Содержание
- 2. PLAN 1. Introduction General means about hypothyroidism & Diffuse toxic goiter 2. Main body Classification Etiology
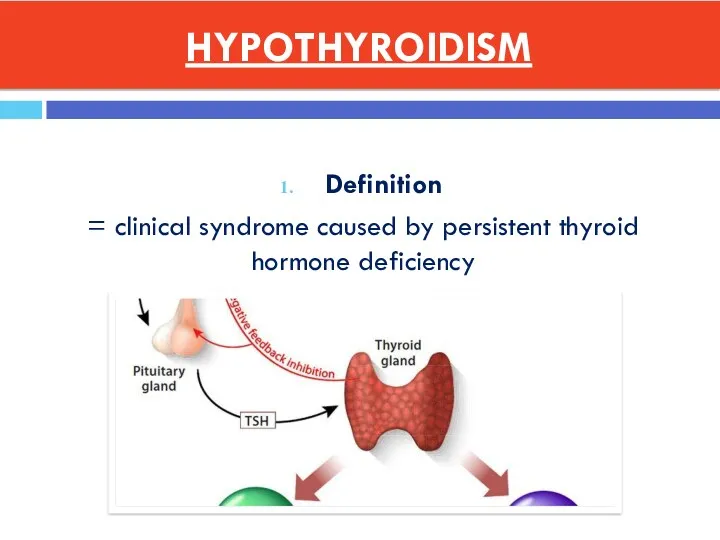
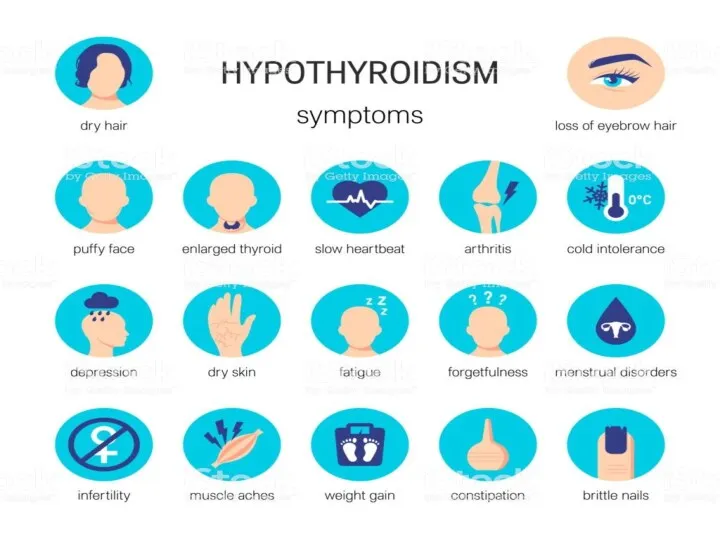
- 5. HYPOTHYROIDISM Definition = clinical syndrome caused by persistent thyroid hormone deficiency
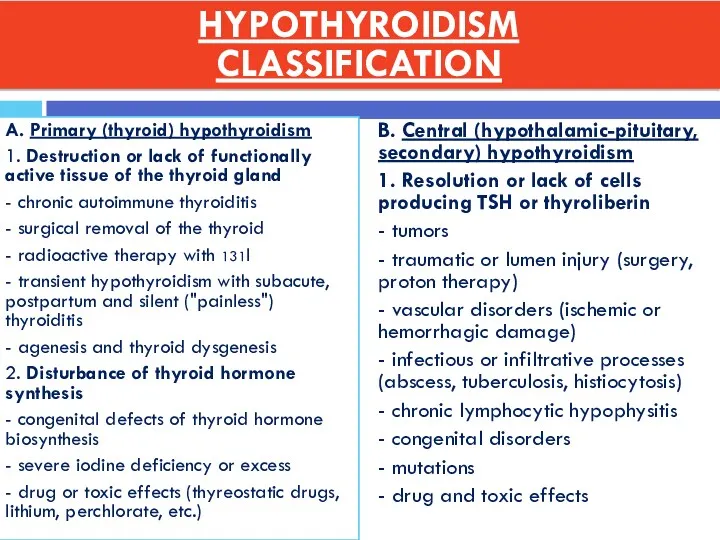
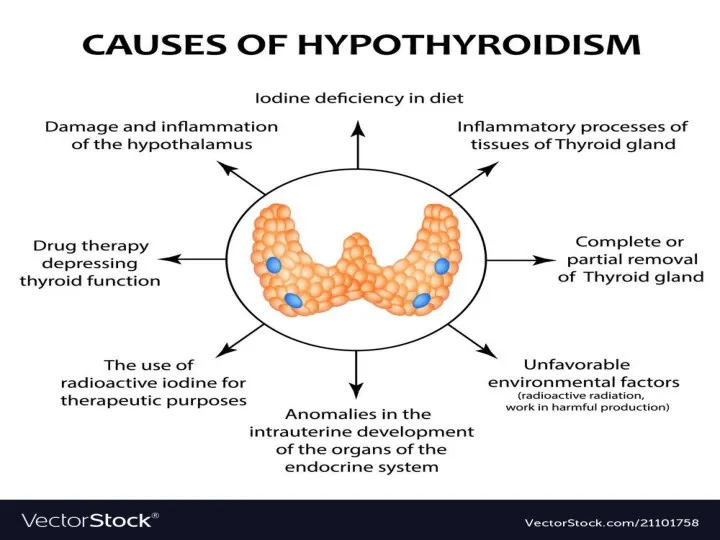
- 6. A. Primary (thyroid) hypothyroidism 1. Destruction or lack of functionally active tissue of the thyroid gland
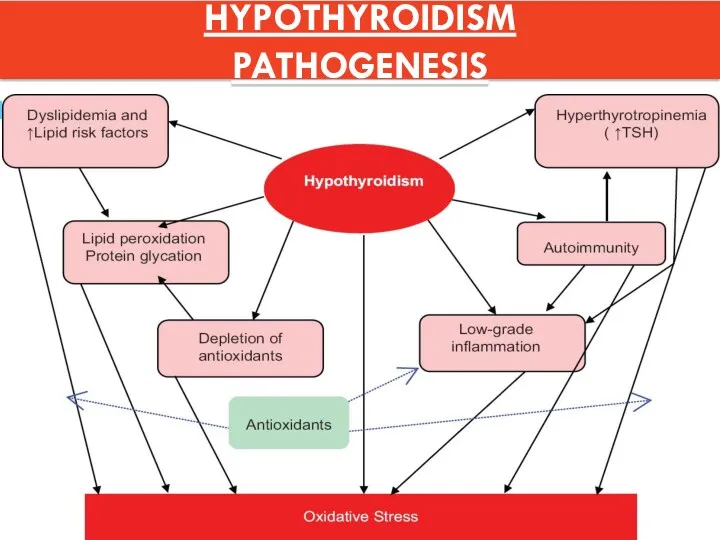
- 8. HYPOTHYROIDISM PATHOGENESIS
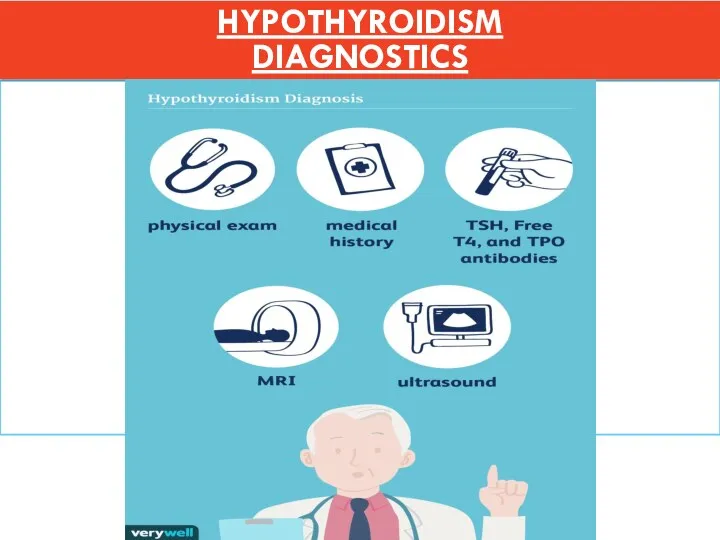
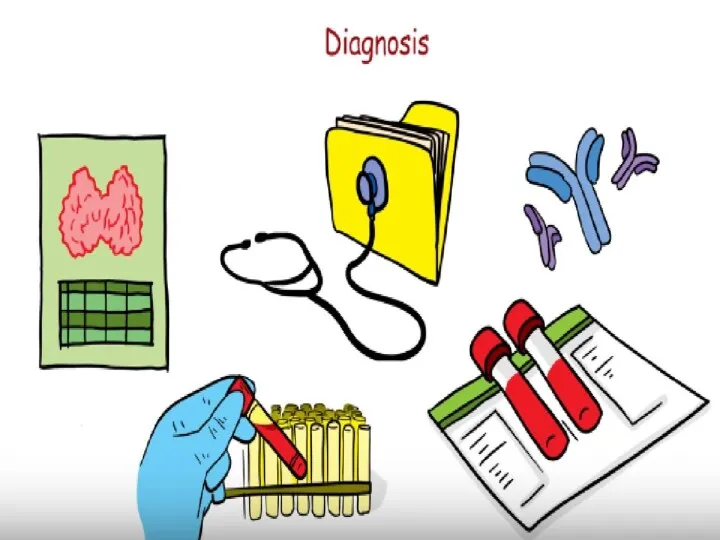
- 11. HYPOTHYROIDISM DIAGNOSTICS
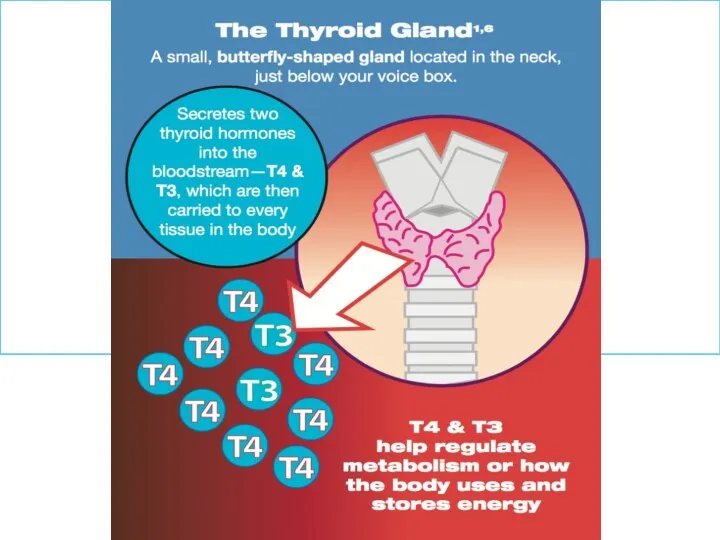
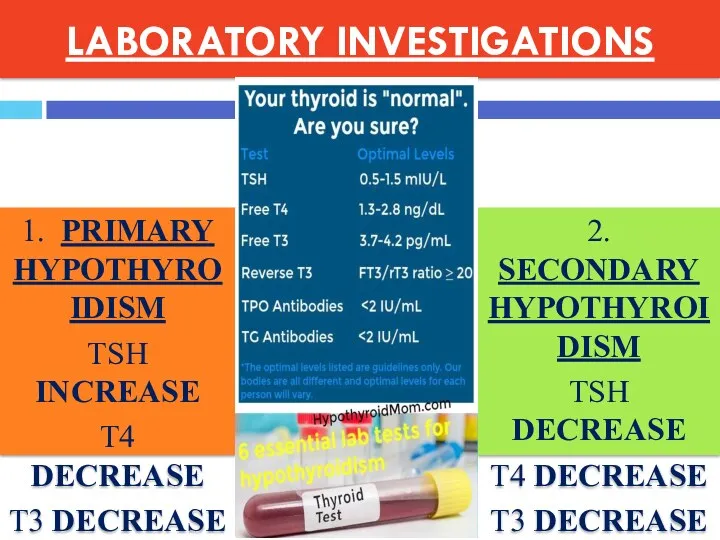
- 12. LABORATORY INVESTIGATIONS 1. PRIMARY HYPOTHYROIDISM TSH INCREASE T4 DECREASE T3 DECREASE 2. SECONDARY HYPOTHYROIDISM TSH DECREASE
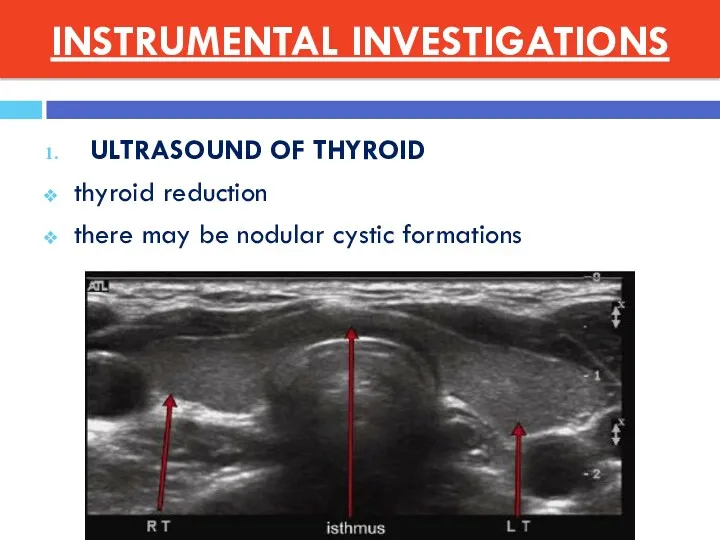
- 13. INSTRUMENTAL INVESTIGATIONS ULTRASOUND OF THYROID thyroid reduction there may be nodular cystic formations
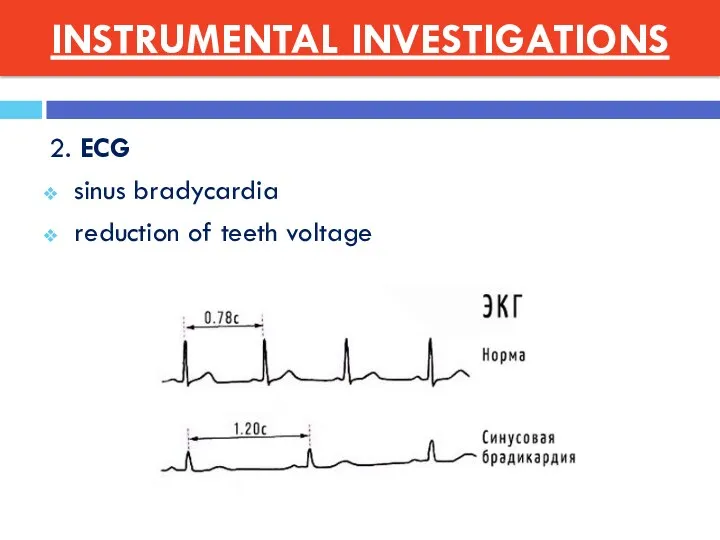
- 14. 2. ECG sinus bradycardia reduction of teeth voltage INSTRUMENTAL INVESTIGATIONS
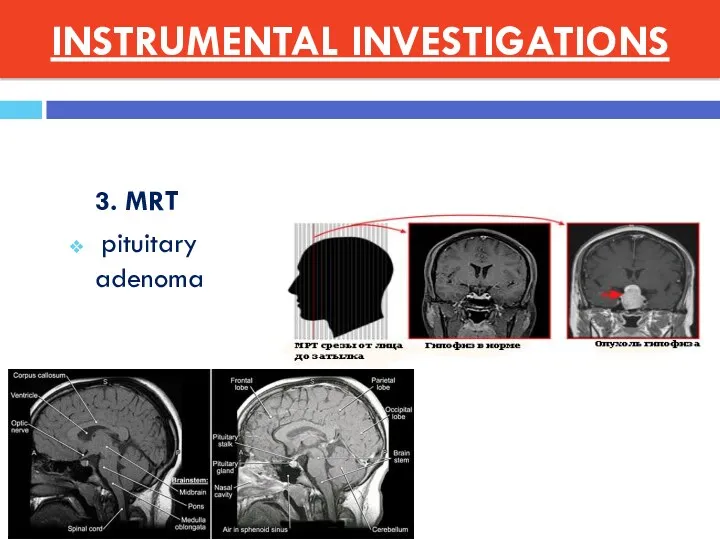
- 15. 3. MRT pituitary adenoma INSTRUMENTAL INVESTIGATIONS
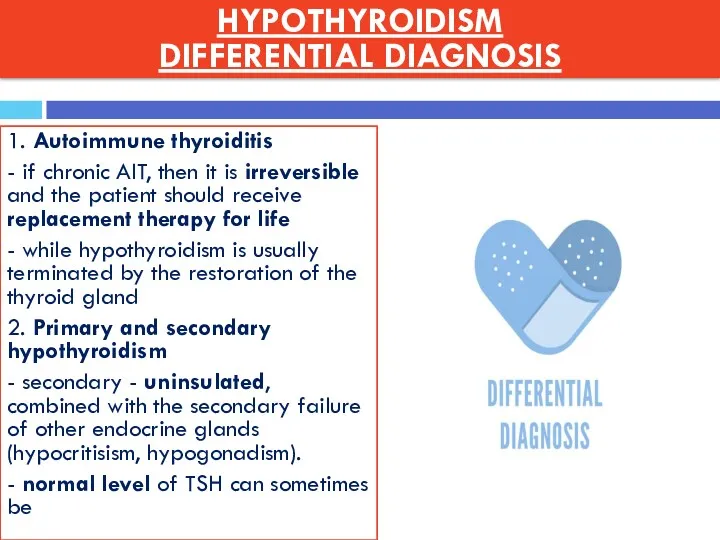
- 16. 1. Autoimmune thyroiditis - if chronic AIT, then it is irreversible and the patient should receive
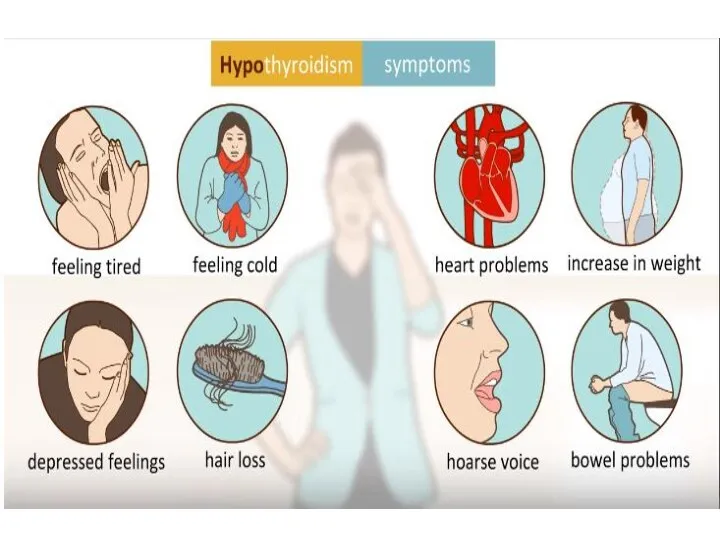
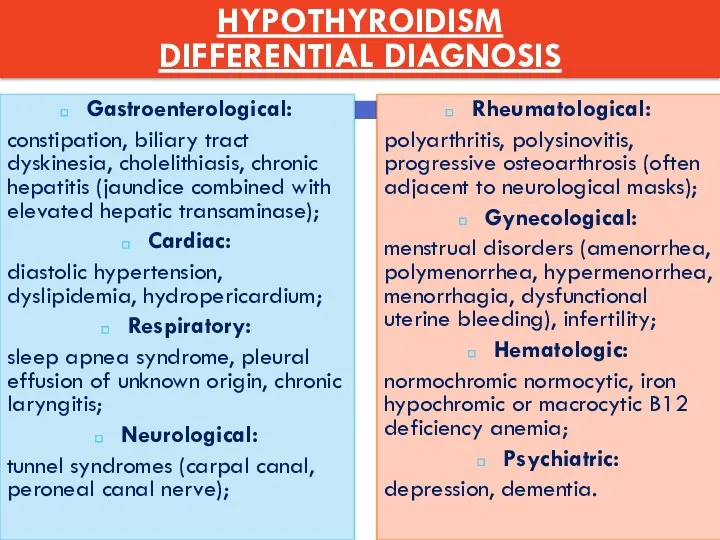
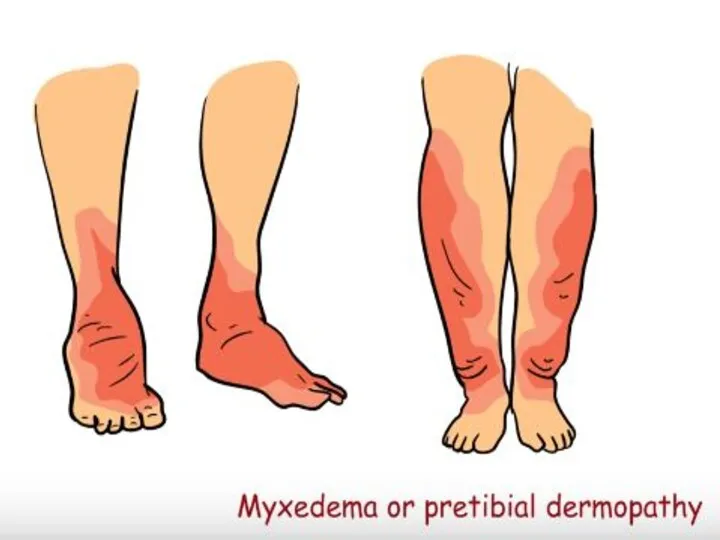
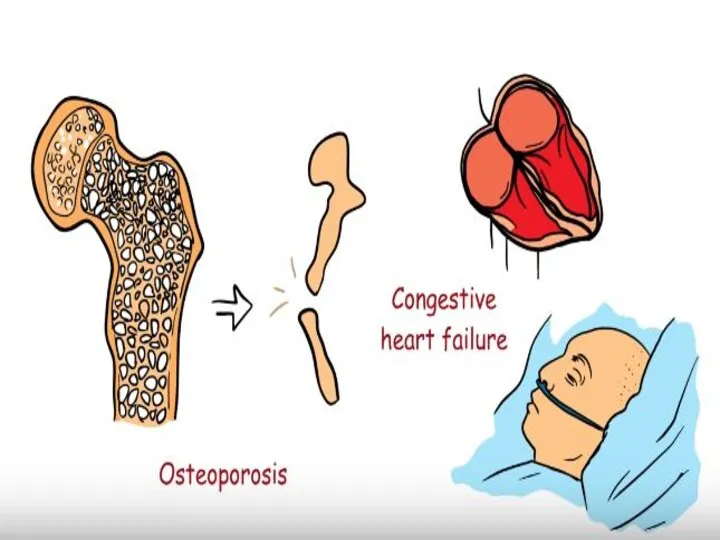
- 17. Rheumatological: polyarthritis, polysinovitis, progressive osteoarthrosis (often adjacent to neurological masks); Gynecological: menstrual disorders (amenorrhea, polymenorrhea, hypermenorrhea,
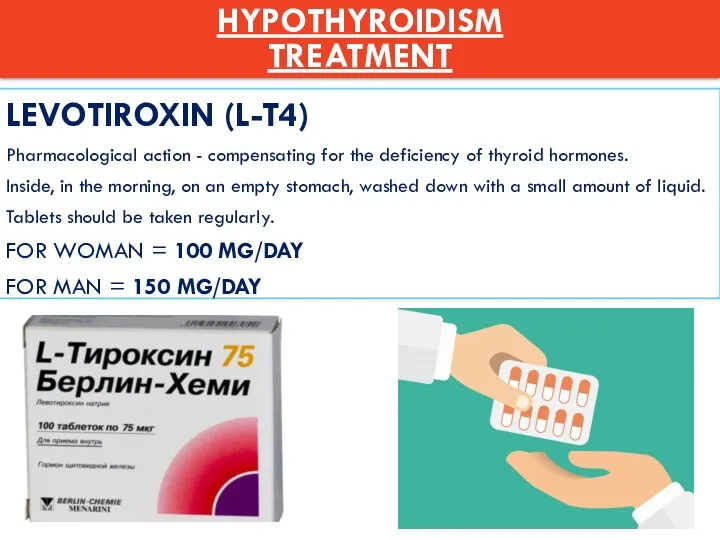
- 18. LEVOTIROXIN (L-T4) Pharmacological action - compensating for the deficiency of thyroid hormones. Inside, in the morning,
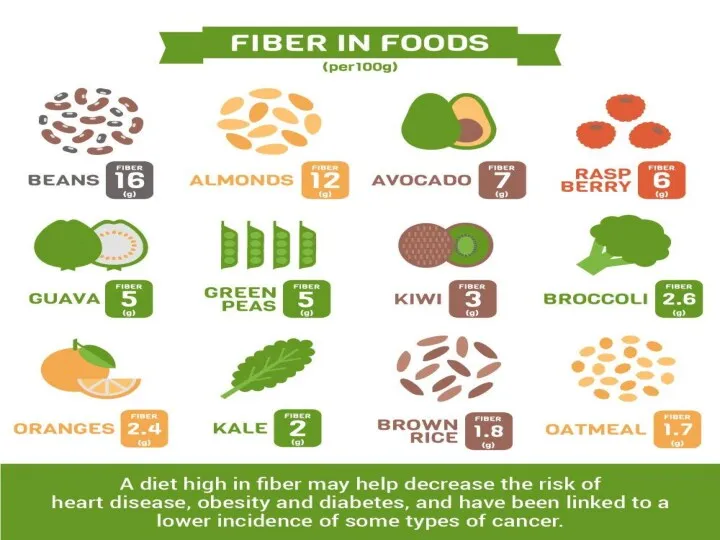
- 19. CONCLUSION Low-fat diet with plenty of fiber Patients activation Outdoor stay Wearing warm clothes
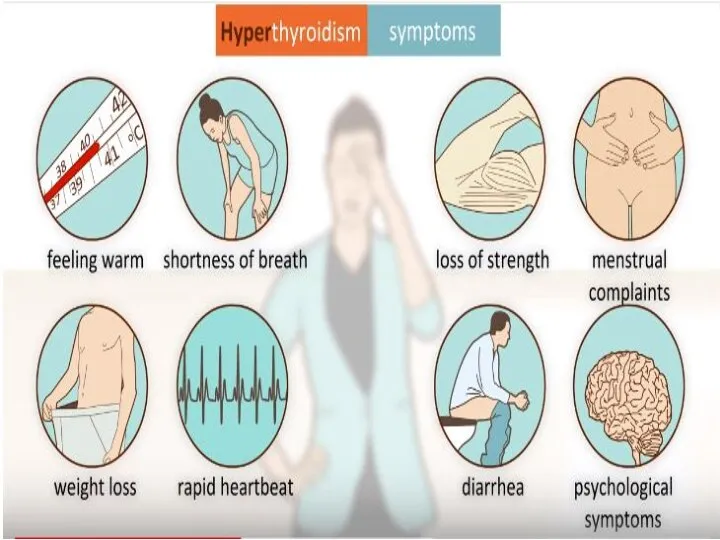
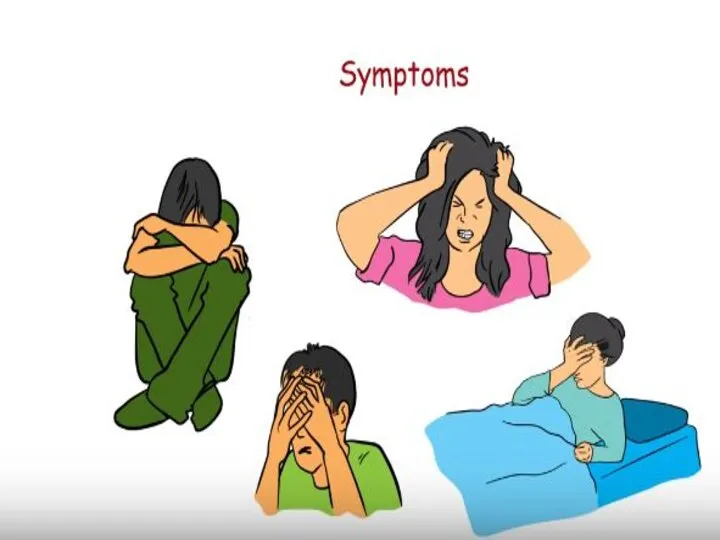
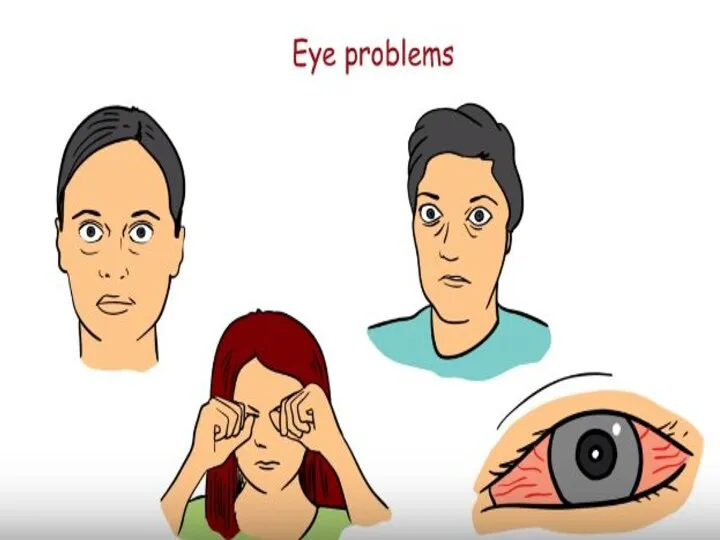
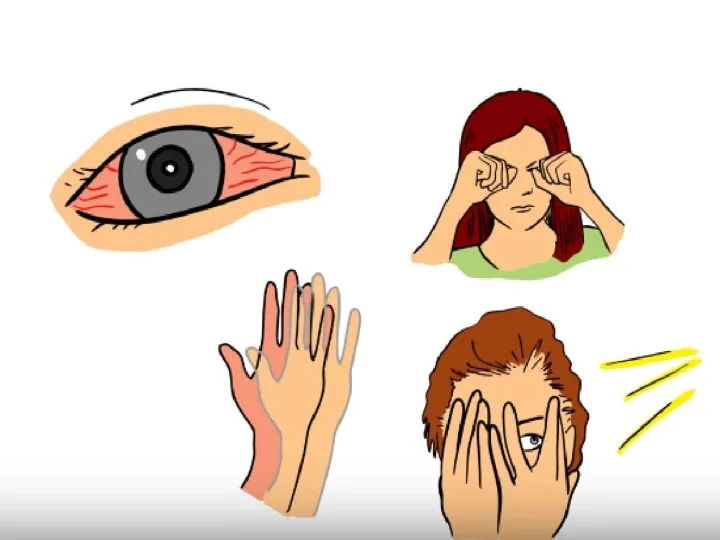
- 21. DIFFUSE TOXIC GOITER Definition = systemic autoimmune disease, which develops as a result of the production
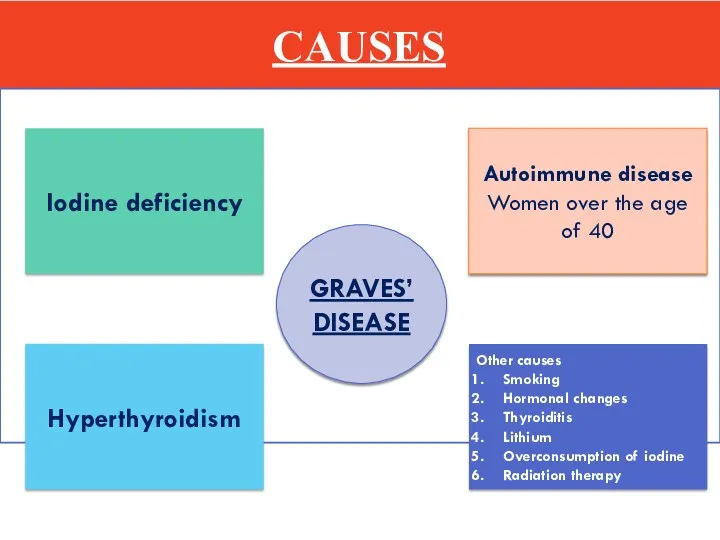
- 22. CAUSES GRAVES’ DISEASE Iodine deficiency Autoimmune disease Women over the age of 40 Hyperthyroidism Other causes
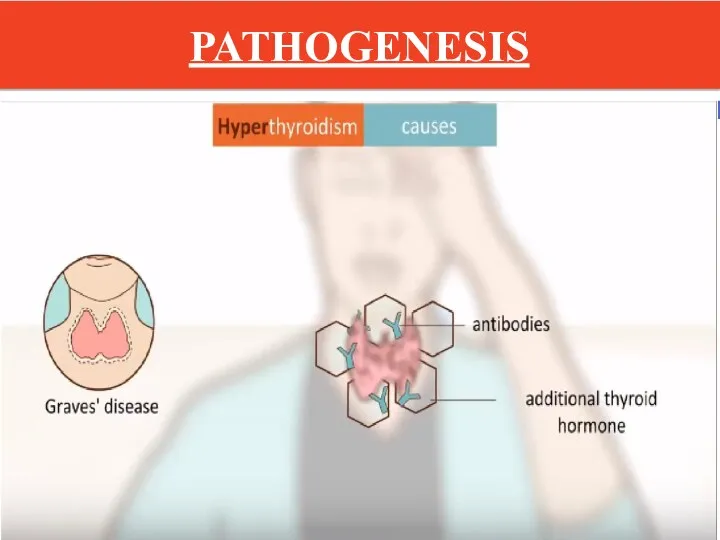
- 23. PATHOGENESIS
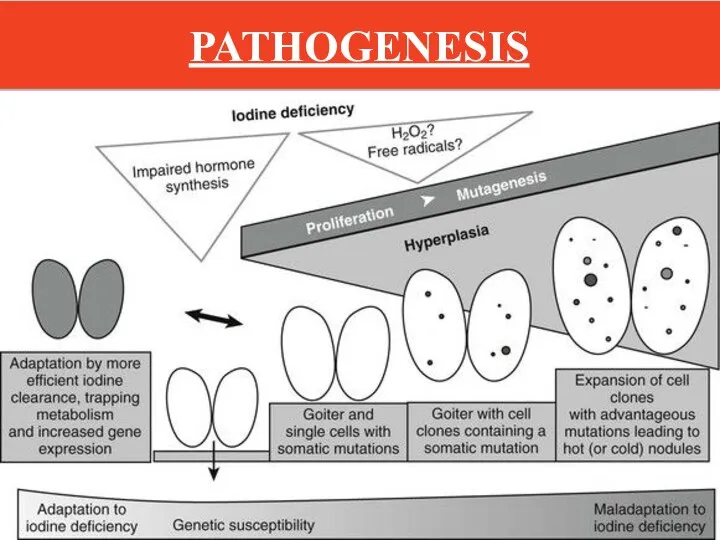
- 24. PATHOGENESIS
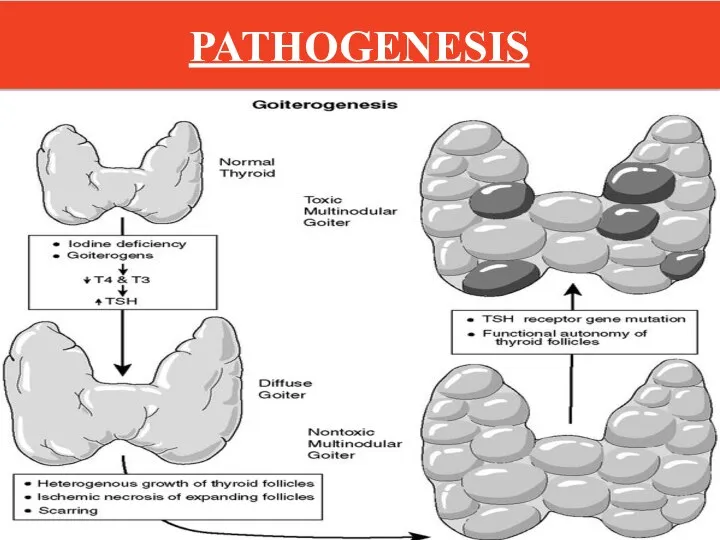
- 25. PATHOGENESIS
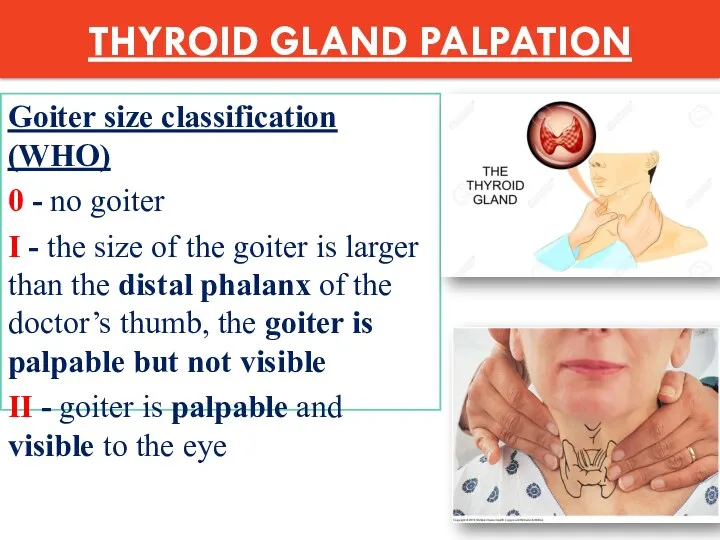
- 35. THYROID GLAND PALPATION Goiter size classification (WHO) 0 - no goiter I - the size of
- 36. Study of functional activity of the thyroid gland Thyroid hormones in the blood TSH DECREASE (
- 37. Study of immunological markers ANTIBODIES TO r-TSH - 99-100% ANTIBODIES TO TPO (TYREOPEROXIDASE) – 40-60%
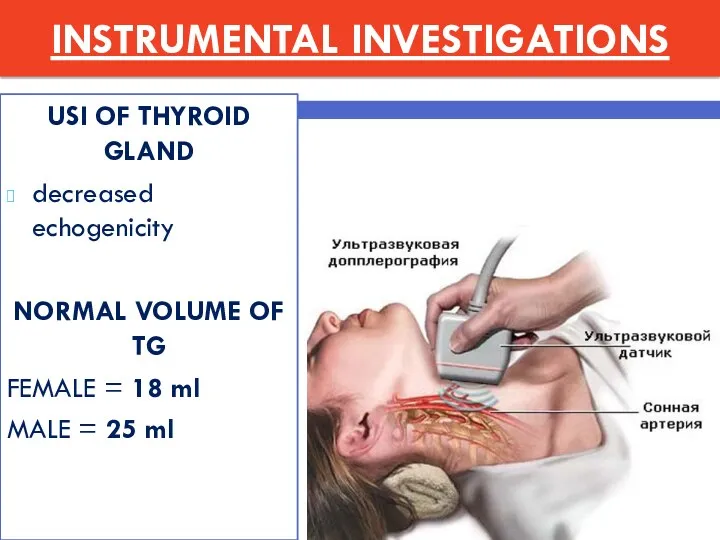
- 38. INSTRUMENTAL INVESTIGATIONS USI OF THYROID GLAND decreased echogenicity NORMAL VOLUME OF TG FEMALE = 18 ml
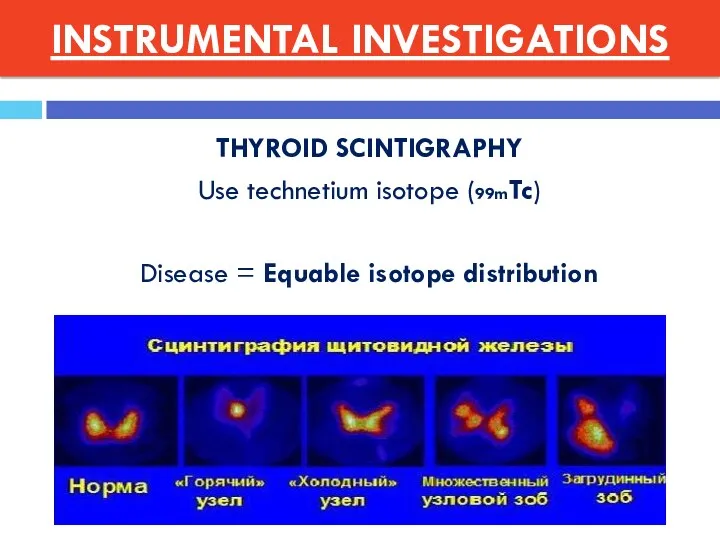
- 39. THYROID SCINTIGRAPHY Use technetium isotope (99mTc) Disease = Equable isotope distribution INSTRUMENTAL INVESTIGATIONS
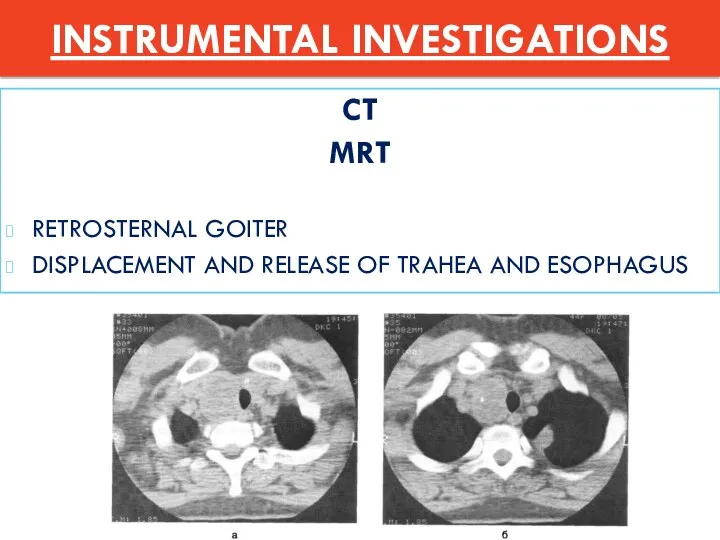
- 40. CT MRT RETROSTERNAL GOITER DISPLACEMENT AND RELEASE OF TRAHEA AND ESOPHAGUS INSTRUMENTAL INVESTIGATIONS
- 41. DIFFERENTIAL DIAGNOSTICS Thyrotoxicosis due to destruction of thyroid tissue Painless silent thyroiditis Subacute thyroiditis Radiation thyroiditis
- 43. NON-MEDICAL TREATMENT Limiting physical activity To give up smoking
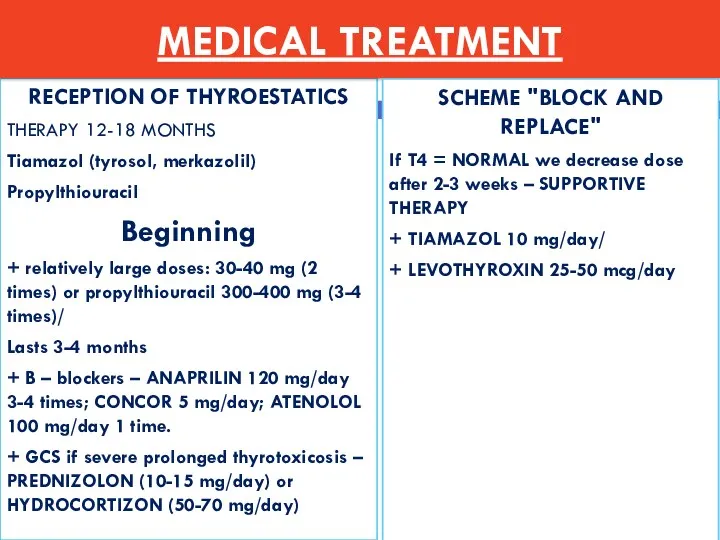
- 44. RECEPTION OF THYROESTATICS THERAPY 12-18 MONTHS Tiamazol (tyrosol, merkazolil) Propylthiouracil Beginning + relatively large doses: 30-40
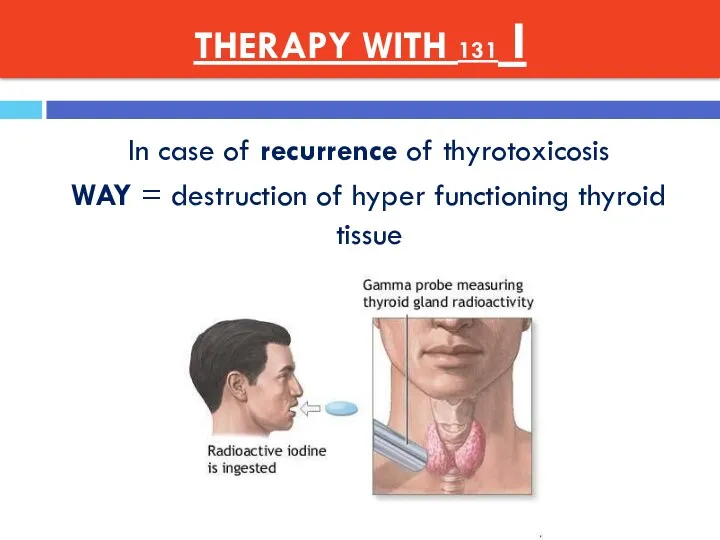
- 45. THERAPY WITH 131 I In case of recurrence of thyrotoxicosis WAY = destruction of hyper functioning
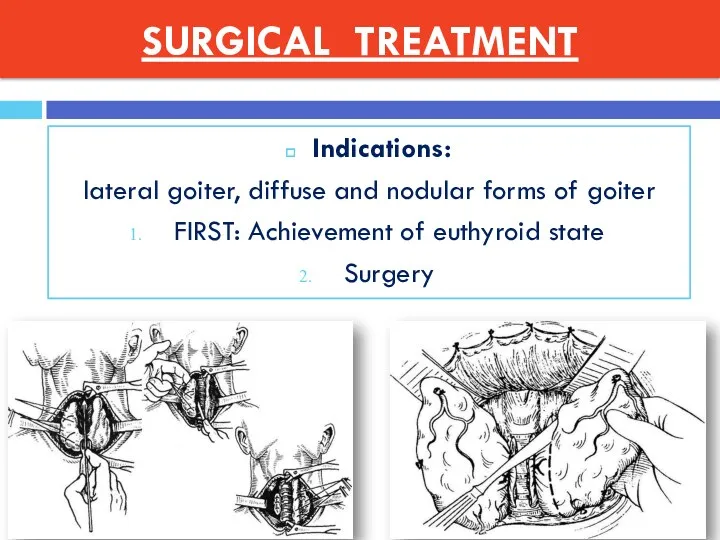
- 46. SURGICAL TREATMENT Indications: lateral goiter, diffuse and nodular forms of goiter FIRST: Achievement of euthyroid state
- 50. Скачать презентацию





 Отравления ядами растительного происхождения
Отравления ядами растительного происхождения Неврозы. Классификация. Этиология. Профилактика
Неврозы. Классификация. Этиология. Профилактика Мегаколон и доликолон у детей. Болезнь Гиршпрунга у детей
Мегаколон и доликолон у детей. Болезнь Гиршпрунга у детей Тағамдық токсикоинфекциялар
Тағамдық токсикоинфекциялар Психотропные средства с возбуждающим действием на ЦНС
Психотропные средства с возбуждающим действием на ЦНС Дәрігелік құпия және дәрігерлік қателік
Дәрігелік құпия және дәрігерлік қателік Возбудители туберкулеза
Возбудители туберкулеза Тактика диагностики и лечения инциденталом надпочесников
Тактика диагностики и лечения инциденталом надпочесников История развития патофизиологии
История развития патофизиологии Артрит и артроз. Причины, симптомы, осложнения, лечение
Артрит и артроз. Причины, симптомы, осложнения, лечение Адам эмбриологиясы. Эмбриондық дамудың ұрықтық кезеңі. Ұрықтан тыс мүшелер
Адам эмбриологиясы. Эмбриондық дамудың ұрықтық кезеңі. Ұрықтан тыс мүшелер Врач общей практики в США
Врач общей практики в США Послеродовые кровотечения
Послеродовые кровотечения Профилактика передачи ВИЧ от матери к ребенку
Профилактика передачи ВИЧ от матери к ребенку Лечение деформирующего артроза
Лечение деформирующего артроза Методи дослідження в клінічній генетиці
Методи дослідження в клінічній генетиці Травмы и инородные тела гортани
Травмы и инородные тела гортани Ауыз қуысы зақымдануының жалпы этиологиясы және патогенезі
Ауыз қуысы зақымдануының жалпы этиологиясы және патогенезі Аденоидит. Патологическое разрастание (гипертрофия) аденоидов
Аденоидит. Патологическое разрастание (гипертрофия) аденоидов Соматометрия (антропометрия)
Соматометрия (антропометрия) Починка, коррекция и реставрация полных съемных протезов
Починка, коррекция и реставрация полных съемных протезов Бүйрек туберкулезі
Бүйрек туберкулезі Рак яичников
Рак яичников Гисто- и органогенез кожи. Строение кожи. Производные кожи – железы, волосы, ногти. Кожа – орган иммунной системы. Регенерация
Гисто- и органогенез кожи. Строение кожи. Производные кожи – железы, волосы, ногти. Кожа – орган иммунной системы. Регенерация Психические и поведенческие расстройства вследствие употребления психоактивных веществ.Алоголизм. Стадии алкоголизма
Психические и поведенческие расстройства вследствие употребления психоактивных веществ.Алоголизм. Стадии алкоголизма Тынысалу деп
Тынысалу деп Методика исследования органов пищеварения у детей
Методика исследования органов пищеварения у детей Психосоматические расстройства
Психосоматические расстройства