Содержание
- 2. Tuberculosis (TB), which is caused by bacteria of the Mycobacterium tuberculosis complex, is one of the
- 3. If properly treated, TB caused by drug-susceptible strains is curable in the vast majority of cases.
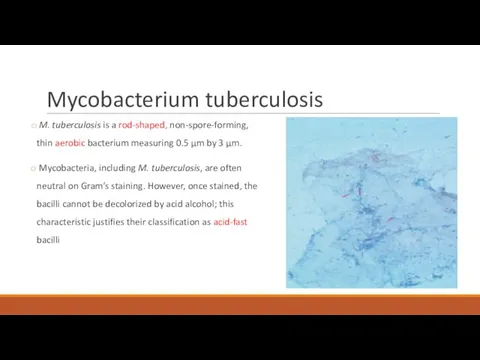
- 4. Mycobacterium tuberculosis M. tuberculosis is a rod-shaped, non-spore-forming, thin aerobic bacterium measuring 0.5 μm by 3
- 5. Transmission and infection Transmission usually takes place through the airborne spread of droplet nuclei produced by
- 6. Most infectious patients: Cavitary pulmonary disease or, much less common, laryngeal TB Patients with positive sputum
- 7. Natural history of the disease 10% of infected persons will eventually develop active TB in their
- 8. TB is classified as pulmonary, extrapulmonary, or both. Depending on several factors linked to different populations
- 9. Pulmonary TB
- 10. Primary Pulmonary TB Clinical illness directly following infection. Is common among children and immunocompromised persons. May
- 11. Symptoms May be asymptomatic or may present with fever and occasionally pleuritic chest pain. Most commonly
- 12. In young children and in persons with impaired immunity (e.g. malnutrition or HIV), primary pulmonary TB
- 13. Bronchiectasis may develop in any segment/lobe damaged by progressive caseating pneumonia. Occult hematogenous dissemination commonly follows
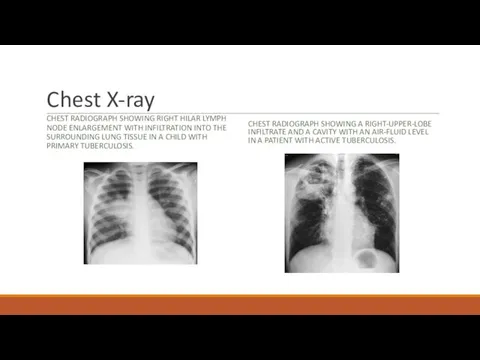
- 14. Chest X-ray CHEST RADIOGRAPH SHOWING RIGHT HILAR LYMPH NODE ENLARGEMENT WITH INFILTRATION INTO THE SURROUNDING LUNG
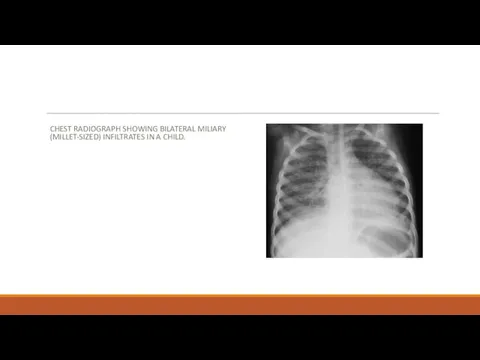
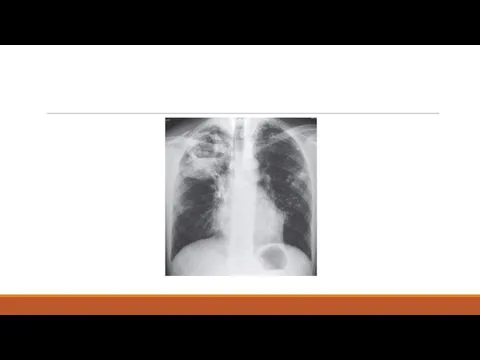
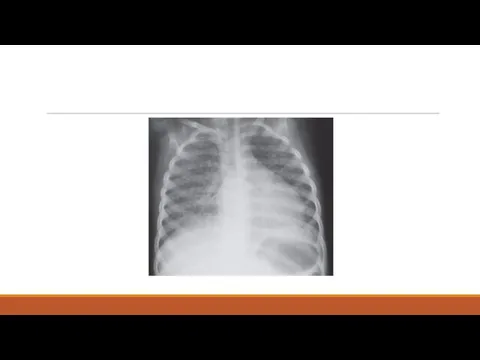
- 15. CHEST RADIOGRAPH SHOWING BILATERAL MILIARY (MILLET-SIZED) INFILTRATES IN A CHILD.
- 16. Secondary Pulmonary TB Bacilli may reactivate after many years because of frequent cavitation, is more often
- 17. Symptoms Early in the course of disease symptoms and signs are often nonspecific: fever, chills, night
- 19. Hemoptysis develops in 20-30% of cases, and massive hemoptysis may ensue as a consequence of the
- 20. Diagnosis Physical findings are of limited use in pulmonary TB. The most common hematologic findings are
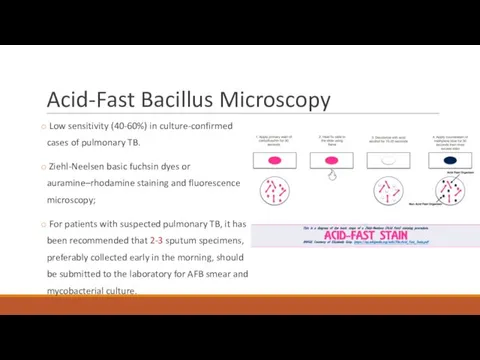
- 21. Acid-Fast Bacillus Microscopy Low sensitivity (40-60%) in culture-confirmed cases of pulmonary TB. Ziehl-Neelsen basic fuchsin dyes
- 22. Gene Xpert Fully automated amplification of mycobacterial nucleic acid (DNA PCR) Most useful for the rapid
- 23. Mycobacteria culture A low-cost Definitive diagnosis MGIT cultures usually become positive after a period ranging from
- 24. Drug Susceptibility testing Any initial isolate of M. tuberculosis should be tested for susceptibility to isoniazid
- 25. HIV-ASSOCIATED TB Likely main cause of infectious-related death in this population If CD4 is low (less
- 26. Treatment The two main aims of TB treatment: to prevent morbidity and death by curing TB
- 27. Isoniazid (H) – s/e liver toxicity, peripheral neuropathy (should be administered with pyridoxine) Rifampin (R) –
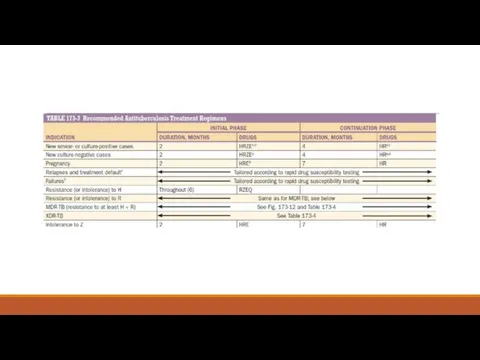
- 28. Treatment regimen Divided into 2 phases: An initial, or bactericidal phase - the majority of the
- 30. Patients with pulmonary disease should have their sputum examined monthly until cultures become negative to allow
- 31. Treatment failure and relapse Current isolate must be urgently tested for susceptibility to first- and second-line
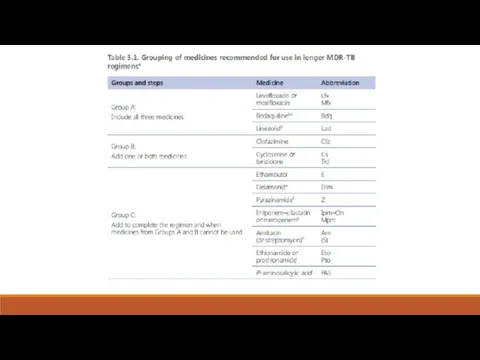
- 32. MDR-TB treatment For the treatment of patients with isoniazid-resistant disease, it is recommended to use a
- 33. In 2013 and 2014, respectively, bedaquiline and delamanid—the first two drugs specifically developed for TB during
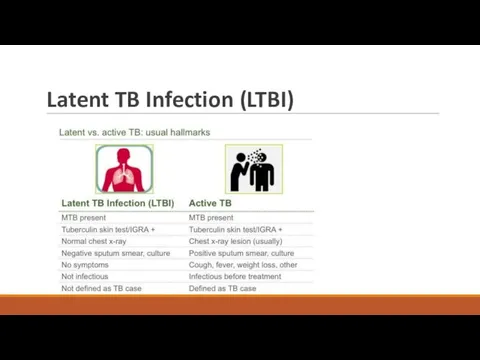
- 35. Latent TB Infection (LTBI)
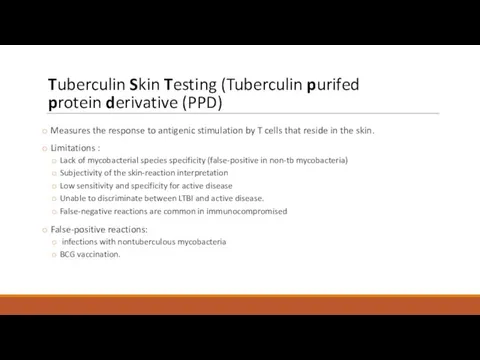
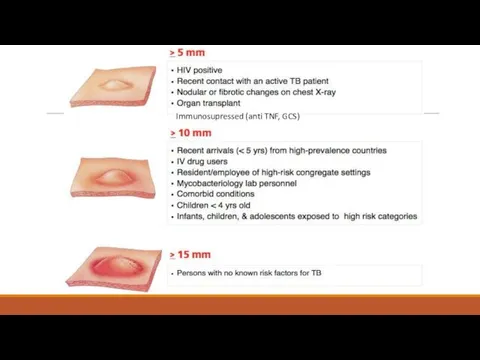
- 36. Tuberculin Skin Testing (Tuberculin purifed protein derivative (PPD) Measures the response to antigenic stimulation by T
- 38. Immunosupressed (anti TNF, GCS)
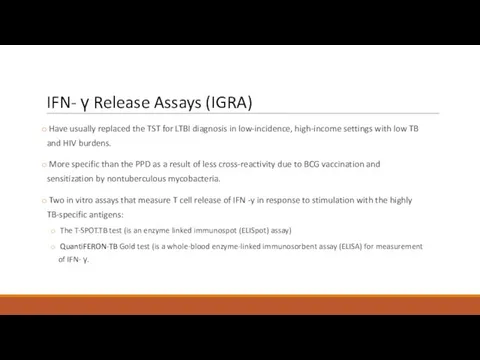
- 39. IFN- γ Release Assays (IGRA) Have usually replaced the TST for LTBI diagnosis in low-incidence, high-income
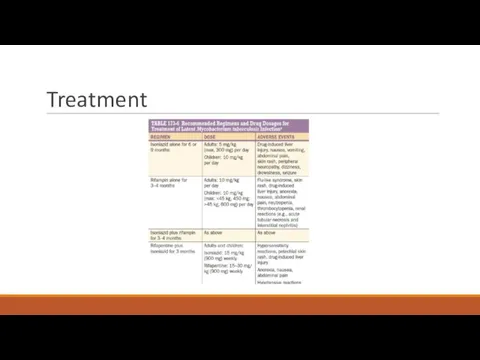
- 40. Treatment
- 41. PREVENTION The best way to prevent TB is to diagnose and isolate infectious cases rapidly and
- 42. Extrapulmonary TB
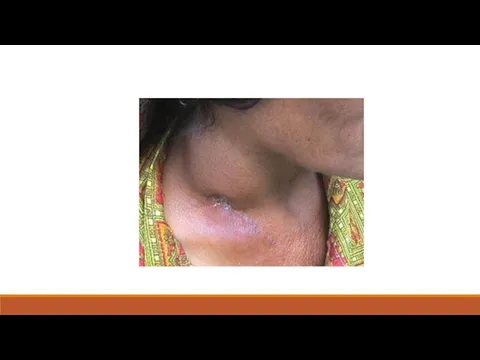
- 43. Tuberculous Lymphadenitis Most commo form of extrapulmonary TB (35-40%) Cervical adenopathy Peak age of onset of
- 45. Pleural Tuberculosis Cough, pleuritic chest pain, fever, or dyspnea. Small to moderate, unilateral pleural effusion About
- 46. TB of the Upper Airways Nearly always a complication of advanced cavitary pulmonary TB May involve
- 47. Genitourinary TB ~10–15% of all extrapulmonary cases Urinary frequency, dysuria, nocturia, hematuria, and flank or abdominal
- 48. Skeletal Tuberculosis ~10% of extrapulmonary cases. Most often involves the spine, arthritis in weight-bearing joints and
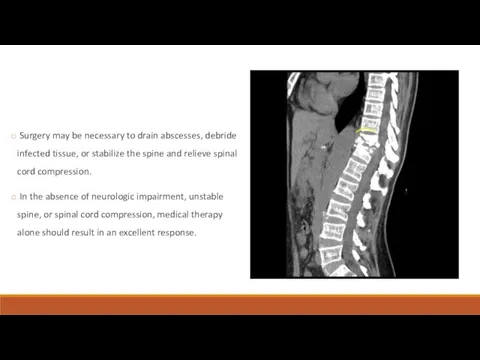
- 49. Surgery may be necessary to drain abscesses, debride infected tissue, or stabilize the spine and relieve
- 50. Meningitis ~5% of extrapulmonary cases Acute or subacute Headache and slight mental changes after a pro-drome
- 51. MILIARY TUBERCULOSIS Any progressive, disseminated form of tuberculosis; the disease can occur during primary dissemination or
- 54. THANK YOU!
- 55. QUESTIONS
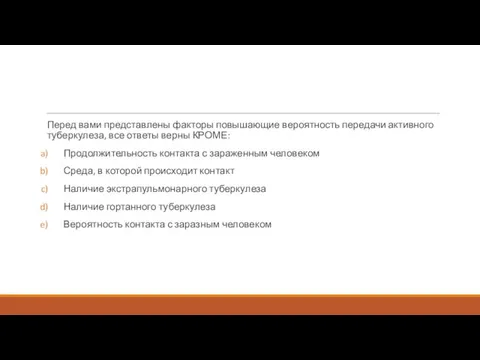
- 56. Перед вами представлены факторы повышающие вероятность передачи активного туберкулеза, все ответы верны КРОМЕ: Продолжительность контакта с
- 57. 42-летний мужчина из Нигерии приезжает в отделение реанимации из-за высокой температуры, усталости, потери веса и кашля
- 59. Перевести пациента на воздушнокапельный карантин, пока три анализа мокроты не придут с признаками присутсвия кислотоустойчивых бацилл.
- 60. 18-летний молодой человек из Южной Африки пришел в клинику с жалобами из 2 недельного прогрессирующего недомогания
- 62. Диссеминированный Экстрапульмонарный Лимфаденит Плевральный Вторичный кавитарный
- 63. 50-летний человек госпитализирован в связи с активным легочным туберкулезом с положительным мазком мокроты на кислотоустойчивые бациллы.
- 64. Все следующие люди, получающие реакции PPD туберкулина кожи, должны лечиться с связи подозрением на скрытый туберкулез
- 66. Скачать презентацию












 Улучшение качества материнской и неонатальной помощи. (Модуль 15)
Улучшение качества материнской и неонатальной помощи. (Модуль 15) Синдром легочной диссеминации. Диссеминированный туберкулез легких
Синдром легочной диссеминации. Диссеминированный туберкулез легких Нейроофтальмологические нарушения при нейромышечных заболеваниях
Нейроофтальмологические нарушения при нейромышечных заболеваниях Острые пневмонии у детей
Острые пневмонии у детей Приклади хвороби органів ШКТ
Приклади хвороби органів ШКТ Введение в фитотерапию
Введение в фитотерапию Ранняя диагностика острого лейкоза у детей
Ранняя диагностика острого лейкоза у детей Синдром диабетической стопы
Синдром диабетической стопы О вреде абортов
О вреде абортов Рак слизистой оболочки полости рта. Клиника, диагностика, лечение
Рак слизистой оболочки полости рта. Клиника, диагностика, лечение Семиотика заболеваний мочевой системы у детей
Семиотика заболеваний мочевой системы у детей Автоматические поточные линии
Автоматические поточные линии ЭКГ
ЭКГ Педиатрия как наука о здоровом и больном ребёнке.Место педиатрии в системе общей медицины. Возрастная периодизация в педиатрии
Педиатрия как наука о здоровом и больном ребёнке.Место педиатрии в системе общей медицины. Возрастная периодизация в педиатрии Острая кишечная непроходимость у детей
Острая кишечная непроходимость у детей Гестационная трофобластическая болезнь
Гестационная трофобластическая болезнь Медицина в Средневековье
Медицина в Средневековье Кровообращение и гомеостаз
Кровообращение и гомеостаз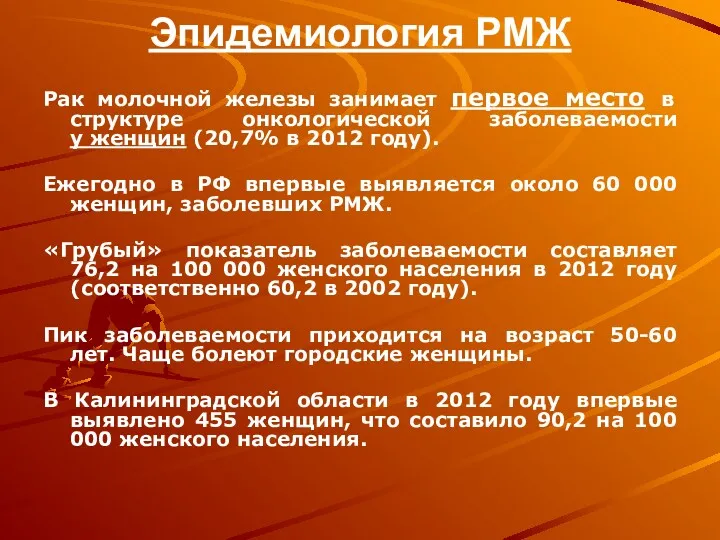 Эпидемиология РМЖ
Эпидемиология РМЖ Метаболический синдром и НАЖБП в современных условиях. Актуальность коморбидности
Метаболический синдром и НАЖБП в современных условиях. Актуальность коморбидности Гигиена аптечных заведений
Гигиена аптечных заведений Клубные наркотики
Клубные наркотики Логопедия. Дизартрия
Логопедия. Дизартрия Координаторная сфера. Мозжечок. Синдромы поражения
Координаторная сфера. Мозжечок. Синдромы поражения Орально-мануальные техники
Орально-мануальные техники Анатомо-физиологические особенности лёгких. (Лекция 11)
Анатомо-физиологические особенности лёгких. (Лекция 11) Общественное здоровье-высшая ценность человечества
Общественное здоровье-высшая ценность человечества Ерте жастағы балалардағы сөйлеу тілінің тежелуінің алдын алудың ерекшеліктері
Ерте жастағы балалардағы сөйлеу тілінің тежелуінің алдын алудың ерекшеліктері