Содержание
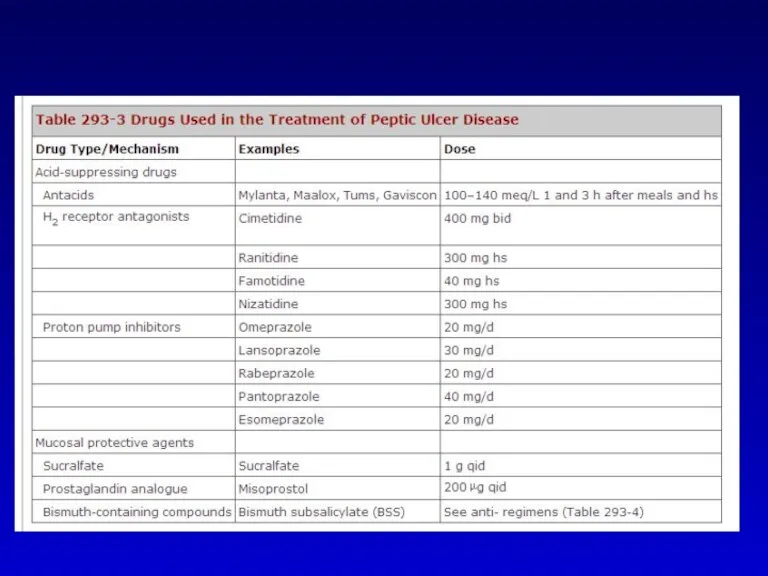
- 2. Discussion outline Definitions Risk factors Complications Clinical presentation Management – HBP, NSAIDS Refractory PUD Prophylaxis
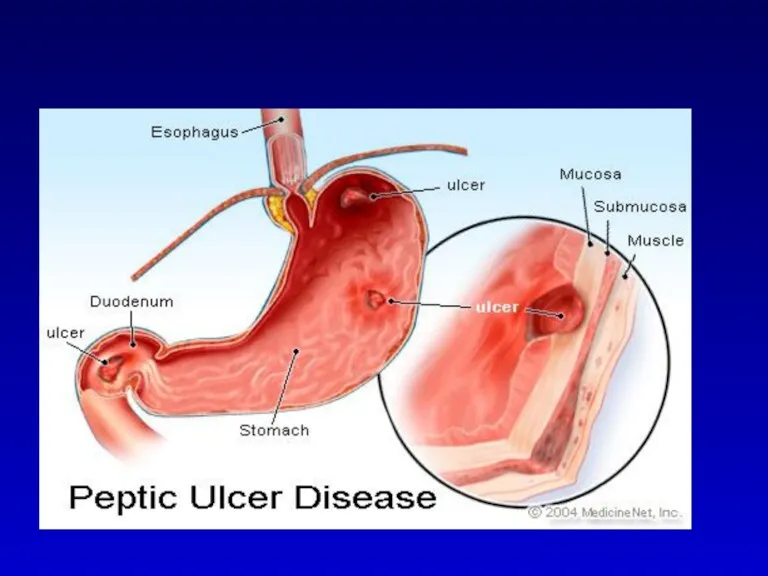
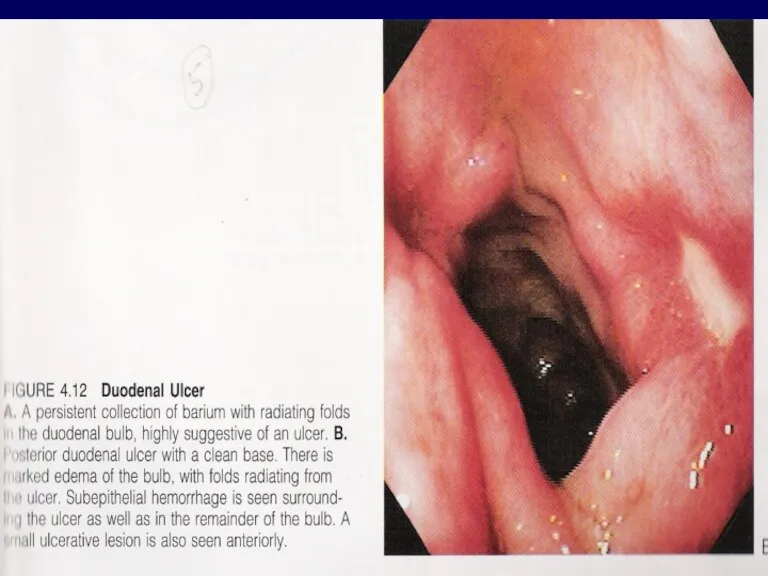
- 3. DEFINITION An ulcer in the gastrointestinal (GI) tract may be defined as a break in the
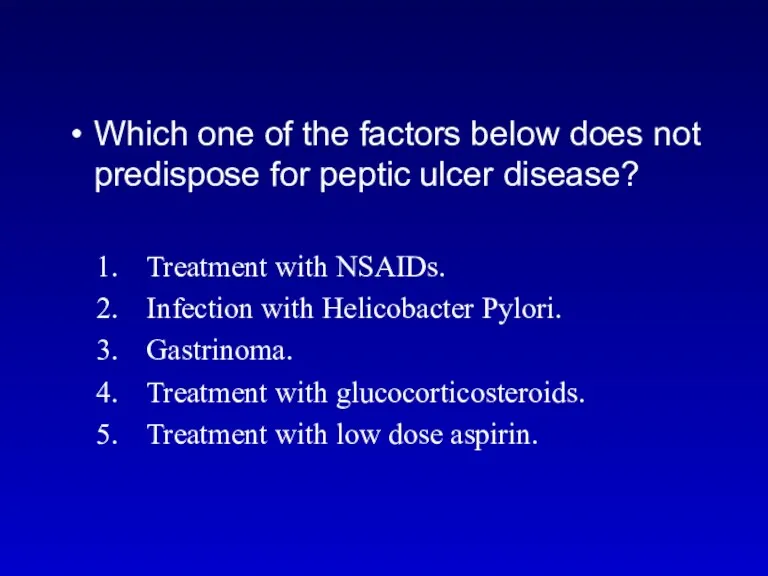
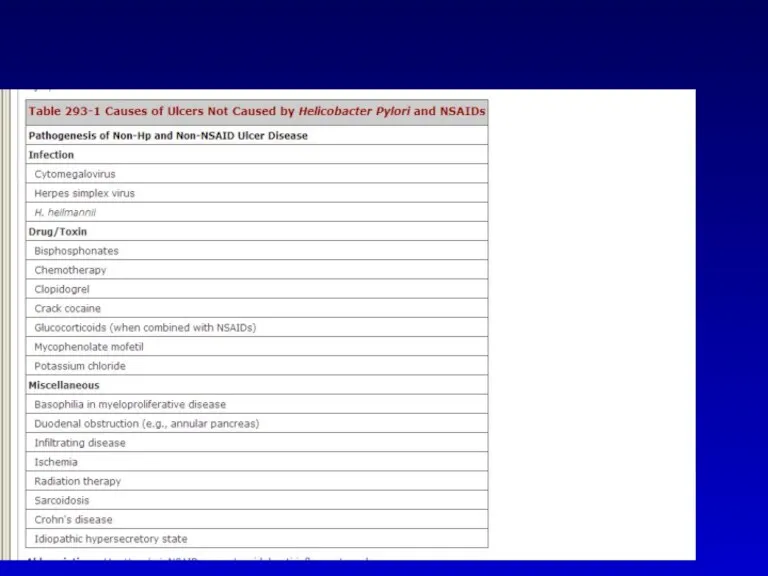
- 8. Which one of the factors below does not predispose for peptic ulcer disease? Treatment with NSAIDs.
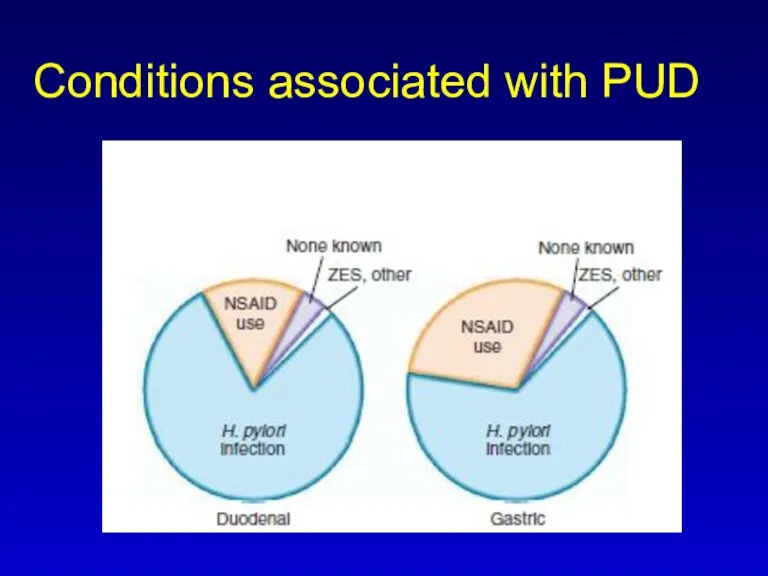
- 9. Conditions associated with PUD
- 13. Which one is the most common complication of PUD? 1. infection 2 . bleeding 3 .
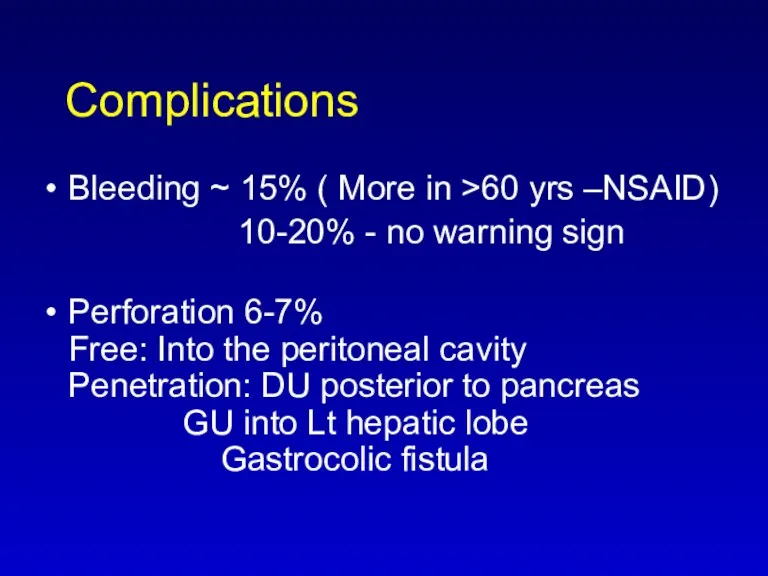
- 14. Complications Bleeding ~ 15% ( More in >60 yrs –NSAID) 10-20% - no warning sign Perforation
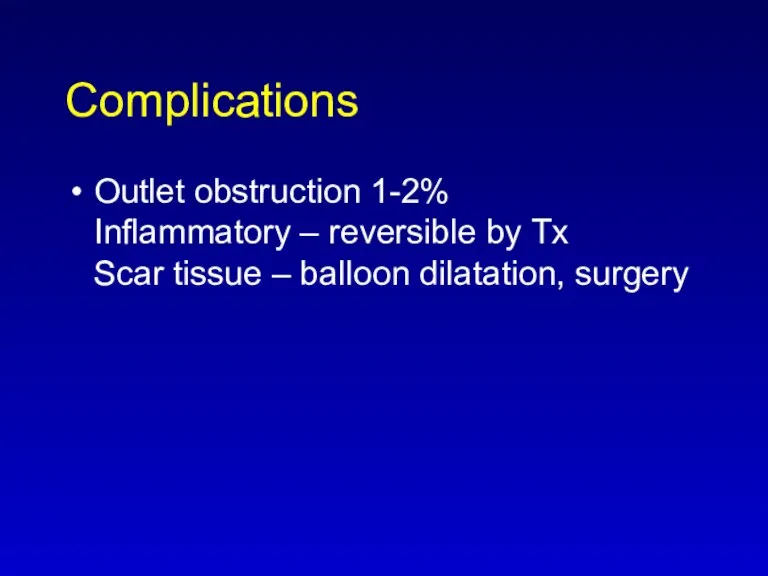
- 16. Complications Outlet obstruction 1-2% Inflammatory – reversible by Tx Scar tissue – balloon dilatation, surgery
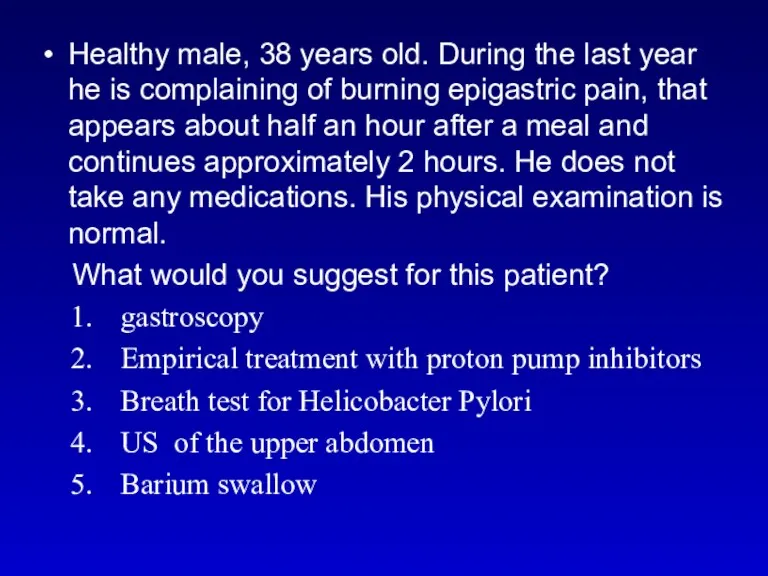
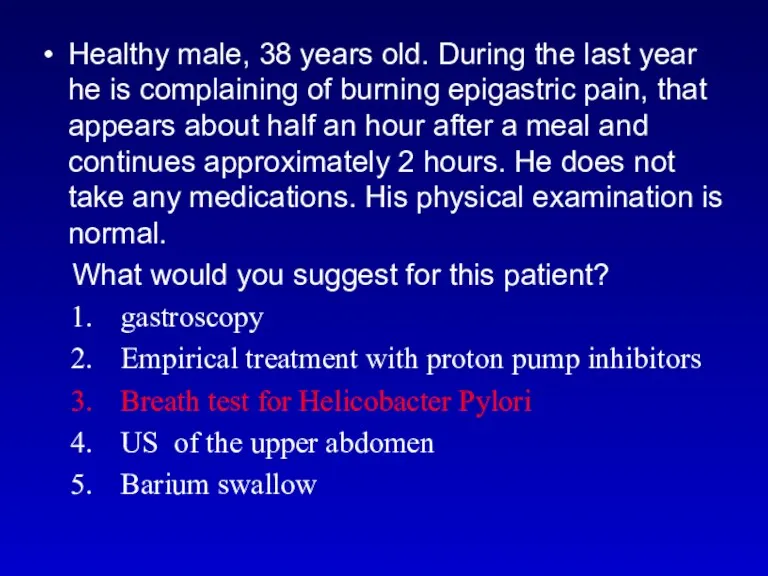
- 17. Healthy male, 38 years old. During the last year he is complaining of burning epigastric pain,
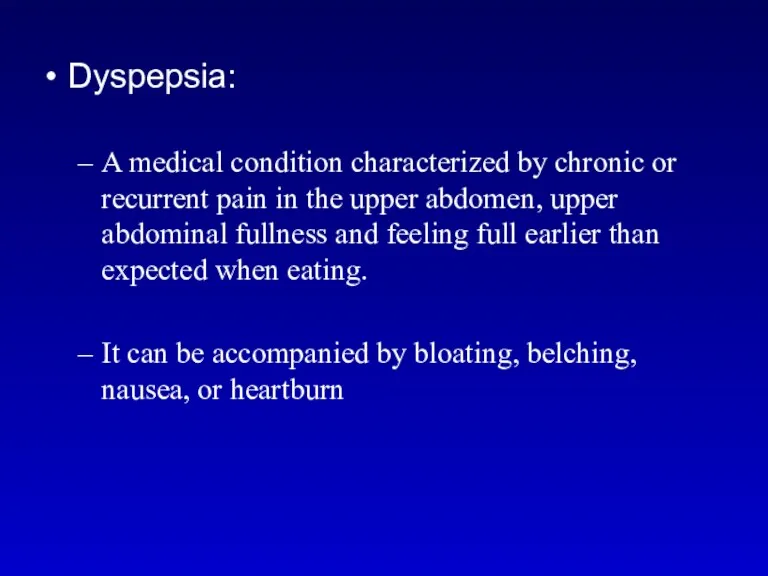
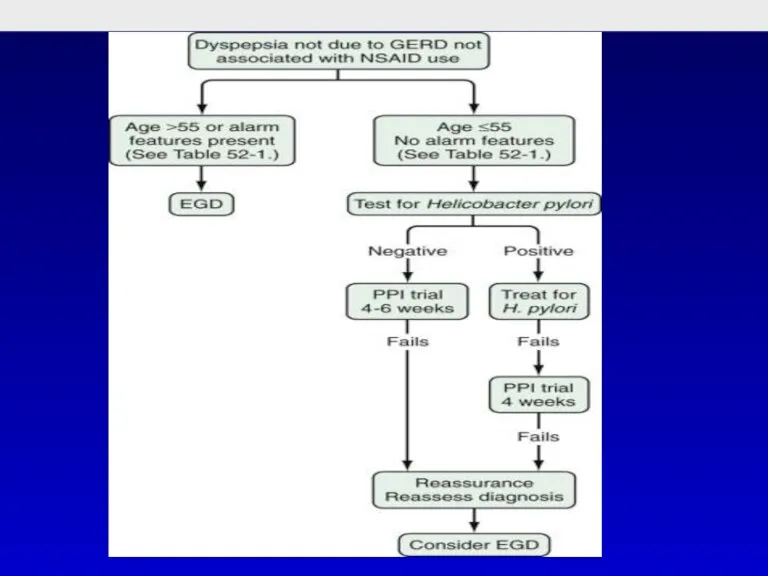
- 18. Dyspepsia: A medical condition characterized by chronic or recurrent pain in the upper abdomen, upper abdominal
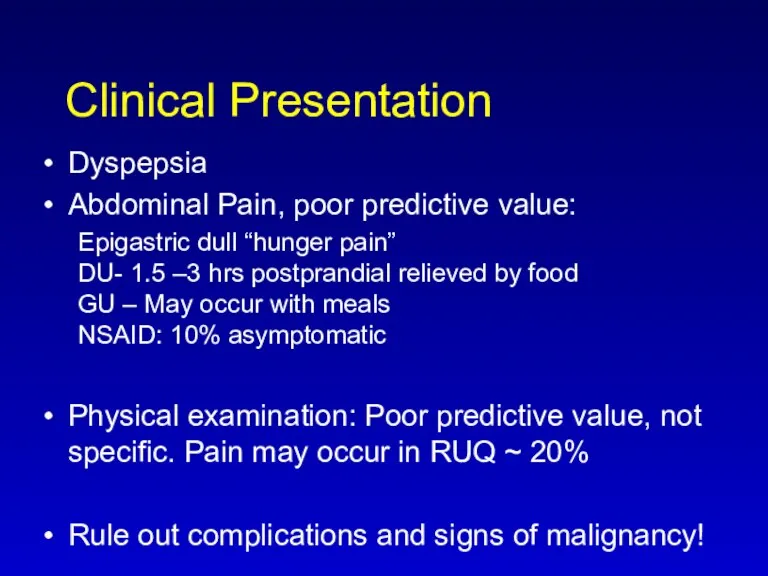
- 19. Clinical Presentation Dyspepsia Abdominal Pain, poor predictive value: Epigastric dull “hunger pain” DU- 1.5 –3 hrs
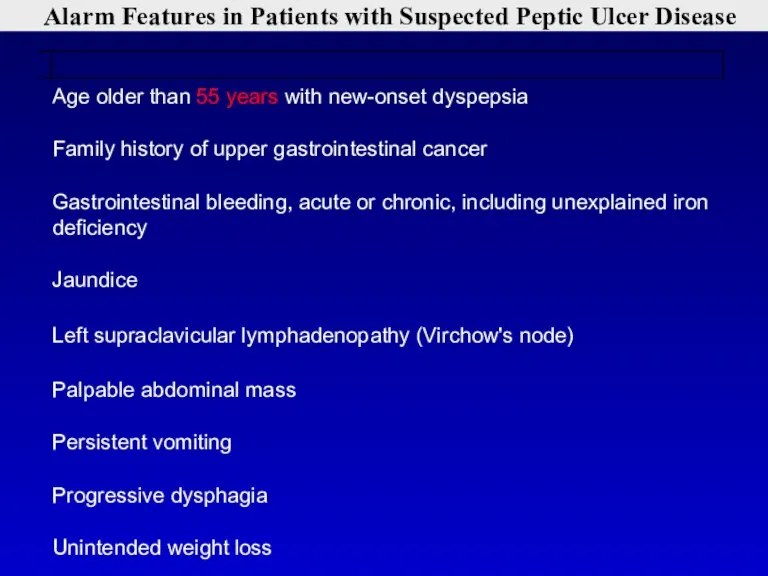
- 20. Alarm Features in Patients with Suspected Peptic Ulcer Disease
- 22. Healthy male, 38 years old. During the last year he is complaining of burning epigastric pain,
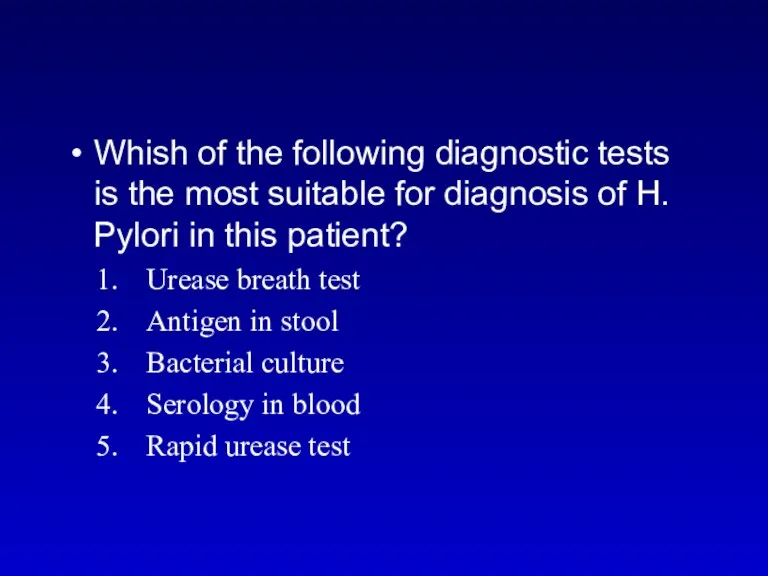
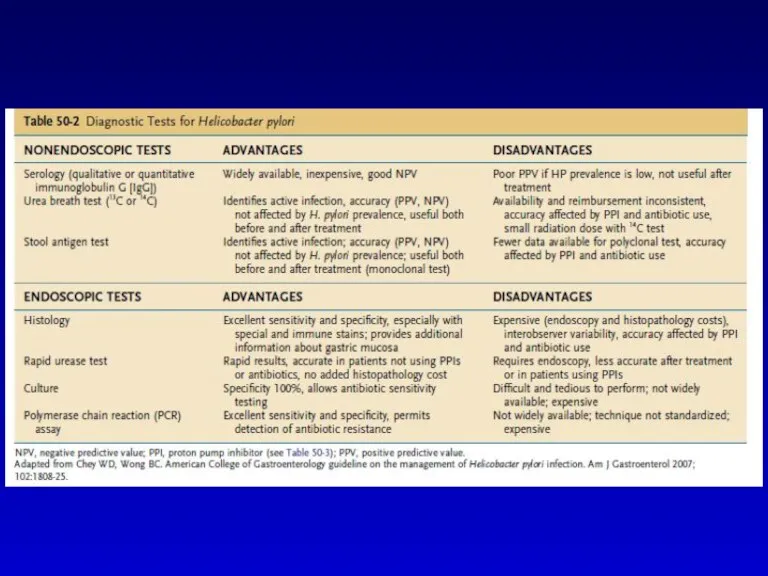
- 23. Whish of the following diagnostic tests is the most suitable for diagnosis of H. Pylori in
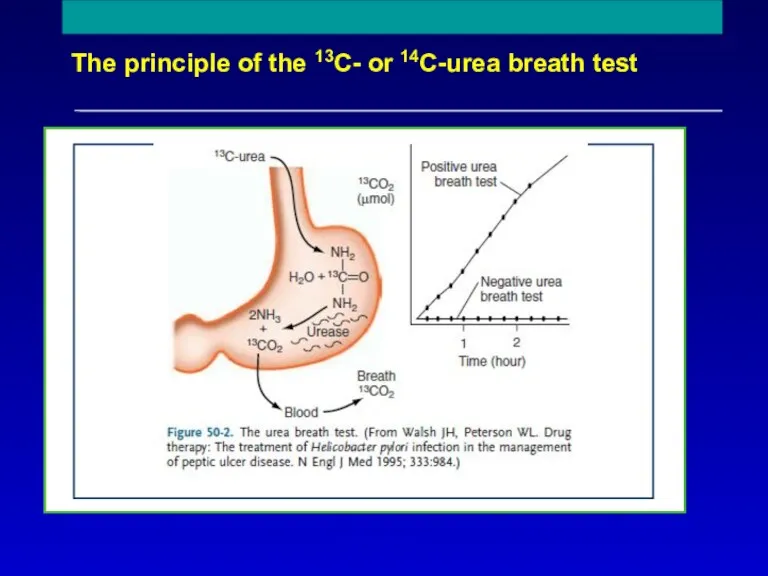
- 25. The principle of the 13C- or 14C-urea breath test Reproduced with permission from Mr Phil Johnson,
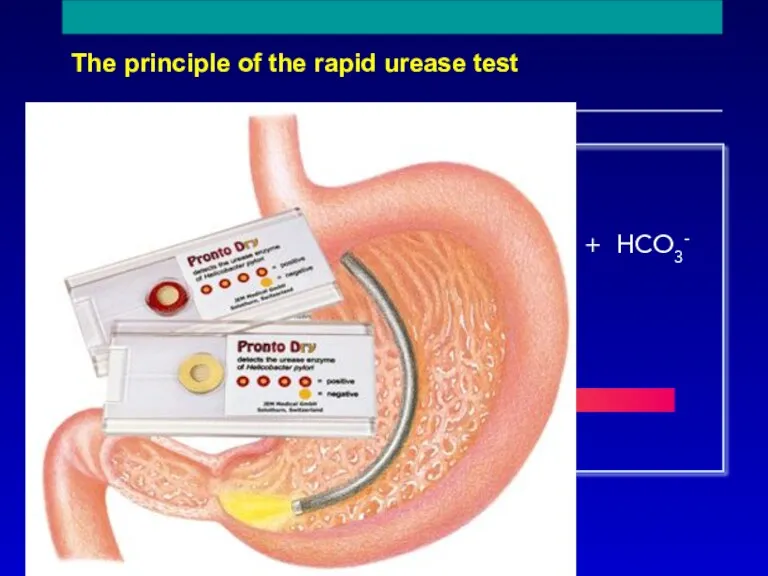
- 26. The principle of the rapid urease test NH2 C NH2 O + 2H2O + H+ 2NH4+
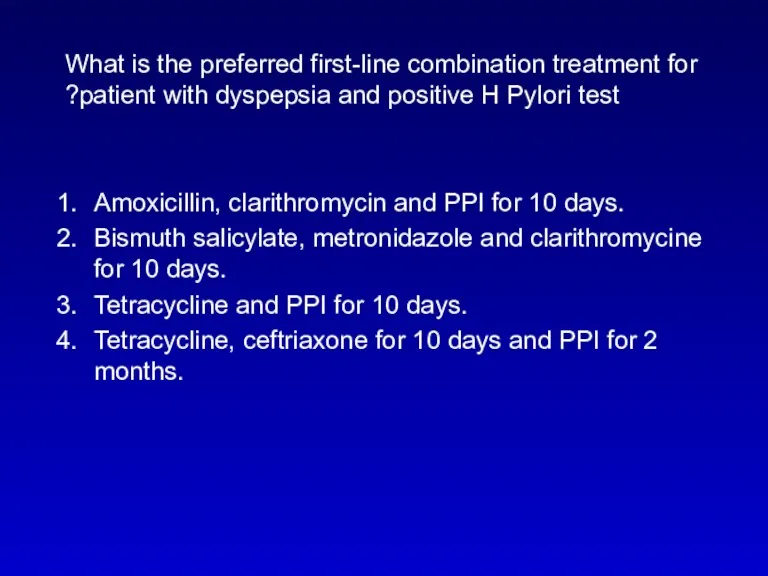
- 27. What is the preferred first-line combination treatment for patient with dyspepsia and positive H Pylori test?
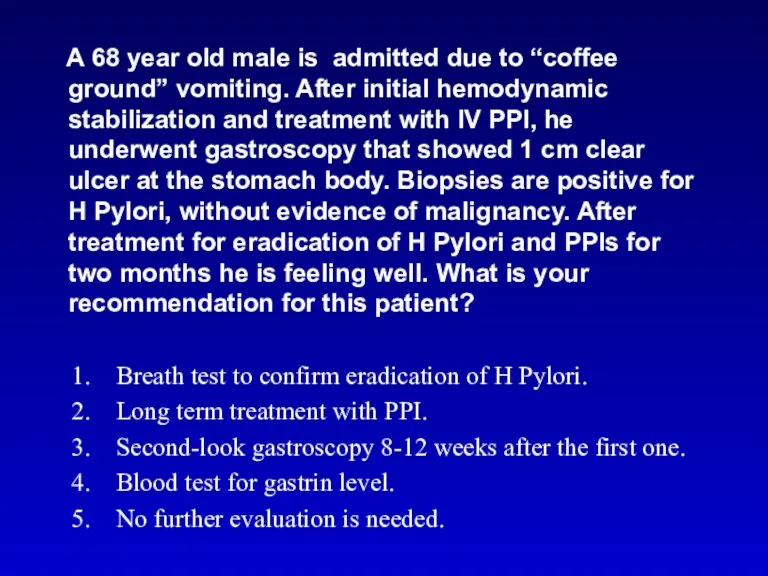
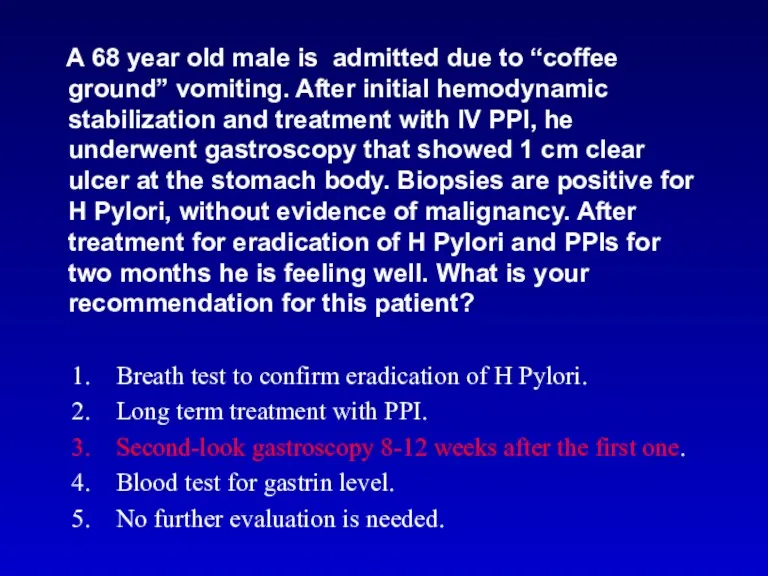
- 29. A 68 year old male is admitted due to “coffee ground” vomiting. After initial hemodynamic stabilization
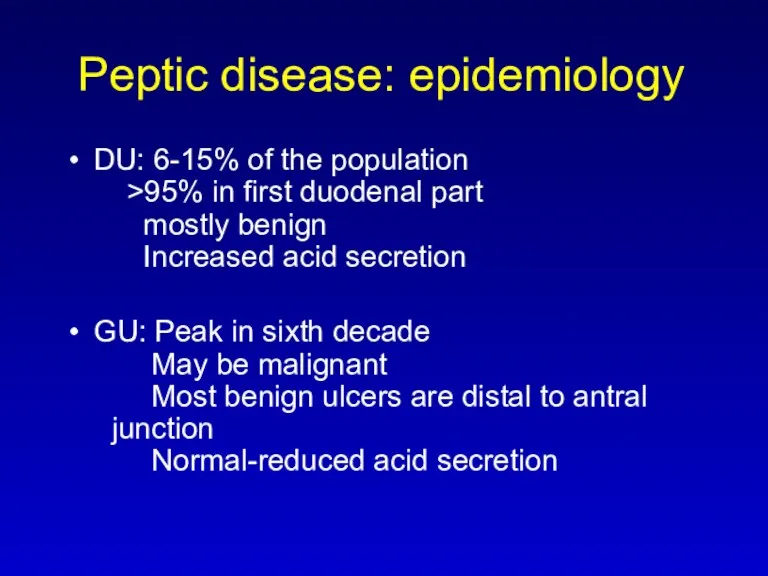
- 30. Peptic disease: epidemiology DU: 6-15% of the population >95% in first duodenal part mostly benign Increased
- 32. A 68 year old male is admitted due to “coffee ground” vomiting. After initial hemodynamic stabilization
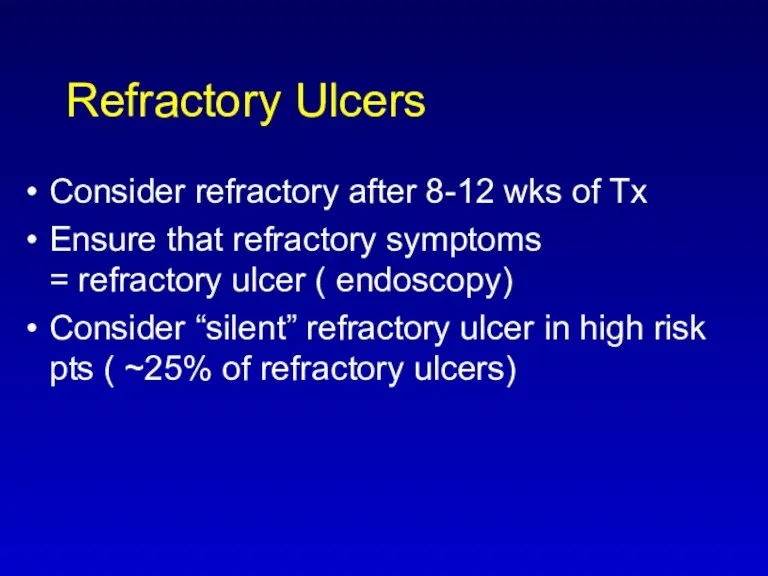
- 33. Refractory Ulcers Consider refractory after 8-12 wks of Tx Ensure that refractory symptoms = refractory ulcer
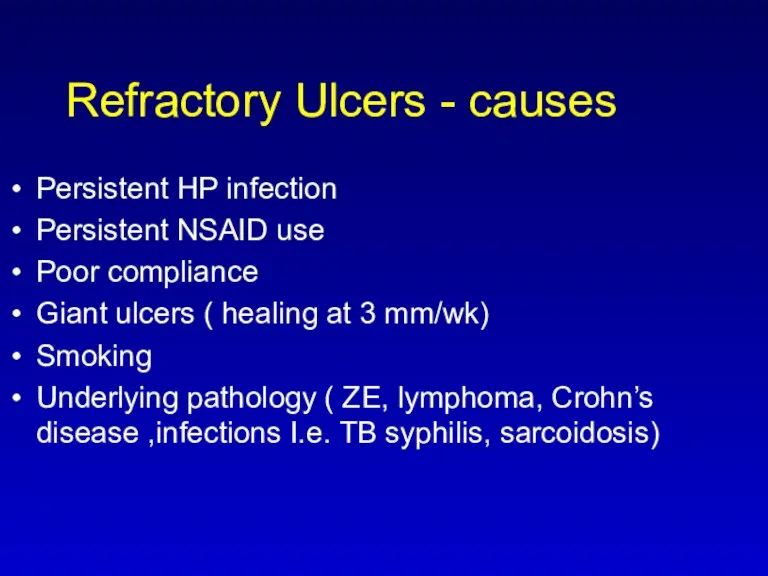
- 34. Refractory Ulcers - causes Persistent HP infection Persistent NSAID use Poor compliance Giant ulcers ( healing
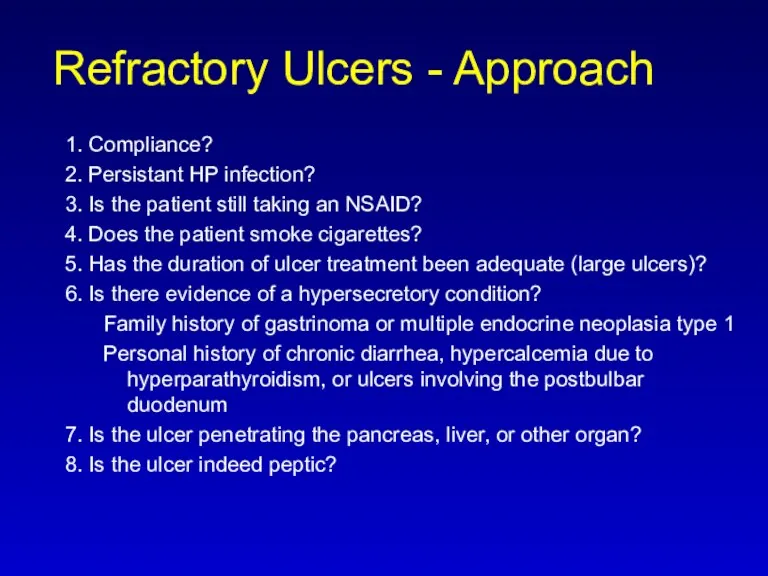
- 35. Refractory Ulcers - Approach 1. Compliance? 2. Persistant HP infection? 3. Is the patient still taking
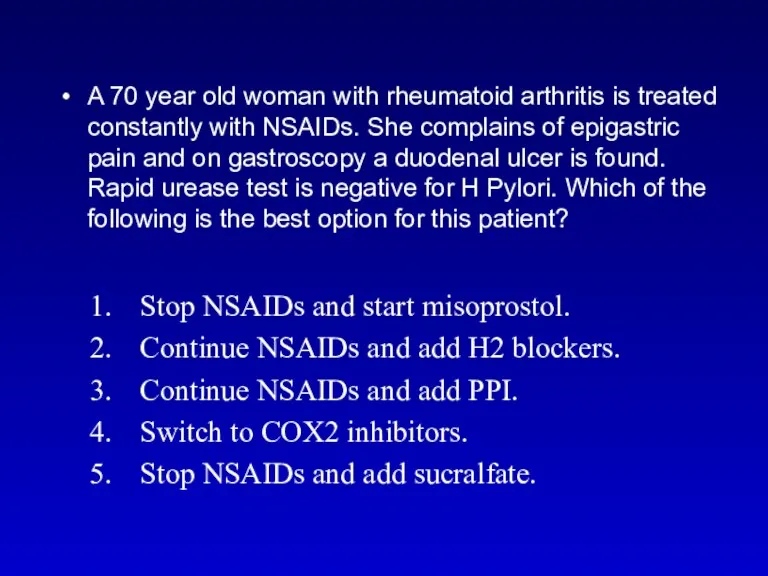
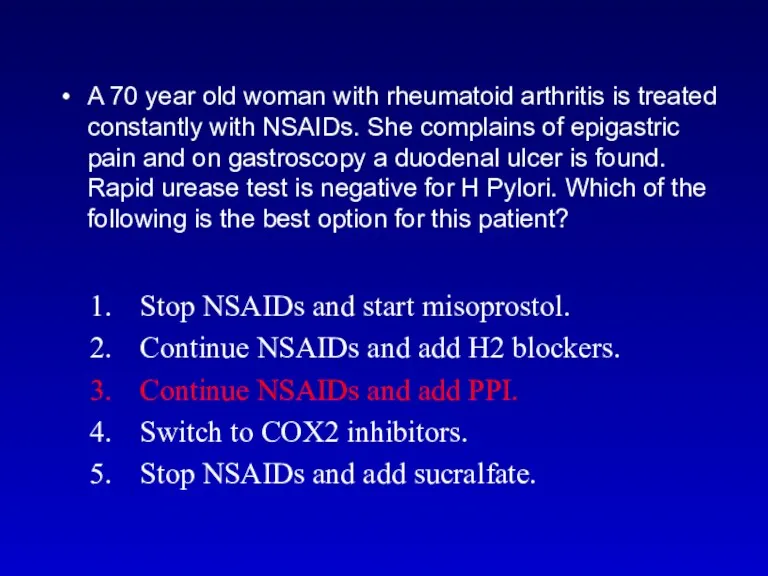
- 36. A 70 year old woman with rheumatoid arthritis is treated constantly with NSAIDs. She complains of
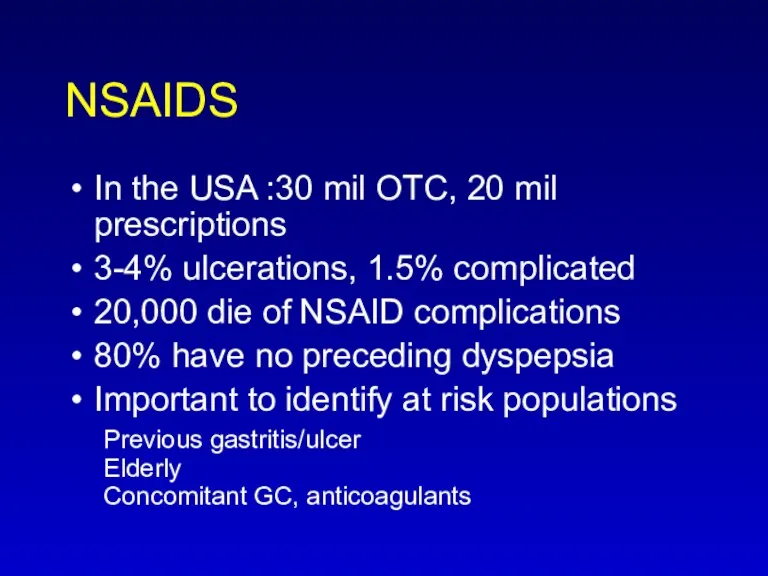
- 37. NSAIDS In the USA :30 mil OTC, 20 mil prescriptions 3-4% ulcerations, 1.5% complicated 20,000 die
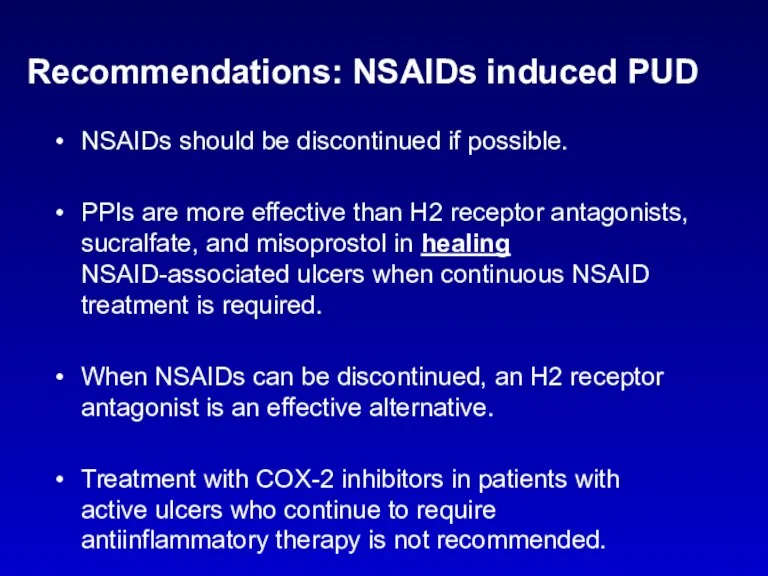
- 39. Recommendations: NSAIDs induced PUD NSAIDs should be discontinued if possible. PPIs are more effective than H2
- 40. A 70 year old woman with rheumatoid arthritis is treated constantly with NSAIDs. She complains of
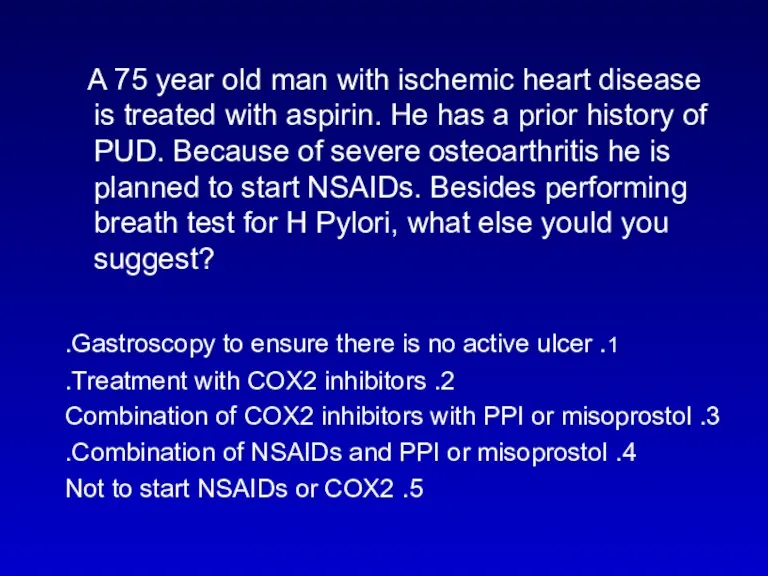
- 41. A 75 year old man with ischemic heart disease is treated with aspirin. He has a
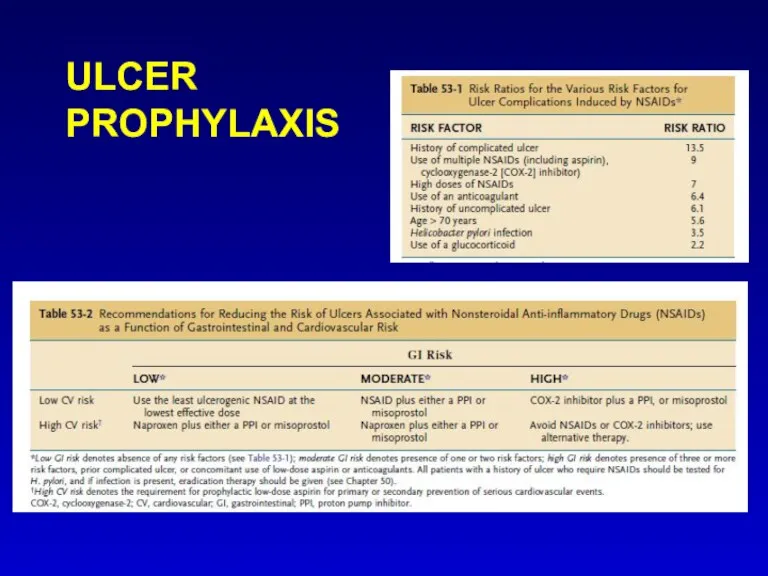
- 42. ULCER PROPHYLAXIS
- 43. What is the best treatment to prevent stress ulcers in intubated patients? PPI H2B SULCRAFATE MISOPROSTOL
- 44. Discussion outline Definitions Risk factors Complications Clinical presentation Management – HBP, NSAIDS Refractory PUD Prophylaxis
- 46. Скачать презентацию



 Профилактика нарушений осанки опорно-двигательного аппарата у детей дошкольного возраста
Профилактика нарушений осанки опорно-двигательного аппарата у детей дошкольного возраста Нарушения белой крови
Нарушения белой крови Наследственно-дегенеративные заболевания
Наследственно-дегенеративные заболевания Энцефалиты
Энцефалиты Организация производства экстракта полыни гмелина (Artemisia gmelini)
Организация производства экстракта полыни гмелина (Artemisia gmelini) Дерматологические аспекты ВИЧ-инфекции
Дерматологические аспекты ВИЧ-инфекции Бронх тал құрылысы
Бронх тал құрылысы Ботулизм
Ботулизм Непрерывное медицинское образование – важнейшая составляющая повышения эффективности здравоохранения
Непрерывное медицинское образование – важнейшая составляющая повышения эффективности здравоохранения Тромболитическая терапия в остром периоде мозгового инсульта
Тромболитическая терапия в остром периоде мозгового инсульта Гормональная регуляция обмена белков, воды и электролитов
Гормональная регуляция обмена белков, воды и электролитов Нервная анорексия, булимия
Нервная анорексия, булимия Организация противоэпидемических мероприятий при чрезвычайных ситуациях
Организация противоэпидемических мероприятий при чрезвычайных ситуациях Абдоминальнокардиалды синдром жайлы түсінік беру
Абдоминальнокардиалды синдром жайлы түсінік беру Инфекциялық аурулардан өлгендерді зертеу әдістері
Инфекциялық аурулардан өлгендерді зертеу әдістері Алгоритм диагностики и оказания скорой помощи при острых отравлениях
Алгоритм диагностики и оказания скорой помощи при острых отравлениях Анатомо-физиологические особенности костно-мышечной системы у детей
Анатомо-физиологические особенности костно-мышечной системы у детей Диагностика и лечение анемии
Диагностика и лечение анемии Здоровый образ жизни как необходимое условие сохранения и укрепления здоровья человека и общества
Здоровый образ жизни как необходимое условие сохранения и укрепления здоровья человека и общества Всемирный день чистых рук
Всемирный день чистых рук Оздоровление членов профсоюза ПАО ЮГОК
Оздоровление членов профсоюза ПАО ЮГОК Гигиена нервной и сенсорной систем
Гигиена нервной и сенсорной систем Введение в травматологию и ортопедию. (Лекция 1)
Введение в травматологию и ортопедию. (Лекция 1) Лекция: Болезни прорезывания зубов. Принципы диагностики и лечения
Лекция: Болезни прорезывания зубов. Принципы диагностики и лечения Неорганические вещества в медицине
Неорганические вещества в медицине Вегетативные пароксизмы у детей: синдром циклической рвоты
Вегетативные пароксизмы у детей: синдром циклической рвоты Ancient medicine
Ancient medicine Школа нескучного материнства. Вводный урок
Школа нескучного материнства. Вводный урок