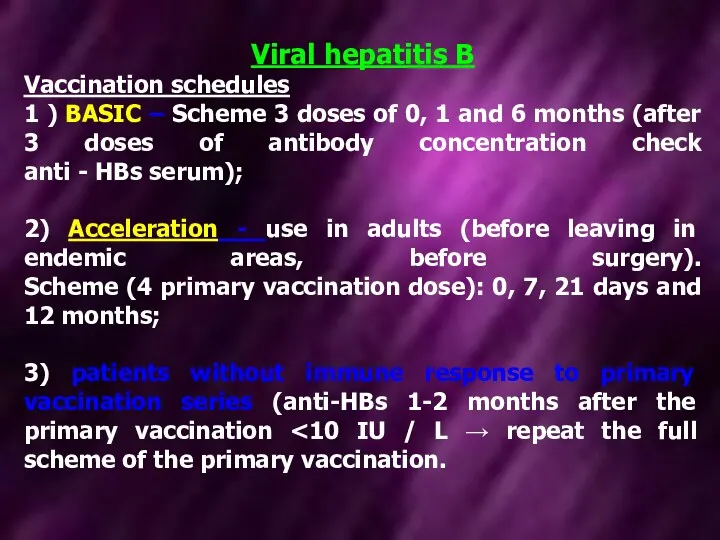
- 38. Viral hepatitis В Vaccination schedules 1 ) BASIC – Scheme 3 doses of 0, 1 and
- 40. Скачать презентацию
 Профессия медицинской сестры
Профессия медицинской сестры Әйелдер кеңесі және босану үйінің қызметінің көрсеткіші мен құрылымы
Әйелдер кеңесі және босану үйінің қызметінің көрсеткіші мен құрылымы Первая помощь при неотложных состояниях
Первая помощь при неотложных состояниях Вирусология. Клиническая и экологическая микробиология. Инфекция и иммунитет при вирусных заболеваниях. (Модуль 3.22)
Вирусология. Клиническая и экологическая микробиология. Инфекция и иммунитет при вирусных заболеваниях. (Модуль 3.22) Медикаментозды остеопороз: алдын алудағы және түзетуге негізгі ұстанымдар
Медикаментозды остеопороз: алдын алудағы және түзетуге негізгі ұстанымдар Травма живота
Травма живота Коллекция фиточаев Целебные травы Ольхона
Коллекция фиточаев Целебные травы Ольхона Протоонкогены и передача клеточного сигнала
Протоонкогены и передача клеточного сигнала Красный плоский лишай
Красный плоский лишай Искусственные объекты, которые мы готовы или не готовы внедрить в свое тело для его совершенствования или поддержания здоровья
Искусственные объекты, которые мы готовы или не готовы внедрить в свое тело для его совершенствования или поддержания здоровья Грипп – острая инфекционная болезнь
Грипп – острая инфекционная болезнь Организация медицинского освидетельствования граждан при постановке их на воинский учёт
Организация медицинского освидетельствования граждан при постановке их на воинский учёт Принципы выбора, методы оценки эффективности и безопасности антиаритмических препаратов
Принципы выбора, методы оценки эффективности и безопасности антиаритмических препаратов Антисептические средства (тема №3)
Антисептические средства (тема №3) Сестринский процесс при туберкулезе органов дыхания у взрослых
Сестринский процесс при туберкулезе органов дыхания у взрослых Психопатология, психопатия и акцентуация характера
Психопатология, психопатия и акцентуация характера анаэробная инфекция
анаэробная инфекция Жатыр мойны және денесінің обыры тақырыбына презентация
Жатыр мойны және денесінің обыры тақырыбына презентация Диагностика геморрагических лихорадок, клещевого энцефалита, лайм-боррелиоза
Диагностика геморрагических лихорадок, клещевого энцефалита, лайм-боррелиоза Этико-правовое регулирование биомедицинских исследований на человеке и на животных
Этико-правовое регулирование биомедицинских исследований на человеке и на животных Особенности подросткового возраста
Особенности подросткового возраста Дезинфекционные технологии и оборудование для обеззараживания воздуха
Дезинфекционные технологии и оборудование для обеззараживания воздуха Иммуномодуляторы. Иммунокорректоры
Иммуномодуляторы. Иммунокорректоры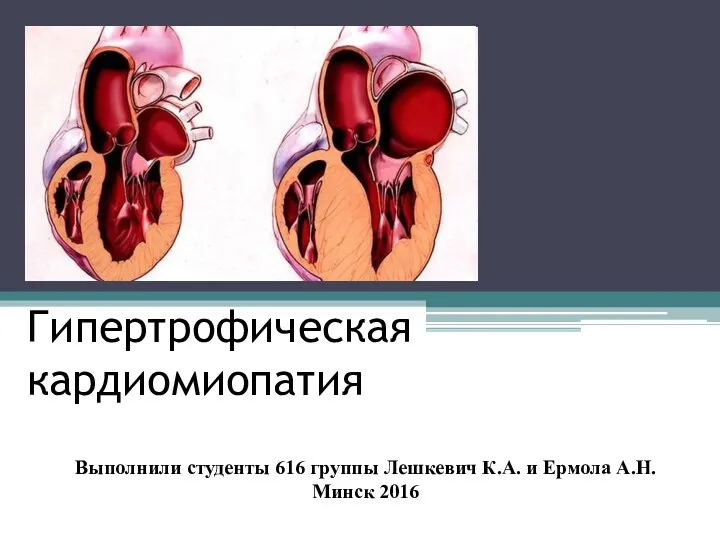 Гипертрофическая кардиомиопатия
Гипертрофическая кардиомиопатия Инфузионная терапия при шоке
Инфузионная терапия при шоке Биоэтические проблемы проекта Геном человека
Биоэтические проблемы проекта Геном человека Болезни десен и пародонта. Лекция №4
Болезни десен и пародонта. Лекция №4 Герпетическая инфекция
Герпетическая инфекция