Содержание
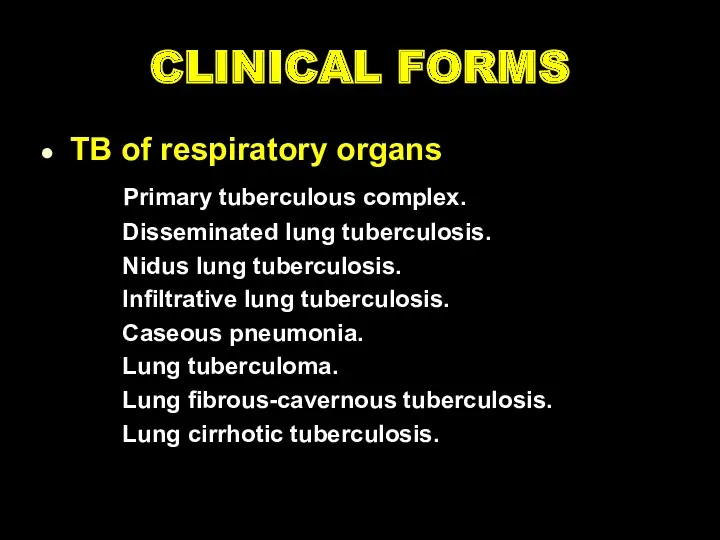
- 2. CLINICAL FORMS TB of respiratory organs Primary tuberculous complex. Disseminated lung tuberculosis. Nidus lung tuberculosis. Infiltrative
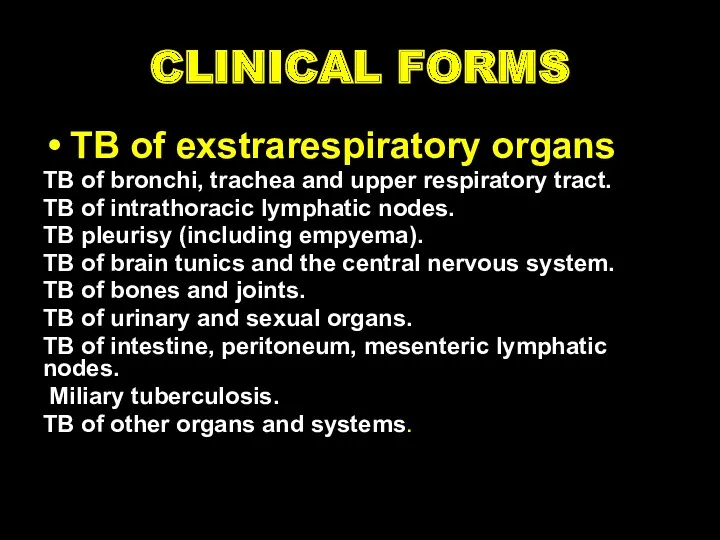
- 3. CLINICAL FORMS TB of exstrarespiratory organs TB of bronchi, trachea and upper respiratory tract. TB of
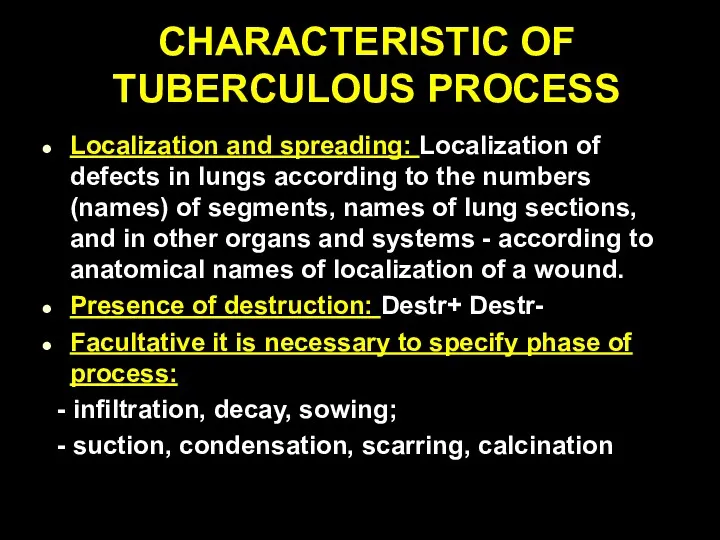
- 4. CHARACTERISTIC OF TUBERCULOUS PROCESS Localization and spreading: Localization of defects in lungs according to the numbers
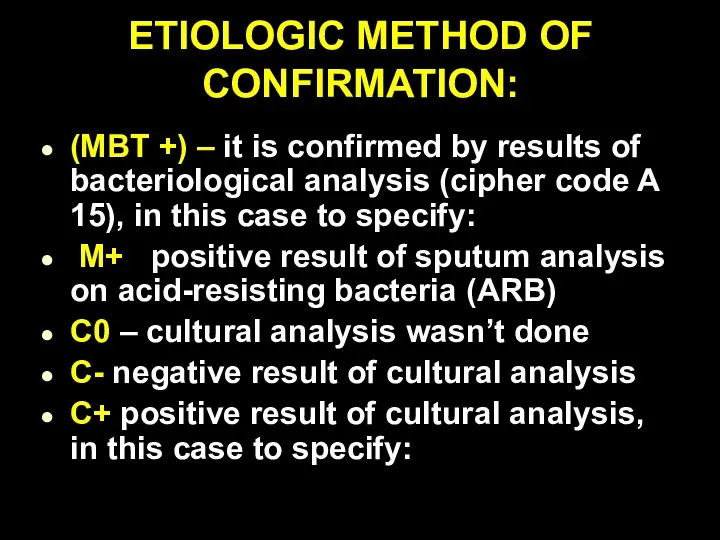
- 5. ETIOLOGIC METHOD OF CONFIRMATION: (MBT +) – it is confirmed by results of bacteriological analysis (cipher
- 6. (Resist 0) MBT resistance to preparations of I line wasn’t analyzed; (Resist -) resistance to preparations
- 7. Types of TB cases New case of TB – A patient who has never been treated
- 8. Previously treated case of TB 1. Relapse patients have previously been treated for TB, were declared
- 9. Case of multidrug-resistant TB (MDR-TB) – TB that is resistant to two first-line drugs: isoniazid and
- 10. Clinical forms of pulmonary tuberculosis There such clinical forms of pulmonary TB, as milliary, disseminated, focal,
- 11. Clinical forms of extra-pulmonary tuberculosis It depends on the affected organ. Miliary tuberculosis, tuberculosis of intrathoracic
- 12. Phases of TB There are such TB process phases: infiltration, decay (corresponding Destruction +), contamination, resorption,
- 13. Diagnosis examples New case of TB (01.02.2016) upper lobe of right lung (infiltrative), contamination phase, Destr
- 14. RADIOLOGICAL SYNDROMS To explain radiological features of tuberculosis clinical form we must understand radiological syndroms. There
- 15. Abnormal pulmonary pattern syndrome Increased and enriching the lung picture (at inflammatory processes, collagenous diseases, tumor,
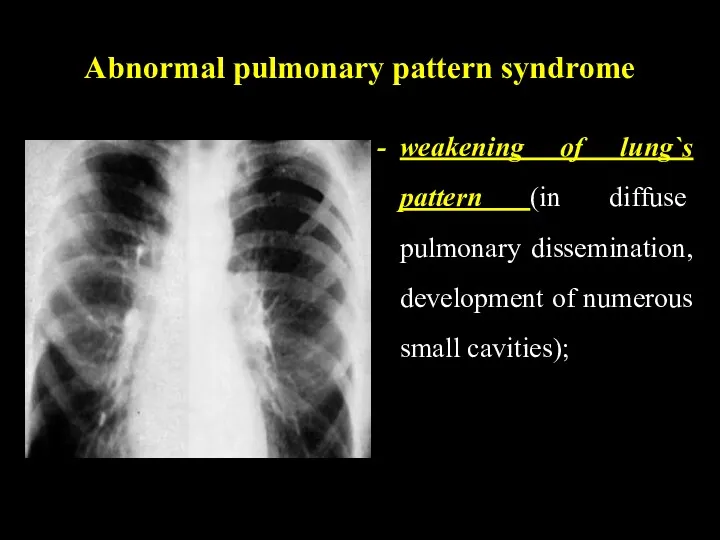
- 16. Abnormal pulmonary pattern syndrome weakening of lung`s pattern (in diffuse pulmonary dissemination, development of numerous small
- 17. Abnormal pulmonary pattern syndrome depletion of the picture (at inflating the lungs, lung arterial nets hypoplasia);
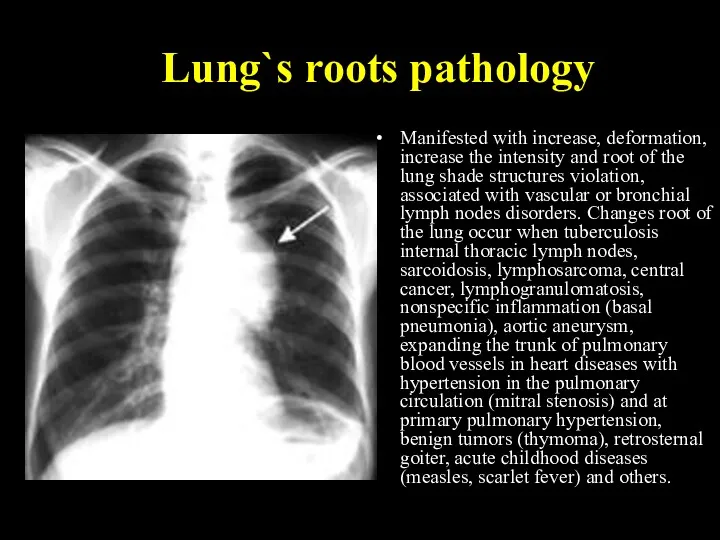
- 18. Lung`s roots pathology Manifested with increase, deformation, increase the intensity and root of the lung shade
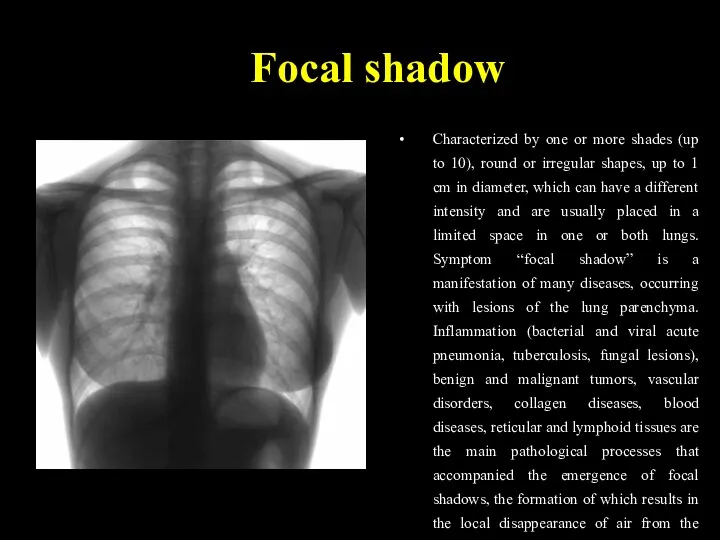
- 19. Focal shadow Characterized by one or more shades (up to 10), round or irregular shapes, up
- 20. Infiltrative shadow This syndrome characterized by shadow areas of more than 1 cm, round or irregular
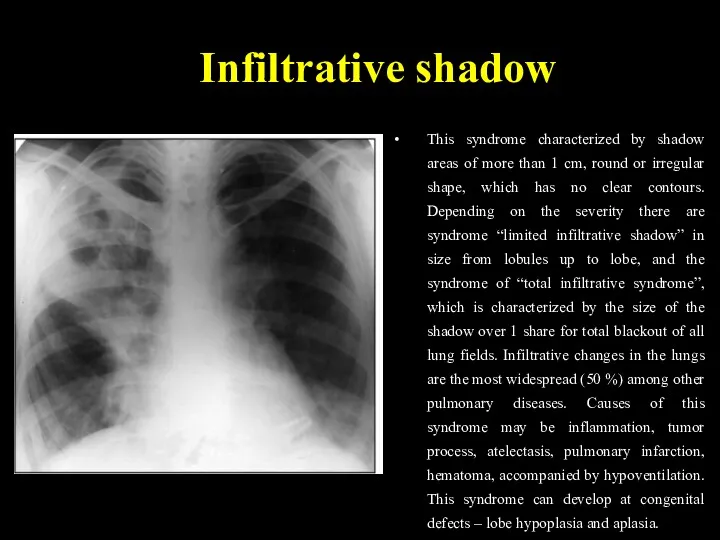
- 21. Disseminative syndrome Characterized by multiple focal and retinal shadows of varying intensity to 1 cm in
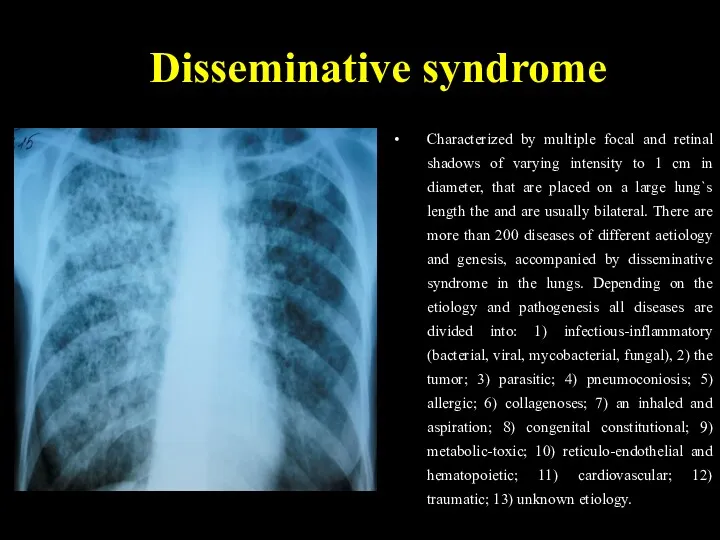
- 22. Rounded shadow Characterized by volume spherical or oval formation of correct, incorrect or polycyclic forms with
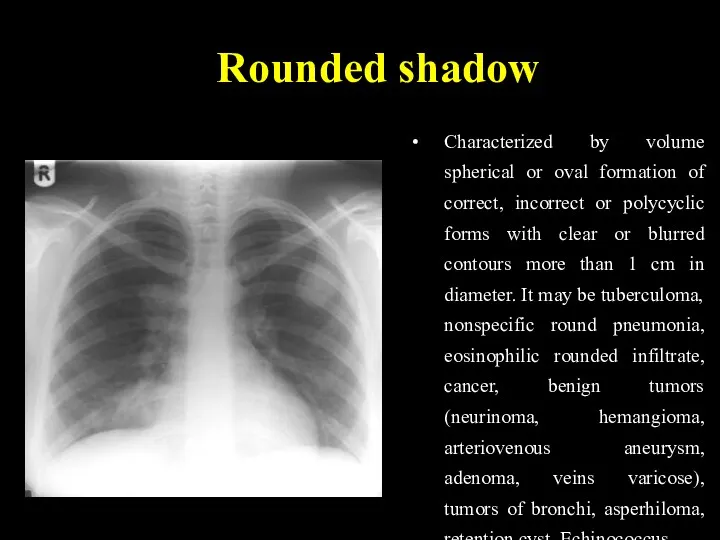
- 23. Ring-like shadow It characterized by rounded enlightenment, which is surrounded by a ring-liked shadow. Enlightenment in
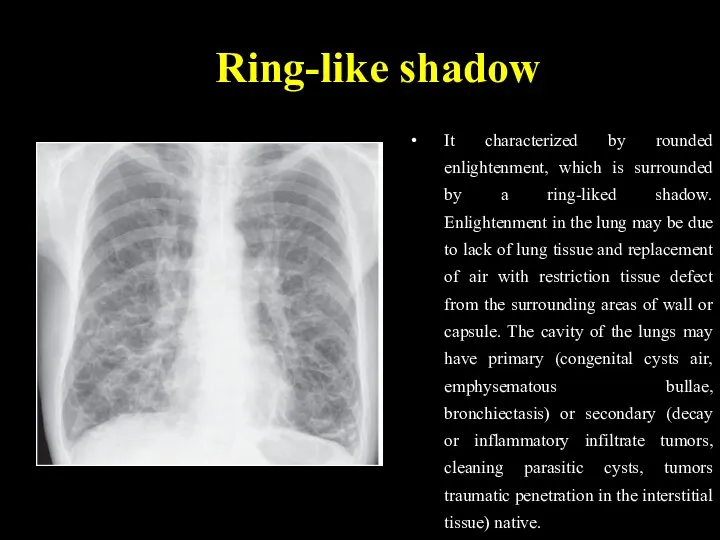
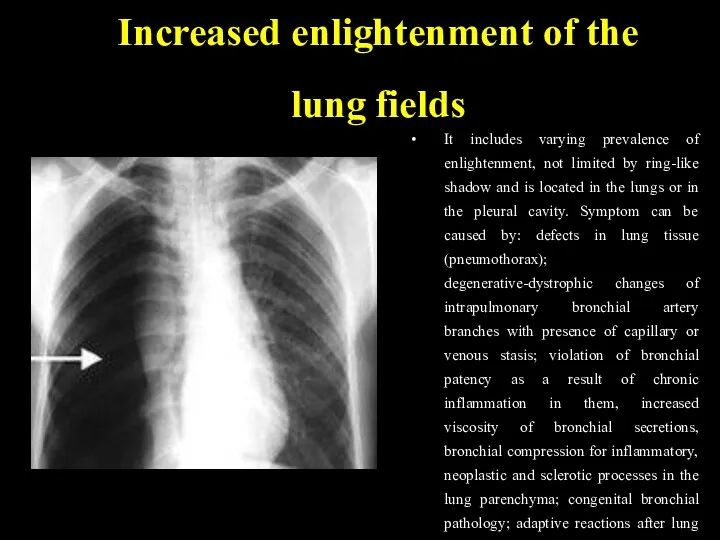
- 24. Increased enlightenment of the lung fields It includes varying prevalence of enlightenment, not limited by ring-like
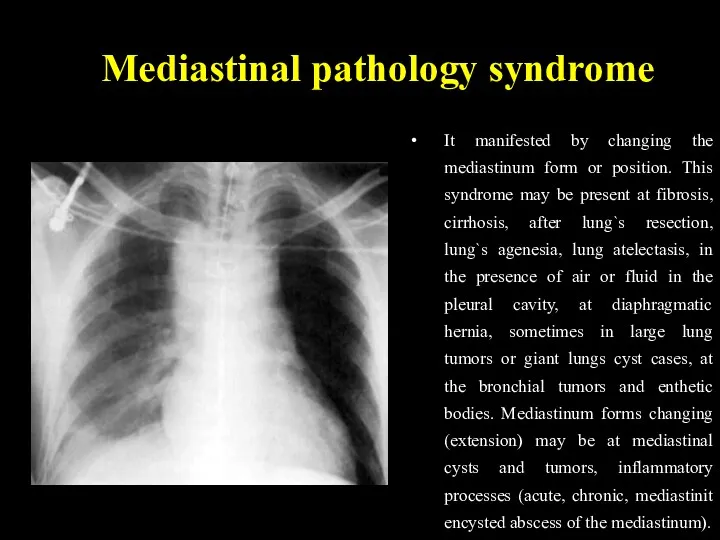
- 25. Mediastinal pathology syndrome It manifested by changing the mediastinum form or position. This syndrome may be
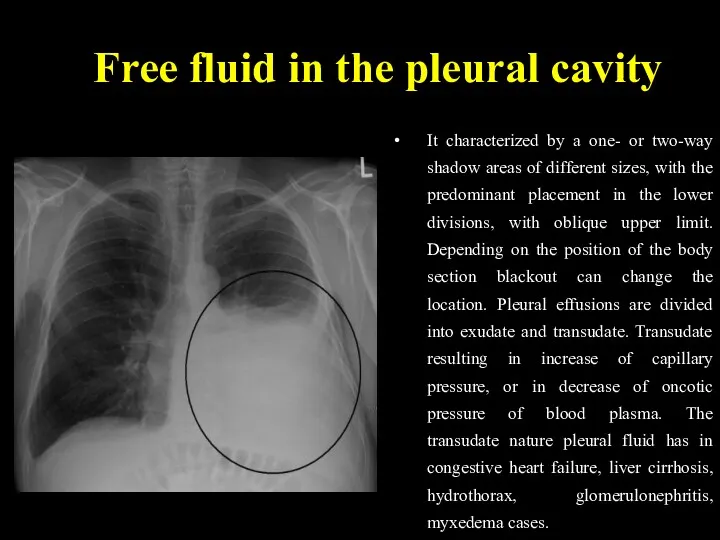
- 26. Free fluid in the pleural cavity It characterized by a one- or two-way shadow areas of
- 27. Free fluid in the pleural cavity The most frequent cause of exudative pleurisy of different etiology
- 28. Depending on pathogenesis the tuberculosis is divided primary and secondary. Primary tuberculosis develops after the first
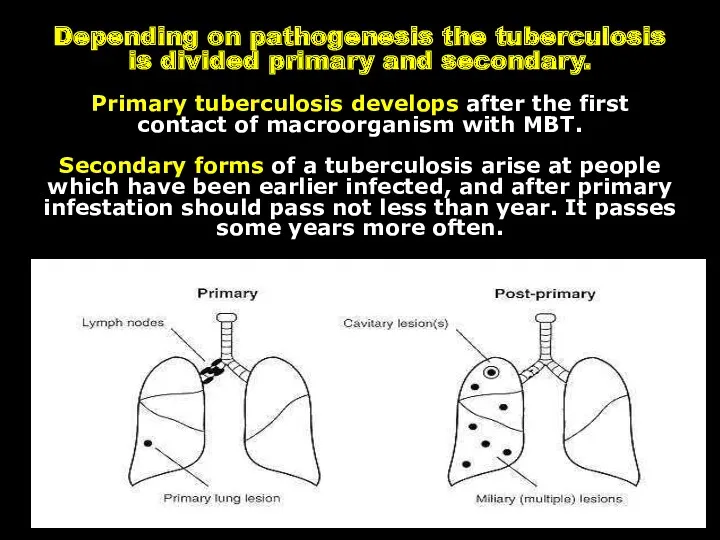
- 29. PRIMARY TUBERCULOSIS Primary is considered tuberculosis that develops in firstly infected persons. The period from the
- 30. Para-specific reactions (tuberculosis “masks”) In primary tuberculosis there are situations where the disease occurs more on
- 31. “Flu-like” TB mask The most frequently tuberculosis in active phase occurs in such frequent, long, unusual
- 32. “pneumonic” mask The second frequency is “pneumonic” mask. This is repeated recurrent pneumonia, especially in the
- 33. Poncet`s disease Tuberculosis can begin on type “rheumatic” mask, called “Poncet`s disease”. It manifested a long
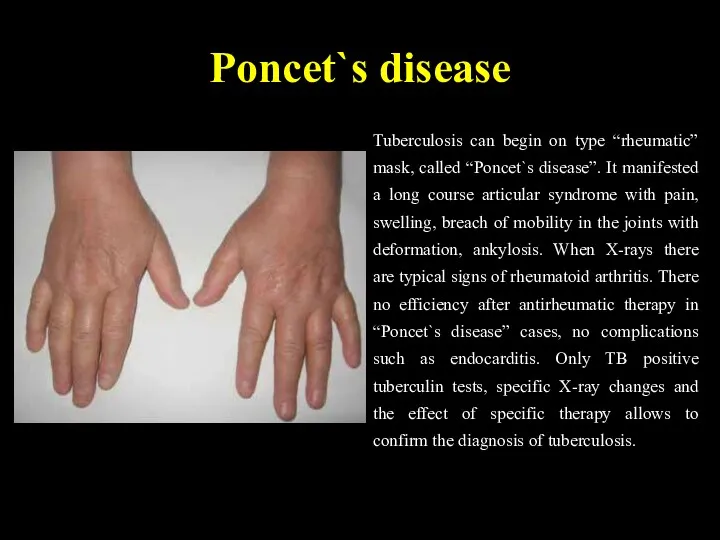
- 34. “Neurological” TB mask “Neurological” TB mask manifests as long, persistent neuralgia, which can not be usually
- 35. “Lupus-like” TB mask “Lupus-like” mask manifests typical erythema on the face in the form of "butterfly",
- 36. “Hematological” mask “Hematological” mask of tuberculosis occurs with bone marrow hypoplasia, leukopenia, anemia, thrombocytopenia, sometimes with
- 37. Keratoconjunctivitis phlyctenular Keratoconjunctivitis phlyctenular. Most often its tubercular-allergic process in children with broncho-adenitis and tuberculosis of
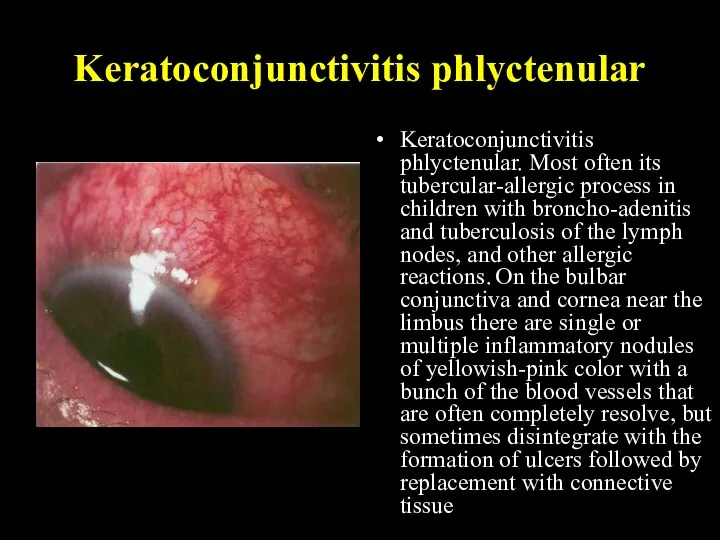
- 38. CHARACTERISTIC SIGNS OF PRIMARY TUBERCULOSIS: the intensity of tuberculin reactions organism hypersensibilization to MBT injury of
- 39. PRIMARY TUBERCULOUS COMPLEX 1. PATHOGENESIS After the penetration of MBT into the lungs, primary lesion (primary
- 40. PRIMARY TUBERCULOUS COMPLEX The dynamic study of primary pulmonary processes among children has allowed to allot
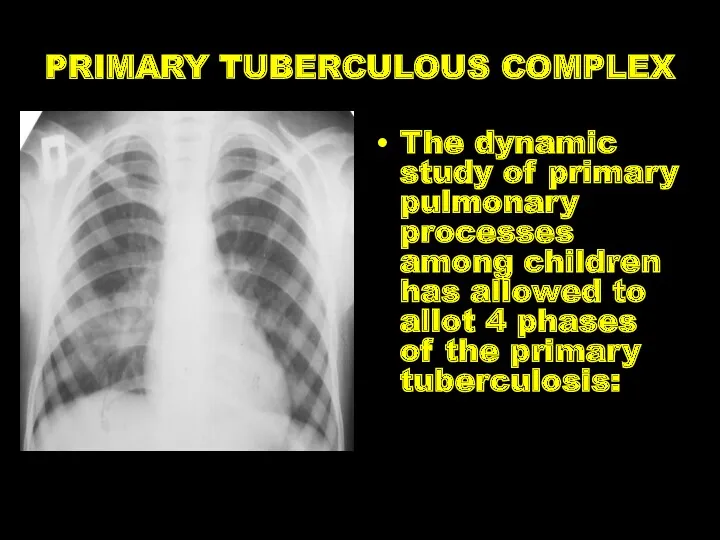
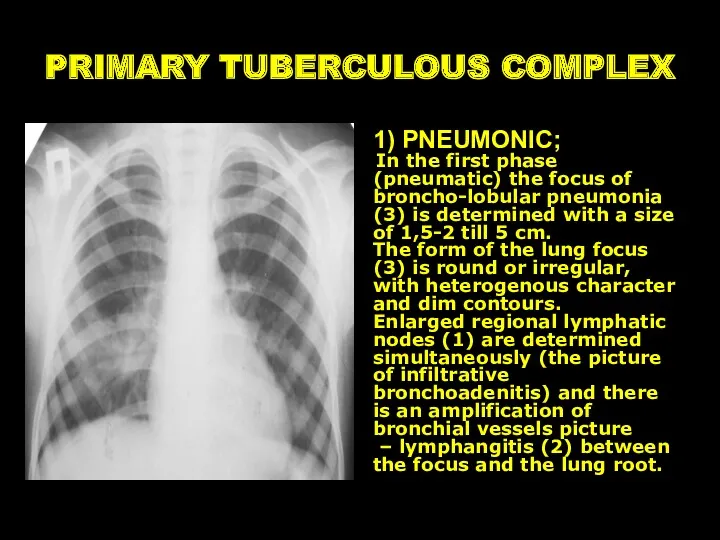
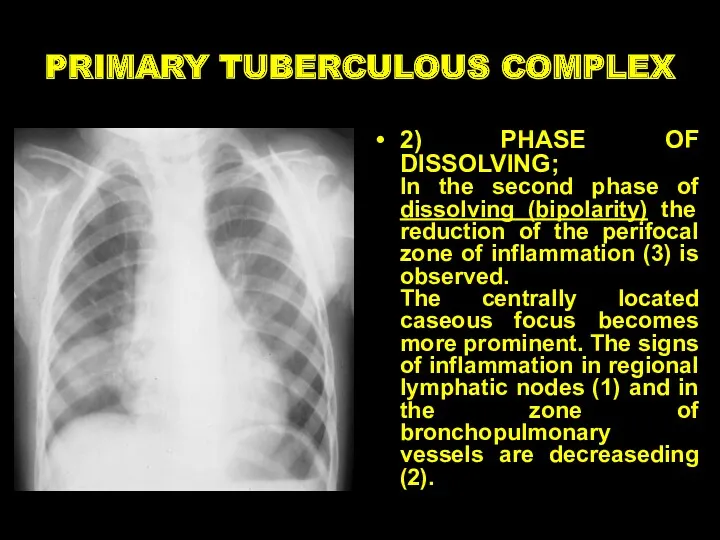
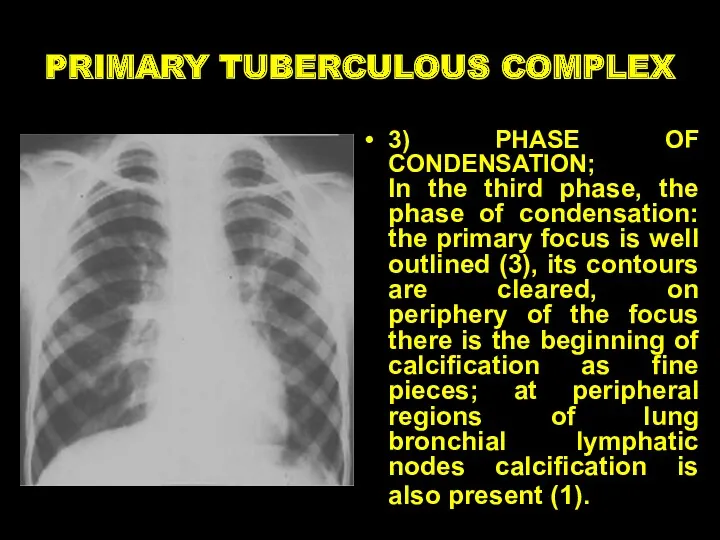
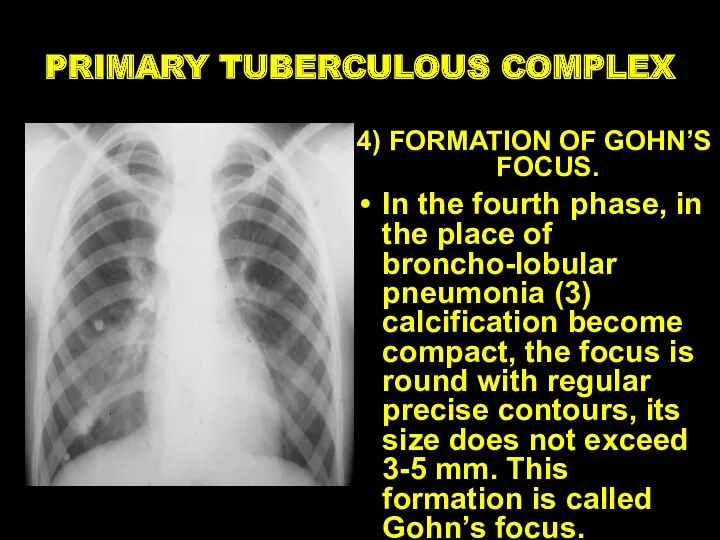
- 41. PRIMARY TUBERCULOUS COMPLEX 1) PNEUMONIC; In the first phase (pneumatic) the focus of broncho-lobular pneumonia (3)
- 42. PRIMARY TUBERCULOUS COMPLEX 2) PHASE OF DISSOLVING; In the second phase of dissolving (bipolarity) the reduction
- 43. PRIMARY TUBERCULOUS COMPLEX 3) PHASE OF CONDENSATION; In the third phase, the phase of condensation: the
- 44. PRIMARY TUBERCULOUS COMPLEX 4) FORMATION OF GOHN’S FOCUS. In the fourth phase, in the place of
- 45. TUBERCULOSIS OF INTRATHORACIC LYMPHATIC NODES Bronchoadenitis is a disease of the lymph nodes of the lungs
- 46. Clinical pattern of tuberculous bronchoadenitis acute intoxication specific clinical symptoms: subfebrile temperature, deterioration of general condition,
- 47. Clinico-roentgenologically variants of intrathoracic lymphatic nodes TB tumour like (tumoursimilar) form infiltrative form Left side tumorous
- 48. Miliary tuberculosis Generalized TB clinical form with the hematogenic type of dissemination and acute course
- 49. Sub-acute disseminated tuberculosis Bilateral lung injury with predominant affecting upper lobes and trend for destructive progressive
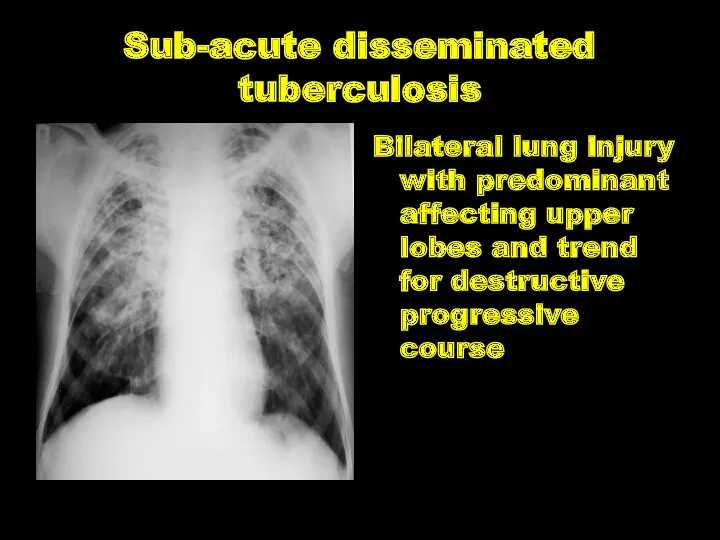
- 50. Chronic disseminated tuberculosis Disseminated lung injury with the wavy course and progressive alveoli substitution by connective
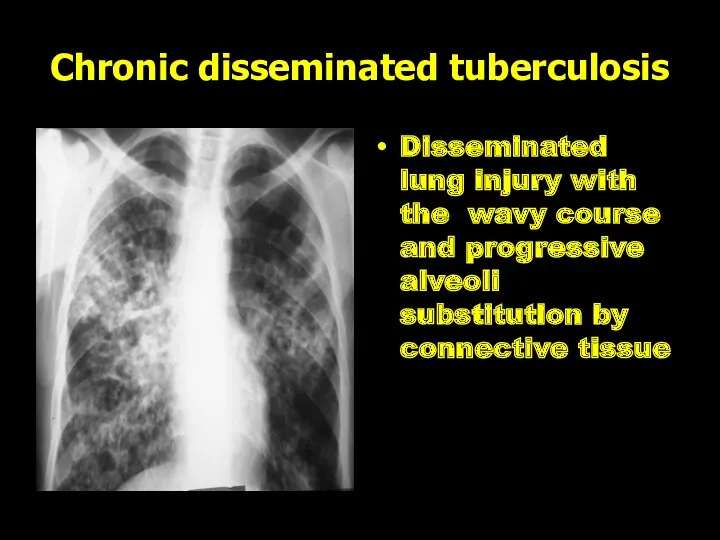
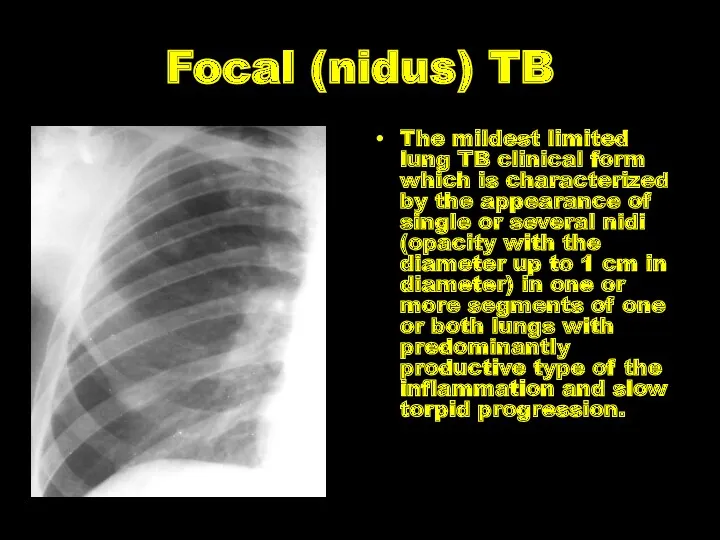
- 51. Focal (nidus) TB The mildest limited lung TB clinical form which is characterized by the appearance
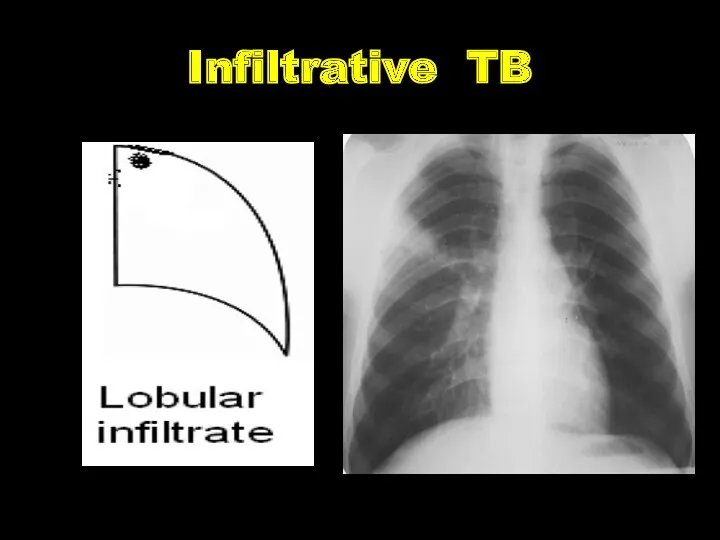
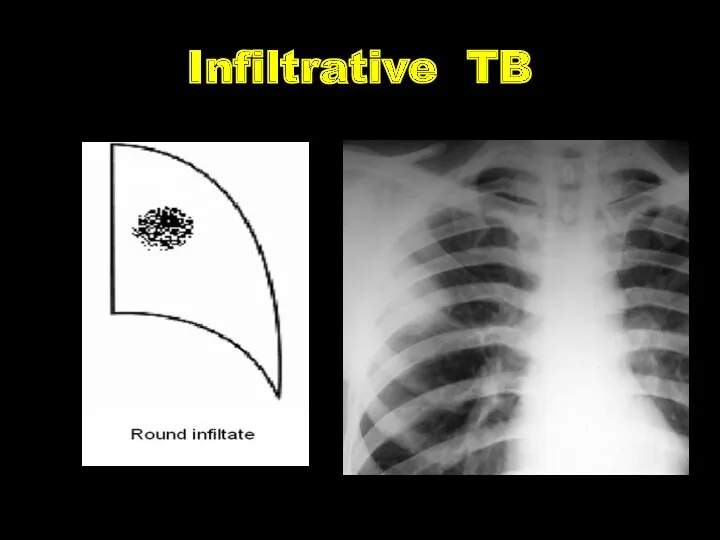
- 52. Infiltrative TB The expansive lung TB clinical form which is characterized by the appearance of different
- 53. Infiltrative TB
- 54. Infiltrative TB
- 55. Infiltrative TB
- 56. Infiltrative TB
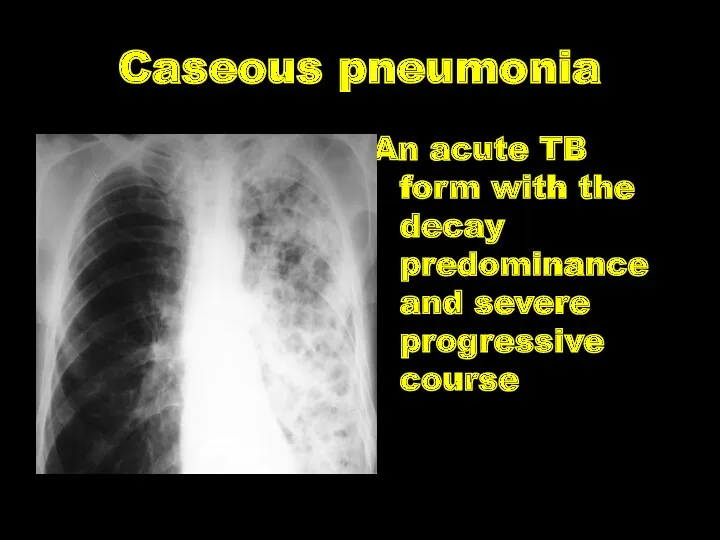
- 57. Caseous pneumonia An acute TB form with the decay predominance and severe progressive course
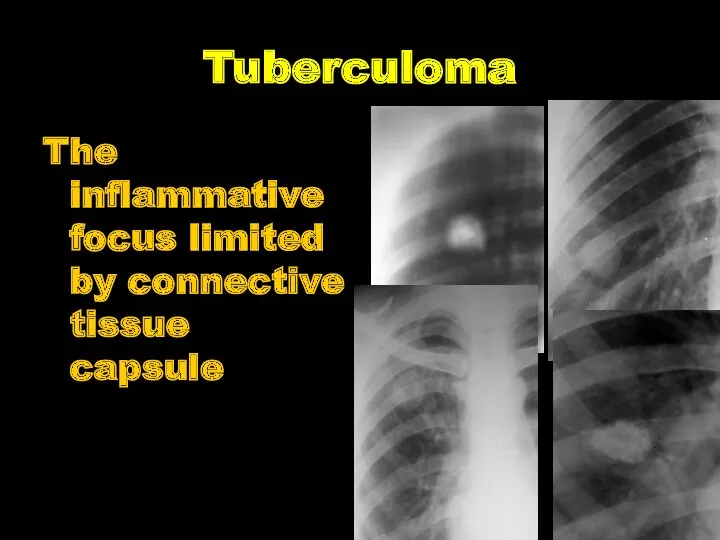
- 58. Tuberculoma The inflammative focus limited by connective tissue capsule
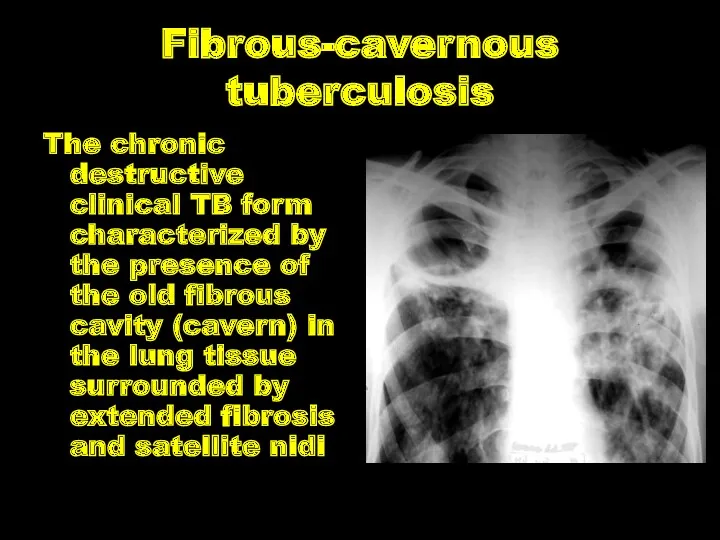
- 59. Fibrous-cavernous tuberculosis The chronic destructive clinical TB form characterized by the presence of the old fibrous
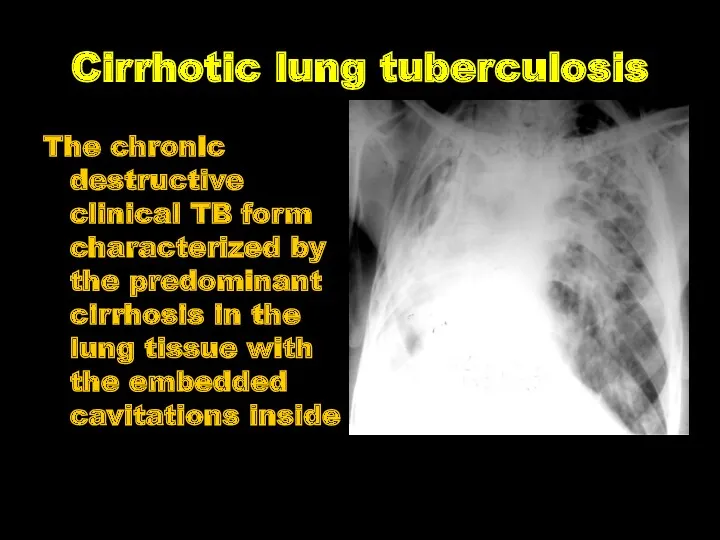
- 60. Cirrhotic lung tuberculosis The chronic destructive clinical TB form characterized by the predominant cirrhosis in the
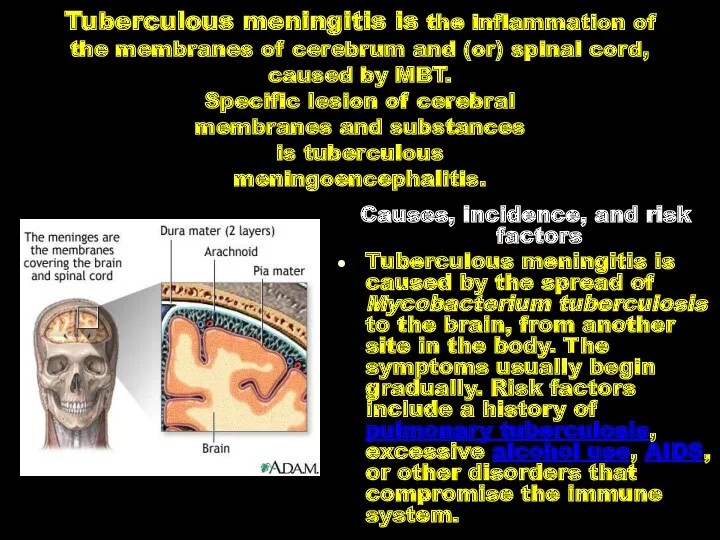
- 61. Tuberculous meningitis is the inflammation of the membranes of cerebrum and (or) spinal cord, caused by
- 62. Pathogenesis. Tuberculous meningitis may be primary (in 20 %) and secondary (in 80 %), as children
- 63. Pathological anatomy. The specific process is predominantly localized in the soft membrane of cerebral base, in
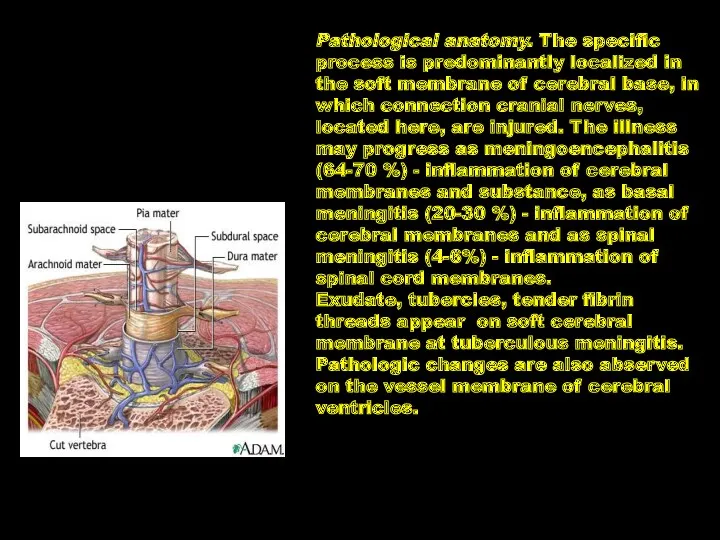
- 64. Clinic of Tuberculous meningitis I. A prodromic period the duration is from 1 to 4 weeks:
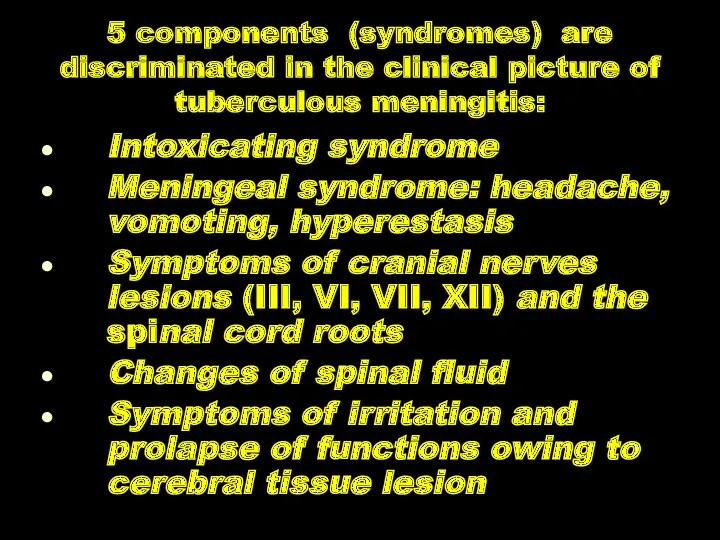
- 65. 5 components (syndromes) are discriminated in the clinical picture of tuberculous meningitis: Intoxicating syndrome Meningeal syndrome:
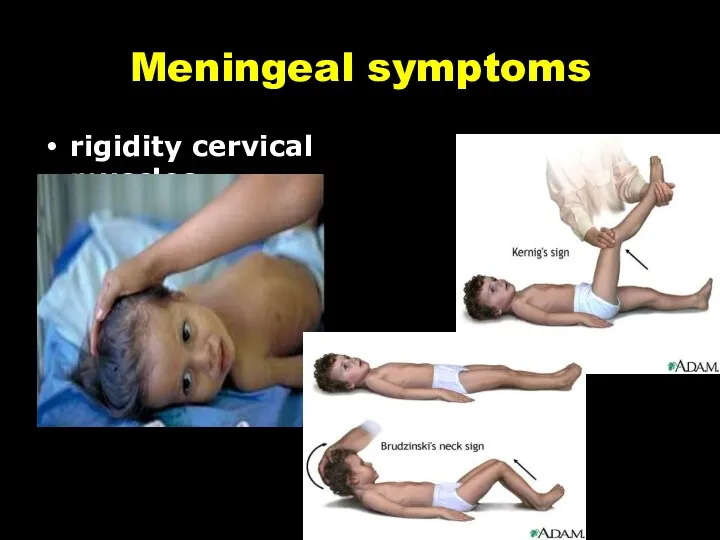
- 66. Meningeal symptoms rigidity cervical muscles
- 68. Скачать презентацию







 Врачебно-профессиональное консультирование подростков
Врачебно-профессиональное консультирование подростков Профилактика нарушений зрения у школьников
Профилактика нарушений зрения у школьников Системная склеродермия
Системная склеродермия Қалқанша безі гормондарының. Препараттары және антитиреоидты дәрілер
Қалқанша безі гормондарының. Препараттары және антитиреоидты дәрілер Переломы костей таза
Переломы костей таза Basics of parasitic diseases in surgery
Basics of parasitic diseases in surgery Клинико-психологическое сопровождение в рамках третичной профилактики пожилых с болезнью Пика
Клинико-психологическое сопровождение в рамках третичной профилактики пожилых с болезнью Пика Лабораторная диагностика туберкулёзной инфекции
Лабораторная диагностика туберкулёзной инфекции Приготовление детских лекарственных форм в условиях аптеки
Приготовление детских лекарственных форм в условиях аптеки Механическая травма. Синдром длительного сдавления. Переломы
Механическая травма. Синдром длительного сдавления. Переломы Общение медсестры с детьми
Общение медсестры с детьми Личная гигиена и профилактика пролежней. Питание и кормление пациентов
Личная гигиена и профилактика пролежней. Питание и кормление пациентов Инфаркт миокарда
Инфаркт миокарда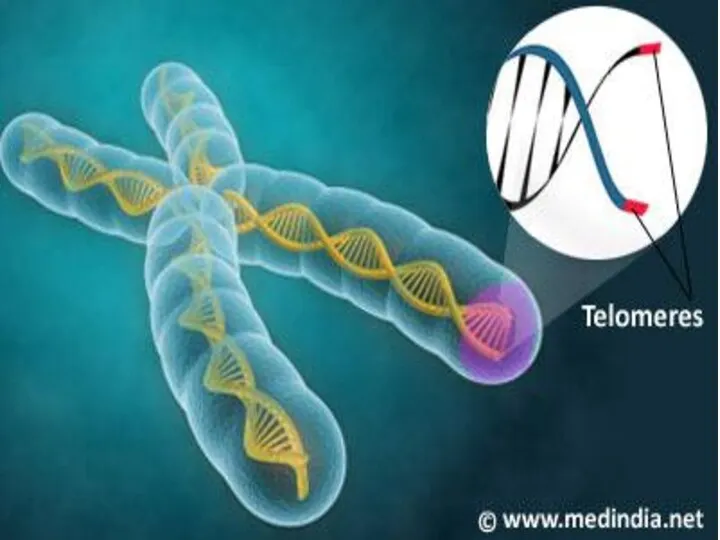 ДНК – ның теломерлік бөлімдерінің репликациялануы
ДНК – ның теломерлік бөлімдерінің репликациялануы Слизистые оболочки в норме и патологии
Слизистые оболочки в норме и патологии Менингококковая инфекция у детей
Менингококковая инфекция у детей Ас қорыту жолдарының ісіктері
Ас қорыту жолдарының ісіктері Этика и деонтология для работников регистратур медицинских организаций
Этика и деонтология для работников регистратур медицинских организаций Аномалии развития женской половой системы
Аномалии развития женской половой системы Кисты и свищи поджелудочной железы, классификация, диагностика, современные методы лечения
Кисты и свищи поджелудочной железы, классификация, диагностика, современные методы лечения Оказание первой медицинской помощи пострадавшим от действия электрического тока
Оказание первой медицинской помощи пострадавшим от действия электрического тока Әлеуметтік диагностика
Әлеуметтік диагностика Основы иммунитета
Основы иммунитета Подготовка к лабораторным исследованиям (2)
Подготовка к лабораторным исследованиям (2) Оказание медицинской помощи при остром коронарном синдроме (ОКС)
Оказание медицинской помощи при остром коронарном синдроме (ОКС) Аллергические состояния, проявления в полости рта. Клиника, диагностика, лечение
Аллергические состояния, проявления в полости рта. Клиника, диагностика, лечение № 2 Симптомдық артериальды гипертензия. № 3 вариант: Иценко-Кушинг синдромы кезіндегі
№ 2 Симптомдық артериальды гипертензия. № 3 вариант: Иценко-Кушинг синдромы кезіндегі Синдром уплотнения легочной ткани. Пневмония
Синдром уплотнения легочной ткани. Пневмония