Содержание
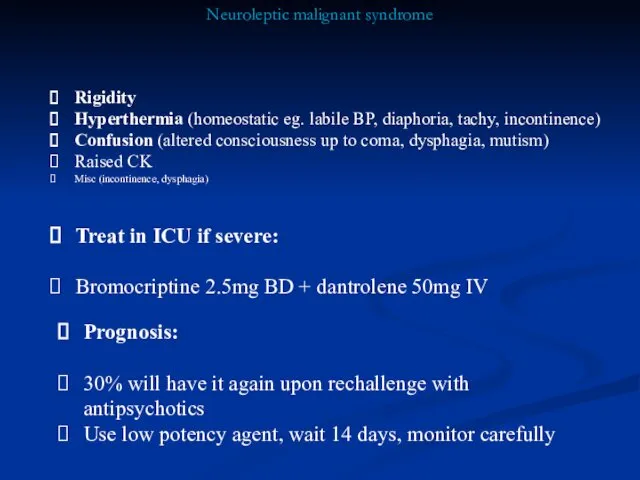
- 2. Neuroleptic malignant syndrome Rigidity Hyperthermia (homeostatic eg. labile BP, diaphoria, tachy, incontinence) Confusion (altered consciousness up
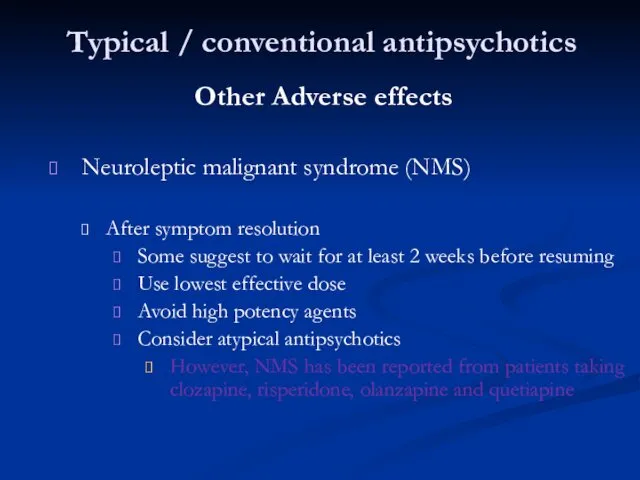
- 3. Typical / conventional antipsychotics Other Adverse effects Neuroleptic malignant syndrome (NMS) After symptom resolution Some suggest
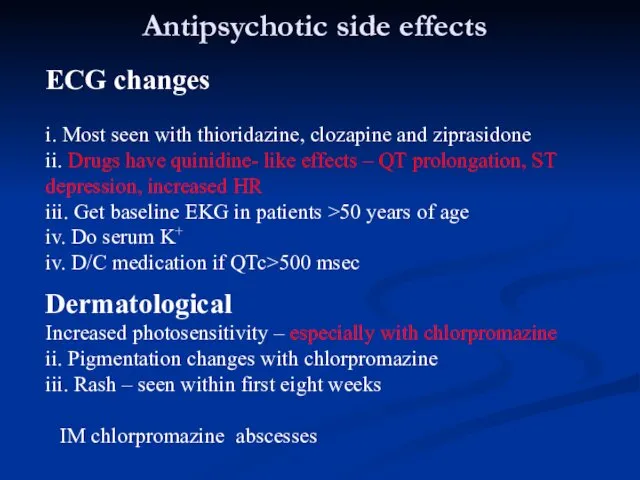
- 4. Antipsychotic side effects ECG changes i. Most seen with thioridazine, clozapine and ziprasidone ii. Drugs have
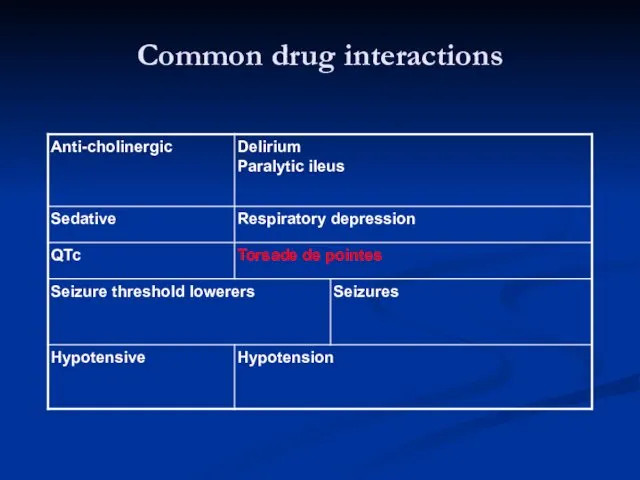
- 5. Common drug interactions
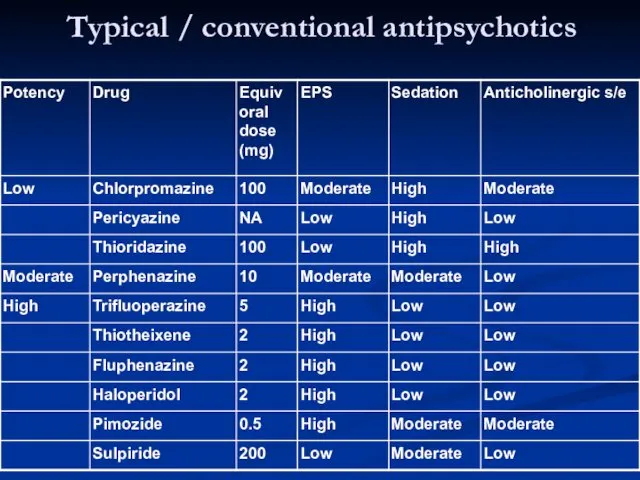
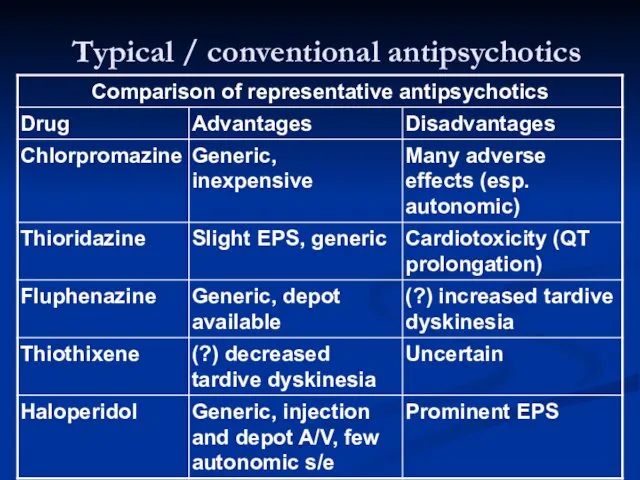
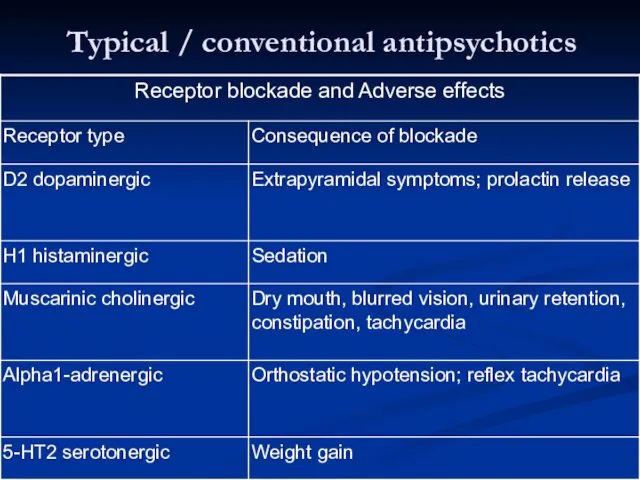
- 6. Typical / conventional antipsychotics
- 7. Typical / conventional antipsychotics
- 8. Typical / conventional antipsychotics
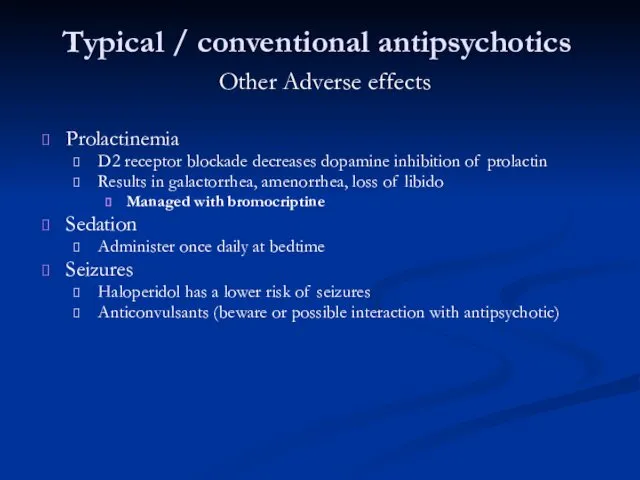
- 10. Typical / conventional antipsychotics Other Adverse effects Prolactinemia D2 receptor blockade decreases dopamine inhibition of prolactin
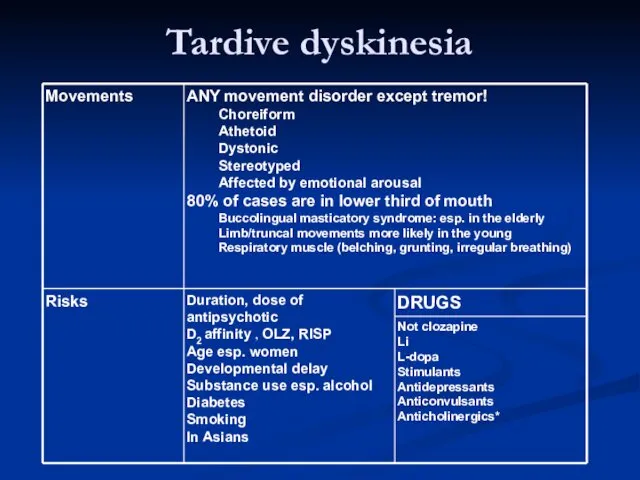
- 11. Tardive dyskinesia
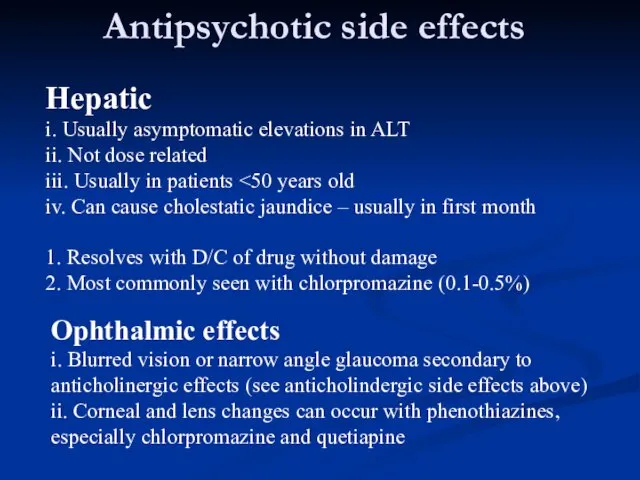
- 12. Antipsychotic side effects Hepatic i. Usually asymptomatic elevations in ALT ii. Not dose related iii. Usually
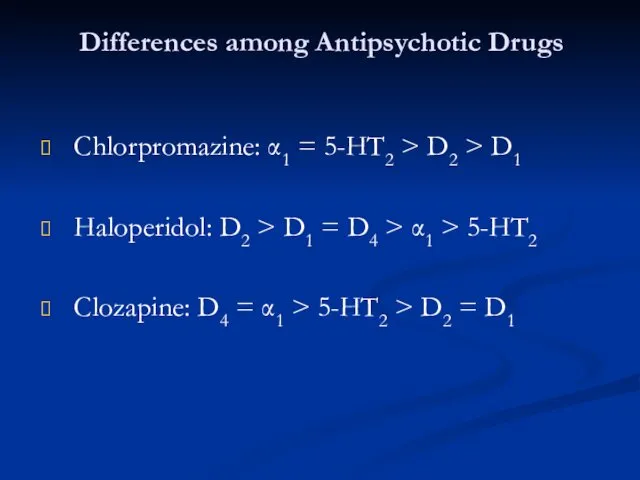
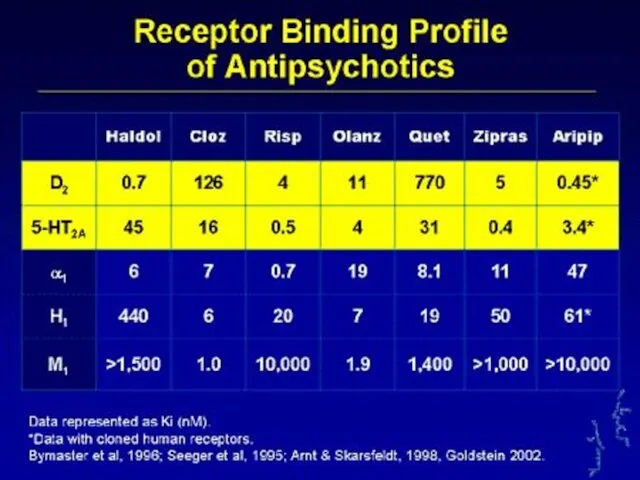
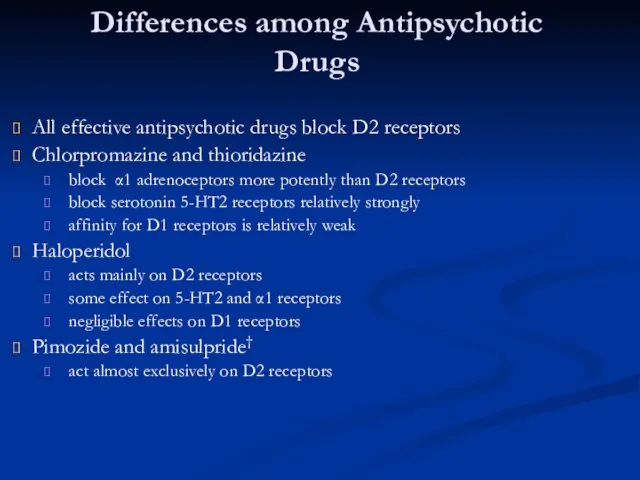
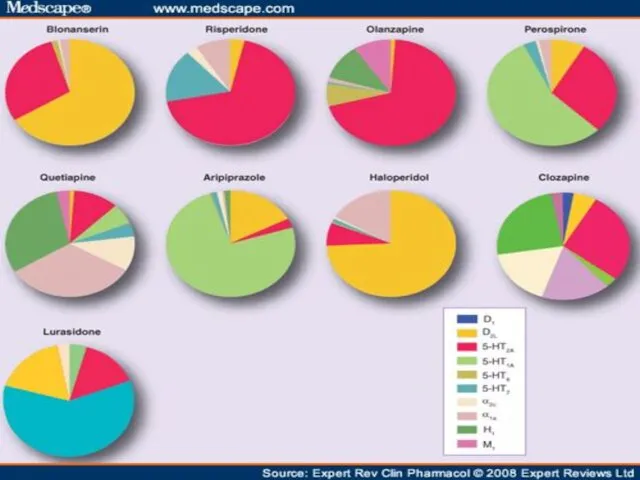
- 13. Differences among Antipsychotic Drugs Chlorpromazine: α1 = 5-HT2 > D2 > D1 Haloperidol: D2 > D1
- 15. Differences among Antipsychotic Drugs All effective antipsychotic drugs block D2 receptors Chlorpromazine and thioridazine block α1
- 16. Atypical antipsychotics
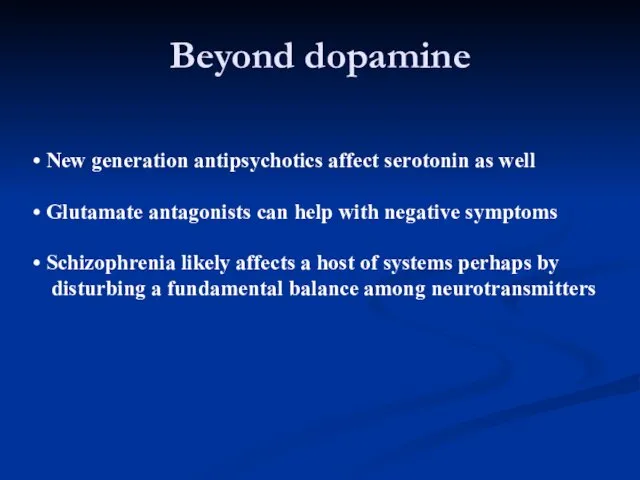
- 17. Beyond dopamine New generation antipsychotics affect serotonin as well Glutamate antagonists can help with negative symptoms
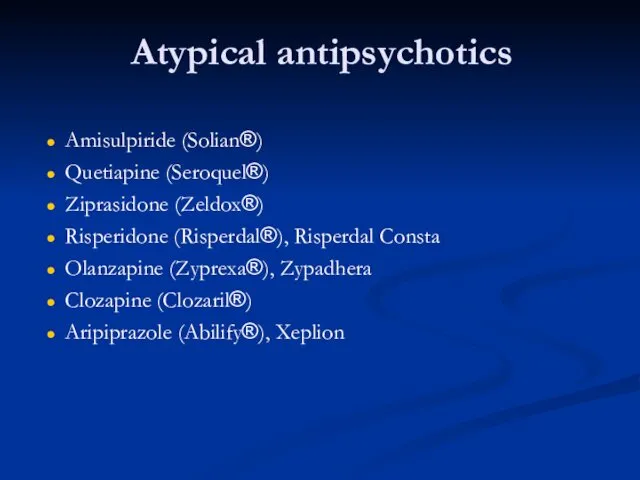
- 18. Atypical antipsychotics Amisulpiride (Solian®) Quetiapine (Seroquel®) Ziprasidone (Zeldox®) Risperidone (Risperdal®), Risperdal Consta Olanzapine (Zyprexa®), Zypadhera Clozapine
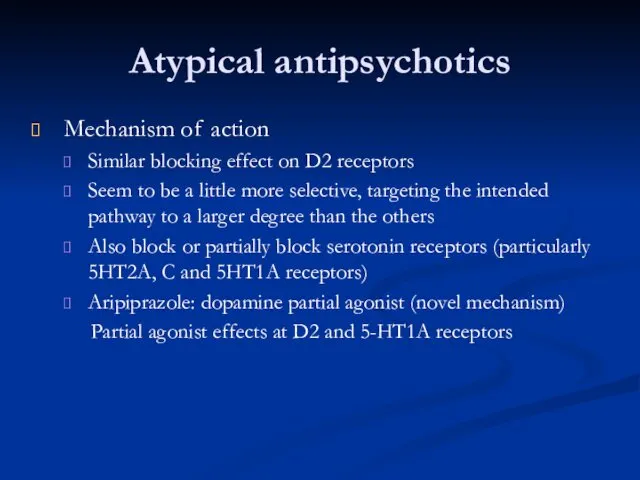
- 20. Atypical antipsychotics Mechanism of action Similar blocking effect on D2 receptors Seem to be a little
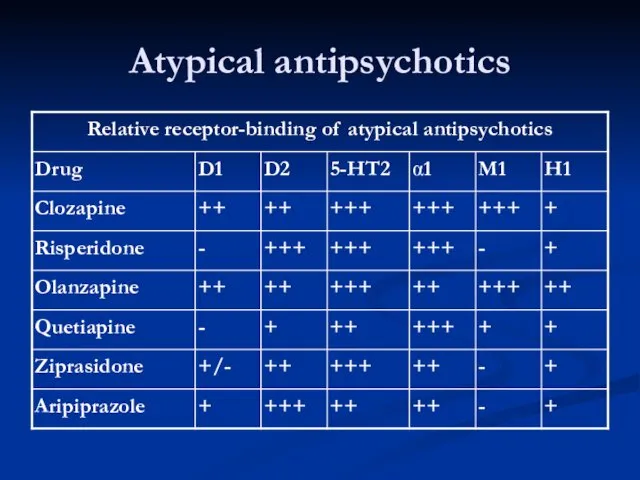
- 21. Atypical antipsychotics
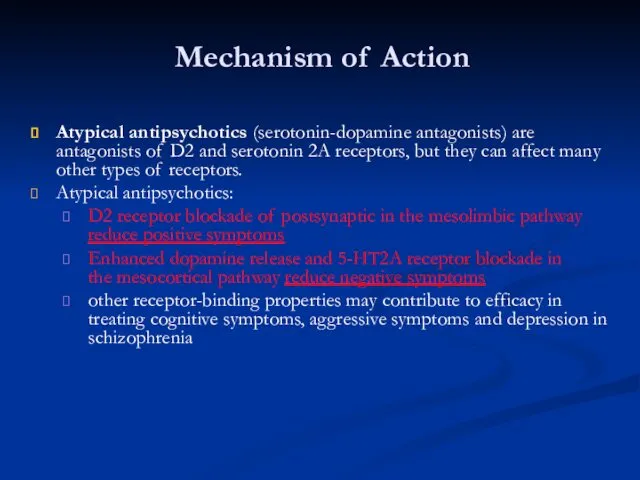
- 22. Mechanism of Action Atypical antipsychotics (serotonin-dopamine antagonists) are antagonists of D2 and serotonin 2A receptors, but
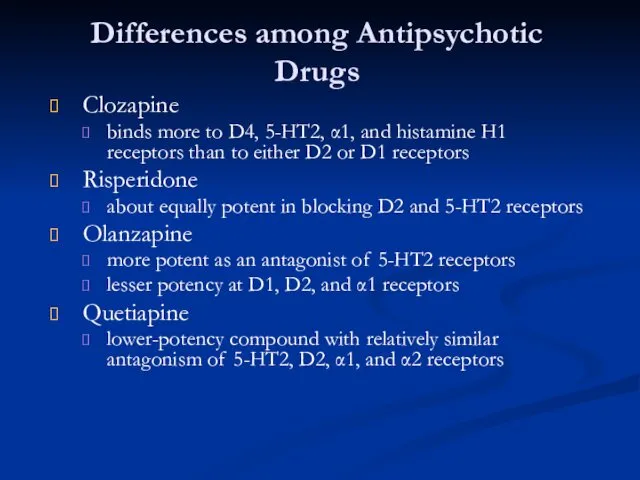
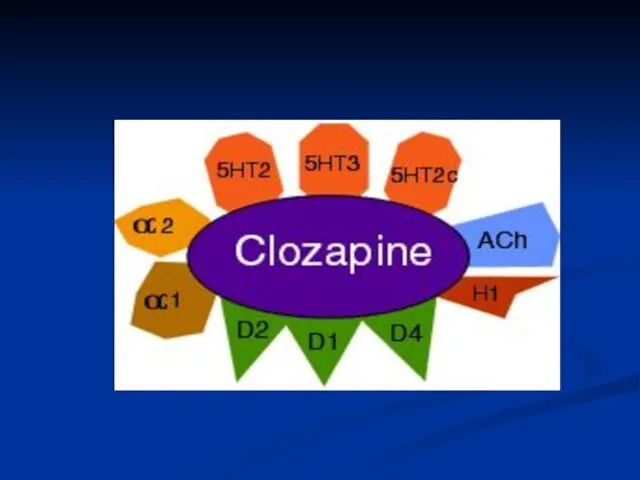
- 23. Differences among Antipsychotic Drugs Clozapine binds more to D4, 5-HT2, α1, and histamine H1 receptors than
- 24. Atypical antipsychotics lower doses reduced side effects more effective (especially negative symptoms) better compliance Evidence? trials
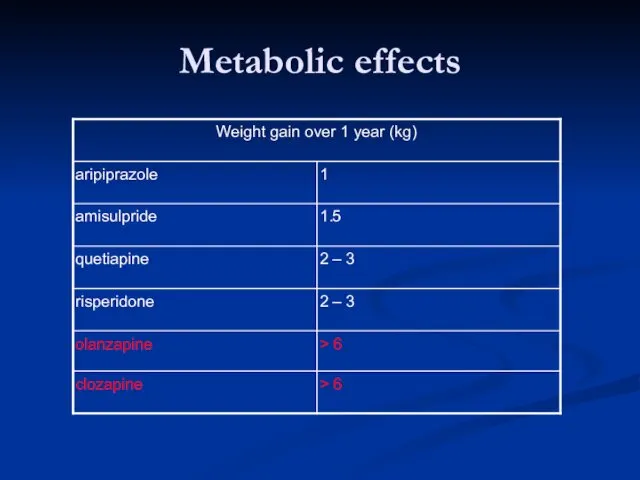
- 25. Metabolic effects
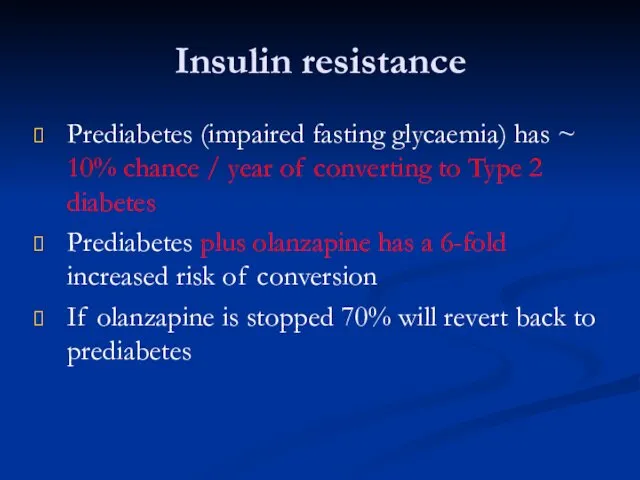
- 26. Insulin resistance Prediabetes (impaired fasting glycaemia) has ~ 10% chance / year of converting to Type
- 27. Stroke in the elderly Risperidone and olanzapine associated with increased risk of stroke when used for
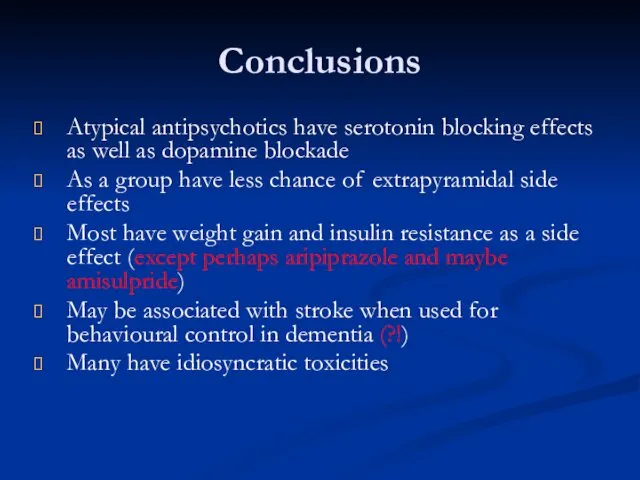
- 28. Conclusions Atypical antipsychotics have serotonin blocking effects as well as dopamine blockade As a group have
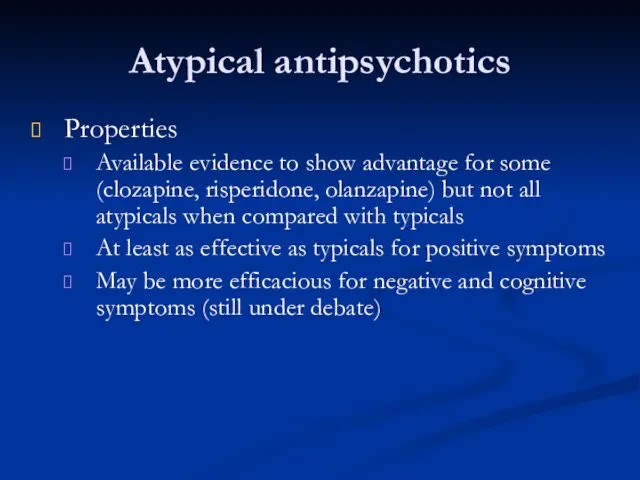
- 29. Atypical antipsychotics Properties Available evidence to show advantage for some (clozapine, risperidone, olanzapine) but not all
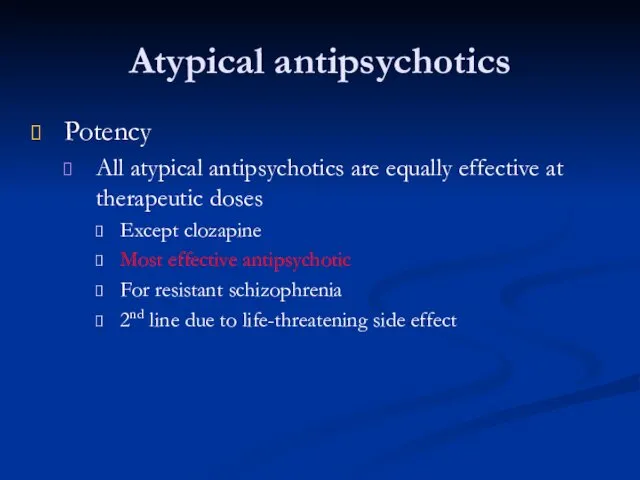
- 30. Atypical antipsychotics Potency All atypical antipsychotics are equally effective at therapeutic doses Except clozapine Most effective
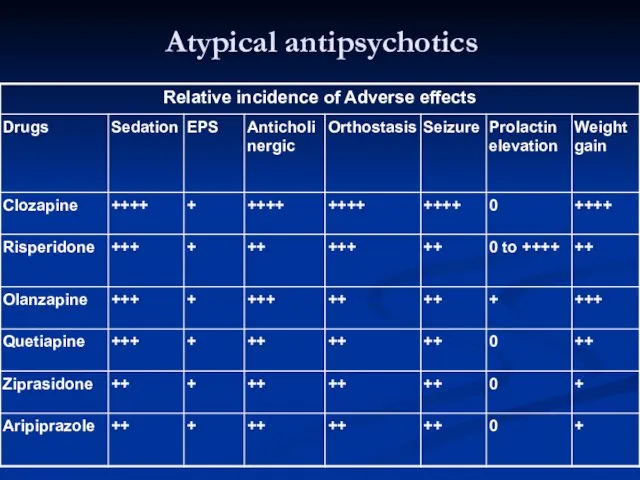
- 31. Atypical antipsychotics
- 32. Atypical antipsychotics 1st line atypical antipsychotics All atypicals except clozapine NICE recommendations Atypical antipsychotics considered when
- 33. Atypical antipsychotics 2nd line atypical antipsychotic Clozapine Most effective antipsychotic for reducing symptoms and preventing relapse
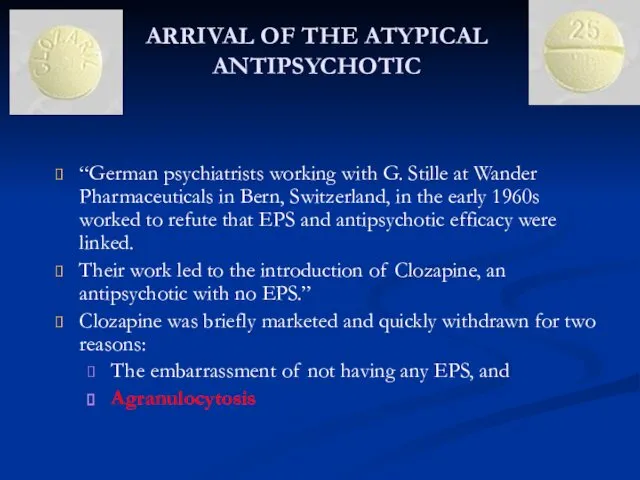
- 34. ARRIVAL OF THE ATYPICAL ANTIPSYCHOTIC “German psychiatrists working with G. Stille at Wander Pharmaceuticals in Bern,
- 36. NEUROBIOLOGY OF CLOZAPINE All schizophrenic patients do not respond to antipsychotics that have an affinity for
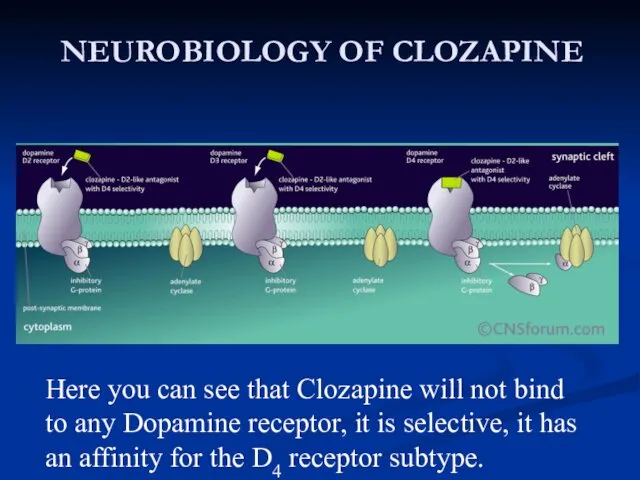
- 37. NEUROBIOLOGY OF CLOZAPINE Here you can see that Clozapine will not bind to any Dopamine receptor,
- 38. Mechanism of Action The exact mechanism of action unknown, however, it is believed that Clozapine selectively
- 39. Dosages and Treatment Length The regular dosage given to patients is approximately 900mg per day, but
- 40. Atypical antipsychotics Clozapine BNF (British National Formulary)52 (September 2006) Leucocyte and differential blood count normal before
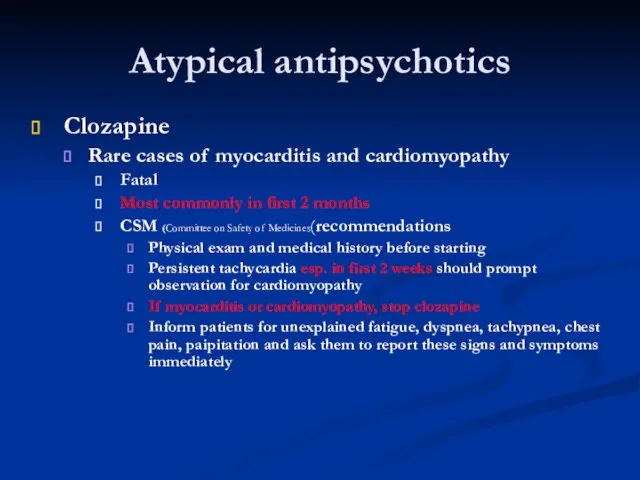
- 41. Atypical antipsychotics Clozapine Rare cases of myocarditis and cardiomyopathy Fatal Most commonly in first 2 months
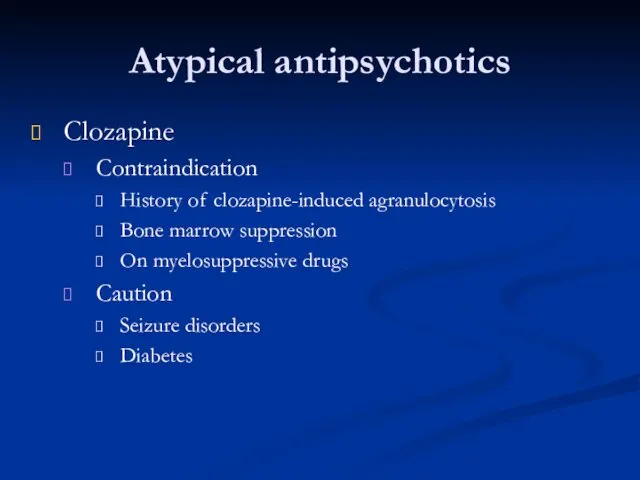
- 42. Atypical antipsychotics Clozapine Contraindication History of clozapine-induced agranulocytosis Bone marrow suppression On myelosuppressive drugs Caution Seizure
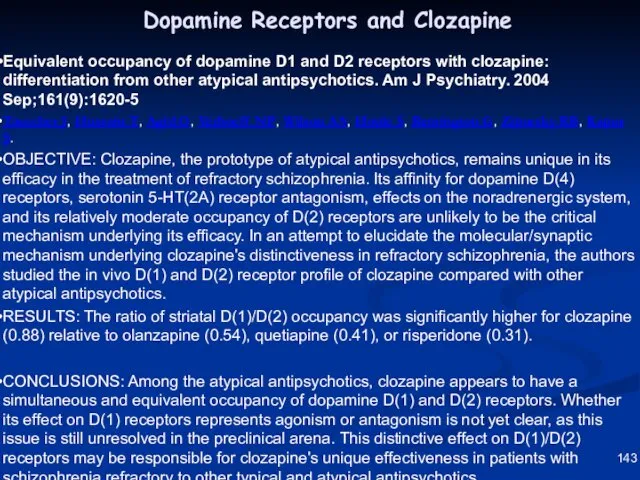
- 43. 143 Equivalent occupancy of dopamine D1 and D2 receptors with clozapine: differentiation from other atypical antipsychotics.
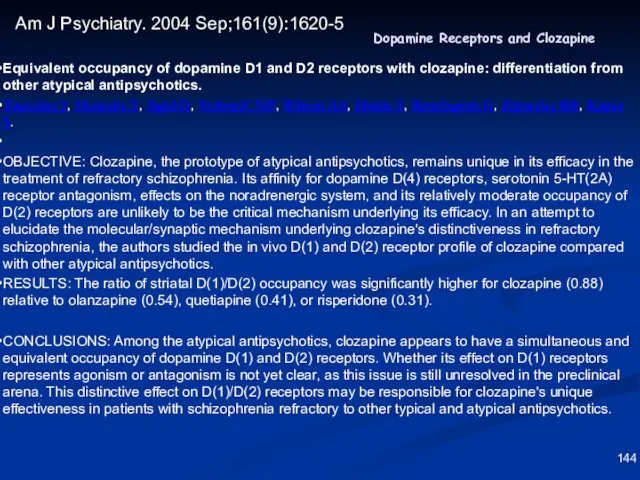
- 44. 144 Equivalent occupancy of dopamine D1 and D2 receptors with clozapine: differentiation from other atypical antipsychotics.
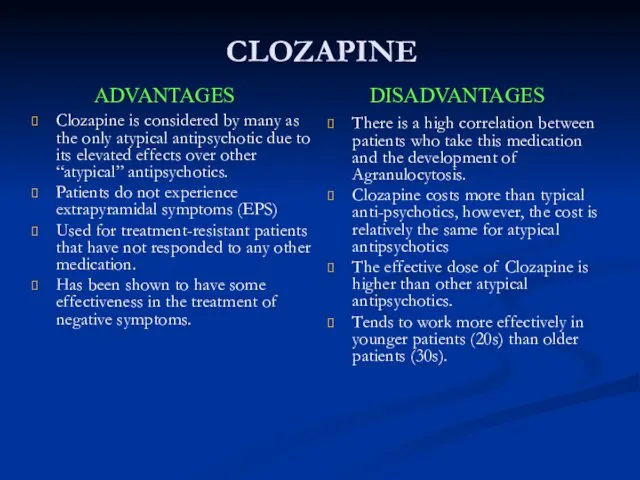
- 45. CLOZAPINE Clozapine is considered by many as the only atypical antipsychotic due to its elevated effects
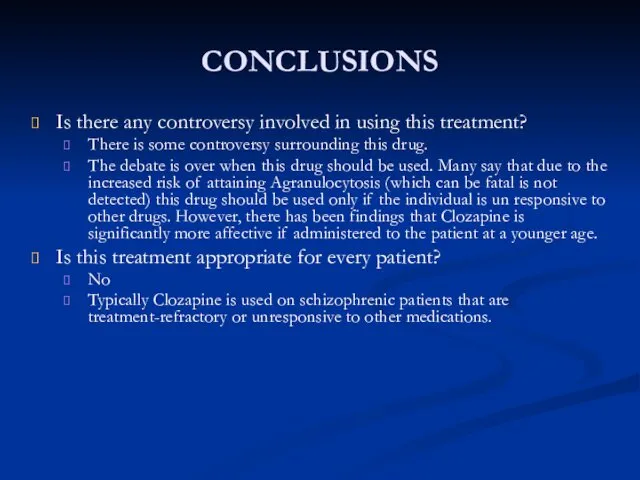
- 46. CONCLUSIONS Is there any controversy involved in using this treatment? There is some controversy surrounding this
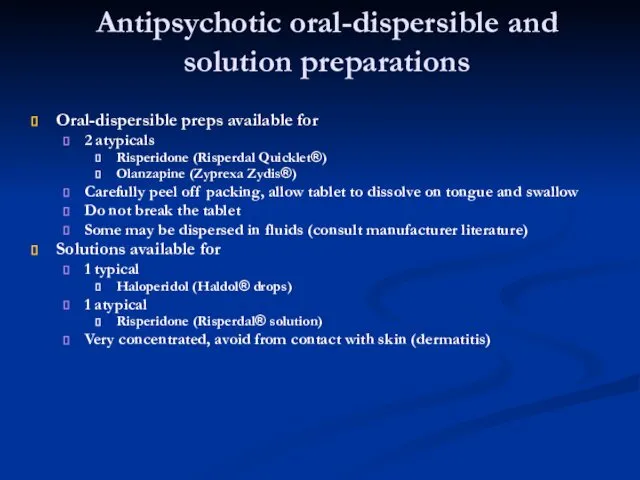
- 47. Antipsychotic oral-dispersible and solution preparations Oral-dispersible preps available for 2 atypicals Risperidone (Risperdal Quicklet®) Olanzapine (Zyprexa
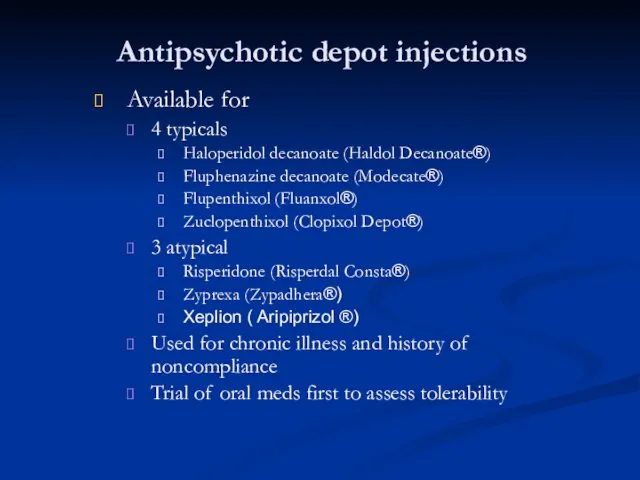
- 48. Antipsychotic depot injections Available for 4 typicals Haloperidol decanoate (Haldol Decanoate®) Fluphenazine decanoate (Modecate®) Flupenthixol (Fluanxol®)
- 49. Antipsychotics in schizophrenia Selection of typical antipsychotics Equally efficacious Chosen by side effect profile Atypical antipsychotics
- 50. Antipsychotics in schizophrenia Treatment response First 7 days Decreased agitation, hostility, combativeness, anxiety, tension and aggression
- 52. Antipsychotics in schizophrenia Acute phase Initiate therapy Titrate as tolerated to average effective dose Stabilization phase
- 53. Non-antipsychotic agents Benzodiazepines Useful in some studies for anxiety, agitation, global impairment and psychosis Schizophrenic patients
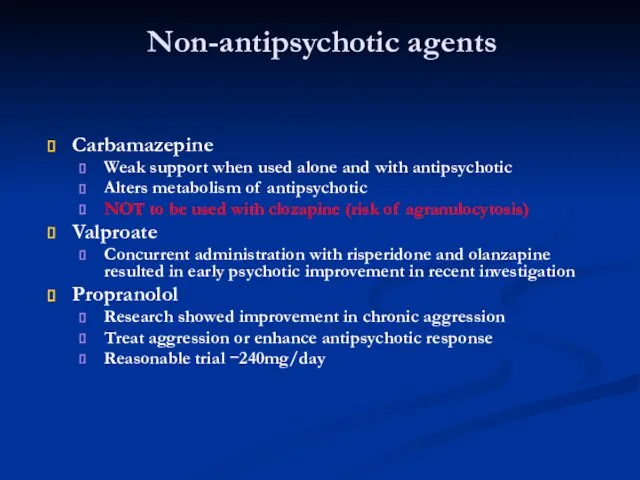
- 54. Non-antipsychotic agents Carbamazepine Weak support when used alone and with antipsychotic Alters metabolism of antipsychotic NOT
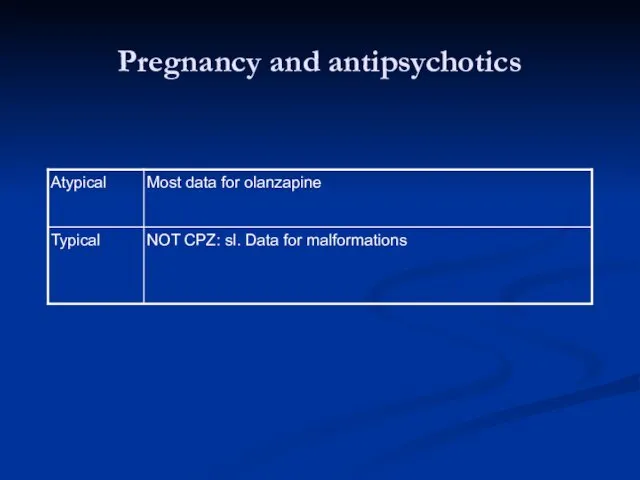
- 55. Pregnancy and antipsychotics
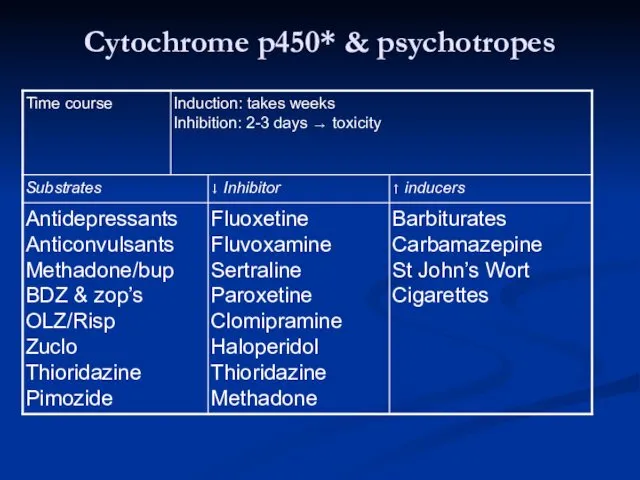
- 56. Cytochrome p450* & psychotropes
- 58. Скачать презентацию




 Синдромы поражения височной доли
Синдромы поражения височной доли Противоэпилептические средства
Противоэпилептические средства Повышенная воздушность лёгких
Повышенная воздушность лёгких Заседание Президиума Профсоюза
Заседание Президиума Профсоюза Роль ранней вертикализации в функциональном восстановлении больных с острым инсультом
Роль ранней вертикализации в функциональном восстановлении больных с острым инсультом Ісіктерге қысқаша шолу, ісіктердің пайда болуы
Ісіктерге қысқаша шолу, ісіктердің пайда болуы Sepsis of newborns
Sepsis of newborns Современные антисептические средства
Современные антисептические средства Методики лечения пульпита не сохраняющие жизнеспособность пульпы
Методики лечения пульпита не сохраняющие жизнеспособность пульпы Экстракорпоральные методы лечения сепсиса
Экстракорпоральные методы лечения сепсиса Артерии и вены большого круга кровообращения. Особенности коронарного кровообращения. (Лекция 13.2)
Артерии и вены большого круга кровообращения. Особенности коронарного кровообращения. (Лекция 13.2) Первая помощь при отморожении
Первая помощь при отморожении Стрептококковые пиодермиты
Стрептококковые пиодермиты Световая микроскопия
Световая микроскопия 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation
2020 ESC Guidelines for the diagnosis and management of atrial fibrillation Азық микотоксикоздар
Азық микотоксикоздар Инфаркт миокарда
Инфаркт миокарда Современные подходы к фармакотерапии ХВН с позиций коррекции эндотелиальной дисфункции
Современные подходы к фармакотерапии ХВН с позиций коррекции эндотелиальной дисфункции Респираторный дистресс-синдром
Респираторный дистресс-синдром ГБУЗ НО Дзержинский перинатальный центр
ГБУЗ НО Дзержинский перинатальный центр Патофизиология. Повреждение клетки. (Лекция 6)
Патофизиология. Повреждение клетки. (Лекция 6) Сбор данных для системы контроля качества в здравоохранении
Сбор данных для системы контроля качества в здравоохранении Артросиндесмология. Соединение костей
Артросиндесмология. Соединение костей КТ и МРТ
КТ и МРТ Фурункул, карбункул, рожа, панариций и др. Хирургическая инфекция мягких тканей
Фурункул, карбункул, рожа, панариций и др. Хирургическая инфекция мягких тканей Психофизиологические основы учебного и производственного труда. Средства физической культуры в регулировании работоспособности
Психофизиологические основы учебного и производственного труда. Средства физической культуры в регулировании работоспособности Хорея Сиденгама
Хорея Сиденгама Анаэробная раневая инфекция (газовая гангрена)
Анаэробная раневая инфекция (газовая гангрена)