Содержание
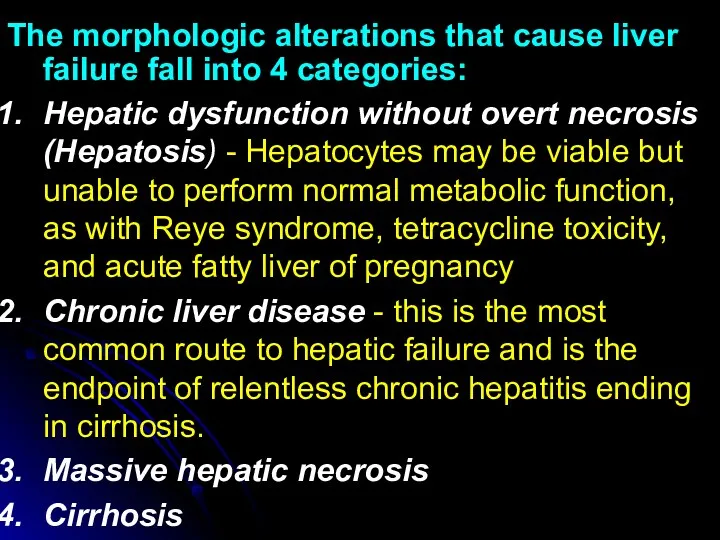
- 2. The morphologic alterations that cause liver failure fall into 4 categories: Hepatic dysfunction without overt necrosis
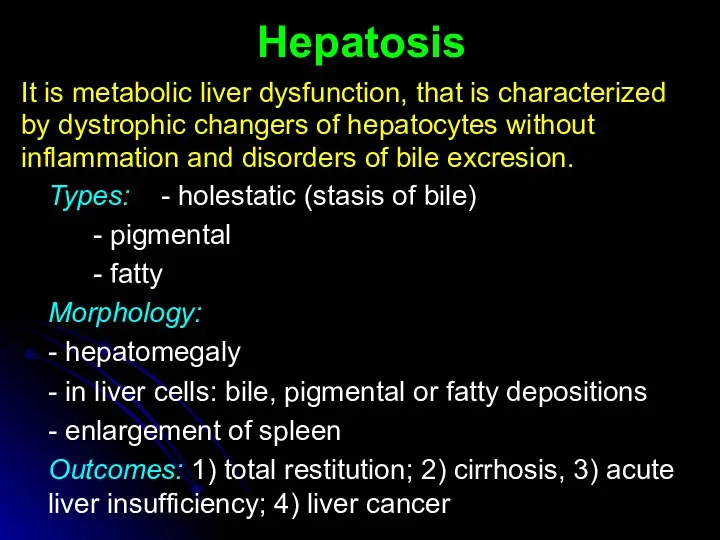
- 3. Hepatosis It is metabolic liver dysfunction, that is characterized by dystrophic changers of hepatocytes without inflammation
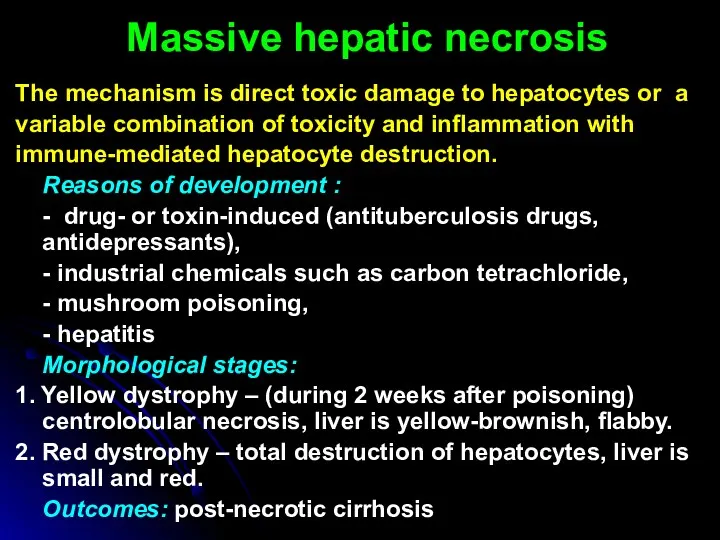
- 4. Massive hepatic necrosis The mechanism is direct toxic damage to hepatocytes or a variable combination of
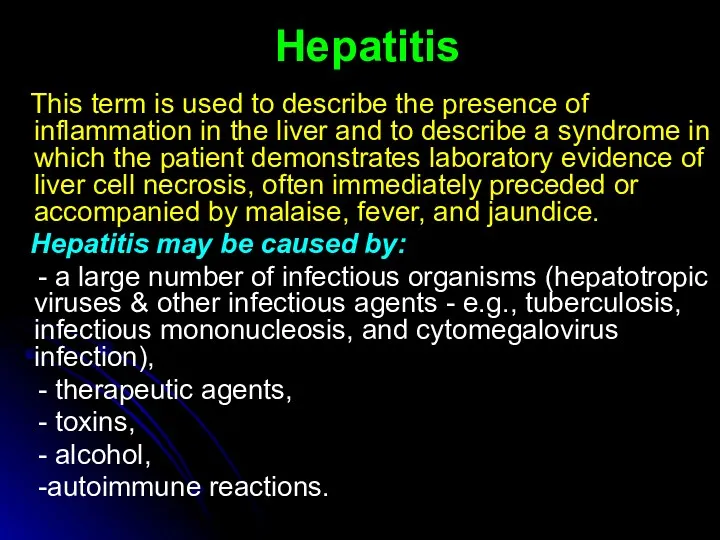
- 5. Hepatitis This term is used to describe the presence of inflammation in the liver and to
- 6. Hepatotropic viruses infect primarily hepatocytes. The known hepatotropic viruses include: hepatitis A virus (HAV), hepatitis В
- 7. HBV and HCV are mostly often transmitted by the parenteral route: - blood transfusions (high risk
- 8. CLINICAL SYMPTOMS 1. Asymptomatic infection (serologic evidence only) 2. Acute hepatitis a. Anicteric b. Icteric 3.
- 9. Acute Viral Hepatitis Sporadic attacks of acute hepatitis caused by all of the hepatotropic viruses are
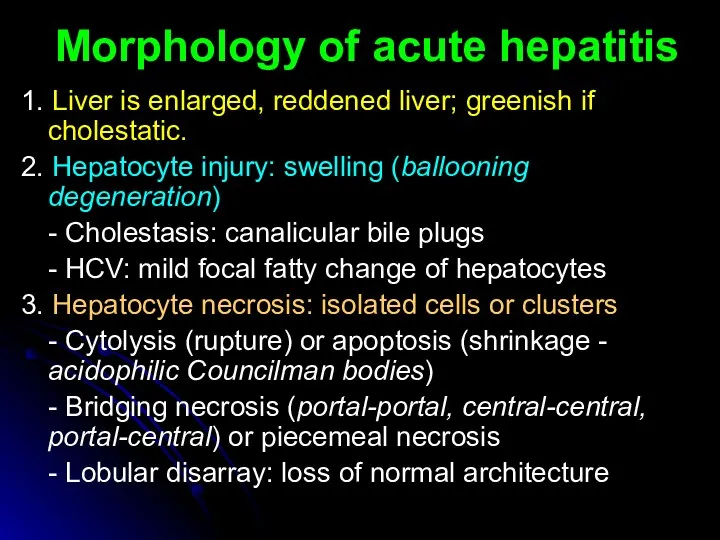
- 10. 1. Liver is enlarged, reddened liver; greenish if cholestatic. 2. Hepatocyte injury: swelling (ballooning degeneration) -
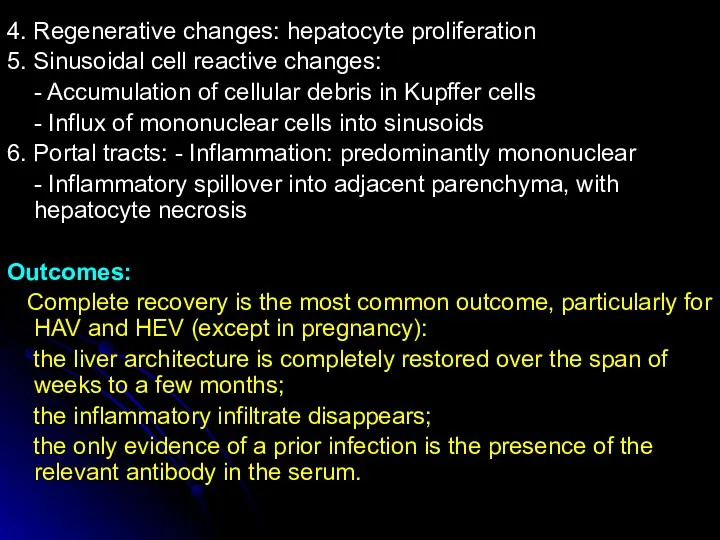
- 11. 4. Regenerative changes: hepatocyte proliferation 5. Sinusoidal cell reactive changes: - Accumulation of cellular debris in
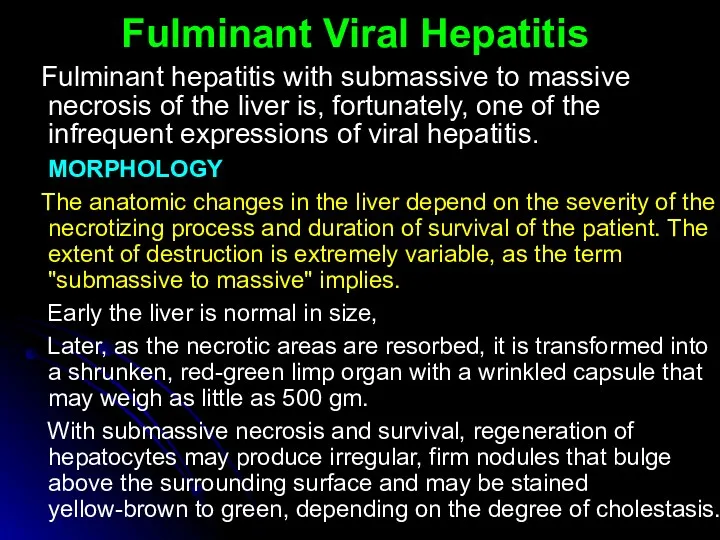
- 12. Fulminant Viral Hepatitis Fulminant hepatitis with submassive to massive necrosis of the liver is, fortunately, one
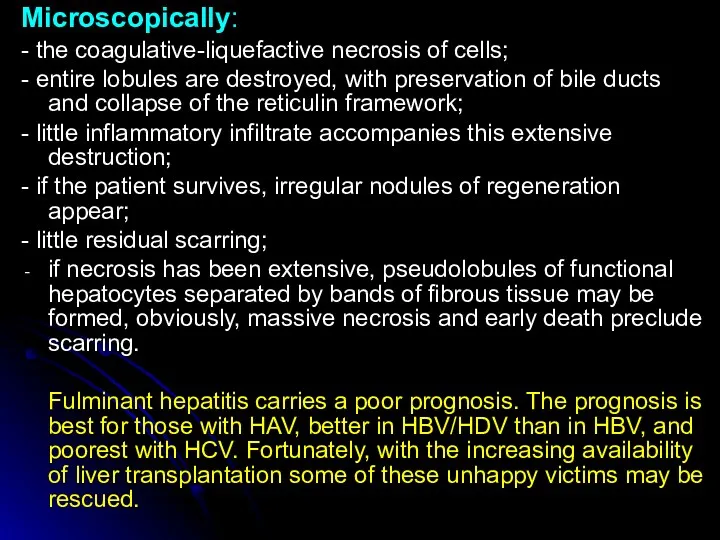
- 13. Microscopically: - the coagulative-liquefactive necrosis of cells; - entire lobules are destroyed, with preservation of bile
- 14. Chronic Hepatitis Chronic hepatitis is defined as the continuation of hepatic inflammation and necrosis for longer
- 15. CPH is characterized clinically by: - persistence of elevated levels of liver aminotransferase enzymes (AST and
- 16. In contrast, in chronic "lobular" hepatitis: the portal tracts are only mildly inflamed and random hepatocytes
- 17. Chronic Active Hepatitis In contrast to the previous condition, САН is characterized by progressive destruction of
- 18. Active destruction of hepatocytes at the interface between the periportal inflammatory infiltrate and adjacent hepatocytes, leading
- 19. AUTOIMMUNE CHRONIC HEPATITIS Chronic hepatitis unrelated to known viral agents or toxins is frequently ascribed to
- 20. Liver cirrhosis Cirrhosis is a result of advanced liver disease. It is characterized by replacement of
- 21. According to cause: Alcoholic liver disease (ALD) Alcoholic cirrhosis, Non-alcoholic steatohepatitis (NASH), Viral hepatitis (B, C),
- 22. According to morphology: Micronodular (less then 3 mm), Macronodular (more then 3 mm), Mixed, Septal According
- 23. CLINICAL SYMPTOMS Cirrhosis has many possible manifestations. These signs and symptoms may be either as a
- 24. Spider angiomata or spider nevi are vascular lesions consisting of a central arteriole surrounded by many
- 25. Hypogonadism, a decrease in sex hormones manifest as impotence, infertility, loss of sexual drive, and testicular
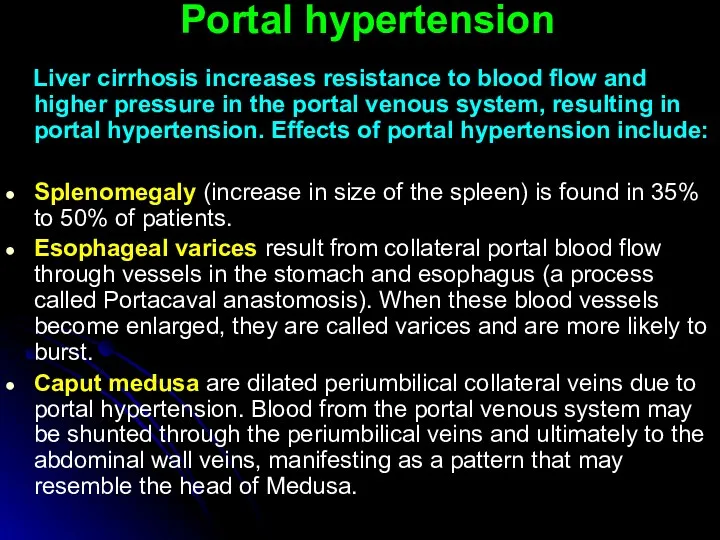
- 26. Portal hypertension Liver cirrhosis increases resistance to blood flow and higher pressure in the portal venous
- 28. Скачать презентацию
 Лейкокория у детей
Лейкокория у детей Методика исследования периферических и внутригрудных лимфатических узлов
Методика исследования периферических и внутригрудных лимфатических узлов Инфекционные болезни - чума
Инфекционные болезни - чума Наложение шин на руку
Наложение шин на руку Сердечно-легочная реанимация
Сердечно-легочная реанимация Жүктілікпен байланысты гипертензиясы Ерте токсикоздар
Жүктілікпен байланысты гипертензиясы Ерте токсикоздар Воздействие на поведение водителя психотропных, наркотических веществ, алкоголя и медицинских препаратов
Воздействие на поведение водителя психотропных, наркотических веществ, алкоголя и медицинских препаратов Косметические средства ухода за кожей детей при аномалиях конституции
Косметические средства ухода за кожей детей при аномалиях конституции Diet and teen health
Diet and teen health Зрительный нерв. Заболевания зрительного нерва
Зрительный нерв. Заболевания зрительного нерва Реанимационная помощь
Реанимационная помощь Дәрілік заттардың әсерінің ағза қасиеттеріне тәуелділігі. Фармакологиялық әсердің дәрілік заттардың қасиеттері мен қолдану
Дәрілік заттардың әсерінің ағза қасиеттеріне тәуелділігі. Фармакологиялық әсердің дәрілік заттардың қасиеттері мен қолдану Antimicrobial drugs
Antimicrobial drugs Снотворные и противосудорожные средства. Противопаркинсонические средства
Снотворные и противосудорожные средства. Противопаркинсонические средства Предмет и задачи медицинской микробиологии. История микробиологии. Медицинская микробиология XXI века
Предмет и задачи медицинской микробиологии. История микробиологии. Медицинская микробиология XXI века Ошибки диагностики и лечения при сочетанной травме
Ошибки диагностики и лечения при сочетанной травме Профилактика стоматологических заболеваний в раннем детском возрасте
Профилактика стоматологических заболеваний в раннем детском возрасте Вскармливание детей грудного возраста. Раздел 1.Лекция 6
Вскармливание детей грудного возраста. Раздел 1.Лекция 6 Современные направления пластической хирургии в акушерстве и гинекологии
Современные направления пластической хирургии в акушерстве и гинекологии Местные анестетики
Местные анестетики Всероссийский день трезвости
Всероссийский день трезвости ВКР: Анализ работы медсестры процедурного кабинета хирургического отделения стационара
ВКР: Анализ работы медсестры процедурного кабинета хирургического отделения стационара Врожденные аномалии грудной клетки
Врожденные аномалии грудной клетки Вреден ли фаст-фуд для нашего здоровья
Вреден ли фаст-фуд для нашего здоровья Здоровый образ жизни и профилактика основных неинфекционных заболеваний
Здоровый образ жизни и профилактика основных неинфекционных заболеваний Қазіргі заманғы денсаулық сақтау, әлемдік тенденция, дамыған елдер
Қазіргі заманғы денсаулық сақтау, әлемдік тенденция, дамыған елдер Иммуногенез бұзылуының морфологиясы. Тимустың, шеткері лимфалық тіндердің иммунгенез бұзылғандағы өзгерістері
Иммуногенез бұзылуының морфологиясы. Тимустың, шеткері лимфалық тіндердің иммунгенез бұзылғандағы өзгерістері Жүкті студенттердің медико-әлеуметтік аспектілері
Жүкті студенттердің медико-әлеуметтік аспектілері