Содержание
- 2. Туберкулез верхних дыхательных путей как самостоятельное заболевание диагностируют очень редко. Наиболее часто эта форма является осложнением
- 3. Case report I A 48 year-old male presented with history of sore throat, occasional fever, malaise
- 4. Случай 1 48-летний мужчина с историей боли в горле, прерывная лихорадка, недомогание на протяжении 1 года.
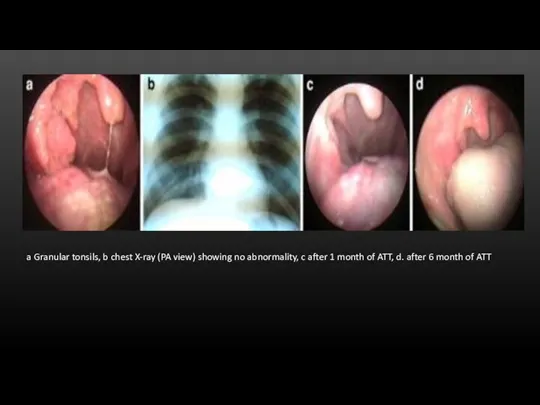
- 5. a Granular tonsils, b chest X-ray (PA view) showing no abnormality, c after 1 month of
- 6. Biopsy was taken from ulcerated area of right tonsils and sent for histopathological examination. Histology revealed
- 7. Case report II A 22 year old female presented with a history of odynophagia, haemoptysis, occasional
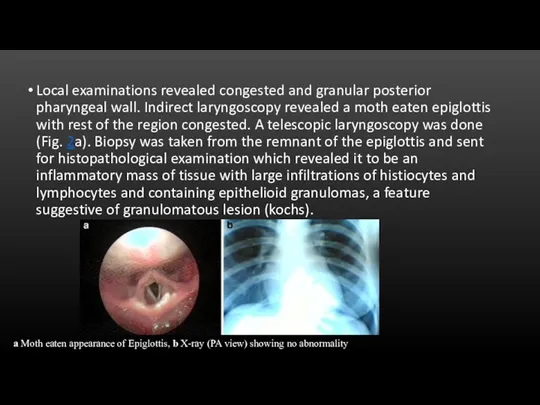
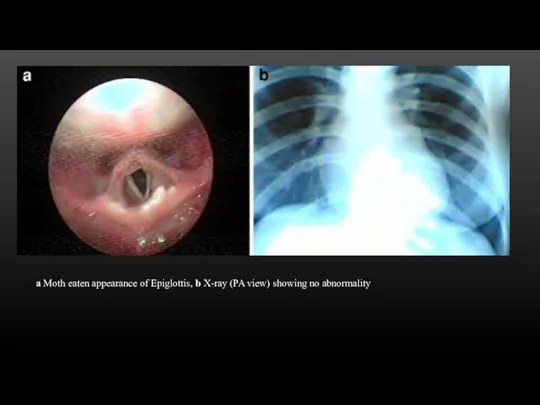
- 8. Local examinations revealed congested and granular posterior pharyngeal wall. Indirect laryngoscopy revealed a moth eaten epiglottis
- 9. a Moth eaten appearance of Epiglottis, b X-ray (PA view) showing no abnormality
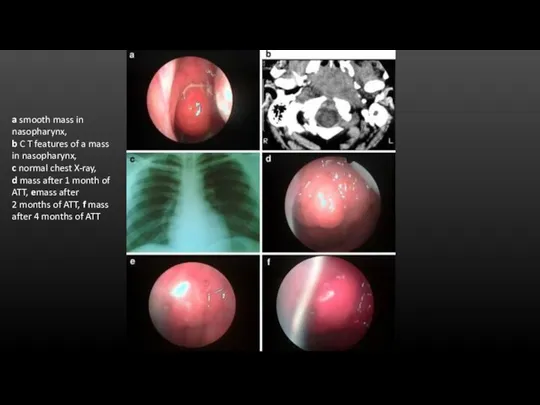
- 10. Case report III A 24 year old male student presented in the OPD with history of
- 11. a smooth mass in nasopharynx, b C T features of a mass in nasopharynx, c normal
- 12. Case report III With all the above mentioned investigations, a diagnosis of primary tuberculosis of nasopharynx
- 13. Conclusion Commonly URT primary TB can be misdiagnosed as traumatic or aphthous ulcer, haematological disorder, other
- 15. Скачать презентацию
 Врачебно-профессиональное консультирование подростков
Врачебно-профессиональное консультирование подростков Профилактика нарушений зрения у школьников
Профилактика нарушений зрения у школьников Системная склеродермия
Системная склеродермия Қалқанша безі гормондарының. Препараттары және антитиреоидты дәрілер
Қалқанша безі гормондарының. Препараттары және антитиреоидты дәрілер Переломы костей таза
Переломы костей таза Basics of parasitic diseases in surgery
Basics of parasitic diseases in surgery Клинико-психологическое сопровождение в рамках третичной профилактики пожилых с болезнью Пика
Клинико-психологическое сопровождение в рамках третичной профилактики пожилых с болезнью Пика Лабораторная диагностика туберкулёзной инфекции
Лабораторная диагностика туберкулёзной инфекции Приготовление детских лекарственных форм в условиях аптеки
Приготовление детских лекарственных форм в условиях аптеки Механическая травма. Синдром длительного сдавления. Переломы
Механическая травма. Синдром длительного сдавления. Переломы Общение медсестры с детьми
Общение медсестры с детьми Личная гигиена и профилактика пролежней. Питание и кормление пациентов
Личная гигиена и профилактика пролежней. Питание и кормление пациентов Инфаркт миокарда
Инфаркт миокарда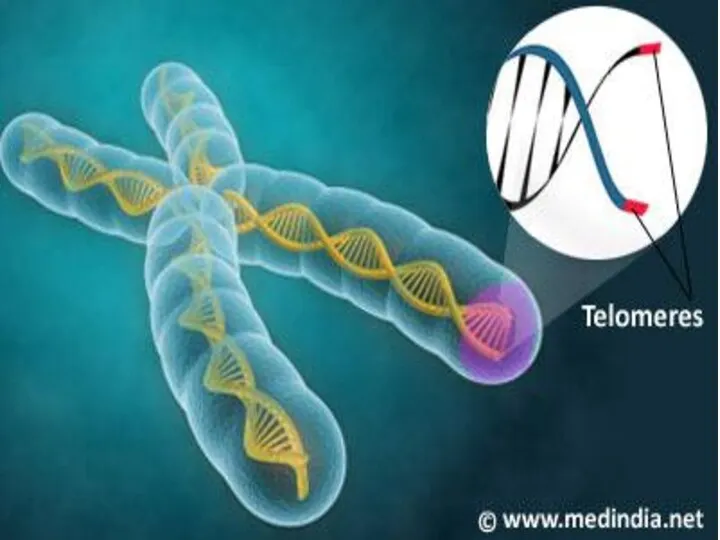 ДНК – ның теломерлік бөлімдерінің репликациялануы
ДНК – ның теломерлік бөлімдерінің репликациялануы Слизистые оболочки в норме и патологии
Слизистые оболочки в норме и патологии Менингококковая инфекция у детей
Менингококковая инфекция у детей Ас қорыту жолдарының ісіктері
Ас қорыту жолдарының ісіктері Этика и деонтология для работников регистратур медицинских организаций
Этика и деонтология для работников регистратур медицинских организаций Аномалии развития женской половой системы
Аномалии развития женской половой системы Кисты и свищи поджелудочной железы, классификация, диагностика, современные методы лечения
Кисты и свищи поджелудочной железы, классификация, диагностика, современные методы лечения Оказание первой медицинской помощи пострадавшим от действия электрического тока
Оказание первой медицинской помощи пострадавшим от действия электрического тока Әлеуметтік диагностика
Әлеуметтік диагностика Основы иммунитета
Основы иммунитета Подготовка к лабораторным исследованиям (2)
Подготовка к лабораторным исследованиям (2) Оказание медицинской помощи при остром коронарном синдроме (ОКС)
Оказание медицинской помощи при остром коронарном синдроме (ОКС) Аллергические состояния, проявления в полости рта. Клиника, диагностика, лечение
Аллергические состояния, проявления в полости рта. Клиника, диагностика, лечение № 2 Симптомдық артериальды гипертензия. № 3 вариант: Иценко-Кушинг синдромы кезіндегі
№ 2 Симптомдық артериальды гипертензия. № 3 вариант: Иценко-Кушинг синдромы кезіндегі Синдром уплотнения легочной ткани. Пневмония
Синдром уплотнения легочной ткани. Пневмония