Содержание
- 2. Emergencies Types Airway/Respiratory Intestinal Obstruction Intestinal Perforation Signs Respiratory distress Abdominal distension Peritonitis Pneumoperitoneum
- 3. Airway/Respiratory Neck Masses Cystic Hygromas Tracheal anomalies Thoracic masses/pulmonary lesions Congenital lobar emphysema Overdistension of one
- 4. Cystic Hygroma Multiloculated cystic spaces lined by endothelial cells Separated by fine walls containing numerous smooth
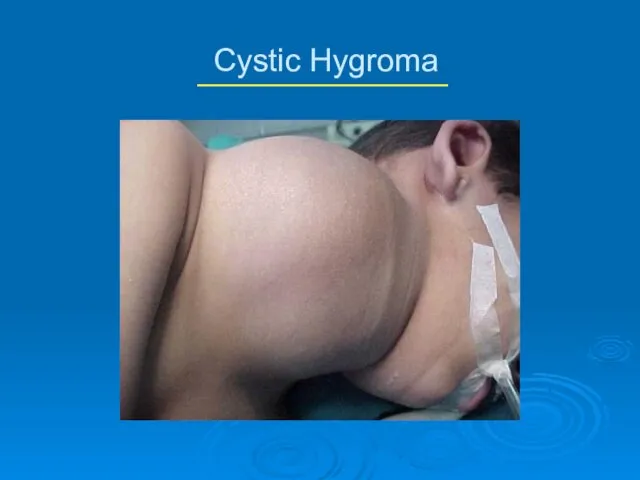
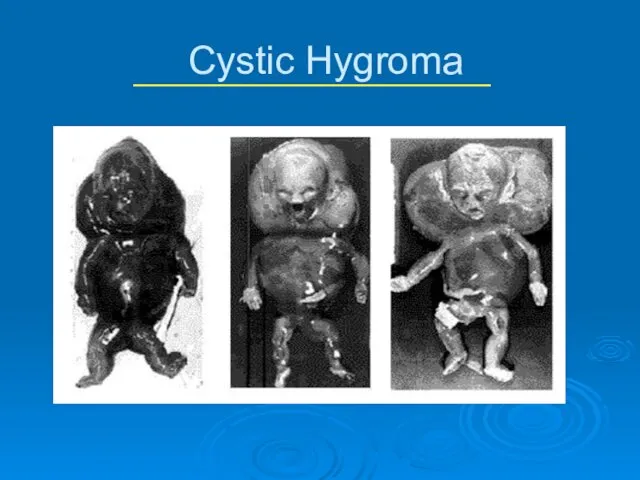
- 5. Cystic Hygroma Complications Respiratory—large hygromas can extend into oropharynx and trachea Inflammation/Infection Hemorrhage Treatment Dependent on
- 6. Cystic Hygroma
- 7. Cystic Hygroma
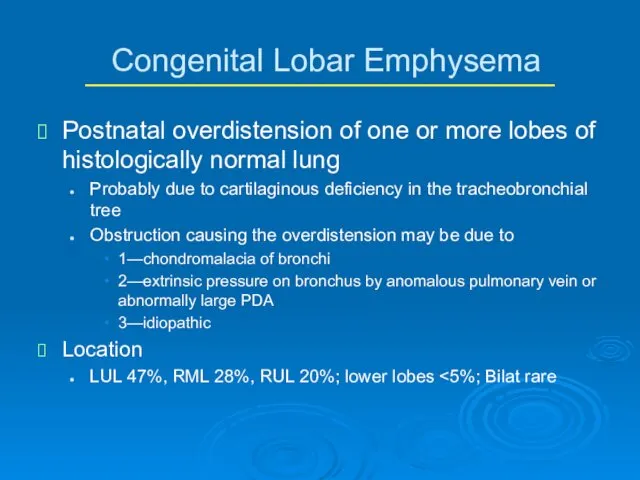
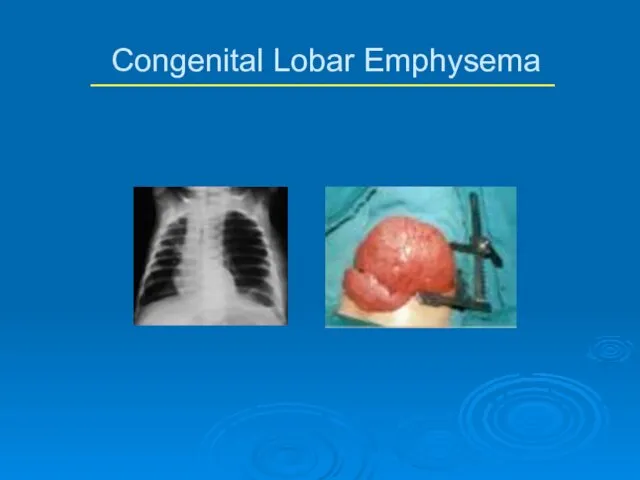
- 8. Postnatal overdistension of one or more lobes of histologically normal lung Probably due to cartilaginous deficiency
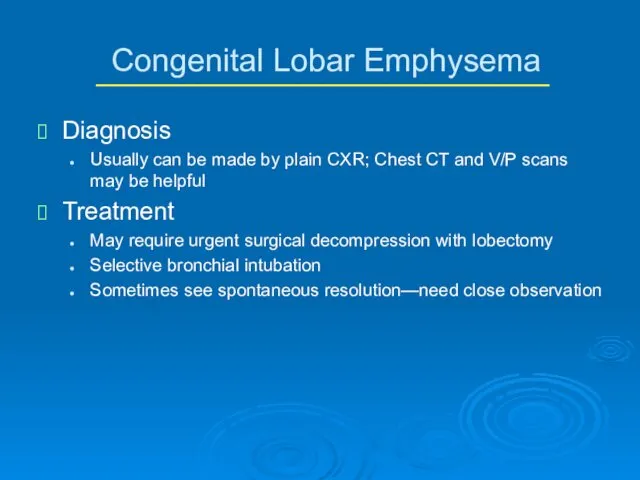
- 9. Congenital Lobar Emphysema Diagnosis Usually can be made by plain CXR; Chest CT and V/P scans
- 10. Congenital Lobar Emphysema
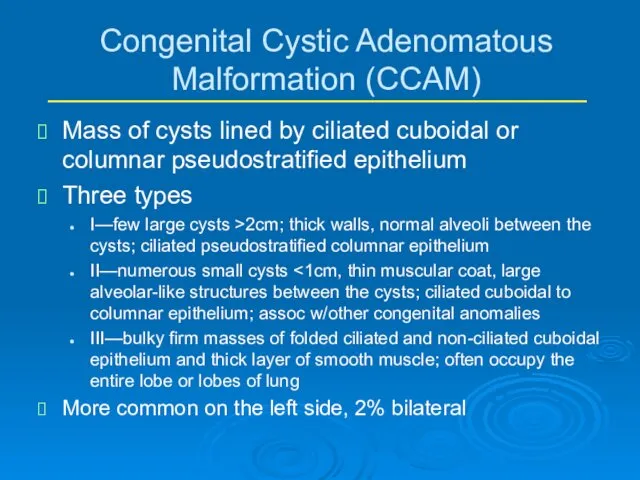
- 11. Congenital Cystic Adenomatous Malformation (CCAM) Mass of cysts lined by ciliated cuboidal or columnar pseudostratified epithelium
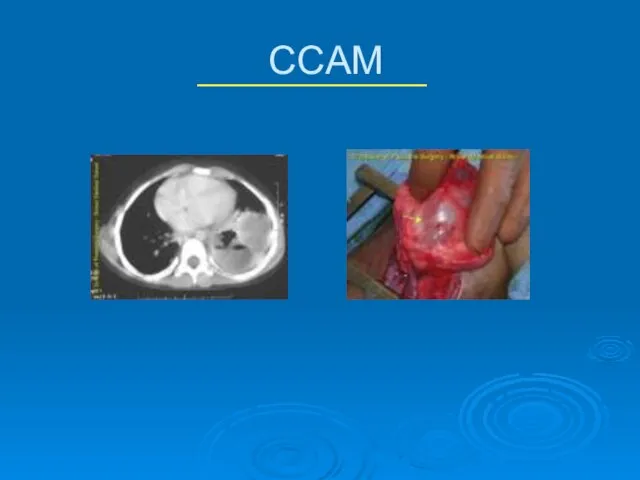
- 12. CCAM Diagnosis CT scan allows differentiation of types Some can be diagnosed on prenatal US Treatment
- 13. CCAM
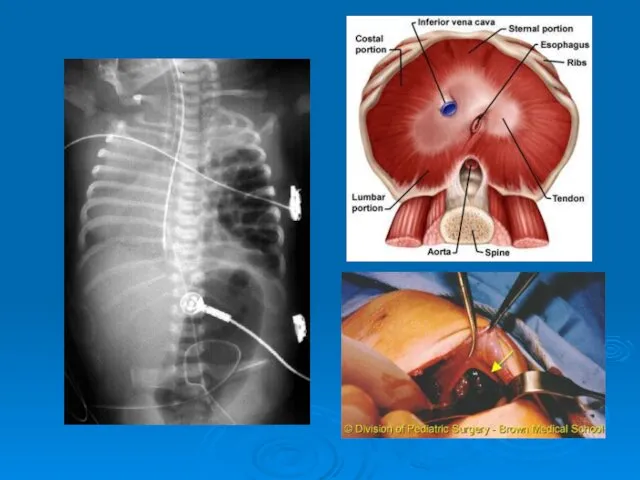
- 14. Congenital Diaphragmatic Hernia Intro 1 in 200-5000 live births, females >males Etiology unknown Large percentage of
- 16. Tracheoesophageal Fistula and Esophageal Atresia
- 19. Intestinal Obstruction Incidence approx 1 per 500-1000 live births Approx 50% due to atresia or stenosis
- 20. Anatomic Differentiation Upper GI Duodenal atresias/webs small bowel atresias malrotation/midgut volvulus GERD Meconium ileus pyloric stenosis
- 21. Lower GI Colonic atresia Meconium plug Hirschsprung’s Small Left Colon Syndrome Magalocystis-Microcolon-Intestinal Hypoperistalsis Syndrome Imperforate anus
- 22. Urgency to Treat Emergencies Free air on KUB Peritonitis Acute increase in abd distension Clinical deterioration
- 23. Urgency to Treat Further workup Contrast enemas for distal obstructions KUB/Cross-table lateral Milk Scans for GERD
- 24. Common Disorders NEC Duodenal Atresia Small Bowel Atresia Malrotation/Volvulus Hirschsprung’s
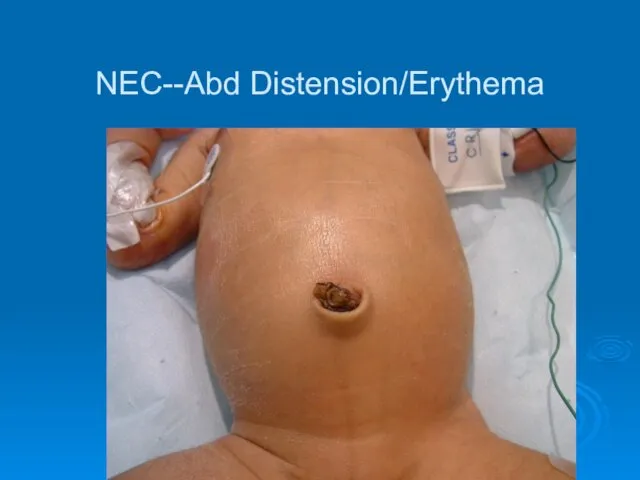
- 25. NEC Con’t Presentation distension, tachycardia, lethargy, bilious output, heme pos stools, oliguria DX clinical KUB may
- 26. NEC Treatment Medical NPO, sump tube, Broad Abx after cx’s drawn, serial KUB/lateral x-rays, frequent abd
- 27. NEC Outcomes Overall survival ~ 80%, improving in LBW In pts w/perforation, 65% perioperative mortality, no
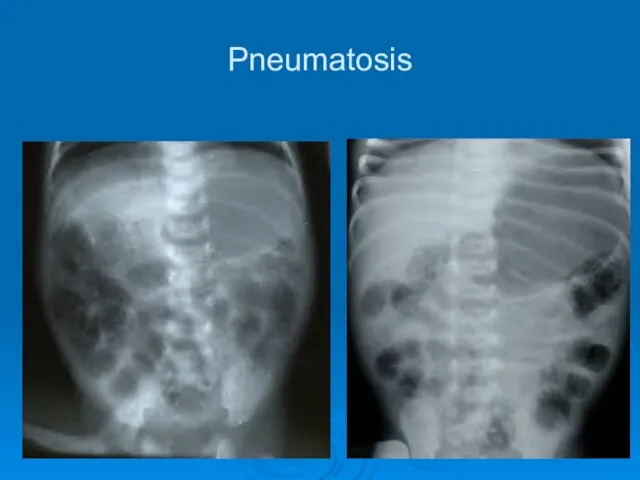
- 28. Pneumatosis
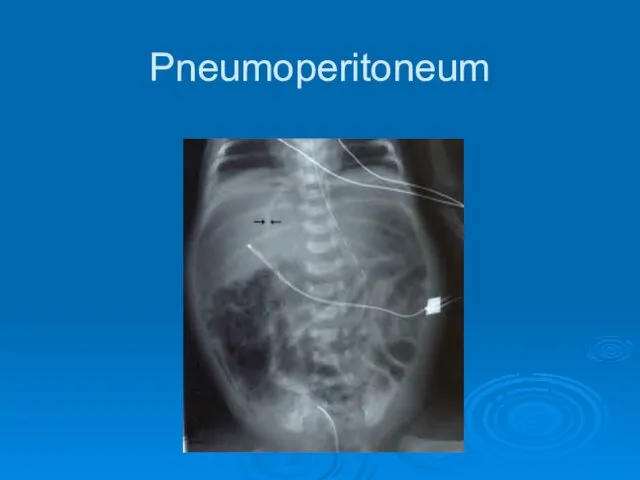
- 29. Pneumoperitoneum
- 30. NEC--Abd Distension/Erythema
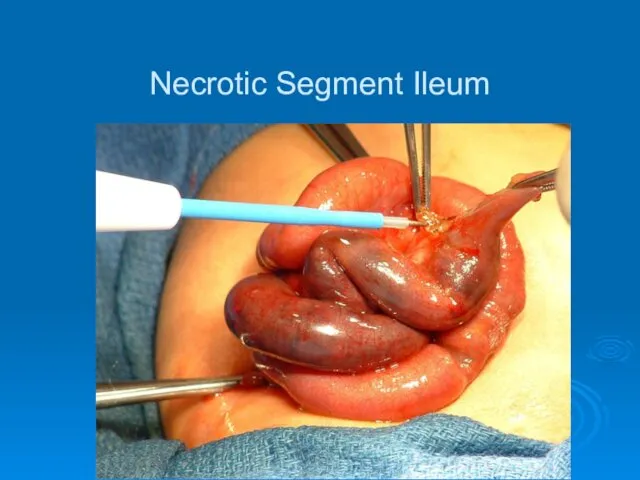
- 31. Necrotic Segment Ileum
- 32. Resection
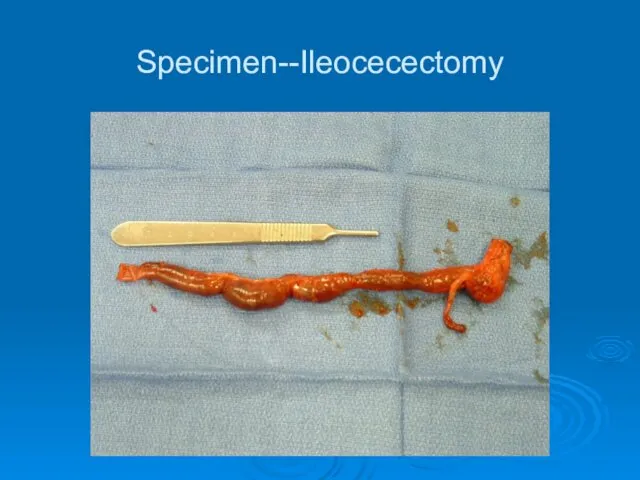
- 33. Specimen--Ileocecectomy
- 34. Ileostomy
- 35. Common Disorders NEC Duodenal Atresia Small Bowel Atresia Malrotation Hirschsprung’s
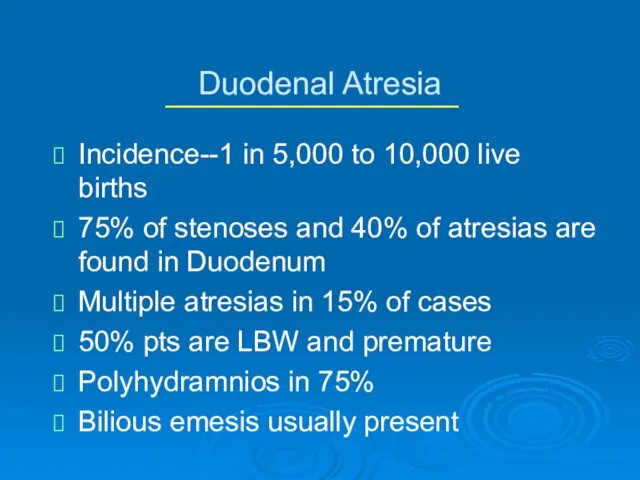
- 36. Duodenal Atresia Incidence--1 in 5,000 to 10,000 live births 75% of stenoses and 40% of atresias
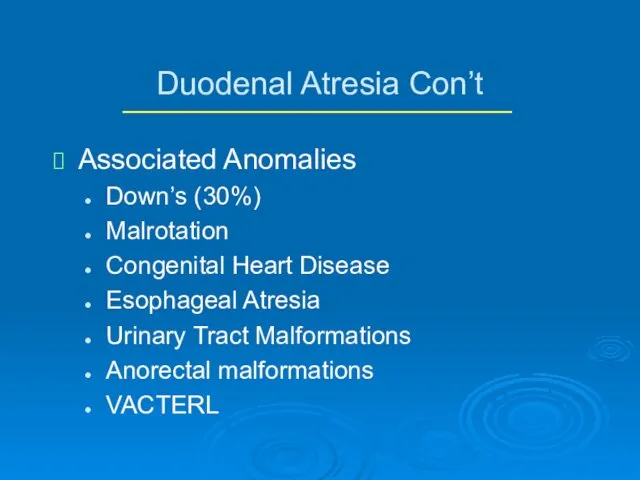
- 37. Duodenal Atresia Con’t Associated Anomalies Down’s (30%) Malrotation Congenital Heart Disease Esophageal Atresia Urinary Tract Malformations
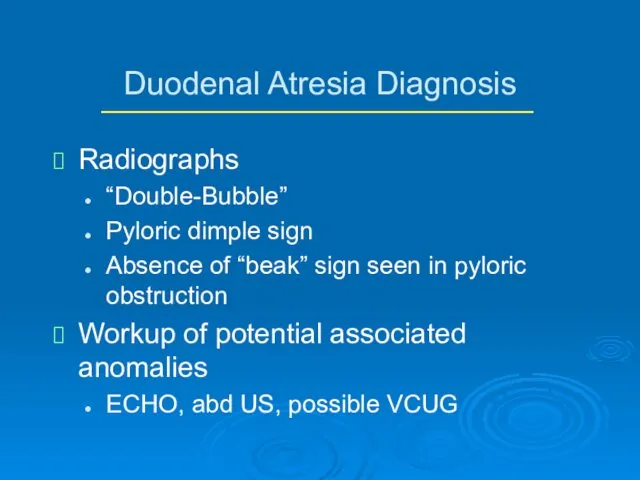
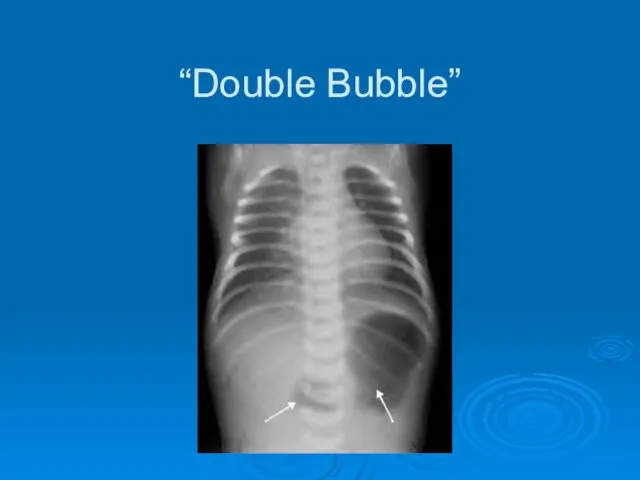
- 38. Duodenal Atresia Diagnosis Radiographs “Double-Bubble” Pyloric dimple sign Absence of “beak” sign seen in pyloric obstruction
- 39. “Double Bubble”
- 40. Duodenal Atresia Treatment Nasogastric decompression, hydration Surgery Double diamond duodenoduodenostomy Con’t prolonged NG decompression, sometimes more
- 41. Common Disorders NEC Duodenal Atresia Small Bowel Atresia Malrotation Hirschsprung’s
- 42. Small Bowel Atresia Jejunal is most common, about 1 per 2,000 live births Atresia due to
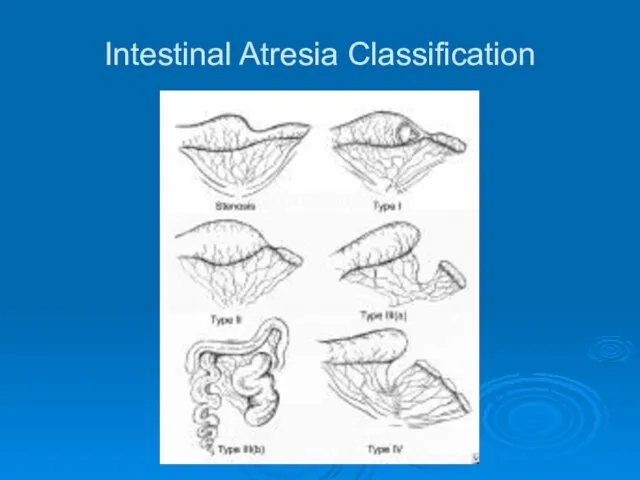
- 43. Intestinal Atresia Classification
- 44. Small Bowel Atresia Con’t Associated Anomalies other atresias Hirschsprung’s Biliary atresia polysplenia syndrome (situs inversus, cardiac
- 45. Atresia--Diagnosis and Treatment Plain films show dilated loops small bowel Contrast enema shows small unused colon
- 46. Common Disorders NEC Duodenal Atresia Small Bowel Atresia Malrotation/Volvulus Hirschsprung’s
- 47. Malrotation 1 per 6,000 live births can be asymptomatic throughout life Usually presents in first 6
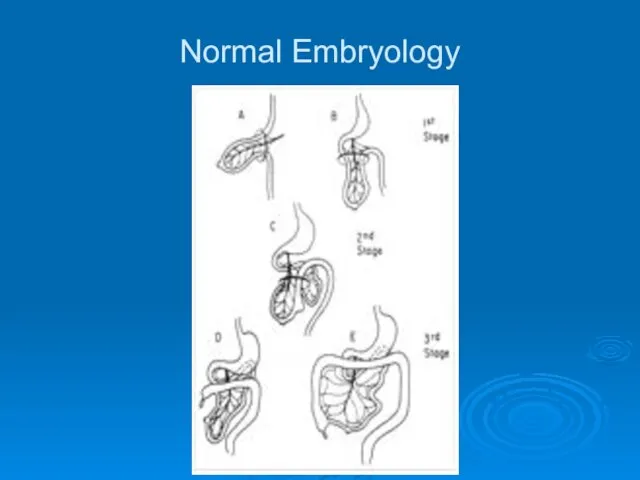
- 48. Normal Embryology
- 49. Malrotation Classification Nonrotation when neither duodenojejunal or cecocolic limbs undergo correct rotation Abn Rotation of Duodenojejunal
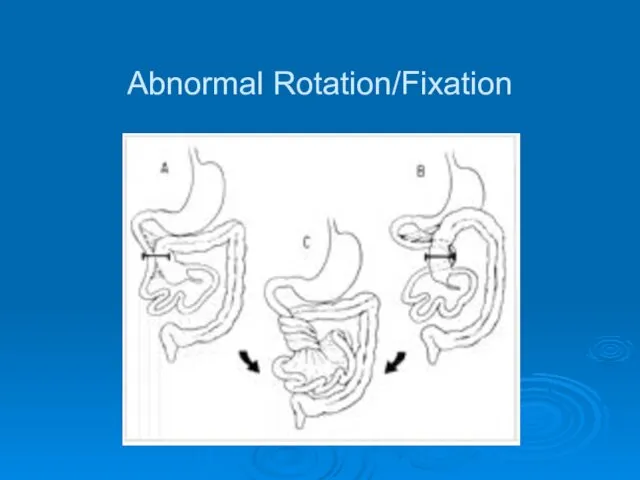
- 50. Abnormal Rotation/Fixation
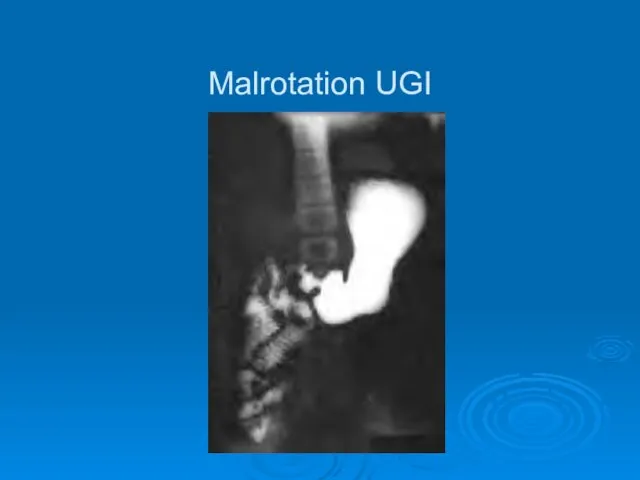
- 51. Malrotation Diagnosis Varying symptoms from very mild to catastrophic **Bilious emesis is Volvulus until proven otherwise**
- 52. Malrotation UGI
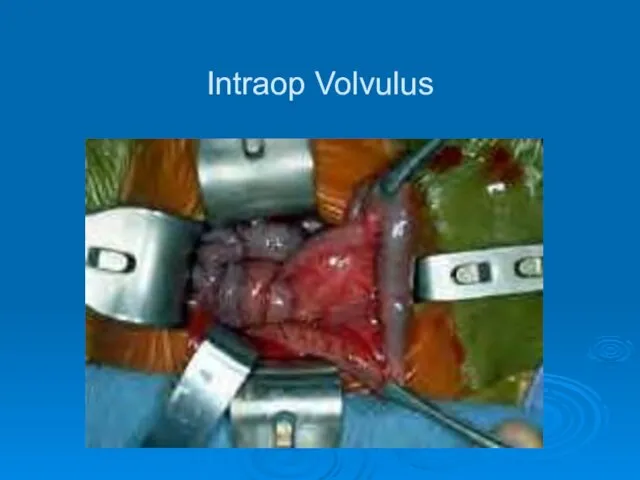
- 53. Intraop Volvulus
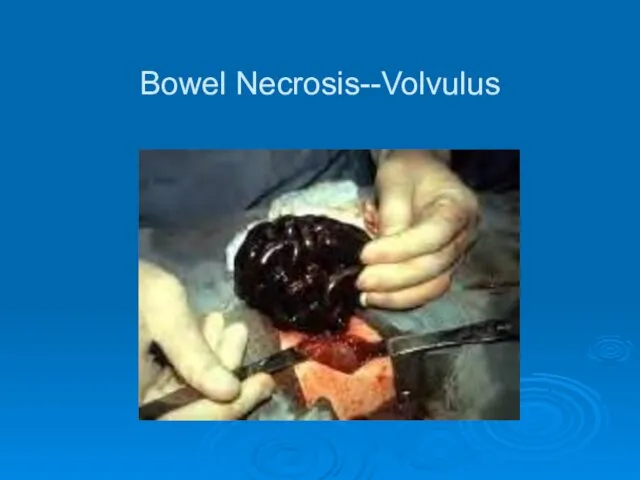
- 54. Bowel Necrosis--Volvulus
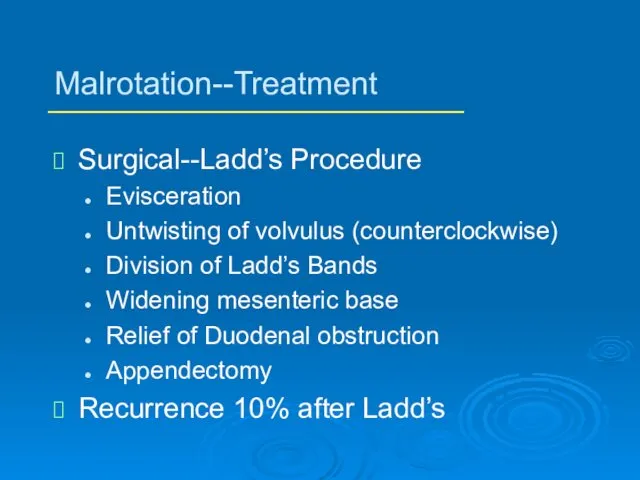
- 55. Malrotation--Treatment Surgical--Ladd’s Procedure Evisceration Untwisting of volvulus (counterclockwise) Division of Ladd’s Bands Widening mesenteric base Relief
- 56. Common Disorders NEC Duodenal Atresia Small Bowel Atresia Malrotation Hirschsprung’s
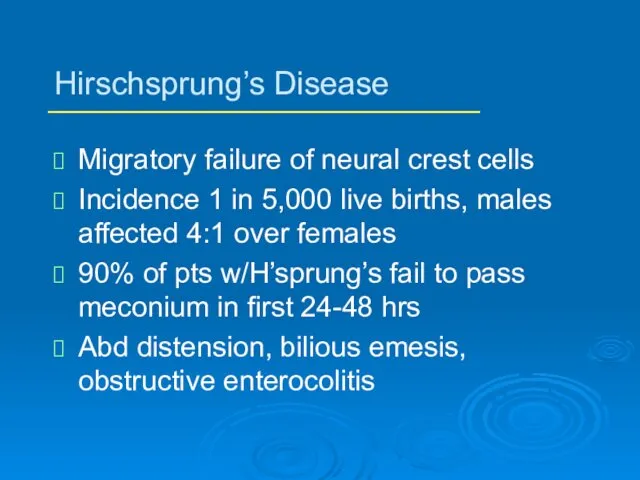
- 57. Hirschsprung’s Disease Migratory failure of neural crest cells Incidence 1 in 5,000 live births, males affected
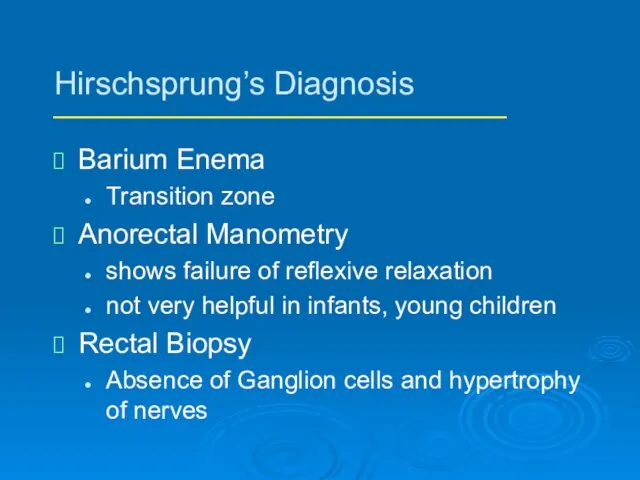
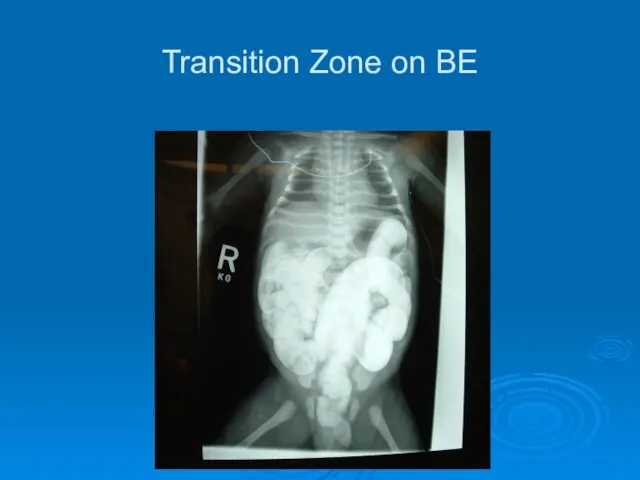
- 58. Hirschsprung’s Diagnosis Barium Enema Transition zone Anorectal Manometry shows failure of reflexive relaxation not very helpful
- 59. Transition Zone on BE
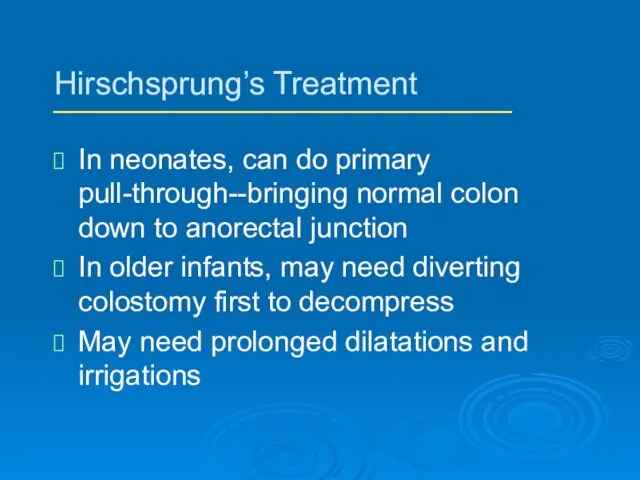
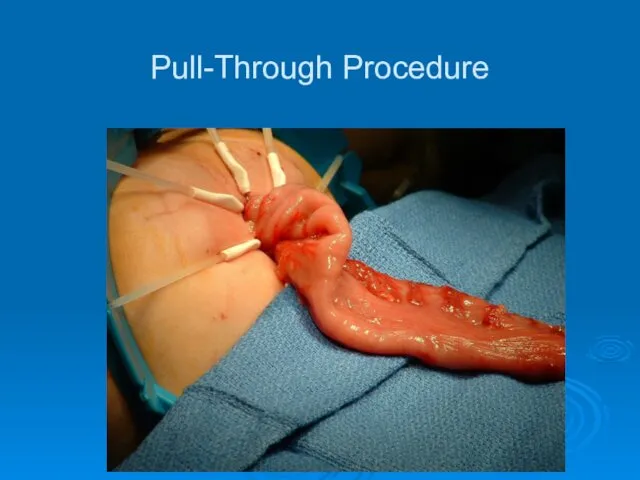
- 60. Hirschsprung’s Treatment In neonates, can do primary pull-through--bringing normal colon down to anorectal junction In older
- 61. Pull-Through Procedure
- 64. Скачать презентацию






 Психологические особенности женщин на этапе подготовки ЭКО (психоаналитический подход)
Психологические особенности женщин на этапе подготовки ЭКО (психоаналитический подход) Клиническая эпидемиология
Клиническая эпидемиология Язвенно-некротический энтероколит новорожденных
Язвенно-некротический энтероколит новорожденных Первичные вирусные энцефалиты у детей
Первичные вирусные энцефалиты у детей Анатомо-физиологические особенности строения полости рта новорожденного
Анатомо-физиологические особенности строения полости рта новорожденного Вірус віспи
Вірус віспи Принципы гигиенической регламентации химических веществ
Принципы гигиенической регламентации химических веществ Биологические эффекты воздействия ионизирующего излучения на организм человека
Биологические эффекты воздействия ионизирующего излучения на организм человека Смерть клиническая и биологическая
Смерть клиническая и биологическая Алгоритмы диагностики в общей врачебной практике, семейной медицине
Алгоритмы диагностики в общей врачебной практике, семейной медицине КОГБУЗ Яранская центральная районная больница
КОГБУЗ Яранская центральная районная больница Тромбоз. Причины, диагностика
Тромбоз. Причины, диагностика Трихоцефалёз. Этиология. Клиника. Диагностика. Лечение
Трихоцефалёз. Этиология. Клиника. Диагностика. Лечение Технология гомеопатических таблеток. Викторина
Технология гомеопатических таблеток. Викторина Воспалительные заболевания женских половых органов
Воспалительные заболевания женских половых органов Методы оценки удовлетворенности пациента качеством предоставленных медицинских услуг
Методы оценки удовлетворенности пациента качеством предоставленных медицинских услуг Пролиферациялық қабыну
Пролиферациялық қабыну Бешенство
Бешенство Профилактика ОРВИ и гриппа
Профилактика ОРВИ и гриппа Ұйқы физилогиясы.Ұйқы фазасы,бұзылысы және емдеу әдісі
Ұйқы физилогиясы.Ұйқы фазасы,бұзылысы және емдеу әдісі Развитие глотки, пищевода, желудка, кишечника
Развитие глотки, пищевода, желудка, кишечника Ретинобластома – злокачественная опухоль сетчатки глаза
Ретинобластома – злокачественная опухоль сетчатки глаза Внебольничные пневмонии и грипп
Внебольничные пневмонии и грипп Терминальные состояния
Терминальные состояния Трансвагинальная эхография в первом триместре беременности
Трансвагинальная эхография в первом триместре беременности Лучевое исследование легких
Лучевое исследование легких ДВС-синдром. ТЭЛА
ДВС-синдром. ТЭЛА