Содержание
- 2. RISK FACTORS Fair skinned. Hair color other than black. Excessive sun exposure . Melanoma in first-degree
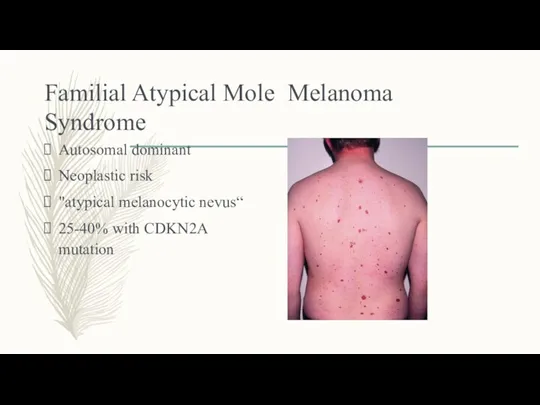
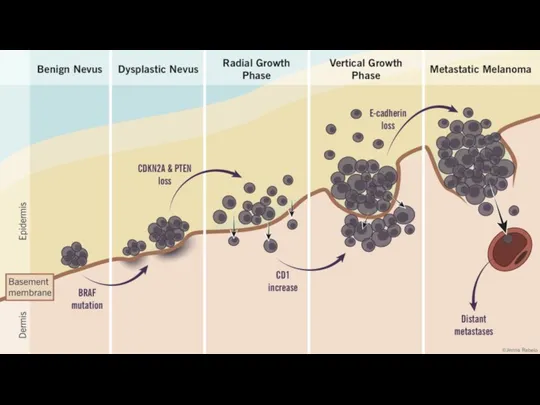
- 3. Familial Atypical Mole Melanoma Syndrome Autosomal dominant Neoplastic risk "atypical melanocytic nevus“ 25-40% with CDKN2A mutation
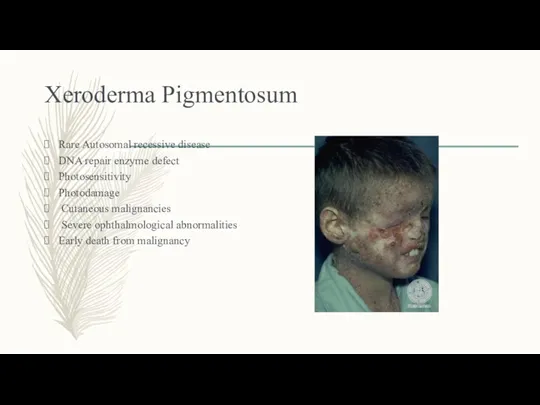
- 4. Xeroderma Pigmentosum Rare Autosomal recessive disease DNA repair enzyme defect Photosensitivity Photodamage Cutaneous malignancies Severe ophthalmological
- 5. Ultraviolet light
- 6. UVC ( Completely absorbed by the atmosphere and is non-relevant for UV induced skin carcinogenesis. UVB
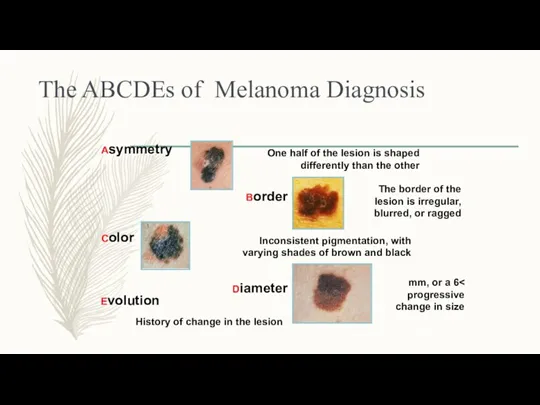
- 8. The ABCDEs of Melanoma Diagnosis Asymmetry One half of the lesion is shaped differently than the
- 9. TYPES OF MELANOMA
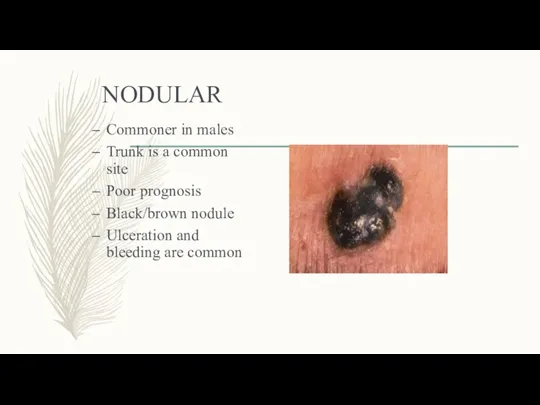
- 10. NODULAR Commoner in males Trunk is a common site Poor prognosis Black/brown nodule Ulceration and bleeding
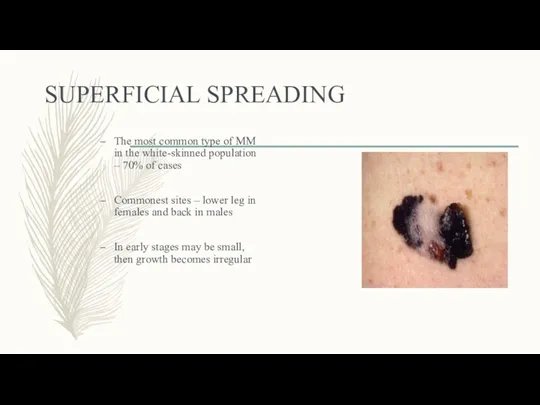
- 11. SUPERFICIAL SPREADING The most common type of MM in the white-skinned population – 70% of cases
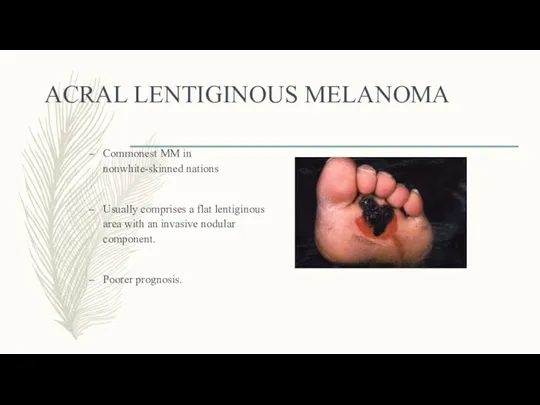
- 12. ACRAL LENTIGINOUS MELANOMA Commonest MM in nonwhite-skinned nations Usually comprises a flat lentiginous area with an
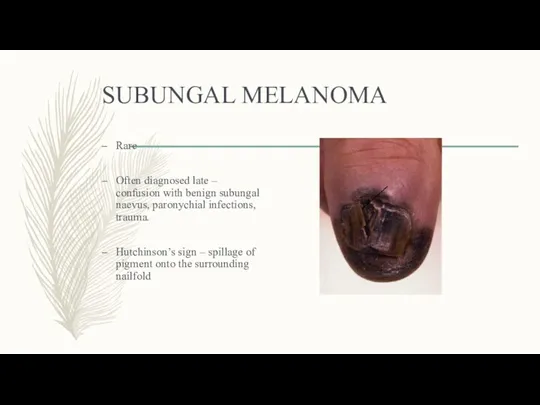
- 13. SUBUNGAL MELANOMA Rare Often diagnosed late – confusion with benign subungal naevus, paronychial infections, trauma. Hutchinson’s
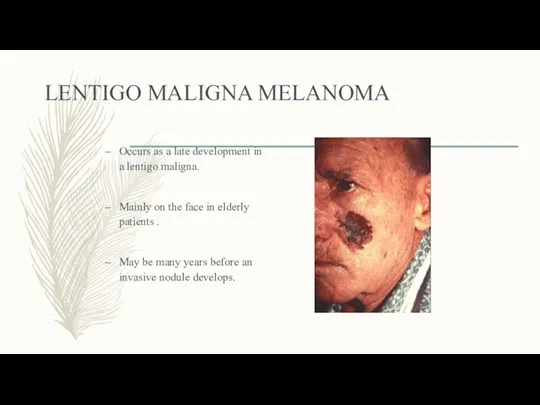
- 14. LENTIGO MALIGNA MELANOMA Occurs as a late development in a lentigo maligna. Mainly on the face
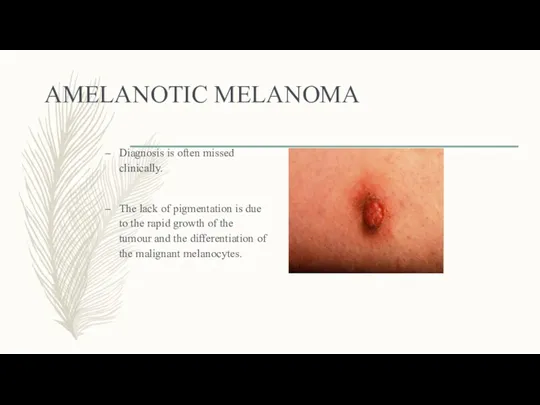
- 15. AMELANOTIC MELANOMA Diagnosis is often missed clinically. The lack of pigmentation is due to the rapid
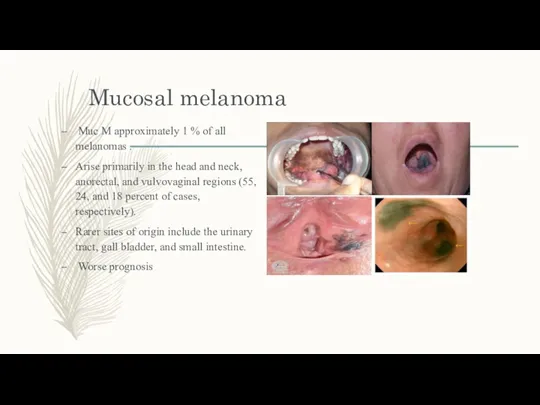
- 16. Mucosal melanoma Muc M approximately 1 % of all melanomas . Arise primarily in the head
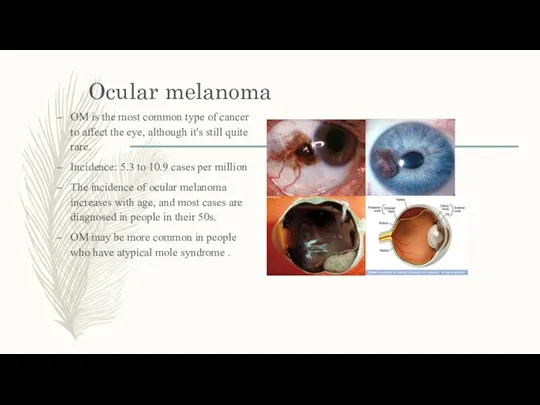
- 17. Ocular melanoma OM is the most common type of cancer to affect the eye, although it's
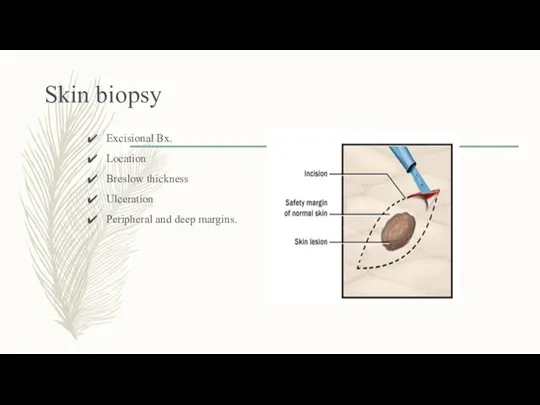
- 18. Skin biopsy Excisional Bx. Location Breslow thickness Ulceration Peripheral and deep margins.
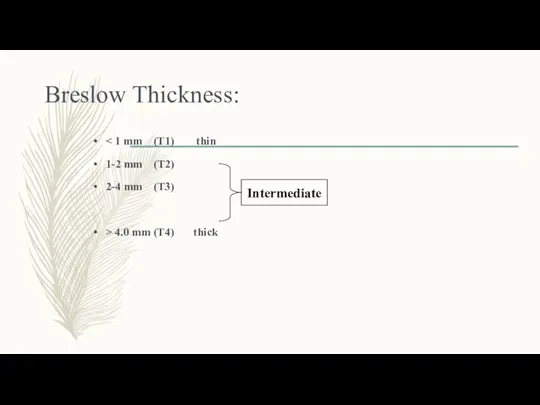
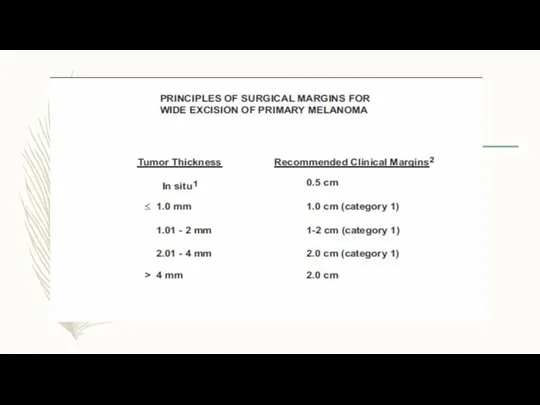
- 19. Breslow Thickness: 1-2 mm (T2) 2-4 mm (T3) > 4.0 mm (T4) thick Intermediate
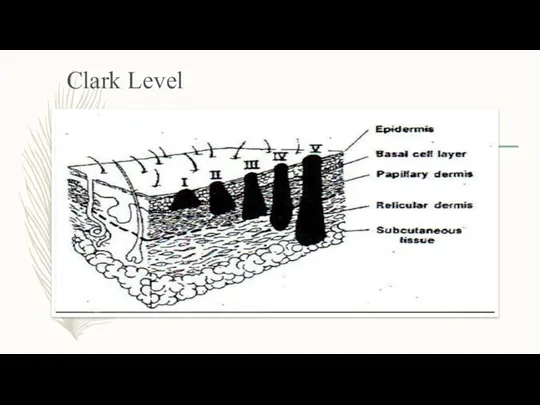
- 20. Clark Level
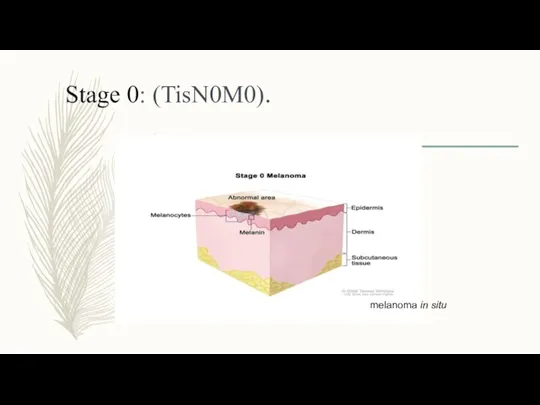
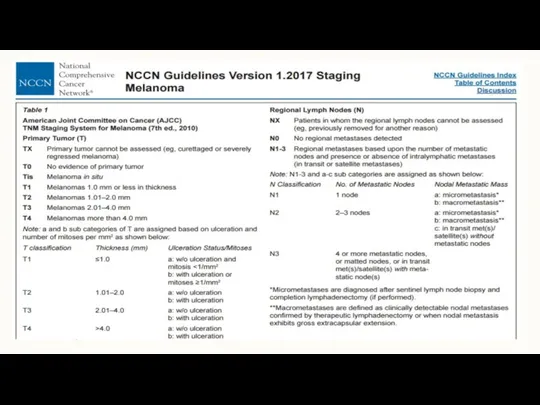
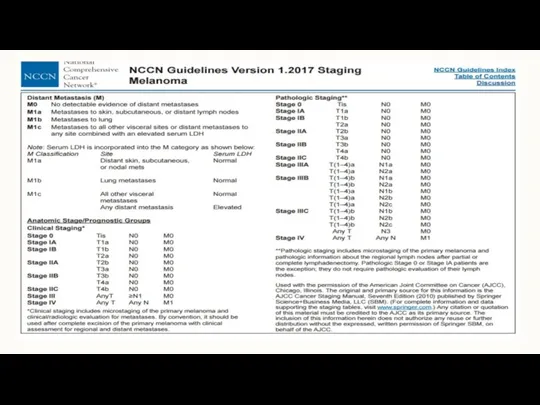
- 21. Stage 0: (TisN0M0). melanoma in situ
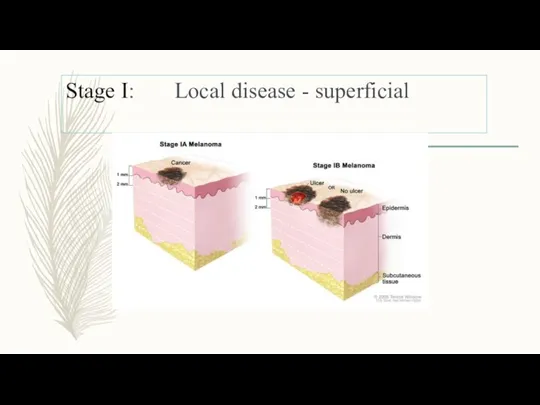
- 22. Stage I: Local disease - superficial
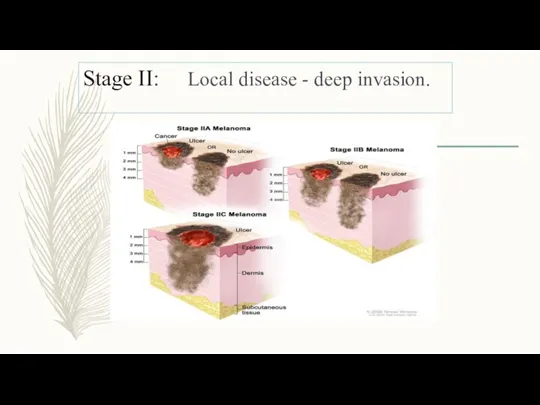
- 23. Stage II: Local disease - deep invasion.
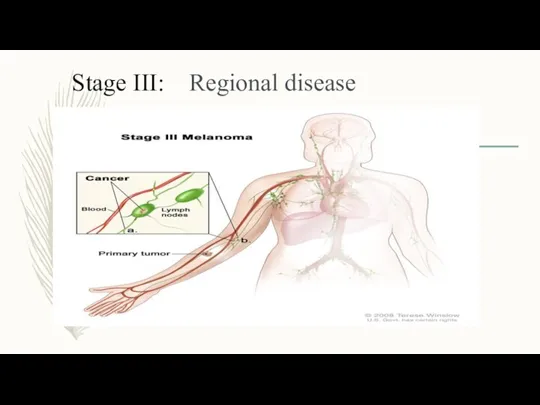
- 24. Stage III: Regional disease
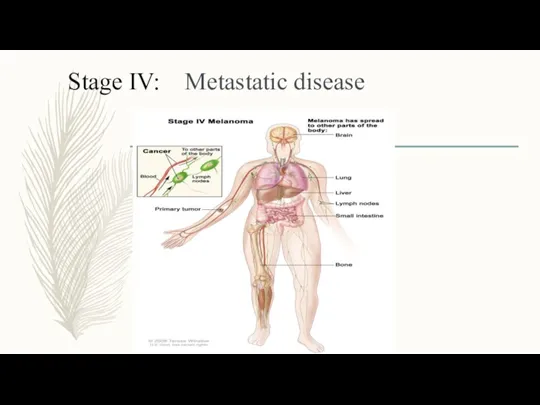
- 25. Stage IV: Metastatic disease
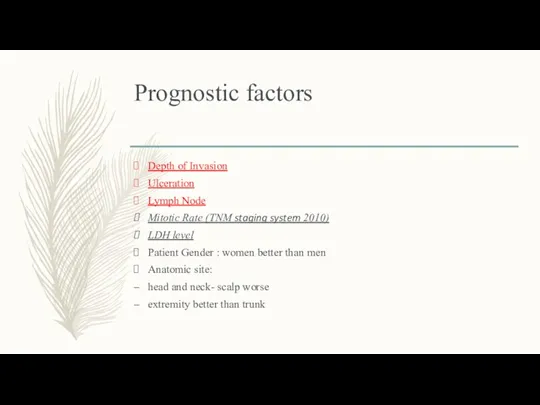
- 26. Prognostic factors Depth of Invasion Ulceration Lymph Node Mitotic Rate (TNM staging system 2010) LDH level
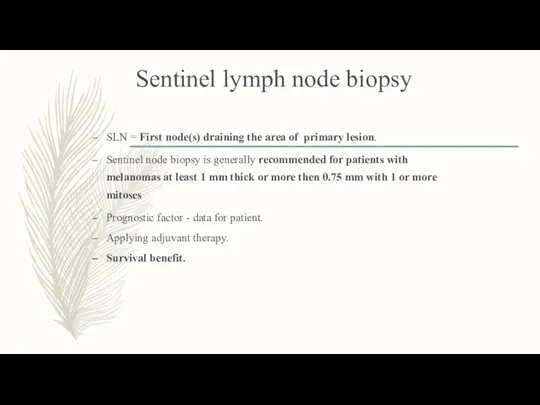
- 31. Sentinel lymph node biopsy SLN = First node(s) draining the area of primary lesion. Sentinel node
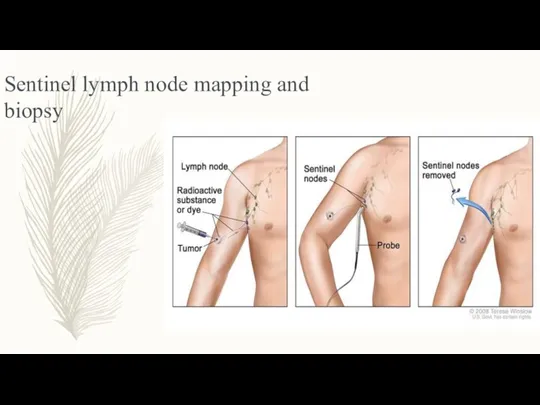
- 32. Sentinel lymph node mapping and biopsy
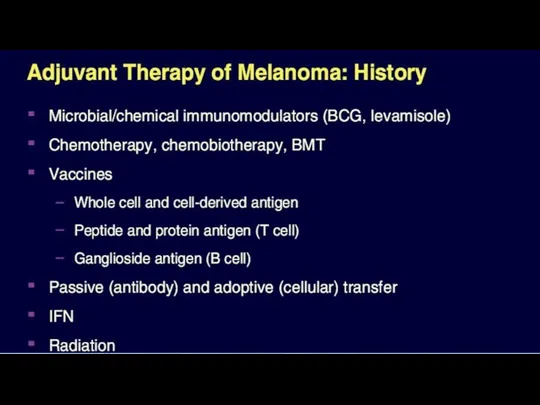
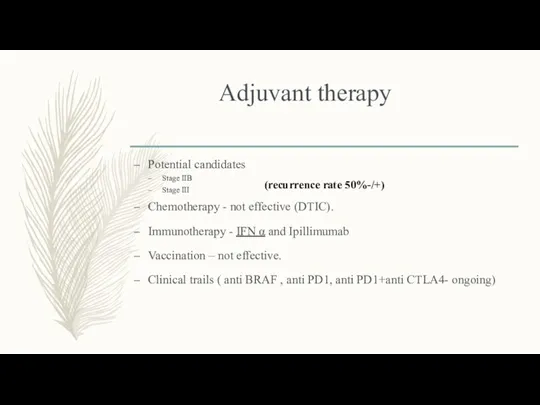
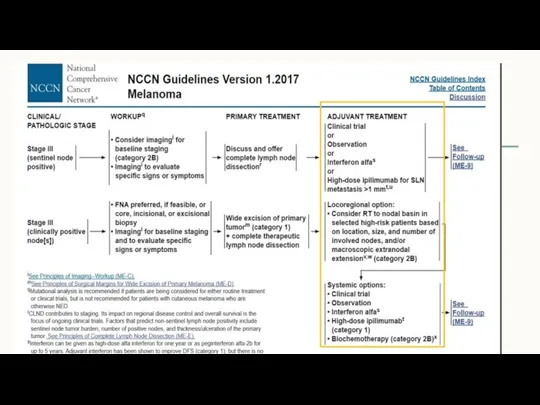
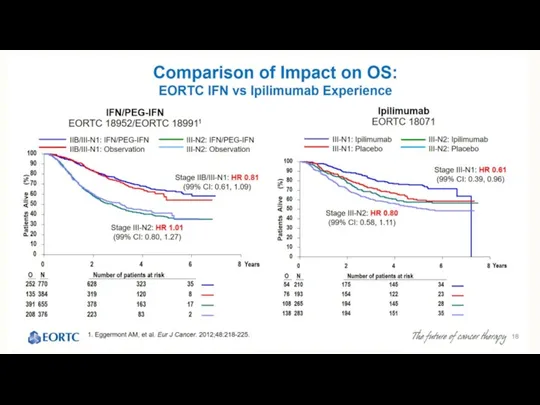
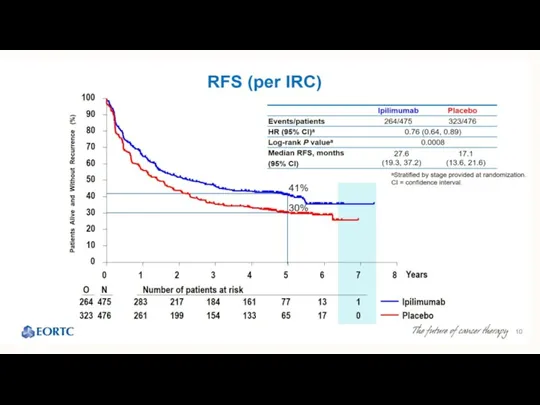
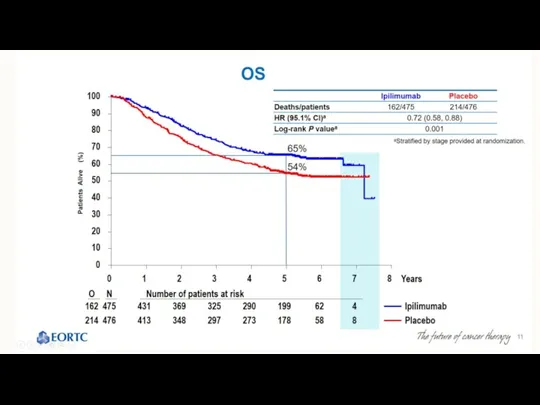
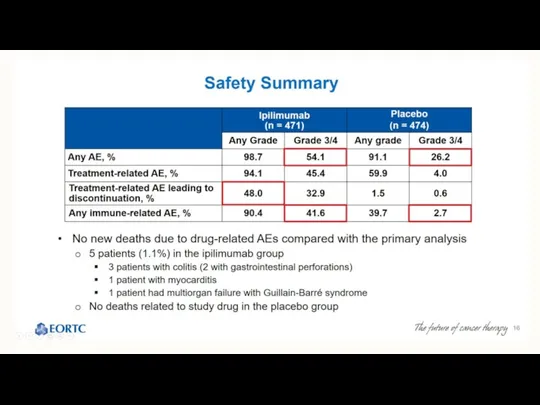
- 34. Adjuvant therapy Potential candidates Stage IIB Stage III Chemotherapy - not effective (DTIC). Immunotherapy - IFN
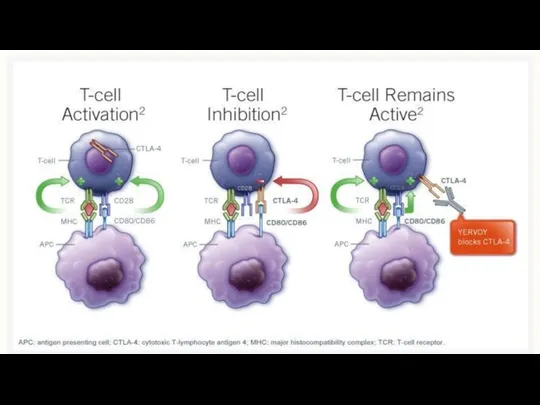
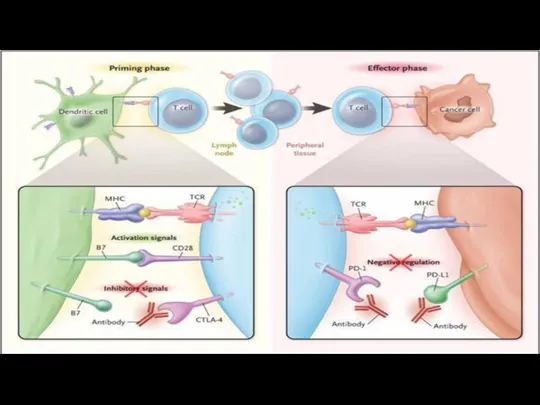
- 36. IPILIMUMAB Yervoy Anti CTLA4 Antibody
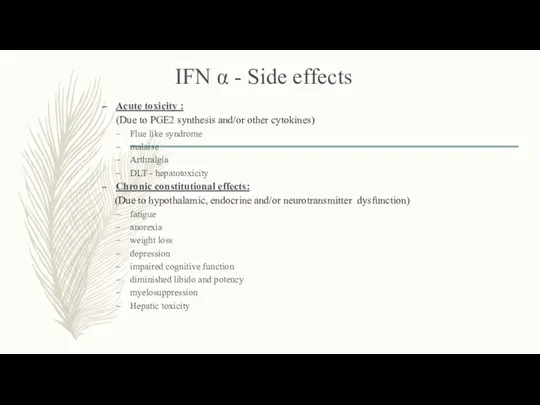
- 42. IFN α - Side effects Acute toxicity : (Due to PGE2 synthesis and/or other cytokines) Flue
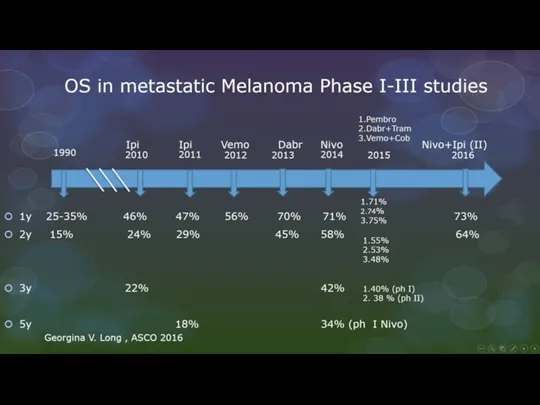
- 43. Treatment Options for advanced Melanoma
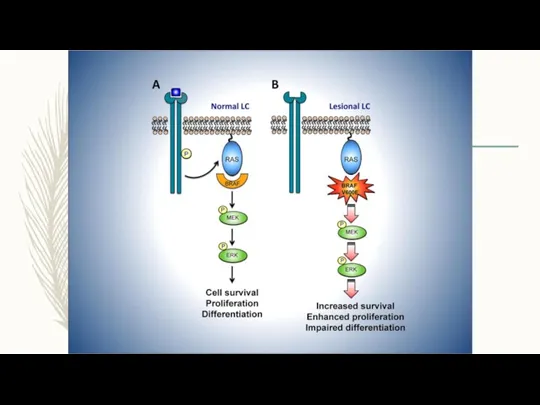
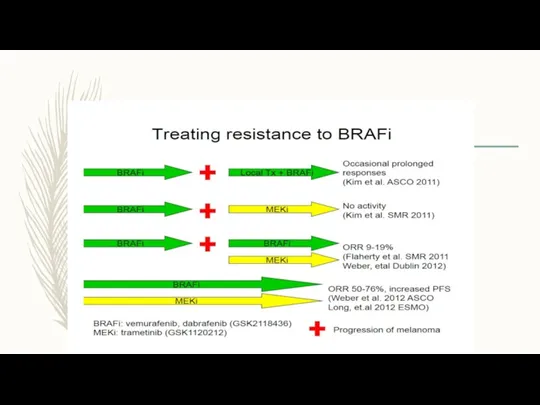
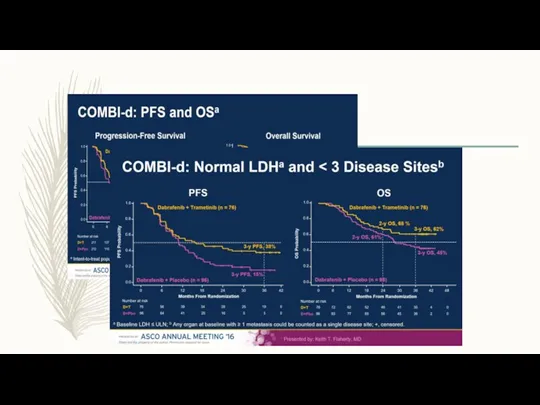
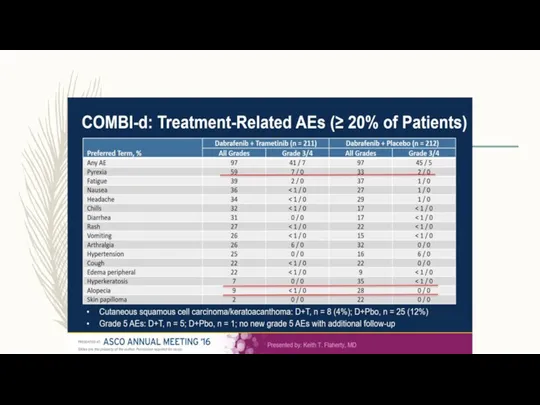
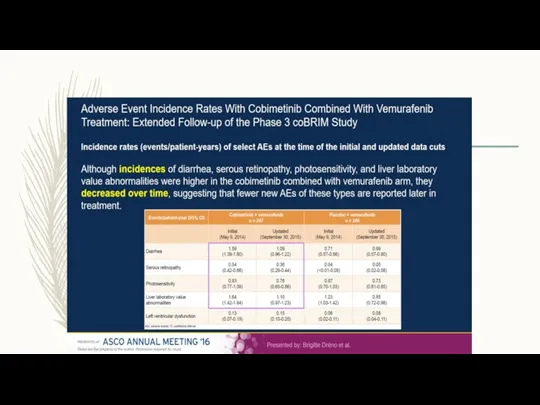
- 44. BRAF\MEK Inhibitors Dabrafenib (TAFINLAR) Trametinib ( MEKINIST) Vemurafenib ( ZELBORAF) Cobimetinib (COTELIC)
- 50. Imunotherapy
- 52. Ipillimumab (Yervoy) In pooled analysis of 12 studies, a plateau in the survival curve begins at
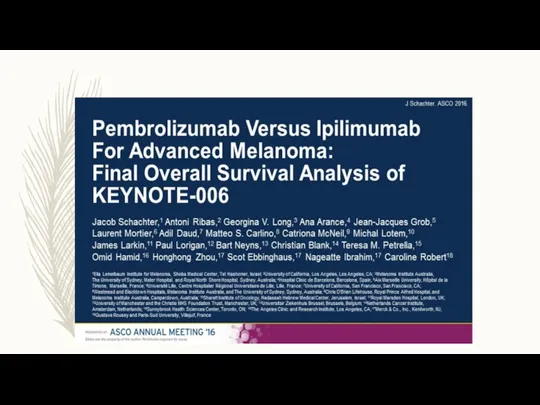
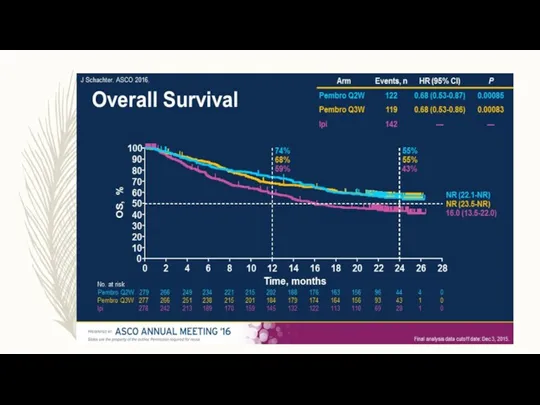
- 54. Anti PD1 therapy : Opdivo (Nivolumab) Keytruda (Pembrolizumab)
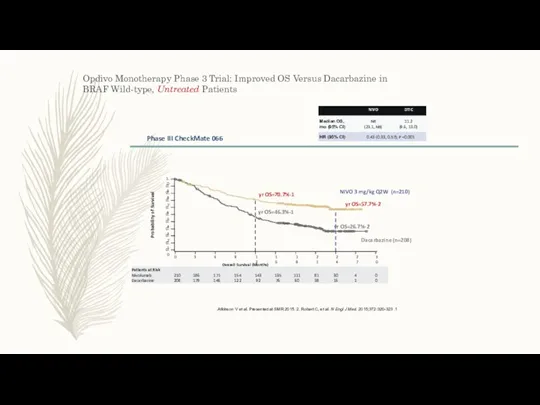
- 55. Opdivo Monotherapy Phase 3 Trial: Improved OS Versus Dacarbazine in BRAF Wild-type, Untreated Patients 1. Atkinson
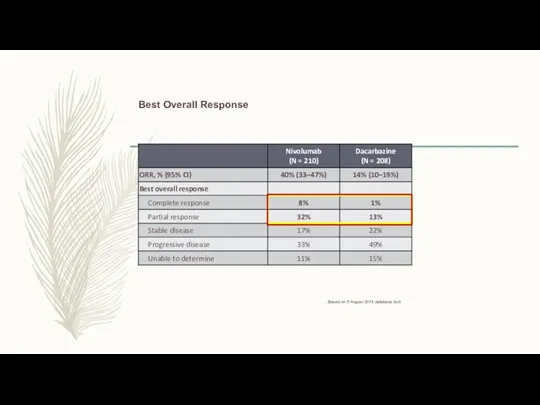
- 56. Best Overall Response Based on 5 August 2014 database lock.
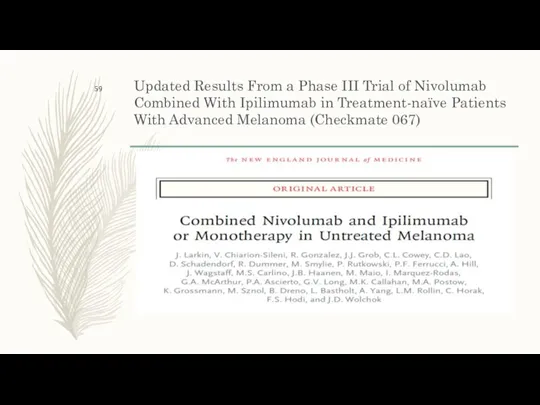
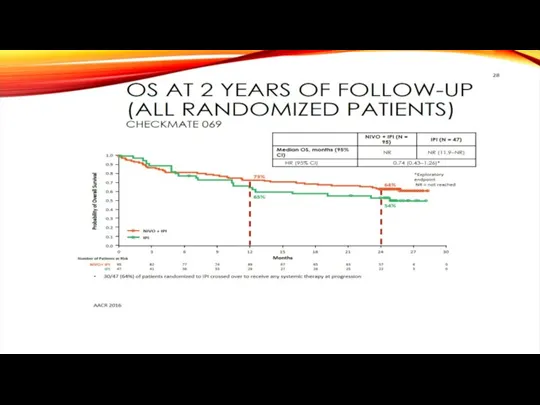
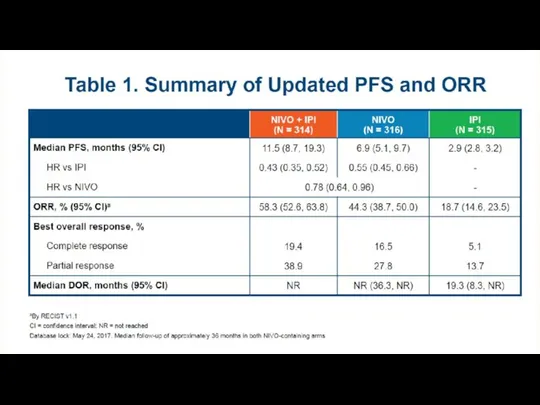
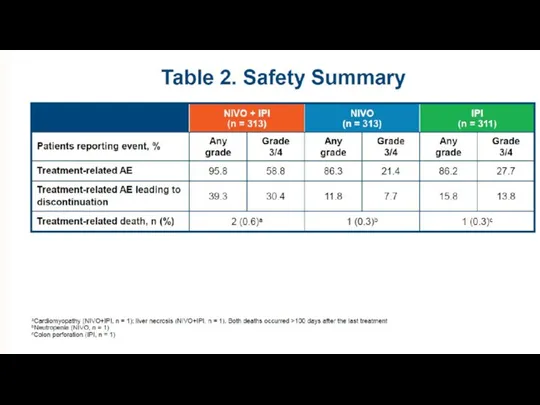
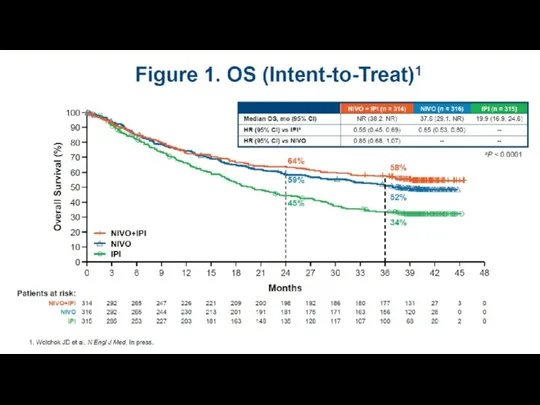
- 59. Updated Results From a Phase III Trial of Nivolumab Combined With Ipilimumab in Treatment-naïve Patients With
- 60. OS at 2 Years of Follow-up (All Randomized Patients) Checkmate 069 30/47 (64%) of patients randomized
- 61. Response To Treatment
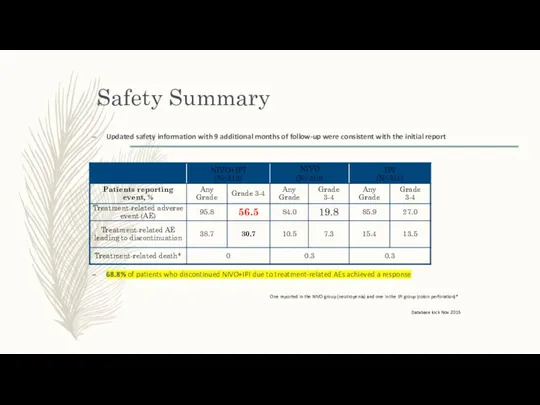
- 62. Safety Summary Updated safety information with 9 additional months of follow-up were consistent with the initial
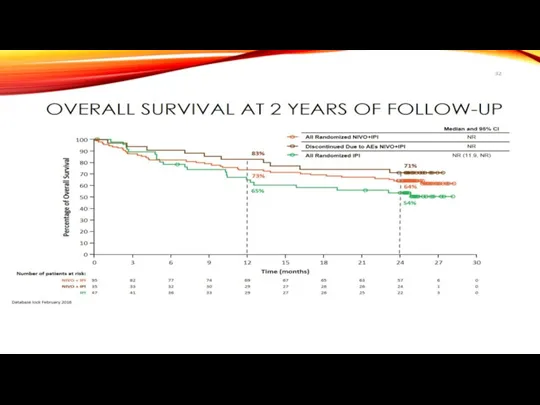
- 65. Overall Survival at 2 Years of Follow-up 83% 71% 73% 64% 65% 54% Database lock February
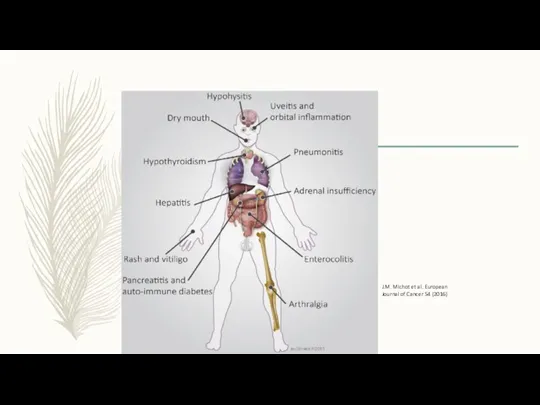
- 66. J.M. Michot et al. European Journal of Cancer 54 (2016)
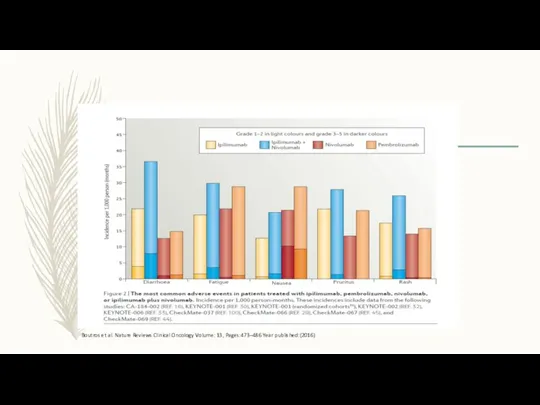
- 67. Boutros et al. Nature Reviews Clinical Oncology Volume: 13, Pages:473–486 Year published:(2016)
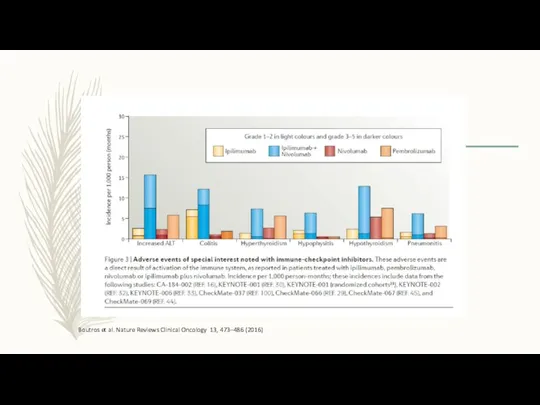
- 68. Nature Reviews Clinical Oncology Volume: 13, Pages: 473–486 Year published: (2016) DOI: doi:10.1038/nrclinonc.2016.58 Published online 04
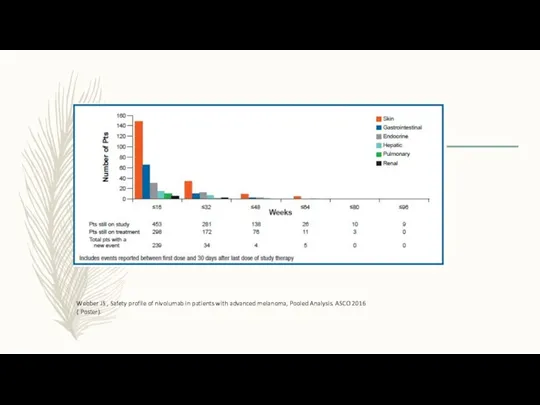
- 69. Webber JS , Safety profile of nivolumab in patients with advanced melanoma, Pooled Analysis. ASCO 2016
- 72. Скачать презентацию



 Тіс, тіс қатарлары ақауын емдеу
Тіс, тіс қатарлары ақауын емдеу Десмургія. Техніка накладення пов'язок і шин
Десмургія. Техніка накладення пов'язок і шин Роль медицинской сестры палатной при соблюдении лечебно-охранительного режима в стационаре
Роль медицинской сестры палатной при соблюдении лечебно-охранительного режима в стационаре проект
проект Обезболивание. Наркоз
Обезболивание. Наркоз Науқастың күтімі және оның маңызы
Науқастың күтімі және оның маңызы Ботулизм. Возбудители ботулизма
Ботулизм. Возбудители ботулизма Сердце, аорта, кровь, вены, капилляры
Сердце, аорта, кровь, вены, капилляры Расстройства личности и поведения в зрелом возрасте (психопатии)
Расстройства личности и поведения в зрелом возрасте (психопатии) Гепатит B. Молекулярная биология
Гепатит B. Молекулярная биология Лечение артериальной гипертензии
Лечение артериальной гипертензии Мозжечок, синдромы поражения. Экстрапирамидная система, синдромы поражения
Мозжечок, синдромы поражения. Экстрапирамидная система, синдромы поражения Острые лимфобластные лейкозы
Острые лимфобластные лейкозы Первая помощь при травмах
Первая помощь при травмах Методы изучения генетики. Медико-генетическое консультирование
Методы изучения генетики. Медико-генетическое консультирование Таным туралы ілім. Медициналық, ғылыми танымның ерекшелігі
Таным туралы ілім. Медициналық, ғылыми танымның ерекшелігі Ethics and Human Rights in Medicine and Medical Research
Ethics and Human Rights in Medicine and Medical Research Меланома кожи. Диагностика, клиника и лечение
Меланома кожи. Диагностика, клиника и лечение Легионеллез
Легионеллез Отек и выпот
Отек и выпот Прогнозирование потребности в лекарственных средствах
Прогнозирование потребности в лекарственных средствах Актуализация формулярной системы в гериатрическом стационаре
Актуализация формулярной системы в гериатрическом стационаре Грыжи. Составные элементы грыжи
Грыжи. Составные элементы грыжи Частная анатомия зубов
Частная анатомия зубов Ранняя диагностика острого лейкоза у детей
Ранняя диагностика острого лейкоза у детей Наследственные болезни человека
Наследственные болезни человека Модели взаимоотношения врач-пациент. Моральные принципы и правила проведения исследований на человеке и животных
Модели взаимоотношения врач-пациент. Моральные принципы и правила проведения исследований на человеке и животных Климактерический синдром
Климактерический синдром