Содержание
- 2. A 12-year-old girl CC: Blurred vision 1 day History taking
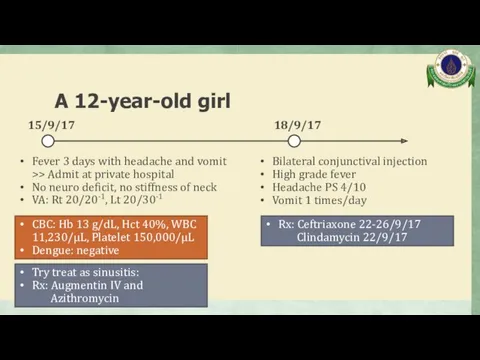
- 3. A 12-year-old girl Fever 3 days with headache and vomit >> Admit at private hospital No
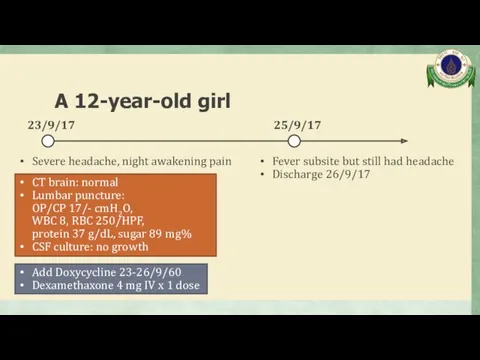
- 4. A 12-year-old girl Severe headache, night awakening pain 23/9/17 25/9/17 Fever subsite but still had headache
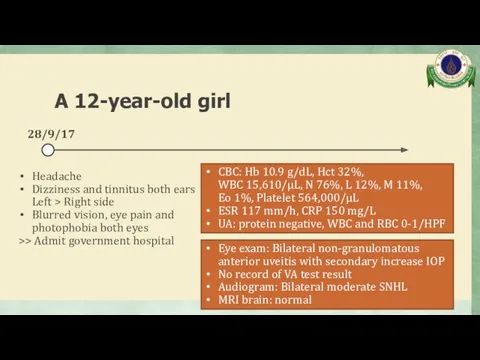
- 5. A 12-year-old girl Headache Dizziness and tinnitus both ears Left > Right side Blurred vision, eye
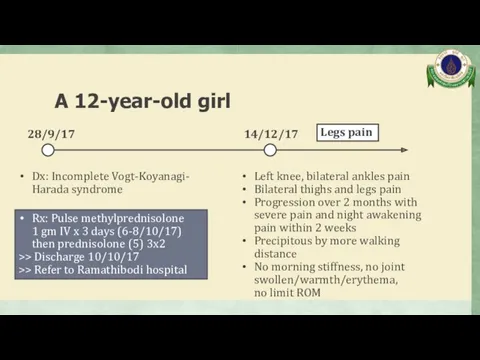
- 6. A 12-year-old girl Dx: Incomplete Vogt-Koyanagi- Harada syndrome 28/9/17 Rx: Pulse methylprednisolone 1 gm IV x
- 7. Past history No history of eye trauma No history of anorexia/weight loss No history of photosensitivity
- 8. A 12-year-old girl Physical examination
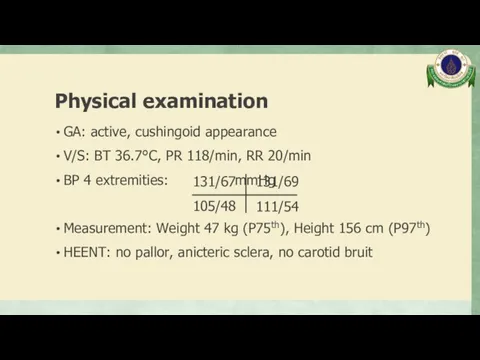
- 9. Physical examination GA: active, cushingoid appearance V/S: BT 36.7°C, PR 118/min, RR 20/min BP 4 extremities:
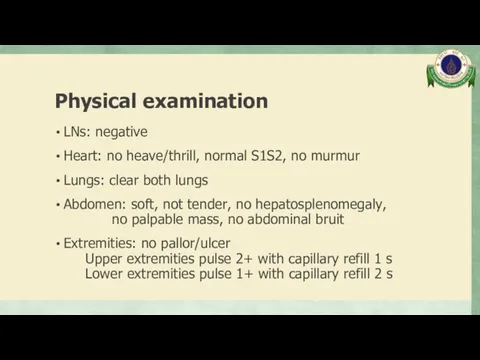
- 10. Physical examination LNs: negative Heart: no heave/thrill, normal S1S2, no murmur Lungs: clear both lungs Abdomen:
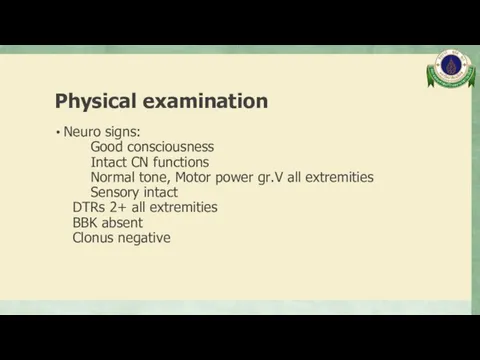
- 11. Physical examination Neuro signs: Good consciousness Intact CN functions Normal tone, Motor power gr.V all extremities
- 12. A 12-year-old girl Problem list
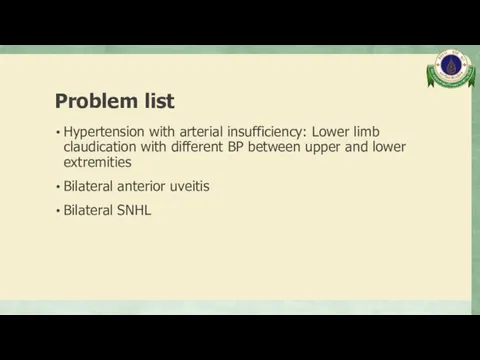
- 13. Problem list Hypertension with arterial insufficiency: Lower limb claudication with different BP between upper and lower
- 14. A 12-year-old girl Differential diagnosis
- 15. Differential diagnosis Takayasu arteritis Cogan’s syndrome Vogt-Koyanagi-Harada syndrome
- 16. A 12-year-old girl Investigation
- 17. Investigation
- 18. Complete blood count Hb 13.6 g/dL, Hct 43.3% WBC 13,300/µL, N 75%, L 15%, M 9%,
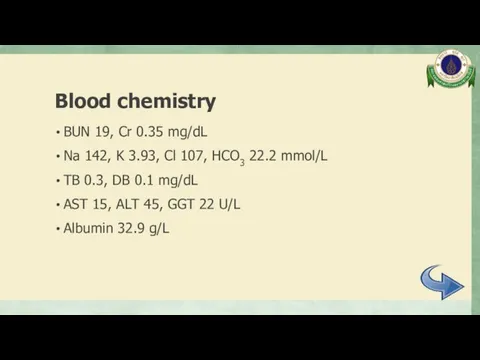
- 19. Blood chemistry BUN 19, Cr 0.35 mg/dL Na 142, K 3.93, Cl 107, HCO3 22.2 mmol/L
- 20. Inflammatory markers ESR 8 mm/hr CRP
- 21. Urinalysis Sp. gr. 1.019, pH 5, protein negative, blood negative WBC 0-1, RBC 0-1 /HPF
- 22. Immunology ANA negative
- 23. CTA whole aorta Diffuse mild to moderate irregular luminal narrowing involving celiac trunk, SMA, mid part
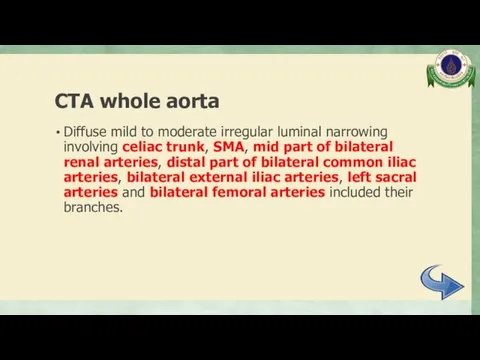
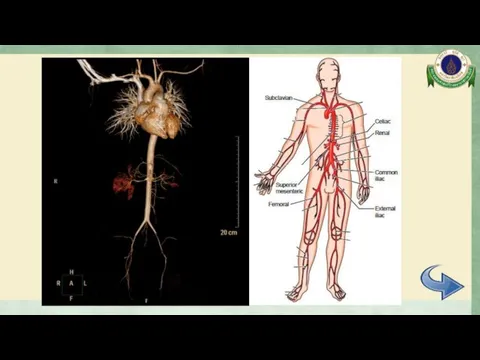
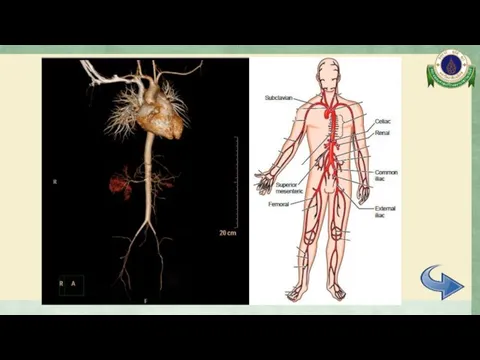
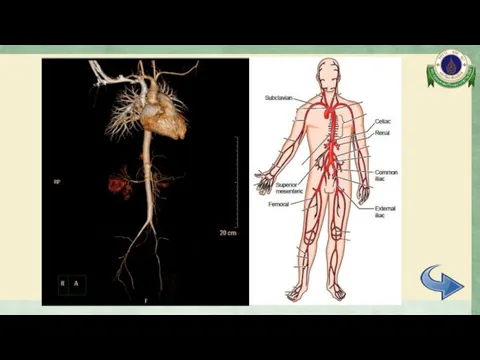
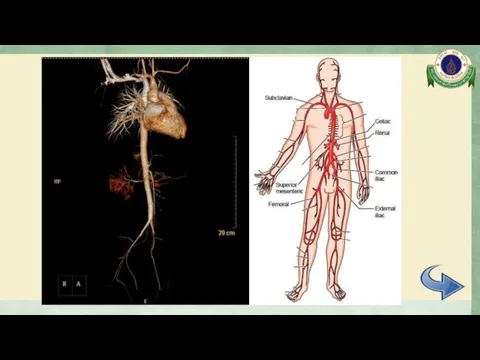
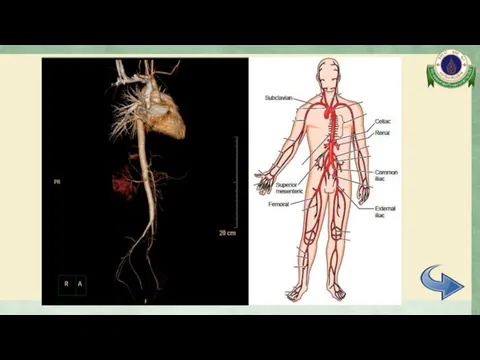
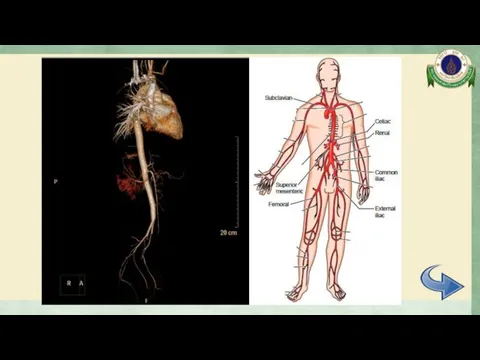
- 24. CTA whole aorta Surrounding soft tissue thickening with delayed mural enhancement at bilateral external iliac arteries
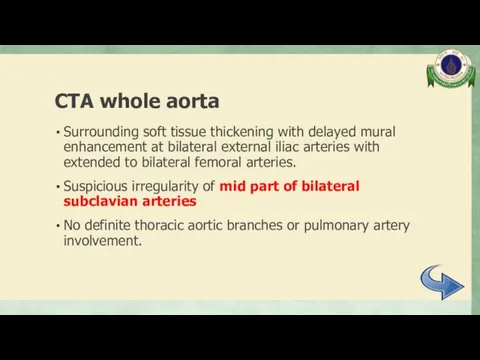
- 25. CTA whole aorta
- 26. CTA whole aorta
- 27. CTA whole aorta
- 28. CTA whole aorta
- 29. CTA whole aorta
- 30. CTA whole aorta
- 31. CTA whole aorta
- 32. Electrocardiogram Normal sinus rhythm, rate 110/min, normal axis No chamber enlargement
- 33. Echocardiogram Normal cardiac function Trivial to mild MR and AR No coarctation of aorta or aortic
- 34. Eye examination VA: Rt 20/80, 20/50 with PH Lt 20/50, 20/40 with PH IOP Rt 15,
- 35. Audiogram Moderately severe sensorineural hearing loss both ears
- 36. A 12-year-old girl Differential diagnosis
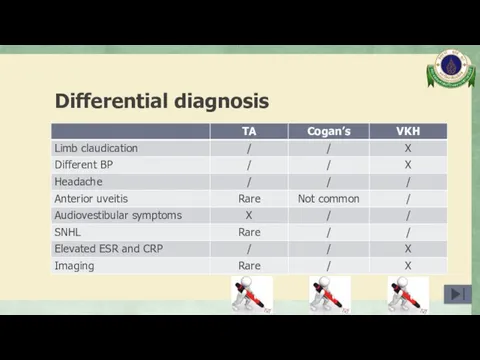
- 37. Differential diagnosis Takayasu arteritis Cogan’s syndrome Vogt-Koyanagi-Harada syndrome
- 38. Differential diagnosis
- 39. Takayasu arteritis (TA) Arteritis, often granulomatous Predominantly affecting the aorta and/or its major branches Arthritis Rheum
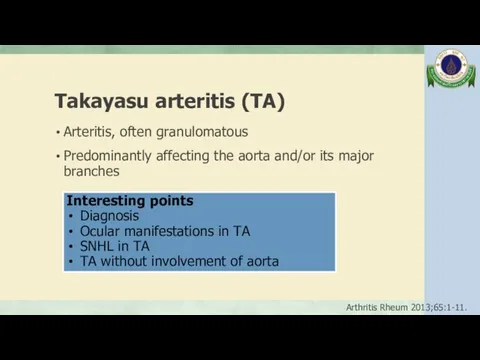
- 40. EULAR/PRINTO/PRES classification criteria of childhood TA Angiographic abnormalities plus 1 of 5 following criteria (sens 100%,
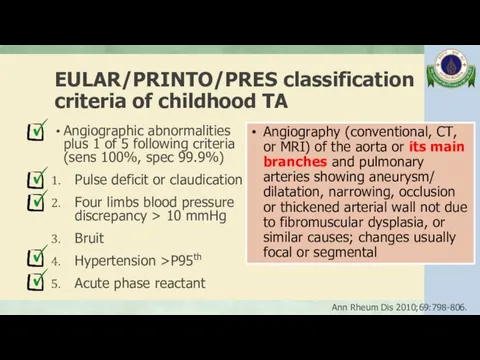
- 41. Ocular manifestations in TA Prevalence is varied from 8.1% - 68% Retina 2011;31:1170-8.
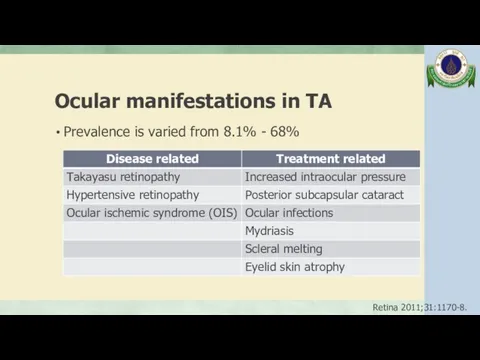
- 42. Ocular manifestations in TA Retrospective cohort 78 TA patients, Korea Cross-sectional study 61 TA patients, India
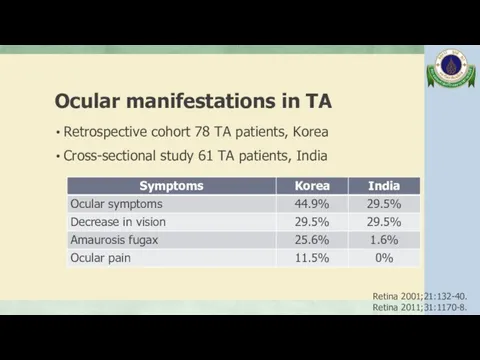
- 43. Ocular manifestations in TA Retrospective cohort 78 TA patients, Korea Cross-sectional study 61 TA patients, India
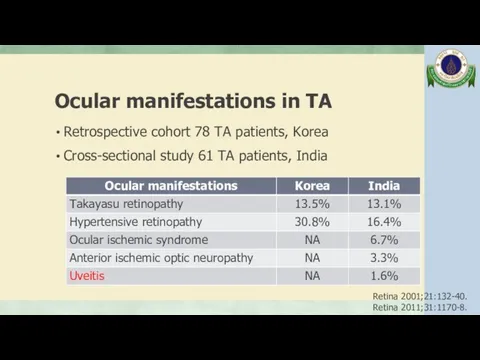
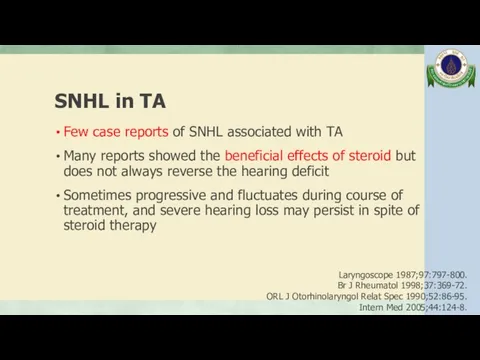
- 44. SNHL in TA Few case reports of SNHL associated with TA Many reports showed the beneficial
- 45. SNHL in TA The cause of the hearing impairment associated with TA is unknown, may be
- 46. SNHL in TA The mechanisms of the hearing loss in TA are reversible circulatory disturbances due
- 47. TA without involvement of aorta Retrospective review 85 CT angiography in TA patient, 1994-2003, Korea 95%
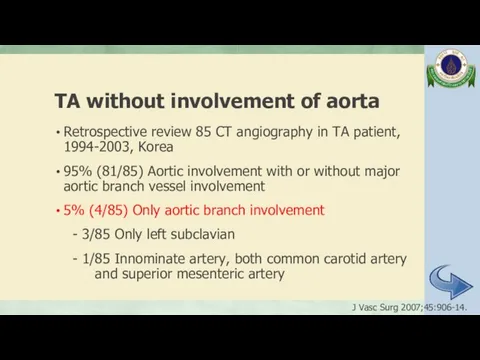
- 48. Cogan’s syndrome (CS) Characterized by ocular inflammatory lesions, including interstitial keratitis, uveitis, and episcleritis, and inner
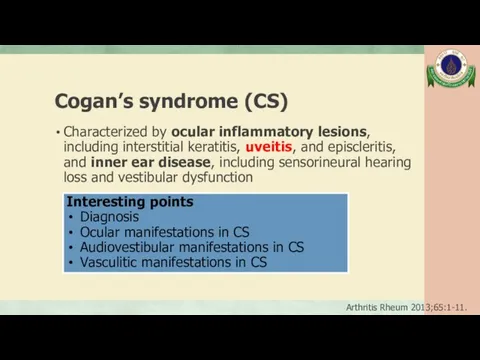
- 49. Typical CS Defined by following 3 conditions: (1) Ocular symptoms typically an isolated non-syphilitic interstitial keratitis
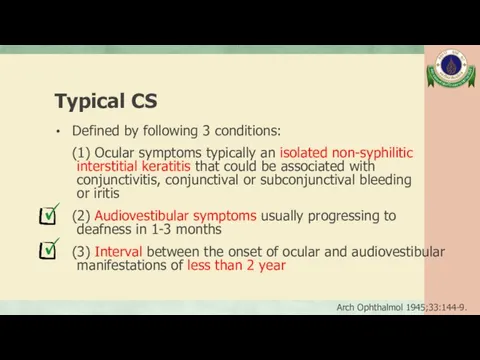
- 50. Atypical CS Any of following conditions: (1) Inflammatory ocular manifestations including episcleritis, scleritis, retinal artery occlusion,
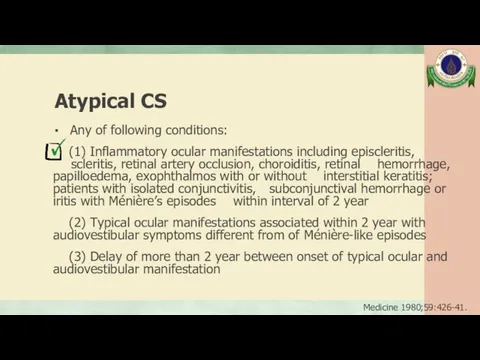
- 51. Ocular manifestations in CS 80% Interstitial keratitis, mostly bilateral involvement; inflamed small blood vessels invade the
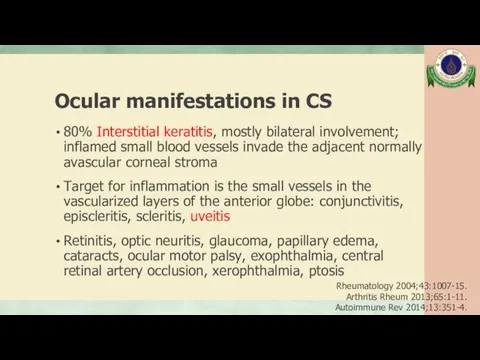
- 52. Audiovestibular manifestations in CS Sudden onset of hearing loss, vertigo, tinnitus, nausea, vomiting Often resolving after
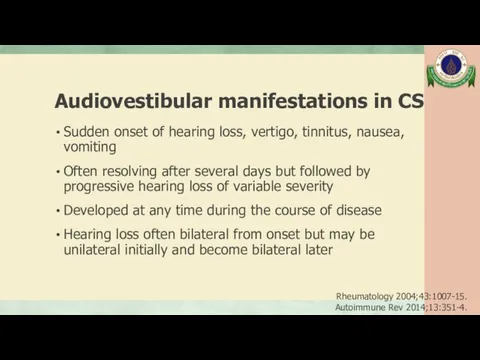
- 53. Vasculitic manifestations in CS May include arteritis (affecting small, medium, or large arteries), aortitis, aortic aneurysms,
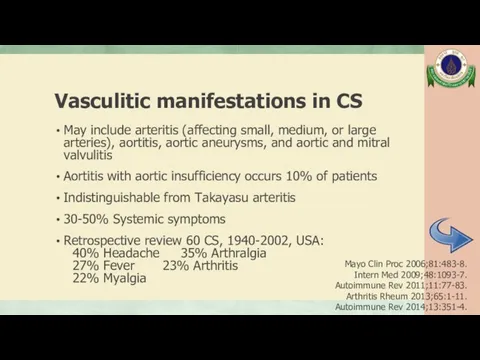
- 54. Vogt-Koyanagi-Harada syndrome (VKH) Systemic autoimmune disease; main target is melanin-containing-cells present in the eye, meninges, ear
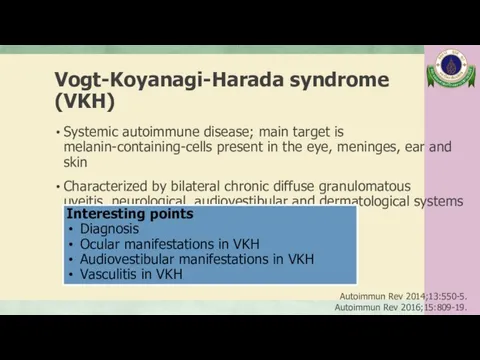
- 55. Clinical course of VKH Prodromal phase: Few days prior to ocular symptoms, predominately neurological and auditory
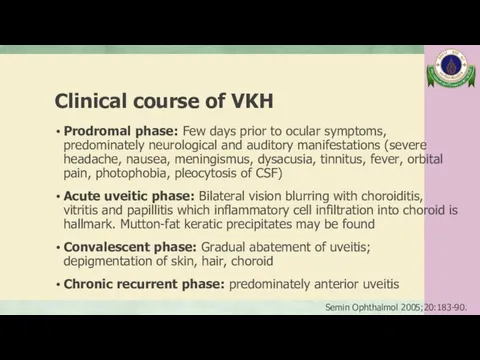
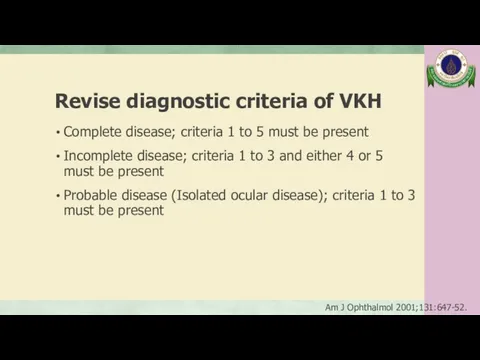
- 56. Revise diagnostic criteria of VKH Complete disease; criteria 1 to 5 must be present Incomplete disease;
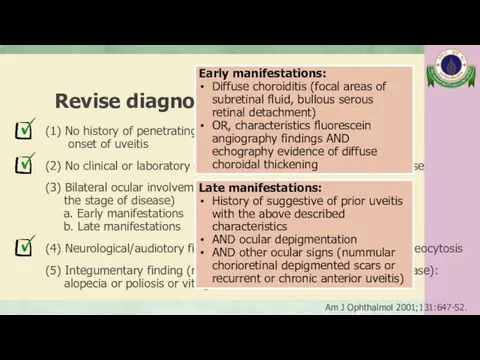
- 57. Revise diagnostic criteria of VKH (1) No history of penetrating ocular trauma or surgery preceding onset
- 58. Ocular manifestations in VKH The posterior manifestation is the hallmark, demonstrating vitreous cells with bilateral exudative
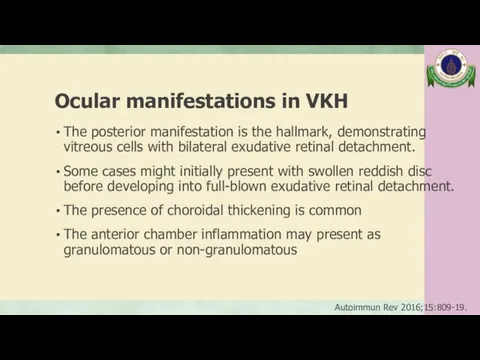
- 59. Ocular manifestations in VKH Signs of depigmentation: - Sunset glow: changes of fundus represent choroidal depigmentation
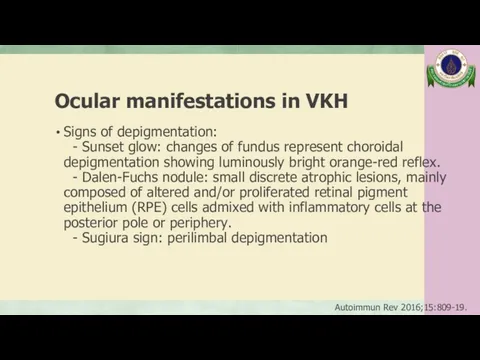
- 60. Audiovestibular manifestations in VKH SNHL (27-50%), tinnitus (34-43%) and vertigo/dizziness (4-25%) Typically bilateral and mild HL,
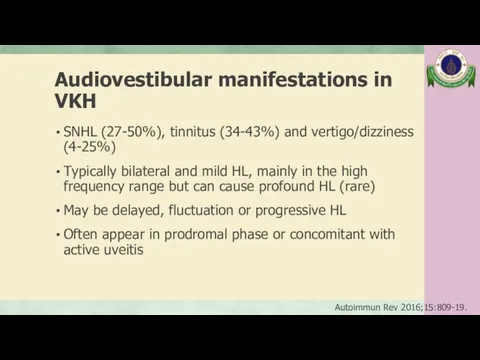
- 61. Vasculitis in VKH Case report of a 44-year-old female in Japan, developed VKH after diagnosed aortitis
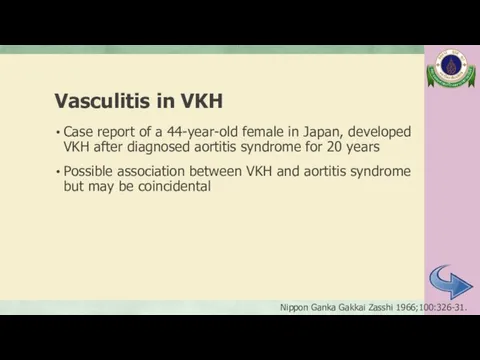
- 62. A 12-year-old girl Management
- 63. Management J Cliln Pathol 2002;55:481-6. Autoimmun Rev 2016;15:809-19. J Multidiscip Healthc 2017;11:1-11.
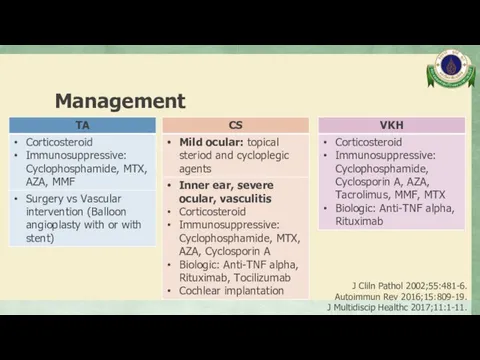
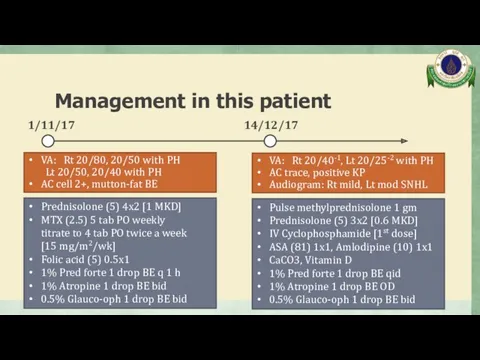
- 64. Management in this patient 1/11/17 14/12/17 Prednisolone (5) 4x2 [1 MKD] MTX (2.5) 5 tab PO
- 65. Management in this patient 11/1/18 IV Cyclophosphamide [2nd dose] Prednisolone (5) 2x2 [0.4 MKD] ASA (81)
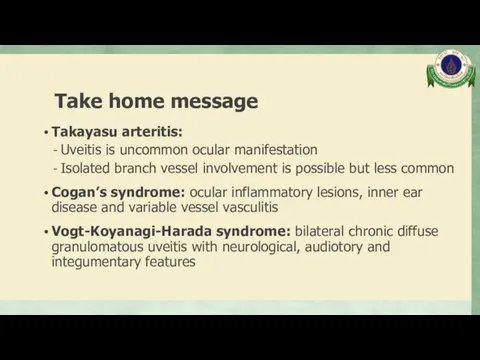
- 66. Take home message Takayasu arteritis: Uveitis is uncommon ocular manifestation Isolated branch vessel involvement is possible
- 67. Thank you
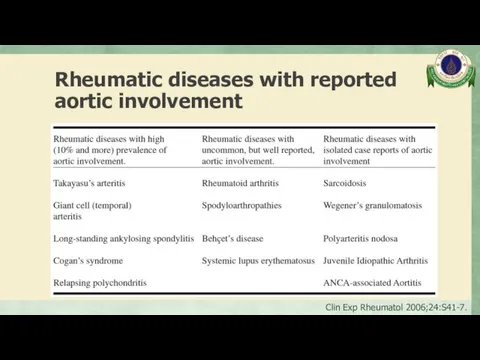
- 68. Rheumatic diseases with reported aortic involvement Clin Exp Rheumatol 2006;24:S41-7.
- 69. Vasculitis Inflammation of blood vessel walls The inflammatory infiltrate may be one that is predominantly neutrophilic,
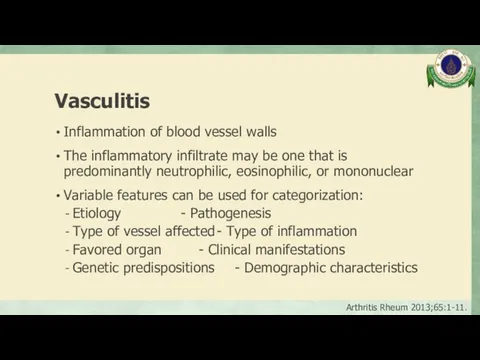
- 70. Vasculitis Arthritis Rheum 2013;65:1-11.
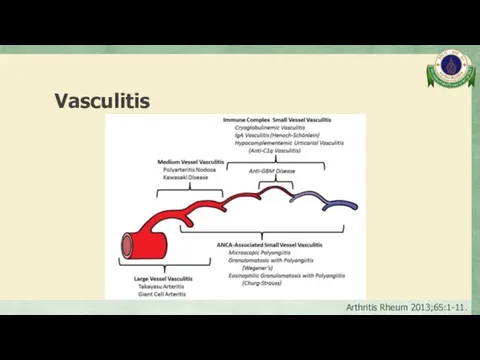
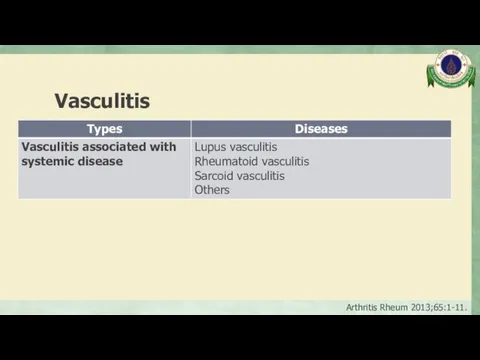
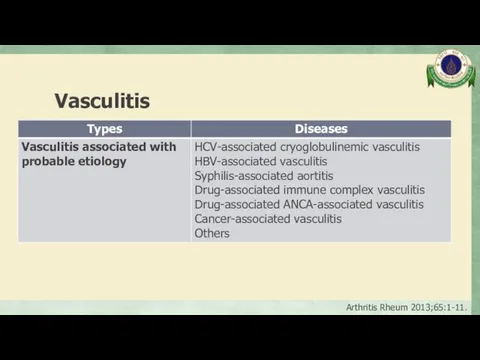
- 71. Vasculitis Arthritis Rheum 2013;65:1-11.
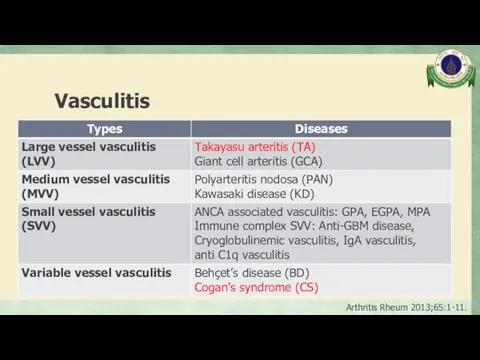
- 72. Vasculitis Arthritis Rheum 2013;65:1-11.
- 73. Vasculitis Arthritis Rheum 2013;65:1-11.
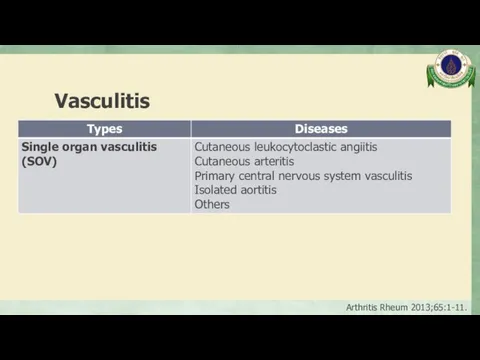
- 74. Vasculitis Arthritis Rheum 2013;65:1-11.
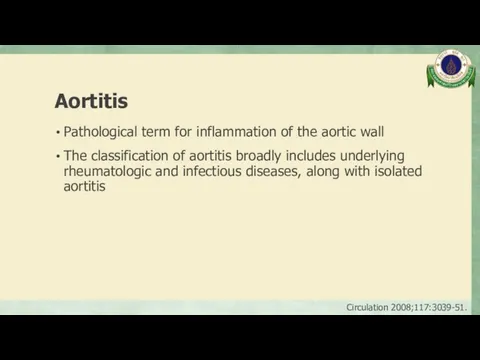
- 75. Aortitis Pathological term for inflammation of the aortic wall The classification of aortitis broadly includes underlying
- 76. Clinical presentation Asymptomatic General syndrome: fever, malaise, weight loss, high ESR Pain (chest, back, abdominal): acute
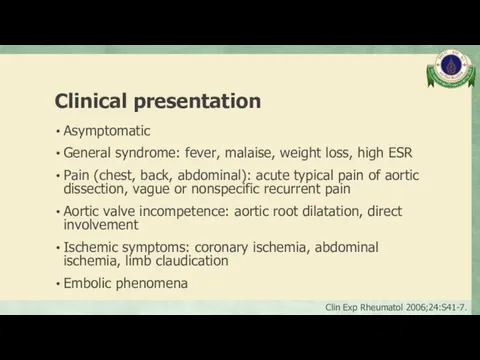
- 77. Causes of aortitis Inflammatory: Large vessel vasculitis: TAK, GCA Rheumatoid arthritis Systemic lupus erythematosus HLA-B27 associated
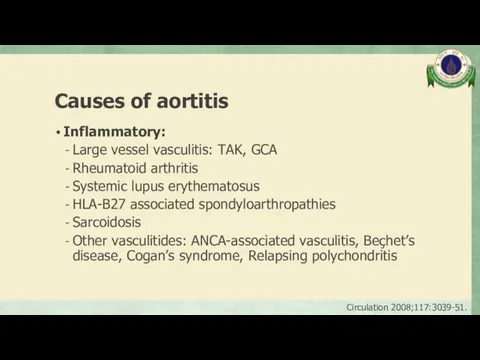
- 78. Causes of aortitis Isolated aortitis: Isolated idiopathic (thoracic aortitis) Chronic periaortitis: Idiopathic retroperitoneal fibrosis, Inflammatory abdominal
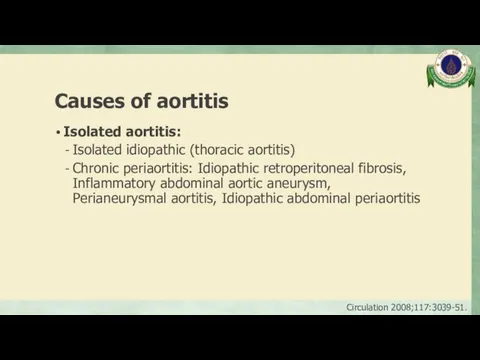
- 79. Causes of aortitis Infectious: Bacteria: Salmonella spp., Staphylococcus spp., Streptococcus pneumoniae, other Syphilis Mycobacterium Other Circulation
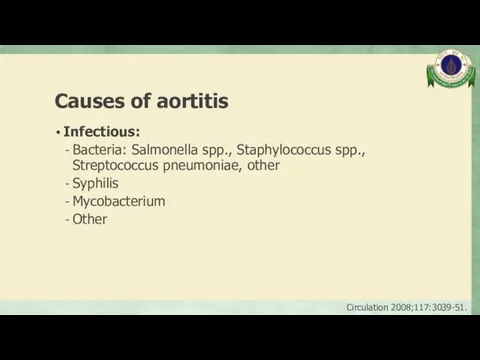
- 80. Laboratory testing Markers of inflammation: ESR, CRP Complete blood count Kidney and liver function Additional laboratory
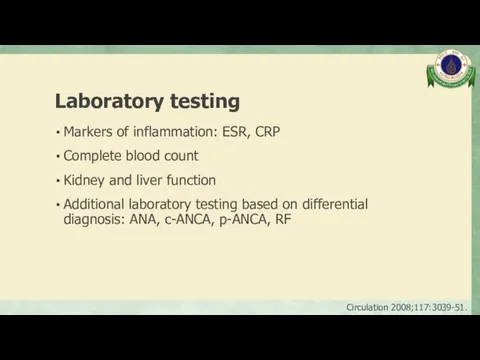
- 81. Imaging modalities Korean J Radiol 2017;18:786-98.
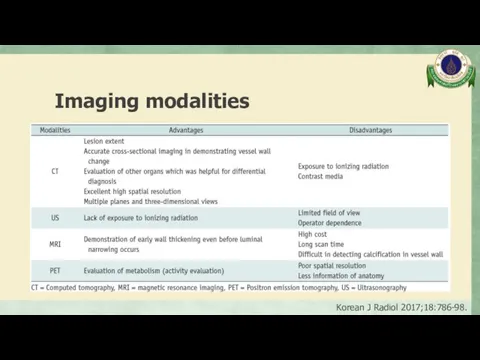
- 82. ACR classification criteria of TA ≥ 3 of 6 criteria (sens 90.5%, spec 97.8%) Age at
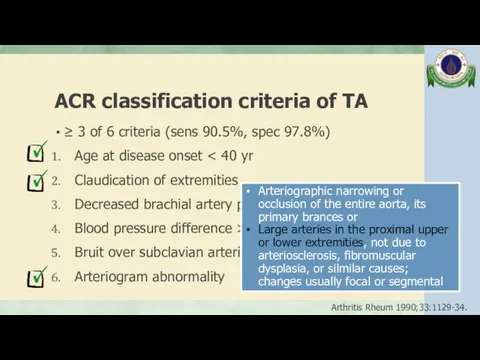
- 83. Takayasu arteritis (TA) Incidence 0.4-1 case/1,000,000/year Onset usually occurs before the age of 50 years, which
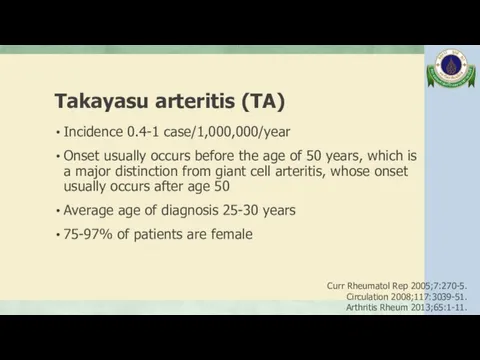
- 84. Angiographic classification of TA from the Takayasu conference 1994 Int J Cardiol 2012;159:14-20.
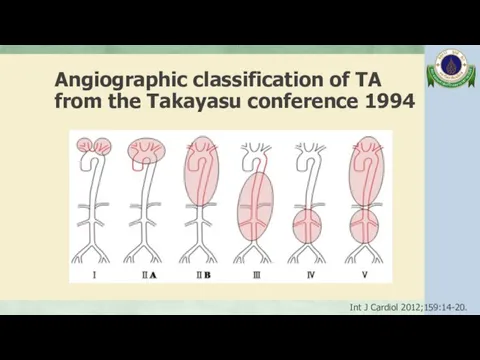
- 86. Скачать презентацию


![Management in this patient 11/1/18 IV Cyclophosphamide [2nd dose] Prednisolone](/_ipx/f_webp&q_80&fit_contain&s_1440x1080/imagesDir/jpg/423837/slide-64.jpg)
 Немедикаментозное лечение и профилактика кардиоваскулярных заболеваний
Немедикаментозное лечение и профилактика кардиоваскулярных заболеваний Медико-генетикалық кеңестің нәрестенің туа біткен ақаулықтарын алдын-алудағы рөлі және диагностикасы
Медико-генетикалық кеңестің нәрестенің туа біткен ақаулықтарын алдын-алудағы рөлі және диагностикасы Респираторные формы аллергии у детей
Респираторные формы аллергии у детей Медицинская арахноэнтомология
Медицинская арахноэнтомология Лечебно-охранительный режим ЛПУ. Безопасная больничная среда
Лечебно-охранительный режим ЛПУ. Безопасная больничная среда Психологические аспекты тандема врач-ассистент-пациент
Психологические аспекты тандема врач-ассистент-пациент Желчегонные средства
Желчегонные средства Консультирование больных с метаболическим синдромом
Консультирование больных с метаболическим синдромом Дүниежүзілік денсаулық сақтау ұйымы (ДДҰ) Қазақстанда
Дүниежүзілік денсаулық сақтау ұйымы (ДДҰ) Қазақстанда Факторы здоровья
Факторы здоровья Заполнение данных о работе скорой, в том числе скорой специализированной, медицинской помощи
Заполнение данных о работе скорой, в том числе скорой специализированной, медицинской помощи История нейрохирургии
История нейрохирургии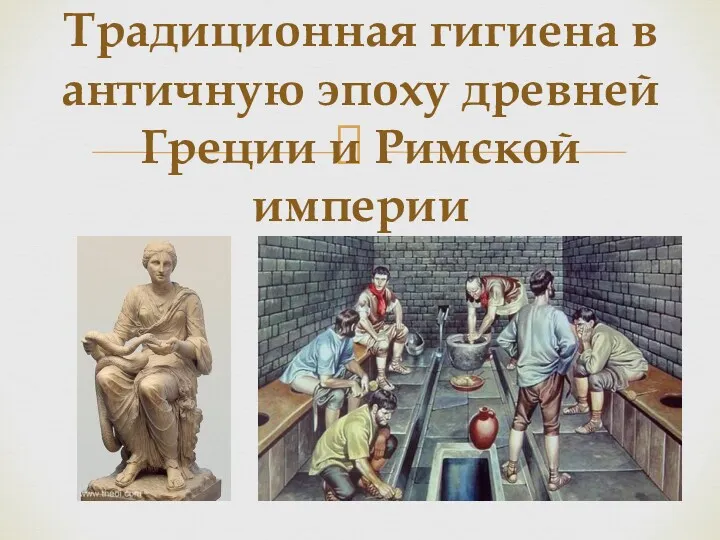 Традиционная гигиена в античную эпоху древней Греции и Римской империи
Традиционная гигиена в античную эпоху древней Греции и Римской империи Лечебное воздействие звука на человека. Человек - отражение вселенной
Лечебное воздействие звука на человека. Человек - отражение вселенной Болезнь Виллебранда
Болезнь Виллебранда Переливание крови
Переливание крови Нейропластичность и нейродегенерация
Нейропластичность и нейродегенерация Искусственная вентиляция легких
Искусственная вентиляция легких Строение и работа мышц
Строение и работа мышц Дивертикул толстой кишки
Дивертикул толстой кишки Закрытая травма живота у детей
Закрытая травма живота у детей Заикание у детей и взрослых
Заикание у детей и взрослых Медико-этические и социально-правовые аспекты современной трансплантологии
Медико-этические и социально-правовые аспекты современной трансплантологии Стационардағы медбикенің қол жуу маңыздылығы
Стационардағы медбикенің қол жуу маңыздылығы Профилактика туберкулеза. Диспансерное наблюдение, группы учета. Вакцинация БЦЖ и ее осложнения
Профилактика туберкулеза. Диспансерное наблюдение, группы учета. Вакцинация БЦЖ и ее осложнения Первая помощь при отравлениях
Первая помощь при отравлениях ECA solutions for poultry farming
ECA solutions for poultry farming Патология многоплодной беременности
Патология многоплодной беременности