Содержание
- 2. Agenda What is Nanoknife? The system Peri-Operative Considerations Nanoknife Treatment Planning Software Planning Procedure, Tips &
- 3. WHAT IS NANOKNIFE?
- 4. NanoKnife® Therapy: What is It? The NanoKnife® System is indicated for the surgical ablation of soft
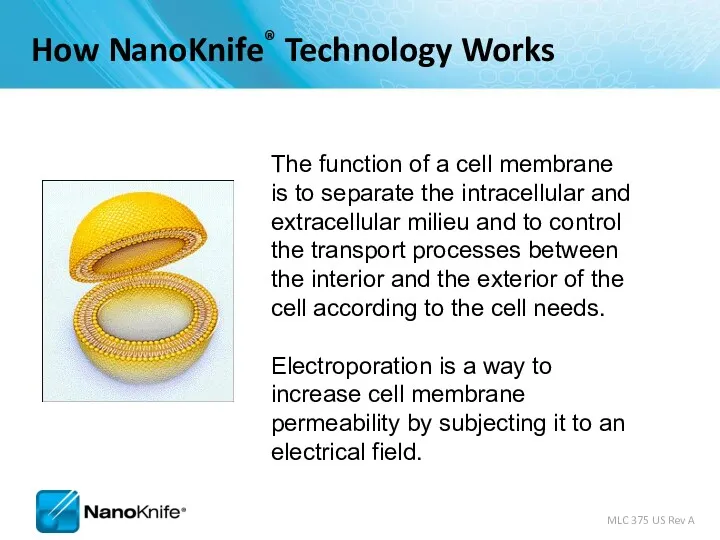
- 5. The function of a cell membrane is to separate the intracellular and extracellular milieu and to
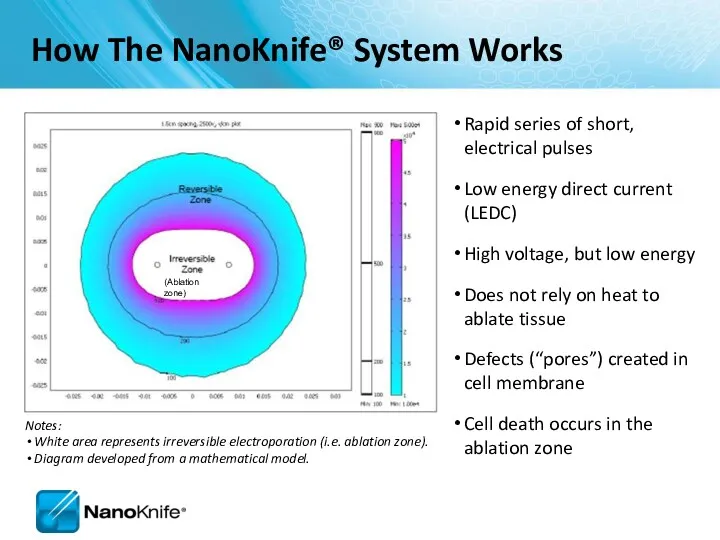
- 6. Rapid series of short, electrical pulses Low energy direct current (LEDC) High voltage, but low energy
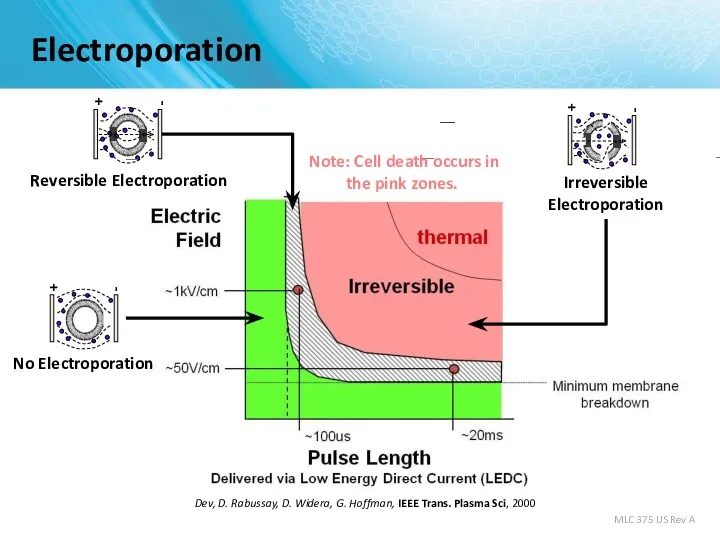
- 7. Electroporation S. Dev, D. Rabussay, D. Widera, G. Hoffman, IEEE Trans. Plasma Sci, 2000 Note: Cell
- 8. Uses high voltage, low energy electrical pulses to achieve tissue effect Does not rely on heat
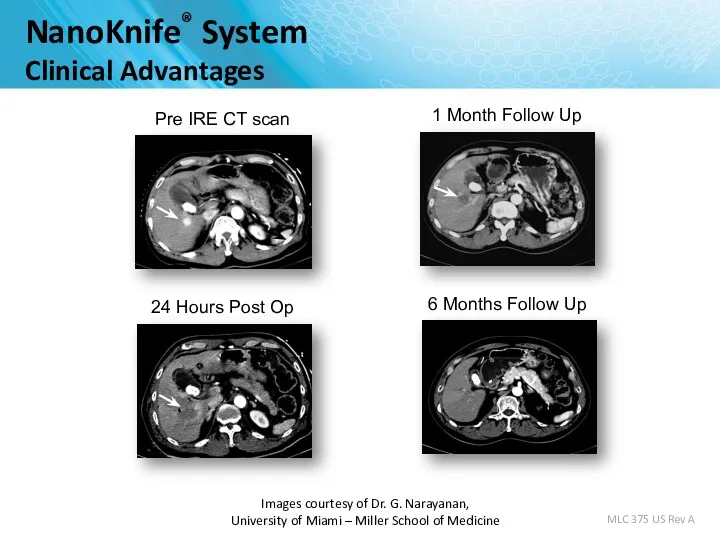
- 9. Images courtesy of Dr. G. Narayanan, University of Miami – Miller School of Medicine MLC 375
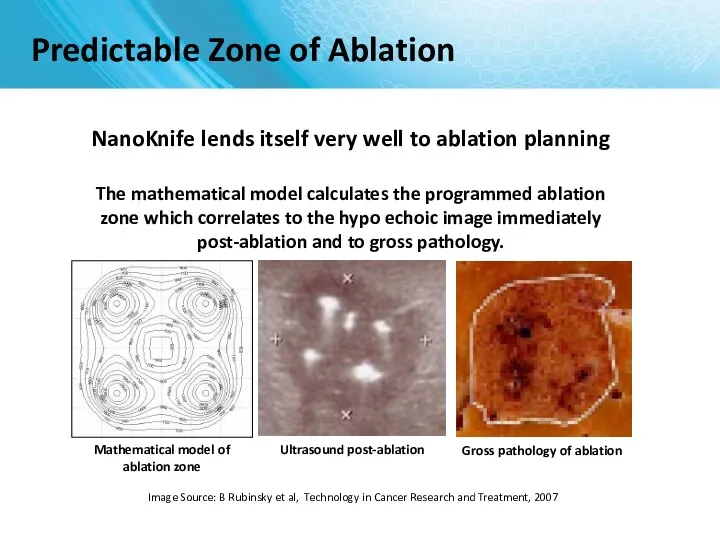
- 10. Image Source: B Rubinsky et al, Technology in Cancer Research and Treatment, 2007 NanoKnife lends itself
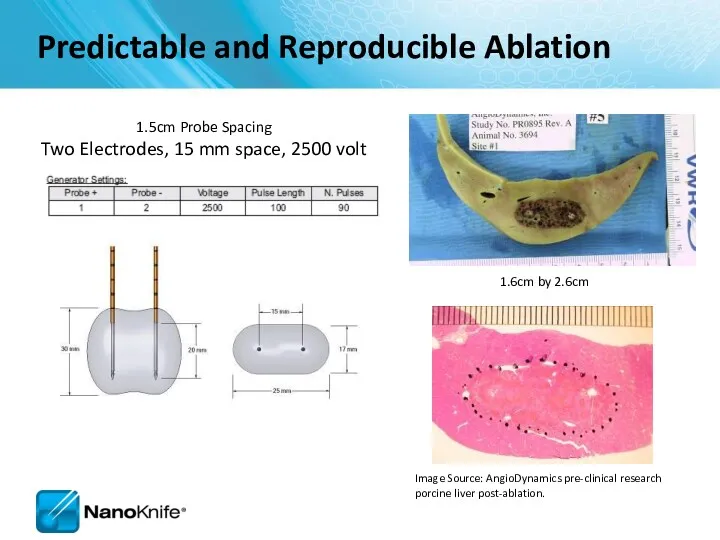
- 11. 1.6cm by 2.6cm 1.5cm Probe Spacing Two Electrodes, 15 mm space, 2500 volt Image Source: AngioDynamics
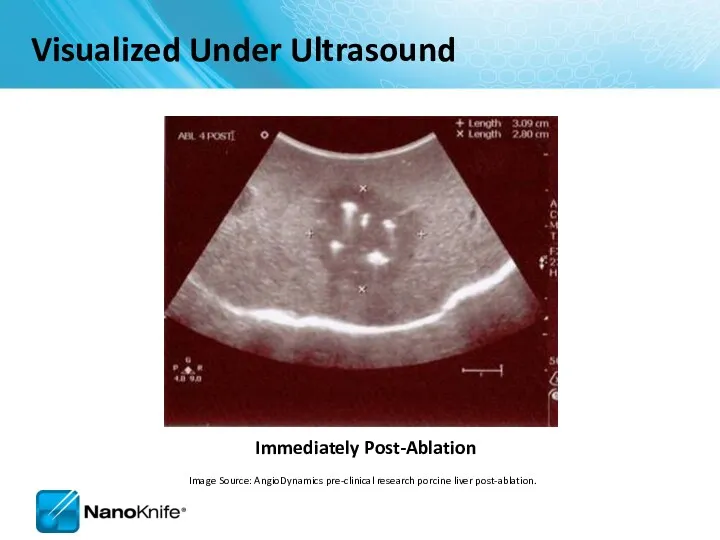
- 12. Immediately Post-Ablation Visualized Under Ultrasound Image Source: AngioDynamics pre-clinical research porcine liver post-ablation.
- 13. THE NANOKNIFE SYSTEM
- 14. FDA 510(k) clearance for the surgical ablation of soft tissue. It has not received clearance for
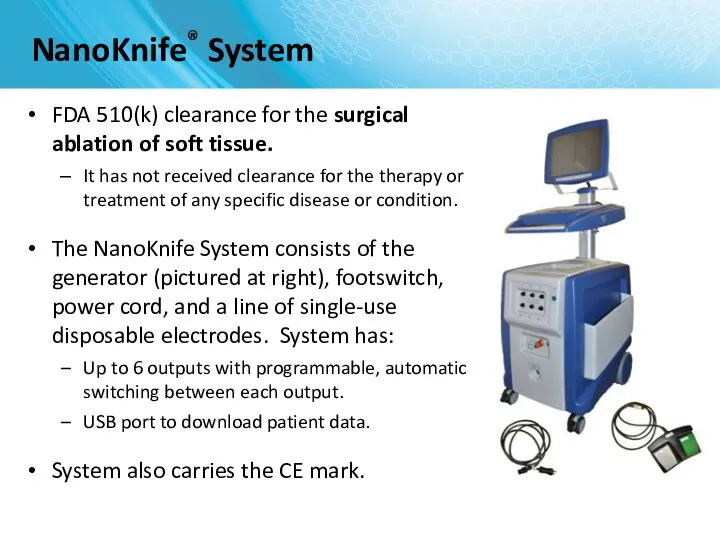
- 15. Monopolar Electrode Single Electrode Disposable 15 cm length 25 cm length In the event insufflation is
- 16. Monopolar Electrode Key Features 19 gauge needle with depth markings Echogenic needle surface Active electrode length
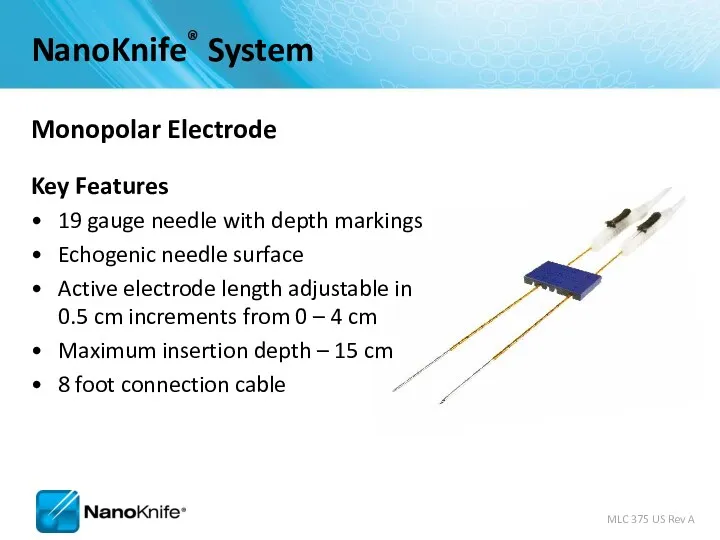
- 17. Activation Probe
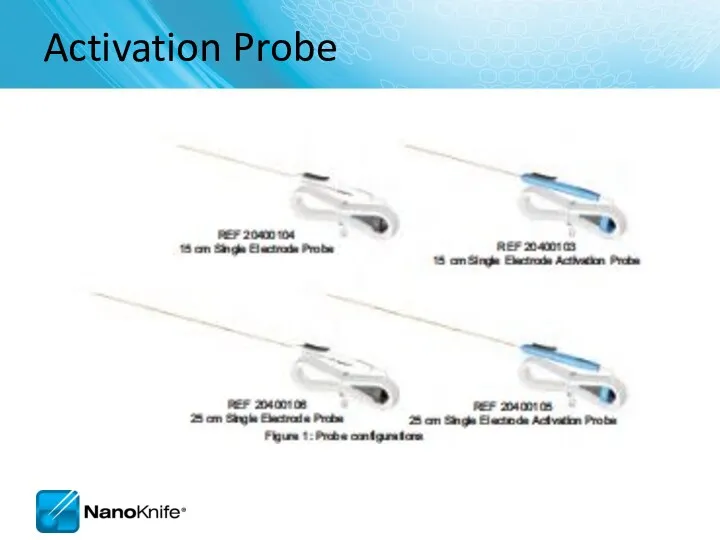
- 18. External synchronization device. The ECG Trigger Monitor automatically detects the R Wave (when energy is delivered)
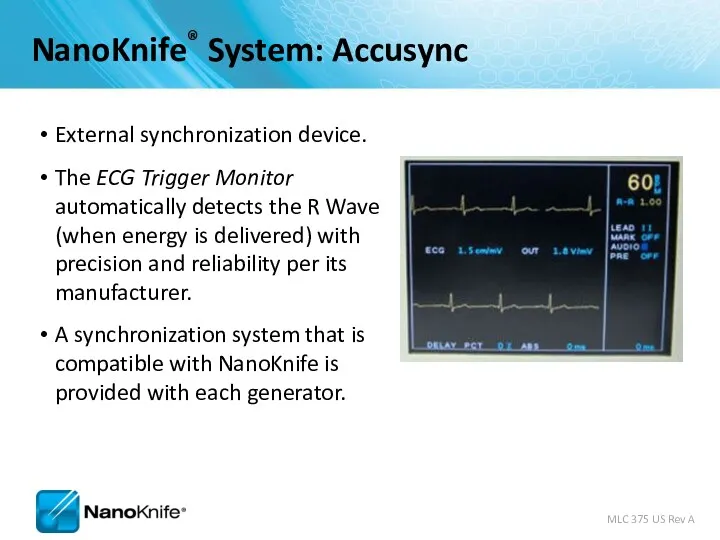
- 19. Energy Delivery 0 15 30 45 60 75 90 105 120 135 0 3kV max Synchronized
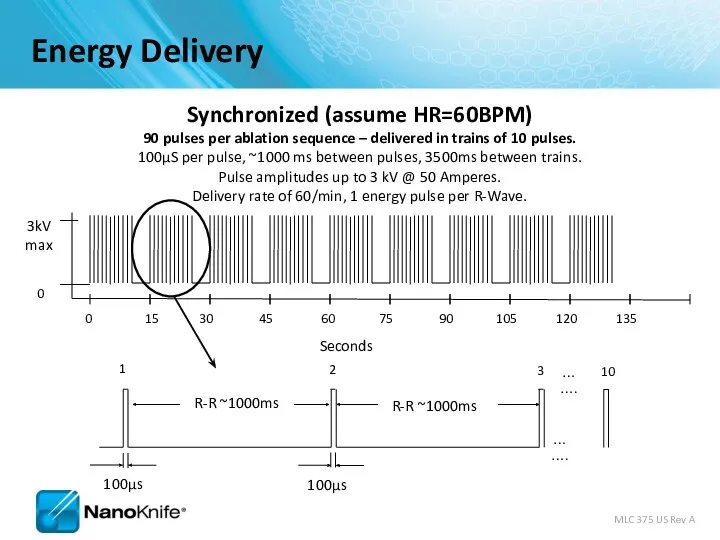
- 20. Why NanoKnife® Therapy? Differentiate your institution from competing hospitals On the cutting edge of defining new
- 21. PERI-OPERATIVE CONSIDERATIONS University of Louisville
- 22. Objectives NanoKnife Components Room Set Up Patient Set Up Anesthesia Considerations Treatment Planning Procedural Overview
- 23. NanoKnife System consists of the NanoKnife® System
- 24. NANOKNIFE ROOM PREPARATION
- 25. Room Preparation General anesthesia cart All monitoring & resuscitation equipment required for general anesthesia per ASA
- 26. Patient Set up Position patient for optimal access Consider type of access; percutaneous, laparoscopic, open Consider
- 27. Patient Set Up (Cont’d) Physician to discuss with anesthesiologist Muscle blockade required during energy delivery Alert
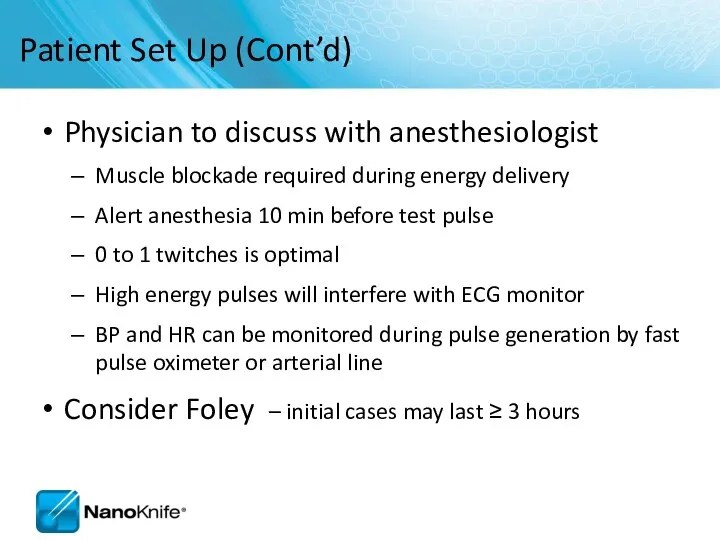
- 28. ECG Sync Device – Patient Lead Set Up
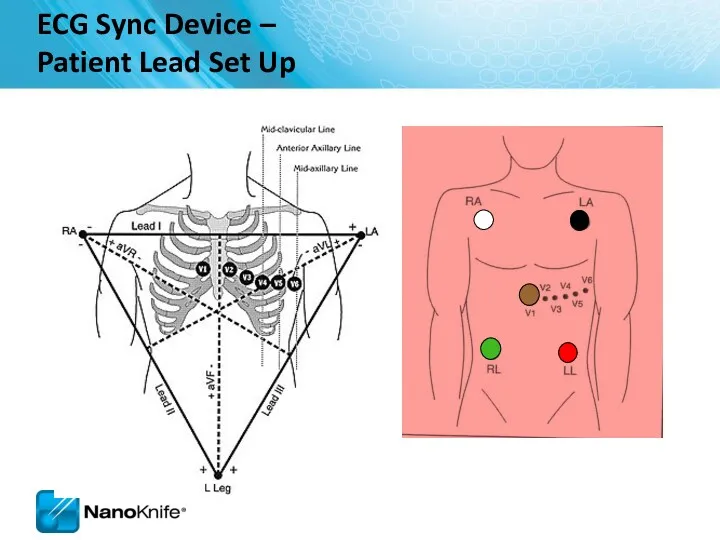
- 29. Pink dots indicate R-wave output. Set delay to zero. Lead III is selected in this example
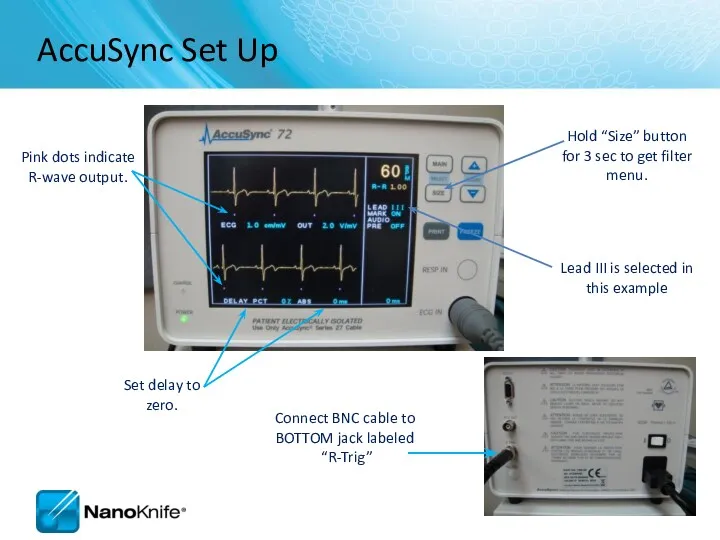
- 30. PROCEDURAL OVERVIEW
- 31. Procedure Steps – Part I Set-up AccuSync - select best lead vector Determine lesion size and
- 32. Procedure Steps – Part II Update treatment planning software with actual inter-probe measurements Re-position & Re-measure
- 33. SOFTWARE PLANNING
- 34. Getting Started Confirm the updated software is in place during start up
- 35. Information Screen There are five sections in the Information screen 1 2 3 4 5
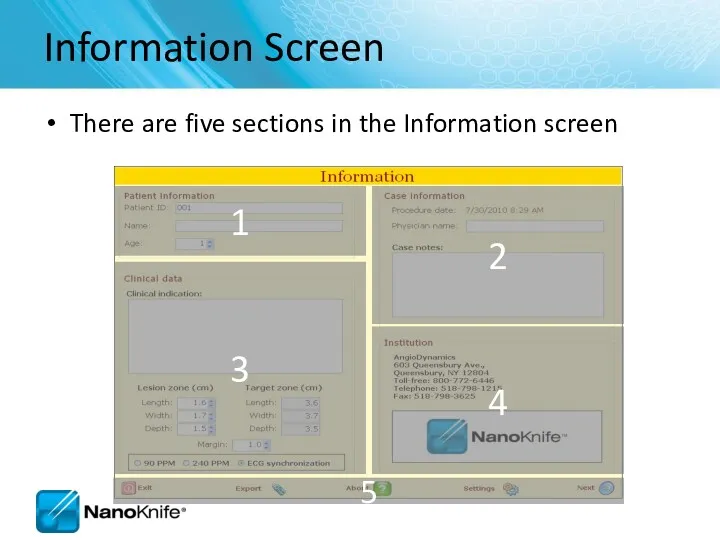
- 36. Patient Information
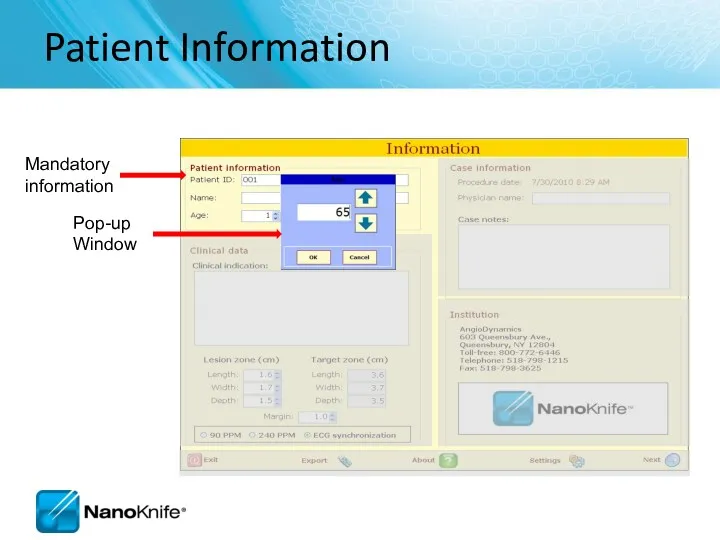
- 37. Case Information Key information about the case (e.g. type of chemotherapy they completed etc. ) Auto
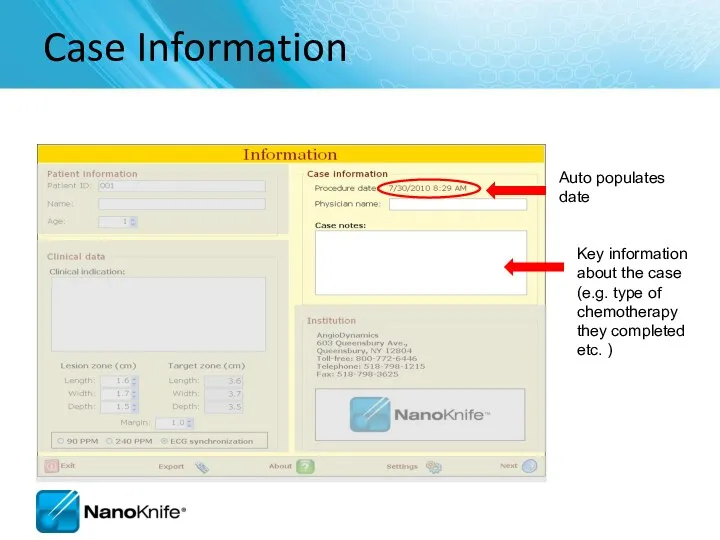
- 38. Clinical Data Enter lesion type Enter dimensions
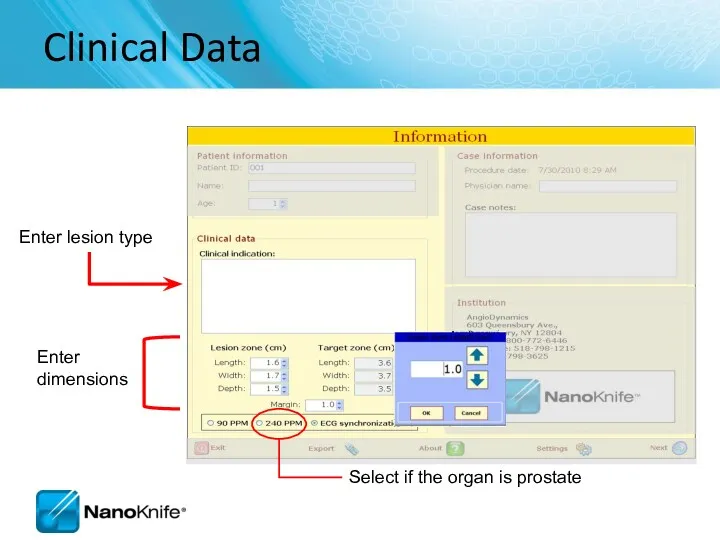
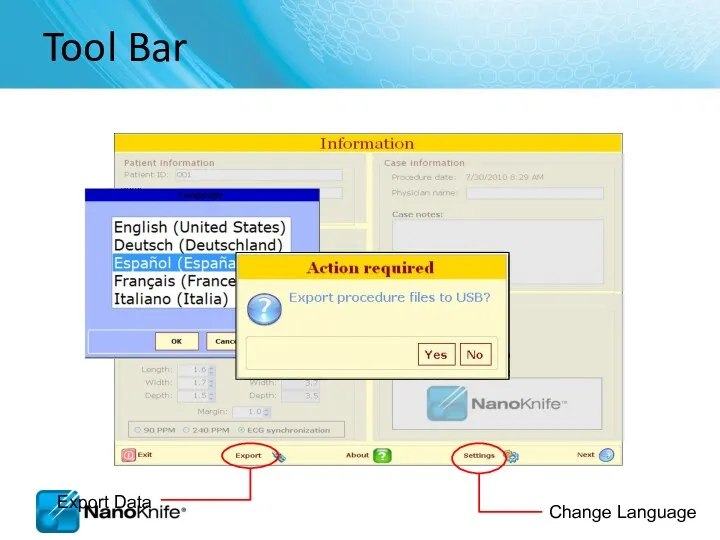
- 39. Tool Bar
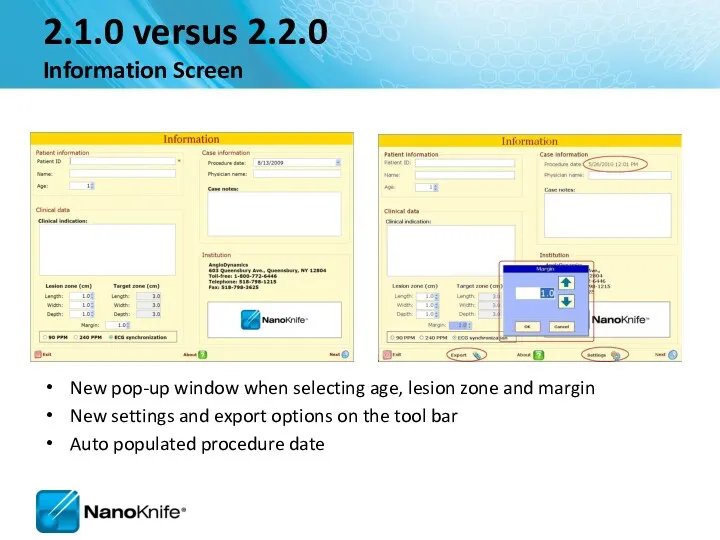
- 40. 2.1.0 versus 2.2.0 Information Screen New pop-up window when selecting age, lesion zone and margin New
- 41. Objective: Accurately Correlate 3 Phases Probes in Tissue Probes on Grid Plot Probes in Cross Sectional
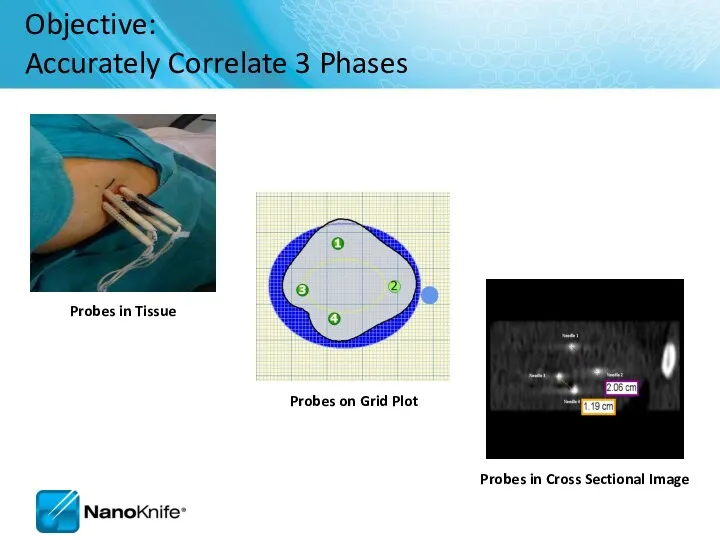
- 42. Labeling Length, Width, Depth Width and Depth Orientation Change with Anatomical Approach 1.5 x 3.0 x
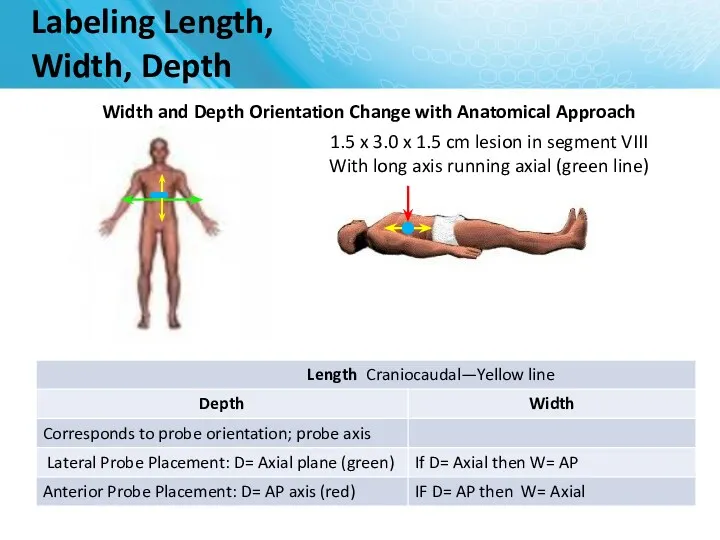
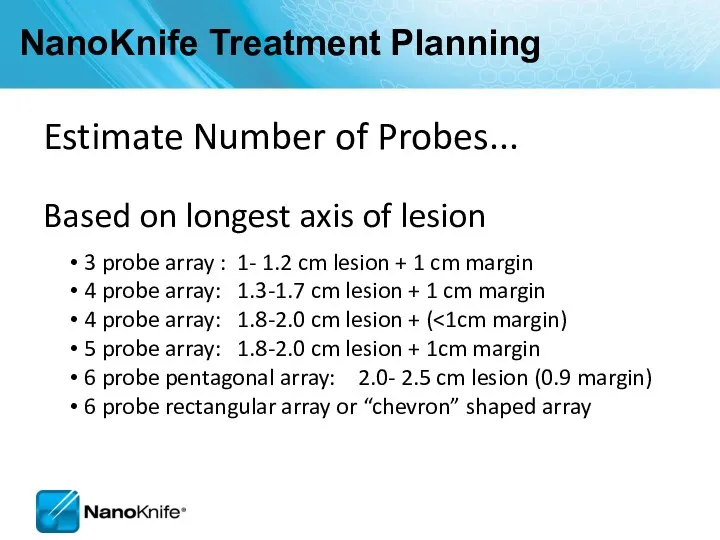
- 43. NanoKnife Treatment Planning Estimate Number of Probes... Based on longest axis of lesion 3 probe array
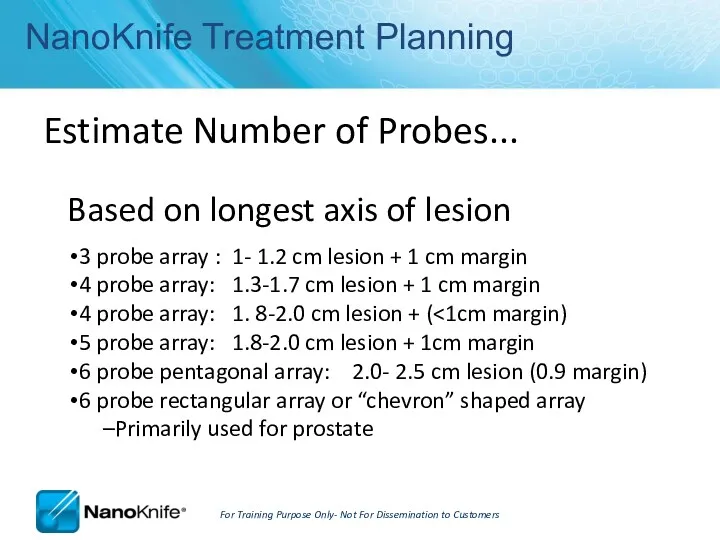
- 44. Electrode Positioning Flexible – customize to lesion size using 2 to 6 electrodes 0.5 to 2.0
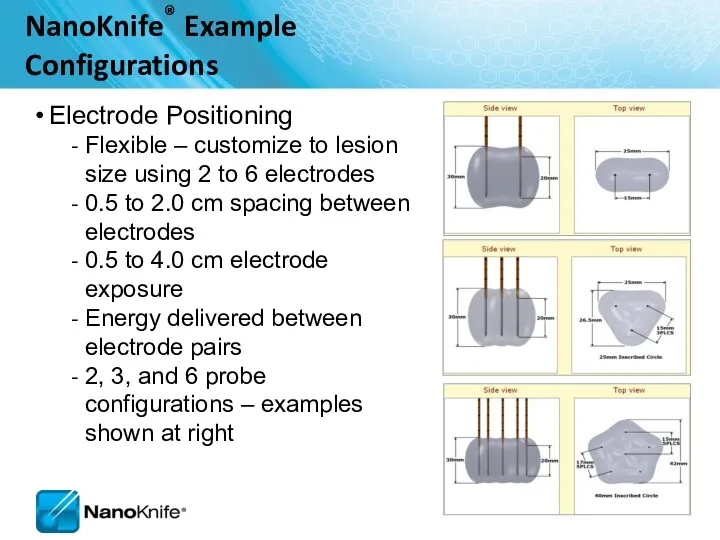
- 45. Probe Selection Screen
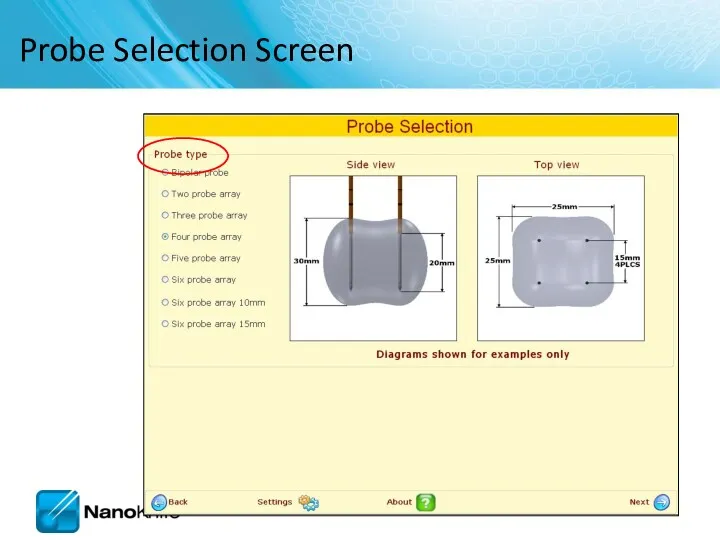
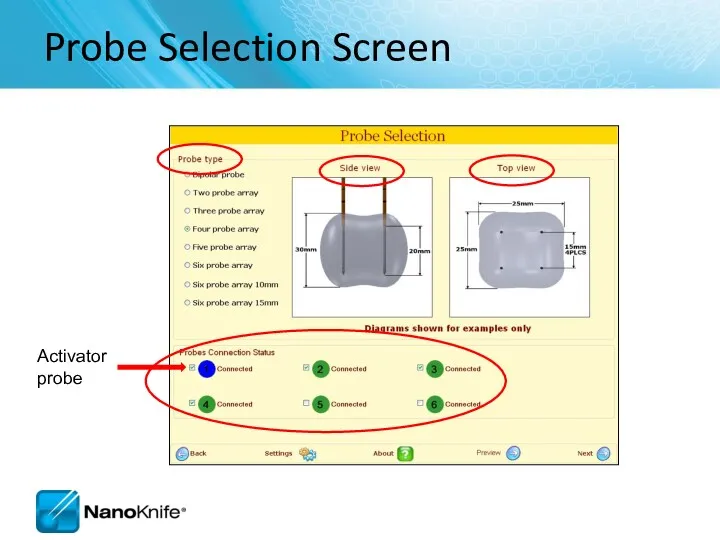
- 46. Probe Selection Screen
- 47. 2.1.0 versus 2.2.0 Probe Selection Screen RFID probes identified Activator probe is indicated as blue Standard
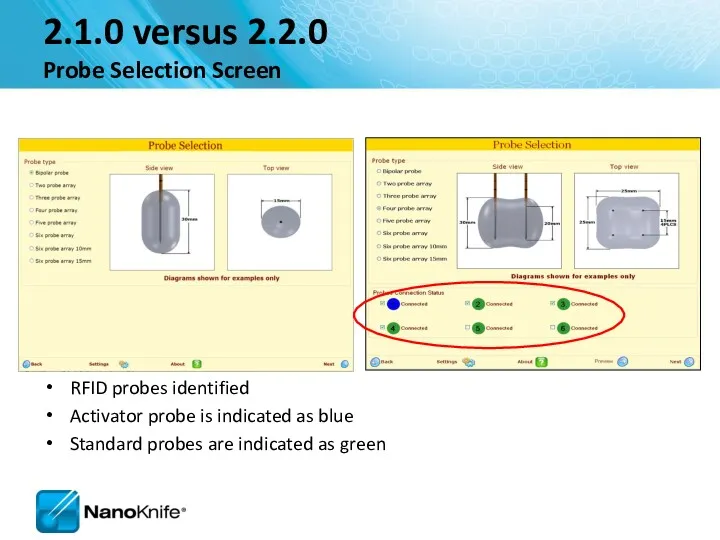
- 48. Probe Placement Grid Probe icons Probe Exposure notated here
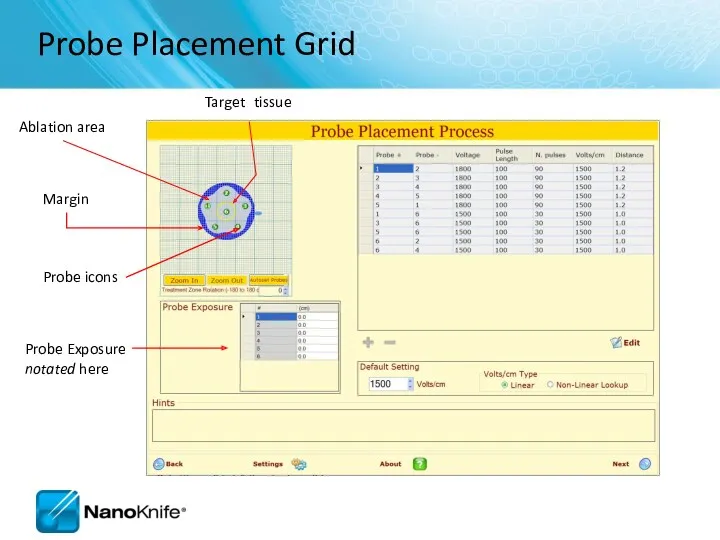
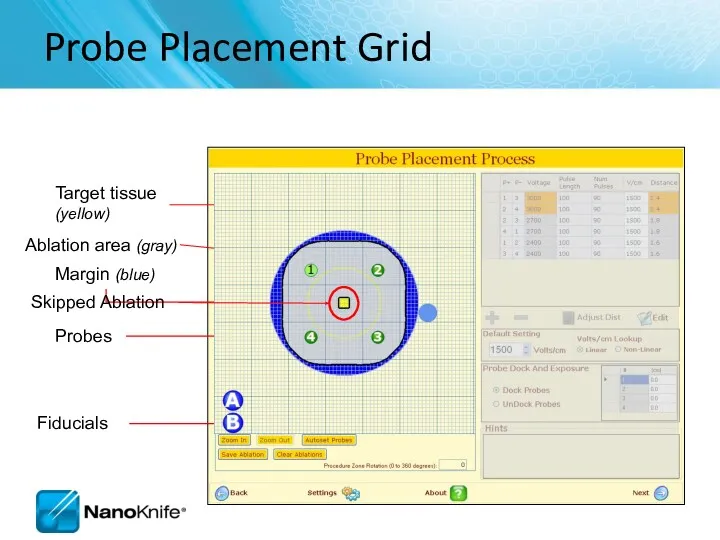
- 49. Head Orient Grid to Anatomical Approach Anterior Probe Placement into 1.5 x 3.0 x 1.5 lesion
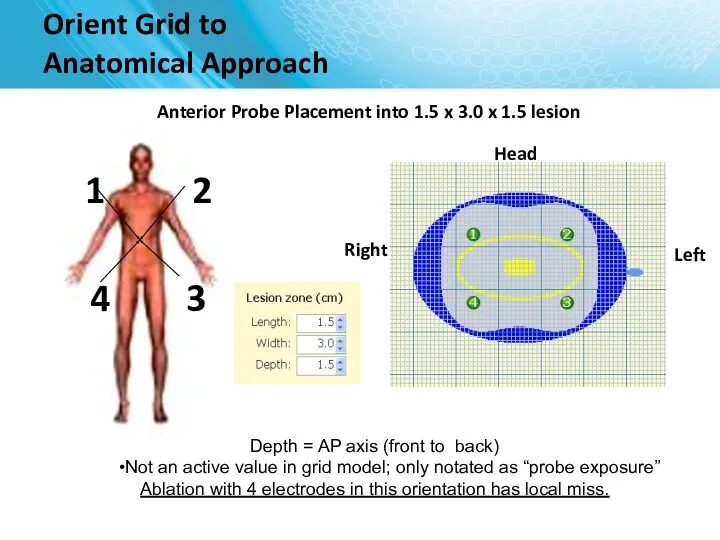
- 50. Orient Grid to Anatomical Approach Head Lateral Probe Placement 1.5 x 3.0 x 1.5 lesion Depth
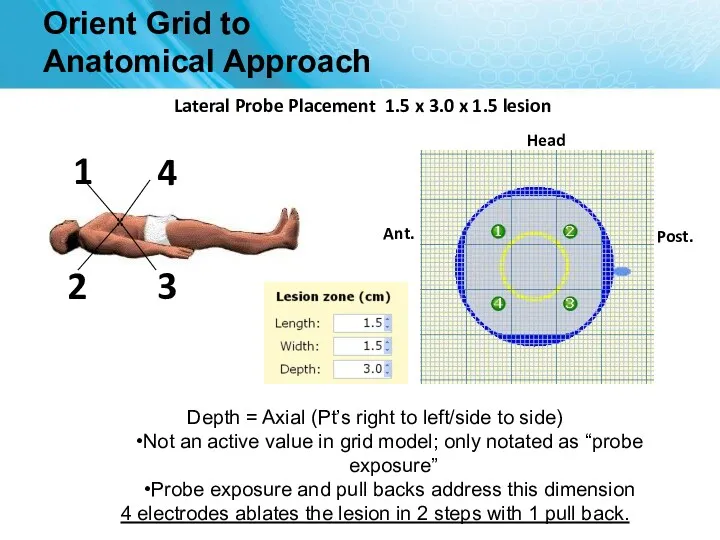
- 51. Probe Placement Process Screen 1 2 3 4 5
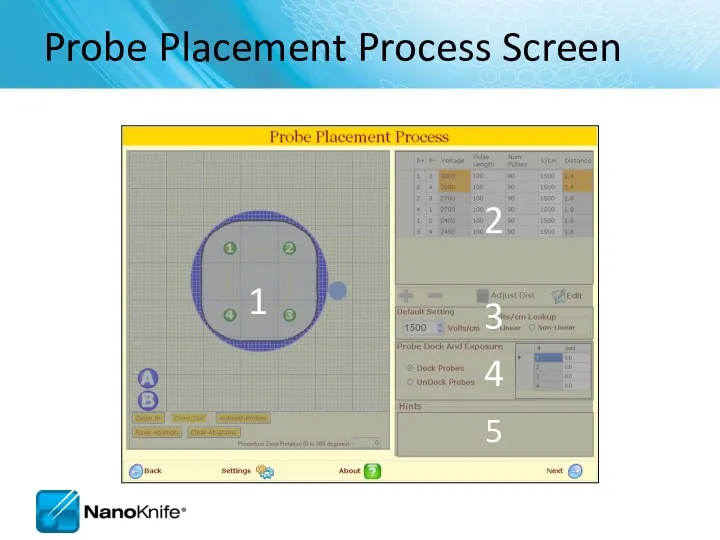
- 52. Probe Placement Grid Probes Target tissue (yellow) Ablation area (gray) Fiducials Skipped Ablation
- 53. Probe Placement Grid Save initial set up Clear ablations
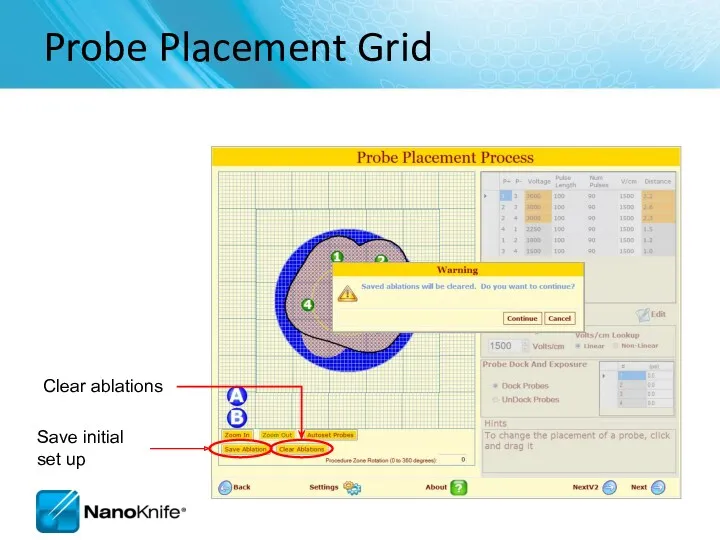
- 54. Ablation Spreadsheet Enter probe distances and have them automatically placed on the grid
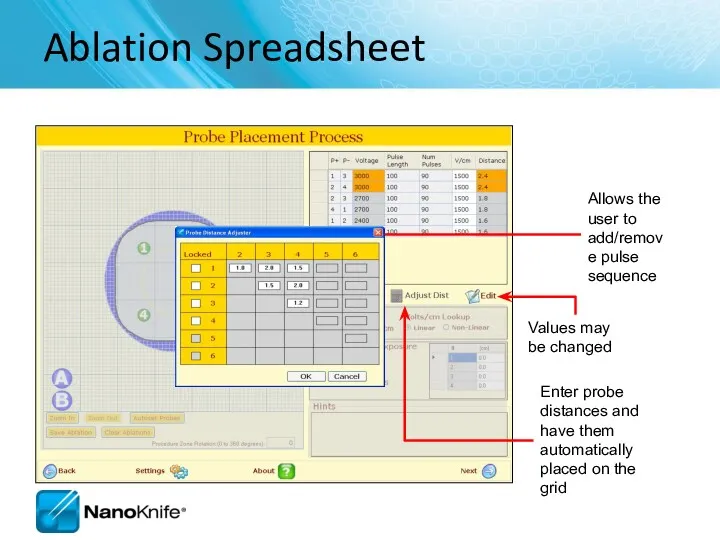
- 55. Adjusting Voltage Change setting to obtain required Volts/cm
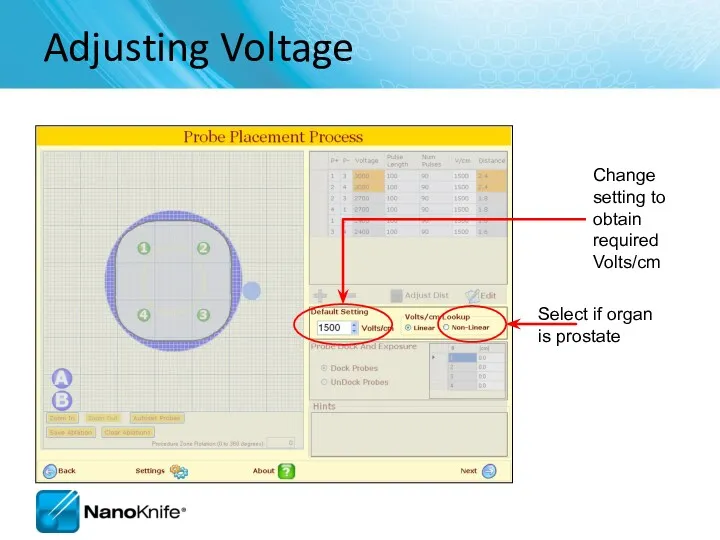
- 56. Probe Dock and Exposure Table Disconnect / reconnect the probes from the Generator
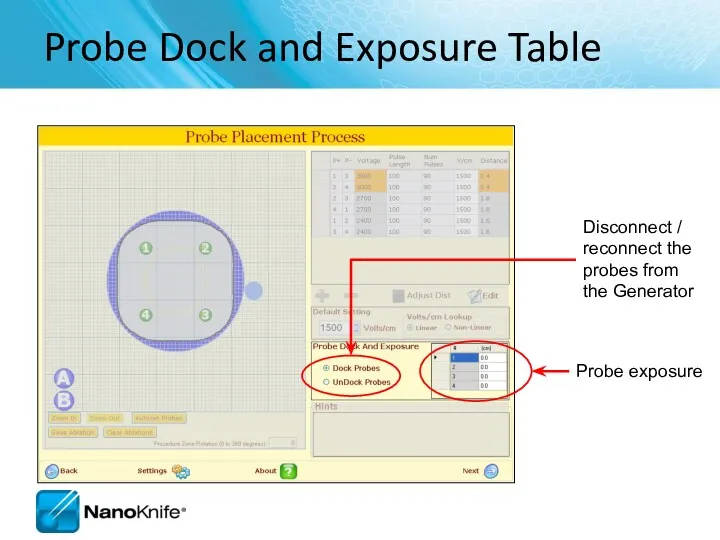
- 57. Hint Box Hints box provides additional instructions
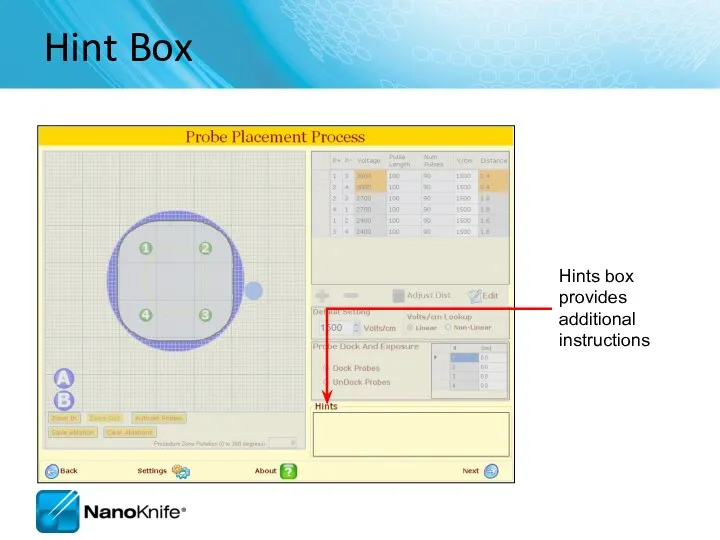
- 58. 2.1.0 versus 2.2.0 Probe Placement Screen Probe Placement Grid is larger Skipped lesions identified Overlapping Ablation
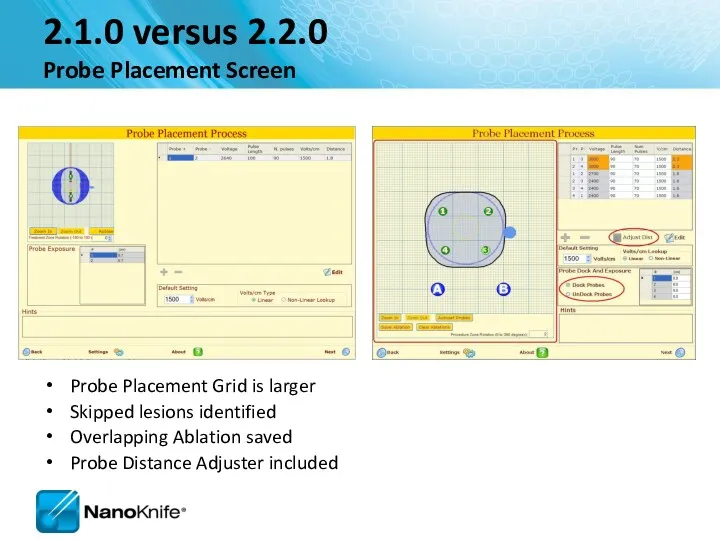
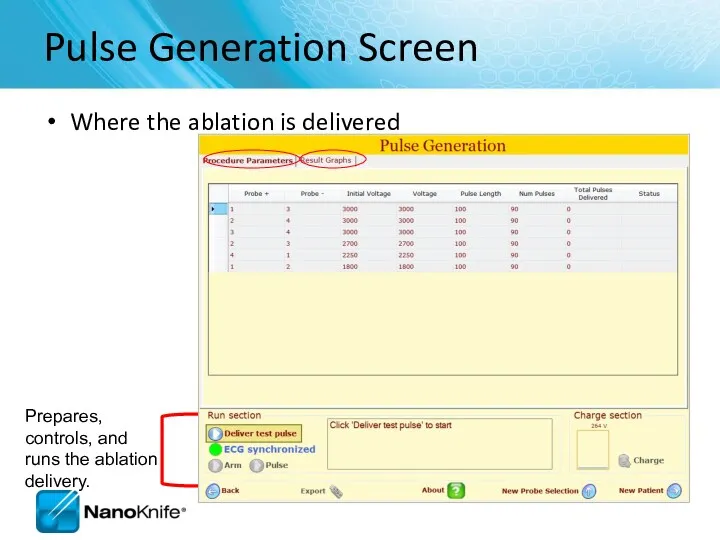
- 59. Pulse Generation Screen Where the ablation is delivered
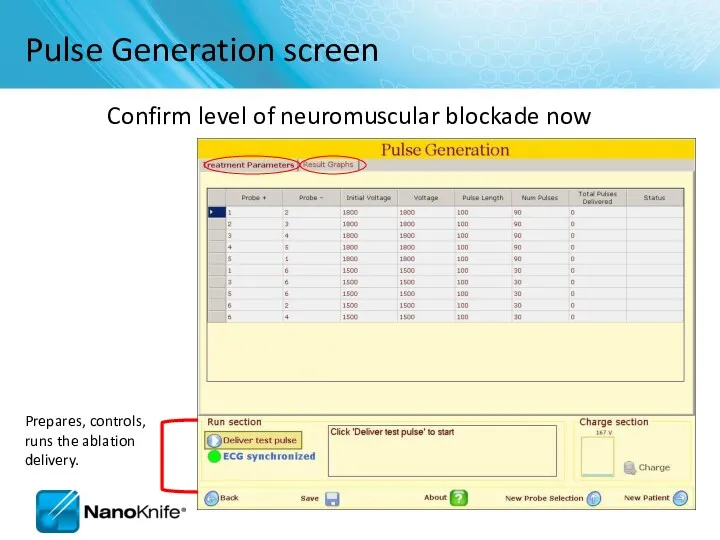
- 60. If unsuccessful, the system will guide the user to check the probe connections to ensure they
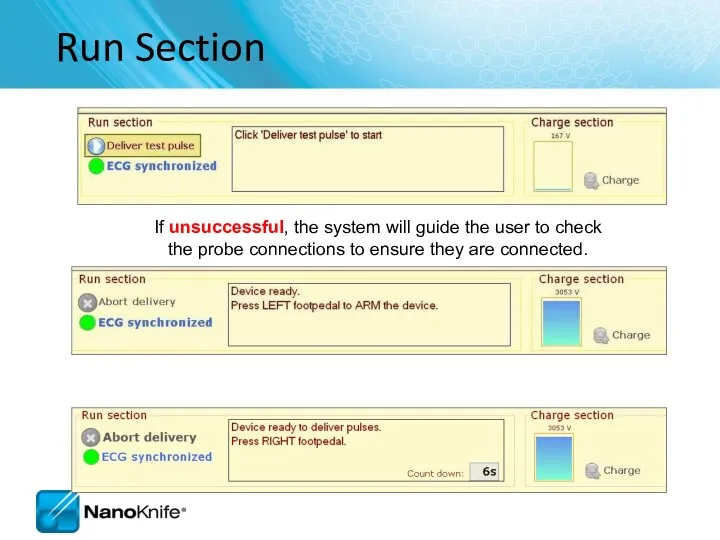
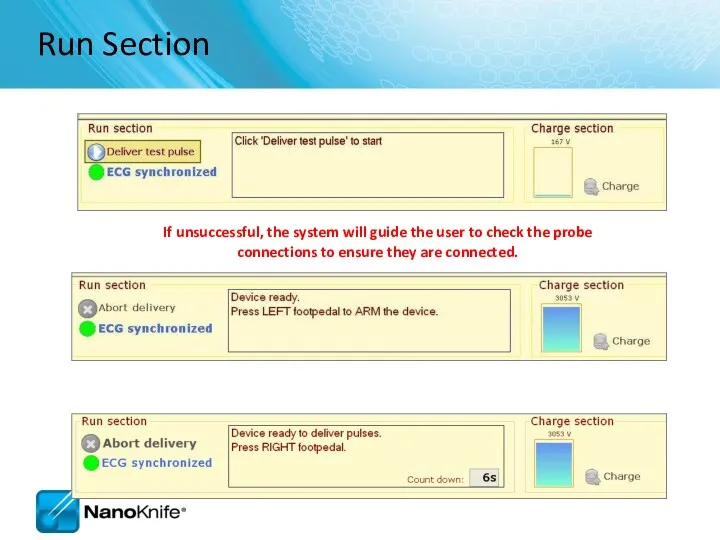
- 61. 2.1.0 versus 2.2.0 Pulse Generation Screen Different progress bar Export button available
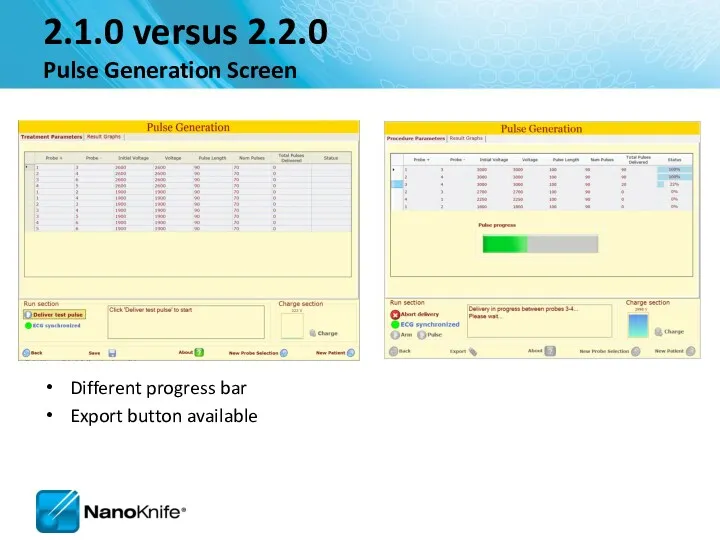
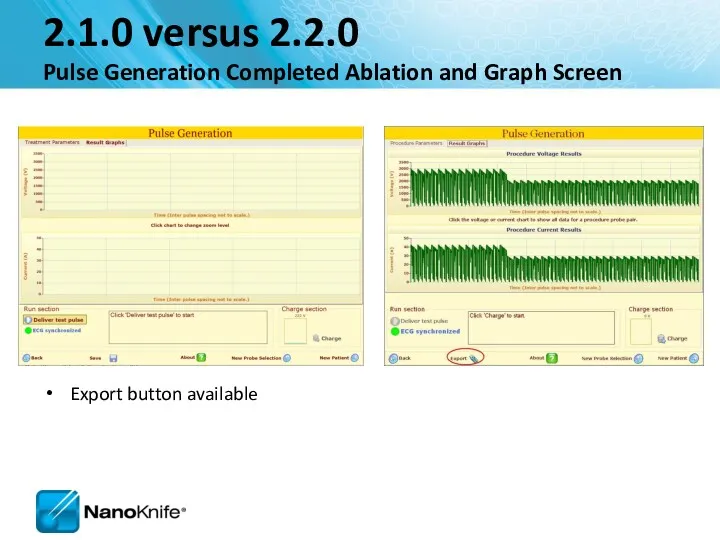
- 62. Ablation Delivery Completed
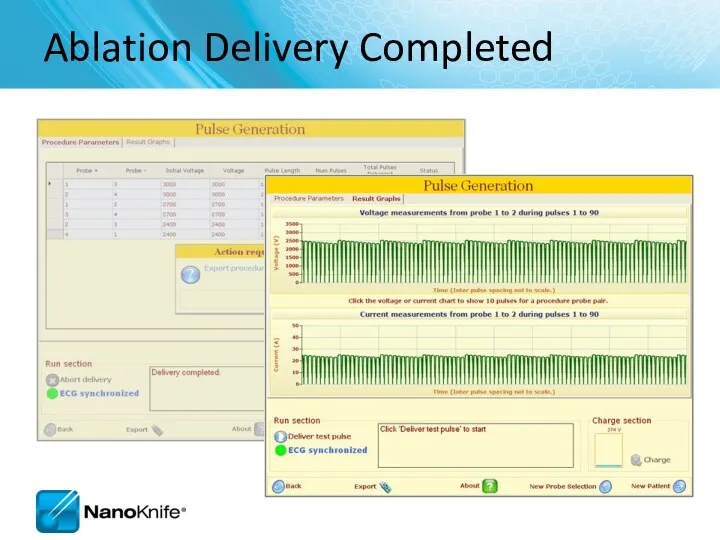
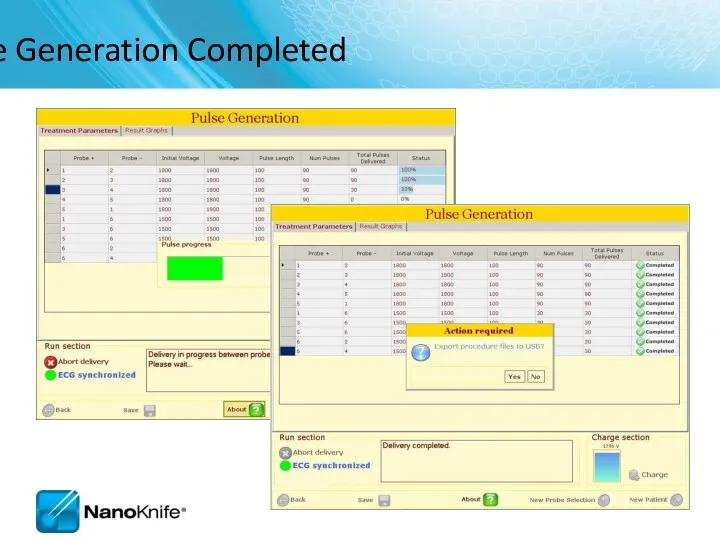
- 63. 2.1.0 versus 2.2.0 Pulse Generation Completed Ablation and Graph Screen Export button available
- 64. Pulse Generation screen Confirm level of neuromuscular blockade now
- 65. Run Section If unsuccessful, the system will guide the user to check the probe connections to
- 66. Four Probe Ablation Sequence 1 2 3 4
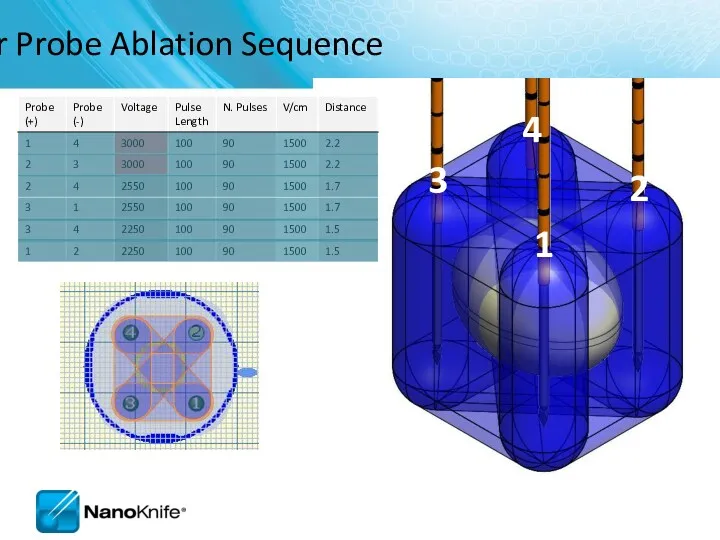
- 67. Pulse Generation Completed
- 68. View Results Graph
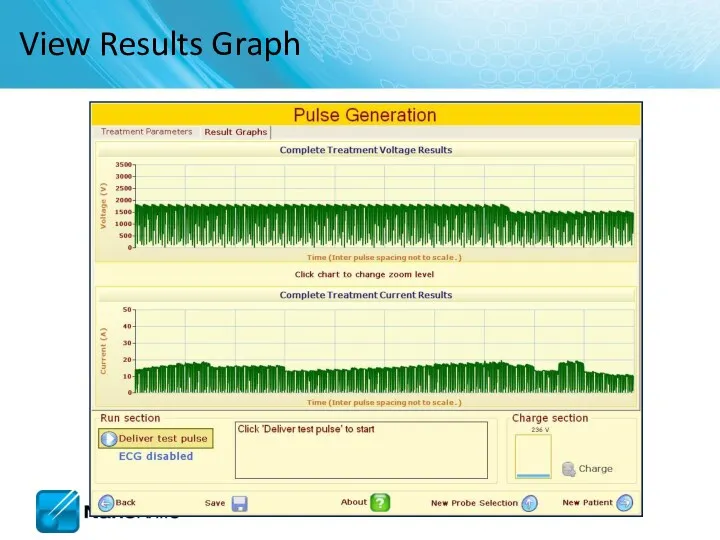
- 69. NANOKNIFE TREATMENT PLANNING – PRACTICAL CONSIDERATIONS USING 2.1.0 LESION ESTIMATOR For Training Purpose Only- Not For
- 70. Target organs Liver Pancreas Lung Kidney Manageable starting points Endophytic lesions ≤ 2cm Single probe groupings
- 71. NanoKnife Treatment Planning Estimate Number of Probes... Based on longest axis of lesion 3 probe array
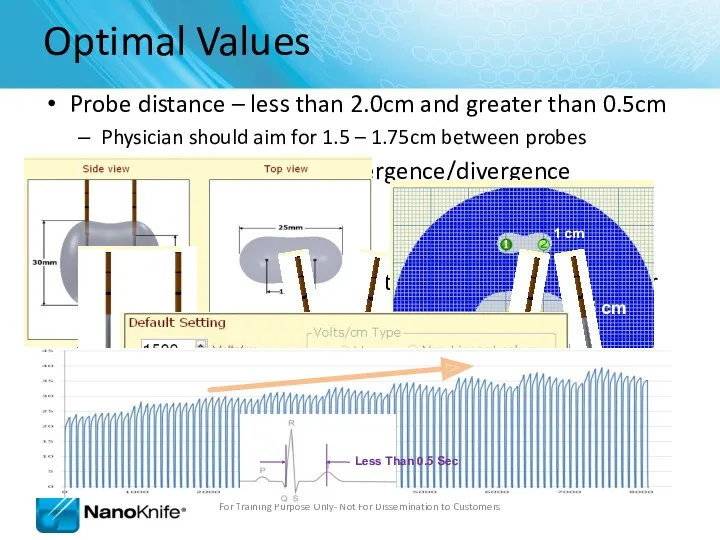
- 72. Keep electrodes parallel Avoid convergence Tips are closer together Avoid divergence Tips are further apart Equal
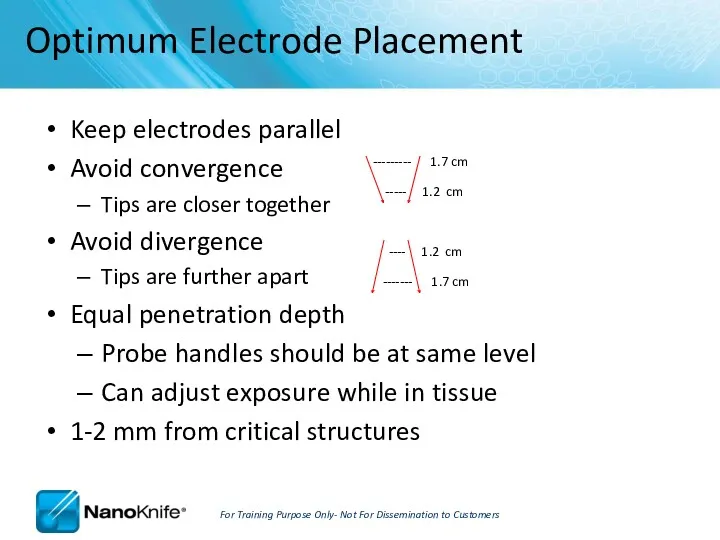
- 73. Optimum Placement Parameters For Training Purpose Only- Not For Dissemination to Customers
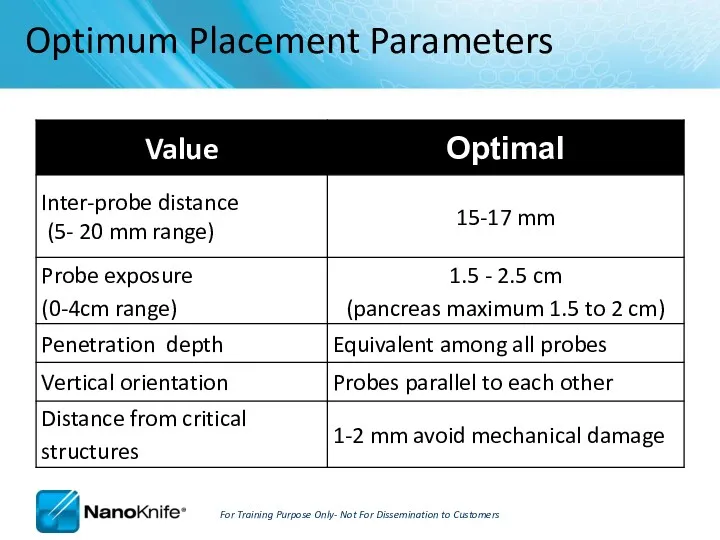
- 74. Treatment Planning Parameters For Training Purpose Only- Not For Dissemination to Customers
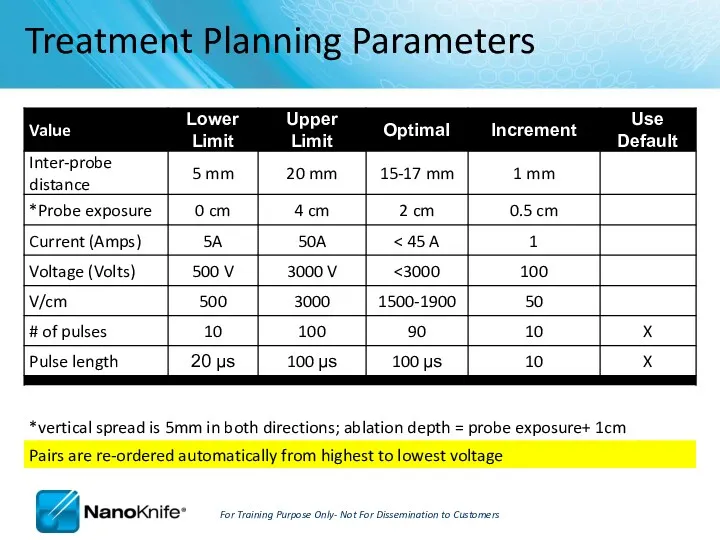
- 75. How can you tell if you got an effective treatment? Short answer: There are no certain
- 76. Hydrolysis is the dissociation of water molecules A ‘muffled’ sound during pulses is common and benign
- 77. It’s always a good idea to… RE-IMAGE when probe placement, inter-probe distance or relative ablation zone
- 78. Liver Good starting place Possibility for combined treatment on larger lesions (IRE at/near critical structures +
- 79. Kidney Very conductive ( draws 20-23 Amps) 2-2.5 max probe exposure Pulses into adrenal gland can
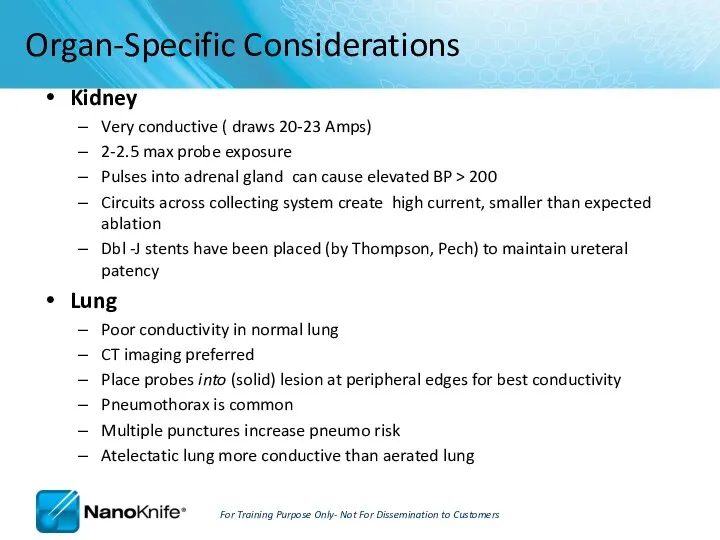
- 80. Procedure Tips, Tricks, and Troubleshooting September 16, 2010
- 81. Learning Objectives NanoKnife Set-Up AccuSync 72 Set-Up ECG Synchronized Pulse Delivery Proper Sync Function ECG Sync
- 82. NanoKnife Set-Up The power button is located on the back panel of the generator. This is
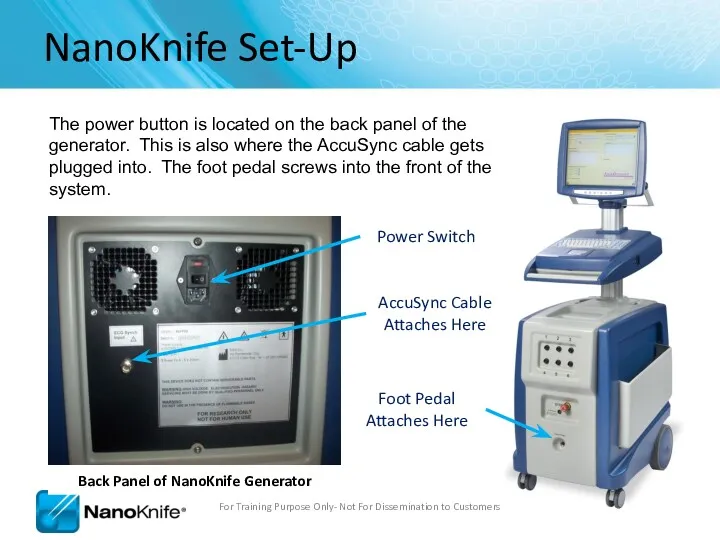
- 83. Demo Mode In the event the system boots in demo mode, check to make sure the
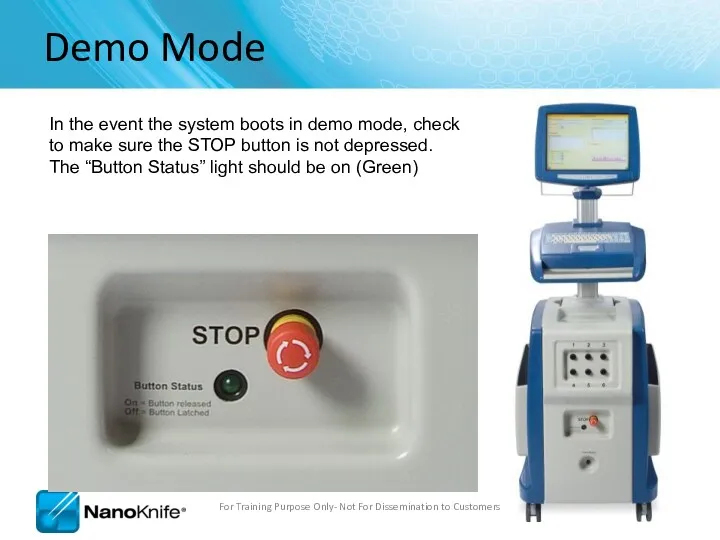
- 84. Power Switch Patient Leads AccuSync Set-Up For Training Purpose Only- Not For Dissemination to Customers
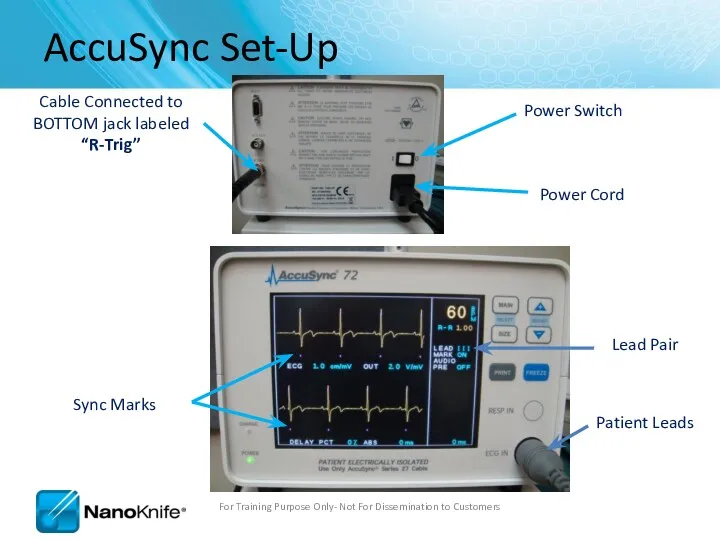
- 85. AccuSync Set Up For Training Purpose Only- Not For Dissemination to Customers Recommend attaching AccuSync Leads
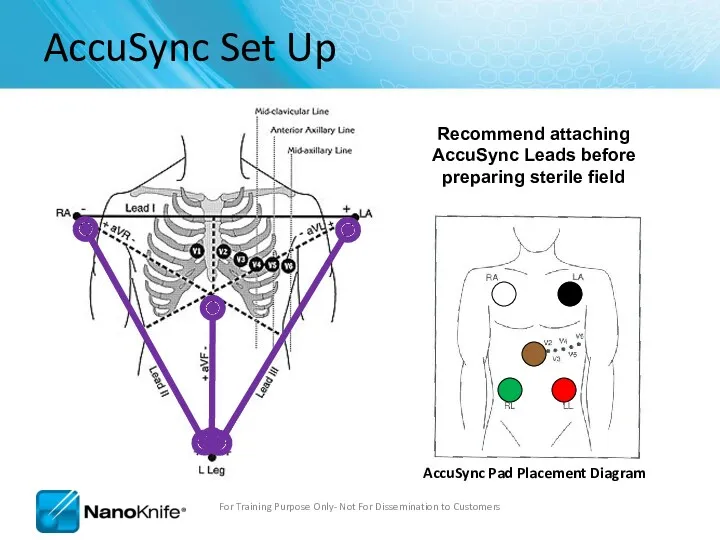
- 86. Software with AccuSync The generator will start in ECG Synchronization mode (default setting) You won’t be
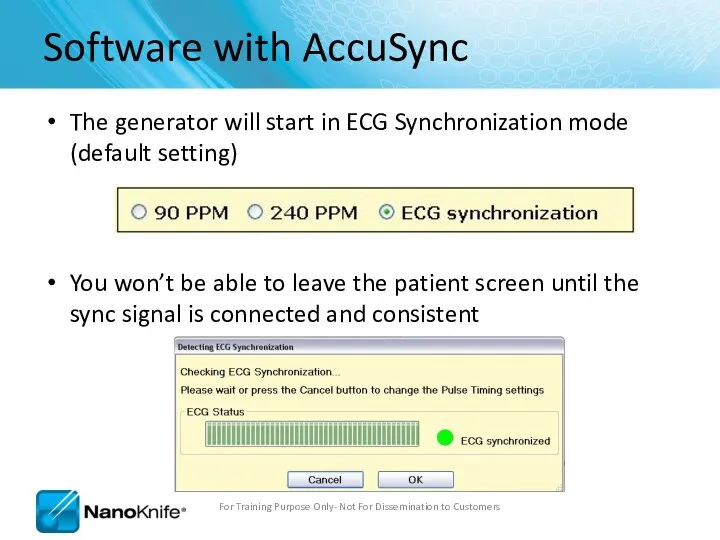
- 87. Select 2-3 leads with the Biggest R wave and smallest T wave Tip: Use same lead
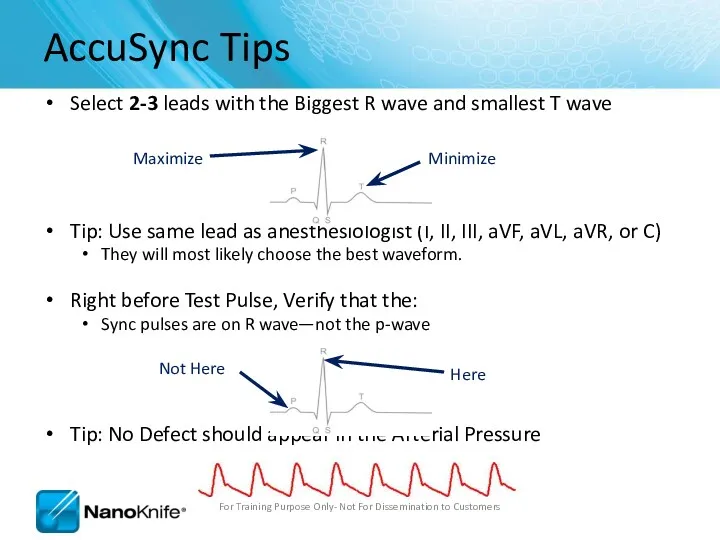
- 88. ECG Synchronized Pulse Delivery Sync device (e.g. AccuSync 72) senses the rising slope of the R-wave,
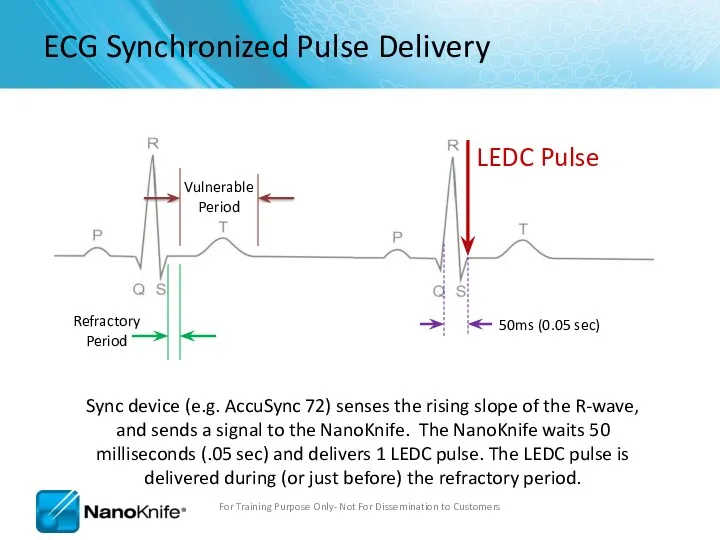
- 89. No Saturation For Training Purpose Only- Not For Dissemination to Customers
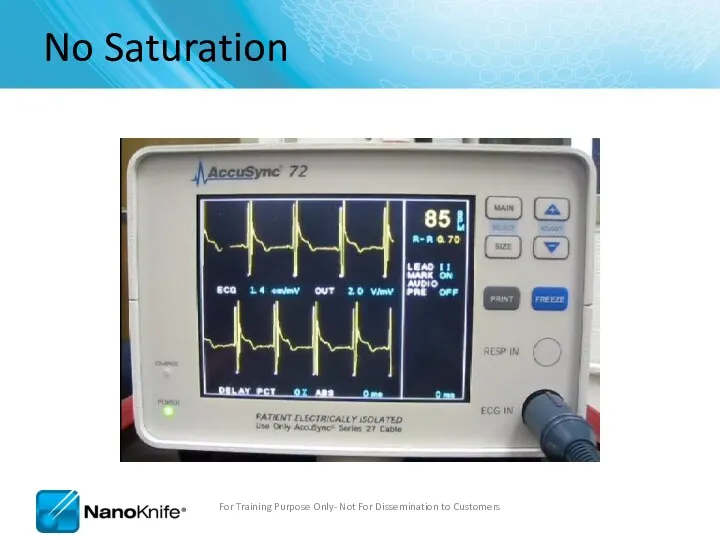
- 90. Heavy Saturation Recommend changing lead pair to resolve saturation For Training Purpose Only- Not For Dissemination
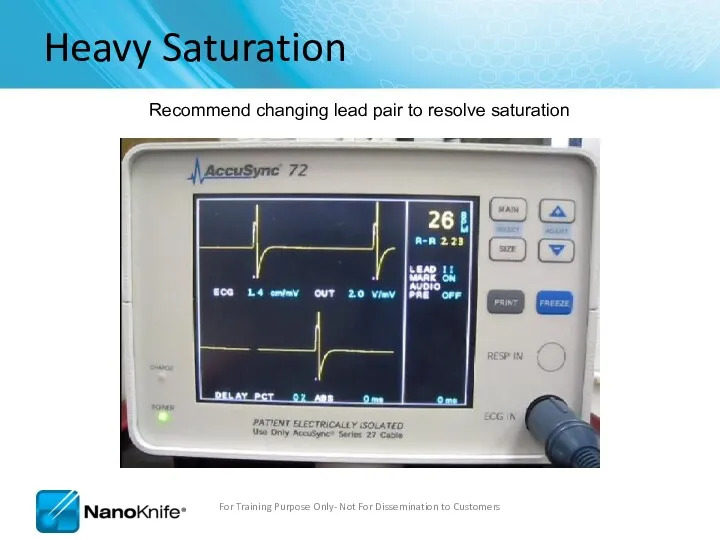
- 91. Trouble Shooting Saturation Remove the BNC Cable from the back of the AccuSync Box For Training
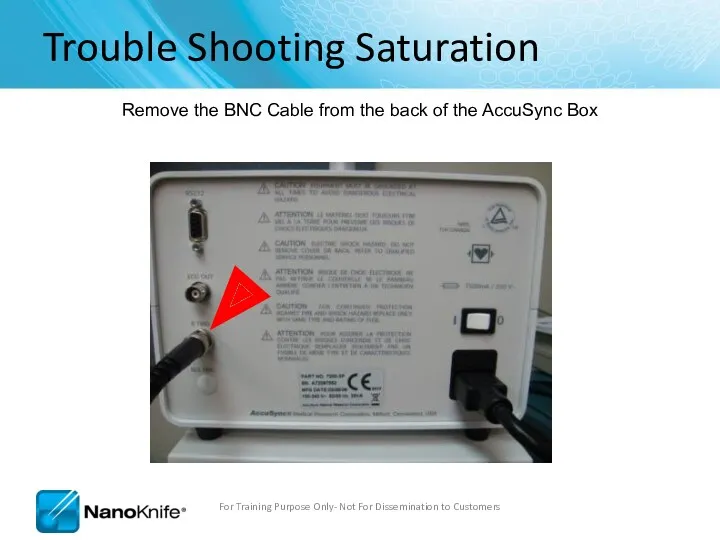
- 92. Trouble Shooting Saturation Warning Message will Appear on Generator Screen For Training Purpose Only- Not For
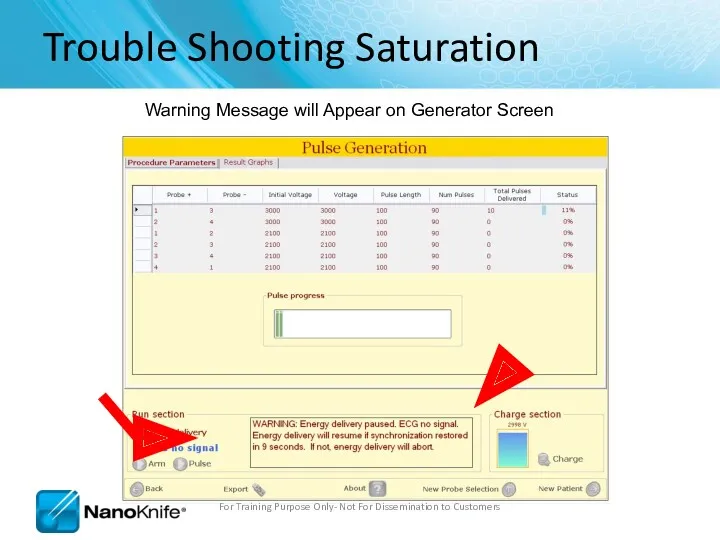
- 93. Trouble Shooting Saturation After 15 seconds, a new window appears giving you 120 seconds before the
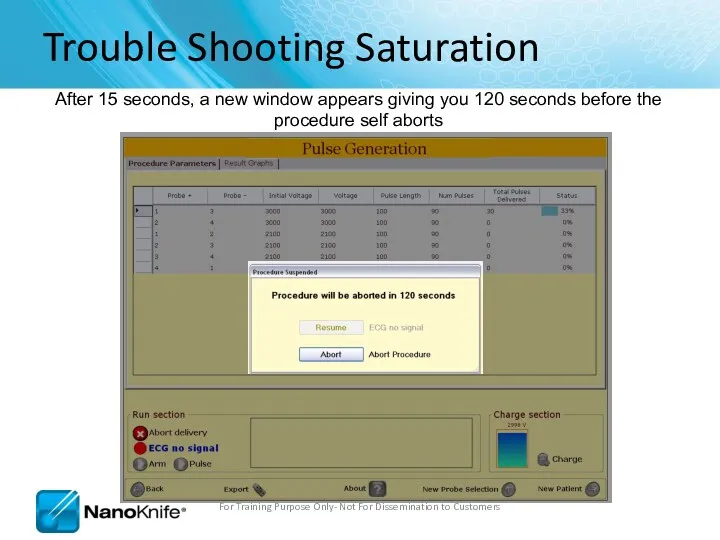
- 94. Trouble Shooting Saturation Press the “MAIN” button. (just tap it, don’t hold it down) For Training
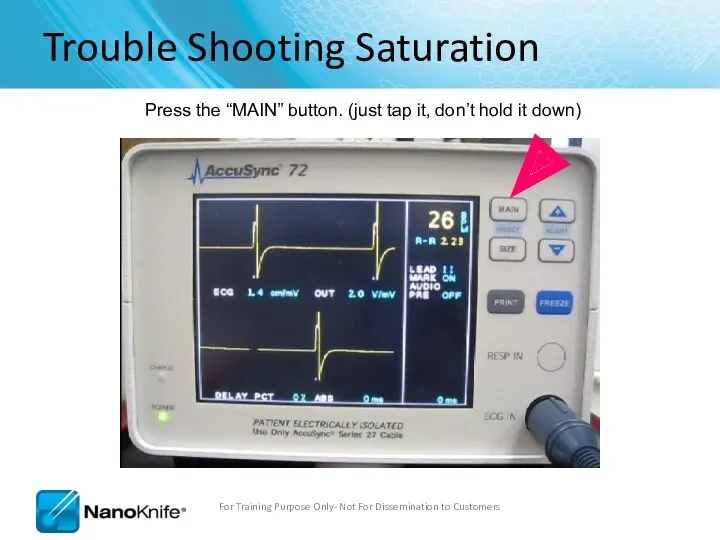
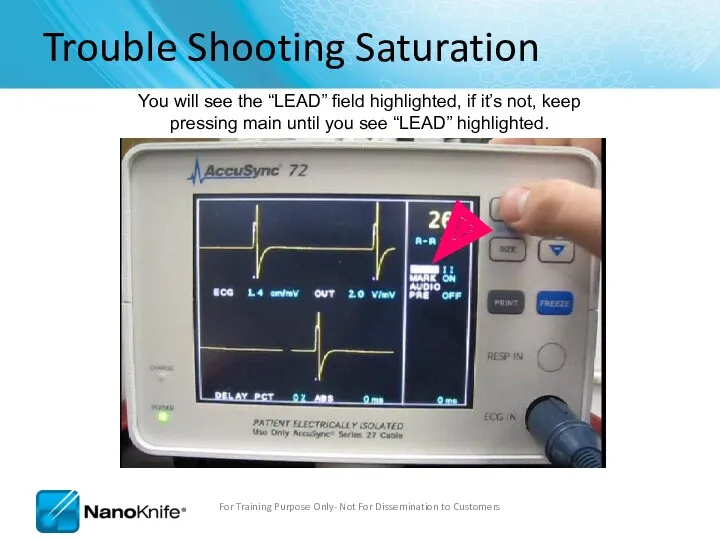
- 95. Trouble Shooting Saturation You will see the “LEAD” field highlighted, if it’s not, keep pressing main
- 96. Trouble Shooting Saturation Then press the “+” or “-” arrow to change the lead pair. (Remember,
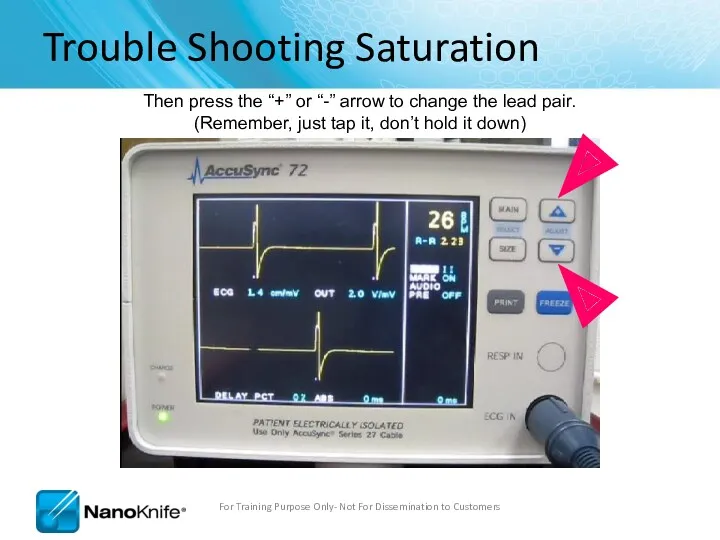
- 97. Trouble Shooting Saturation This will change the lead pair. Pressing “+”/UP arrow goes to lead III
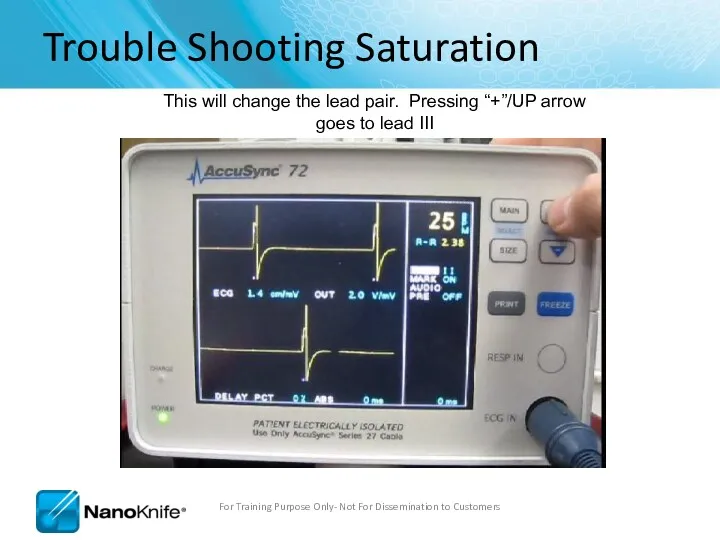
- 98. Trouble Shooting Saturation After a second or two, you can start to see nice waveform For
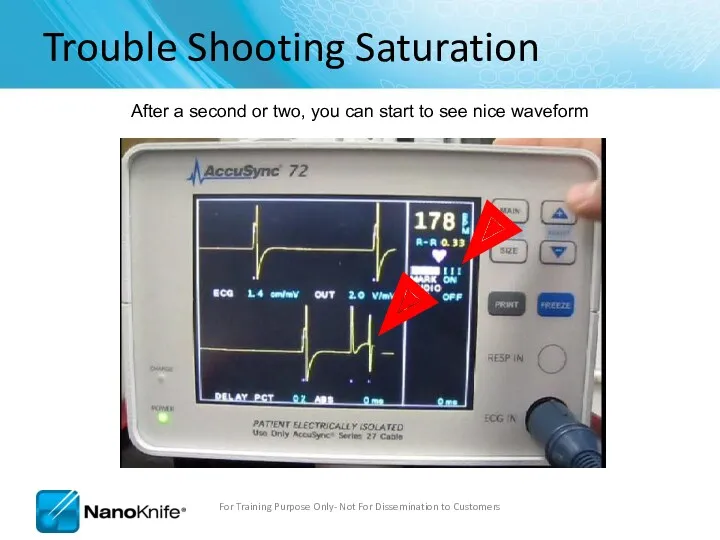
- 99. Trouble Shooting Saturation Reattach the BNC Cable to the back of the AccuSync Box After verifying
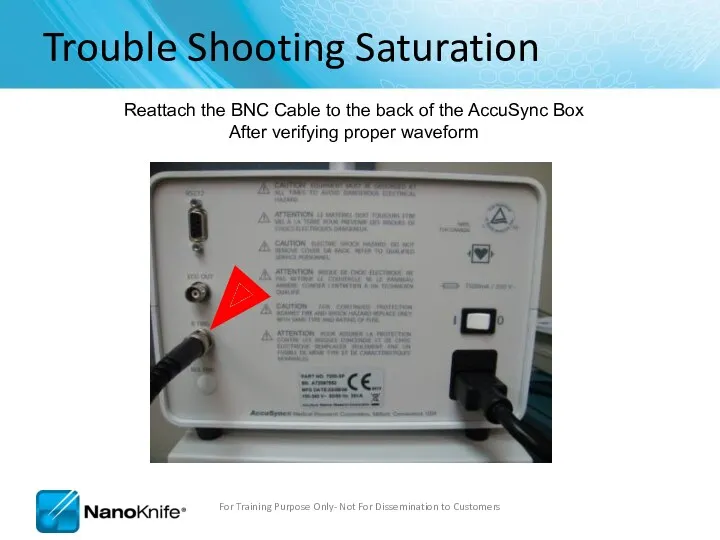
- 100. Trouble Shooting Saturation Clicking Resume will continue the treatment from where it left off. For Training
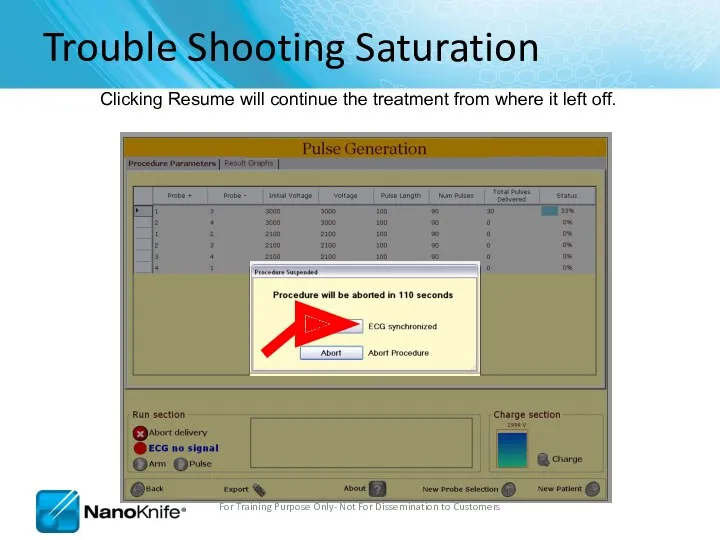
- 101. Trouble Shooting Saturation Now your treatment time will decrease! For Training Purpose Only- Not For Dissemination
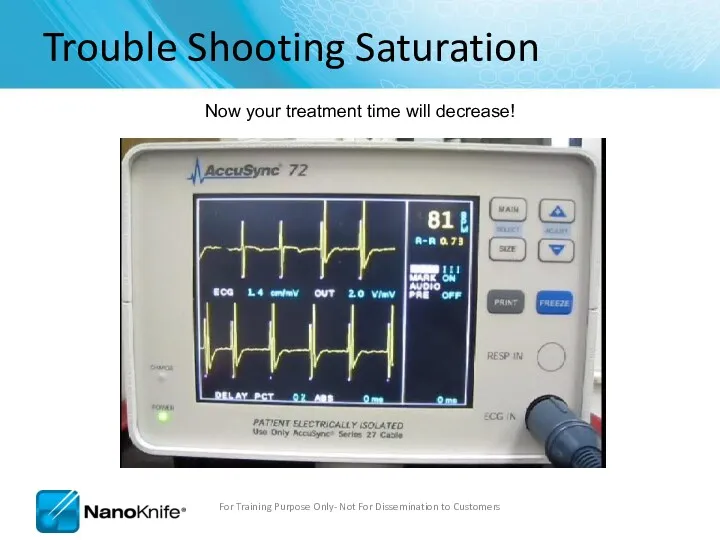
- 102. AccuSync Troubleshooting For Training Purpose Only- Not For Dissemination to Customers NanoKnife does not see sync
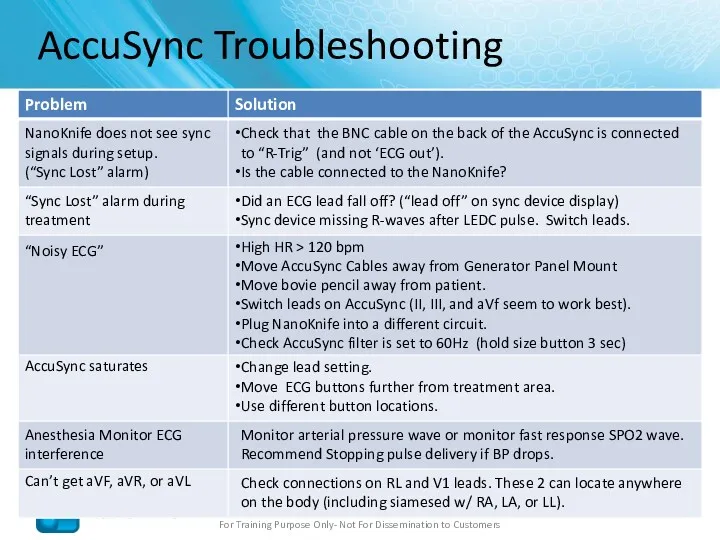
- 103. NanoKnife Troubleshooting For Training Purpose Only- Not For Dissemination to Customers NanoKnife Does not turn on
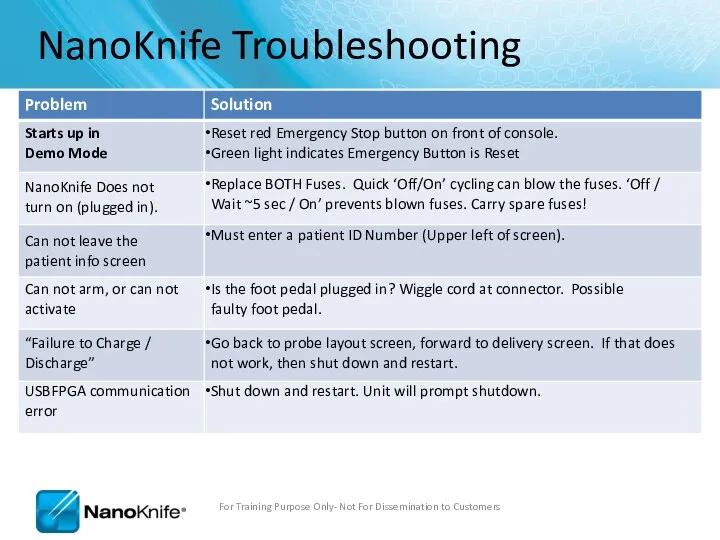
- 104. Procedure Troubleshooting Loud popping during pulse delivery; may also have over-current alarm. ** Stop ablation** Reduce
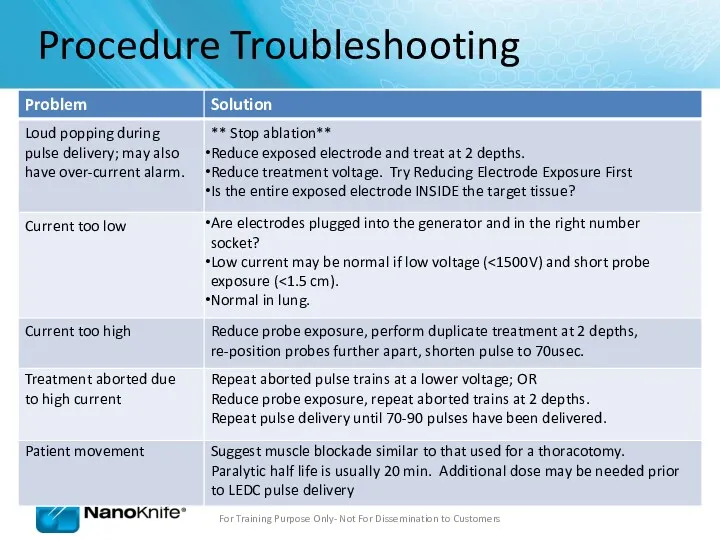
- 105. Procedure Troubleshooting Probes are migrating out during pulse delivery ** Stop ablation** Check to ensure cables
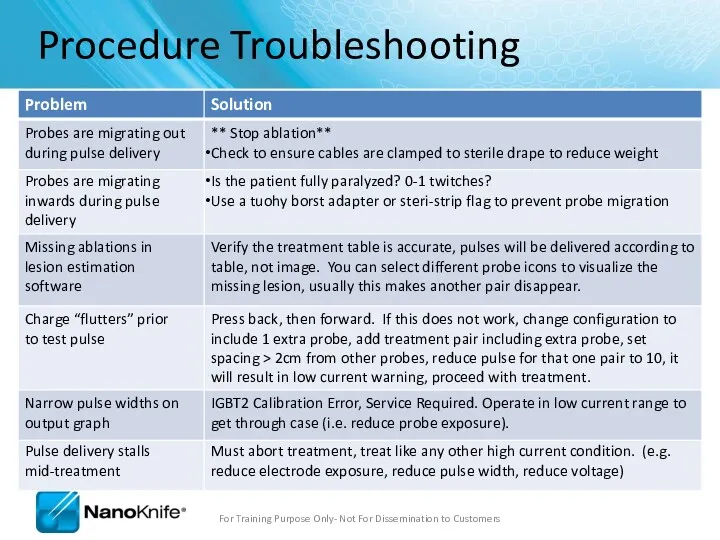
- 106. Procedure Troubleshooting Software Lags Shut down and restart system. Do this between patients to prevent this
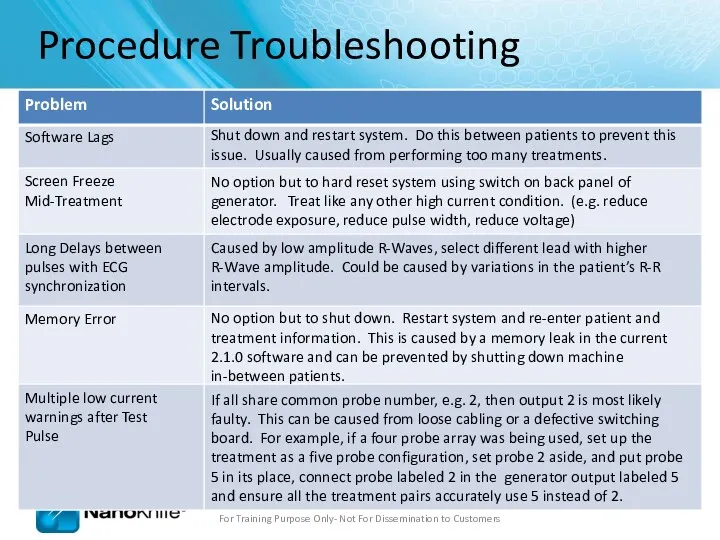
- 107. Ohms Law V=IR V= Voltage (Volts) – “The Input” R = Resistance (Ohms) - “Tissue Dependent”
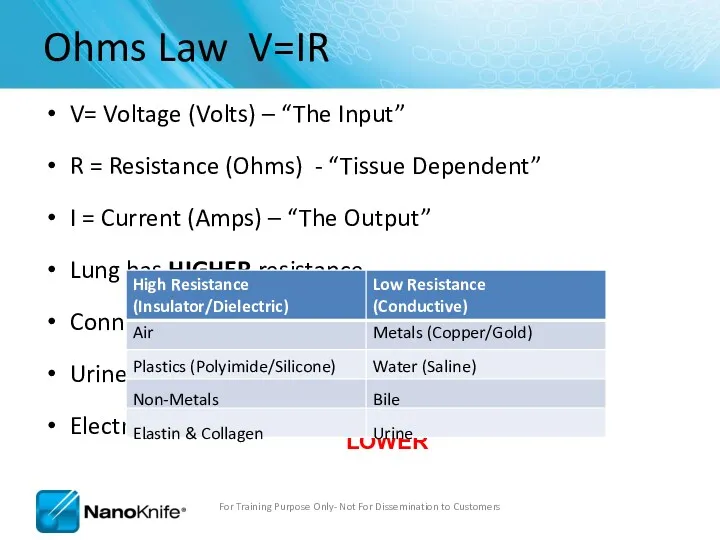
- 108. Current Output For Training Purpose Only- Not For Dissemination to Customers V = I x R
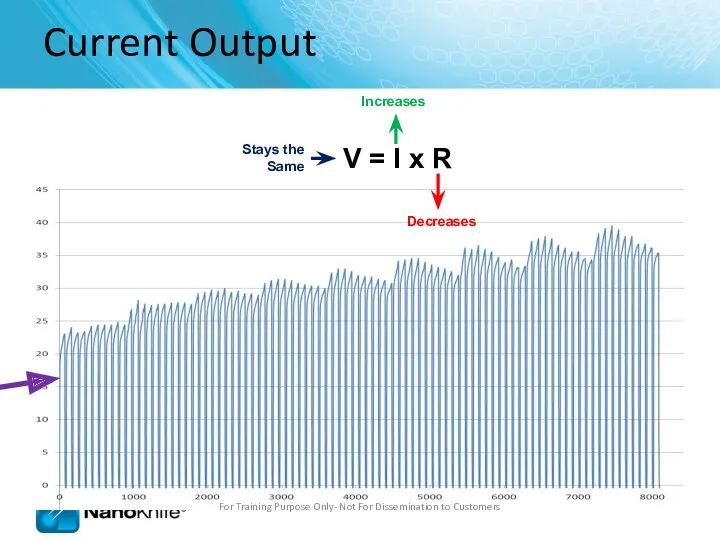
- 109. Current Output For Training Purpose Only- Not For Dissemination to Customers
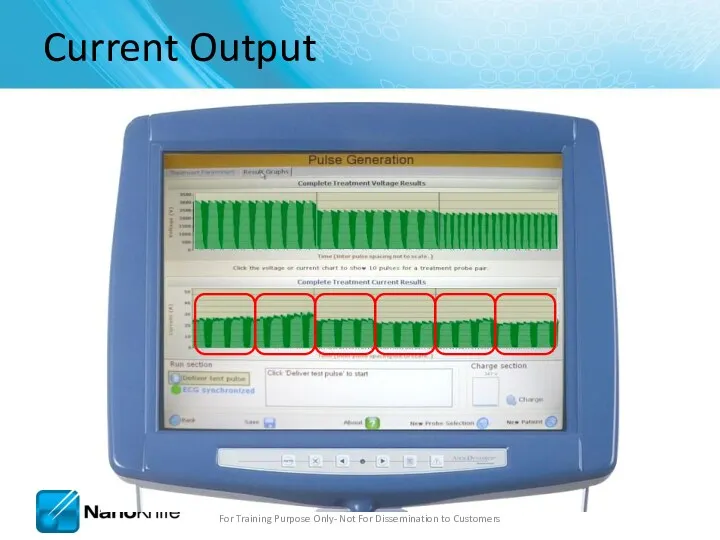
- 110. Probe distance – less than 2.0cm and greater than 0.5cm Physician should aim for 1.5 –
- 111. Review Questions What options are available to solve an over-current condition? Reduce Probe Exposure / Reduce
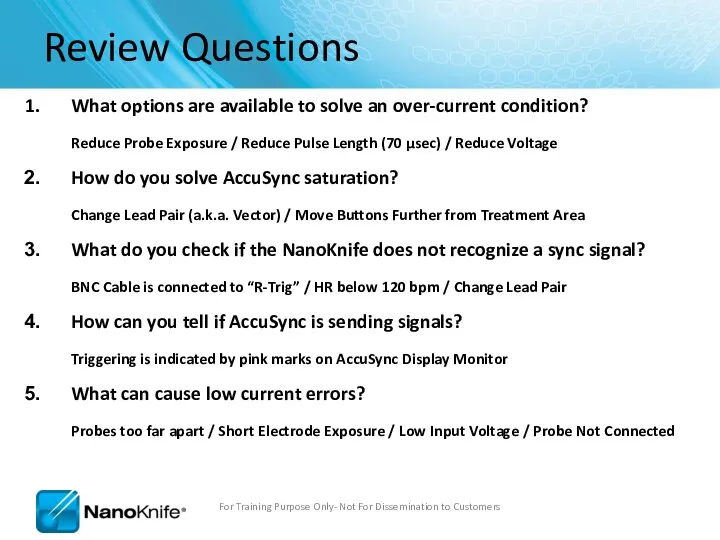
- 112. Highlights Make sure: BNC Cable is Attached to “R Trig” Pink Marks Indicates Proper Sync Output
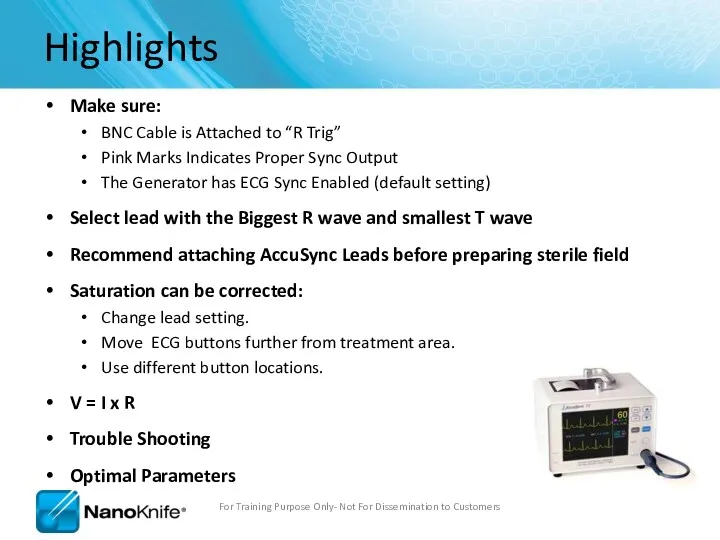
- 114. Скачать презентацию

 Медицинское обеспечение детей и подростков в образовательных организациях
Медицинское обеспечение детей и подростков в образовательных организациях Рефлекторные синдромы шейного остеохондроза
Рефлекторные синдромы шейного остеохондроза Урогенитальный хламидиоз
Урогенитальный хламидиоз Эндокриндік жүйе
Эндокриндік жүйе Темір жетіспеушілік анемияның клиникалық көріністері
Темір жетіспеушілік анемияның клиникалық көріністері Гастроэзофагеальная рефлюксная болезнь
Гастроэзофагеальная рефлюксная болезнь Дизайны клинических исследований
Дизайны клинических исследований Гирудотерапия на современном этапе
Гирудотерапия на современном этапе Первая медицинская помощь при отравлении химическими веществами. Наиболее характерные признаки химического отравления
Первая медицинская помощь при отравлении химическими веществами. Наиболее характерные признаки химического отравления Өт шығару жолдарының ауруларымен балаларда диспансерлік бақылауды ұйымдастыру
Өт шығару жолдарының ауруларымен балаларда диспансерлік бақылауды ұйымдастыру Антиаритмические препараты. Неотложная помощь при тахи-брадиаритмиях
Антиаритмические препараты. Неотложная помощь при тахи-брадиаритмиях Опухоли зрительного нерва
Опухоли зрительного нерва Занятие для детей по оказанию первой помощи при ИМ и МИ
Занятие для детей по оказанию первой помощи при ИМ и МИ Причины и предрасполагающие факторы к возникновению рахита
Причины и предрасполагающие факторы к возникновению рахита Заболевания век, слезных органов, орбиты и конъюнктивы
Заболевания век, слезных органов, орбиты и конъюнктивы Сурфактантная терапия
Сурфактантная терапия Микрорефлексотерапия пациента с хронической обструктивной болезнью легких в стадии обострения
Микрорефлексотерапия пациента с хронической обструктивной болезнью легких в стадии обострения Инфузионная терапия
Инфузионная терапия Исследование защитных свойств зубных паст
Исследование защитных свойств зубных паст Первичные бесполостные морфологические признаки кожи
Первичные бесполостные морфологические признаки кожи Методы клинической биохимии. Контроль качества лабораторных исследований
Методы клинической биохимии. Контроль качества лабораторных исследований Будова та розвиток чоловічих і жіночих статевих органів
Будова та розвиток чоловічих і жіночих статевих органів Синдром гиперстимуляции яичников, как процедуры ЭКО
Синдром гиперстимуляции яичников, как процедуры ЭКО Первая медицинская помощь при травмах и повреждениях верхних и нижних конечностей. Занятие №2
Первая медицинская помощь при травмах и повреждениях верхних и нижних конечностей. Занятие №2 Очаговые поражения легких: дифференциальная диагностика
Очаговые поражения легких: дифференциальная диагностика Gynecological infections and abnormalities
Gynecological infections and abnormalities Предварительные и периодические медицинские осмотры работников
Предварительные и периодические медицинские осмотры работников Бейімделу физиологиясы
Бейімделу физиологиясы