Содержание
- 2. Laryngeal edema Laryngeal edema is a common cause of airway obstruction in the recently extubated intensive
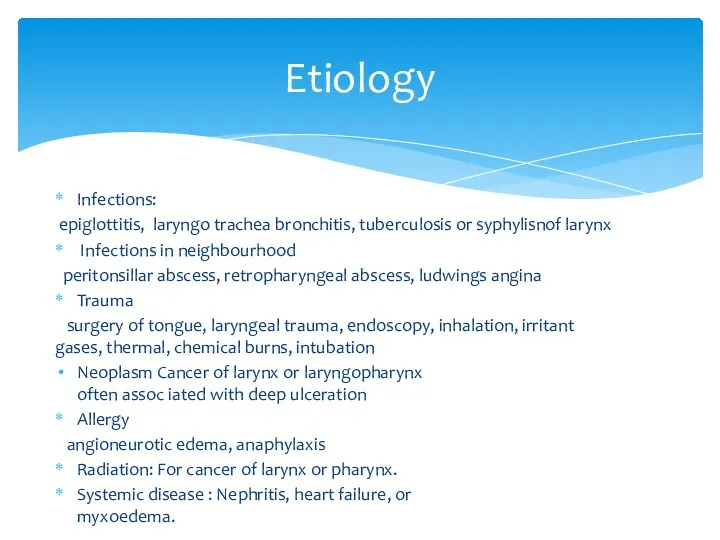
- 4. Infections: epiglottitis, laryngo trachea bronchitis, tuberculosis or syphylisnof larynx Infections in neighbourhood peritonsillar abscess, retropharyngeal abscess,
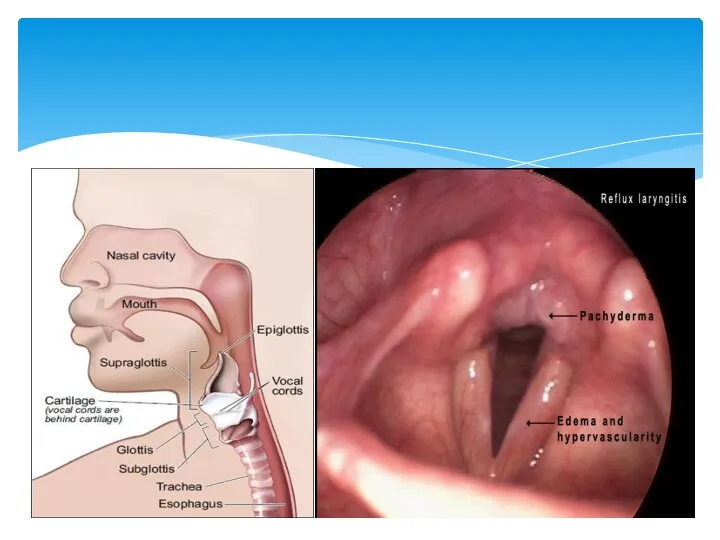
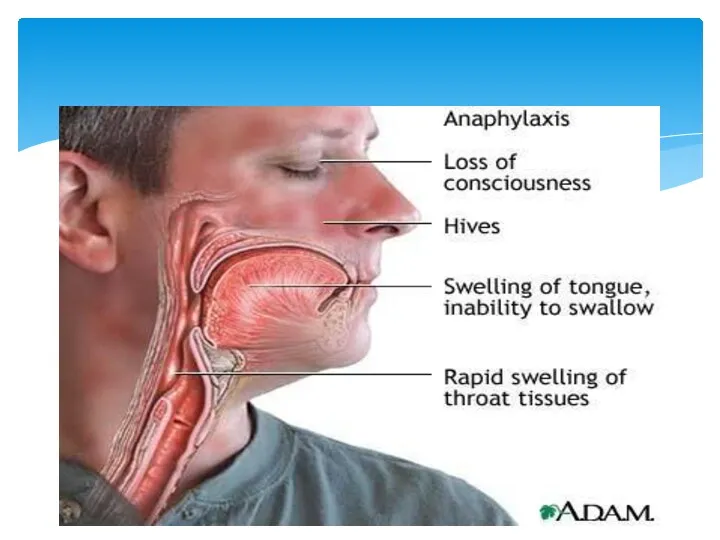
- 5. Airway obstruction Inspiratory stridor Diagnostics Indirect laryngoscopy shows oedema of supraglottic or subglottic region. Children may
- 7. Intubation/ tracheostomy Steroids (thermal, chemical) Adrenaline (1:1000) i/m 0,3-0,5ml repeated every 15 minutes Steroids are useful
- 8. Level 1: Steroid therapy decreases post-extubation stridor and need for reintubation in patients at increased risk
- 9. Laryngeal stenosis is a congenital or acquired narrowing of the airway that may affect the supraglottis,
- 10. ETIOLOGY 1.Trauma: External blunt penetrating Internal intubation post tracheostomy post surgery post radiotherapy thermal/ chemical burns
- 11. ETIOLOGY 2. Chronic inflammatory disease tuberculosis/ leprosy sacoidosis scleroma histoplasmosis diphtheria syphilis 3. Benign disorders intrinsic
- 12. ETIOLOGY 4. Malignant disorders Intrinsic SCC/ minor salivary gland tumor sarcoma/ lymphomas Extrinsic Thyroid malignancy 5.
- 13. PATHOPHYSIOLOGY Knowledge of pathophysiologyy is essential that it gives idea regarding time/ frequency of intervention, surgical
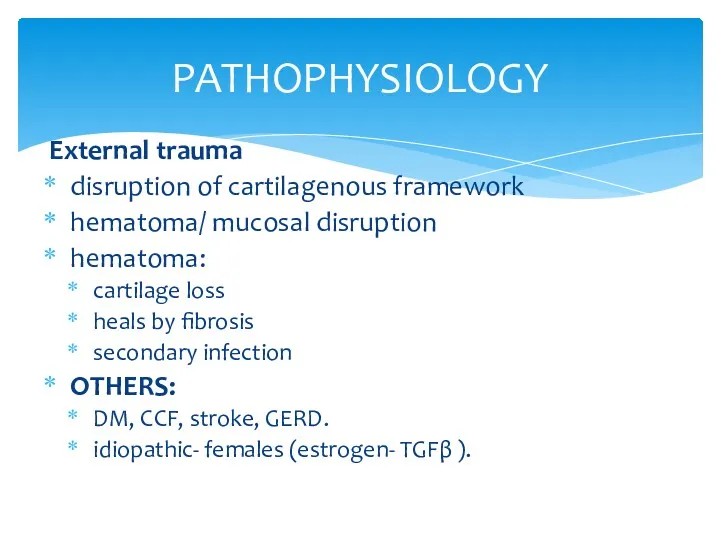
- 14. PATHOPHYSIOLOGY External trauma disruption of cartilagenous framework hematoma/ mucosal disruption hematoma: cartilage loss heals by fibrosis
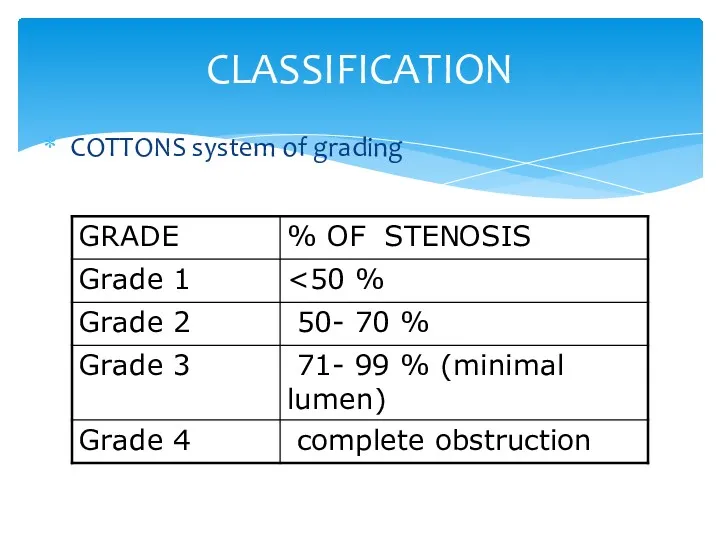
- 15. CLASSIFICATION COTTONS system of grading
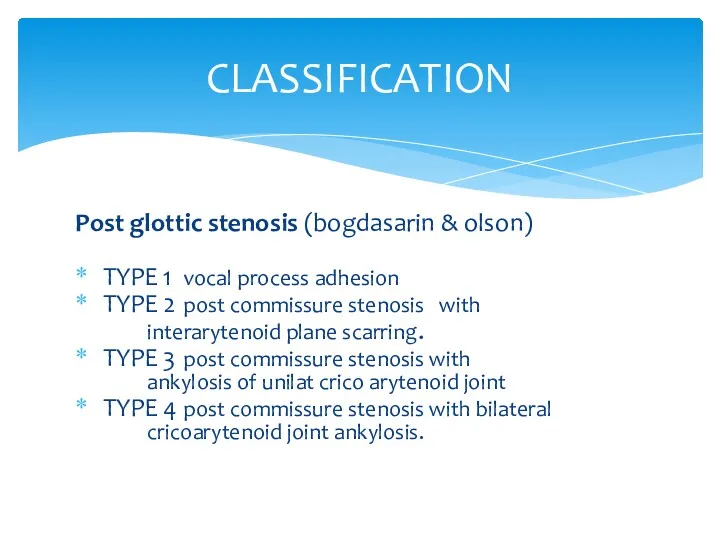
- 16. CLASSIFICATION Post glottic stenosis (bogdasarin & olson) TYPE 1 vocal process adhesion TYPE 2 post commissure
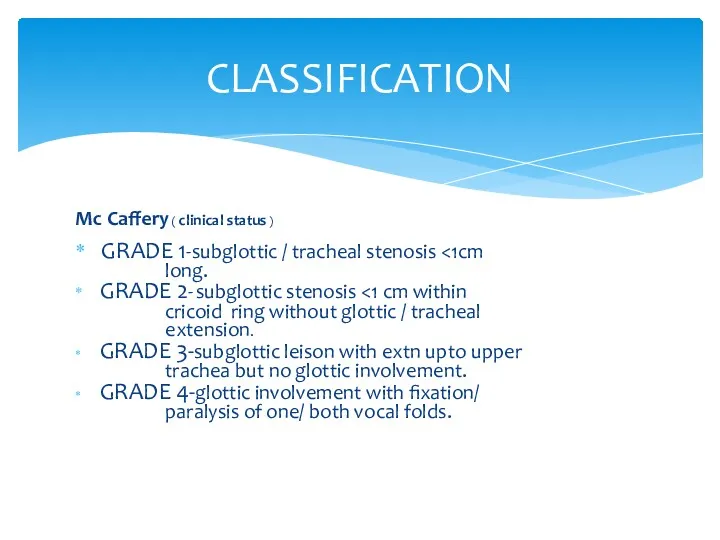
- 17. CLASSIFICATION Mc Caffery ( clinical status ) GRADE 1-subglottic / tracheal stenosis long. GRADE 2- subglottic
- 20. Stridor is a common presenting sign in laryngeal obstruction. Supraglottic or glottic obstruction generally presents as
- 21. The main symptoms of laryngeal stenosis relate to airway, voice, and feeding. Progressive respiratory difficulty is
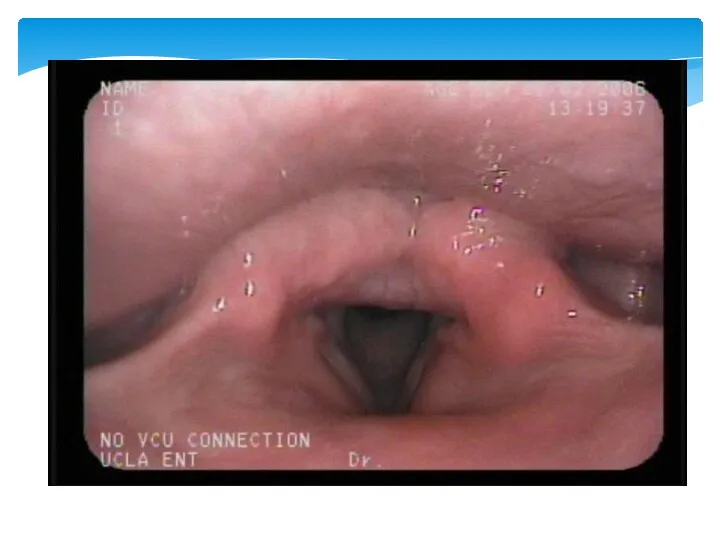
- 22. ASSESSMENT OF LTS History : trauma, mode of onset, effect on airway, voice etc… Indirect/ Direct
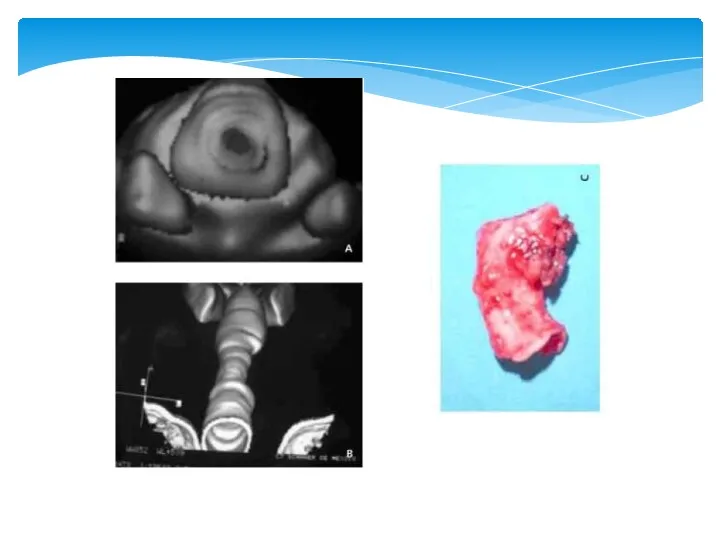
- 23. Radiologic evaluation Radiologic evaluation is performed after stabilization of the airway. Radiography helps assess the exact
- 24. New Technology Trans-nasal “Esophagoscope” Expanded diagnostic endoscopy Laryngoscopy Bronchoscopy Esophagoscopy 2.0 mm Working Channel Biopsies Injections
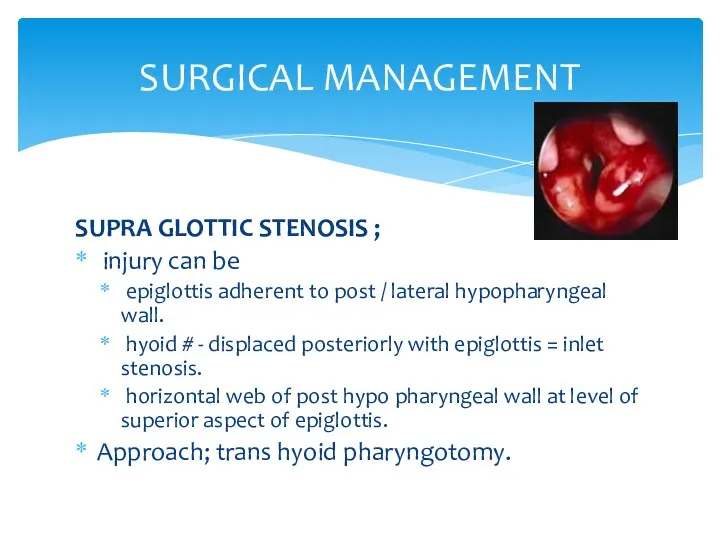
- 25. SURGICAL MANAGEMENT SUPRA GLOTTIC STENOSIS ; injury can be epiglottis adherent to post / lateral hypopharyngeal
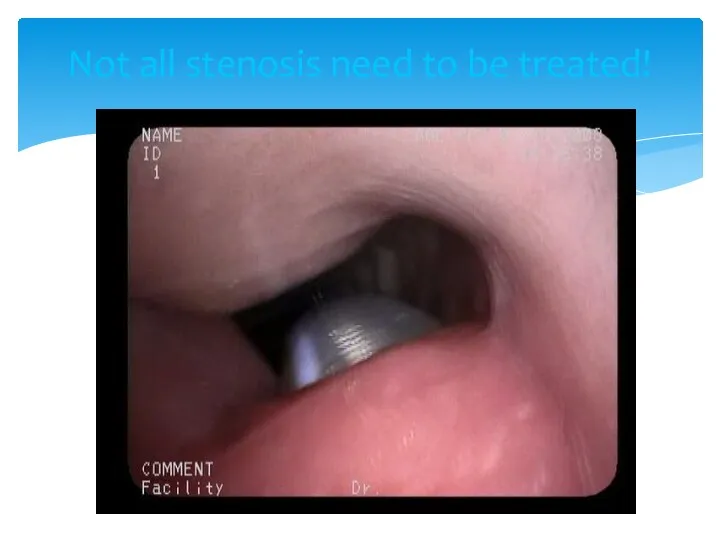
- 27. Not all stenosis need to be treated!
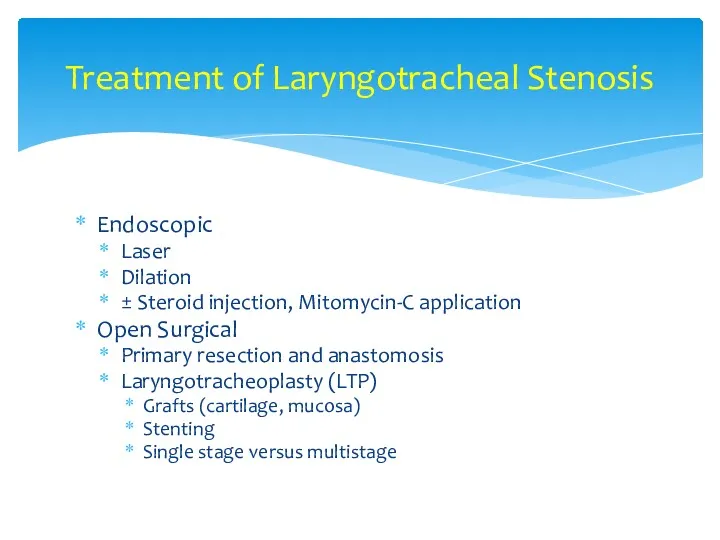
- 28. Treatment of Laryngotracheal Stenosis Endoscopic Laser Dilation ± Steroid injection, Mitomycin-C application Open Surgical Primary resection
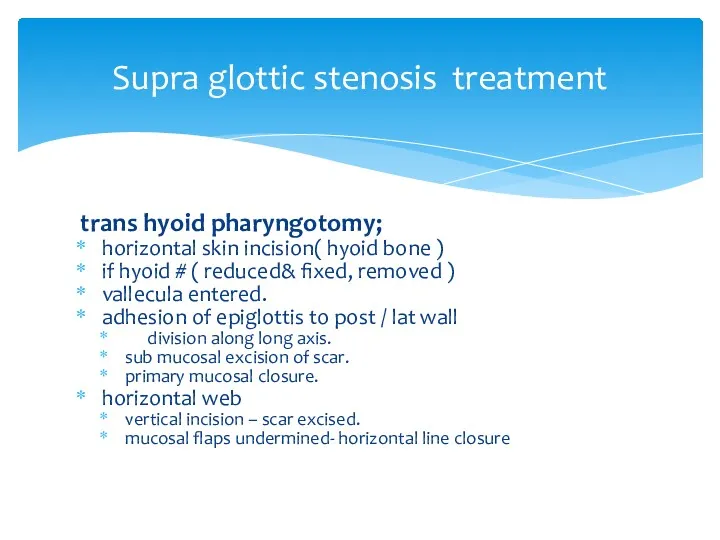
- 29. Supra glottic stenosis treatment trans hyoid pharyngotomy; horizontal skin incision( hyoid bone ) if hyoid #
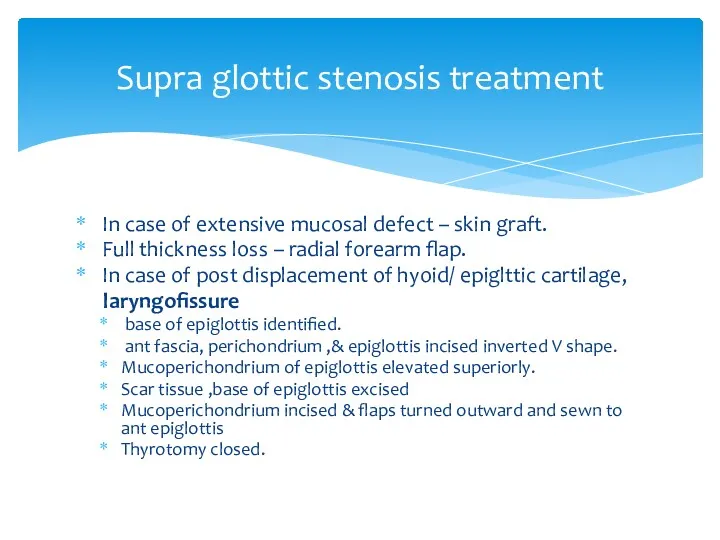
- 30. Supra glottic stenosis treatment In case of extensive mucosal defect – skin graft. Full thickness loss
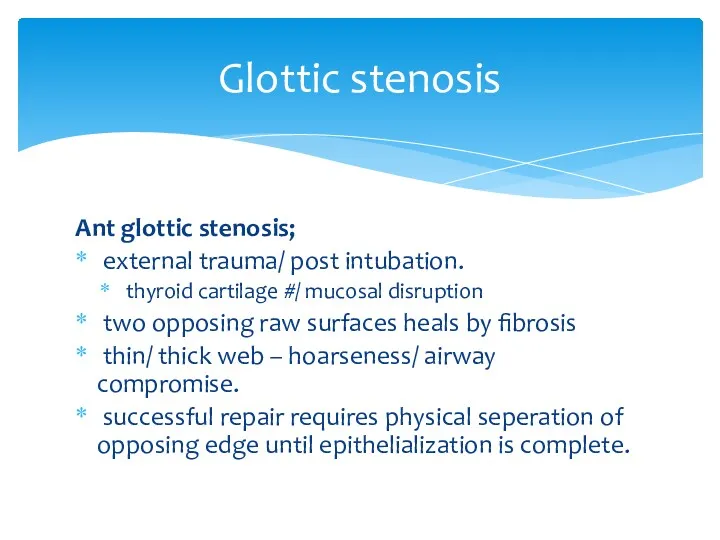
- 31. Glottic stenosis Ant glottic stenosis; external trauma/ post intubation. thyroid cartilage #/ mucosal disruption two opposing
- 32. Glottic stenosis Ant glottic web ; MLS / CO2 laser excision – keel insertion keel inserted
- 33. Glottic stenosis Ant glottic stenosis; external laryngo fissure indications; sub glottic extension >5 mm inlet stenosis.
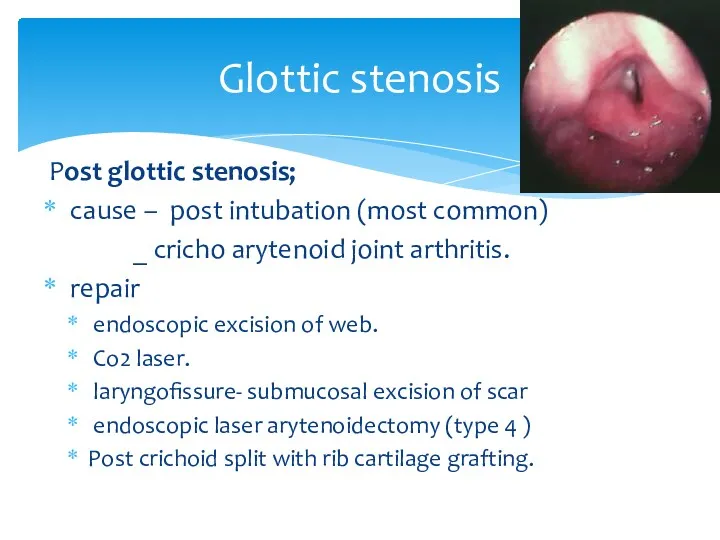
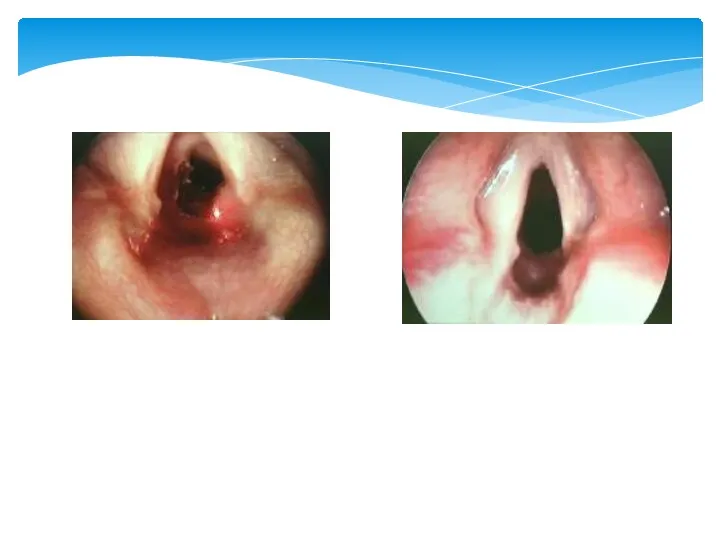
- 34. Glottic stenosis Post glottic stenosis; cause – post intubation (most common) _ cricho arytenoid joint arthritis.
- 36. Glottic stenosis complete glottic stenosis; laryngofissure ( main stay of treatment ) Stenosis divided at midline.
- 37. Glottic stenosis Alternative approach; Epiglottic flap indication severe glottic stenosis with 50% reduction in A-P diameter
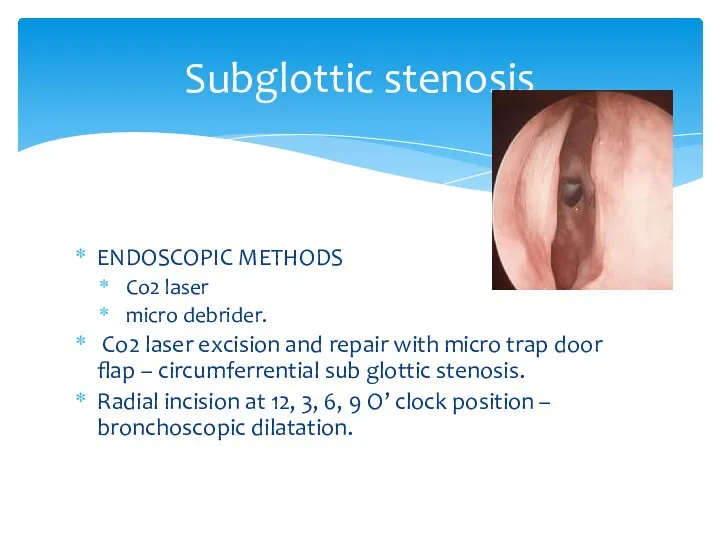
- 38. Subglottic stenosis ENDOSCOPIC METHODS Co2 laser micro debrider. Co2 laser excision and repair with micro trap
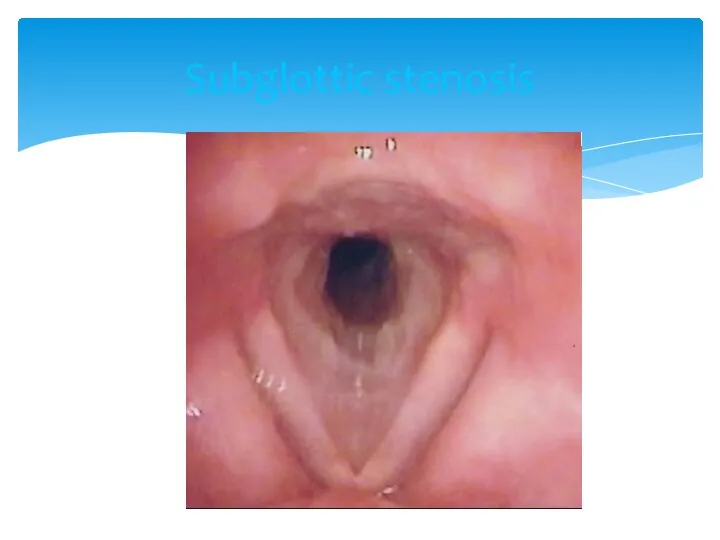
- 39. Subglottic stenosis
- 40. Subglottic stenosis EXTERNAL APPROACH; scar resection and SSG grafting. hyoid sterno hyoid muscle interposition graft .
- 42. LTS IN PEDIATRIC AGE GROUP ANATOMY; situated at a higher level funnel shape; midcricoid area 2-3
- 43. LTS IN PEDIATRIC AGE GROUP ETIOLOGY; congenital cong sub glottic stenosis vocal cord paralysis sub glottic
- 44. LTS IN PEDIATRIC AGE GROUP MANAGEMENT; endoscopic open techniques ant cricoid split laryngo tracheoplasty laryngo tracheal
- 45. LTS IN PEDIATRIC AGE GROUP POST OP MANAGEMENT; antibiotic cover anti reflux medication 6 wk endoscopy-
- 46. RESTENOSIS PREVENTION; steroids,mitomycin-c anti reflux/ antibiotics tissue engineering techniques fetal fibroblasts transposition( IL6,8) tissue engineered scaffolds
- 48. Скачать презентацию



 Периоды жизнедеятельности человека. Роль сестринского персонала в сохранении и укреплении здоровья
Периоды жизнедеятельности человека. Роль сестринского персонала в сохранении и укреплении здоровья Влияние ВИЧ на репродуктивную функцию подростка
Влияние ВИЧ на репродуктивную функцию подростка Заболевания передающиеся половым путем
Заболевания передающиеся половым путем Федеральный проект Демография
Федеральный проект Демография Хронический пульпит
Хронический пульпит Синдромы Дауна и Патау
Синдромы Дауна и Патау Деформирующий артроз коленного сустава. Лечение
Деформирующий артроз коленного сустава. Лечение Основы иммунологии. Иммунитет. Иммунная система человека
Основы иммунологии. Иммунитет. Иммунная система человека Дыхательная недостаточность
Дыхательная недостаточность Инфекция или инфекционный процесс
Инфекция или инфекционный процесс Пародонт аурулары. Анықтамасы, жіктелуі, этиологиясы, потогенезі. Пародонт ауруларымен науқастары комплексті тексеру
Пародонт аурулары. Анықтамасы, жіктелуі, этиологиясы, потогенезі. Пародонт ауруларымен науқастары комплексті тексеру Скелет верхней и нижней конечности
Скелет верхней и нижней конечности Организация медико-генетической службы
Организация медико-генетической службы Дом для мамы: я выбираю жизнь
Дом для мамы: я выбираю жизнь Нервно-психическое развитие ребёнка раннего возраста
Нервно-психическое развитие ребёнка раннего возраста Хронический панкреатит и внешнесекреторная недостаточность поджелудочной железы у детей
Хронический панкреатит и внешнесекреторная недостаточность поджелудочной железы у детей Фармацевтическая терминология. Основные понятия фармацевтической терминологии
Фармацевтическая терминология. Основные понятия фармацевтической терминологии Острая почечная и острая печеночная недостаточность
Острая почечная и острая печеночная недостаточность Хроническая обструктивная болезнь легких
Хроническая обструктивная болезнь легких Организация оказания медицинской помощи в амбулаторно - поликлинических учреждениях
Организация оказания медицинской помощи в амбулаторно - поликлинических учреждениях Атипичные нейролептики нового поколения (антипсихотики)
Атипичные нейролептики нового поколения (антипсихотики) Роль медицинской сестры в профилактике и лечении пролежней
Роль медицинской сестры в профилактике и лечении пролежней Прием пациента в стационар. Ведение сестринской документации
Прием пациента в стационар. Ведение сестринской документации Ес және назар аудару бұзылыстарының клиникалық мінездемесі.Сана- сезімнің бұзылыстары
Ес және назар аудару бұзылыстарының клиникалық мінездемесі.Сана- сезімнің бұзылыстары Медико-соціальна експертиза при захворюваннях органів системи кровообігу
Медико-соціальна експертиза при захворюваннях органів системи кровообігу Шина Вебера. Шина Порта
Шина Вебера. Шина Порта Профилактики стоматологических заболеваний у беременных женщин. Содержание стоматологического просвещения для беременных женщин
Профилактики стоматологических заболеваний у беременных женщин. Содержание стоматологического просвещения для беременных женщин Дамудың туа біткен ақауларының түрлері
Дамудың туа біткен ақауларының түрлері