Содержание
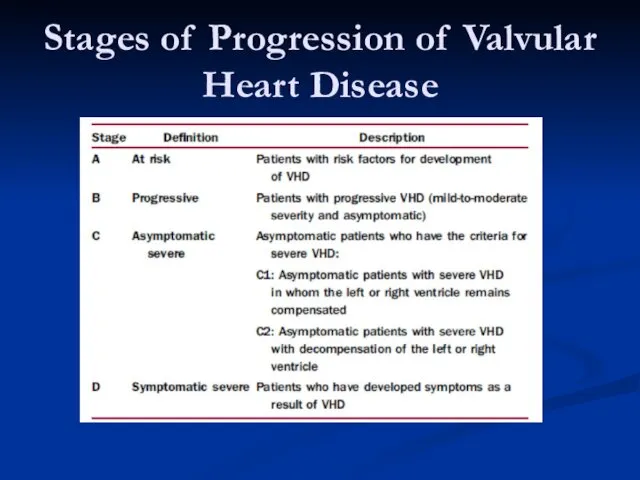
- 3. Stages of Progression of Valvular Heart Disease
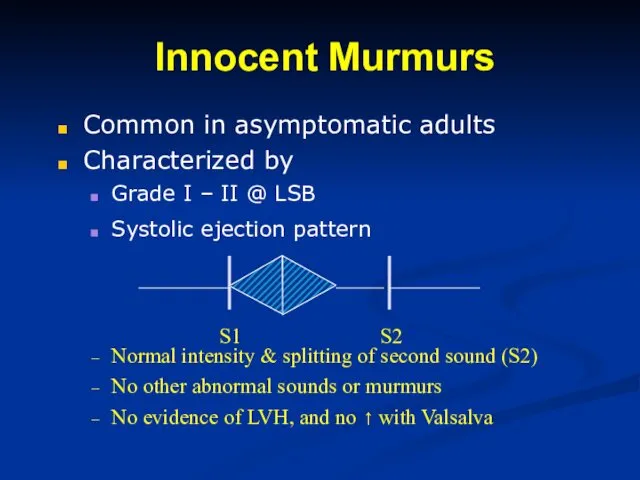
- 4. Innocent Murmurs Common in asymptomatic adults Characterized by Grade I – II @ LSB Systolic ejection
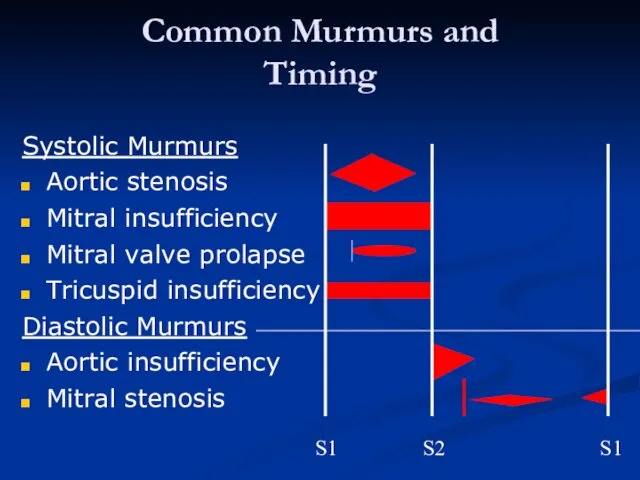
- 5. Common Murmurs and Timing Systolic Murmurs Aortic stenosis Mitral insufficiency Mitral valve prolapse Tricuspid insufficiency Diastolic
- 6. Mitral Valve Stenosis
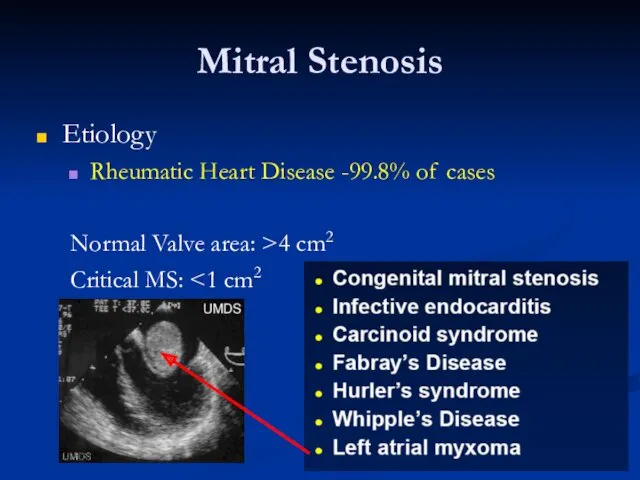
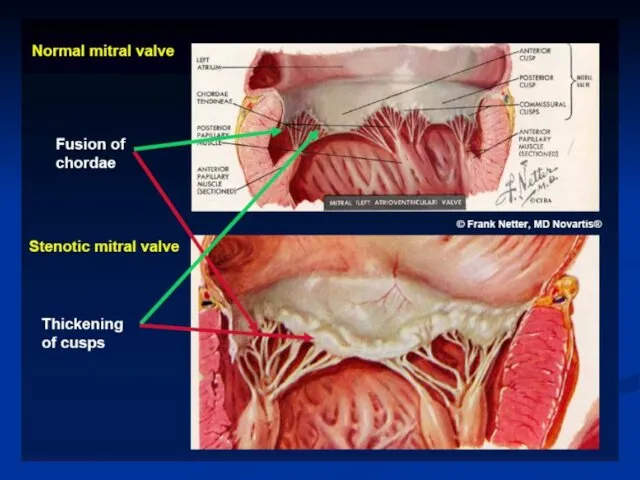
- 7. Mitral Stenosis Etiology Rheumatic Heart Disease -99.8% of cases Normal Valve area: >4 cm2 Critical MS:
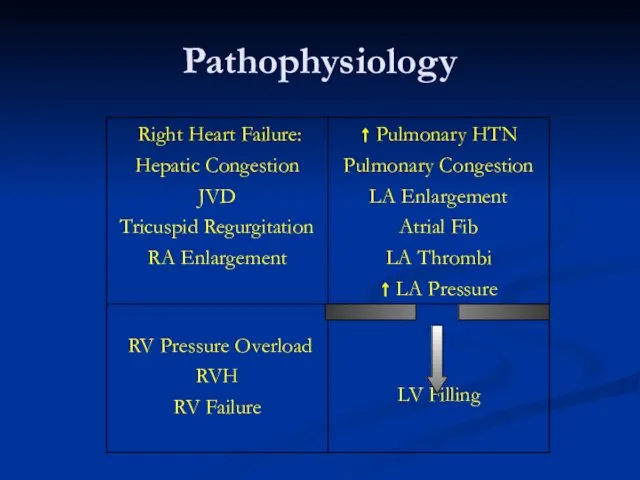
- 9. Pathophysiology
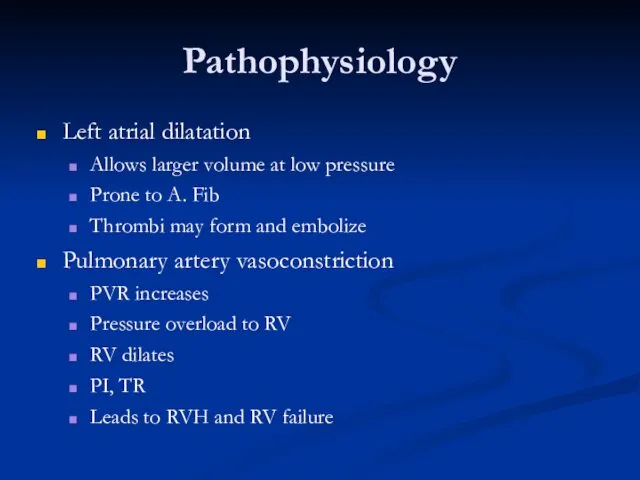
- 10. Pathophysiology Left atrial dilatation Allows larger volume at low pressure Prone to A. Fib Thrombi may
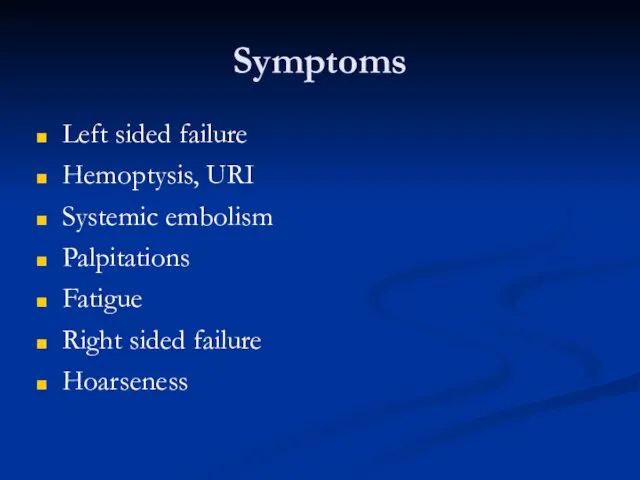
- 11. Symptoms Left sided failure Hemoptysis, URI Systemic embolism Palpitations Fatigue Right sided failure Hoarseness
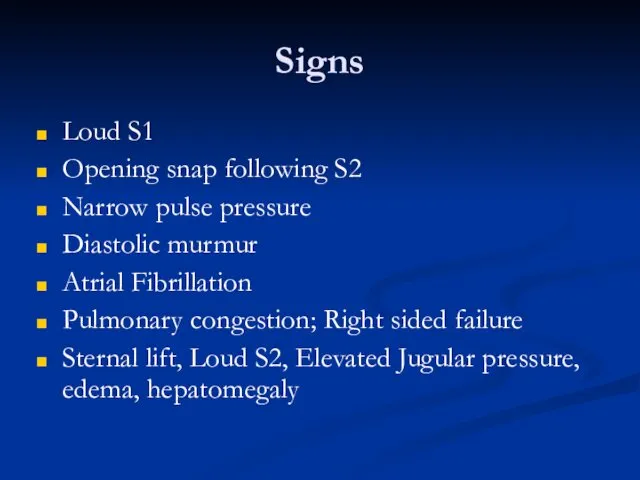
- 12. Signs Loud S1 Opening snap following S2 Narrow pulse pressure Diastolic murmur Atrial Fibrillation Pulmonary congestion;
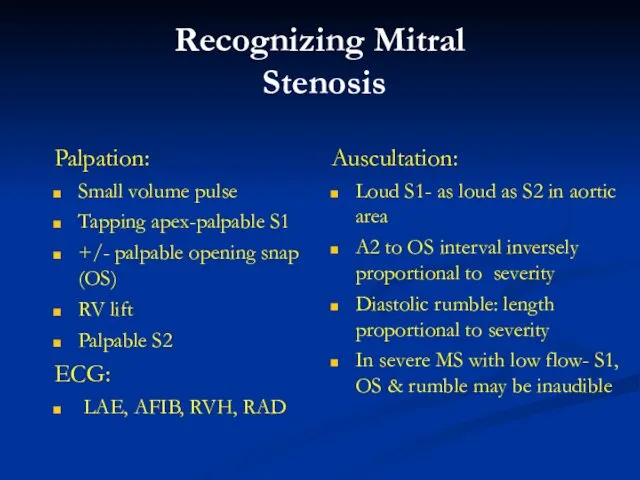
- 13. Recognizing Mitral Stenosis Palpation: Small volume pulse Tapping apex-palpable S1 +/- palpable opening snap (OS) RV
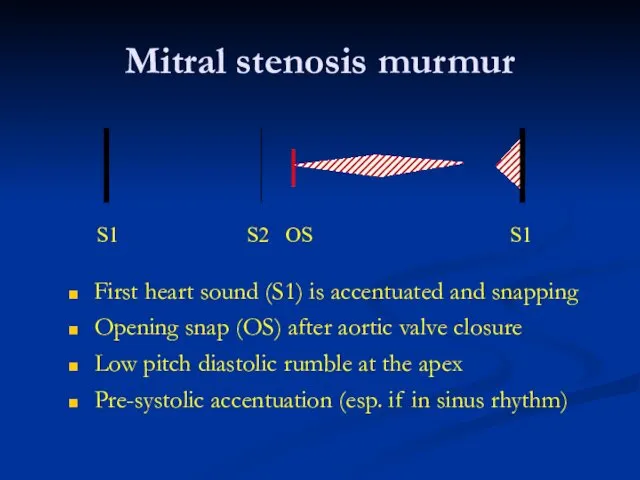
- 14. Mitral stenosis murmur First heart sound (S1) is accentuated and snapping Opening snap (OS) after aortic
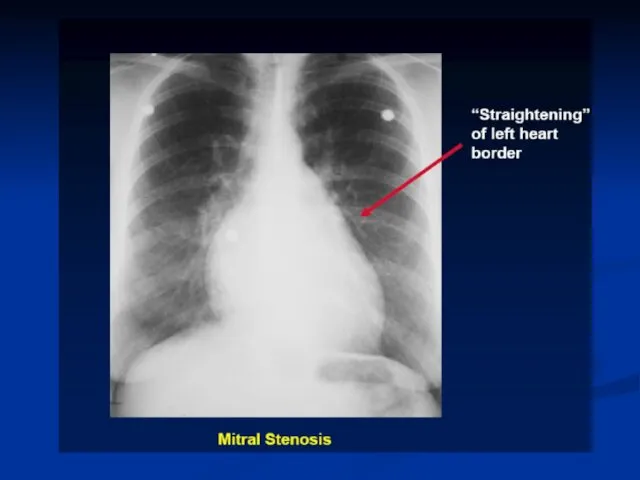
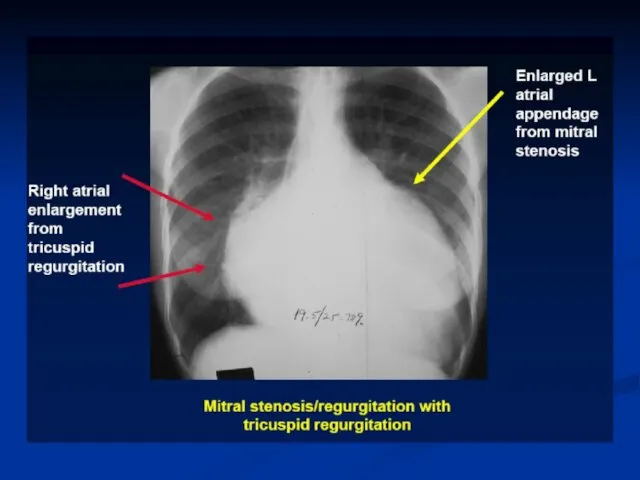
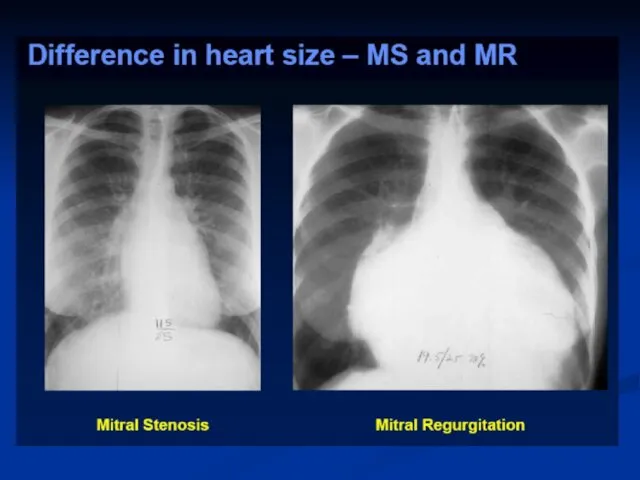
- 15. Lab Diagnosis EKG: A Fib, LAE, RVH CXR: Large LA, Pulm venous congestion, RV dilatation, interstitial/alveolar
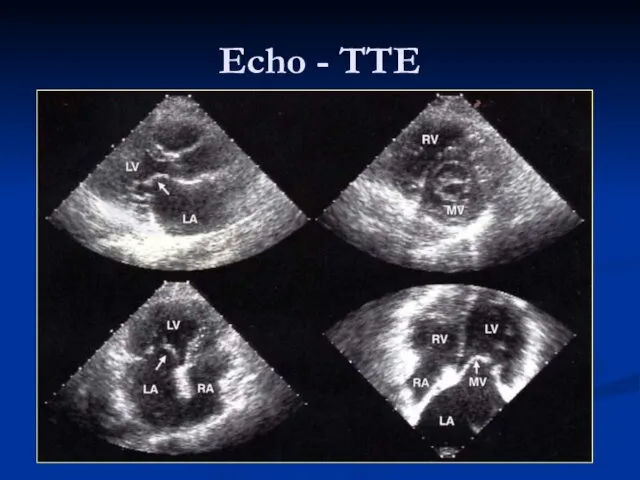
- 18. Echo - TTE
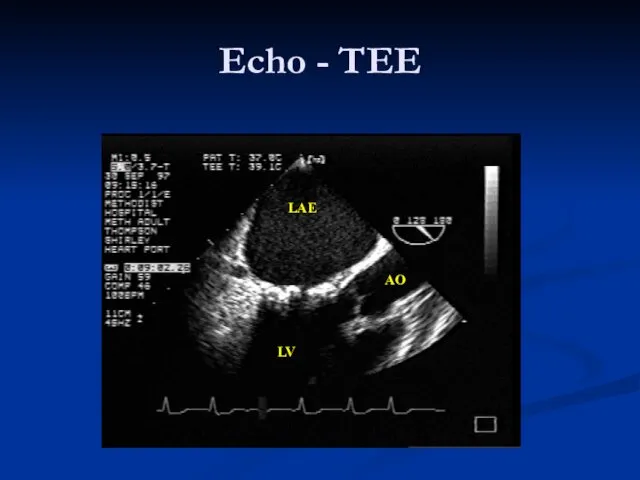
- 19. LAE LV AO Echo - TEE
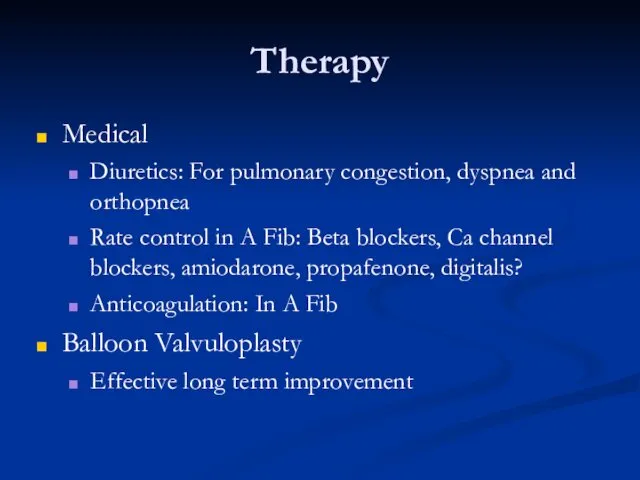
- 20. Therapy Medical Diuretics: For pulmonary congestion, dyspnea and orthopnea Rate control in A Fib: Beta blockers,
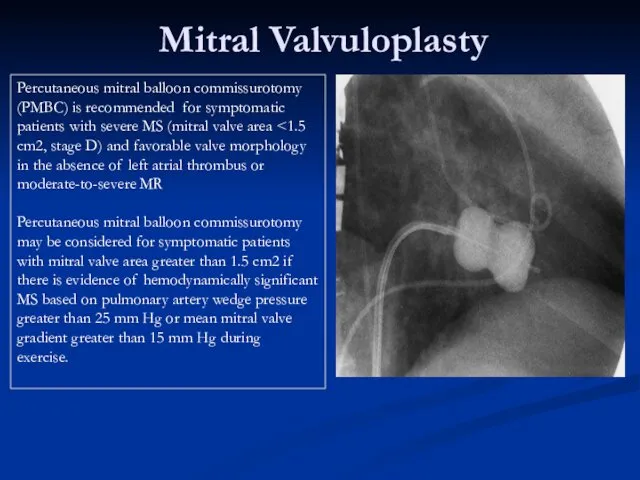
- 21. Mitral Valvuloplasty Percutaneous mitral balloon commissurotomy (PMBC) is recommended for symptomatic patients with severe MS (mitral
- 25. Therapy Surgical Mitral commissurotomy: Effective long term improvement Mitral Valve Replacement Mechanical Bioprosthetic
- 26. MV Surgery Mitral valve surgery (repair, commissurotomy, or valve replacement) is indicated in severely symptomatic patients
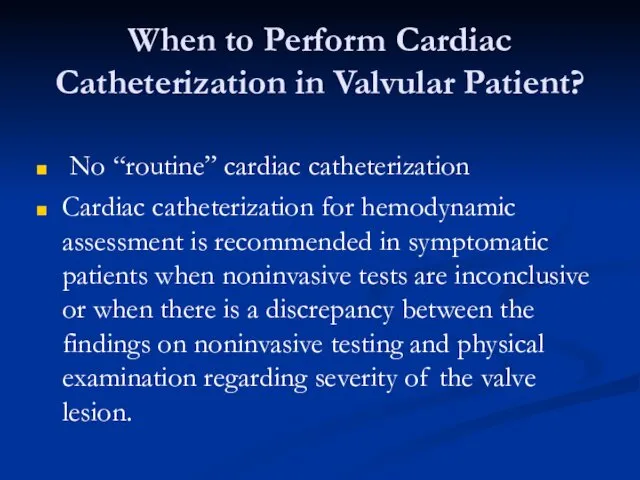
- 28. When to Perform Cardiac Catheterization in Valvular Patient? No “routine” cardiac catheterization Cardiac catheterization for hemodynamic
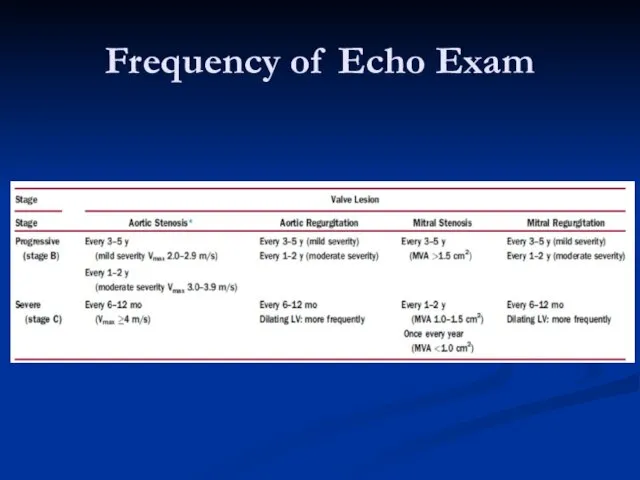
- 29. Frequency of Echo Exam
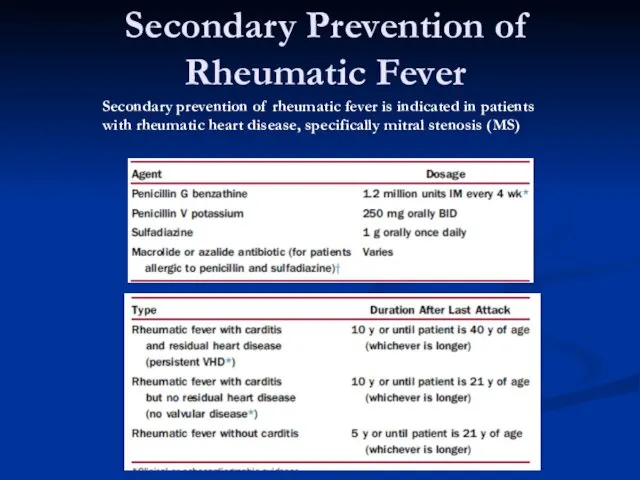
- 30. Secondary Prevention of Rheumatic Fever Secondary prevention of rheumatic fever is indicated in patients with rheumatic
- 31. Mitral Regurgitation
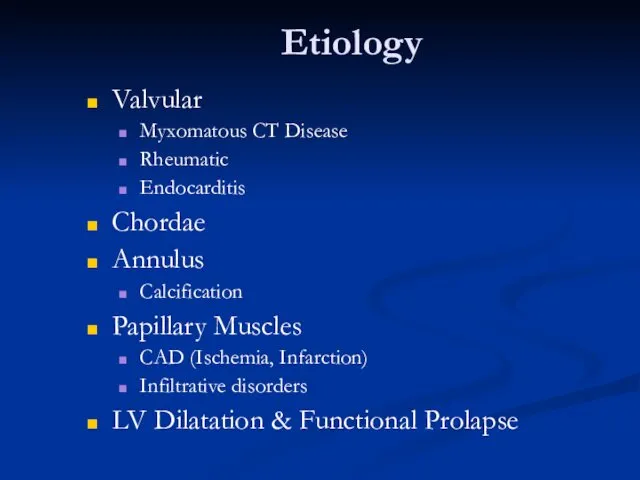
- 32. Etiology Valvular Myxomatous CT Disease Rheumatic Endocarditis Chordae Annulus Calcification Papillary Muscles CAD (Ischemia, Infarction) Infiltrative
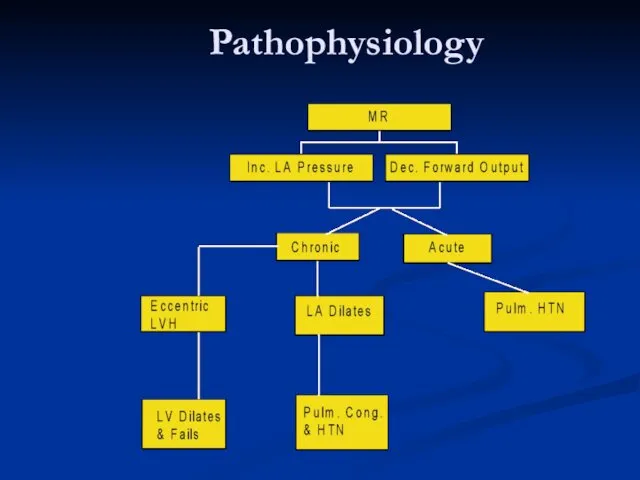
- 33. Pathophysiology
- 34. Symptoms Similar to MS Dyspnea, Orthopnea, PND Fatigue Pulmonary HTN, Right sided failure Systemic embolization in
- 35. Signs Chronic MR Hyperdynamic, Displaced apex beat Apical holosystolic murmur Pounding pulse Variable Pulm. HTN Acute
- 36. Diagnosis EKG: LVH, LAE CXR: Cardiac enlargement Echo: Abnormal anatomy, chamber size, EF, Qualitative assessment of
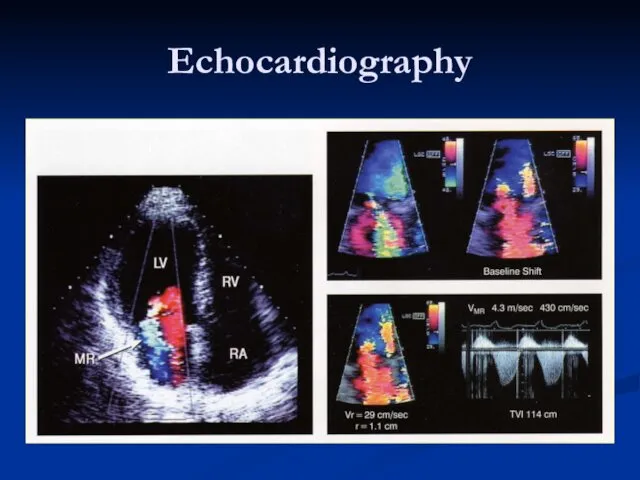
- 39. Echocardiography
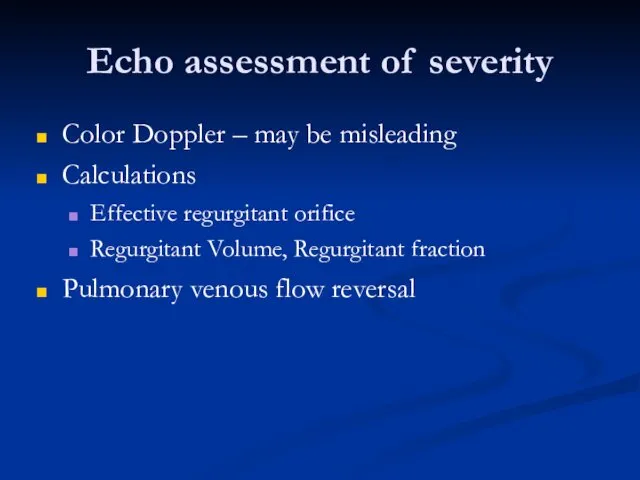
- 40. Echo assessment of severity Color Doppler – may be misleading Calculations Effective regurgitant orifice Regurgitant Volume,
- 41. Therapy MEDICAL Diuretics: reduce vol. Overload Vasodilators: Increase forward output and decrease LV size Digitalis: Control
- 45. MV Repair 1. Mitral valve repair is performed at a lower operative mortality rate than MVR.
- 46. Mitral Valve Prolapse
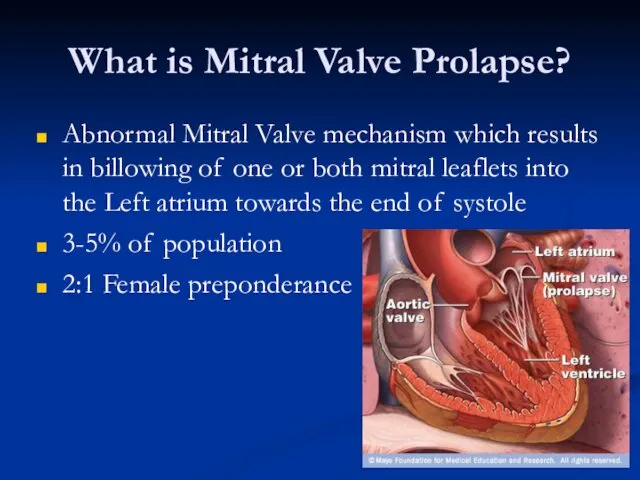
- 47. What is Mitral Valve Prolapse? Abnormal Mitral Valve mechanism which results in billowing of one or
- 48. Pathophysiology Forms Functional Common LV is small, Hyperdynamic Valve is normal Organic (Myxomatous Degeneration) Uncommon LV:
- 49. Symptoms Most patients: None Chest pain Palpitations Easy fatigability Arrhythmias TIA MR
- 50. Signs Mid-systolic Click Systolic murmur with co-existent MR Other connective tissue disorders
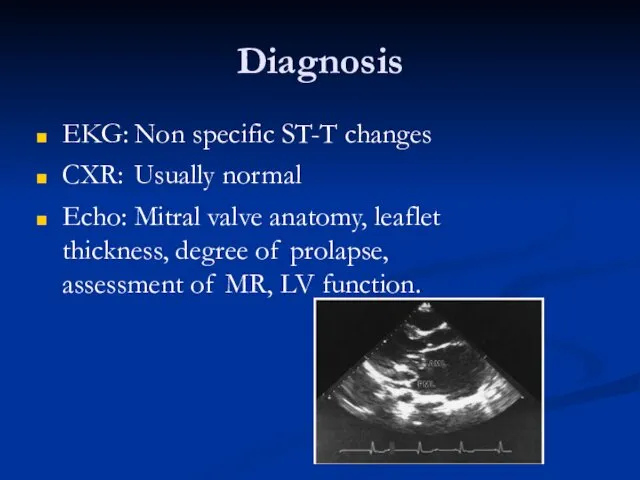
- 51. Diagnosis EKG: Non specific ST-T changes CXR: Usually normal Echo: Mitral valve anatomy, leaflet thickness, degree
- 53. Скачать презентацию







 Головные вши (Pediculus humanus capitis)
Головные вши (Pediculus humanus capitis) Гипоплазия эмали: этиология, патогенез, клиника, диагностика, лечение. Наследственные пороки развития твердых тканей зубов
Гипоплазия эмали: этиология, патогенез, клиника, диагностика, лечение. Наследственные пороки развития твердых тканей зубов Көз туберкулезі
Көз туберкулезі Анализ результатов лечения гидроцефалии у детей
Анализ результатов лечения гидроцефалии у детей Основные принципы асептики в терапевтической стоматологии. Инфекционный контроль
Основные принципы асептики в терапевтической стоматологии. Инфекционный контроль Организация ортопедического отделения. Зуботехническая лаборатория
Организация ортопедического отделения. Зуботехническая лаборатория Лечебная физкультура
Лечебная физкультура Стационарлық көмек деңгейіндегі заманауи автоматтандырылған деректер базасымен таныстыру
Стационарлық көмек деңгейіндегі заманауи автоматтандырылған деректер базасымен таныстыру Обеспечение безопасного пространства для пациента и персонала в медицинских организациях
Обеспечение безопасного пространства для пациента и персонала в медицинских организациях Рациональное питание
Рациональное питание Закаливание организма
Закаливание организма Служение больницы и учреждения. Анонимные Наркоманы
Служение больницы и учреждения. Анонимные Наркоманы Одонтогенді гайморит
Одонтогенді гайморит Firearm injuries
Firearm injuries Прививка против гриппа
Прививка против гриппа Особенности сестринского ухода в гериатрии. Болезни органов дыхания у гериатрических пациентов
Особенности сестринского ухода в гериатрии. Болезни органов дыхания у гериатрических пациентов Компенсаторно-приспособительные реакции
Компенсаторно-приспособительные реакции Правила постановки периферического венозного катетера
Правила постановки периферического венозного катетера Тағамдық және санитарлы микробиология
Тағамдық және санитарлы микробиология Особо опасные инфекции (ООИ)
Особо опасные инфекции (ООИ) Гангрена, некроз, язвы, свищи
Гангрена, некроз, язвы, свищи Жүктілік кезіндегі гипертензивті жағдайлар
Жүктілік кезіндегі гипертензивті жағдайлар Дүниежүзілік денсаулық сақтау ұйымы (ДДҰ) Қазақстанда
Дүниежүзілік денсаулық сақтау ұйымы (ДДҰ) Қазақстанда Оқу кестелері мен муляждарды қолдану арқылы ауыз қуысы мен ауыз қуысы құрылымдарының функцияларын зерттеу
Оқу кестелері мен муляждарды қолдану арқылы ауыз қуысы мен ауыз қуысы құрылымдарының функцияларын зерттеу Патогенна дія хімічних та біологічних факторів на організм. Роль спадковості в патології. (Лекція 4)
Патогенна дія хімічних та біологічних факторів на організм. Роль спадковості в патології. (Лекція 4) Средства, влияющие на афферентную нервную систему
Средства, влияющие на афферентную нервную систему Хірургічні захворювання прямої кишки
Хірургічні захворювання прямої кишки Алгоритм манипуляций по оказанию больным первой медицинской помощи при возникновении неотложных ситуаций
Алгоритм манипуляций по оказанию больным первой медицинской помощи при возникновении неотложных ситуаций